Abstract
The objective of this study is to examine the extent of underreporting of total caloric intake and associated factors in a low-income, low-literacy, predominantly Caribbean Latino community in Lawrence, Massachusetts. Two hundred fifteen Latinos participated in a diabetes prevention study, with eligibility included a ≥30% risk of developing diabetes in 7.5 years. Dietary self-reported energy intake (EI) was assessed using three randomly selected days of 24-hour diet recalls. Basal metabolic rate (BMRest) was estimated using the Mifflin-St Jeor equation. Underreporting was determined by computing a ratio of EI to BMRest, with a ratio of 1.55 expected for sedentary populations. Linear regression analyses were used to identify factors associated with underreporting (EI:BMRest ratio). The population was predominately female (77%), middle-aged [mean =52 years; standard deviation (SD)=11], obese (78% had a BMI≥30 kg/m2); low-literate (62% < high school education), unemployed (57% reported no job), married or living with partner (52%), and some had a family history of diabetes (37% had siblings with diabetes). Reported total daily EI was 1540 kcal (SD=599), whereas estimated BMR was 1495.7 kcal/day (SD=245.1). When multiplied by an activity factor (1.20 for sedentariness), expected caloric intake was 1794 (SD=294.0), indicating underreporting by an average of 254 Kcal/day. Mean EI/BMRest was 1.03 (SD=0.37), and was lower for participants with higher BMI, siblings with diabetes, sedentary lifestyle, and the unemployed. EI underreporting is prevalent in this low-income, low- literacy Caribbean Latino population. Future studies are needed to develop dietary assessment measures that minimize underreporting in this population.
Keywords: diet
INTRODUCTION
Understanding of the relationship between diet and health outcomes requires accurate self-reports of dietary intake. Although misreporting occurs in both directions, underestimation of energy intake (EI) is more prevalent (1). It is well known from large scale studies in non-Hispanic populations that underreporting is pervasive, and is associated with body mass index (BMI) and female gender (2). In addition, several studies have shown that underreporting of EI is associated with low income (3, 4), older age (5–7), higher social desirability (1, 3, 8), and lower educational levels (9). However, few studies have examined issues regarding the accuracy of dietary assessment in the Caribbean Latino population.
Assessment of dietary intake in Caribbean Latinos in the United States presents numerous challenges. Culture, language, education, socioeconomic status, consumption of traditional foods, understanding ingredients, perceptions about food portion sizes, societal pressures regarding body image and ideal body weight, and health consequences of lifestyle choices all present challenges to accurate dietary assessment (10, 11). Most work conducted in dietary assessment of Latino populations (12) has been done with Mexican-Americans, whose cultures are distinct from Caribbean Latinos.
Dietary assessment is prone to errors, regardless of the method of measurement (8, 13, 14). The commonly used methods including 24-hour diet recall interviews (24HR), food frequency questionnaires, and diet diaries are all associated with challenges for accurate assessment. These include participant memory, awareness of intake, portion size estimation, and psychological traits that motivate one or more biases. The magnitude of underreporting varies widely between studies and populations, and is dependant not only upon the population studied, but also the methods and administration of dietary assessment. Because of the expense involved, few studies utilize biomarkers of energy intake (i.e., doubly labeled water) (15). An acceptable and more economical estimate of EI is the estimated basal metabolic rate (BMRest) (16, 17). The purpose of the current study is to use the EI to BMRest ratio to determine the extent of EI underreporting and associated factors in a Caribbean Latinos at high risk of developing type 2 diabetes.
SUBJECTS AND METHODS
Subjects
A total of 215 residents of Lawrence, Massachusetts, USA were enrolled in the Lawrence Latino Diabetes Prevention Project (LLDPP) from November 2004 to March 2007 (18). The goal of LLDPP was to implement and evaluate a diabetes prevention program for Caribbean Latinos at high risk of developing type 2 diabetes.
Subjects were eligible for the LLDPP if they: 1) had ≥30% chance of becoming diabetic within 7.5 years as predicted by the Stern formula (a model using age, sex, ethnicity, fasting glucose level, systolic blood pressure, HDL cholesterol level, waist, and immediate family history of diabetes) (19), 2) were ≥ 25 years of age and Latino, and 3) had a BMI ≥ 24 kg/m2.
Baseline diet, physical activity, anthropometric, and demographic data from the LLDPP were used for this investigation. The institutional review boards of University of Massachusetts Medical School and the Greater Lawrence Family Health Center approved the study protocol.
Dietary assessment
Three unannounced 24HR were completed by telephone using the Nutritional Data System for Research (NDS-R versions 2005–2006, Minneapolis, MN) (20). The NDS-R utilizes the multiple-pass technique, allowing for several distinct opportunities to obtain information about the participant’s food intake during the previous 24 hours. The NDS-R database includes culturally unique foods. All participants received a food portion visuals booklet prior to receiving the assessment calls to facilitate portion size estimation. All interviewers were bilingual (Spanish-English) registered dietitians, trained in the use of the software and dietary assessment methodology, and familiar with foods particular to this population. All calls were recorded; including time spent per call, and day of completion. Ten percent of calls were subject to more vigorous quality control measures, comparing data received to telephone recordings. All 215 subjects completed baseline 24HR, and all but two had 3 dietary recalls each (2 weekdays and 1 weekend call). Nutrient values were calculated from NDS-R, EI and percentage of calories from carbohydrate, protein, and fat were included in the analysis.
Basal metabolic rate estimation
The Mifflin St-Jeor Equation was chosen to estimate basal metabolic rate BMRest because it provided the best estimation of age-specific energy intake of overweight and obese individuals (16, 17).
EI/BMRest has been used extensively as a measure of the validity of energy intake in food intake studies (12, 21–25). Using data from whole-body calorimetry and doubly labeled water studies to determine energy expenditure, Goldberg and colleagues (26) suggested a cut-off limit of 1.55 for EI/BMRest to evaluate energy intake data. EI/BMRest ratio below this cut-off is incompatible with long-term survival (26). A lower ratio indicates underreporting and a higher ratio indicates overreporting of EI (27).
Assessment of physical activity, anthropometric, depression symptomatology, and demographic variables
Physical activity was assessed as part of the 24HR. This methodology has been used in several previous projects, and our group has validated it in a White population using both accelerometers and standard questionnaires (28). Data collected are summarized as metabolic equivalent task (MET) hours per day (MET-hr/day), based on the reported time spent at each activity and activity intensity level (29). MET is a physiological concept that expresses the energy cost (calories) of physical activities as multiples of resting metabolic rate. Body weight and height were measured using a scale calibrated every 6 months by the Division of Weights and Measures, City of Lawrence, Massachusetts, and a stadiometer using standard methodology (30). BMI was calculated as weight (kg)/height(m)2.
Depressive symptomatology was assessed using the 20-item Center for Epidemiological Studies-Depression Scale (CES-D) (31). Patient demographic information was collected using a baseline questionnaire, and entered into Epi Info software program (version 6.04d January 2001), using double-entry to prevent entry error.
Statistical analyses
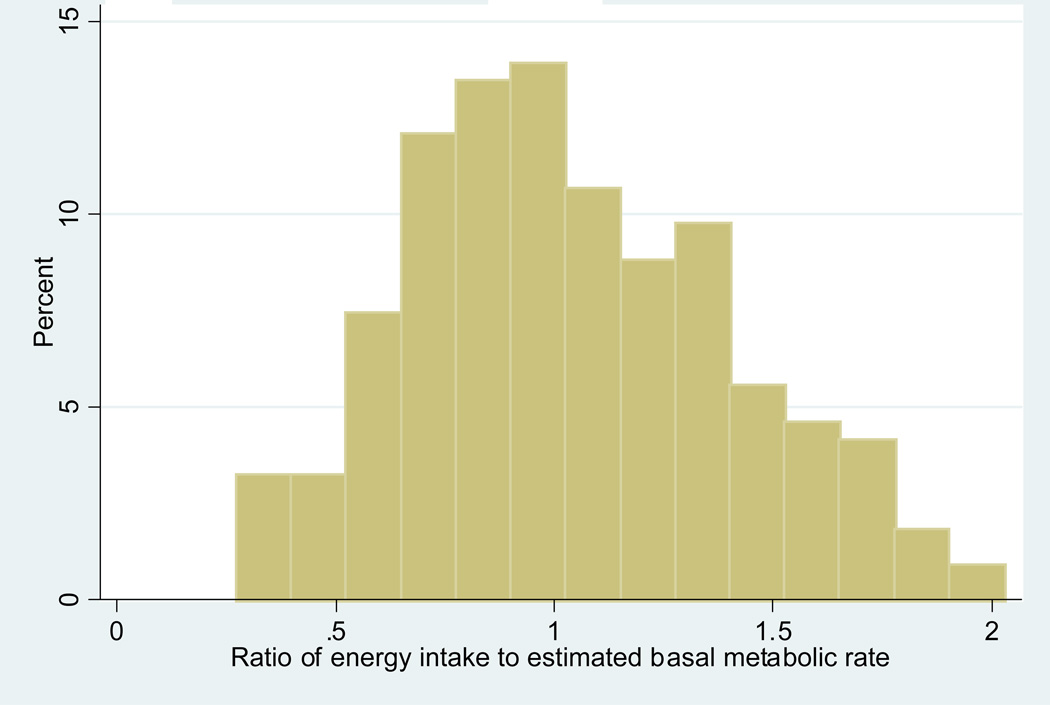
Subjects’ characteristics were summarized using means (standard deviation) and frequencies (percent). To estimate underreporting, EI/BMRest was computed. We examined the distribution of EI/BMRest and found it was approximately normally distributed (see figure 1). To estimate expected caloric intake, we used BMRest multiplied by a physical activity factor of 1.20, because our population was largely sedentary (32).
Figure 1.
Distribution for ratio of energy intake to estimated basal metabolic rate Ratio of energy intake to estimated basal metabolic rate
Linear regression analysis was used to evaluate factors associated with EI/BMRest. The dependent variable was EI/BMRest. Independent variables were evaluated separately and included demographics, BMI, physical activity, and depression score. The final, multivariable model was built in a forward stepwise manner, identifying the most strongly associated variable first (e.g., BMI). Variables were retained in the model based on the strength of support for the mechanism, in addition to statistical criteria such as percent change in coefficient and statistical significance levels.
RESULTS and DISCUSSION
Sample characteristics are reported in Table 1. The population was predominantly female, middle-aged, obese, poorly educated, unemployed, and 37% had siblings with diabetes. Reported total daily EI (1540 kcal/day) was barely higher than BMRest (1496 kcal/day). Mean EI/BMRest was 1.03 (SD=0.37), with a ratio of 1.55 expected for sedentary populations. When BMRest was multiplied by an activity factor (1.20 for sedentariness), expected caloric intake was 1794 kcal (SD=294), indicating underreporting by an average of 254 kcal/day.
Table 1.
Characteristics of study participants and bivariate results of simple linear regression models predicting ratio of energy intake to estimated basal metabolic rate (EI:BMRest) (n=215), Lawrence Latino Diabetes Prevention Project (LLDPP)
| Frequency/Mean | %/SD | Minimum | Maximum | b (SE)a | p value | |
|---|---|---|---|---|---|---|
| Demographic variable | ||||||
| Gender | ||||||
| Male | 50 | 23.3 | - | |||
| Female | 165 | 76.7 | 0.02 (0.06) | 0.74 | ||
| Age (years) | 51.5 | 11.11 | 26.6 | 79.1 | −0.002 (0.002) | 0.29 |
| BMI (kg/m2) | 34.4 | 6.0 | 21.4 | 57.2 | −0.02 (0.004) | <0.001 |
| Height (cm) | 159.8 | 8.8 | 141.0 | 193.0 | ||
| Weight (kg) | 87.4 | 15.9 | 46.3 | 147.4 | ||
| BMI (kg/m2) | ||||||
| Thin to Normal (<25) | 8 | 3.7 | - | |||
| Overweight (25–30) | 40 | 18.6 | −0.12 (0.14) | 0.39 | ||
| Obese (>30) | 167 | 77.7 | −0.23 (0.13) | 0.08 | ||
| Education | ||||||
| Never attended school | 5 | 2.4 | - | |||
| Some elementary school or high school | 122 | 59.2 | −0.18 (0.17) | 0.30 | ||
| High school or GED completed | 46 | 22.3 | −0.10 (0.17) | 0.56 | ||
| Vocational or tech school | 10 | 4.9 | 0.13 (0.20) | 0.53 | ||
| University or College | 23 | 11.2 | −0.06 (0.18) | 0.76 | ||
| Smoking in the past 3 months (yes) | 25 | 12.3 | −0.04 (0.08) | 0.60 | ||
| Marital status | - | |||||
| Single | 39 | 18.9 | −0.11 (0.07) | 0.13 | ||
| Married or Living with Partner | 107 | 51.9 | −0.12 (0.08) | 0.12 | ||
| Separated, Divorced or Widowed | 60 | 29.1 | ||||
| Employment status | ||||||
| Full-time | 64 | 30.8 | - | |||
| Part-time | 26 | 12.5 | 0.64 (10.69) | 0.95 | ||
| Unemployed | 118 | 56.7 | 8.91 (7.20) | 0.22 | ||
| Family history of diabetes or high blood sugar | ||||||
| Father | ||||||
| No | 142 | 72.1 | - | |||
| Yes | 37 | 18. 8 | 2.43 (8.86) | 0.78 | ||
| Don't know / not sure | 18 | 9.1 | 1.07 (11.75) | 0.93 | ||
| Mother | ||||||
| No | 133 | 67.5 | - | |||
| Yes | 56 | 28.4 | 6.44 (7.48) | 0.39 | ||
| Don't know / not sure | 8 | 4.1 | −4.67 (17.07) | 0.79 | ||
| Sibling | ||||||
| No | 121 | 61.4 | - | |||
| Yes | 72 | 36.6 | −4.43 (7.05) | 0.53 | ||
| Don't know / not sure | 4 | 2.0 | −8.33 (23.84) | 0.73 | ||
| Dietary self-reported intakeb | ||||||
| Energy intake (kcal/day) | 1540.22 | 598.95 | 367.51 | 3657.58 | 0.001 (0.005) | 0.83 |
| % calories from CHO | 56.4 | 8.9 | 24.0 | 75.0 | 0.72 (0.35) | 0.04 |
| % calories from protein | 17.7 | 5.44 | 8.48 | 60.24 | 1.59 (0.56) | 0.005 |
| % of calories from fat | 26.5 | 6.28 | 11.76 | 47.1 | −0.09 (0.50) | 0.86 |
| Estimated basal metabolic rate (kcal/day) | 1495.74 | 245.08 | 983.86 | 2238.08 | ||
| Estimated BMR * 1.20 activity factor (Kcal/day) | 1794.88 | 294.09 | 1180.64 | 1206.65 | ||
| Ratio of energy intake to estimated metabolic rate | 1.03 | 0.37 | 0.27 | 2.03 | ||
| Physical activity (metc-hours/day) | ||||||
| Total | 28.31 | 6.30 | 23.16 | 66.76 | −0.10 (0.51) | 0.84 |
| Leisure time | 0.91 | 1.36 | 0 | 10 | −0.61 (2.29) | 0.79 |
| Household | 4.37 | 2.93 | 0 | 17.58 | −0.30 (1.10) | 0.78 |
| Occupational | 4.23 | 8.93 | 0 | 55.33 | −0.07 (0.38) | 0.85 |
| Psychosocial variable | ||||||
| CES-Dd Depression score | 16.60 | 11.30 | 0 | 45 | 0.42 (0.28) | 0.14 |
| <10 | 65 | 30.23 | - | |||
| 10–15 | 38 | 17.67 | −2.46 (9.29) | 0.79 | ||
| >=16 | 112 | 52.09 | 6.73 (7.08) | 0.34 | ||
| Stern index c | 0.54 | 0.18 | 0.30 | 0.96 | −3.87 (17.41) | 0.82 |
b stands for regression coefficient (as an estimate of) and SE stands for its standard error.
dietary intake was from 24 hour recalls and represents 3 days.
met stands for metabolic equivalent task.
CES-D stands for Center for Epidemiologic Studies Depression Scale.
Stern index was calculated based on formula from the publication: Stern MP, Williams K, Haffner SM. Identification of persons at high risk for type 2 diabetes mellitus: do we need the oral glucose tolerance test? Ann Intern Med 2002; 136:575–581.
An average total physical activity expenditure of 28.3 MET-hr/day; predominantly from household and occupational activity, is considered sedentary using our cutoff of <30 MET-hr/day, which is similar to other sedentary classifications (33). Half of subjects (52%) had a CES-D score ≥16, the conventional threshold for clinical depression.
Table 1 also presents bivariate results from linear regression analyses predicting EI/BMRest. Higher BMI and lower percentages of calories from carbohydrate and protein were significantly associated with a lower EI/BMRest ratio. In the final multivariate linear regression model (Table 2), EI/BMRest was lower for Latinos with higher BMI (b=−0.02, p<0.01), having siblings with diabetes (b=−0.09, p=0.07), physical inactivity (b=−0.04, p<0.05), and being unemployed (b=−0.12, p=0.04).
Table 2.
Results of final linear regression models predicting ratio of energy intake to estimated basal metabolic rate (EI:BMRest), Lawrence Latino Diabetes Prevention Project (LLDPP)
| Variable | b (SE)† | p value |
|---|---|---|
| BMI | −0.02 (0 .004) | <0.001 |
| Siblings (Ref: no diabetes) | −0.09 (0.05) | 0.07 |
| Employment status (Ref: Full-time) | ||
| Part-time | −0.21 (0.08) | 0.01 |
| Unemployed | −0.12 (0.06) | 0.04 |
| Leisure time | −0.04 (0.02) | 0.05 |
| physical activity |
b stands for regression coefficient (as an estimate of β) and SE stands for its standard error.
Compared to other studies of dietary underreporting, EI/BMRest was considerably lower in our population. A mean ratio of EI/BMRest of 1.38 was reported from adults aged 18–64 years in Northern Ireland or the Republic of Ireland (34), and 1.44 in African-American women with type 2 diabetes (35). In the Third National Health and Nutrition Examination Survey, EI/BMRest was 1.47 for men and 1.26 for non-pregnant women (7, 12). An EI/BMRest population level of at least 1.55 is expected for a sedentary population (12), and the present sample satisfies the criteria of sedentary with less than 10% of energy expenditure at a moderate intensity of 4 METs or higher. This physical activity level is lower than the predominantly non-Latino Massachusetts healthy population of 30 met-hr/day (36).
Consistent with other studies, EI/BMRest was lower for subjects with higher BMI. BMI tends to be highly correlated with adiposity (and lower energy expenditure) (37). The association of BMI with underreporting of energy intake using 24HR (or other dietary assessment tools) (2, 38, 39) has been ascribed to factors ranging from an inability to accurately perceive portion sizes (40) to social desirability bias (41).
In these data, unemployed participants underreported more than those working full time. Since the study population is fairly homogenous, we were unable to detect an association with education and income. In addition, Latinos having siblings with diabetes and those who were physically inactive were also more likely to underreport their EI, associations which have not been reported previously. Possible explanations include a social desirability bias (i.e., the defensive tendency to report behaviors more in keeping with the perception of social norms). This may be the result of an increased awareness of the connection between diet and diabetes or an awareness of diet in relation to body size. Unfortunately, we did not measure this trait.
Baseline measures were used in the analyses. For low-literacy participants, learning from written materials may be difficult, even when they are supplied with the appropriate visuals, and this can affect portion size estimation (42). This estimation requires an ability to remember portions of particular foods consumed and correlate this with two dimensional images of portion sizes, which is a trained ability. Recipe ingredients and portions are also difficult to report accurately, because many Latinos do not measure their foods, but experientially replicate recipes learned from their older generations. In addition, meals are commonly prepared by other family members, further complicating the ability to describe ingredients. We found that reporting of fat, as a proportion of calories, is nearly 20% lower than expected (i.e., 26.5% vs. the US average of 32.8%) (43).
The Caribbean Latino community has distinct ideas of “good” foods, and “bad” foods, which do not necessarily coincide with ideas held by non-Latino populations (44). For example, instead of corn-based grains popular to Mexican Latinos, Caribbean Latinos favor rice as the staple grain, along with starchy vegetables such as yucca, green plantains, and cassava. The Spanish language also presents difficulty, as different vocabularies are used for the same food depending on the country of origin. However, our registered dietitian telephone callers were quite experienced in these diverse challenges, having worked with Caribbean Latinos for many years. Social trust is an important aspect of day-to-day interactions. Participant trust in the caller increased over time, with the callers reporting greater ease of assessment with subsequent calls. The first call took longer than subsequent calls because it included time spent with introductions, social conventions, and discussion of topics not directly related to dietary assessment.
To our knowledge, this is the first report of accuracy of dietary intake in Caribbean Latinos at elevated risk of type 2 diabetes, however, there are several limitations. First, this is a cross-sectional study; therefore, we can not establish a temporal relationship between underreporting and its associated factors. Second, we did not have a biomarker of EI; however, the validity of using ratio of EI/BMRest to estimate underreporting has been demonstrated in previous studies. Finally, our results may not be generalized to all Latinos as participants in this study were predominantly females and Puerto Rican/Dominican.
CONCLUSIONS
Underreporting is found to be common in the Caribbean Latinos as indicated by a low EI/BMRest, and accurate measurement of diet is influenced by factors such as BMI and lifestyle. Dietary assessment tools are needed for this unique population that encourages accurate reporting of foods, portion sizes, and ingredients. Dietary intake is a key component in diabetes prevention and outcome assessment, and further research into methodology aimed at correcting factors of underreporting for this population is warranted.
REFERENCES
- 1.Maurer J, Taren DL, Teixeira PJ, Thomson CA, Lohman TG, Going SB, Houtkooper LB. The psychosocial and behavioral characteristics related to energy misreporting. Nutr Rev. 2006;64:53–66. doi: 10.1111/j.1753-4887.2006.tb00188.x. [DOI] [PubMed] [Google Scholar]
- 2.Hebert JR, Patterson RE, Gorfine M, Ebbeling CB, St Jeor ST, Chlebowski RT. Differences between estimated caloric requirements and self-reported caloric intake in the women's health initiative. Ann Epidemiol. 2003;13:629–637. doi: 10.1016/S1047-2797(03)00051-6. [DOI] [PubMed] [Google Scholar]
- 3.Tooze JA, Subar AF, Thompson FE, Troiano R, Schatzkin A, Kipnis V. Psychosocial predictors of energy underreporting in a large doubly labeled water study. Am J Clin Nutr. 2004;79:795–804. doi: 10.1093/ajcn/79.5.795. [DOI] [PubMed] [Google Scholar]
- 4.Carter LM, Whiting SJ. Underreporting of energy intake, socioeconomic status, and expression of nutrient intake. Nutr Rev. 1998;56:179–182. doi: 10.1111/j.1753-4887.1998.tb06134.x. [DOI] [PubMed] [Google Scholar]
- 5.Johnson RK, Soultanakis RP, Matthews DE. Literacy and body fatness are associated with underreporting of energy intake in US low-income women using the multiple-pass 24-hour recall: a doubly labeled water study. J Am Diet Assoc. 1998;98:1136–1140. doi: 10.1016/S0002-8223(98)00263-6. [DOI] [PubMed] [Google Scholar]
- 6.Jonnalagadda SS, Mitchell DC, Smiciklas-Wright H, Meaker KB, Van Heel N, Karmally W, Ershow AG, Kris-Etherton PM. Accuracy of energy intake data estimated by a multiple-pass, 24-hour dietary recall technique. J Am Diet Assoc. 2000;100:303–308. doi: 10.1016/s0002-8223(00)00095-x. quiz 309–311. [DOI] [PubMed] [Google Scholar]
- 7.Briefel RR, McDowell MA, Alaimo K, Caughman CR, Bischof AL, Carroll MD, Johnson CL. Total energy intake of the US population: the third National Health and Nutrition Examination Survey, 1988–1991. Am J Clin Nutr. 1995;62:1072S–1080S. doi: 10.1093/ajcn/62.5.1072S. [DOI] [PubMed] [Google Scholar]
- 8.Hebert JR, Ebbeling CB, Matthews CE, Hurley TG, Ma Y, Druker S, Clemow L. Systematic errors in middle-aged women's estimates of energy intake: comparing three self-report measures to total energy expenditure from doubly labeled water. Ann Epidemiol. 2002;12:577–586. doi: 10.1016/s1047-2797(01)00297-6. [DOI] [PubMed] [Google Scholar]
- 9.Bedard D, Shatenstein B, Nadon S. Underreporting of energy intake from a self-administered food-frequency questionnaire completed by adults in Montreal. Public Health Nutr. 2004;7:675–681. doi: 10.1079/PHN2003578. [DOI] [PubMed] [Google Scholar]
- 10.Goris AH, Westerterp KR. Underreporting of habitual food intake is explained by undereating in highly motivated lean women. J Nutr. 1999;129:878–882. doi: 10.1093/jn/129.4.878. [DOI] [PubMed] [Google Scholar]
- 11.Samuel-Hodge CD, Fernandez LM, Henriquez-Roldan CF, Johnston LF, Keyserling TC. A comparison of self-reported energy intake with total energy expenditure estimated by accelerometer and basal metabolic rate in African-American women with type 2 diabetes. Diabetes Care. 2004;27:663–669. doi: 10.2337/diacare.27.3.663. [DOI] [PubMed] [Google Scholar]
- 12.Briefel RR, Sempos CT, McDowell MA, Chien S, Alaimo K. Dietary methods research in the third National Health and Nutrition Examination Survey: underreporting of energy intake. Am J Clin Nutr. 1997;65:1203S–1209S. doi: 10.1093/ajcn/65.4.1203S. [DOI] [PubMed] [Google Scholar]
- 13.Prentice RL, Pettinger M, Anderson GL. Statistical issues arising in the Women's Health Initiative. Biometrics. 2005;61:899–911. doi: 10.1111/j.0006-341X.2005.454_1.x. discussion 911-841. [DOI] [PubMed] [Google Scholar]
- 14.Hoidrup S, Andreasen AH, Osler M, Pedersen AN, Jorgensen LM, Jorgensen T, Schroll M, Heitmann BL. Assessment of habitual energy and macronutrient intake in adults: comparison of a seven day food record with a dietary history interview. Eur J Clin Nutr. 2002;56:105–113. doi: 10.1038/sj.ejcn.1601292. [DOI] [PubMed] [Google Scholar]
- 15.Subar AF, Kipnis V, Troiano RP, Midthune D, Schoeller DA, Bingham S, Sharbaugh CO, Trabulsi J, Runswick S, Ballard-Barbash R, Sunshine J, Schatzkin A. Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: the OPEN study. Am J Epidemiol. 2003;158:1–13. doi: 10.1093/aje/kwg092. [DOI] [PubMed] [Google Scholar]
- 16.Frankenfield D, Roth-Yousey L, Compher C. Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: a systematic review. J Am Diet Assoc. 2005;105:775–789. doi: 10.1016/j.jada.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;51:241–247. doi: 10.1093/ajcn/51.2.241. [DOI] [PubMed] [Google Scholar]
- 18.Merriam PA, Ma Y, Olendzki BC, Tellez T, Rosal MC, Pagoto SL, Ockene IS. Methodology of a Diabetes Prevention Translational Project in a Latino Community. Washington DC: Presented at Society of Behavioral Medicine; 2007. [Google Scholar]
- 19.Stern MP, Williams K, Haffner SM. Identification of persons at high risk for type 2 diabetes mellitus: do we need the oral glucose tolerance test? Ann Intern Med. 2002;136:575–581. doi: 10.7326/0003-4819-136-8-200204160-00006. [DOI] [PubMed] [Google Scholar]
- 20.Schakel SF, Sievert YA, Buzzard IM. Sources of data for developing and maintaining a nutrient database. J Am Diet Assoc. 1988;88:1268–1271. [PubMed] [Google Scholar]
- 21.Black AE, Goldberg GR, Jebb SA, Livingstone MB, Cole TJ, Prentice AM. Critical evaluation of energy intake data using fundamental principles of energy physiology: 2. Evaluating the results of published surveys. Eur J Clin Nutr. 1991;45:583–599. [PubMed] [Google Scholar]
- 22.Klesges RC, Eck LH, Ray JW. Who underreports dietary intake in a dietary recall? Evidence from the Second National Health and Nutrition Examination Survey. J Consult Clin Psychol. 1995;63:438–444. doi: 10.1037//0022-006x.63.3.438. [DOI] [PubMed] [Google Scholar]
- 23.Gnardellis C, Boulou C, Trichopoulou A. Magnitude, determinants and impact of under-reporting of energy intake in a cohort study in Greece. Public Health Nutr. 1998;1:131–137. doi: 10.1079/phn19980020. [DOI] [PubMed] [Google Scholar]
- 24.Stallone DD, Brunner EJ, Bingham SA, Marmot MG. Dietary assessment in Whitehall II: the influence of reporting bias on apparent socioeconomic variation in nutrient intakes. Eur J Clin Nutr. 1997;51:815–825. doi: 10.1038/sj.ejcn.1600491. [DOI] [PubMed] [Google Scholar]
- 25.Schoeller DA. How accurate is self-reported dietary energy intake? Nutr Rev. 1990;48:373–379. doi: 10.1111/j.1753-4887.1990.tb02882.x. [DOI] [PubMed] [Google Scholar]
- 26.Goldberg GR, Black AE, Jebb SA, Cole TJ, Murgatroyd PR, Coward WA, Prentice AM. Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr. 1991;45:569–581. [PubMed] [Google Scholar]
- 27.Black AE. Critical evaluation of energy intake using the Goldberg cut-off for energy intake:basal metabolic rate. A practical guide to its calculation, use and limitations. Int J Obes Relat Metab Disord. 2000;24:1119–1130. doi: 10.1038/sj.ijo.0801376. [DOI] [PubMed] [Google Scholar]
- 28.Matthews CE, Freedson PS, Hebert JR, Stanek EJ, 3rd, Merriam PA, Ockene IS. Comparing physical activity assessment methods in the Seasonal Variation of Blood Cholesterol Study. Med Sci Sports Exerc. 2000;32:976–984. doi: 10.1097/00005768-200005000-00015. [DOI] [PubMed] [Google Scholar]
- 29.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O'Brien WL, Bassett DR, Jr, Schmitz KH, Emplaincourt PO, Jacobs DR, Jr, Leon AS. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 30.Cogil B. Anthropometric Indicators Measurement Guide. Washington: Academy of Educational Development; 2003. [Google Scholar]
- 31.Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 32.Black AE, Coward WA, Cole TJ, Prentice AM. Human energy expenditure in affluent societies: an analysis of 574 doubly-labelled water measurements. Eur J Clin Nutr. 1996;50:72–92. [PubMed] [Google Scholar]
- 33.Talbot LA, Fleg JL, Metter EJ. Secular trends in leisure-time physical activity in men and women across four decades. Prev Med. 2003;37:52–60. doi: 10.1016/s0091-7435(03)00058-6. [DOI] [PubMed] [Google Scholar]
- 34.McGowan MJ, Harrington KE, Kiely M, Robson PJ, Livingstone MB, Gibney MJ. An evaluation of energy intakes and the ratio of energy intake to estimated basal metabolic rate (EI/BMRest) in the North/South Ireland Food Consumption Survey. Public Health Nutr. 2001;4:1043–1050. doi: 10.1079/phn2001185. [DOI] [PubMed] [Google Scholar]
- 35.Amend A, Melkus GD, Chyun DA, Galasso P, Wylie-Rosett J. Validation of dietary intake data in black women with type 2 diabetes. J Am Diet Assoc. 2007;107:112–117. doi: 10.1016/j.jada.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 36.Ma Y, Olendzki BC, Li W, Hafner AR, Chiriboga D, Hebert JR, Campbell M, Sarnie M, Ockene IS. Seasonal variation in food intake, physical activity, and body weight in a predominantly overweight population. Eur J Clin Nutr. 2006;60:519–528. doi: 10.1038/sj.ejcn.1602346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Matthews CE, Fowke JH, Dai Q, Leon Bradlow H, Jin F, Shu XO, Gao YT, Longcope C, Hebert JR, Zheng W. Physical activity, body size, and estrogen metabolism in women. Cancer Causes Control. 2004;15:473–481. doi: 10.1023/B:CACO.0000036445.04238.87. [DOI] [PubMed] [Google Scholar]
- 38.Johansson G, Wikman A, Ahren AM, Hallmans G, Johansson I. Underreporting of energy intake in repeated 24-hour recalls related to gender, age, weight status, day of interview, educational level, reported food intake, smoking habits and area of living. Public Health Nutr. 2001;4:919–927. doi: 10.1079/phn2001124. [DOI] [PubMed] [Google Scholar]
- 39.Bailey RL, Mitchell DC, Miller C, Smiciklas-Wright H. Assessing the effect of underreporting energy intake on dietary patterns and weight status. J Am Diet Assoc. 2007;107:64–71. doi: 10.1016/j.jada.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 40.Wansink B, Chandon P. Meal size, not body size, explains errors in estimating the calorie content of meals. Ann Intern Med. 2006;145:326–332. doi: 10.7326/0003-4819-145-5-200609050-00005. [DOI] [PubMed] [Google Scholar]
- 41.Hebert JR, Ma Y, Clemow L, Ockene IS, Saperia G, Stanek EJ, 3rd, Merriam PA, Ockene JK. Gender differences in social desirability and social approval bias in dietary self-report. Am J Epidemiol. 1997;146:1046–1055. doi: 10.1093/oxfordjournals.aje.a009233. [DOI] [PubMed] [Google Scholar]
- 42.Rosal MC, Olendzki B, Reed GW, Gumieniak O, Scavron J, Ockene I. Diabetes self-management among low-income Spanish-speaking patients: a pilot study. Ann Behav Med. 2005;29:225–235. doi: 10.1207/s15324796abm2903_9. [DOI] [PubMed] [Google Scholar]
- 43.CDC. Trends in Intake of Energy and Macronutrients --- United States, 1971--2000. 2004 http://wwwcdcgov/mmwr/preview/mmwrhtml/mm5304a3htm. [Google Scholar]
- 44.Oakes ME, Slotterback CS. The good, the bad, and the ugly: characteristics used by young, middle-aged, and older men and women, dieters and non-dieters to judge healthfulness of foods. Appetite. 2002;38:91–97. doi: 10.1006/appe.2001.0444. [DOI] [PubMed] [Google Scholar]