Abstract
Objectives
The aim of the study was to determine the evolution of thyroid tests throughout pregnancy and postpartum in healthy women with and without iodine supplementation.
Methods
This was a prospective, randomized, interventional study of iodine supplementation (150 μg/day) from the first trimester until 3 months postpartum versus controls. 111 pregnant women with normal initial thyroid tests were enrolled, undergoing comprehensive thyroid assessment at each trimester. We present results of longitudinal and cross-sectional analyses.
Results
Initial ioduria suggested mild iodine deficiency in both groups, while third-trimester ioduria rose to levels of iodine sufficiency in the iodine-supplemented group. In the longitudinal study, free T4 (FT4) levels decreased in the second and third trimesters compared to the first trimester in both groups, with no change in TSH, and rose postpartum, though lower than the first trimester. FT3 levels and the total T4 (TT4)/thyroxine-binding globulin (TBG) ratio followed the same evolution as FT4. TT4 levels rose due to TBG increase. Thyroglobulin (Tg) of iodine group remained stable, contrasting with the rise in the control group. In the cross-sectional study, there was no difference between the two groups in thyroid tests at any time-point, except for lower Tg in the second trimester and postpartum visits in the iodine group.
Conclusions
In healthy, mildly iodine-deficient pregnant women, a ‘drop’ of FT4 and TT4/TBG without TSH increase occurs between the first and second trimesters, and is not prevented by iodine supplementation, suggesting physiology. Therefore, FT4 is valuable to assess thyroid function in pregnancy in clinical practice with appropriate trimester-specific reference range. It brings up reflection on threshold for diagnosis and treatment of hypothyroxinemia.
Key Words: Iodine, Pregnancy, Free T4, Thyroglobulin, Ioduria
Introduction
The thyroid hormone economy changes profoundly during pregnancy to accommodate maternal and fetal needs [1]. The main factors involved are the βHCG secretion by the placenta (with its stimulatory effect on maternal thyroid), the increased estradiol production (causing a rise in thyroxine-binding globulin – TBG), and the changes in iodine renal clearance and needs. Those changes result in a gradual increase in thyroid hormone production contrasting with a reported drop in free T4 (FT4) levels after the first trimester [1], which is considered by some as pathological, despite normal TSH concentration, and led to the concept of maternal hypothyroxinemia [2]. The definition of maternal hypothyroxinemia is usually set below the 5th or 10th percentile of the reference range for FT4 associated with normal TSH [3,4]. There is, however, the question of threshold for normal values, linked in part to the lack of laboratory reference ranges in pregnancy. The association of isolated maternal hypothyroxinemia with impaired neurocognitive development in the offspring is debated [2,5,6,7]. Iodine has a central role in the thyroid economy, particularly in pregnancy. Therefore, there are efforts worldwide to eradicate iodine deficiency (ID), with special attention to women of childbearing age [3,8,9]. One important issue is to determine to what extent the drop in maternal FT4 is caused by insufficient iodine intake. Based on maternal thyroglobulin (Tg) levels and newborn thyroid volume [10], the benefit of iodine supplementation is clear for women with severe ID [11] and in women selected for thyroid hyperstimulation in early pregnancy, as well as for their offspring. However, there is no definitive evidence of a benefit in terms of maternal thyroid function in healthy pregnant women with normal thyroid function at the beginning of pregnancy [9,12]. We designed a randomized, prospective, interventional study to assess the evolution of thyroid function with and without iodine supplementation in healthy women with normal initial thyroid tests.
Patients and Methods
Design of the Study
Women presenting at their first obstetrical visit between July 2007 and July 2008 were eligible for this study if they met the following criteria: no personal history of thyroid disease, seen before 12 weeks of amenorrhea (WA), with a singleton pregnancy, with normal thyroid tests on a systematic screening: FT4 >12 pmol/l (10th percentile for first trimester in our population), TSH <2.5 mIU/l, and anti-thyroid peroxidase (TPO) antibodies below the threshold of positivity set at 100 UI/ml. A urine sample was collected at the pre-inclusion visit for further urinary iodine excretion (UIE) measurement if the woman was included, thus reflecting baseline first-trimester UIE before any iodine supplementation. Exclusion criteria included iodine supplementation before inclusion and UIE ≥400 μg/l. After signing a consent form, 111 women were randomized into two groups, one group receiving iodine-enriched pregnancy vitamins (Oligobs Maxiode®, 150 μg of iodine, Laboratoire C.C.D, Paris, France), the other one receiving the same vitamin mix but without iodine (Oligobs Grossesse®, Laboratoire C.C.D). All women received a document established by a dietician on how to optimize their dietary iodine intake. The table of randomization (list of the correspondence between the number of a patient and the arm of the study – iodine or not -) was obtained by a method of drawing of lots by blocks, using tables of permutation. This was an open study. Treatment was given from the day of enrolment until delivery and beyond until the 3-month postpartum visit. Compliance with pregnancy vitamin administration was assessed by the hospital pharmacist based on the number of pills brought back at each visit (patient was asked to bring back all blisters, empty or not). One woman from the iodine-supplemented group was excluded shortly after inclusion because ioduria (UIE) was above 400 μg/l. Comprehensive thyroid tests (FT4, total T4 – TT4, TBG, TSH, FT3, reverse T3 – rT3, Tg, anti-Tg antibodies, anti-TPO antibodies, UIE) were performed at each trimester (second trimester 22 WA, third trimester 33 WA), and at the 3-month postpartum visit. The TT4/TBG ratio was calculated according to the following formula: ratio TT4 (nmol/l): 1.287/TBG in mg/l [13].
Thyroid ultrasound was performed at inclusion, third trimester and 3 months postpartum by 2 of us (F.B.D. and S.H.) using an En Visor scanner (Philips Medical System) equipped with a commercially available 5- to 12-MHz linear transducer (50-mm length). Thyroid volume was calculated in ml for each lobe according to the formula 0.52 × height × width × thickness in centimeters. Total thyroid volume was the sum of each lobe's volume, the isthmus was not taken into account in volume calculation.
Assays
Spot UIE was measured by mass spectrometry ICP/MS (Pasteur-Cerba Laboratory, Cergy Pontoise, France; detection threshold 15 μg/l; intra- and inter-series coefficient of variation, CV <10%). FT4, FT3, TT4, TSH, and anti-TPO and anti-Tg antibodies were measured by chemiluminescence (Centaur XP, Siemens Healthcare Diagnostics, France). Tg was measured by immunoradiometric assay (Thyroglobulin IRMA, Cisbio Bioassays, Bagnols-sur-Cèze, France). TBG was measured by RIA: RIA-gnost TBG (Cisbio Bioassays), as was rT3: RIA rT3 (Pasteur Cerba Laboratory). Reference ranges for FT4 and TSH were established in our laboratory in TPO-negative pregnant women during the first trimester (2.5 and 97.5 percentiles): FT4 11.47-19.23 pmol/l and TSH 0.053-3.23 mIU/l. The other reference ranges were provided by the manufacturer: FΤ3 outside pregnancy 3-7 pmol/l; TT4 during pregnancy 82.6-138 nmol/l; anti-Tg antibodies <60 UI/ml; Tg 5-50 μg/l; reference range for TBG for the first trimester 20.5 ± 4.8 mg/l. CVs were for FT4 (intra-assay CV 2.31%; inter-assay CV 1.95%), FT3 (intra-assay CV 2.35%), TT4 (intra-assay CV 1.77%; inter-assay CV 2.9%), TSH (intra-assay CV 2.67%; inter-assay CV 3.97%), anti-TPO (intra-assay CV 4.1%, inter-assay CV 8.0%), anti-Tg (intra-assay CV 5.5%; inter-assay CV 1.8%), Tg (intra-assay CV 2.4%; inter-assay CV 4.5%), rT3 (intra assay CV 8.54%; interassay CV 6.21%) and TBG (inter-assay CV 4.4%).
Statistics
Data were entered and stored on an Access file, and then transferred to R2.14.1 software for statistical analysis. Quantitative variables were expressed as medians and range, qualitative variables were described by counts and percentages. χ2 test or Fisher's exact test was used for category comparison; Mann-Whitney test was used to compare continuous variables.
For each group, we studied the evolution of thyroid tests at each trimester. Distribution normality was tested with a Shapiro test and homoscedasticity with a Bartlett test. As the distribution of our variables was not normal, we used for multiple comparisons the nonparametric Kruskal-Wallis test, followed by Nemenyi test. The analysis was performed in the 86 patients (nonpaired longitudinal analysis for the three trimesters of pregnancy). In addition, paired analysis by the Friedman test was performed in 72 women (42 controls and 30 iodine) from the first to the third trimester, and in a subgroup of 36 women (18 in the iodine- and 18 in the control group) at each visit, and postpartum (longitudinal, paired analysis).
Lastly, we compared the thyroid tests between the iodine-supplemented group and the non-iodine-supplemented group at each trimester and the postpartum visit using the Mann-Whitney test.
Tests of significance were two tailed and considered significant with an alpha level of 0.05.
Results
Baseline Characteristics
Among the 111 women included, 86 were followed until delivery. Twenty-four women did not complete the study (20 in the iodine group and 4 in the control group): in the iodine group, there were 4 miscarriages, one induced abortion (for trisomy 18), 10 cases of digestive intolerance (nausea/vomiting), 3 cases of consent withdrawal and 2 missed data collection; in the control group, there were 3 miscarriages and one digestive intolerance. Initial clinical characteristics of the 86 women (32 in the iodine group and 54 controls) are shown in table 1 and did not differ between the two groups. No patient had thyroid hyperplasia or goiter. Hormonal characteristics at inclusion (table 1) were not different between the two groups. Two women in the iodine group and 5 in the control group had slightly increased anti-Tg antibody concentrations. Median UIE was similar in both groups, below 150 µg/l, in the range of mild ID. 73% of controls had UIE below 150 μg/l versus 65% of women who were randomized in the iodine-supplemented group. 84% of women who knew what type of salt they were taking reported consumption of iodinated salt, with no significant difference between the two groups.
Table 1.
Baseline characteristics of the 86 women followed until delivery
| Iodine-supplemented group | Control group | |
| Subjects | 32 | 54 |
| Age, years | 28 (21–37) | 27 (18–39) |
| BMI, kg/m2 | 21.9 (17.9–30.8) | 22.3 (16.0–39.5) |
| Term at first visit (WA) | 10.0 (7–12) | 10.0 (7.0–12) |
| Parity | 0 (0–2) | 0 (0–4) |
| Smokers at the visit, % | 25.8 | 27.8 |
| Thyroid volume, ml | 10.1 (5.3–16.7) | 9.5 (5.4–18) |
| Initial UIE, µg/l | 111 (28–399) | 103 (14–355) |
| Initial FT4, pmol/l | 14.1 (12–17.2) | 14.8 (12–18.5) |
| Initial TSH, mIU/l | 1.2 (0.1–2.4) | 1.2 (0.2–2.4) |
| FT3, pmol/l | 5.1 (3.8–6.7) | 5.0 (4.1–6.2) |
| Tg, µg/l | 17 (2.4–45.1) | 17.5 (1.3–84.1) |
| TT4, nmol/l | 116.7 (73.3–162) | 111.2 (71.5–157.3) |
| TBG, mg/l | 27.4 (19.5–50) | 26.3 (12.8–48.9) |
Data are presented as median and range. No differences were observed between the 2 groups.
Follow-Up
Women were seen at similar gestational age in both groups: median second trimester 21.6 versus 21.8 WA and median third trimester 33.4 versus 33.2 WA in the iodine group versus controls, respectively.
Evolution of UIE was markedly different in the two groups: in the iodine group, UIE increased progressively during pregnancy, reaching 160 µg/l in the third trimester, while UIE decreased progressively in the control group (76 µg/l), with a significant difference between the two groups in the second and third trimesters (table 2) and postpartum for those studied at 3 months after delivery. 75% of controls versus 43% of women from the iodinated group had UIE below 150 μg/l in the third trimester.
Table 2.
Evolution of thyroid tests throughout the three trimesters of pregnancy and postpartum in women with and without iodine supplementation
| 1st trimester (n = 86) | 2nd trimester (n = 80) | 3rd trimester (n = 76) | Postpartum (n = 36) | |
|---|---|---|---|---|
| FT4, pmol/l | ||||
| Iodine | 14.1 (12–17.2) | 12.0 (9.8–13.8)b | 11.6 (9.2–15.7)b | 13.5 (12.0–18.7) |
| Control | 14.8 (12–18.5) | 11.6 (9.1–17.4)b | 11.7 (8.4–15)b | 13.9 (10.1–16.9)b |
| TT4, nmol/l | ||||
| Iodine | 116.7 (73.3–162) | 137.8 (101.7–176.1)b | 132.6 (103.1–228.6)b | 90.8 (67.5–117.6) |
| Control | 111.2 (71.5–50) | 140.4 (93.6–217)a | 140.6 (95.4–204.2)a | 91.9 (−110.3) |
| TBG, mg/l | ||||
| Iodine | 27.41 (19.54–157.3) | 46.8 (28.3–62.2)b | 52.3 (31.9–65.5)b | 19.9 (16.2–28.2) |
| Control | 26.28 (12.8–48.91) | 48.1 (23.7–68.2)b | 48.9 (28.8–67.3)b | 22.2 (16.0–28.8) |
| TSH, mIU/l | ||||
| Iodine | 1.17 (0.1–2.4) | 1.14 (0.3–3.1) | 1.1 (0.2–3.6) | 1.1 (0.5–2.6) |
| Control | 1.18 (0.2–2.4) | 1.12 (0.5–2.7) | 1.37 (0.4–2.6) | 1.0 (0.5–2.2) |
| FT3, pmol/l | ||||
| Iodine | 5.12 (3.85–6.74) | 4.4 (3.4–5)b | 4.2 (3.4–4.8)b | 4.9 (3.4–5.6) |
| Control | 4.99 (4.1–6.2) | 4.3 (3.4–5.2)b | 4.1 (3.6–5.1)b | 4.7 (3.9–5.6)b |
| Tg, µg/l | ||||
| Iodine | 17.0 (2.4–45.1) | 13.5 (0.4–38.4) | 17.5 (2.5–56.2) | 11.5 (4.4–37)c |
| Control | 17.5 (1.3–84.1) | 19.1 (1.8–59.1) | 19.6 (3.8–98.6) | 23.1 (3.0–45.5) |
| UIE, µg/l | ||||
| Iodine | 111 (28–399) | 118.5 (38–470)c | 160.5 (18–358)d | 131 (45–406)c |
| Control | 103 (14–365) | 95.5 (17–228) | 76 (16–303) | 68 (19–278) |
| Thyroid volume, ml | ||||
| Iodine | 10.0 (5.3–16.7) | ND | 9.73 (5.4–15.5) | 8.5 (3.8–13.8) |
| Control | 9.4 (5.4–18.0) | ND | 10.13 (4.2–25.5) | 9.7 (6.6–18.9) |
Results are expressed as median and range. ND = Not done.
p value from Niemenyi test comparing thyroid tests in the 2nd and 3rd trimesters and postpartum with the 1st trimester of their respective group (iodine and controls): ap < 0.01, bp < 0.0001. p value from the Mann-Whitney test comparing thyroid tests at each visit between the iodine and control groups: cp < 0.05, dp < 0.001.
In this unpaired analysis, 86 women (32 in the iodine and 54 in the control group) were studied in the 1st trimester, 80 in the 2nd trimester (31 in the iodine, 49 in the control group), 76 in the 3rd trimester (30 in the iodine, 46 in the control group), and 36 postpartum (18 in iodine, 18 in controls). The 1st trimester results refer to the time before the start of supplementation; all others refer to the time during supplementation.
Evolution of Thyroxine Levels
Unpaired Analysis in the 86 Women (table 2)
FT4 levels dropped similarly in both groups between the first and second trimester visit (by 15% in the iodine group and 21.6% in controls), remaining steady at the third-trimester visit. In the postpartum period, FT4 reached levels intermediary between the first trimester and the other trimesters of pregnancy.
TT4 levels displayed a mirror image in their evolution compared to FT4 with a rise between the first and second trimester visit (by 15 and 20.8%, respectively), which remained steady at the third trimester visit. There was a parallel evolution for TBG, though the rise was more marked in proportion (41% in the iodine and 38% in the control group). The T4/TBG ratio followed the same evolution as FT4, with lower values at the second and third trimester visits.
Paired Analysis
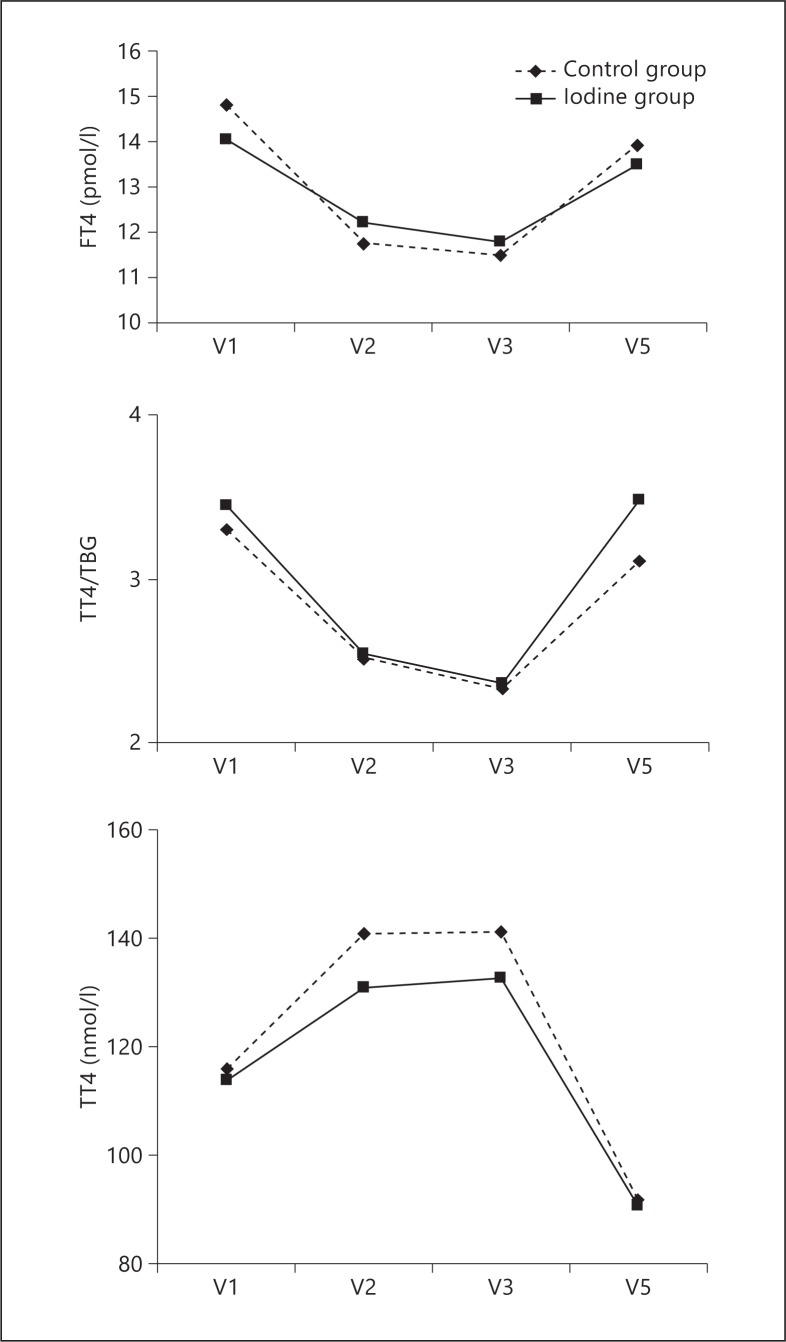
The paired analysis in 72 women at each trimester showed a similar pattern of evolution than the unpaired analysis for FT4, TT4, TBG and T4/TBG in both groups. The paired analysis of the subgroup of 36 women followed until postpartum was also similar during pregnancy. In the postpartum period, we observed a significant rise in FT4, and TT4/TBG (fig. 1), and a drop in TT4 and TBG in both groups. In addition, the area under the curve was similar for FT4 in both groups (37.7 in the iodine group and 37.5 in the control group, NS).
Fig. 1.
Evolution of median FT4, TT4, TT4/TBG in 36 women followed at each trimester during pregnancy and 3 months postpartum (n = 18 in both groups): paired analysis. V1 = 1st trimester visit; V2 = 2nd trimester visit; V3 = 3rd trimester visit; V5 = postpartum visit. FT4 and T4/TBG have similar evolution in the iodine and control groups: V2 vs. V1, p < 0.001; V3 vs. V1, p < 0.01; V5 vs. V2, p < 0.05; V5 vs. V3, p < 0.05. TT4 has similar evolution in the iodine and control groups: V5 vs. V2, p < 0.001; V5 vs. V3, p < 0.001; V5 vs. V1 reaches significance only in the iodine group (p < 0.05). No difference was found between the two groups at each time interval.
Comparison between Groups
In a cross-sectional analysis, there was no difference at any time point between the iodine and control groups for FT4, TT4, TBG and TT4/TBG. In addition, in a paired analysis, the difference between FT4 at the first and second trimesters was similar when comparing the iodine (2.22 pmol/l) and the control group (2.97 pmol/l, p = 0.25).
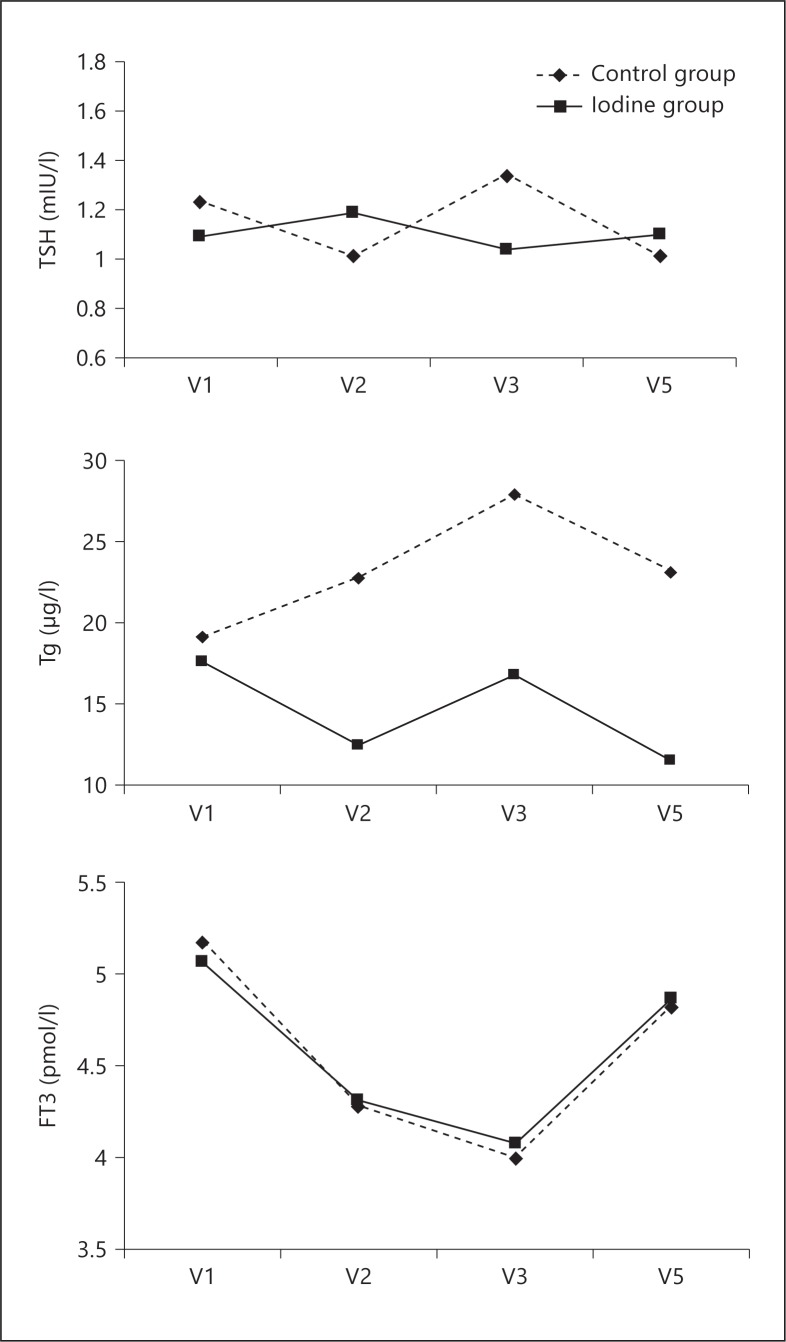
Evolution of Other Thyroid Tests (table 2; fig. 2)
Fig. 2.
Evolution of median FT3, TSH, and Tg in 36 women followed at each trimester of pregnancy and 3 months postpartum (n = 18 in both groups): paired analysis. FT3 has similar evolution in the iodine and control groups: V2 vs. V1, p < 0.01; V3 vs. V1, p < 0.01; V5 vs. V2, p < 0.05; V5 vs. V3, p < 0.01. There is no difference in TSH over time and between the two groups. The rise in Tg is not significant in the control group, while Tg is lower in the 2nd trimester (p < 0.05) and postpartum (p < 0.01) in the iodine group. Tg was lower in the iodine group compared to the control group in the 2nd trimester (p < 0.05) and postpartum (p < 0.02).
FT3 followed the same evolution as FT4 in both groups, i.e. a lower value at the second and third trimester visits compared to the first trimester, with intermediate values postpartum, and no difference between the iodine and control groups at any given time point, in the unpaired and paired analyses. We observed no change in TSH or in thyroid volume at the different visits, again with no difference between the two groups, using paired and unpaired analyses. Regarding serum Tg concentration, there was no significant difference in the unpaired analysis between the different time points and between the two groups. However, the paired analysis showed, in the iodine group only, a lower Tg in the second trimester (p < 0.001) and also postpartum (p < 0.001) compared to the first trimester. There was no significant difference in the control group. When comparing the iodine with the control group, Tg was significantly higher at the second trimester (p = 0.05 for the group of 72, and p = 0.025 for the group of 36 women) and the postpartum visit (p < 0.02, group of 36). Lastly, we did not observe postpartum thyroiditis in the 36 women studied at 3 months after delivery, with negative thyroid antibodies (according to antibody concentrations).
Discussion
We report here a prospective, interventional, randomized study of early iodine supplementation in healthy pregnant women from an area of mild ID. Our population was selected on the basis of normal first-trimester thyroid tests, including negative anti-TPO antibodies (<100 UI/ml). Eligibility criteria included the threshold FT4 >12 pmol/l, corresponding to the 10th percentile of TPO-negative pregnant women (reference range at this stage of pregnancy established in our laboratory), this threshold ruling out initial hypothyroxinemia, and TSH <2.5 mIU/l, threshold recommended by the ATA and the Endocrine Society at this stage of pregnancy [3,4]. Thus, we feel confident that we have selected women with normal thyroid function, allowing us to study the potential impact of iodine supplementation on the physiological evolution of thyroid function in mildly iodine-deficient area throughout pregnancy. We have chosen a supplementation with 150 μg/day, being the current recommendation of the ATA and the Endocrine Society [3,4]. This dose is supposed to provide, along with the iodine from the diet, the 250 μg/day that is considered as optimal in pregnancy [8]. Other interventional studies included supplementation with lower doses (100 μg/day [10]), similar doses (150 μg/day [14], 120/180 μg/day [15], 50/200 μg/day [16]), or higher doses (200 μg/day [17], 230 μg/day [18], 300 μg/day [19], 200/300 μg/day [20]). Of note, we started the iodine supplementation as early as possible (median 10th WA) for a randomized interventional study in a clinical setting. This explains that some women did not complete the study because of miscarriages. Others had severe nauseas and/or vomiting preventing absorption of pills: this was particularly true with the iodinated pills, which turned out to be less palatable and unfortunately caused more gastrointestinal intolerance than their noniodinated counterparts, leading to exclusion from the study, usually within the first week (10 in the iodine group vs. one control). This explained the imbalance in dropout between the two groups. The smaller size of the treated group is the main limitation of our study. We confirmed the status of mild ID at first trimester inclusion in both groups based on UIE below 150 μg/l. The increase in UIE throughout pregnancy in the group actually receiving iodine contrasts with the decrease in the control group, similar to the decrease previously reported by Stilwell et al. [21] confirms the good compliance established by pharmacist records, and thus documents the improvement of iodine status in the iodine-supplemented group reaching levels of iodine sufficiency (>150 μg/l) at the third trimester; however, this was not true in all supplemented patients, as recently reported by Santiago et al. [20] in a randomized study with 200 μg/day of iodine supplementation, which could reflect the complexity of iodine metabolism during pregnancy. Furthermore, UIE in the third trimester in the control group (median 76 μg/l) is only slightly higher than the UIE we observed between 2003 and 2005 in an unselected population of 330 pregnant women tested during the second part of pregnancy (median 64 μg/l, 86% below 150 μg/l) [22], confirming that our area remains mildly iodine deficient.
We report in both groups a similar drop in FT4 levels in the second and third trimesters (up to 20%), without increase in TSH. This was true whatever the mode of analysis, paired or unpaired. This has been previously reported [1] and was interpreted either as a spurious measurement due to unreliable FT4 assay in pregnancy [23], or as hypothyroxinemia, considered ‘pathological ’ and possibly linked to ID [2]. We used a chemiluminescence assay that was shown to be reliable in pregnancy when compared to the direct equilibrium dialysis method coupled to mass spectrometry which is considered as the gold standard for FT4 measurement during and outside pregnancy [24]. As recently reviewed by Zimmerman [25], in the controlled trials with a similar design (with a supplementation from 100 to 230 μg/day) conducted in mild to moderately iodine-deficient pregnant women, there was no difference in maternal thyroxine levels between iodine-supplemented and control groups [10,14,16,17,18]. Only 2 of those studies reported lower maternal TSH [10,17]. In a study using higher dosage of supplementation (300 μg/day), Velasco et al. [19] reported lower FT4 and FT3 than in controls in the third trimester, which was unexpected, and was also associated with higher cord blood TSH of unclear significance. More recently, the same group reported a randomized study of iodized salt, 200 or 300 μg of KI/day, and showed a similar drop in FT4 (and FT3) without difference depending on the treatment group [20]. Thus, in our population, iodine supplementation given as early as the 10th week of gestation does not prevent the drop in FT4, which should be considered as a physiological feature in women with initial normal thyroid function since there is no concomitant increase in TSH. Therefore, it should be emphasized that the goal of iodine supplementation should not be the inhibition of FT4 drop. It could be hypothesized that iodine prophylaxis started well before conception could have more impact on FT4 during pregnancy, as suggested in an observational study of iodized salt consumption [26]. However, even in that case, a 20% drop in FT4 was observed, and so far, there is no interventional randomized data supporting this hypothesis. Furthermore, we also observed a drop in FT3 levels of a similar magnitude to the FT4 drop, not prevented by iodine supplementation, which further supports a physiological evolution. On the other hand, in women with predisposition to thyroid disease, in situation of ID, it is likely that FT4 levels fall lower than observed here due to the ‘stress ’ of pregnancy on a failing thyroid [1]. We present here a full assessment of thyroxine status throughout pregnancy, including FT4 and TT4 measurements and calculation of the TT4/TBG ratio. Indeed, there is an old debate about the respective value of TT4, FT4 measurements and the TT4/TBG ratio in pregnancy [23,27,28,29], especially based on the potential interference of FT4 immunoassays with binding protein. Interestingly, the TT4/TBG ratio, which is considered as a valid proxy for FT4 levels assessment [13] followed the same pattern as FT4 levels in our population. Thus, lower levels of FT4 should be considered as a ‘fact and not an artefact ’ [28]. Indeed, it is not because this result does not fit our preconception of what FT4 levels should be in pregnancy that the FT4 assay should be discarded [29]. Thus, our data bring convincing evidence that FT4 is a valuable assay to assess thyroid function in pregnancy in a daily clinical practice. However, it is important to establish laboratory-specific, trimester-specific FT4 reference ranges in pregnancy to define where biochemical hypothyroxinemia starts and avoid unnecessary treatment, which should be based primarily on fetal needs. It should be noted that the ATA guidelines do not recommend treatment of isolated hypothyroxinemia [4], while the recent Endocrine Society guidelines leave it to the discretion of the care giver [3]. On the other hand, TT4 increased as expected at the second trimester remaining steady afterwards and was unchanged with iodine supplementation. Therefore, iodine prophylaxis with 150 μg/day had no impact on FT4 or on TT4 level evolution, suggesting that, when thyroxine levels are the end point, it might not be required in a population with initial normal thyroid tests. However, when looking at Tg levels, iodine supplementation prevented the rise observed in controls, particularly in the paired analysis. We had also shown previously in the same population that maternal Tg at delivery was higher in the control group [30]. Our results on Tg are similar to those of Glinoer et al. [10] and Pedersen et al. [17], but at odds with those of Liesenkotter et al. [18], Nohr et al. [14] and Antonangeli et al. [16]. Interestingly, there was no difference in smoking status in our two groups, including the subgroup with paired analysis (data not shown). Tg is recognized as a marker of ID and is increased in endemic goiter [9]. Thus, iodine prophylaxis in pregnancy could be beneficial to decrease the prevalence of goitrogenesis in women [9]. However, if this is strongly suggested in women with initial hyper-stimulated thyroid [10], this has not been proven yet in women with strictly normal initial thyroid function [25]. In addition, we did not observe in our limited series a significant change in thyroid volume assessed by ultrasound, whether the women took iodine prophylaxis or not, suggesting that Tg could be a more sensitive parameter at least in the short term.
In conclusion, the early ‘drop ’ in FT4 levels and TT4/TBG without TSH increase during normal pregnancy in a mildly iodine-deficient area can be considered physiological since it is not influenced by iodine supplementation. Thus, FT4 is valuable to assess thyroid function in pregnancy in clinical practice as long as appropriate trimester-specific reference range is available. We have established our own reference range throughout pregnancy, setting the threshold for isolated hypothyroxinemia in our population. Therefore, the lower FT4 after the first trimester should not be mistaken for hypothyroxinemia. The question of the threshold for therapeutic intervention remains, especially since we lack strong clinical end point in the offspring. The meaning of such a drop in free available T4 and T3 at a time where the global production of thyroid hormones is increased to meet maternal and fetal needs is unknown and counter-intuitive. We could speculate that circulating levels of thyroid hormones may not give a full picture of the complex fetomaternal thyroid economy, which also includes the placenta as an important player [31]. These results on free thyroid hormones contrast with the impact of iodine supplementation on maternal Tg, and thus do not challenge the benefit of iodine prophylaxis in pregnancy.
Disclosure Statement
No conflict of interest. This work was funded by a grant from the French Ministry of Health and was promoted by the Direction of Clinical Research of Nice University Hospital. Vitamin treatment was provided by the Laboratory CCD (Paris, France) free of charge, and with no compensation in return.
Acknowledgements
We wish to thank the women who participated in this study and the pharmaceutical laboratory CCD (Paris, France), which kindly provided free treatments for all patients during the entire study. We wish to dedicate this paper to the memory of Eva Baez, data manager.
References
- 1.Glinoer D. The regulation of thyroid function in pregnancy: pathways of endocrine adaptation from physiology to pathology. Endocr Rev. 1997;18:404–433. doi: 10.1210/edrv.18.3.0300. [DOI] [PubMed] [Google Scholar]
- 2.Morreale de Escobar G, Obregon MJ, Escobar del Rey F. Is neuropsychological development related to maternal hypothyroidism or to maternal hypothyroxinemia? J Clin Endocrinol Metab. 2000;85:3975–3987. doi: 10.1210/jcem.85.11.6961. [DOI] [PubMed] [Google Scholar]
- 3.De Groot L, Abalovich M, Alexander EK, Amino N, Barbour L, Cobin RH, Eastman CJ, Lazarus JH, Luton D, Mandel SJ, Mestman J, Rovet J, Sullivan S. Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97:2543–2535. doi: 10.1210/jc.2011-2803. [DOI] [PubMed] [Google Scholar]
- 4.Stagnaro-Green A, Abalovich M, Alexander E, Azizi F, Mestman J, Negro R, Nixon A, Pearce EN, Soldin O, Sullivan S, Wiersinga W. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid. 2011;21:1–45. doi: 10.1089/thy.2011.0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pop VJ, Brouwers EP, Vader HL, Vulsma T, van Baar AL, de Vijlder JJ. Maternal hypothyroxinaemia during early pregnancy and subsequent child development: a 3 year prospective study. Clin Endocrinol. 2003;59:282–288. doi: 10.1046/j.1365-2265.2003.01822.x. [DOI] [PubMed] [Google Scholar]
- 6.Henrichs J, Bongers-Schokking JJ, Schenk JJ, Ghassabian A, Schmidt HG, Visser TJ, Hooijkaas H, de Muinck Keizer-Schrama SMPF, Hofman A, Jaddoe VVW, Visser W, Steegers EAP, Verhulst FC, de Rijke YB, Tiemeier H. Maternal thyroid function during early pregnancy and cognitive functioning in early childhood: the generation R study. J Clin Endocrinol Metab. 2010;95:4227–4234. doi: 10.1210/jc.2010-0415. [DOI] [PubMed] [Google Scholar]
- 7.Lazarus JH, Bestwick JP, Channon S, Paradice R, Maina A, Rees R, Chiusano E, John R, Guaraldo V, George LM, Perona M, Dall'Amico D, Parkes AB, Joomun M, Wald NJ. Antenatal thyroid screening and childhood cognitive function. N Engl J Med. 2012;366:493–501. doi: 10.1056/NEJMoa1106104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO Secretariat. Andersson M, de Benoist B, Delange F, Zupan J. Prevention and control of iodine deficiency in pregnant and lactating women, and in children less than 2 years of age: conclusions and recommendations of the Technical Consultation. Public Health Nutr. 2007;10:1606–1611. doi: 10.1017/S1368980007361004. [DOI] [PubMed] [Google Scholar]
- 9.Zimmermann MB. Iodine deficiency. Endocr Rev. 2009;30:376–408. doi: 10.1210/er.2009-0011. [DOI] [PubMed] [Google Scholar]
- 10.Glinoer D, De Nayer P, Delange F, Lemone M, Toppet V, Spehl M, Grün JP, Kinthaert J, Lejeune B. A randomized trial for the treatment of mild iodine deficiency during pregnancy: maternal and neonatal effects. J Clin Endocrinol Metab. 1995;80:258–269. doi: 10.1210/jcem.80.1.7829623. [DOI] [PubMed] [Google Scholar]
- 11.Delange F. Iodine deficiency as a cause of brain damage Postgrad Med J. 2011;77:217–220. doi: 10.1136/pmj.77.906.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pearce EN. What do we know about iodine supplementation in pregnancy? J Clin Endocrinol Metab. 2009;94:3188–3190. doi: 10.1210/jc.2009-1512. [DOI] [PubMed] [Google Scholar]
- 13.Petrovic I, Savin S, Spasic S, Cvejic D, Paunkovic N, Paunkovic J. The T4/TBG ratio in healthy subjects and in patients with disorders of thyroid function: correlation with T4 concentrations. Jugoslov Med Biohem. 2005;24:241–246. [Google Scholar]
- 14.Nohr SB, Jorgensen A, Pedersen KM, Laurberg P. Postpartum dysfunction in pregnant thyroid peroxidase antibody-positive women iodine deficiency: is iodine supplementation safe? J Clin Endocrinol Metab. 2000;85:3191–3198. doi: 10.1210/jcem.85.9.6799. [DOI] [PubMed] [Google Scholar]
- 15.Romano R, Jannini EA, Pepe M, Grimaldi A, Olivieri M, Spennati P, Cappa F, D'armiento M. The effects of iodoprophylaxis on thyroid size during pregnancy. Am J Obstet Gynecol. 1991;164:482–485. doi: 10.1016/s0002-9378(11)80004-9. [DOI] [PubMed] [Google Scholar]
- 16.Antonangeli L, Maccehini D, Cavaliere R, Di Giulio C, Reinhardt B, Pinchera A, Aghini-Lombardi F. Comparison of two different doses of iodide in the prevention of gestational goiter in marginal iodine deficiency: a longitudinal study. Eur J Endocrinol. 2002;147:29–34. doi: 10.1530/eje.0.1470029. [DOI] [PubMed] [Google Scholar]
- 17.Pedersen KM, Laurberg P, Iversen E, Knudsen PR, Gregersen HE, Rasmussen OS, Larsen KR, Eriksen GM, Johannesen PL. Amelioration of some pregnancy-associated variations in thyroid function by iodine supplementation. J Clin Endocrinol Metab. 1993;77:1078–1083. doi: 10.1210/jcem.77.4.8408456. [DOI] [PubMed] [Google Scholar]
- 18.Liesenkötter KP, Göpel W, Bogner U, Stach B, Grüters A. Earliest prevention of endemic goiter by iodine supplementation during pregnancy. Eur J Endocrinol. 1996;134:443–448. doi: 10.1530/eje.0.1340443. [DOI] [PubMed] [Google Scholar]
- 19.Velasco I, Carreira M, Santiago P, Muela JA, Garcia-Fuentes E, Sanchez-Munoz B, Gonzalez-Fernadez MC, Rodriguez A, Caballero F, Machado A, Gonzalez-Romero S, Anarte MT, Soriguer F. Effect of iodine prophylaxis during pregnancy on neurocognitive development of children during the first two years of life. J Clin Endocrinol Metab. 2009;94:3234–3241. doi: 10.1210/jc.2008-2652. [DOI] [PubMed] [Google Scholar]
- 20.Santiago P, Velasco I, Muela JA, Sanchez B, Martinez J, Rodriguez A, Berrio M, Gutierrez-Repiso C, Carreira M, Moreno A, Garcia-Fuentes E, Soriguer F. Infant neurocognitive development is independent of the use of iodised salt or iodine supplements given during pregnancy. Br J Nutr. 2013;4:1–9. doi: 10.1017/S0007114512005880. [DOI] [PubMed] [Google Scholar]
- 21.Stilwell G, Reynolds PJ, Parameswaran V, Blizzard L, Greenaway TM, Burgess JR. The influence of gestational stage on urine iodine excretion in pregnancy. J Clin Metab Endocrinol. 2008;93:1737–1742. doi: 10.1210/jc.2007-1715. [DOI] [PubMed] [Google Scholar]
- 22.Hiéronimus S, Bec-Roche M, Ferrari P, Chevalier N, Fénichel P, Brucker-Davis F. Iodine status and thyroid function of 330 pregnant women from Nice area assessed during the second part of pregnancy. Ann Endocrinol. 2009;70:218–224. doi: 10.1016/j.ando.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 23.Lee RH, Spencer CA, Mestman JH, Miller EA, Petrovic I, Braverman LE, Goodwin TM. Free T4 immunoassays are flawed during pregnancy. Am J Obstet Gynecol. 2009;200:260.e1–260.e6. doi: 10.1016/j.ajog.2008.10.042. [DOI] [PubMed] [Google Scholar]
- 24.Anckaert E, Poppe K, Van Uytfanghe K, Schiettecatte J, Foulon W, Thienpont LM. FT4 immunoassays may display a pattern during pregnancy similar to the dialysis ID-LC/tandem MS candidate reference measurement procedure in spite of susceptibility towards binding protein alterations. Clin Chem Acta. 2010;411:1348–1353. doi: 10.1016/j.cca.2010.05.032. [DOI] [PubMed] [Google Scholar]
- 25.Zimmermann MB. The effects of iodine deficiency in pregnancy and infancy. Paed Perinatal Epidemiol. 2012;26(suppl 1):108–117. doi: 10.1111/j.1365-3016.2012.01275.x. [DOI] [PubMed] [Google Scholar]
- 26.Moleti M, Pio Lo Presti V, Campolo MC, Mattina F, Galletti M, Mandofilno M, Violi MA, Giorgianni G, De Domenico D, Trimarchi F, Vermiglio F. Iodine prophylaxis using iodized salt and risk of maternal thyroid failure in conditions of mild iodine deficiency. J Clin Endocrinol Metab. 2008;93:2616–2621. doi: 10.1210/jc.2008-0352. [DOI] [PubMed] [Google Scholar]
- 27.Soldin OP, Tractenberg RE, Hollowell JG, Jonklaas J, Janicic N, Soldin SJ. Trimester-specific changes in maternal thyroid hormone, thyrotropin, and thyroglobulin concentrations during gestation: trends and associations across trimesters in iodine sufficiency. Thyroid. 2004;14:1084–1090. doi: 10.1089/thy.2004.14.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ball R, Freedman DB, Holmes JC, Midgley JEM, Sheehan CP. Low-normal concentrations of free thyroxin in serum in late pregnancy: physiological fact, not technical artefact. Clin Chem. 1989;35:1891–1896. [PubMed] [Google Scholar]
- 29.Migdley JE, Christofides ND. Free thyroxine assays: no going back! Am J Obstet Gynecol. 2010;202:e6. doi: 10.1016/j.ajog.2009.08.033. [DOI] [PubMed] [Google Scholar]
- 30.Hiéronimus S, Ferrari P, Gal J, Berthier F, Azoulay S, Bongain A, Fenichel P, Brucker-Davis F. Relative impact of iodine supplementation and maternal smoking on cord blood thyroglobulin in pregnant women with normal thyroid function. Eur Thyr J. 2012;1:264–273. doi: 10.1159/000342915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burns R, O'Herlihy C, Smyth PP. The placenta as a compensatory iodine storage organ. Thyroid. 2011;21:541–546. doi: 10.1089/thy.2010.0203. [DOI] [PubMed] [Google Scholar]