Case Presentation
Dr. Reza Taslimi (Internist):A 34-year-old HIV positive-man was admitted to the hospital due to fever and abdominal pain. Constant and generalized abdominal pain started 3 months prior to admission (PTA) in upper quadrants of abdomen followed by mild odynophagia, early satiety and more than 20 kg weight loss since then. Intermittent fever begun 7 days PTA and cough, sputum and dyspnea started since 5 days PTA. His general condition deteriorated and became drowsy 2-3 days PTA, so was referred to our center by patient’s accompanies. Patient was a known case of intravenous heroin and a recent case of crack user. He smoked cigarette more than 2 packs a day and drinks alcohol occasionally. On admission day he looked toxic and lethargic. BP:95/60 mmHg, PR:128/min, RR:28/min, Temperature:41.5°c and O2 saturation in room air :92%. Physical Exam (P/E) of skin revealed multiple tattoos and some scars. Head and neck P/E were normal. P/E of heart showed tachycardia without murmur. There were fine crackles in lower zone of left lung associated with generalized wheezing. On abdominal examination, there was abdominal distension with shifting dullness, hepatomegaly (8cm below costal margin) and generalized tenderness without guarding or rebound. There was two plus pitting edema in lower extremities. Peripheral lymphadenopathy was not detected. Patient was admitted to intensive care unit. Abdominal Ultrasound showed liver enlargement with two large heterogeneous mass. Common bile duct and portal vein diameters were normal. Gall bladder was normal and moderate ascites was detected. In transthoracic echocardiography (TTE) ejection fraction was normal and there was no vegetation. In upper GI endoscopy esophageal candidiasis was seen. Colonoscopy was unremarkable, urine analysis was normal, and urine culture and blood culture results were negative. Laboratory findings (Table 1) and ascitic fluid analysis (Table 2) are presented. Chest X-ray (Figure 1 ) and abdominal CT scan (Figures 2 and 3) were performed.
Table 1. Laboratory findings .
| WBC | 14700/µl | BUN | 7 mg/dl | LDH | 1800 IU/L |
| PMN | 82% | Cr | 0.6 mg/dl | Serum protein | 5.8 gr/dl |
| Lym | 18% | Na | 140 meq/l | Albumin | 2.4 gr/dl |
| Hb | 12 gr/dl | K | 3.6 meq/l | AST | 35 IU/L |
| Plt | 257000/µl | Ca | 8.2 mg/dl | ALT | 23 IU/L |
| FBS | 87 mg/dl | Ph | 2.4 mg/dl | ALP | 1018 IU/L |
| Direct Bilirubin | 0.3 mg/dl | Total Bilirubin | 0.8 mg/dl | GGT | 80 IU/L |
| PTT | 32 Sec | PT | 12.5 Sec | ESR | 29 mm/hr |
| αFP | 1.5 ng/ml | CEA | 1.2 ng/ml | CA 19-9 | 14 U/ml |
| CA 125 | 13 u/ml | HBs Ag | negative | HBc Ab | Negative |
| HCV Ab | negative | HIV Ab | positive |
Table 2. Ascitic fluid analysis .
| color | yellow | |
| Appearance | Semi turbid | |
| WBC | 170/mlPMN=58% , Lymph=42% | |
| RBC | 300/ml | |
| Alb | 1.5 gr/Serum Alb=2.4 gr/dl (SAAG=0.9) | |
| Prot | 3 gr/dl | |
| LDH | 850 IU/L | |
| Glucose | 67 mg/dl |
Fig1 .

Ill defined consolidation is noted in left lower lobe.
Fig 2 .

Two hypodence masses in both liver lobes.
Fig 3 .

Large hypodence masses in liver causing hepatomegaly & pressure effect on portal veins and stomach
Dr. Minoo Mohraz: May we review the imaging studies results first?
Radiological discussion
Hadi Rokni( Radiologist): In PA Chest X ray heart, mediastinum and bony thorax are normal. No pleural effusion is noted. Ill defined consolidation is noted in left lower lobe without obscuration of left heart border but with subtle obscuration of left hemidiaphragm border.
Contrast enhanced abdominal CT scan in portal phase shows large hypodense masses in both liver lobes causing hepatomegaly and pressure effect on portal veins, hepatic veins and stomach.
Although multiple liver masses have a long list of differential diagnoses, but it is more limited in AIDS patients. Mycobacterium avium intracellular (MAI) infections, fungal infections like actinomycosis Israeli or blastomycosis can produce liver masses and also lung infiltrates but in this case the masses are too large; although the size cannot exclude these differential diagnoses. Lymphoma can produce large liver masses and also lung infiltrates.1 Kaposi sarcoma can produce liver masses but usually smaller masses with peripheral periportal distribution, without or with mild enhancement and usually with skin or mucosal involvements. Leiomyomatosis or peliosis hepatis which can be seen in AIDS patients as a cause of liver masses also have smaller size and would be enhanced. So primary hepatic lymphoma and MAI or fungal infections are the most probable diagnoses, especially lymphoma.2,3
RIZZI et al. presented the ultrasounds and CT scan findings of 26 patients with diagnosis of AIDS and liver lymphoma. 10 patients had primary and 16 had secondary neoplasms and they found that, majority of both primary and secondary liver lymphomas were multiple lesions. Ultrasound findings showed hypoechoic lesions in 25 (96.1%) patients. In the same study, CT scan showed that all lesions were hypodense with enhancing-ring contrast in only six (23%) patients.4 Our case presented with two large lobulated lesions which both have heterogenous echogenecity in the ultrasound. In the same study, CT scan showed that all lesions were hypodense with ring enhancing contrast in only six (23%) patients, the lesions in our case were also hypodense and without significant enhancement.
Peixoto et al. reported 3 cases of primary non hodgkin’s lymphoma of liver. They found out that all hepatic lesions showed target sign on ultrasound. In computed tomography all cases showed a heterogeneous, hypodense mass with a ring enhancement.5
Clinical discussion
Dr. Minoo Mohraz (infectious disease specialist ): There is insufficient data on HIV in east Mediterranean region. Estimated 460000 people living with HIV infection in this region.
The number of new HIV infection in rejoin increased to 75000 in 2009.6
In 2 countries (Djibouti and southern Sudan), HIV prevalence among pregnant women exceeds 1%. HIV prevalence in other countries across the region remains low.7
There is evidence of HIV prevalence over 5% among men having sex with men, and prevalence 2-4% among sex workers in some countries.
There are many causes for ascites. The most common cause is cirrhosis, which accounts for approximately 80 percent of cases. Other causes include malignancy such as peritoneal carcinomatosis, lymphoma with lymphatic obstruction; heart failure; infections such as tuberculosis, pelvic inflammatory disease; end stage renal disease (ESRD); pancreatic disease; pseudomyxoma peritonei; Meige’s syndrome and trauma.8
Classification of ascites by serum-to-ascites albumin gradient (SAAG): Differential diagnosis of high SAAG (≥1.1g/dl) consist of cirrhosis, congestive heart failure, fulminant hepatic failure, fatty liver of pregnancy, liver metastases, portal vein thrombosis, alcoholic hepatitis, Budd-Chiari syndrome, veno-occlusive disease, myxedema and dialysis related ascites.8
Differential diagnosis of low SAAG (<1.1g/dl) consist of nephrotic syndrome, peritoneal carcinomatosis, biliary disease without cirrhosis, connective tissue disease (serosities), tuberculosis and pelvic inflammatory disease (chlamydial or gonococcal).
Causes of hepatic disease in HIV infection:
These include: first: hepatitis including hepatitis B and C.9 Other viral hepatitis is HDV, cytomegalovirus, Epstien-Barr virus, herpes simplex virus, adenovirus, varicella-zoster virus, HIV. Also hepatotoxic drugs and ethanol may damage liver.
Second: granulomatous inflammation including mycobacterial infection (Mycobacterium avium complex, Mycobacterium tuberculosis, Other atypical mycobacteria ), fungal infection (Histoplasma capsulatum, Cryptococcus neoformans, Coccidioides immitis, Candida albicans ), protozoa (Pneumocystis carinii, Toxoplasma gondii, Microsporida, Schistosoma, Cryptosporidium parvum ).10
Third: mass lesions including Kaposi’s sarcoma, non-Hodgkin’s lymphoma (NHL) and other neoplasms.11
Fourth: vascular lesions including peliosis hepatis.12
Liver mass lesions in HIV positive persons:
The first mass lesion which is going to be explained is Kaposi sarcoma (K.S). One third of all patients have cutaneous involvement. Abdominal pain, hepatosplenomegaly and increased alkaline phosphates (ALP) are present.13 Central necrosis is common in these lesions. The second one is NHL B cell type. 14% of patients have liver involvement. There are 15 reports of primary liver NHL.14 Fever, night sweat, weight loss and increased ALP are present. Multiple liver mass larger than K.S may present.15 Other visceral lymph nodes are involved in 90%. The other liver mass lesions which can be seen in these patients are fibrosarcoma, chronic lymphocytic leukemia, leiomyoma, hepatoma, cholangiocarcinoma, metastatic lesion and mixed solid-cystic masses such as MAC, CMV, Fungi, Protozoa, gram-negative microorganisms and staphylococci aureus .
HIV associated lymphoproliferative disorders:
HIV associated lymphoma affects 5-10% of HIV infected individuals. The vast majority of them are systemic B-cell type NHL. 20% involves CNS and consists primary CNS lymphoma. Primary effusion lymphoma accounting for less than 1 to 4 percent of cases.16 HIV associated Burkitt lymphoma is one of the common forms of lymphoma in this disease and 25-40% are EBV associated.
Dr. Mohraz’s diagnosis:
lymphoma.
Pathology discussion
Dr. Sotoudeh (pathologist):
Histological features and immumohistochemical (IHC) studies performed on the liver needle biopsy specimen were diagnostic for Burkitt lymphoma in this patient.
Association of HIV infection and AIDS with lymphoproliferative disorders and some other types of malignancies has been recognized since 1981, as early as HIV associated diseases were defined. Natural history of HIV and AIDS related malignancies has changed since the introduction of more effective anti-viral therapy for the patients.17
Patients with HIV infection are in definite risk of development of lymphoma. 5-10% of these patients are believed to be diagnosed with lymphoid malignancies.The risk increases constantly in the survivors and may reach up to 29% by the third year of antiviral therapy. Multiple pathways are possibly involved in the pathogenesis of lymphoma in HIV patients. Most of the lymphomas detected in these patients are high grade diffuse large B-cell type similar to the tumors seen in organ transplant recipients. However, unlike the tumors in transplanted patients, EBV DNA sequence is much less frequently found. EBV associated large B-cell lymphoma is mostly seen in HIV patients with primary CNS lymphomas.18 Burkitt lymphoma (diffuse small non-cleaved lymphoma) is the second most common lymphoma in HIV patients and is a highly aggressive tumor. 30-50% of these tumors are reported to be associated with EBV infection.19
The patient presented in this clinic pathological conference is a typical case of HIV associated primary hepatic Burkitt lymphoma.
The tumor has been multifocal in liver but extensive imaging and other works up could not detect any lymph adenopathy or other sites of involvement by the tumor.The liver biopsy showed a tumoral tissue composed of small cells with high nucleo-cytoplasmic ratio and small amount of cytoplasm (Figure 4).
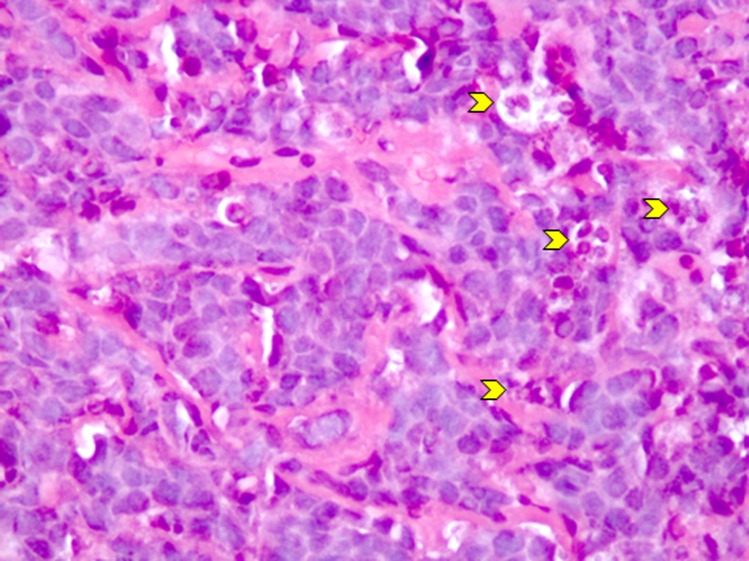
Fig 4 .
Tumor cells are small but have relatively large nuclei and small amount of cytoplasm. Macrophages shown by arrow heads are frequently seen among the tumor cells. The reason for the so-called starry sky in low power microscopy.
The tumor cells showed brisk mitotic activity forming sheets that occupied the liver paren-chyma. Low power examination showed the so- called starry sky appearance. IHC staining of the tumor cells showed reaction for LCA, CD20 and CD10. Almost all (98%) of tumor cell nuclei showed reaction for Ki67. No reaction could be demonstrated in tumor cells by antibodies against cytokeratin, CD3, CD99, CD23, Bcl2 and CD34 (Figure 5). PCR for CMV was inconclusive.
Fig 5 .

IHC studies show strong and diffuse reaction of the tumor cells for LCA and CD20. Moderate positive reaction of tumor cells for CD10 is observed. Reaction of 98% of tumor cell nuclei for Ki67 protein indicates a high proliferation activity in the tumor cells and corresponds to the large number of mitotic figures observed in the histological sections.
Final Pathological Diagnosis
Primary hepatic Burkitt lymphoma in a HIV patient
CONFLFLICT OF INTEREST
The authors declare no conflict of interest related to this work.
Please cite this paper as :
R Taslimi, M Esfandbod, M Mohraz, M Soutodeh, H Rokni. Case 2-2011: A 34 year-old man with fever and abdominal pain. Middle East J Dig Dis 2012;4:55-59.
References
- 1.Villafañe MF, Trione N, Corti M, Mendez N, Gancedo E, Zamora N. et al. Primary liver AIDS-related lympoma. Rev Inst Med Trop Sao Paulo. 2006;48:229–31. doi: 10.1590/s0036-46652006000400011. [DOI] [PubMed] [Google Scholar]
- 2. Diagnostic imaging, abdomen. Text book of radiology. First Edition, PART II,Hepatobillary and Pancreas, liver. Federle MR, Brooke RJ.2004.
- 3.Restrepo CS, Martínez S, Lemos JA, Carrillo JA, Lemos DF, Ojeda P. et al. Imaging manifestations of Kaposi sarcoma. Radiographics. 2006;26:1169–85. doi: 10.1148/rg.264055129. [DOI] [PubMed] [Google Scholar]
- 4.Rizzi EB, Schinina V, Cristofaro M, David V, Bibbolino C. Non-hodgkin’s lymphoma of the liver in patients with AIDS: sonographic, CT, and MRI findings. J Clin Ultrasound. 2001;29:125–9. doi: 10.1002/1097-0096(200103/04)29:3<125::aid-jcu1011>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 5.Góis Peixoto MC, Peixoto Filho AAA, Rodrigues Ribeiro AC, D’Ippolito G. Non-Hodgkin’s lymphoma presenting as a single liver mass. Radiol Bras. 2009;42:1. [Google Scholar]
- 6.Runyon BA, Montano AA, Akriviadis EA, Antillon MR, Irving MA, McHutchison JG. The serum-ascites albumin gradient is superior to the exudate-transudate concept in the differential diagnosis of ascites. Ann Intern Med. 1992;117:215–20. doi: 10.7326/0003-4819-117-3-215. [DOI] [PubMed] [Google Scholar]
- 7.Weber R, Sabin CA, Friis-Møller N, Reiss P, El-Sadr WM, Kirk O. et al. Liver-related deaths in persons infected with the human immunodeficiency virus: the D:A:D study. Arch Intern Med. 2006;166:1632–41. doi: 10.1001/archinte.166.15.1632. [DOI] [PubMed] [Google Scholar]
- 8.Poles MA, Dieterich DT, Schwarz ED, Weinshel EH, Lew EA, Lew R. et al. Liver biopsy findings in 501 patients infected with human immunodeficiency virus (HIV) J Acquir Immune Defic Syndr Hum Retrovirol. 1996;11:170–7. doi: 10.1097/00042560-199602010-00008. [DOI] [PubMed] [Google Scholar]
- 9.Spano JP, Costagliola D, Katlama C, Mounier N, Oksenhendler E, Khayat D. AIDS-related malignancies: state of the art and therapeutic challenges. J Clin Oncol. 2008;26:4834–42. doi: 10.1200/JCO.2008.16.8252. [DOI] [PubMed] [Google Scholar]
- 10.Plettenberg A, Lorenzen T, Burtsche BT, Rasokat H, Kaliebe T, Albrecht H. et al. Bacillary angiomatosis in HIV-infected patients--an epidemiological and clinical study. Dermatology. 2000;201:326–31. doi: 10.1159/000051547. [DOI] [PubMed] [Google Scholar]
- 11.Dezube BJ. Clinical presentation and natural history of AIDS--related Kaposi’s sarcoma. Hematol Oncol Clin North Am. 1996;10:1023–9. doi: 10.1016/s0889-8588(05)70382-8. [DOI] [PubMed] [Google Scholar]
- 12.Nador RG, Cesarman E, Chadburn A, Dawson DB, Ansari MQ, Sald J. et al. Primary effusion lymphoma: a distinct clinicopathologic entity associated with the Kaposi’s sarcoma-associated herpes virus. Blood. 1996;88:645–56. [PubMed] [Google Scholar]
- 13.Simonelli C, Spina M, Cinelli R, Talamini R, Tedeschi R, Gloghini A. et al. Clinical features and outcome of primary effusion lymphoma in HIV-infected patients: a single-institution study. J Clin Oncol. 2003;21:3948–54. doi: 10.1200/JCO.2003.06.013. [DOI] [PubMed] [Google Scholar]
- 14.Cote TR, Biggar RJ, Rosenberg PS, Devesa SS, Percy C, Yellin FJ. et al. Non-Hodgkin’s lymphoma among people with AIDS: incidence, presentation and public health burdenAIDS/Cancer Study Group. Int J Cancer. 1997;73:645–50. doi: 10.1002/(sici)1097-0215(19971127)73:5<645::aid-ijc6>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 15.Lim ST, Karim R, Nathwani BN, Tulpule A, Espina B, Levine AM. AIDS-related Burkitt’s lymphoma versus diffuse large-cell lymphoma in the pre-highly active antiretroviral therapy (HAART) and HAART eras: significant differences in survival with standard chemotherapy. J Clin Oncol. 2005;23:4430–8. doi: 10.1200/JCO.2005.11.973. [DOI] [PubMed] [Google Scholar]
- 16.Naresh KN, Stebbing J, Bower M. Lymphoid and histiocytic proliferations in HIV-positive patients: problems in diagnosis. J HIV Ther. 2009;14:21–3. [PubMed] [Google Scholar]
- 17.Levine AM. Management of AIDS-related lymphoma. Curr Opin Oncol. 2008;20:522–8. doi: 10.1097/CCO.0b013e3283094ec7. [DOI] [PubMed] [Google Scholar]
- 18.http://www.amfar.org/abouthiv/article.aspx?id=3592. http://www.amfar.org/abouthiv/article.aspx?id=3592
- 19.http://www.unaids.org/documents/20101123_FS_mena_em_en.pdf. http://www.unaids.org/documents/20101123_FS_mena_em_en.pdf