Abstract
Objective
to review and update the evidence for different forms of manual therapy (MT) for patients with different stages of non-specific low back pain (LBP).
Data sources
MEDLINE, Cochrane-Register-of-Controlled-Trials, PEDro, EMBASE.
Method
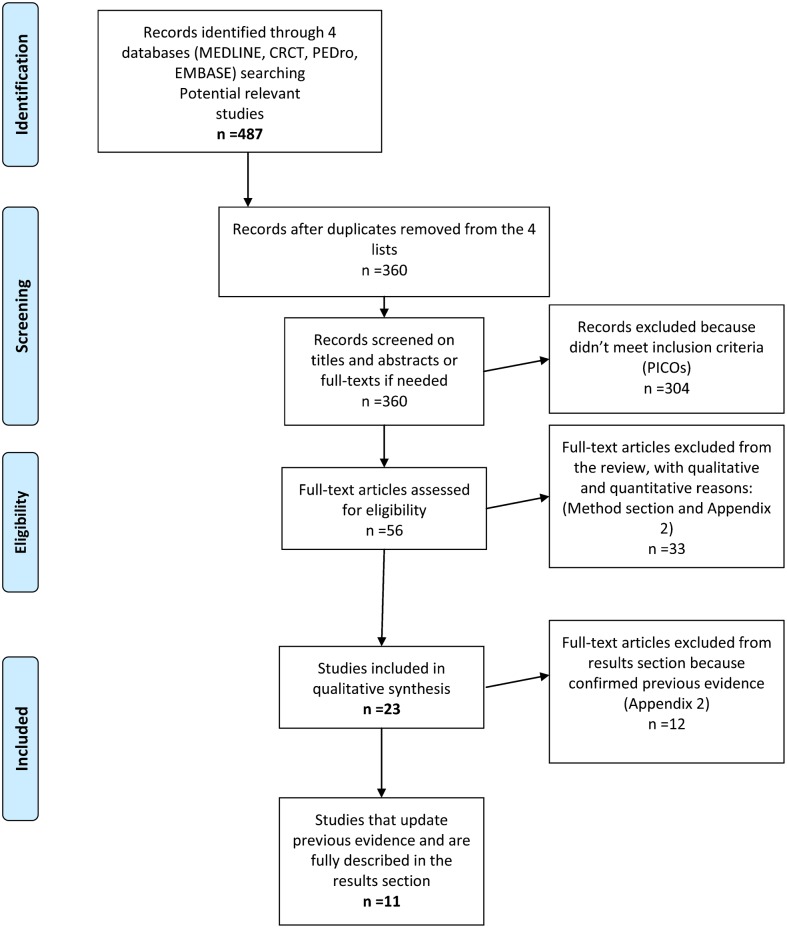
A systematic review of MT with a literature search covering the period of January 2000 to April 2013 was conducted by two independent reviewers according to Cochrane and PRISMA guidelines. A total of 360 studies were evaluated using qualitative criteria. Two stages of LBP were categorized; combined acute–subacute and chronic. Further sub-classification was made according to MT intervention: MT1 (manipulation); MT2 (mobilization and soft-tissue-techniques); and MT3 (MT1 combined with MT2). In each sub-category, MT could be combined or not with exercise or usual medical care (UMC). Consequently, quantitative evaluation criteria were applied to 56 eligible randomized controlled trials (RCTs), and hence 23 low-risk of bias RCTs were identified for review. Only studies providing new updated information (11/23 RCTs) are presented here.
Results
Acute–subacute LBP: STRONG-evidence in favour of MT1 when compared to sham for pain, function and health improvements in the short-term (1–3 months). MODERATE-evidence to support MT1 and MT3 combined with UMC in comparison to UMC alone for pain, function and health improvements in the short-term.
Chronic LBP: MODERATE to STRONG-evidence in favour of MT1 in comparison to sham for pain, function and overall-health in the short-term. MODERATE-evidence in favour of MT3 combined with exercise or UMC in comparison to exercise and back-school was established for pain, function and quality-of-life in the short and long-term. LIMITED-evidence in favour of MT2 combined with exercise and UMC in comparison to UMC alone for pain and function from short to long-term. LIMITED-evidence of no effect for MT1 with extension-exercise compared to extension-exercise alone for pain in the short to long-term.
Conclusion
This systematic review updates the evidence for MT with exercise or UMC for different stages of LBP and provides recommendations for future studies.
Keywords: Non-specific low back pain, Manual therapy, Spinal manipulation, Efficacy, Randomized controlled trials
Introduction
After headaches and chronic fatigue, low back pain (LBP) is the most reported complaint, with more than 80% of the population reporting LBP at some point in their life.1,2 In developed countries, LBP has enormous and growing indirect and direct costs for society and public health organizations.3,4
The majority of LBP cases are described as non-specific as there is no identifiable pathology on radiological imaging.2 Indeed there is a poor correlation between findings on radiological imaging and symptoms, with a radiological diagnosis identified in only 15% of cases.5–9 Hence, LBP is often a symptom of unknown origin and etiology.2,5,10,11
Many factors have been identified as possible causes or contributing factors to LBP. For example nociceptive inputs, particularly in acute–subacute conditions from various spine structures can cause pain, including zygapophysial joints, intervertebral discs and sacro-iliac joints.5,12–14 In chronic LBP, psychosocial factors are of prime importance in explaining the prolongation of pain.2,15,16 Additional factors linked to chronic LBP include obesity and physical deconditioning associated with sedentary lifestyles.2,17 Moreover, genetic factors have been strongly linked to LBP through their influence on pain perception and psychosocial factors.2,18
In general terms, in the case of acute LBP, reports suggest that 75–90% of cases recover within 6 weeks irrespective of medical intervention, whereas up to 25% are at risk of developing chronic pain and disability.1,2 Indeed, many individuals with LBP have a number of persisting or recurring symptoms.1,5,8,19 Chronic LBP therefore represents a considerable challenge because recovery is unlikely to occur, despite considerable medical advances.20
In physical therapy practice, various forms of manual therapy (MT) are currently used to manage LBP.7,21–23 Manual therapists use a range of treatment approaches including various passive techniques such as mobilization and manipulation as well as a variety of different forms of exercise. The use of these approaches, along with clinical reasoning based on the bio-psycho-social model, represents the essence of MT (www.ifompt.com).24
This systematic review (SR) focuses on the effects of commonly used MT approaches identified through a comprehensive evidence based search strategy of low-risk of bias clinical trials. Three categories of passive MT techniques are defined; MT1 (lumbopelvic manipulation: high-velocity-low-amplitude thrust) MT2 (non-thrust lumbo-pelvic mobilization and soft-tissue techniques),25–27 and MT3 (combination of MT1 and MT2). We also considered passive MT techniques (MT1–3) combined or not with exercise (specific or general) or combined with usual medical care (UMC) (stay active, reassurance, education and medication).11,27,28
The popularity and use of MT for the management of LBP has grown, in part supported by the inclusion of MT in various clinical practice guidelines.5,10,23,29 This is despite uncertainty regarding the levels of evidence for the effectiveness of different approaches in MT at different stages of LBP.5,7,10,22,29–36
Previous SRs have reported that in general terms, MT is considered better than a placebo treatment or no treatment at all for LBP.7,30,35–40 These reviews failed to establish levels of evidence for other forms of treatment such as UMC or exercise in comparison to MT.35,37,39,40 In addition, previous SRs have not investigated which MT approaches (MT1–3), when combined with UMC or exercise, are more effective for LBP. The present SR updates previous reviews, and is the first to focus specifically on different MT approaches for different stages of LBP. New findings, as well as new evidence to inform findings from previous systematic reviews,41–45 are presented.
Methods
This SR was conducted in accordance with the PRISMA and Cochrane-Collaboration-Back-Review-Group (CCBRG) updated guidelines for SR.46,47
Search strategy
A literature search of randomized controlled trials (RCTs) published in English between 2000 and 2013, on the efficacy of MT in the treatment of LBP was conducted independently by two reviewers in four electronic databases: MEDLINE, Cochrane-Register-of-Controlled-Trials, PEDro, and EMBASE. The detailed search strategy in MEDLINE is presented in Appendix 1, and was adapted to search in the three other databases.
Based on information revealed in the titles and abstracts, a first selection of articles was performed using the inclusion criteria described below. A final selection was conducted after a blinded critical appraisal of the quality of the studies. A consensus was reached at each step (Fig. 1) on the studies to be included. In cases of disagreement, a third reviewer made the necessary decision.
Figure 1.
PRISMA flowchart of inclusion.
Inclusion criteria
Study design
RCTs from the period of January 2000 to April 2013 were included only if (i) they presented a low-risk of bias, (ii) if LBP cases treated with MT were compared to a randomized control group receiving either no treatment, a placebo procedure, or another effective therapy for LBP and (iii) if the randomization methods were appropriate and clearly reported, with moreover (iv) a single (assessors blinded) or quasi-double-blind design (assessors and patients blinded).
Patients
LBP is distinguished on the basis of the duration of the pain episode: acute (<6 weeks), subacute (6–12 weeks) and chronic (>12 weeks).2,29 However, this distinction may not be satisfactory and it has been argued that categorization should be on the basis of other factors including location, symptoms, duration, frequency, and severity.48 In this SR, we used a combination of duration, location and symptoms to specify the study population:
Studies were included if subjects were males and females aged between 18 and 60 years suffering from acute–subacute (0–12 weeks) or chronic (>12 weeks) LBP. Acute and subacute categories were combined because of their similarities in contrast to chronic LBP category, where psycho-social factors appear more important.16,49,50
LBP is defined as pain in the lower back between the lowest ribs and inferior gluteal folds.46,51 Given that people with LBP may present with radicular pain, LBP is defined according to the following Quebec-Task-Force (QTF) classification: (1) LBP alone (QTF 1), (2) LBP with radiating pain into the thigh but not below the knee (QTF 2), (3) LBP with nerve root pain without neurologic deficit (QTF 3), or (4) LBP with nerve root pain with neurologic deficit (QTF 4).52 In the present SR, only trials that contained patients in classes QTF 1–3 were included.
Interventions
Among the included trials, we considered three categories of the most common MT techniques represented in the intervention groups. MT1 comprised high-velocity-low-amplitude thrust of the lumbo-pelvic region with ‘cavitation’.7,21,22,27,37,53 MT2 comprised mobilization and soft-tissue-techniques including ‘myofascial’, ‘myotensive’ or ‘harmonic’ techniques on the lumbo-pelvic region.22,27,37,54 MT3 comprised the combination of MT1 and MT2. Furthermore, sub-categorization of groups MT1–3 was based on the addition or not of exercises either specific (for example based on directional preference, stabilization, and motor control) or general (for example global strengthening, cardiovascular endurance, stretching and range-of-motion exercises) or UMC.1,21,32,55
Control groups
The control groups received no treatment, placebo, UMC, or exercise.
Outcome measures of effectiveness
The outcome measures were classified according to the CCBRG recommendations: pain, function, overall-health and quality of life (Table 1). Timing of the follow-up measurements was defined as very-short-term (end of treatment/discharge to 1 month), short-term (1–3 months), intermediate-term (3 months–1 year), or long-term (1 year or more).46,47,51
Table 1. Classification of outcome measures and Cochrane Collaboration Back Review Group (CCBRG) levels of evidence for evaluating interventions46,47.
| Outcome measures | Validated assessment tools |
| Pain | Visual Analogue Scale or Numerical Pain Rating Scale |
| Functional disabilities | Oswestry Disability Index, Roland Morris Disability Questionnaire, Fear Avoidance Belief Questionnaire, Disability Rating Index, or Patient Specific Function Scale |
| Overall-health improvement | Short form health survey |
| Quality of life | Patient Satisfaction with Care, Modified Zung Self-Rated Depression Score and State Trait Anxiety Inventory, return to work, sick leave, and medication use, adverse effects |
| Strength of evidence | Conditions description |
| Strong | Consistent findings from multiple ‘high quality trials’ = level A |
| Moderate | Consistent findings among multiple ‘low quality trials’ corresponding to moderate quality in this systematic review = Level B, and/or one level A |
| Limited | One level B |
| Conflicting | Inconsistent findings among multiple trials |
| No evidence | No trials |
Quality assessment
Two independent reviewers assessed the risk of bias, methodological quality, data-extraction and clinical relevance of each trial.
Quantitative and qualitative criteria were assessed by applying the CCBRG criteria.46,47 Quantitative risk of bias was assessed using an 11-point check-list (see Appendix 1).47
Qualitative criteria were: a clear distinction and separation between combined acute–subacute and chronic LBP categories at baseline; a detailed description of the MT intervention allowing the reviewers to classify the MT techniques according to MT1–MT3 classification system; and a single-blind (assessors blinded) or quasi-double-blind (assessors and patients blinded) design.
We considered as ‘high-quality’ those RCTs with quasi-double-blind designs that met at least 9/11 of the CCBRG criteria. ‘Low-quality’ RCTs status was assigned to studies of single-blind design with a minimum score of 7/11 (Tables 2 and 3). The dichotomy of classification into ‘high’ or ‘low’ qualities study is required when using the system of CCBRG to determine the strength of evidence (Table 1) and must be clearly described. To reduce the number of studies included in this SR, only studies that present new findings or update previous SR are described. Moreover similarly to another SR,56 to facilitate clarity of presentation, RCTs were only included if they were of low-risk of bias, and either high quality (indicated by a ‘A’) or moderate quality (indicated by a ‘B’).
Table 2. Summary of articles for patients with acute–subacute LBP.
| AUTHORS sample size LBP status | Methodological quality of studies | Intervention+co-intervention | Comparison group+co-intervention | Outcomes measures of interest | Clinical relevance status on timing outcomes: between groups P value and effect sizes |
| Santilli et al.57 (2006) N = 102 | Level A 10/11 | MT1 | Sham MT1 | Local and radiating pain (VAS) | YES: at 45 days, P<0.0001 and MD = 1.8; at 90 days, P<0.0001 and MD = 1.8 |
| ALBP 1–3 | Care provider not blinded | 5 times per week for maximum 4 weeks | 5 times per week for maximum 4 weeks | Time to pain free status | YES: At 180 days, for local pain: P<0.005 and MD = 22% and for radiating pain: P<0.0001 and MD 35% |
| Overall-Health (SF-36) | NO: non-significant differences between groups | ||||
| Hoiriis et al.58 (2004) N = 192 | Level A 9/11 | MT1+drug placebo | Sham MT1+myorelaxant drug | Pain (VAS) | YES: 4 weeks, P<0.05 and SMD = 0.70 |
| ALBP 1 | Care provider not blinded? no intention-to-treat-analysis | 7 sessions over 2 weeks for all groups | Sham MT1+placebo drug | Functional disabilities (ODI) | NO: at 4 weeks, NS and SMD = 0.35 (MT1 vs myorelaxant), 0.29 (MT1 vs placebo) |
| Von Heymann et al.59 (2013) N = 101 | Level A 10/11 | MT1+drug placebo | Sham MT1+placebo drug | Pain (VAS) | YES: at 9 days between groups P = 0.013 and MD = 2.0 |
| ALBP 1-2 | Care provider not blinded | 2–3 sessions over 1 week for all groups | Sham MT1+diclofenac | Functional disabilities (RMDQ) | YES: at 9 days between groups P = 0.013 and SMD = 0.60 |
| Quality of life (SF-12, medication consumption, work-off) | NO: non-significant differences between groups | ||||
| Bishop et al.60 (2010) N = 88 | Level B 8/11 | MT1 + UMC | UMC alone | Functional disabilities (RMDQ) | YES: at 16–24 weeks, P = 0.002 and MD = 2.6 |
| ALBP 1–2 | Care provider and patients not blinded, no intention-to-treat-analysis | 2–3 sessions over 4 weeks | |||
| Cruser et al.61 (2012) N = 63 | Level B 9/11 | MT3+UMC | UMC alone | Pain (VAS) | YES: at 4 weeks: for pain now, P = 0.025 and SMD = 1.04; for pain typical, P = 0.020 and SMD = 0.88 |
| ALBP 1–3 | Care provider and patients not blinded | 4 sessions over 4 weeks | Functional disabilities (RMDQ) | YES: at 4 weeks: P = 0.026 and SMD = 0.56 |
Note: ALBP = acute LBP; ASLBP = acute and subacute LBP: 1 = LBP alone, 2 = LBP radiating not below knee, 3 = LBP radiating below knee without neurologic deficit. MT = manual therapy; MT1 = spinal manipulation, MT2 = spinal mobilization techniques; MT3 = MT1+MT2. UMC = usual medical care. NS = non-statistically significant difference. SMD = between groups standardized mean of difference; MD = between groups mean of difference. Yes = P<0.05+moderate-large effect size (SMD, MD) in favour of MT. VAS = Visual Analogical Scale; NPRS = Numerical Pain Rating Scale; ODI = Oswestry Disability Index; RMDQ = Roland-Morris Disability Questionnaire; SF-36 = short-form-health-survey.
Table 3. Summary of articles for patients with chronic LBP.
| AUTHORS Sample size LBP status | Methodological quality of studies | Intervention group+co-intervention | Comparison group+co-intervention | Outcomes measures of interest | Clinical relevance status on timing outcomes: between groups p-value and effect sizes |
| Ghroubi et al.62 (2007) N = 64CLBP1 | Level A 9/11Care provider not blinded? for ITT | MT14 sessions per week over 1 month | Sham MT11 session over 1 month | Pain (VAS)Functional disabilities (ODI) | YES: at 4 weeks, P<0.001 and SMD = 0.86; 8 weeks, P<0.001 and SMD = 0.54 |
| YES: at 8 weeks, P<0.001 and SMD = 0.40 | |||||
| Senna et al.63 (2011) N = 93CLBP1–2 | Level A 10/11Care provider not blinded | MT1 non-maintained | Sham MT1 | Pain (VAS) | YES: at 10 months, P<0.005 and MD = 1.9 |
| MT1 maintained 3 sessions per week over 1 month for all groups, with 1 session/2 weeks during 9 months for MT1 maintained | Functional disabilities (ODI)Overall-Health (SF36) | YES: at 10 months, P<0.001 and MD = 18.9YES: at 10 months, P<0.001 and MD = 7.8 | |||
| Niemistö et al.32 (2003) N = 204CLBP1–3 | Level B 8/11Care provider and patients not blinded? for ITT | MT2+exercise and UMC4 sessions of 60 minutes over 1 month | UMC1 session of 60 minutes over 1 month | Pain (VAS)Functional disabilities (ODI) | YES: at 1 year, P<0.001 and SMD = 0.60YES: at 1 year, P = 0.002 and SMD = 0.45 |
| Aure et al.49 (2003) N = 49CLBP1–3 | Level B 9/11Care provider and patients not blinded | MT3+exercise2 sessions of 45 minutes per week over 8 weeks for each group | Exercise | Pain (VAS) | YES: at 1 year: P<0.05 and MD = 1.5 |
| Functional disabilities (ODI) | YES: at 1 year: P<0.05 and MD = 9 | ||||
| Quality of life: Return to work | YES: at 1 month, P<0.01 and MD = 40% | ||||
| Cecchi et al.34 (2010) N = 210CLBP1–2 | Level B 9/11Care provider not blinded | MT3+UMC4–6 sessions of 20 minutes/week over 4–6 weeks | Back school+UMC Physiotherapy+UMC15 sessions of 60’ over 3 weeks | Pain (NPRS) | YES: at 1 year, P<0.001 and SMD = 0.7 (MT3+UMC vs Back school+UMC), and SMD = 1.1 ( MT3+UMC vs physiotherapy+UMC) |
| Functional disabilities (RMDQ) | YES: at 1 year: P<0.001 and SMD = 0.7 (MT3+UMC vs Back school+UMC) and SMD = 0.73 (MT3+UMC vs physiotherapy+UMC) | ||||
| Rasmussen et al.64 (2008) N = 72CLBP1–3 | Level B 8/11No for patient and care provider blinded and? for ITT | MT1+extension exercises3 sessions over 1 month+everyday exercise over 1 month. | Extension exercises aloneEveryday exercise over 1 month | Back and leg pain (VAS) | NO: at 1 month and 1 year, NS differences for all outcomes measures |
Note: CLBP = chronic LBP: 1 = LBP alone, 2 = LBP radiating not below knee, 3 = LBP radiating below knee without neurologic deficit. MT = manual therapy, MT1 = spinal manipulation, MT2 = spinal mobilization techniques, MT3 = MT1+MT2, MT3+specific and general exercises. UMC = usual medical care. NS = non-statistically significant difference. SMD = between groups standardized mean of difference, MD = between groups mean of difference. Yes = P<0.05+moderate-large effect size (SMD, MD) in favour of MT. VAS = Visual Analogical Scale, NPRS = Numerical Pain Rating Scale, ODI = Oswestry Disability Index, RMDQ = Roland-Morris Disability Questionnaire, SF-36 = short-form-health-survey.
Strength of evidence and clinical relevance
Strength of evidence was determined by grouping similar ‘Patients Interventions Comparisons Outcomes Study design’ to provide an overall level of evidence (Table 1) on the efficacy of the MT techniques (Table 4). Based on CCBRG guidelines,47,51 the effect sizes were independently collected or calculated by two authors, and used to assess the clinical relevance of MT interventions on outcome measures. We report the between groups means of difference (MD = mean A–mean B) or Cohen’s standardized means of difference (SMD = mean A–mean B/mean SD). In this SR, the clinical relevance was determined by two conditions and scored by ‘YES’ in favour of the intervention group; if there were (i) significant difference between groups (P<0.05) associated (ii) with between groups effect sizes equal or superior to the minimal clinically important difference (MD) or moderate to large effect (SMD) on specific outcome measure (Tables 2 and 3).
Table 4. Summary findings from systematic review for MT combined or not with exercise or usual medical care for LBP. Strength of new and updated evidence is shown in underlined and in bold text. Confirmation of previous evidence shown in bold text.
| Categories of MT interventions vs comparison group | Quality of evidence (A = high; B = moderate) | Strength of evidence for interventions |
| ACUTE (<6 weeks) and SUBACUTE (6–12 weeks) LBP | ||
| MT1 vs Sham MT1 | 3 RCTs, Level A57–59 n = 395 | STRONG evidence in favour of MT1 in comparison to sham MT1 for acute LBP, for PAIN, function, overall-health and quality of life improvements in the short-term (<3 months). |
| MT1 and MT3 combined with UMC vs UMC alone | 2 RCTs Level B60,61 n = 151 | MODERATE evidence in favour of MT1 and MT3 combined with UMC in comparison to UMC alone for PAIN, functional improvement and quality of life from very-short to short-term in patients with acute LBP. |
| MT1 with ROM exercise vs MT2 with exercise or exercise alone | 2 RCTs Level B n = 243 (Cleland et al., 2009; Childs et al., 2004) | MODERATE evidence in favour of MT1 with exercise as compared to MT2 with exercise or exercise alone for pain relief and function improvement at very-short-term and short-term. Functional improvement is also present at intermediate-term (6 months) in a specific subgroup of patients with acute–subacute LBP. |
| MT3 combined with exercise ‘early’ vs the same intervention ‘delayed’ | 1 RCT Level B n = 102 (Wand et al., 2004) | LIMITED evidence in favour of an early intervention of MT3 combined with exercise in comparison to the same intervention delayed, on functional status and overall improvement at very-short-term and on overall improvement at intermediate-term in patients with acute LBP. |
| MT3 with UMC vs UMC alone | 2 RCTs Level B n = 339 (Curtis et al., 2000; Juni et al., 2009) | MODERATE evidence for no difference between MT3 combined with IMC in comparison to UMC alone, for pain reduction, functional recovery, and improvement in quality of life for very-short to intermediate-term in acute LBP. |
| MT3 combined with exercise vs UMC alone | 1 RCT Level B n = 402 (Hay et al., 2005) | LIMITED evidence for no difference between MT3 combined with exercise vs UMC alone in terms of pain reduction and improvements of function from short to long-term in patients with acute–subacute LBP |
| MT2 vs Sham ultra sound | 1 RCT Level A n = 240 (Hancock et al., 2007) | MODERATE evidence for no difference between MT2 and sham ultra sound in terms of pain reduction and functional improvements from very-short to short-term in acute LBP population. |
| MT3 combined with interferential therapy vs MT3 or interferential therapy alone | 1 RCT Level B n = 240 (Hurley et al., 2004) | LIMITED evidence for no difference between MT3 associated with interferential therapy and MT3 alone or interferential therapy alone in terms of pain reduction, functional improvements, and quality of life improvement in patients with acute–subacute LBP. |
| CHRONIC LBP (>12 weeks ) | ||
| MT1 vs Sham MT1 | 2 RCTs Level A62,63 n = 157 | MODERATE-STRONG evidence in favour of MT1 as compared to sham MT1, in terms of pain reduction, functional improvements and overall-health improvement at SHORT-term to INTERMEDIATE-term in patients with chronic LBP. |
| MT3 combined with exercise or with UMC vs exercise alone and back school | 2 RCTs level B34,49 n = 259 | MODERATE evidence in favour of MT3 combined with exercise or with UMC as compared to exercise alone and back school in terms of pain and function and quality of life improvement from short to long-term in patients with chronic LBP. |
| MT2 combined with exercise and UMC vs UMC alone | 1 RCT Level B32 n = 204 | LIMITED evidence in favour of MT2 combined with exercise and UMC in comparison to UMC alone in terms of pain reduction and function improvement from short to long-term in patients with chronic LBP. |
| MT1 with extension exercise vs extension exercise alone | 1 RCT Level B64 n = 72 | LIMITED evidence for no difference between MT1 combined with extension exercise in comparison to extension exercise alone in improving pain in the short-term and long-term in patients with chronic LBP. |
| MT2 vs UMC MT2 vs acupuncture | 1 RCT Level B n = 262 (Cherkin et al., 2001) | LIMITED evidence in favour of MT2 as compared to UMC and acupuncture in terms of pain, function, and quality of life from short-term to long-term in patients with chronic LBP. |
| MT3 vs exercise | 2 RCTs Level B n = 452 (Ferreira et al., 2007; Critchley et al., 2007) | MODERATE evidence for no difference between interventions in terms of pain reduction, functional recovery and quality of life improvement in patients with chronic LBP. |
| MT3 vs Sham MT3 | 1 RCT Level A n = 91 (Licciardone et al., 2003) | MODERATE evidence for no difference between interventions in terms of pain reduction, functional improvement, and patient satisfaction with care in very short-term and intermediate-term for patients with chronic LBP. |
Note: MT = manual therapy; MT1 = manipulation; MT2 = mobilization and soft-tissue-techniques; MT3 = MT1+MT2. UMC = usual medical care; exercise = specific and/or general exercise.
Results
Two reviewers performed the initial selection of articles based on keywords. Upon discussion, the reviewers achieved consensus on inclusion of 56 trials that met the selection criteria based on their titles and abstracts. After critical appraisal of these 56 studies, 23 RCTs were retained (Fig. 1). Only 11/23 of these RCTs were found to have new evidence or updated previous SRs and are fully presented here. Appendix 2 and Table 4 present a summary of the remaining 12 RCTs that are not detailed in this results section.
The studies’ characteristics and effect sizes on outcome measures are presented for acute–subacute (Table 2) and chronic LBP (Table 3). A qualitative SR was undertaken on the 11 low-risk of bias RCTs, five studies were classified as level A quality, and six as level B quality.
Effects of interventions on acute and subacute LBP
MT versus sham-MT
Santilli et al.,57 Hoiriis et al.,58 and von Heymann et al.59 (studies rated as level A quality) assessed the effects of MT1 in comparison to sham-MT1 in patients with acute LBP.
Santilli et al.57 compared lumbo-pelvic rotational manipulation toward the pain-free direction to simulated manipulation not following any specific pattern and not involving rapid thrust. The frequency of treatment was 5 days per week until pain relief occurred or up to a maximum of 20 sessions of 5 minutes. For LBP up to 3 months, MT1 was more effective in decreasing local pain, radiating pain, and the duration of pain with clinical relevance (P<0.0001 and mean of difference of 1.8). No statistically significant differences were found for overall-health improvement and psychosocial outcomes. At 6 months, the percentage of pain-free patients was significantly higher in the MT1 group with mean difference of 22% for local pain (P<0.005) and of 35% for radiating pain (P<0.001). Two patients, one in MT1 and one in sham-MT1, were dissatisfied with treatment and stopped.
Hoiriis et al.58 investigated the effects of lumbo-pelvic manipulation in prone or side-lying position combined with a drug placebo, in comparison to sham-MT1 combined with a muscle relaxant or with a drug placebo. Sham-MT1 consisted of manual light pressure on the lumbar spine in both positions (prone and side-lying). All groups received eight visits over 2 weeks and showed significant improvements in pain relief and disability (P<0.0001) and depression scores (P<0.0001). Clinically relevant differences between groups could only be identified in favour of the intervention group for pain relief in the very short term with P<0.05 and standardized mean difference of 0.70. However, further evaluation revealed that the perception of true MT was significantly higher (P<0.05) in the intervention group than in either of the two control groups. Indeed, the sham maneuver did not closely approximate the manipulation technique.
von Heymann et al.59 explored the efficacy of lumbo-pelvic rotational manipulation in side-lying position and placebo-diclofenac in comparison to Sham-MT1 with diclofenac or placebo-diclofenac. Sham MT1 was performed using real manipulation in a prone position but at the incorrect location (i.e. on a non-dysfunctional sacro-iliac-joint) to mimic as closely as possible the intervention being tested. This sham procedure is not supposed to have any influence on the lumbar dysfunction and is not believed to harm the patient. All groups received 2–3 visits over a 1 week period. There was a clear and clinically relevant difference at very-short-term follow up (9 days) between the groups (P = 0.013), the intervention group showed a standardized mean difference of 0.60 on functional improvement with similar result for pain and quality of life. No adverse effects or harm were reported in this study. These results suggested that real MT1 had clinically superior effects than NSAID and placebo interventions.
MT with UMC versus UMC alone
Bishop et al.60 and Cruser et al.61 (studies rated as level B quality) compared respectively MT1 (2–3 sessions per week over four weeks) and MT3 (1 session per week over four weeks) combined with UMC, to UMC alone in patients with acute LBP from QTF 1–2.
Bishop et al.60 reported clinically relevant differences in favour of the intervention group in terms of functional improvement (P = 0.002 and mean difference of 2.6) at 16 and 24 weeks, but there were no significant differences for pain and physical functioning. In the short-term (4 weeks), Cruser et al.61 determined clinically relevant differences in favour of MT3 compared to UMC alone for pain now (P = 0.025 and SMD of 1.04) and pain typical (P = 0.020 and SMD of 0.88) and a standardized mean difference of 0.56 for function associated with significantly greater satisfaction with treatment and overall-health improvement (P<0.01). The authors concluded that compared to UMC, MT160 and MT361 combined with UMC provides clinically greater improvement in function and pain relief.
Effects of interventions on chronic LBP
MT versus sham-MT
Ghroubi et al.62 and Senna et al.63 (studies rated as level A quality) investigated, respectively, the effectiveness of MT1 in a side-lying position (painful side-up) and MT1 in supine position (toward the painful side), as compared to sham-MT1 (mimic of lumbo-pelvic manipulation without final impulsion to provide minimal likelihood of therapeutic effect); on pain, function and overall health in patients with chronic LBP from QTF 1–2. True-MT1 of 4 sessions spread over one month for Ghroubi et al.,62 or 16 sessions over 1 month for Senna et al.,63 led to significant improvements for pain ([Ghroubi et al.62 reported standardized mean difference of 0.86 at 4–8 weeks with P<0.001]; [Senna et al.63 reported mean difference of 1.9 at 10 months with P<0.005]), for functional outcomes ([Ghroubi et al.62 reported standardized mean difference of 0.40 at 4–8 weeks with P<0.001]; [Senna et al.63 reported mean difference of 18.9 at 10 months with P<0.001]). Only Senna et al.63 reported an overall-health improvement of mean difference of 7.8 at 10 months (P<0.001). The authors62,63 concluded that MT1 is clinically effective in treating patients with chronic LBP in the short-term, but to obtain long-term benefit on all outcome measures requires maintenance of MT1 every 2 weeks.63
MT combined with other interventions
Niemistö et al.32 (rated as level B quality) investigated the effects of combined MT2 (myotensive lumbo-pelvic mobilization techniques) with exercises (stabilizing exercise to correct lumbo-pelvic rhythm) and UMC in comparison to UMC alone (patient education, stay active approach, ergonomic instruction, home general exercises, and educational-booklet) in patients with chronic LBP from QTF 1–3. They found that the intervention group provided clinically relevant improvements in pain relief (P<0.001 and standardized mean difference of 0.60) and function (P = 0.002 and standardized mean difference of 0.45) from the short to long-term (up to one year). However, there were no significant differences between the groups in terms of the quality-of-life and medical costs.
Aure et al.49 (rated as level B quality) evaluated the effectiveness of MT3 (consisting of mobilization and rotational manipulation in side-lying position from T10 to the pelvis) combined with specific and general exercise in comparison to exercises only in patients with chronic LBP from QTF 1–3. Both groups received 16 sessions of 45 minutes over 8 weeks. The results showed statistically significant improvements in terms of pain reduction and function in both groups. However, there was a greater improvement in all outcome measures for the intervention group leading to clinically relevant differences in the very-short to long-term on pain (at one year: P<0.05 and mean difference of 1.5) and functional improvement (at one year: P<0.05 and mean difference of 9), as well as for return to work rate (at 2 months; P<0.01 mean difference of 40%).
Cecchi et al.34 (rated as level B quality) compared one group receiving MT3 combined with UMC, to another group receiving back-school with UMC to another group receiving individual physiotherapy (passive and assisted mobilization, active exercises, massage, and proprioceptive-neuromuscular-facilitation) with UMC in patients with chronic LBP of type QTF 1–2. The results showed that MT3 led to clinically relevant decrease in pain (at 12 months: P<0.001, standardized mean of difference of 0.7 and 1.1) and a greater functional recovery (at 12 months: P<0.001, standardized mean of difference of 0.70 and 0.73) than the two control groups at long term. However, the intervention group (MT3) received significantly more treatment than the two control groups at follow-up. Pain recurrence and drug intake were also significantly reduced in the MT3 group (P<0.001).
Rasmussen et al.64 (rated as a level B quality) compared the effects of combined MT1 (in a side-lying position at the lumbar level of reduced movement) with exercises (two different extension exercises performed as often as possible during the day and at least once per hour), to the extension exercises alone in patients with chronic LBP classified as QTF 1–3. Both groups showed clinically relevant back and leg pain reduction, and no difference between the groups could be observed at the one month and one year follow-ups. Importantly, four patients in the intervention group and three in the control group reported worsening of back pain after 4 weeks, 3 months and one year.
Discussion
The purpose of this SR was to assess and update the evidence pertaining to the effectiveness of different MT approaches in isolation or when combined with exercise or UMC in the management of LBP. Thus, this SR deviates and provides clinicians and researchers with new information compared with other recent high quality SRs41,43,45 which are focused more on manipulation. A detailed summary of these updated findings, as well as the strength of their evidence and level of agreement with existing studies, are presented in Table 4.7,30,35–38,41,43,45
In comparison to recent SRs,36,41,43,45 the present results highlight a number of new issues in the management of LBP with MT:
Firstly, in comparison to previous reports of limited-evidence41,43 showing no-difference between true and sham manipulation, the results of this SR show moderate to strong evidence57–59,62,63 for the beneficial effects of MT1 in comparison to sham-MT1. These differences are demonstrated in terms of pain relief, functional improvement, and overall-health and quality of life improvements in the short-term for all stages of LBP.
Secondly, in patients with acute–subacute LBP, in contrast to the previous reports of limited evidence of no-difference for manipulation combined with other interventions,41 we determined moderate-evidence60,61 to support MT1 and MT3 combined with UMC, in comparison to UMC alone, for pain, function, overall-health and quality of life.60,61
Thirdly in patients with chronic LBP, in contrast to the previous reports of varying quality evidence (ranging from limited to strong) that manipulation has short term efficacy when combined with other interventions,43 we found moderate evidence34,49 in support of the use of MT3 combined with exercises or UMC, in comparison to exercise alone or back-school, for pain, function and return to work from short to long-term. In addition limited evidence32 supports the use of MT2 combined with exercises and UMC, in comparison to UMC alone, for pain and function from short to long-term. Finally, there is limited evidence of no-difference in efficacy for MT1 combined with extension-exercises, in comparison to extension-exercises alone for pain.64
The highest quality clinical research study is the conventional RCT. These studies have good internal validity but at the expense of external validity. An alternative for ‘real world’ application is a pragmatic RCT which has good external validity but poor internal validity.65 Pragmatic clinical trials are becoming a frequently used tool to evaluate complex interventions.66 Another possibility is to extend the conventional RCT to retain some of its key advantages (e.g. Cochrane criteria shown in Appendix 1), and use a ‘quasi-double-blind’ design to make a realistic compromise between internal and external validity. The CONSORT guidelines should also be considered to develop high quality study designs.67
One of the key issues in MT research is developing a plausible placebo or sham technique. A sham manipulation should be an appropriate placebo procedure because it mimics interaction between the intervention, the patient, the practitioner and the environment. Moreover, researchers need to conceptualize placebo not only as a comparative inert intervention, but also as a potential mechanism to partially account for treatment effects associated with MT.68
In the present SR, only five studies were placebo-controlled, four of them using sham adjustment,31,57,58,62,63 while one used a real manipulation at the incorrect spinal level to achieve an authentic placebo response.59 Further research is required to identify a plausible placebo response.
In the majority of RCTs addressing the effectiveness of MT, LBP patients are treated as a homogeneous group while recent research suggests that people with LBP in fact comprise a heterogeneous group.40,65,69 Consequently, the concept of subgrouping among people with LBP is growing in the MT literature.65 Classification of patient into sub-groups and the application of specific MT interventions for each sub-group have been shown to be more efficient.28,69–74 For example, a treatment based classification system to identify MT for people with LBP is one form of subgrouping.28 The Start-Back-Tool is another approach that aims to sub-classify according to psychosocial issues, and has been found to be more effective than a non-subgrouping approach.75,76 Moreover, the patients’ beliefs and expectations regarding treatment effects of MT interventions has also shown to be an important predictor of treatment outcome.77 Targeted MT for specific subgroups is important because of the heterogeneity of people with LBP, future clinical trials should address the ‘wash-out’ effect of applying treatments for unclassified LBP.78
In terms of quality of the MT management, MT should always be based on evidence-based-practice, which incorporates patient values (bio-psycho-social influences), clinical expertise and reasoning on part of the clinician, as well as the best available clinical research evidence.5,79–81 It could also be useful to establish a minimum level of practical skills across the range of commonly used MT techniques to manage people with LBP, and to improve clinical reasoning skills dealing with the complexity of LBP.65 Future studies should incorporate clinical expertise as a factor in treatment trials for LBP.
Limitations
The results of our SR should be interpreted in the light of some limitations. Firstly, there was heterogeneity in the RCTs evaluated in this study including the data presentation and outcome measures. Consequently, a meta-analysis enabling pooled statistics of effect was not possible. Furthermore, the strength of evidence comprising this SR is limited (particularly for the stronger level of evidence) due to the difficulty of a true double-blind study design and because of the limited number of high quality studies. Finally, only studies published in English from 2000 to 2013 were reviewed, leading to the possibility of relevant articles existing in other languages or before 2000.
Conclusions
This SR, based on low-risk of bias studies, has provided a comprehensive review of different MT approaches in patients with different stages of LBP, informing evidence-based-practice. Based on the results of this SR, a variety of manual procedures combined or not with other interventions, including exercise, may improve patient management. The summary findings of this review are both comprehensive and novel and may be used to guide clinical practice and future studies of this topic.
Recommendations for future research to investigate MT include pragmatic high quality RCTs to maximize the application of results to clinical practice and to reflect the complexity of clinical reasoning and multi-modal management of MT. Future studies should also investigate targeted MT for specific subgroups of people with LBP, and continue to address the complex issue of the best placebo procedure in MT trials.
Acknowledgments
The authors thank for their contributions: Dr Léon Plaghki as scientific adviser and Anne Klöcker for writing corrections (University of Louvain, Belgium).
Appendix 1
Search strategy in MEDLINE
In MeSH (MEDLINE), ‘Manual Therapy’ was used as a free-term. The result of the MeSH Heading was ‘Musculoskeletal-Manipulations’ and we added ‘Low-Back-Pain’ to the MEDLINE search box as follows: ‘Musculoskeletal-Manipulations’[Mesh] AND ‘Low-Back-Pain’[Mesh] AND (‘humans’[MeSH-Terms] AND (‘male’[MeSH-Terms] OR ‘female’[MeSH-Terms]) AND Randomized-Controlled-Trial[ptyp] AND English[lang] AND ‘adult’[MeSH-Terms] AND ‘2000/01/01’[PDat]: ‘2013/04/01’[PDat]).
Risk of bias assessment
Criteria list for methodological quality assessment from Cochrane Collaboration Back Review Group
A Was the method of randomization adequate? Yes/No/Don’t know
B Was the treatment allocation concealed? Yes/No/Don’t know
C Were the groups similar at baseline regarding the most important prognostic indicators? Yes/No/Don’t know
D Was the patient blinded to the intervention? Yes/No/Don’t know
E Was the care provider blinded to the intervention? Yes/No/Don’t know
F Was the outcome assessor blinded to the intervention? Yes/No/Don’t know
G Were cointerventions avoided or similar? Yes/No/Don’t know
H Was the compliance acceptable in all groups? Yes/No/Don’t know
I Was the drop-out rate described and acceptable? Yes/No/Don’t know
J Was the timing of the outcome assessment in all groups similar? Yes/No/Don’t know
K Did the analysis include an intention-to-treat analysis? Yes/No/Don’t know
Operationalization of the criteria list
A: A random (unpredictable) assignment sequence. Examples of adequate methods are computer generated random number table and use of sealed opaque envelopes. Methods of allocation using date of birth, date of admission, hospital numbers, or alternation should not be regarded as appropriate.
B: Assignment generated by an independent person not responsible for determining the eligibility of the patients. This person has no information about the persons included in the trial and has no influence on the assignment sequence or on the decision about eligibility of the patient.
C: In order to receive a ‘yes,’ groups have to be similar at baseline regarding demographic factors, duration and severity of complaints, percentage of patients with neurologic symptoms, and value of main outcome measure(s).
D: The reviewer determines if enough information about the blinding is given in order to score a ‘yes.’
E: The reviewer determines if enough information about the blinding is given in order to score a ‘yes.’
F: The reviewer determines if enough information about the blinding is given in order to score a ‘yes.’
G: Cointerventions should either be avoided in the trial design or similar between the index and control groups.
H: The reviewer determines if the compliance to the interventions is acceptable, based on the reported intensity, duration, number and frequency of sessions for both the index intervention and control intervention(s).
I: The number of participants who were included in the study but did not complete the observation period or were not included in the analysis must be described and reasons given. If the percentage of withdrawals and drop-outs does not exceed 20% for short-term follow-up and 30% for long-term follow-up and does not lead to substantial bias a ‘yes’ is scored. (NB these percentages are arbitrary, not supported by literature).
J: Timing of outcome assessment should be identical for all intervention groups and for all important outcome assessments.
K: All randomized patients are reported/analyzed in the group they were allocated to by randomization for the most important moments of effect measurement (minus missing values) irrespective of noncompliance and cointerventions.
Appendix 2
Studies that confirmed previous evidence (1) and studies that have been excluded from the SR (2)
| 1. Authors, Journals and quality score of included studies that confirmed previous evidence (Table 4) | |||
| ACUTE–SUBACUTE LBP | CHRONIC LBP | ||
| Childs et al.1 Ann Intern Med (2004) level B (9/11) | Licciardone et al.9 Spine (2003) level A (9/11) | ||
| Cleland et al.2 Spine (2009) level B (8/11) | Cherkin et al.10 Arch Intern Med (2001) level B (9/11) | ||
| Wand et al.3 Spine (2004) level B (9/11) | Ferreira et al.11 Pain (2007) level B (8/11) | ||
| Curtis et al.4 Spine (2000) level B (8/11) | Critchley et al.12 Spine (2007) level B (9/11) | ||
| Jüni et al.5 Ann Rheum Dis (2009) level B (9/11) | |||
| Hay et al.6 Lancet (2005) level B (9/11) | |||
| Hancock et al.7 Lancet (2007) level A (10/11) | |||
| Hurley et al.8 Spine (2004) level B (9/11) | |||
| 2. Authors, Journals and qualitative and/or quantitative criteria for reason of exclusion | |||
| Bogefeldt et al.13 Clin Rehabil (2008) | Outcome: only sick leave | Hertzman-Miller et al.14 Am J Public Health (2002) | Patients: Mixed LBP status. Intervention: No for categorization of MT |
| Cairns et al.15 Spine (2006) | Intervention: no for categorization of MT (6/11 Cochrane-list) | Hondras et al.16 JMPT (2009) | Patients: Mixed LBP status |
| Chiradejnant et al.17 Aust J Physiother (2003) | Patients: mixed LBP status (6/11 Cochrane-list) | Hsieh et al.18 Spine (2002) | Patients: Mixed LBP status |
| Chown et al.19 Physiother (2008) | 5/11 Cochrane-list | Hurwitz et al.20 Spine (2002) | Patients: Mixed LBP status. Intervention: No for categorization of MT |
| Eisenberg et al.21 Spine (2007) | Intervention: no for categorization of MT | Kilpikoski et al.22 Adv Physiother (2009) | Patients: Mixed LBP status |
| Ferreira et al.23 Man Ther (2009) | 4/11 Cochrane-list | Konstantinou et al.24 JMPT (2007) | Patients: Mixed LBP status (6/11 Cochrane-list) |
| Flynn et al.25 Spine (2002) | 5/11 Cochrane-list | Kool et al.26 Arch Phys Med Rehabil (2007) | Intervention: No for categorization of MT. Outcomes: no adequate outcomes |
| Geisser et al.27 Clin J Pain (2005) | 5/11 Cochrane-list | Miller et al.28 JMMT (2005) | Intervention: No for categorization of MT |
| Giles and Muller29 Spine (2003) | Patients: mixed neck and LBP | Mohseni-Bandpei et al.30 Phys Ther (2006) | 6/11 Cochrane-list |
| Goldby et al.31 Spine (2006) | Intervention: no for categorization of MT (6/11 Cochrane-list) | Nagrale et al.32 JMMT (2012) | Intervention: No for categorization of MT (neurodynamic) |
| Grunnesjo et al.33 JMPT (2004) | ‘No’ for co-intervention (steroid injections only in IG) | Niemisto et al.34 Spine (2005) | Patients: Mixed LBP status. (6/11 Cochrane-list) |
| Haas et al.35 Spine J (2004) | 6/11 Cochrane-list | Paatelma et al.36 J Rehabil Med (2008) | Patients: Mixed LBP status |
| Hagen et al.37 Spine (2003) | Intervention: no for categorization of MT | Parkin-Smith et al.38 Arch Phys Med Rehabil (2012) | ‘No’ for assessor blinded (7/11 Cochrane-list) |
| Hallegraeff et al.39 Percept Mot Skills (2009) | ‘No’ for assessor blinded (7/11 Cochrane-list) | Rasmussen-Barr et al.40 Man Ther (2003) | Patients : mixed LBP status (6/11 Cochrane-list) |
| Hancock et al.41 Eur Spine J (2008) | ‘No’ for assessor blinded (8/11 Cochrane-list) | Riipinen et al.42 J Rehabil Med (2005) | Outcomes: no adequate outcomes |
| Hemmila et al.43 JMPT (2002) | Intervention : no for categorization of MT (4/11 Cochrane-list) | Team UBT.44 BMJ (2004) | Patients: Mixed LBP status |
1. Childs JD, Fritz JM, Flynn TW, Irrgang JJ, Johnson KK, Majkowski GR, et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med. 2004;141:920–8.
2. Cleland JA, Fritz JM, Kulig K, Davenport TE, Eberhart S, Magel J, et al. Comparison of the effectiveness of three manual physical therapy techniques in a subgroup of patients with low back pain who satisfy a clinical prediction rule: a randomized clinical trial. Spine. 2009;34:2720–9.
3. Wand BM, Bird C, McAuley JH, Dore CJ, MacDowell M, De Souza LH. Early intervention for the management of acute low back pain: a single-blind randomized controlled trial of biopsychosocial education, manual therapy, and exercise. Spine. 2004;29:2350–6.
4. Curtis P, Carey TS, Evans P, Rowane MP, Mills Garrett J, Jackman A. Training primary care physicians to give limited manual therapy for low back pain: patient outcomes. Spine. 2000;25:2954–60; discussion 60–1.
5. Jüni P, Battaglia M, Nüesch E, Hämmerle G, Eser P, van Beers R, et al. A randomised controlled trial of spinal manipulative therapy in acute low back pain. Ann Rheum Dis. 2009;68:1420–7.
6. Hay EM, Mullis R, Lewis M, Vohora K, Main CJ, Watson P, et al. Comparison of physical treatments versus a brief pain-management programme for back pain in primary care: a randomised clinical trial in physiotherapy practice. Lancet. 2005;365:2024–30.
7. Hancock MJ, Maher CG, Latimer J, McLachlan AJ, Cooper CW, Day RO, et al. Assessment of diclofenac or spinal manipulative therapy, or both, in addition to recommended first-line treatment for acute low back pain: a randomised controlled trial. Lancet. 2007;370:1638–43.
8. Hurley DA, McDonough SM, Dempster M, Moore AP, Baxter GD. A randomized clinical trial of manipulative therapy and interferential therapy for acute low back pain. Spine. 2004;29:2207–16.
9. Licciardone JC, Stoll ST, Fulda KG, Russo DP, Siu J, Winn W, et al. Osteopathic manipulative treatment for chronic low back pain: a randomized controlled trial. Spine. 2003;28:1355–62.
10. Cherkin DC, Eisenberg D, Sherman KJ, Barlow W, Kaptchuk TJ, Street J, et al. Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self-care education for chronic low back pain. Arch Intern Med. 2001;161:1081–8.
11. Ferreira ML, Ferreira PH, Latimer J, Herbert RD, Hodges PW, Jennings MD, et al. Comparison of general exercise, motor control exercise and spinal manipulative therapy for chronic low back pain: A randomized trial. Pain. 2007;131:31–7.
12. Critchley DJ, Ratcliffe J, Noonan S, Jones RH, Hurley MV. Effectiveness and cost-effectiveness of three types of physiotherapy used to reduce chronic low back pain disability: a pragmatic randomized trial with economic evaluation. Spine. 2007;32:1474–81.
13. Bogefeldt J, Grunnesjo MI, Svardsudd K, Blomberg S. Sick leave reductions from a comprehensive manual therapy programme for low back pain: the Gotland Low Back Pain Study. Clin Rehabil. 2008;22:529–41.
14. Hertzman-Miller RP, Morgenstern H, Hurwitz EL, Yu F, Adams AH, Harber P, et al. Comparing the satisfaction of low back pain patients randomized to receive medical or chiropractic care: results from the UCLA low-back pain study. Am J Public Health. 2002;92:1628–33.
15. Cairns MC, Foster NE, Wright C. Randomized controlled trial of specific spinal stabilization exercises and conventional physiotherapy for recurrent low back pain. Spine. 2006;31:E670–81.
16. Hondras MA, Long CR, Cao Y, Rowell RM, Meeker WC. A randomized controlled trial comparing 2 types of spinal manipulation and minimal conservative medical care for adults 55 years and older with subacute or chronic low back pain. J Manipulative Physiol Ther. 2009;32:330–43.
17. Chiradejnant A, Maher CG, Latimer J, Stepkovitch N. Efficacy of ‘therapist-selected’ versus ‘randomly selected’ mobilisation techniques for the treatment of low back pain: a randomised controlled trial. Aust J Physiother. 2003;49:233–41.
18. Hsieh CY, Adams AH, Tobis J, Hong CZ, Danielson C, Platt K, et al. Effectiveness of four conservative treatments for subacute low back pain: a randomized clinical trial. Spine. 2002;27:1142–8.
19. Chown M, Whittamore L, Rush M, Allan S, Stott D, Archer M. A prospective study of patients with chronic back pain randomized to group exercise, physiotherapy or osteopathy. Physiother. 2008;94:21–8.
20. Hurwitz EL, Morgenstern H, Harber P, Kominski GF, Belin TR, Yu F, et al. A randomized trial of medical care with and without physical therapy and chiropractic care with and without physical modalities for patients with low back pain: 6-month follow-up outcomes from the UCLA low back pain study. Spine. 2002;27:2193–204.
21. Eisenberg DM, Post DE, Davis RB, Connelly MT, Legedza AT, Hrbek AL, et al. Addition of choice of complementary therapies to usual care for acute low back pain: a randomized controlled trial. Spine. 2007;32:151–8.
22. Kilpikoski S, Alèn M, Paatelma M, Simonen R, Heinonen A, Videman T. Outcome comparison among working adults with centralizing low back pain: secondary analysis of a randomized controlled trial with 1-year follow-up. Adv Physiother. 2009;11:210–7.
23. Ferreira ML, Ferreira PH, Latimer J, Herbert RD, Maher C, Refshauge K. Relationship between spinal stiffness and outcome in patients with chronic low back pain. Man Ther. 2009;14:61–7.
24. Konstantinou K, Foster N, Rushton A, Baxter D, Wright C, Breen A. Flexion mobilizations with movement techniques: the immediate effects on range of movement and pain in subjects with low back pain. J Manipulative Physiol Ther. 2007;30:178–85.
25. Flynn T, Fritz J, Whitman J, Wainner R, Magel J, Rendeiro D, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002;27:2835–43.
26. Kool J, Bachmann S, Oesch P, Knuesel O, Ambergen T, de Bie R, et al. Function-centered rehabilitation increases work days in patients with nonacute nonspecific low back pain: 1-year results from a randomized controlled trial. Arch Phys Med Rehabil. 2007;88:1089–94.
27. Geisser ME, Wiggert EA, Haig AJ, Colwell MO. A randomized, controlled trial of manual therapy and specific adjuvant exercise for chronic low back pain. Clin J Pain. 2005;21:463–70.
28. Miller E, Schenck R, Karnes J, Rouselle J. A comparison of a McKenzie approach to a specific spine stabilization program for chronic low back pain. J Man Manip Ther. 2005;13:103–12.
29. Giles LG, Muller R. Chronic spinal pain: a randomized clinical trial comparing medication, acupuncture, and spinal manipulation. Spine. 2003;28:1490–502; discussion 502–3.
30. Mohseni-Bandpei MA, Critchley J, Staunton T, Richardson B. A prospective randomized controlled trial of spinal manipulation and ultrasound in the treatment of chronic low back pain. Phys Ther. 2006;92:34–42.
31. Goldby LJ, Moore AP, Doust J, Trew ME. A randomized controlled trial investigating the efficiency of musculoskeletal physiotherapy on chronic low back disorder. Spine. 2006;31:1083–93.
32. Nagrale AV, Patil SP, Gandhi RA, Learman K. Effect of slump stretching versus lumbar mobilization with exercise in subjects with non-radicular low back pain: a randomized clinical trial. J Man Manip Ther. 2012;20:35–42.
33. Grunnesjo MI, Bogefeldt JP, Svardsudd KF, Blomberg SI. A randomized controlled clinical trial of stay-active care versus manual therapy in addition to stay-active care: functional variables and pain. J Manipulative physiol Ther. 2004;27:431–41.
34. Niemisto L, Rissanen P, Sarna S, Lahtinen-Suopanki T, Lindgren KA, Hurri H. Cost-effectiveness of combined manipulation, stabilizing exercises, and physician consultation compared to physician consultation alone for chronic low back pain: a prospective randomized trial with 2-year follow-up. Spine. 2005;30:1109–15.
35. Haas M, Groupp E, Kraemer DF. Dose-response for chiropractic care of chronic low back pain. Spine J. 2004;4:574–83.
36. Paatelma M, Kilpikoski S, Simonen R, Heinonen A, Alen M, Videman T. Orthopaedic manual therapy, McKenzie method or advice only for low back pain in working adults: a randomized controlled trial with one year follow-up. J Rehabil Med. 2008;40:858–63.
37. Hagen E, Grasdal A, Eriksen H. Does early intervention with a light mobilization program reduce long-term sick leave for low back pain: a 3 year follow-up study. Spine. 2003;28:309–15.
38. Parkin-Smith GF, Norman IJ, Briggs E, Angier E, Wood TG, Brantingham JW. A structured protocol of evidence-based conservative care compared with usual care for acute nonspecific low back pain: a randomized clinical trial. Arch Phys Med Rehabil. 2012;93:11–20.
39. Hallegraeff JM, de Greef M, Winters JC, Lucas C. Manipulative therapy and clinical prediction criteria in treatment of acute nonspecific low back pain. Percept Mot Skills. 2009;108:196–208.
40. Rasmussen-Barr E, Nilsson-Wikmar L, Arvidsson I. Stabilizing training compared with manual treatment in sub-acute and chronic low-back pain. Man Ther. 2003;8:233–41.
41. Hancock MJ, Maher CG, Latimer J, Herbert RD, McAuley JH. Independent evaluation of a clinical prediction rule for spinal manipulative therapy: a randomised controlled trial. Eur Spine J. 2008;17:936–43.
42. Riipinen M, Niemisto L, Lindgren KA, Hurri H. Psychosocial differences as predictors for recovery from chronic low back pain following manipulation, stabilizing exercises and physician consultation or physician consultation alone. J Rehabil Med. 2005;37:152–8.
43. Hemmila HM, Keinanen-Kiukaanniemi SM, Levoska S, Puska P. Long-term effectiveness of bone-setting, light exercise therapy, and physiotherapy for prolonged back pain: a randomized controlled trial. J Manipulative Physiol Ther. 2002;25:99–104.
44. Team UBT. United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: effectiveness of physical treatments for back pain in primary care. BMJ. 2004;329:1377.
References
- 1.Waddell G. The back pain revolution. 2nd ed. Edinburgh: Churchill Livingstone; 2005. [Google Scholar]
- 2.Balague F, Mannion AF, Pellise F, Cedraschi C. Non-specific low back pain. Lancet. 2012;379:482–91. doi: 10.1016/S0140-6736(11)60610-7. [DOI] [PubMed] [Google Scholar]
- 3.Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain. 2000;84:95–103. doi: 10.1016/S0304-3959(99)00187-6. [DOI] [PubMed] [Google Scholar]
- 4.Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8:8–20. doi: 10.1016/j.spinee.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Delitto A, George SZ, Van Dillen LR, Whitman JM, Sowa G, Shekelle P, et al. Low back pain. J Orthop Sports Phys Ther. 2012;42:A1–57. doi: 10.2519/jospt.2012.42.4.A1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hidalgo B, Gilliaux M, Poncin W, Detrembleur C. Reliability and validity of a kinematic spine model during active trunk movement in healthy subjects and patients with chronic non-specific low back pain. J Rehabil Med. 2012;44:756–63. doi: 10.2340/16501977-1015. [DOI] [PubMed] [Google Scholar]
- 7.Di Fabio RP. Efficacy of manual therapy. Phys Ther. 1992;72:853–64. doi: 10.1093/ptj/72.12.853. [DOI] [PubMed] [Google Scholar]
- 8.McCullough BJ, Johnson GR, Martin BI, Jarvik JG. Lumbar MR imaging and reporting epidemiology: do epidemiologic data in reports affect clinical management? Radiology. 2012;262:941–6. doi: 10.1148/radiol.11110618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maus TP, Aprill CN. Lumbar diskogenic pain, provocation diskography, and imaging correlates. Radiol Clin North Am. 2012;50:681–704. doi: 10.1016/j.rcl.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 10.Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15((Suppl 2)):S192–300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Delitto A, Erhard RE, Bowling RW. A treatment-based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Phys Ther. 1995;75:470–85. doi: 10.1093/ptj/75.6.470. discussion 85–9. [DOI] [PubMed] [Google Scholar]
- 12.Vanelderen P, Szadek K, Cohen SP, De Witte J, Lataster A, Patijn J, et al. 13. Sacroiliac joint pain. Pain Pract. 2010;10:470–8. doi: 10.1111/j.1533-2500.2010.00394.x. [DOI] [PubMed] [Google Scholar]
- 13.Kallewaard JW, Terheggen MA, Groen GJ, Sluijter ME, Derby R, Kapural L, et al. 15. Discogenic low back pain. Pain Pract. 2010;10:560–79. doi: 10.1111/j.1533-2500.2010.00408.x. [DOI] [PubMed] [Google Scholar]
- 14.van Kleef M, Vanelderen P, Cohen SP, Lataster A, van Zundert J, Mekhail N. 12. Pain originating from the lumbar facet joints. Pain Pract. 2010;10:459–69. doi: 10.1111/j.1533-2500.2010.00393.x. [DOI] [PubMed] [Google Scholar]
- 15.O’Sullivan P. It’s time for change with the management of non-specific chronic low back pain. Br J Sports Med. 2012;46:224–7. doi: 10.1136/bjsm.2010.081638. [DOI] [PubMed] [Google Scholar]
- 16.Riipinen M, Niemisto L, Lindgren KA, Hurri H. Psychosocial differences as predictors for recovery from chronic low back pain following manipulation, stabilizing exercises and physician consultation or physician consultation alone. J Rehabil Med. 2005;37:152–8. doi: 10.1080/16501970410022426. [DOI] [PubMed] [Google Scholar]
- 17.Verbunt JA, Smeets RJ, Wittink HM. Cause or effect? Deconditioning and chronic low back pain. Pain. 2010;149:428–30. doi: 10.1016/j.pain.2010.01.020. [DOI] [PubMed] [Google Scholar]
- 18.Tegeder I, Lotsch J. Current evidence for a modulation of low back pain by human genetic variants. J Cell Mol Med. 2009;13:1605–19. doi: 10.1111/j.1582-4934.2009.00703.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Valat JP, Goupille P, Vedere V. Low back pain: risk factors for chronicity. Rev Rhum Engl Ed. 1997;64:189–94. [PubMed] [Google Scholar]
- 20.Krismer M, van Tulder M, Low Back Pain Group of the B and Joint Health Strategies for Europe P. Strategies for prevention and management of musculoskeletal conditions. Low back pain (non-specific). Best Pract Res Clin Rheumatol. 20072177–91. [DOI] [PubMed] [Google Scholar]
- 21.Cleland JA, Fritz JM, Kulig K, Davenport TE, Eberhart S, Magel J, et al. Comparison of the effectiveness of three manual physical therapy techniques in a subgroup of patients with low back pain who satisfy a clinical prediction rule: a randomized clinical trial. Spine. 2009;34:2720–9. doi: 10.1097/BRS.0b013e3181b48809. [DOI] [PubMed] [Google Scholar]
- 22.Harvey E, Burton AK, Moffett JK, Breen A, team UBt. Spinal manipulation for low-back pain: a treatment package agreed to by the UK chiropractic, osteopathy and physiotherapy professional associations. Man Ther. 2003846–51. [DOI] [PubMed] [Google Scholar]
- 23.Farrell JP, Jensen GM. Manual therapy: a critical assessment of role in the profession of physical therapy. Phys Ther. 1992;72:843–52. doi: 10.1093/ptj/72.12.843. [DOI] [PubMed] [Google Scholar]
- 24.Zusman M. Hands on, hands off? The swings in musculoskeletal physiotherapy practice. Man Ther. 2013;18((3)):e13. doi: 10.1016/j.math.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 25.Maitland J. Spinal manipulation made simple: a manual of soft tissue techniques. Berkeley, CA: North Atlantic Books; 2000. [Google Scholar]
- 26.Fryer G, Johnson JC, Fossum C. The use of spinal and sacroiliac joint procedures within the British osteopathic profession. Part 2: Treatment. Int J Osteopath Med. 2010;13:152–9. [Google Scholar]
- 27.Cook C. Orthopedic manual therapy: an evidence-based approach. Upper Saddle River, NJ; London: Pearson/Prentice Hall; 2007. [Google Scholar]
- 28.Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther. 2007;37:290–302. doi: 10.2519/jospt.2007.2498. [DOI] [PubMed] [Google Scholar]
- 29.van Tulder M, Becker A, Bekkering T, Breen A, del Real MT, Hutchinson A, et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J. 2006;15((Suppl 2)):S169–91. doi: 10.1007/s00586-006-1071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Licciardone JC, Brimhall AK, King LN. Osteopathic manipulative treatment for low back pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskel Disord. 2005;6:43. doi: 10.1186/1471-2474-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Licciardone JC, Stoll ST, Fulda KG, Russo DP, Siu J, Winn W, et al. Osteopathic manipulative treatment for chronic low back pain: a randomized controlled trial. Spine. 2003;28:1355–62. doi: 10.1097/01.BRS.0000067110.61471.7D. [DOI] [PubMed] [Google Scholar]
- 32.Niemistö L, Lahtinen-Suopanki T, Rissanen P, Lindgren KA, Sarna S, Hurri H. A randomized trial of combined manipulation, stabilizing exercises, and physician consultation compared to physician consultation alone for chronic low back pain. Spine. 2003;28:2185–91. doi: 10.1097/01.BRS.0000085096.62603.61. [DOI] [PubMed] [Google Scholar]
- 33.Eisenberg DM, Post DE, Davis RB, Connelly MT, Legedza AT, Hrbek AL, et al. Addition of choice of complementary therapies to usual care for acute low back pain: a randomized controlled trial. Spine. 2007;32:151–8. doi: 10.1097/01.brs.0000252697.07214.65. [DOI] [PubMed] [Google Scholar]
- 34.Cecchi F, Molino-Lova R, Chiti M, Pasquini G, Paperini A, Conti AA, et al. Spinal manipulation compared with back school and with individually delivered physiotherapy for the treatment of chronic low back pain: a randomized trial with one-year follow-up. Clin Rehabil. 2010;24:26–36. doi: 10.1177/0269215509342328. [DOI] [PubMed] [Google Scholar]
- 35.Assendelft WJ, Morton SC, Yu EI, Suttorp MJ, Shekelle PG. Spinal manipulative therapy for low back pain. A meta-analysis of effectiveness relative to other therapies. Ann Intern Med. 2003;138:871–81. doi: 10.7326/0003-4819-138-11-200306030-00008. [DOI] [PubMed] [Google Scholar]
- 36.Bokarius AV, Bokarius V. Evidence-based review of manual therapy efficacy in treatment of chronic musculoskeletal pain. Pain Pract. 2010;10:451–8. doi: 10.1111/j.1533-2500.2010.00377.x. [DOI] [PubMed] [Google Scholar]
- 37.Bronfort G, Haas M, Evans RL, Bouter LM. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J. 2004;4:335–56. doi: 10.1016/j.spinee.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 38.Rajadurai V, Murugan K. Spinal manipulative therapy for low back pain: a systematic review. Phys Ther. 2009;14:260–70. [Google Scholar]
- 39.Ernst E, Canter PH. A systematic review of systematic reviews of spinal manipulation. J R Soc Med. 2006;99:192–6. doi: 10.1258/jrsm.99.4.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Koes BW, Assendelft WJ, van der Heijden GJ, Bouter LM. Spinal manipulation for low back pain. An updated systematic review of randomized clinical trials. Spine. 1996;21:2860–71. doi: 10.1097/00007632-199612150-00013. discussion 72–3. [DOI] [PubMed] [Google Scholar]
- 41.Rubinstein SM, Terwee CB, Assendelft WJ, de Boer MR, van Tulder MW. Spinal manipulative therapy for acute low-back pain. Cochrane Database Syst Rev. 2012;9:CD008880. doi: 10.1002/14651858.CD008880.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rubinstein SM, Terwee CB, Assendelft WJ, de Boer MR, van Tulder MW. Spinal manipulative therapy for acute low back pain: an update of the cochrane review. Spine. 2013;38:E158–77. doi: 10.1097/BRS.0b013e31827dd89d. [DOI] [PubMed] [Google Scholar]
- 43.Rubinstein SM, van Middelkoop M, Assendelft WJ, de Boer MR, van Tulder MW. Spinal manipulative therapy for chronic low-back pain. Cochrane Database Syst Rev. 2011;((2)):CD008112. doi: 10.1002/14651858.CD008112.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walker BF, French SD, Grant W, Green S. A Cochrane review of combined chiropractic interventions for low-back pain. Spine. 2011;36:230–42. doi: 10.1097/BRS.0b013e318202ac73. [DOI] [PubMed] [Google Scholar]
- 45.Standaert CJ, Friedly J, Erwin MW, Lee MJ, Rechtine G, Henrikson NB, et al. Comparative effectiveness of exercise, acupuncture, and spinal manipulation for low back pain. Spine. 2011;36:S120–30. doi: 10.1097/BRS.0b013e31822ef878. [DOI] [PubMed] [Google Scholar]
- 46.van Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group for Spinal Disorders. Spine. 1997;22:2323–30. doi: 10.1097/00007632-199710150-00001. [DOI] [PubMed] [Google Scholar]
- 47.van Tulder M, Furlan A, Bombardier C, Bouter L Editorial Board of the Cochrane Collaboration Back Review G. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine. 2003;28:1290–9. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 48.Dionne CE, Dunn KM, Croft PR, Nachemson AL, Buchbinder R, Walker BF, et al. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. Spine. 2008;33:95–103. doi: 10.1097/BRS.0b013e31815e7f94. [DOI] [PubMed] [Google Scholar]
- 49.Aure OF, Nilsen JH, Vasseljen O. Manual therapy and exercise therapy in patients with chronic low back pain: a randomized, controlled trial with 1-year follow-up. Spine. 2003;28:525–31. doi: 10.1097/01.BRS.0000049921.04200.A6. discussion 31–2. [DOI] [PubMed] [Google Scholar]
- 50.Niemisto L, Sarna S, Lahtinen-Suopanki T, Lindgren KA, Hurri H. Predictive factors for 1-year outcome of chronic low back pain following manipulation, stabilizing exercises, and physician consultation or physician consultation alone. J Rehabil Med. 2004;36:104–9. doi: 10.1080/16501970310019151. [DOI] [PubMed] [Google Scholar]
- 51.Furlan AD, Pennick V, Bombardier C, van Tulder M, Editorial Board CBRG. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine. 2009;34:1929–41. doi: 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 52.Loisel P, Vachon B, Lemaire J, Durand MJ, Poitras S, Stock S, et al. Discriminative and predictive validity assessment of the quebec task force classification. Spine. 2002;27:851–7. doi: 10.1097/00007632-200204150-00013. [DOI] [PubMed] [Google Scholar]
- 53.Bronfort G. Spinal manipulation: current state of research and its indications. Neurol Clin. 1999;17:91–111. doi: 10.1016/s0733-8619(05)70116-x. [DOI] [PubMed] [Google Scholar]
- 54.Hengeveld E, Banks K, Maitland GD. Oxford: Elsevier Butterworth-Heinemann; 2005. In: Hengeveld E, Banks K, (eds.) Maitland’s vertebral manipulation. 7th ed. [Google Scholar]
- 55.Kent P, Mjosund HL, Petersen DH. Does targeting manual therapy and/or exercise improve patient outcomes in nonspecific low back pain? A systematic review. BMC Med. 2010;8:22. doi: 10.1186/1741-7015-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hegedus EJ, Goode A, Butler RJ, Slaven E. The neurophysiological effects of a single session of spinal joint mobilization: does the effect last? J Man Manip Ther. 2011;19:143–51. doi: 10.1179/2042618611Y.0000000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Santilli V, Beghi E, Finucci S. Chiropractic manipulation in the treatment of acute back pain and sciatica with disc protrusion: a randomized double-blind clinical trial of active and simulated spinal manipulations. Spine J. 2006;6:131–7. doi: 10.1016/j.spinee.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 58.Hoiriis KT, Pfleger B, McDuffie FC, Cotsonis G, Elsangak O, Hinson R, et al. A randomized clinical trial comparing chiropractic adjustments to muscle relaxants for subacute low back pain. J Manipulative physiol Ther. 2004;27:388–98. doi: 10.1016/j.jmpt.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 59.von Heymann WJ, Schloemer P, Timm J, Muehlbauer B. Spinal high-velocity low amplitude manipulation in acute nonspecific low back pain: a double-blinded randomized controlled trial in comparison with diclofenac and placebo. Spine. 2013;38:540–8. doi: 10.1097/BRS.0b013e318275d09c. [DOI] [PubMed] [Google Scholar]
- 60.Bishop PB, Quon JA, Fisher CG, Dvorak MF. The Chiropractic Hospital-based Interventions Research Outcomes (CHIRO) study: a randomized controlled trial on the effectiveness of clinical practice guidelines in the medical and chiropractic management of patients with acute mechanical low back pain. Spine J. 2010;10:1055–64. doi: 10.1016/j.spinee.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 61.Cruser DA, Maurer D, Hensel K, Brown SK, White K, Stoll ST. A randomized, controlled trial of osteopathic manipulative treatment for acute low back pain in active duty military personnel. J Man Manip Ther. 2012;20:5–15. doi: 10.1179/2042618611Y.0000000016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ghroubi S, Elleuch H, Baklouti S, Elleuch MH. Chronic low back pain and vertebral manipulation. Ann Readapt Med Phys. 2007;50:570–6. doi: 10.1016/j.annrmp.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 63.Senna MK, Machaly SA. Does maintained spinal manipulation therapy for chronic nonspecific low back pain result in better long-term outcome? Spine. 2011;36:1427–37. doi: 10.1097/BRS.0b013e3181f5dfe0. [DOI] [PubMed] [Google Scholar]
- 64.Rasmussen J, Laetgaard J, Lindecrona AL, Qvistgaard E, Bliddal H. Manipulation does not add to the effect of extension exercises in chronic low-back pain (LBP). A randomized, controlled, double blind study. Joint Bone Spine. 2008;75:708–13. doi: 10.1016/j.jbspin.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 65.Ford JJ, Hahne AJ. Complexity in the physiotherapy management of low back disorders: Clinical and research implications. Man Ther. 2013 Mar 1. pii: S1356-689X(13)00029-5. [Google Scholar]
- 66.Hotopf M. The pragmatic randomized controlled trial. Adv Psychiatr Treat. 2002;8:326–33. [Google Scholar]
- 67.Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Int J Surg. 2012;10:28–55. doi: 10.1016/j.ijsu.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 68.Bialosky JE, Bishop MD, George SZ, Robinson ME. Placebo response to manual therapy: something out of nothing? J Man Manip Ther. 2011;19:11–9. doi: 10.1179/2042618610Y.0000000001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Leboeuf-Yde C, Lauritsen JM, Lauritzen T. Why has the search for causes of low back pain largely been nonconclusive? Spine. 1997;22:877–81. doi: 10.1097/00007632-199704150-00010. [DOI] [PubMed] [Google Scholar]
- 70.Fersum KV, Dankaerts W, O’Sullivan PB, Maes J, Skouen JS, Bjordal JM, et al. Integration of subclassification strategies in randomised controlled clinical trials evaluating manual therapy treatment and exercise therapy for non-specific chronic low back pain: a systematic review. Br J Sports Med. 2010;44:1054–62. doi: 10.1136/bjsm.2009.063289. [DOI] [PubMed] [Google Scholar]
- 71.Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE. Identifying subgroups of patients with acute/subacute ‘nonspecific’ low back pain: results of a randomized clinical trial. Spine. 2006;31:623–31. doi: 10.1097/01.brs.0000202807.72292.a8. [DOI] [PubMed] [Google Scholar]
- 72.O’Sullivan P. Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther. 2005;10:242–55. doi: 10.1016/j.math.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 73.Childs JD, Fritz JM, Piva SR, Erhard RE. Clinical decision making in the identification of patients likely to benefit from spinal manipulation: a traditional versus an evidence-based approach. J Orthop Sports Phys Ther. 2003;33:259–72. doi: 10.2519/jospt.2003.33.5.259. [DOI] [PubMed] [Google Scholar]
- 74.Vibe Fersum K, O’Sullivan P, Skouen JS, Smith A, Kvale A. Efficacy of classification-based cognitive functional therapy in patients with non-specific chronic low back pain: A randomized controlled trial. Eur J Pain. 2013;17((6)):916–28. doi: 10.1002/j.1532-2149.2012.00252.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hill JC, Dunn KM, Main CJ, Hay EM. Subgrouping low back pain: a comparison of the STarT Back Tool with the Orebro Musculoskeletal Pain Screening Questionnaire. Eur J Pain. 2010;14:83–9. doi: 10.1016/j.ejpain.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hill JC, Whitehurst DG, Lewis M, Bryan S, Dunn KM, Foster NE, et al. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet. 2011;378:1560–71. doi: 10.1016/S0140-6736(11)60937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bishop MD, Bialosky JE, Cleland JA. Patient expectations of benefit from common interventions for low back pain and effects on outcome: secondary analysis of a clinical trial of manual therapy interventions. J Man Manip Ther. 2011;19:20–5. doi: 10.1179/106698110X12804993426929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dankaerts W, O’Sullivan P. The validity of O’Sullivan’s classification system (CS) for a sub-group of NS-CLBP with motor control impairment (MCI): overview of a series of studies and review of the literature. Man Ther. 2011;16:9–14. doi: 10.1016/j.math.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 79.Moseley AM, Herbert RD, Sherrington C, Maher CG. Evidence for physiotherapy practice: a survey of the Physiotherapy Evidence Database (PEDro). Aust J Physiother. 2002;48:43–9. doi: 10.1016/s0004-9514(14)60281-6. [DOI] [PubMed] [Google Scholar]
- 80.Danneels L, Beernaert A, De Corte K, Descheemaeker F, Vanthillo B, van Tiggelen D, et al. A didactical approach for musculoskeletal physiotherapy: The planetary model. J Musculoskeletal Pain. 2011;19:218–24. [Google Scholar]
- 81.Sackett DL. Evidence-based medicine and treatment choices. Lancet. 1997;349:570. doi: 10.1016/S0140-6736(97)80122-5. author reply 2–3. [DOI] [PubMed] [Google Scholar]