Abstract
Background
Health researchers have explored how different aspects of neighborhood characteristics contribute to health and well-being, but current understanding of built environment factors is limited.
Purpose
This study explores whether the association between stress and health varies by residential neighborhood, and if yes, whether built and social neighborhood environment characteristics act as moderators.
Methods
This study uses multilevel modeling and variables derived from geospatial data to explore the role of neighborhood environment in moderating the association of stress with health. Individual-level data (N=4,093) were drawn from residents of 45 neighborhoods within Philadelphia County, PA, collected as part of the 2006 Philadelphia Health Management Corporation's Household Health Survey.
Results
We find that the negative influence of high stress varied by neighborhood, that residential stability and affluence (social characteristics) attenuated the association of high stress with health, and that the presence of hazardous waste facilities (built environment characteristics) moderated health by enhancing the association with stress.
Conclusions
Our findings suggest that neighborhood environment has both direct and moderating associations with health, after adjusting for individual characteristics. The use of geospatial data could broaden the scope of stress–health research and advance knowledge by untangling the intertwined relationship between built and social environments, stress, and health. In particular, future studies should integrate built environment characteristics in health-related research; these characteristics are modifiable and can facilitate health promotion policies.
Keywords: Stress, Health, Neighborhood environment, Philadelphia
Introduction
Recent literature on neighborhood effects typically adopts multilevel designs, incorporating contextual data, to explain variations in health across residential areas. Researchers have explored how different aspects of neighborhood characteristics are associated with health and well-being [1, 2], though our current understanding of the mechanisms and processes by which neighborhood “gets under the skin” is limited [3, 4]. The research focus has begun to shift from asking whether to why neighborhood matters [5]. Although health researchers have worked to identify direct associations between health outcomes and neighborhood, the need for further exploration of potential mechanisms and indirect associations is needed. In this paper, our outcome measure is a composite measure of health (described below).
Stress is one of the precursors of illness. Stress has been linked to a wide range of health and social outcomes, such as cardiovascular diseases [6], cancers [7], deviant behaviors [8] as well as biological reactions [9]. Little is known, however, about whether stress varies by neighborhood and, if it does, what accounts for the variation. Kasl [10] defined “stress” as having four dimensions: an environmental exposure or experience; an appraisal of an environmental condition; a response to environmental exposure; and an interactive association between environmental demands and personal capability to fulfill these demands. Following Kasl, the formation of stress may be associated with both individual and neighborhood environment factors. To date, most neighborhood research has focused on the social dimension, finding socioeconomic conditions, deprivation, and social capital related to health [11, 12]. In contrast, measures of the neighborhood-built environment, even though potentially modifiable, have received relatively little attention in the literature.
In this paper, we explore several interrelated questions regarding stress and health: Does the association between stress and health vary by residential neighborhood? If yes, does the interaction between individual stress and neighborhood explain the phenomenon? Is the built environment as important as social environment in understanding the variation of stress across neighborhoods? To answer these questions, we explore the indirect relationship between neighborhood and health. Explicitly, if the association of stress with health varies by neighborhood, those factors moderating this spatially varying association should have an indirect influence on health. Furthermore, we investigate whether variables associated with the built environment were as crucial as the social environment factors that have been emphasized in the literature.
Research Framework
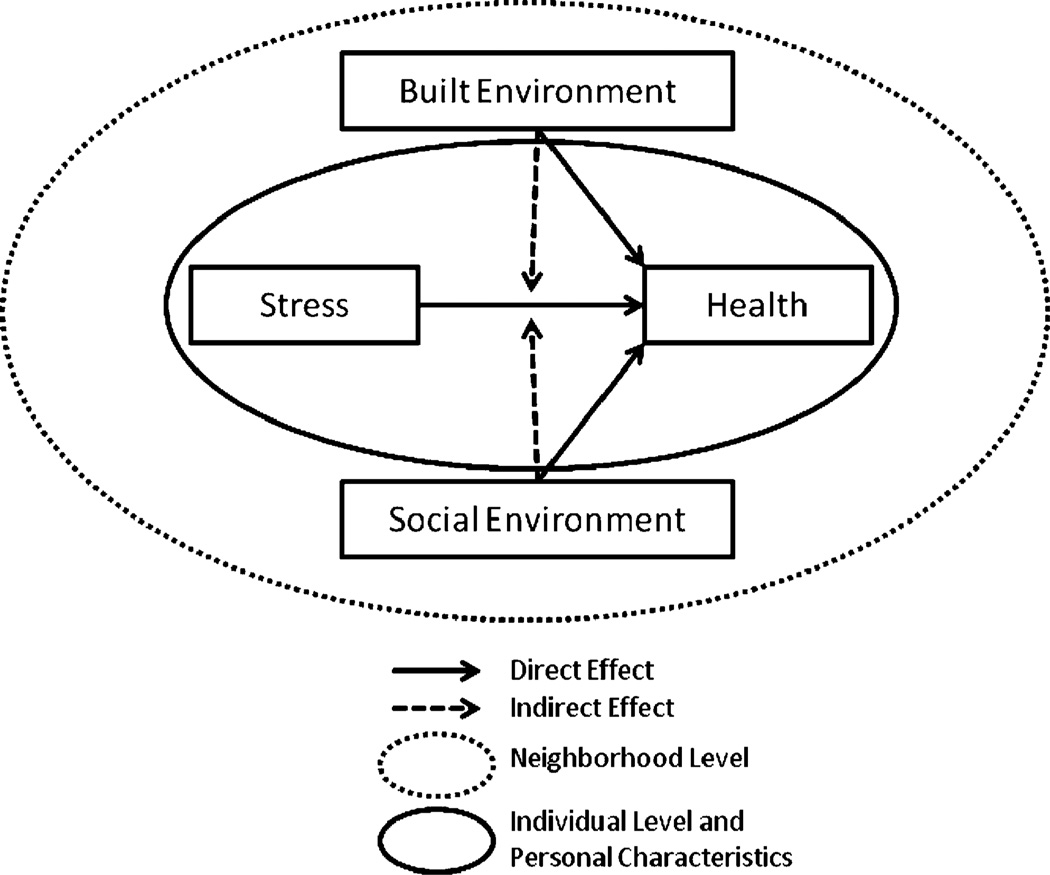
This paper provides a unique integration of geospatial data on built and social environment factors with individual-level survey data and explores associations that may provide insight in to how neighborhood environment “gets under the skin” [3]. The emergence of multilevel modeling and the multilevel framework has generated what has been described as an “explosion” of neighborhood effects studies, particularly in social research [13]. How “place gets into people” and how people influence place is enormously complex and multidimensional [4]. Unfortunately, this complexity and multidimensionality (e.g., endogenous effects, selection) is often simplified in multilevel modeling frameworks [14–17]. Figure 1 outlines the research framework of this study. Individuals are assumed to be embedded in their residential neighborhood. Within individuals, stress should be directly associated with (solid arrow) health. Beyond the individual level, both the social and the built environment are expected to be associated with variations in individual health across neighborhoods. Furthermore, the neighborhood environment is anticipated to be indirectly related to the association between stress and health (dashed arrow). We are particularly interested in the interaction between environment and stress [18].
Fig. 1.
Research framework of this study
At the individual level, demographic characteristics and socioeconomic status variables are fundamental predictors of health. The former comprises age, gender, marital status, and race/ethnicity while the latter includes employment status, education, health insurance, and poverty. Prior studies provided consistent findings that individual factors can be important determinants of health [19]. Unemployment, low education, and age were found to be negatively related to health [20], but marriage was protective for measures of well-being [21]. Similarly, access to health care, health insurance, and transportation were important and positively associated with health [22, 23].
At the neighborhood level, recent studies have demonstrated that social factors directly affect human health [24, 25]. Better social capital, neighborhood trust, and socioeconomic composition were related to improved health in the US [26]. In disadvantaged areas, explanations for poor health outcomes included poor air and water quality [27], environmental pollution sources [28], inferior housing conditions [29], low-quality food supply [30], insufficient investment in infrastructure [31], and crime [32]. While these studies provide evidence of the direct association of individual and neighborhood characteristics with health, few studies consider indirect associations between neighborhood characteristics and health. At least one recent study explored indirect associations more closely [33] concluding that the stability of a neighborhood moderates the relationship between stress and health. We incorporate both built and social environments into research as potential moderators to better understand pathways to health.
The association between the built environment and stress and mental health has been well-established in psychology [34, 35]. Poor neighborhood resources [22, 36], noise or busy traffic [37–39], and hazardous exposure [40–43] all have been reported to have positive associations with stress or other psychiatric symptoms. Clinically, respondents affected by very low doses of chemicals who showed physical symptoms as well as subtle psychological disturbances were identified as experiencing “hazardous waste syndrome” [44]. That is, stress and mental health may, in part, be determined by built environment characteristics. These characteristics, therefore, should be included in multilevel modeling studies as moderators. The interaction between stress and the built environment can help answer whether the effect of stress on health varies in magnitude as a function of the built environment. We introduce three possible built environment moderators: hazardous waste, traffic, and health care infrastructure.
In addition to the built environment, we consider components of the social environment as possible moderators. We focus on neighborhood safety, residential stability, and socioeconomic composition. It has been well documented that high crime rates are associated with a wide range of stress symptoms such as sleep disturbances, anxiety, and stress disorder [45, 46]. Similarly, witnessing acts of violence, being victims of crimes, or being aware of offenses are all associated with poor mental health [3, 47]. On the other hand, residential stability has been found to moderate the association between stress and health; operating through social support [48]. For example, a recent study concluded that the associations between stress and health were weaker for residents of more stable neighborhoods compared with those in high turnover areas [33]. A stable neighborhood enhances face-to-face interactions and strengthens participation among residents, provides a sense of consistency and belonging, and also promotes emotional support as well as access to material resources when individuals were exposed to stressors [33, 49]. Socioeconomic composition—usually measured by income, occupation, and education—has been argued to be the fundamental proxy describing the environment where people live. Several studies have found that life stress events, i.e., job loss, were more likely to be experienced by the members of poor neighborhoods [50, 51]. In addition, lower socioeconomic status (SES) status neighborhoods were associated with failing infrastructure and discriminatory behavior [52]. A longitudinal study concluded that the characteristics of poor infrastructure neighborhoods were sources of stress [53]. Thus, neighborhood socioeconomic composition appears to be a main component of the social environment and can help to capture the influence of omitted variables associated with stress. In summary, our analytic plan explores the moderating effects of both built and social environment.
Research Hypotheses
Our research framework leads to five hypotheses. (1) Higher stress is associated with worse health; even after controlling for other individual characteristics. (2) Built environment characteristics are associated with individual health, including that: (2.a) the presence of hazardous facilities is negatively related to health; (2.b) high traffic exposure is negatively related with health; and (2.c) greater availability of health care is positively related with health. As regards the moderating effects of the built environment between stress and health, we expect the negative association between stress and health to be (3.a) weaker in the neighborhood with less hazardous exposure; (3.b) less pronounced in the neighborhood with less traffic; and (3.c) reduced by the availability of health care. And with respect to the association between social environment factors and individual health, we expect: (4.a) neighborhood safety to be positively associated with health; (4.b) stable neighborhoods to be positively associated with health; and, (4.c) that socioeconomic composition is positively associated with health. (5) Finally, with regard to the moderating effects of the social environment between stress and health we expect: (5.a) neighborhood safety to weaken the negative association between stress and health; (5.b) the association between stress and health to be weakened in a stable neighborhood, and (5.c) the association between stress and health to be weakened in high-SES neighborhoods.
Methods
Study Population and Design
Individual-level data come from the Philadelphia Health Management Corporation's (PHMC) 2006 Household Health Survey, including comprehensive data on personal health behavior and health care experience in a five-county area in southeast Pennsylvania [54]. The 2006 PHMC was a telephone survey of over 10,000 households; the participants were interviewed in English or Spanish. A random-digit dial methodology based on a stratified sampling frame was used to ensure representation within 54 smaller geographic areas across a five-county area of southeast Pennsylvania. The response rate for the PHMC 2006 was 24% based on the American Association for Public Opinion Research response rate criterion #3 (which does not include partial interviews in the numerator and does not include all phone numbers of unknown eligibility in the denominator, but rather a proportion based on known residential plus non-residential phone numbers). This study is based on the data collected in PHMC 2006 on the 4,093 respondents of Philadelphia County. The 2006 PHMC also provides balancing weights, which are used in this study to reflect the varying probabilities of a person with particular features being selected for an interview [54]. The balancing weights are used in the multivariate analysis. While the response rate is low the proportion of the respondents in PHMC 2006 closely matches the demographic (age, race), social (marital status), and economic (educational attainment, employment status, poverty status) structure of Philadelphia County as reported by the US Census Bureau in their 3-year 2006–2008 release of the American Community Survey (ACS) [55]. The expected and notable exception is the lower participation of men in the PHMC (30% vs. 47% in the ACS). Research finds no significant biases as a result of response rate differences based on surveys with 50% and 25% response rates [56]. In a recent study, Holbrook, Krosnick and Pfent [57] found that lower response rates do decrease demographic representativeness though not by much and suggest that “This evidence challenges the assumptions that response rates are a key indicator of survey quality” (p. 528). Philadelphia County was divided into 45 neighborhoods based on aggregations of census tracts and input on the neighborhood boundaries from local planners, officials, and organizers [54]. Since the 1980s, the 45 neighborhood boundaries have remained unchanged across all previous PHMC surveys. Neighborhood-level data come from several data sources introduced below (see Table 1 for descriptive statistics).
Table 1.
Descriptive statistics of variables in this study
| Variables | VIF | Mean | SD | Min | Max |
|---|---|---|---|---|---|
| Individual level (N=4093) | |||||
| Health | NA | 0.00 | 0.86 | −2.72 | 1.17 |
| Stress level (reference = no stress) | |||||
| Below average | 2.08 | 0.19 | 0.39 | 0.00 | 1.00 |
| Average | 2.55 | 0.33 | 0.47 | 0.00 | 1.00 |
| Above average | 2.27 | 0.20 | 0.40 | 0.00 | 1.00 |
| High stress | 2.07 | 0.16 | 0.36 | 0.00 | 1.00 |
| Demographics | |||||
| Age (continuous) | 2.41 | 49.88 | 17.44 | 18.00 | 100.00 |
| Gender (Male=1, female=0) | 1.08 | 0.30 | 0.46 | 0.00 | 1.00 |
| Race (African American=1, non-African American=0) | 1.39 | 0.41 | 0.49 | 0.00 | 1.00 |
| Marital status (reference=single) | |||||
| Married/cohabiting (1, else=0) | 1.47 | 0.39 | 0.49 | 0.00 | 1.00 |
| Widowed/separated (1, else=0) | 1.71 | 0.28 | 0.45 | 0.00 | 1.00 |
| Socioeconomic status | |||||
| Employed (1, else=0, reference=others) | 2.58 | 0.53 | 0.50 | 0.00 | 1.00 |
| Retired (1, else=0, reference=others) | 3.30 | 0.22 | 0.42 | 0.00 | 1.00 |
| Incapable of working (1, else=0, reference=others) | 1.77 | 0.11 | 0.31 | 0.00 | 1.00 |
| Education (over high school=1, else=0) | 1.25 | 0.45 | 0.50 | 0.00 | 1.00 |
| Poverty status (below poverty line=1, else=0) | 1.22 | 0.17 | 0.38 | 0.00 | 1.00 |
| Religious service attendance (reference=never) | |||||
| Attending yearly (yes=1, no=0) | 1.83 | 0.26 | 0.44 | 0.00 | 1.00 |
| Attending monthly (yes=1, no=0) | 1.65 | 0.15 | 0.36 | 0.00 | 1.00 |
| Attending weekly (yes=1, no=0) | 2.21 | 0.41 | 0.49 | 0.00 | 1.00 |
| Neighborhood participation (reference=none) | |||||
| Joining one group (yes=1, else=0) | 1.21 | 0.23 | 0.42 | 0.00 | 1.00 |
| Joining at least two groups (yes=1, else=0) | 1.31 | 0.22 | 0.41 | 0.00 | 1.00 |
| Neighborhood trust | 1.19 | 0.00 | 0.99 | −2.98 | 1.70 |
| Access to medical resources | |||||
| Insured (having health insurance=1, else=0) | 1.50 | 0.89 | 0.31 | 0.00 | 1.00 |
| Dental insurance (having dental insurance=1, else=0) | 1.48 | 0.63 | 0.48 | 0.00 | 1.00 |
| Having regular source of care (yes=1, else=0) | 1.10 | 0.90 | 0.30 | 0.00 | 1.00 |
| Transportation difficulty in seeing a doctor (no=1, yes=0) | 1.15 | 0.88 | 0.32 | 0.00 | 1.00 |
| Neighborhood Level (N=45) | |||||
| Neighborhood safety | 2.87 | 0.00 | 1.00 | −1.86 | 2.12 |
| Residential stability | 6.11 | 0.00 | 0.93 | −3.25 | 1.64 |
| Medical resources | 1.81 | 0.00 | 1.00 | −0.55 | 4.03 |
| Daily vehicle miles traveled (standardized) | 1.29 | 0.00 | 1.00 | −1.13 | 4.14 |
| Social disadvantage | 3.55 | 0.00 | 1.00 | −1.65 | 2.38 |
| Concentrated affluence | 5.26 | 0.00 | 1.00 | −1.16 | 3.39 |
| Toxics release inventory sites (present=1, absent=0) | 1.61 | 0.60 | 0.50 | 0.00 | 1.00 |
| Residual waste operations (present=1, absent=0) | 1.39 | 0.40 | 0.50 | 0.00 | 1.00 |
VIF Variance Inflation Factor, SD Standard Deviation, Min. Minimum, Max. Maximum
Measures
Dependent Variable
Health was operationalized using a composite score derived from both physical health condition measures and a self-rated health measure (see Boardman [33]) for a similarly constructed dependent variable). First, respondents were asked if they had any of the following six physical health problems: asthma, a heart problem, diabetes, arthritis, high blood pressure, and high cholesterol. We summed and standardized the number of “no” responses to construct a measure of positive health (i.e., six “no” responses implies the absence of any health problem). Second, participants were also asked to evaluate their overall health from “excellent” to “poor.” Self-rated health has been identified as a valid predictor of various health outcomes, independent from other covariates [58]. This indicator was consistent with physical health (Cronbach's alpha=0.653). We standardized the self-rated health scores and averaged the physical condition measure within individuals to create the dependent variable used in the analysis (where higher scores indicate better health).
Independent Variables—Individual Level
Respondents rated their level of stress during the past year using a scale from 1 (no stress) to 10 (an extreme amount of stress). While we acknowledge the complexity of operationalizing stress, this was the only measure available in the data set. A subjective stress assessment has been argued to provide precisely what a stress researcher needs [59], and it can summarize the equilibrium of environmental demands and individual coping ability and thus reflect day-to-day stress. To capture the potential nonlinear association between stress and health, we categorized the stress level into five groups: stress-free (reference group; 1), below average (2–3), average (4–6), above average (7–8), and high stress (9–10).
Four demographic covariates were used. Age was a continuous variable measured in years. Gender was a dummy variable where males were coded 1 and females 0. Race was coded 1 if respondents self-identified as African Americans and 0 otherwise. Marital status was trichotomized into married/cohabiting, widowed/separated, and single (reference group). Three socioeconomic controls were included in the models. Employment status was categorized into four groups–employed, retired, incapable of working, and others (reference group). Education was a dummy variable coded 1 if respondents completed high school, 0 otherwise. Poverty was captured by a dummy variable, and coded 1 if the family income was below the federal poverty level, 0 otherwise.
We included several controls related to individual social networks in order to account for the effect of duration of residence on health. The PHMC 2006 did not include a question on the duration of residence in the present house/neighborhood so we do not have a direct measure. Several measures within PHMC 2006, however, do provide information on the strength of ties and the degree of embeddedness of respondents within their neighborhood. Religiosity was measured with the frequency of attending religious services. Respondents were categorized into four groups: weekly; monthly; yearly; and never (reference group). Neighborhood participation was measured with the number of local groups respondents belong to, coded as none (reference group), only one group, and two or more groups. In addition, we conducted factor analysis to generate a measure of neighborhood trust based on the extent to which respondents agreed with the following questions: “neighbors are willing to help each other” (factor loading=0.76); “neighbors ever worked together” (0.58); “belong to the neighborhood” (0.77); and “people in the neighborhood can be trusted” (0.74). The internal consistency among these questions was 0.66, and the total variance explained by the sole factor was 51.8%.
We used four variables associated with individual access to medical resources. Insurance status was coded 1 if respondents have health insurance, 0 if not. Dental insurance status was coded 1, otherwise 0. Respondents with a regular source of care were coded 1, 0 otherwise. Finally, we created a transportation difficulty measure, coded 1 if respondents ever canceled doctor appointments due to the lack of transportation.
Independent Variables—Neighborhood Level
At the neighborhood level, we identified four variables associated with built environment characteristics: traffic exposure, hazardous waste exposure based on (a) Toxic Release Inventory (TRI) and (b) Residual Waste Operations (RWO), and a measure of medical infrastructure.
The traffic exposure measure was derived from geospatial data. We used geographic information system (GIS) software, specifically ArcGIS [60], to create a novel, objective indicator of neighborhood-level traffic exposure within each neighborhood: daily vehicle miles traveled (DVMT). Similar to the “annual average daily traffic” by Houston et al. [38], DVMT was expected to capture both direct and moderating effects [18] of traffic exposure on health. Specifically, we used Pennsylvania Department of Transportation [61] geo-referenced data on traffic volume (based on the amount of vehicle traffic that traveled sections of road) to construct DVMT, which was the product of the length of road (in miles) and average daily traffic estimate. The neighborhood boundaries and the traffic network were overlaid in ArcGIS, and then, we averaged the DVMT of every road within each neighborhood. This yielded a measure of traffic exposure for each neighborhood. To avoid small estimated coefficients, the standardized score of DVMT was used in our analysis.
Two variables were correlated with hazardous exposure— the presence of TRI site and RWO site. The TRI site was a facility that manages chemicals released from industries including manufacturing, metal and coal mining, electric utilities, commercial hazardous waste treatment, and other industrial sectors [62]. The RWO was a primary facility related to the materials and products that were not able to be reused, recycled, or composted and require disposal technologies such as landfill and incineration [63]. The Pennsylvania Department of Environment Protection [64] geocoded the addresses of these facilities, and we overlaid these with neighborhood boundaries. The neighborhoods with TRI sites were coded 1, 0 if without. A similar coding scheme was applied to the RWO.
We generated a measure of medical infrastructure and capacity (medical resources) as this was a potential mechanism through which neighborhood can moderate the association of stress with health. Using the 2005–2006 data from the Pennsylvania Department of Health [65], we extracted all the licensed or approved hospitals located in Philadelphia County. Also, we calculated the following variables related to medical resources and condensed in to a factor score: (1) number of licensed and staffed beds per 1,000 population (0.98), number of licensed medical doctors per 1,000 population (0.93), number of hospitals (0.86), and number of patients receiving flu vaccine, age 65 years and older (0.79). Almost 80% of the total variance was explained by one factor.
As with the built environment, we generated four measures of the social environment: social disadvantage, concentrated affluence, residential stability, and neighborhood safety. The first three of these are motivated by Sampson and colleagues and prior research in urban sociology [66, 67]. Social disadvantage and concentrated affluence were derived from 2000 US Census data. Following a factor analysis using the varimax rotation method, seven social condition variables were calculated, and from these, the two factors were identified. Five variables loaded on “social disadvantage”: percent of households with resident/room ratio greater than 1 (0.78), percent of female-headed households (0.86), unemployment rate (0.94), poverty (0.96), and percent of people receiving public assistance (0.90). Two variables loaded on “concentrated affluence”: the percent of residents having at least a bachelor's degree (0.96) and the percent of people reporting managerial or professional occupations (0.95). These two factors together explained over 90% of the total variance. Residential stability was derived from two census variables: the percent of house ownership and the percent of residents living at the same address for 5 years. These two variables were highly correlated (0.71, p<0.001). We averaged the standardized scores to generate a single indicator of residential stability.
Our measure of neighborhood safety was derived from crime data. The tract-level crime data for 2004 from the Philadelphia Police Department were aggregated into neighborhood level and used to define neighborhood safety. The following crimes were summed for each neighborhood and converted to rates per 1,000 people: part I violent crimes, part 1 property crimes, and missing persons. A principal component analysis confirmed the three crime types belonged to the same concept; factor loadings for crime types were 0.91, 0.74, and 0.72, respectively, with 62% of the total variance explained. The factor scores calculated by the regression method represented neighborhood safety.
Analytic Strategy
To test the main hypotheses, we conducted a series of multilevel models using the statistical package HLM 6 [68]. We first implemented a null model where no explanatory variables were included, to justify the use of hierarchical modeling. This basic model was equivalent to a one-way ANOVA with two random effects (see Eq. 1). γ00 refers to the grand mean of the health measure. u0j adjusts the grand mean for the jth neighborhood. For instance, if the average health score of a neighborhood was greater than the grand mean, u0j should be positive. Likewise, if the average score was equal to the grand mean, u0j should be zero. Hence, rij is the offset to the grand mean for the ith respondent in the jth neighborhood. If the Chi-square test for u0j was statistically significant, we then have evidence that the mean health scores were not normally distributed across neighborhoods, suggesting that multilevel analysis may be used.
| Yij = β0j + rij | Individual Level |
| β0j = γ00 + u0j | Neighborhood Level |
| (1) |
where
| Yij | is the health score of the ith individual in the jth neighborhood |
| rij | is the random effect for the ith individual in the jth neighborhood |
| γ00 | is the mean health score in the data |
| u0j | is the random effect for the jth neighborhood |
Following the null model, the relationship between stress and health was examined. The individual characteristics were included in the models, and thus, the first hypothesis can be tested. To examine the direct effects of the neighborhood environment on individual health, the neighborhood-level variables were included in the intercept, and hence, the Eq. 1 could be expanded into Eq. 2, as below:
| (2) |
where
| γ00 | is the adjusted mean health score |
| γ0l | is the direct effect of neighborhood feature l |
| wlj | is the feature l of jth neighborhood |
| βkj | is the fixed effect of individual covariate k |
| xijk | is the covariate k of individual i at neighborhood j |
Finally, to test the moderating effects, the neighborhood-level measures were included in the process of estimating the relationship between stress and health. That is, the interactions between individual stress and neighborhood environment were considered, as shown in Eq. 3:
| γSTRESS,0 | is the adjusted effect of individual stress on health |
| γSTRESS,l | is the moderating effect of the neighborhood feature l |
| (3) |
A statistically significant γSTRESS,l indicates that the association of stress with health varies as a function of the neighborhood environment measure. We tested the random effect of stress across neighborhoods before adding covariates. If the random effect of stress varied by neighborhood, this suggests that neighborhood environment characteristics may account for the relationship between stress and health.
Results
Table 1 presents the descriptive statistics for all the variables in the study. More than one third of PHMC respondents have a stress level above average or high stress. Seventy percent of the respondents were females; 40% were African Americans; the average age was approximately 50 years, and a third of the participants were single. One third of the respondents were either retired or incapable of working, and the poverty rate was 17%. On all of these measures, except percent female, the PHMC closely resembles the population structure of Philadelphia County in 2006–2008 [55]. Over 40% of people attend weekly religious services and a slightly higher percent participate in at least one local group. Almost 90% of respondents report some form of health insurance coverage, though dental coverage was lower (63%). Approximately one in eight had canceled a doctor appointment due to transportation difficulty.
We use variance inflation factor (VIF) to examine whether multicollinearity is of concern. The rule of thumb is a VIF value greater than 10 indicates that results may be biased by collinearity [69]. While HLM does not provide any diagnostic statistics for multicollinearity, we can obtain these by implementing an ordinary least square regression with the same dependent and independent variables. In Table 1, none of the VIFs violated the rule of thumb. The highest VIFs at individual and neighborhood level were 3.3 and 6.1, respectively.
Following our analytic strategy, the random effect at the neighborhood level (u0j=0.1497, p value<0.001) in the null model was significant, suggesting random effects vary from neighborhood to neighborhood. In other words, the individual health scores vary by neighborhood of residence and residential neighborhood characteristics may account for the variations. In addition to the null model, Table 2 contains four other models in which stress and individual factors were added sequentially. First, we investigated the unadjusted relationships between stress and health (model I). Without controlling for other individual variables, the association between stress and health was significant for the high stress group (i.e., in contrast to those without any stress, the people in the high stress group are, on average, 0.29 points lower on our standardized health measure).
Table 2.
Estimates of the relationships between individual characteristics and health (N=4,093)
| Variables | Null | Model I | Model II | Model III | Model IV |
|---|---|---|---|---|---|
| Intercept | 0.0064 | 0.0164 | 1.0642*** | 0.9249*** | 0.9267*** |
| Individual level | |||||
| Stress level | |||||
| Below average | 0.0882 | −0.0875 | −0.0679 | −0.0673 | |
| Average | 0.0488 | −0.2265*** | −0.2134*** | −0.2129*** | |
| Above average | 0.0438 | −0.3038*** | −0.2697*** | −0.2704*** | |
| High stress | −0.2867 *** | −0.4910*** | −0.4391*** | −0.4289*** | |
| Demographics | |||||
| Age | −0.0168*** | −0.0175*** | −0.0174*** | ||
| Gender | −0.0062 | −0.0112 | −0.0139 | ||
| Race (African American) | −0.1512*** | −0.1468*** | −0.1528*** | ||
| Married/cohabiting | 0.0246 | 0.0106 | 0.0112 | ||
| Widowed/separated | −0.0337 | −0.0237 | −0.0241 | ||
| Socioeconomic status | |||||
| Employed | 0.2075*** | 0.1829*** | 0.1817*** | ||
| Retired | −0.1623*** | −0.1550** | −0.1584** | ||
| Incapable of working | −0.6687*** | −0.6324*** | −0.6333*** | ||
| Education | 0.1803*** | 0.1605*** | 0.1604*** | ||
| Poverty status | −0.0800* | −0.0476 | −0.0486 | ||
| Religious service attendance | |||||
| Attending yearly | −0.0526 | −0.0511 | |||
| Attending monthly | −0.0440 | −0.0427 | |||
| Attending weekly | −0.0271 | −0.0267 | |||
| Neighborhood participation | |||||
| Joining one group | 0.0343 | 0.0345 | |||
| Joining at least two groups | 0.0959*** | 0.0957*** | |||
| Neighborhood trust | 0.0220 | 0.0217 | |||
| Access to medical resources | |||||
| Insured | 0.0519 | 0.0520 | |||
| Dental insurance | 0.0050 | 0.0051 | |||
| Having regular source of care | −0.1408*** | −0.1424*** | |||
| No transportation difficulty | 0.2793*** | 0.2784*** | |||
| Variance component | |||||
| Intercept | 0.1497 *** | 0.0200 *** | 0.0074*** | 0.0062*** | 0.0056*** |
| High stress | NA | NA | NA | NA | 0.0161* |
p<.05
p<.01
p<.001
When demographic and socioeconomic covariates were included in model II, the negative association between stress and health was evident. Respondents with average, above average, and high stress were less healthy than those with no stress (the reference group). The strength of the association increased with the level of stress. Specifically, the association between high stress and health was roughly 1.6 and 2.2 times higher than those for above average stress and average stress, respectively. The negative association between high stress and health was larger after controlling for individual demographic and socioeconomic variables. In other words, these individual factors suppressed (or reduced) the noise (the uncorrelated component) between stress and health. Among the covariates, age, race, employment status, education, and poverty status were significant predictors of health. Consistent with expectations, those incapable of working were the least healthy among the employment status groups. Even after adjusting for age, retirees had worse health scores than the employed and others. African Americans had a lower health status. Residents with a high school diploma or not in poverty were healthier than their counterparts. While some studies suggested associations between marital status, gender, and health [70], the current study did not confirm this. The neighborhood-level random effect in model II remained significant while the magnitude shrank.
In model III, individual-level covariates related to religion, neighborhood participation, and access to medical resources were added. The association between stress and health was slightly reduced. Compared with the estimates in model II, all the coefficients of stress decreased but remained significant, and the stress gradient was robust; part of the variation in stress was captured by the inclusion of social participation and the lack of access to medical resources. Although most of the literature supported the argument that religious involvement promotes health [71, 72], we did not find a significant association between religious service attendance and health; though this might be due to the limitations of the measures available. However, residents participating in two or more local groups tended to be healthier than others. While the association between neighborhood trust and health was positive, it was not statistically significant. Respondents with no transportation difficulties accessing medical services were much healthier than those experiencing difficulties.
The neighborhood-level random effect remained significant in model III, indicating that the individual characteristics cannot fully explain the variation of health scores across neighborhoods. In this model, whether the association between stress and health differs by neighborhood was unclear. We included neighborhood characteristics and further examined the moderating effects between stress and health. Following Raudenbush and Bryk [73], we implemented a series of Chi-square tests to determine whether the random effect should be added. The results (not shown) indicate that only the high stress group needed a random effect (uSTRESS,j). Therefore, we extended model III by including this random effect (see Table 2, model IV). The estimated coefficients did not change greatly, and the aforementioned findings hold.
The Role of Neighborhood Environment in Moderating Stress and Health
Following the analytic strategy, the direct effects of both built and social environment were explored by adding the neighborhood covariates to the intercept. Comparing models VI and V (see Table 3), the inclusion of social neighborhood environment factors produced a minor change in the association between stress and health. Only social disadvantage was associated with health. Our social environment findings echo those of several recent studies [24, 74]. Neighborhoods containing a high proportion of disadvantaged residents tend to be characterized by underdeveloped infrastructure, lack of investment, and generally, poor living conditions. Thus, the residents in these areas tended to have worse health than their counterparts in neighborhoods with few disadvantaged residents. The variance component of the intercept decreased by almost 65% but remained significant.
Table 3.
Estimates of direct and moderating associations for both individual and neighborhood environment factors on health (N=4,093)
| Variables | Model V | Model VI | Model VII | Model VIII |
|---|---|---|---|---|
| Intercept | 0.9479*** | 0.9248*** | 0.9266*** | 0.9208*** |
| Individual level | ||||
| Stress level | ||||
| Below average | −0.0729 | −0.0700 | −0.0712 | −0.0706 |
| Average | −0.2173*** | −0.2148*** | −0.2157*** | −0.2152*** |
| Above average | −0.2792*** | −0.2742*** | −0.2752*** | −0.2752*** |
| High stress | −0.4360*** | −0.4345*** | −0.4404*** | −0.4192*** |
| Demographics | ||||
| Age | −0.0177*** | −0.0177*** | −0.0177*** | −0.0177*** |
| Gender | −0.0154 | −0.0115 | −0.0126 | −0.0127 |
| Race (African American) | −0.1341*** | −0.1367*** | −0.1359*** | −0.1364*** |
| Married/cohabiting | 0.0101 | 0.0100 | 0.0112 | 0.0114 |
| Widowed/separated | −0.0187 | −0.0172 | −0.0181 | −0.0161 |
| Socioeconomic status | ||||
| Employed | 0.1764*** | 0.1763*** | 0.1761*** | 0.1757*** |
| Retired | −0.1631*** | −0.1610*** | −0.1616*** | −0.1638*** |
| Incapable of working | −0.6267*** | −0.6261*** | −0.6255*** | −0.6243*** |
| Education | 0.1468*** | 0.1474*** | 0.1465*** | 0.1470*** |
| Poverty status | −0.0442 | −0.0437 | −0.0440 | −0.0439 |
| Religious service attendance | ||||
| Attending yearly | −0.0496 | −0.0504 | −0.0497 | −0.0475 |
| Attending monthly | −0.0396 | −0.0401 | −0.0398 | −0.0397 |
| Attending weekly | −0.0189 | −0.0205 | −0.0201 | −0.0188 |
| Neighborhood participation | ||||
| Joining one group | 0.0321 | 0.0345 | 0.0345 | 0.0338 |
| Joining at least two groups | 0.0909*** | 0.0928*** | 0.0920*** | 0.0912*** |
| Neighborhood trust | 0.0185 | 0.0195 | 0.0198 | 0.0204 |
| Access to medical resources | ||||
| Insured | 0.0445 | 0.0453 | 0.0431 | 0.0432 |
| Dental insurance | 0.0074 | 0.0073 | 0.0089 | 0.0114 |
| Having regular source of care | −0.1392*** | −0.1397*** | −0.1405*** | −0.1417*** |
| No transportation difficulty | 0.2743*** | 0.2729*** | 0.2740*** | 0.2739*** |
| Neighborhood level (N=45) | ||||
| Social Environment | ||||
| Neighborhood safety | 0.0010 | 0.0178 | 0.0083 | 0.0046 |
| Residential stability | 0.0049 | 0.0101 | −0.0116 | −0.0093 |
| Social disadvantage | −0.0466* | −0.0629** | −0.0708*** | −0.0647** |
| Social affluence | 0.0461 | 0.0477 | 0.0290 | 0.0263 |
| Built environment | ||||
| Medical resources | −0.0056 | −0.0058 | 0.0008 | |
| Daily vehicle miles traveled | −0.0482*** | −0.0490*** | −0.0468** | |
| Toxics release inventory sites | 0.0487 | 0.0486 | 0.0296 | |
| Residual waste operations | −0.0369 | −0.0405 | −0.0042 | |
| Moderating effects on high stress | ||||
| Social environment | ||||
| Neighborhood safety | 0.0853 | 0.1076 | ||
| Residential stability | 0.1552** | 0.1391* | ||
| Social disadvantage | 0.0350 | 0.0061 | ||
| Concentrated affluence | 0.1408** | 0.1641** | ||
| Built environment | ||||
| Medical resources | −0.0583 | |||
| Daily vehicle miles traveled | −0.0142 | |||
| Toxics release inventory sites | 0.1158 | |||
| Residual waste operations | −0.2292** | |||
| Variance components | ||||
| Intercept | 0.0020* | 0.0014 | 0.0017 | 0.0014 |
| High stress | 0.0157* | 0.0164* | 0.0150* | 0.0044 |
p<.05
p<.01
p<.001
In model VI, we introduced built environment factors. The association between stress and health was reduced roughly 2% by the built environment variables. As found in earlier studies [37, 75], traffic exposure had an adverse impact on health. While in England, medical resources were found to promote health [24], we did not find evidence of this. The variance component of the intercept was not significant in model VI, which indicated that the inclusion of both built and social environment factors could explain the variation in individual health across neighborhoods.
The final two models were designated to explore whether the neighborhood environment could moderate the association between high stress and health. Model VII showed that the relationship between high stress and health varied both by neighborhood residential stability and concentrated affluence. Specifically, the positive coefficient of residential stability (0.1552) suggested that the association between high stress and health (−0.4404) was reduced among the residents in stable neighborhoods. In other words, high stress had a stronger relationship for the residents in neighborhoods with high turnover rates or low house ownership than for those residents in relatively stable neighborhoods. Similarly, concentrated affluence (0.1408) moderated the negative association between high stress and health. That is, other things equal, the relationship between high stress and health tended to be weaker in more affluent neighborhoods.
With respect to the built environment, the presence of RWOs strengthened the association between high stress and health (see model VIII); high stress increased more than 50% (0.2292/0.4192) in a neighborhood with an RWO. Adjusting for other covariates, the relationship with high stress varied by hazardous exposure. Although we did not find a direct relationship between hazardous exposure and health, the moderating effect on health via stress was present. As noted previously, the presence of a potential threat on health does not necessarily lead to bad health, but could become an indirect factor affecting health. Model VIII confirmed this phenomenon; hazardous waste syndrome seemed to exist in Philadelphia County. The variance components of both the intercept and high stress were not significant, implying that variations in health and high stress at the neighborhood level might be associated with the built and social environment variables. We tested for multicollinearity in model VIII. No independent variables had a VIF greater than 10 (results not shown, but available upon request).
Revisiting Our Hypothesis
Hypothesis 1: We hypothesized that higher personal stress was associated with worse health. This association held even after controlling for other individual characteristics (see Table 2, model IV). Though there was no difference between no stress and below average stress, the gradient of stress from average to high stress verified the negative association between stress and health even after controlling for individual factors. Hypothesis 2: While we anticipated that both hazardous exposure and traffic burden were negatively associated with health, the analytic results confirmed that heavier traffic was associated with poorer health. The hypothesized protective effect of medical resources on health was not found. Hypothesis 3: Although hazardous exposure was not directly associated with health, it appeared to be indirectly related, via high stress. In short, two out of six built environmental hypotheses were confirmed: a heavier traffic burden was related to worse health (2.a), and the negative association between stress and health was weaker in the neighborhoods with less hazardous exposure (3.a). Hypotheses 4 and 5: Neighborhood safety had neither a direct nor a moderating association with health, and thus hypotheses (4.a) and (5.a) were not supported. Regarding residential stability, after controlling for individual social connection and network, a direct association with health was not found, but an indirect link was. Our 5.b hypothesis was verified—an unfavorable association between stress and health was weakened in a stable neighborhood. In our study, socioeconomic composition was measured by social disadvantage and concentrated affluence. We found both direct and indirect associations for socioeconomic composition. Specifically, social disadvantage was negatively related with individual health; a relationship that held in the final model. On the other hand, concentrated affluence moderated the relationship between stress and health, supporting hypothesis 5.c.
Discussion
Theoretically, this study advances the field by revealing potential indirect associations of both built and social environment factors on health for the relationship between stress and health. The negative relationship between stress and health appears to depend on the characteristics of residential neighborhoods, which, as we have shown, should not be considered or modeled as a fixed effect. Much previous research on the stress–health relationship focused on individual characteristics, but by using a GIS-based approach and drawing on geospatial data on the built environment, researchers should be able to incorporate different measures of neighborhood environment into their analysis. This study demonstrated how to fuse novel techniques and data to broaden the questions that can be posed and thus the scope of stress–health research. Such an approach may help to better understand complex relationships between neighborhood factors and health outcomes, improving our knowledge of why and how both built and social environment are important in health research [76]. In particular, some built environment factors are potentially modifiable, and better understanding of such factors may help guide policies that may reduce health inequality.
We have shown that stress has spatially varying relationships with health, and this association was moderated by both social and built environment characteristics. To improve health, policies providing affordable housing and lowering the cost of owning a house could help to establish more stable neighborhoods, reducing the burden of stress. Similarly, we confirmed the presence of potential threats in a neighborhood (i.e., hazardous RWO exposure) may not directly harm residents' health, but the relationship between high stress and health was intensified by the presence of such hazards within the residential neighborhood. That is, echoing the hazardous waste syndrome, “hazardous” facilities do not necessarily cause physical health problems, but their existence may be a source that is indirectly related to individual health via high stress. Enhancing communications between residents, industry and local officials may significantly reduce such indirect effects. Indeed, the relationship between health and neighborhood environments requires further investigation that may provide new insight into issues of environmental justice [76, 77].
There were several limitations in this paper. While the PHMC recruits multiple respondents in a neighborhood, due to confidentiality, precise locations were not available. This limits our ability to obtain individual specific proximity measures to hazardous sites, other neighborhood risks, as well as neighborhood resources. We realize that different risk exposure measures might yield different results [78]. Second, this study was a cross-sectional analysis. The relationships between health and other covariates should be viewed as tentative (note that different variables were derived from multiple sources spanning several years: US Census 2000, built environment data from 2007–2008, and individual survey data from 2006). A longitudinal research design that collects information on individual health and other covariates regularly and, moreover, one that documents changes in the built and social neighborhood environments is required for detecting causality and gaining a better understanding of the reciprocal dynamics between individuals and their residential neighborhood environments [79]. Third, in the literature, there has been little consensus on the appropriate definition of a neighborhood [80]. Census geographic units, such as blockgroups, tracts, and counties, have been used as neighborhoods in multilevel studies. We follow the PHMC definition based on input from local groups, social workers, and policy makers. Other area definitions would change the calibration of built and social neighborhood variables and thus might alter the findings aforementioned. Explicitly, the modifiable areal unit problem (MAUP) [81] and the influence of the level of geographic aggregation on health outcomes are worth noting [82]. Similarly, a major assumption underlying this study was that respondents were only affected by their residential neighborhood. That is, we can only embed people within their residential environment which by default ignores place-specific associations with health outcomes based on other spaces, such as the neighborhood where people work, play, shop, and socialize [83]. A more flexible hierarchical structure, i.e., a cross-classified or multiple membership model where individuals can be embedded in two or more nonhierarchical levels, may be required [84]. Another limitation was related to our measure of individual stress, a single self-rated measure. Any future work should employ a more thorough approach, such as a list of negative life events, chronic strains, or child traumas. Finally, contrary to expectations, our results find no association between gender or marital status and health. We looked more closely at these variables and at interactions with neighborhood participation and trust, but the substantive findings did not change (these results are available on request).
We identified significant variations in health and stress across neighborhoods. While controlling for individual features reduced the neighborhood variation in health, the neighborhood environment variables were still crucial in understanding why people were healthier in certain communities. Residents living in the areas characterized by high traffic volume and percent of disadvantaged population were generally not as healthy as those in the places with reduced traffic and high-SES families. The importance of socioeconomic composition in health research has been discussed in the past decade [1, 84], and our measure of traffic exposure with GIS further validated the relationship between traffic and health [38].
In sum, this study sheds more light on exploring the roles of built and social environment factors in health research. The neighborhood effects on human health have been widely examined; however, many neighborhood effect studies are only concerned whether neighborhood features are important instead of why and how they are important [5]. That is, earlier research underestimated, if not ignored, the interactions (moderating effects) between individual behavior/perception and the residential neighborhood environment where people live [18]. While hierarchical modeling has become popular, one of the strengths of this approach was not always utilized—explaining the interaction between individual and neighborhood characteristics. This study has tried to do this, and in addition, we incorporated several built environment characteristics that typically receive little attention. By doing so, we believe the questions regarding why and how neighborhood environment is crucial to human health can be more fully addressed. The integration of multilevel modeling and geospatial data on the built and social environment has advanced our knowledge of the indirect association between hazardous exposure and health via high stress.
Acknowledgements
This work was partially supported by internal funds from the Social Science Research Institute at Penn State. Additional support has been provided by the Geographic Information Analysis Core at Penn State's Population Research Institute, which receives core funding from the Eunice Kennedy Shriver National Institutes of Child Health and Human Development (R24-HD41025). We thank Laura Cousino Klein, Keith Aronson, Francine Axler, and Brian McManus for their comments and suggestions regarding our manuscript. All errors remain our own.
Contributor Information
Stephen A. Matthews, Email: matthews@pop.psu.edu, Population Research Institute, The Pennsylvania State University, University Park, PA 16802-6211, USA.
Tse-Chuan Yang, Email: tuy111@psu.edu, Social Science Research Institute, The Pennsylvania State University, 803 Oswald Tower, University Park, PA 16802-6211, USA.
References
- 1.Diez Roux AV. Invited commentary: Places, people, and health. Am J Epidemiol. 2002;155:516–519. doi: 10.1093/aje/155.6.516. [DOI] [PubMed] [Google Scholar]
- 2.Kawachi I, Berkman LF. Neighborhoods and health. New York: Oxford University Press; 2003. [Google Scholar]
- 3.Taylor SE, Repetti RL, Seeman T. Health psychology: What is an unhealthy environment and how does it get under the skin? Annu Rev Psychol. 1997;48:411–447. doi: 10.1146/annurev.psych.48.1.411. [DOI] [PubMed] [Google Scholar]
- 4.Cummins S, Curtis S, Diez-Roux AV, Macintyre S. Understanding and representing ‘place’ in health research: A relational approach. Soc Sci Med. 2007;65:1825–1838. doi: 10.1016/j.socscimed.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 5.Morenoff JD, Lynch JW. What makes a place healthy? Neighborhood influences on racial/ethnic disparities in health over the life course. In: Anderson NB, Rodolfo AB, Cohen B, editors. Critical perspectives on racial and ethnic difference in health in late life. Washington: National Academies; 2004. pp. 406–449. [Google Scholar]
- 6.Kristensen TS. Job stress and cardiovascular disease: A theoretic critical review. J Occup Health Psychol. 1996;1:246–260. doi: 10.1037//1076-8998.1.3.246. [DOI] [PubMed] [Google Scholar]
- 7.Sklar LS, Anisman H. Stress and cancer. Psychol Bull. 1981;89:369–406. [PubMed] [Google Scholar]
- 8.Wills TA, Sandy JM, Yaeger AM. Stress and smoking in adolescence: A test of directional hypotheses. Health Psychol. 2002;21:122–130. [PubMed] [Google Scholar]
- 9.Ader R. Psychosomatic and psychoimmunologic research. Psychosom Med. 1980;42:307–321. doi: 10.1097/00006842-198005000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Kasl SV. Stress and health. Annu Rev Public Health. 1984;5:319–341. doi: 10.1146/annurev.pu.05.050184.001535. [DOI] [PubMed] [Google Scholar]
- 11.Stafford M, Marmot M. Neighbourhood deprivation and health: Does it affect us all equally? Int J Epidemiol. 2003;32:357–366. doi: 10.1093/ije/dyg084. [DOI] [PubMed] [Google Scholar]
- 12.Brown AF, Ang A, Pebley AR. The relationship between neighborhood characteristics and self-rated health for adults with chronic conditions. Am J Public Health. 2007;97:926–932. doi: 10.2105/AJPH.2005.069443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Entwisle B. Putting people into place. Demography. 2007;44:687–703. doi: 10.1353/dem.2007.0045. [DOI] [PubMed] [Google Scholar]
- 14.Diez Roux AV. The examination of neighborhood effects on health: Conceptual and methodological issues related to the presence of multiple levels of organization. In: Kawachi I, Berkman LF, editors. Neighborhoods and health. New York: Oxford University Press; 2003. pp. 45–64. [Google Scholar]
- 15.Manski CF. Identification problems in the social sciences. Cambridge: Harvard University Press; 1995. [Google Scholar]
- 16.Oakes JM. The (mis)estimation of neighborhood effects: Causal inference for a practicable social epidemiology. Soc Sci Med. 2004;58:1929–1952. doi: 10.1016/j.socscimed.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 17.Vanderweele TJ. Ignorability and stability assumptions in neighborhood effects research. Stat Med. 2007;27:1934–1943. doi: 10.1002/sim.3139. [DOI] [PubMed] [Google Scholar]
- 18.Muller D, Judd CM, Yzerbyt VY. When moderation is mediated and mediation is moderated. J Pers Soc Psychol. 2005;89:852–863. doi: 10.1037/0022-3514.89.6.852. [DOI] [PubMed] [Google Scholar]
- 19.Kennedy BP, Kawachi I, Glass R, Prothrow-Stith D. Income distribution, socioeconomic status, and self rated health in the United States: Multilevel analysis. BMJ. 1998;317:917–921. doi: 10.1136/bmj.317.7163.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rogers RG, Hummer RA, Nam CB. Living and dying in the USA: Behavioral, health, and social differentials of adult mortality. San Diego: Academic; 2000. [Google Scholar]
- 21.Joung IMA, Stronks K, van de Mheen H, van Poppel FWA, van der Meer JBW, Mackenbach JP. The contribution of intermediary factors to marital status differences in self-reported health. J Marriage Fam. 1997;59:476–490. [Google Scholar]
- 22.Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing racial/ethnic disparities in access to care. Health Serv Res. 2003;38:809–829. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carlisle DM, Leake BD, Shapiro MF. Racial and ethnic disparities in the use of cardiovascular procedures: Associations with type of health insurance. Am J Public Health. 1997;87:263–267. doi: 10.2105/ajph.87.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cummins S, Stafford M, Macintyre S, Marmot M, Ellaway A. Neighbourhood environment and its association with self rated health: Evidence from Scotland and England. J Epidemiol Community Health. 2005;59:207–213. doi: 10.1136/jech.2003.016147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress:Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Ann Behav Med. 2001;23:177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- 26.Kawachi I, Kennedy BP, Glass R. Social capital and self-rated health: A contextual analysis. Am J Public Health. 1999;89:1187–1193. doi: 10.2105/ajph.89.8.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Daniels G, Friedman S. Spatial inequality and the distribution of industrial toxic releases: Evidence from the 1990 TRI. Soc Sci Q. 1999;80:244–262. [Google Scholar]
- 28.Anderton DL, Anderson AB, Oakes JM, Fraser MR. Environmental equity: The demographics of dumping. Demography. 1994;31:229–248. [PubMed] [Google Scholar]
- 29.Robert SA. Community-level socioeconomic status effects on adult health. J Health Soc Behav. 1998;39:18–37. [PubMed] [Google Scholar]
- 30.Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. Am J Public Health. 2005;95:660–667. doi: 10.2105/AJPH.2004.042150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington: National Academy; 2002. [PubMed] [Google Scholar]
- 32.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 33.Boardman JD. Stress and physical health: The role of neighborhoods as mediating and moderating mechanisms. Soc Sci Med. 2004;58:2473–2483. doi: 10.1016/j.socscimed.2003.09.029. [DOI] [PubMed] [Google Scholar]
- 34.Lawrence RJ. Healthy residential environments. In: Bechtel RB, Churchman A, editors. Handbook of environmental psychology. New York: Wiley; 2002. pp. 394–412. [Google Scholar]
- 35.Evans GW, Wells NM, Moch A. Housing and mental health: A review of the evidence and a methodological and conceptual critique. J Soc Issues. 2003;59:475–500. [Google Scholar]
- 36.Campbell JL. Patients' perceptions of medical urgency: Does deprivation matter? Fam Pract. 1999;16:28–32. doi: 10.1093/fampra/16.1.28. [DOI] [PubMed] [Google Scholar]
- 37.Gee GC, Takeuchi DT. Traffic stress, vehicular burden and wellbeing: A multilevel analysis. Soc Sci Med. 2004;59:405–414. doi: 10.1016/j.socscimed.2003.10.027. [DOI] [PubMed] [Google Scholar]
- 38.Houston D, Wu J, Ong P, Winer A. Structural disparities of urban traffic in Southern California: Implications for vehicle-related air pollution exposure in minority and high-poverty neighborhoods. J Urban Aff. 2004;26:565–592. [Google Scholar]
- 39.Song Y, Gee GC, Fan Y, Takeuchi DT. Do physical neighborhood characteristics matter in predicting traffic stress and health outcomes? Transp Res, Part F Traffic Psychol Behav. 2007;10:164–176. [Google Scholar]
- 40.Edelstein MR. Contaminated communities. Boulder: Westview; 1988. [Google Scholar]
- 41.Neutra R, Lipscomb J, Satin K, Shusterman D. Hypotheses to explain the higher symptom rates observed around hazardous waste sites. Environ Health Perspect. 1991;94:31–38. doi: 10.1289/ehp.94-1567952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Elliott SJ, Taylor SM, Walter S, Stieb D, Frank J, Eyles J. Modelling psychosocial effects of exposure to solid waste facilities. Soc Sci Med. 1993;37:791–804. doi: 10.1016/0277-9536(93)90373-c. [DOI] [PubMed] [Google Scholar]
- 43.Luginaah IN, Taylor SM, Elliott SJ, Eyles JD. Community reappraisal of the perceived health effects of a petroleum refinery. Soc Sci Med. 2002;55:47–61. doi: 10.1016/s0277-9536(01)00206-4. [DOI] [PubMed] [Google Scholar]
- 44.Task Force on Clinical Ecology. Clinical ecology—a critical appraisal. West J Med. 1986;144:239–245. [PMC free article] [PubMed] [Google Scholar]
- 45.Osofsky JD. The effects of exposure to violence on young children. Am Psychol. 1995;50:782–788. doi: 10.1037//0003-066x.50.9.782. [DOI] [PubMed] [Google Scholar]
- 46.Berman SL, Kurtines WM, Silverman WK, Serafini LT. The impact of exposure to crime and violence on urban youth. Am J Orthopsychiatry. 1996;66:329–336. doi: 10.1037/h0080183. [DOI] [PubMed] [Google Scholar]
- 47.Green DL, Pomeroy EC. Crime victims: What is the role of social support? J Aggress Maltreat Trauma. 2007;15:97–113. [Google Scholar]
- 48.James SA, Schulz AJ, Van Olphen J. Social capital, poverty, and community health: An exploration of linkages. In: Saegert S, Thompson JP, Warren MR, editors. Social capital and poor communities. New York: Russell Sage Foundation; 2001. pp. 165–188. [Google Scholar]
- 49.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 50.Krivo LJ, Peterson RD. Extremely disadvantaged neighborhoods and urban crime. Soc Forces. 1996;75:619–648. [Google Scholar]
- 51.Fang J, Madhavan S, Bosworth W, Alderman MH. Residential segregation and mortality in New York City. Soc Sci Med. 1998;47:469–476. doi: 10.1016/s0277-9536(98)00128-2. [DOI] [PubMed] [Google Scholar]
- 52.Schulz A, Williams D, Israel B, et al. Unfair treatment, neighborhood effects, and mental health in the Detroit metropolitan area. J Health Soc Behav. 2000;41:314–332. [PubMed] [Google Scholar]
- 53.Dalgard OS, Tambs K. Urban environment and mental health. A longitudinal study. Br J Psychiatry. 1997;171:530–536. doi: 10.1192/bjp.171.6.530. [DOI] [PubMed] [Google Scholar]
- 54.Philadelphia Health Management Corporation. The 2006 household health survey. Philadelphia: Philadelphia Health Management Corporation; 2006. [Google Scholar]
- 55.U.S. Census Bureau. American Community Survey 2006–2008. U.S. Census Bureau; (2006–2008). [Google Scholar]
- 56.Keeter S, Kennedy C, Dimock M, Best J, Craighill P. Gauging the impact of growing nonresponse on estimates from a national RDD telephone survey. Public Opin Q. 2006;70:759–779. [Google Scholar]
- 57.Holbrook AL, Krosnick JA, Pfent A. Response rates in surveys by the news media and government contractor survey research firms. In: Lepkowski J, Harris-Kojetin B, Lavrakas PJ, editors. Advances in telephone survey methodology. New York: Wiley; 2007. pp. 499–528. [Google Scholar]
- 58.Benyamini Y, Idler EL. Community studies reporting association between self-rated health and mortality: Additional studies. 1995 to 1998. Res Aging. 1999;21:392–401. [Google Scholar]
- 59.Lazarus RS. Theory-based stress measurement. Psychol Inq. 1990;1:3–13. [Google Scholar]
- 60.ESRI. ArcGIS Desktop 9.3. Redlands: Environmental Systems Research Institute; 2008. [Google Scholar]
- 61.Pennsylvania Dept of Transportation. PennDOT—Pennsylvania traffic counts 2008. Harrisburg: Bureau of Planning and Research, Geographic Information Division; 2008. [Google Scholar]
- 62.Environmental Protection Agency. Toxic chemical release inventory TRI data for sites in Pennsylvania. [Accessibility verified May 20. 2008]; Available at http://www.pasda.psu.edu. [Google Scholar]
- 63.EnviroCentre. Residual waste research. UK: Glasgow; 2007. [Google Scholar]
- 64.Pennsylvania Department of Environmental Protection. Commercial hazardous waste operations. [Accessibility verified May 20, 2008]; Available at http://www.pasda.psu.edu. [Google Scholar]
- 65.Rosenberry S. Hospital. [Accessibility verified May 20, 2008]; Available at http://www.pasda.psu.edu. [Google Scholar]
- 66.Sampson RJ, Morenoff JD, Earls F. Beyond social capital: Spatial dynamics of collective efficacy for children. Am Sociol Rev. 1999;64:633–660. [Google Scholar]
- 67.Morenoff JD, Sampson RJ. Violent crime and the spatial dynamics of neighborhood transition: Chicago, 1970–1990. Soc Forces. 1997;76:31–64. [Google Scholar]
- 68.Scientific Software Inc. Hierarchical linear and nonlinear modeling HML 6. Lincolnwood: Scientific Software Inc; 2008. [Google Scholar]
- 69.Menard SW. Applied Logistic Regression Analysis. London: Sage; 2002. [Google Scholar]
- 70.Waite LJ, Gallagher M. The case for marriage: Why married people are happier, healthier, and better off financially. New York: Doubleday; 2000. [Google Scholar]
- 71.Hummer RA, Rogers RG, Nam CB, Ellison CG. Religious involvement and U.S. adult mortality. Demography. 1999;36:273–285. [PubMed] [Google Scholar]
- 72.Ellison CG, Hummer RA, Cormier S, Rogers RG. Religious involvement and mortality risk among African American adults. Res Aging. 2000;22:630–667. [Google Scholar]
- 73.Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd ed. Thousand Oaks: Sage; 2002. [Google Scholar]
- 74.Macintyre S, Ellaway A, Cummins S. Place effects on health: How can we conceptualise, operationalise and measure them? Soc Sci Med. 2002;55:125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- 75.Babisch W, Fromme H, Beyer A, Ising H. Increased catecholamine levels in urine in subjects exposed to road traffic noise: The role of stress hormones in noise research. Environ Int. 2001;26:475–481. doi: 10.1016/s0160-4120(01)00030-7. [DOI] [PubMed] [Google Scholar]
- 76.Bowen W. An analytical review of environmental justice research: What do we really know? Environ Manage. 2002;29:3–15. doi: 10.1007/s00267-001-0037-8. [DOI] [PubMed] [Google Scholar]
- 77.Lee C. Environmental justice: Building a unified vision of health and the environment. Environ Health Perspect. 2002;110(Suppl 2):141–144. doi: 10.1289/ehp.02110s2141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Thomas D, Stram D, Dwyer J. Exposure measurement error: Influence on exposure-disease. Relationships and methods of correction. Annu Rev Public Health. 1993;14:69–93. doi: 10.1146/annurev.pu.14.050193.000441. [DOI] [PubMed] [Google Scholar]
- 79.Kan H, Heiss G, Rose KM, Whitsel EA, Lurmann F, London SJ. Prospective analysis of traffic exposure as a risk factor for incident coronary heart disease: The Atherosclerosis Risk in Communities (ARIC) study. Environ Health Perspect. 2008;116:1463–1468. doi: 10.1289/ehp.11290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Galster G. On the nature of neighbourhood. Urban Stud. 2001;38:2111–2124. [Google Scholar]
- 81.Openshaw S. The modifiable areal unit problem Vol. 38 of concepts and techniques in modern geography: CATMOG series. Norwich: GeoBooks; 1983. [Google Scholar]
- 82.Soobader MJ, LeClere FB. Aggregation and the measurement of income inequality: Effects on morbidity. Soc Sci Med. 1999;48:733–744. doi: 10.1016/s0277-9536(98)00401-8. [DOI] [PubMed] [Google Scholar]
- 83.Matthews SA. The salience of neighborhood: Some lessons from sociology. Am J Prev Med. 2008;34:257–259. doi: 10.1016/j.amepre.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 84.Mair CF, Diez Roux AV, Galea S. Are neighborhood characteristics associated with depressive symptoms? A critical review. J Epidemiol Community Health. 2008;62:940–946. doi: 10.1136/jech.2007.066605. [DOI] [PubMed] [Google Scholar]