Abstract
We report a case of very late stent thrombosis 7 years post sirolimus eluting stent implantation presenting as ST elevation MI while on dual antiplatelet therapy. Angiography revealed an aneurysm at the proximal end of the stent. The patient was managed successfully by primary percutaneous coronary intervention (PCI) with adjunct thrombus aspiration and intracoronary abciximab administration followed by deploying a mesh-covered stent MGuard. This very late complication is a rare presentation after a drug illuting stent (DES).
Keywords: Coronary artery aneurysm, Stent thrombosis, Drug eluting stent
1. Introduction
Historically coronary artery aneurysms were first described by Morgagni in 1761.1,2 Coronary artery aneurysm, defined as dilatation of the coronary artery exceeding 50% of the reference vessel diameter, is uncommon and occurs in less than 5% of coronary angiographic series.3
We report a rare case of coronary aneurysm presenting as acute ST elevation MI (STEMI) secondary to very late stent thrombosis (VLST) 7 years after implantation of a first generation sirolimus eluting stent (SES) implantation.
2. Case report
A 52-year-old male normotensive, non-diabetic, non-smoker having strong family history of coronary artery disease (CAD) had effort angina in August 2006. Treadmill test (TMT) done subsequently was positive reversible myocardial ischemia (RMI). Coronary angiography done same month was suggestive of Double vessel disease: Left anterior descending artery (LAD) 90% mid segment stenosis and Left circumflex (LCX) 90% proximal and extending into a large obtuse marginal branch. Subsequently patient underwent angioplasty with stenting using a sirolimus eluting stent (Cypher) 3 × 13 mm to LAD, a Zotarolimus eluting stent (Endeavor) 3 × 24 mm to proximal LCX and a sirolimus eluting stent (Cypher) 2.5 × 28 mm to OM1 branch. Procedure was uncomplicated and the patient was discharged on dual antiplatelet therapy (aspirin and clopidogrel).
Patient was on a regular follow up after the procedure and was continued with long-term dual antiplatelet therapy due to a high-risk profile. In October 2009 patient developed chest discomfort, electrocardiogram (ECG) done subsequently was suggestive of acute inferior STEMI. Angiography done this time was suggestive of in stent thrombosis in the LCX and OM1 stents. The LAD stent was patent with no evidence of any aneurysm. plain old balloon angioplasty (POBA) was done to the culprit lesion followed by IV bolus of t-pa within 4 hours of symptoms. Patient recovered from procedure without complication. A check angiography was not done.
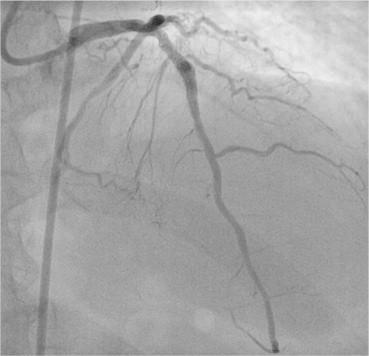
After this event patient continued on dual antiplatelet therapy along with statins, beta blocker and anti-ischemic therapy. TMT done in August 2010 was negative for RMI. Echocardiography showed an inferior wall hypokinesia and left ventricular ejection fraction (LVEF) 50%. In August 2013, 7 years after the first procedure patient had acute onset chest discomfort. Patient presented to hospital within 3 hours of onset of symptoms. ECG done was suggestive of acute anterior wall STEMI. He was immediately shifted to catheterization laboratory for primary angioplasty. Angiography done showed LAD in stent thrombosis with an aneurysm at proximal end of stent. There was angiographic visible thrombus in the stent and the vessel distal to it (Fig. 1). The guide wire initially went proximally between the malapposed stent and the vessel wall (Fig. 2). Although a 2 mm balloon went through the thrombosuction catheter did not go. Another wire was taken which was navigated through the correct path (Fig. 3). A thrombosuction followed by administration of intracoronary abciximab was done which made the vessel look angiographically free of thrombus (Fig. 4). Lesion was predilated with 2 × 12 mm balloon at 20 ATM and with 3 × 10 mm balloon at 10 ATM. The whole length was stented using a mesh-covered MGuard stent 3.5 × 29 mm (Inspire MD) deployed at 10 ATM. This was post dilated with 4 × 12 mm balloon at the site of the aneurysm with good angiographic result (Fig. 5). There was no slow flow encountered during the procedure. The thrombolysis in myocardial infarction (TIMI) flow was three at the end of the procedure. Patient became asymptomatic and was discharged in stable condition after 48 hours. The LVEF at discharge was 35% with a hypo kinetic anterior wall. Clopidogrel was changed to prasugrel and aspirin continued. Atorvastatin dose was increased to 80 mg, beta blockers and angiotensin converting enzyme inhibitors (ACEI) were continued in appropriate doses. 4 weeks following the procedure he is asymptomatic.
Fig. 1.
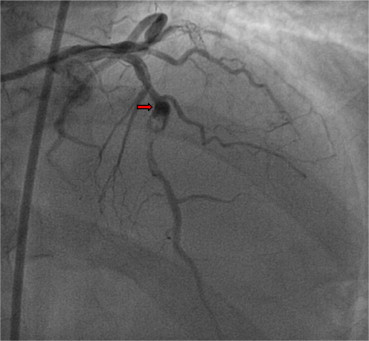
Aneurysm at the proximal end of the stent and angiographically. Visible thrombus.
Fig. 2.
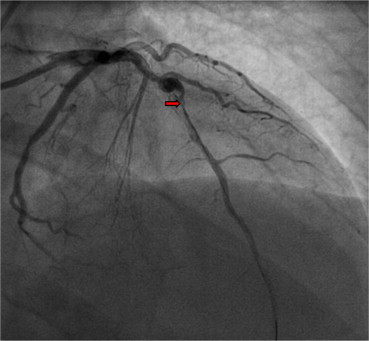
Lesion crossed with a guide wire. Thrombectomy catheter did not cross the stent.
Fig. 3.
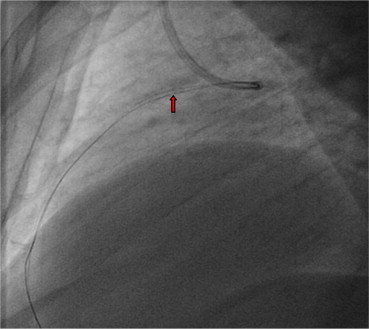
Two guide wires through the stent. The lower wire is through the wall of the aneurysm and mal opposed stent
Fig. 4.
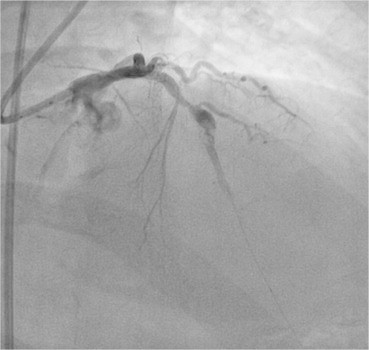
Angiography frame after thrombosuction and intracoronary abciximab.
Fig. 5.
Final picture after deploying MGuard stent with TIMI 3 flow.
3. Discussion
Coronary artery aneurysms are a rare complication of coronary stenting, whose true incidence, clinical course, and treatment are largely unknown. Data on coronary aneurysms are derived mainly from case reports and is uncommon, occurs in less than 5% of coronary angiographic series.3 Coronary aneurysms have been detected from as early as 3 days after DES implantation4 and as late as 9 years after bare metal stent (BMS) implantation.5 As reported in literature sirolimus and paclitaxel DES are more commonly associated with aneurysms formation.6,7
There are a number of postulated causes of DES related coronary artery aneurysms, the antiproliferative drugs along with presence of a polymer can cause delayed re-endothelialization, inflammatory changes in the media of artery and hypersensitivity reactions, all of which can result in coronary artery aneurysm formation.8 Coronary artery aneurysms can be associated with restenosis,9 whereas turbulent and sluggish blood flow in the area of the aneurysm along with metallic stent, can predispose patients to the risk of ST.10,11
In the study by Ong et al12 reported two patients with stent thrombosis presenting as acute STEMI. These patients' angiographic appearances suggested the presence of coronary aneurysm formation with the guide wire passing between the outside of the stent and the vessel wall. These events occurred 25 and 26 months after paclitaxel-eluting stent (PES) implantation. In our case, the guide wire also initially passed between the wall of the aneurysm and the malapposed stent. This was corrected subsequently.
Feres et al10 published two cases of late stent thrombosis (LST) occurring 40 months after SES and 12 months after PES implantation. In both cases there was late-acquired incomplete stent apposition. The incidence of late-acquired stent malapposition has been more commonly noted with DES compared with BMS.13 Virmani et al14 reported a fatal case of LST 18 months after SES implantation associated with a localized hypersensitivity reaction and coronary aneurysm formation. Coronary artery aneurysm can also present as an intense local and systemic inflammatory response usually of infective etiology, early after stent implantation.15
We have previously reported two case reports of coronary artery aneurysms following sirolimus eluting stent implantation and one case of coronary stent fracture resulting in pseudoaneurysm formation.4,16,17 In the first case report two patients developed coronary aneurysms within one month after Sirolimus stent implantation requiring surgical intervention.4 In the second case report large aneurysms were detected at both the proximal and distal ends of the sirolimus stent six months after stent implantation requiring surgery.16
The present cases had two episodes of VLST first at 2 years and then again at 7 years post-DES deployment. Notably, both episodes occurred while the patient was on dual antiplatelet treatment. This may be related to polymer hypersensitivity of the durable polymer in the stent system as the drug disappears within a few months. The second episode of ST may be related to coronary vessel remodeling after DES deployment presenting as an aneurysm formation with stagnation of blood.
To determine the long-term safety continued surveillance after DES implantation is required. Recent improvement in design of DES, absorbable polymer coatings and bio-absorbable DES may prevent this complication from occurring.
Conflicts of interest
All authors have none to declare.
References
- 1.Lima B., Varma S.K., Lowe J.E. Nonsurgical management of left main coronary artery aneurysms: report of 2 cases and review of the literature. Tex Heart Inst J. 2006;33:376–379. [PMC free article] [PubMed] [Google Scholar]
- 2.Robinson F.C. Aneurysms of the coronary arteries. Am Heart J. 1985;109:129–135. doi: 10.1016/0002-8703(85)90425-9. [DOI] [PubMed] [Google Scholar]
- 3.Syed M., Lesch M. Coronary artery aneurysm: a review. Prog Cardiovasc Dis. 1997;40:77–84. doi: 10.1016/s0033-0620(97)80024-2. [DOI] [PubMed] [Google Scholar]
- 4.Gupta R.K., Sapra R., Kaul U. Early aneurysm formation after drug-eluting stent implantation: an unusual life-threatening complication. J Invasive Cardiol. 2006;18:E140–E142. [PubMed] [Google Scholar]
- 5.Porto I., MacDonald S., Banning A.P. Intravascular ultrasound as a significant tool for diagnosis and management of coronary aneurysms. Cardiovasc Intervent Radiol. 2004;27:666–668. doi: 10.1007/s00270-004-0038-0. [DOI] [PubMed] [Google Scholar]
- 6.Lee Y.S., Kim K.S., Chang S.G. Three aneurysms developed in three different drug-eluting stents. Eur Heart J. 2009;30:1309. doi: 10.1093/eurheartj/ehp017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsai J.P., Wang K.T., Yeh H.I., Yin C.J. Aneurysm formation after paclitaxel-eluting coronary stent implantation. Acta Cardiol Sin. 2007;23:50–55. [Google Scholar]
- 8.Aoki J., Kirtane A., Leon M.B., Dangas G. Coronary artery aneurysms after drug-eluting stent implantation. J Am Coll Cardiol Intv. 2008;1:14–21. doi: 10.1016/j.jcin.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Alfonso F., Perez-Vizcayno M.J., Ruiz M. Coronary aneurysms after drug-eluting stent implantation: clinical, angiographic, and intravascular ultrasound findings. J Am Coll Cardiol. 2009;53:2053–2060. doi: 10.1016/j.jacc.2009.01.069. [DOI] [PubMed] [Google Scholar]
- 10.Feres F., Costa J.R., Jr., Abizaid A. Very late thrombosis after drug-eluting stents. Catheter Cardiovasc Interv. 2006;68:83–88. doi: 10.1002/ccd.20692. 248. [DOI] [PubMed] [Google Scholar]
- 11.Aziz S., Morris J.L., Perry R.A. Late stent thrombosis associated with coronary aneurysm formation after sirolimus-eluting stent implantation. J Invasive Cardiol. 2007;19:E96–E98. [PubMed] [Google Scholar]
- 12.Ong A.T., McFadden E.P., Regar E. Late angiographic stent thrombosis (LAST) events with drug-eluting stents. J Am Coll Cardiol. 2005;45:2088–2092. doi: 10.1016/j.jacc.2005.02.086. [DOI] [PubMed] [Google Scholar]
- 13.Jimenez-Quevedo P., Sabate M., Angiolillo D.J. Vascular effects of sirolimus-eluting versus bare-metal stents in diabetic patients: three-dimensional ultrasound results of the Diabetes and Sirolimus-Eluting Stent (DIABETES) trial. J Am Coll Cardiol. 2006;47:2172–2179. doi: 10.1016/j.jacc.2006.01.063. [DOI] [PubMed] [Google Scholar]
- 14.Virmani R., Guagliumi G., Farb A. Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: should we be cautious? Circulation. 2004;109:701–705. doi: 10.1161/01.CIR.0000116202.41966.D4. [DOI] [PubMed] [Google Scholar]
- 15.Saran R.K., Dwivedi S.K., Puri A., Sethi A., Agarwal S.K. Giant coronary artery aneurysm following implantation of Endeavour stent presenting with fever. IHJ. 2012:198–199. doi: 10.1016/S0019-4832(12)60061-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaul U., Gupta R.K., Kachru R. Large coronary artery aneurysms following sirolimus eluting stent implantation. Heart. 2005;91:234. doi: 10.1136/hrt.2004.045047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sandhu P.S., Kaul U. Coronary stent fracture resulting in pseudoaneurysm. IHJ. 2012;64:622–663. doi: 10.1016/j.ihj.2012.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]


