Abstract
BACKGROUND
The prevention and control of hypertension is an essential component for reducing the burden of cardiovascular diseases. Here we describe the prevalence of hypertension in diverse Hispanic/Latino background groups and describe the proportion who are aware of their diagnosis, receiving treatment, and having their hypertension under control.
METHODS
The Hispanic Community Health Study/Study of Latinos is a longitudinal cohort study of 16,415 Hispanics/Latinos, aged 18–74 years from 4 US communities (Bronx, NY; Chicago, IL; Miami, FL; and San Diego, CA). At baseline (2008–2011) the study collected extensive measurements and completed questionnaires related to research on cardiovascular diseases. Hypertension was defined as measured blood pressure ≥140/90mm Hg or use of antihypertensive medication.
RESULTS
The total age-adjusted prevalence of hypertension in this study was 25.5% as compared with 27.4% in non-Hispanic whites in the National Health and Nutrition Examination Survey. Prevalence of hypertension increased with increasing age groups and was highest in Cuban, Puerto Rican, and Dominican background groups. The percent with hypertension who were aware, being treated with medication, or had their hypertension controlled was lower compared with US non-Hispanic whites with hypertension and it was lowest in those without health insurance.
CONCLUSIONS
These findings indicate a significant deficit in treatment and control of hypertension among Hispanics/Latinos residing in the United States, particularly those without health insurance. Given the relative ease of identification of hypertension and the availability of low-cost medications, enabling better access to diagnostic and treatment services should reduce the burden of hypertension in Hispanic populations.
Keywords: blood pressure, epidemiology, Hispanics, hypertension, Latinos, medically uninsured, socioeconomic status.
Hypertension has long been identified as a primary contributor to coronary heart disease, stroke, and heart failure.1 While the onset of hypertension can be delayed or even prevented, its treatment is successful in many with inexpensive medications.1,2 Even with this success, the prevalence of hypertension continues to be at an undesirable level, and its control in the United States is far below what is possible.3 The immigration and growth of Hispanic/Latino populations has increased the need to identify and address their specific health needs. Here, we focus on the prevalence of hypertension and its awareness, treatment, and control in a large and diverse study of Hispanics/Latinos.
The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) was designed and implemented to identify the prevalence of cardiovascular and other health conditions and diseases in this heterogeneous population. The overall goal is to determine whether the prevalence of select chronic diseases is similar or different among the various Hispanic/Latino groups and as compared with other US population groups and to gain insights into risk and protective factors that not only would benefit the Hispanic/Latino population but the US population as a whole. This study of approximately 16,000 men and women, aged 18–74 years, also investigated dental, hearing, neurocognitive, kidney, and liver conditions and diseases.
The analysis presented here is based on blood pressure measurements from the participants’ initial clinical examination and data derived from questionnaires on their personal or family Hispanic/Latino background, education, income, and health insurance. Our goal was to describe the prevalence of hypertension and the percent of those with hypertension who are aware of their condition, are being treated with medications, and have adequately controlled blood pressure. We also examined factors associated with these statistics to quantify their association with levels of education, income, and health insurance. The first results from the HCHS/SOL described the variation in 5 critical cardiovascular risk factors by background group.4 The analysis presented here examines the hypertension results in more detail, with emphasis on factors associated with treating and controlling this contributor to cardiovascular disease.
METHODS
The design and content of the HCHS/SOL is described elsewhere.5,6 Briefly, between 2008 and 2011 the study recruited 16,415 self-identified Hispanic/Latino persons, aged 18–74 years, from 4 communities in the United States (Bronx, NY; Chicago, IL; Miami, FL; San Diego, CA). These sites were selected based on a competitive response to a “Request for Proposals” from the National Heart, Lung, and Blood Institute. While inclusive of the major Hispanic/Latino groups, the study was not designed to be a national sample of Hispanics/Latinos in the United States. All participants provided an informed consent, and approval was received from the institutional review boards of all institutions participating in this study. Since Hispanics/Latinos in the United States can trace their roots to different countries or ancestral origins, the study aimed to recruit persons who self-identified their backgrounds as Cuban, Central American, South American, Dominican, Puerto Rican, or Mexican. The Hispanic/Latino groups in the United States reside with higher concentrations in certain areas of the country. Consequently, each site in this study has a higher number of 1 or 2 Hispanic/Latino background groups and a lower number of the others. Self-reported race, which was collected in this study, was not reported in these analyses because more than one-third of participants did not respond to this question.
In the defined communities, households were sampled using a probability design to improve efficiency and obtain a representation of the broad spectrum of economic diversity. Specifically, to ensure sufficient representation of older persons, the 45–74 year age group was oversampled because the resident population has fewer older than younger persons. Of individuals who were screened, selected, and met eligibility criteria, 42% were enrolled. Unwillingness to participate could occur at the initial household or person recruitment, as well as in those who agreed and were scheduled for the exam visit but did not show after many phone calls.
The distribution of study demographic characteristics indicated that the resultant sample was diverse in socioeconomic status and backgrounds. Analyses require the use of sampling weights adjusted for nonresponse and result in a population with an age, sex, and Hispanic background that matches the communities. The communities sampled for the HCHS/SOL are in urban areas, and in the United States two-thirds of Hispanics live in urban areas of 1 million persons or more and 87% in areas of 250,000 persons or more.7–9 Finally, as indicated by data presented later in this article, the comparison of HCHS/SOL with the National Health and Nutrition Examination Survey (NHANES) shows very comparable results, suggesting that there is not significant bias.
Comprehensive research examinations were conducted at a central research site in each community by trained and certified technicians and interviewers. Blood pressure was measured on the right arm using an OMRON HEM-907 XL (Omron Healthcare, Inc., Lake Forest, IL) automatic sphygmomanometer, with the participant in the seated position and the arm resting. Cuff sizes were determined by measurement of the upper arm circumference. Four cuff sizes were available. Three blood pressures measurements were obtained 1 minute apart following an initial 5-minute rest period. The average of these 3 blood pressure values was used in this analysis. If there were fewer than 3 measurements, all available measurements were averaged. Ninety-nine percent of participants had all 3 measures.
Comparisons were made with results from the 2009–2010 NHANES in which similar protocols were used for measurement of blood pressure, except that an automated device was used in the HCHS/SOL study and a standard mercury device was used by NHANES. Some studies have shown that automatic devices such as those used in HCHS/SOL may show slightly lower blood pressures than mercury sphygmomanometers.10 Here, our analyses included those 16,219 individuals who had no-missing data on average systolic and diastolic blood pressure and self-reported use of blood pressure medication.
Questionnaire data
Participants were asked the following questions:
For awareness of hypertension: Has a doctor ever said that you have high blood pressure or hypertension (no, yes)?
For hypertension treatment: Were any of the medications that you took during the last 4 weeks for high blood pressure or hypertension (no, yes, unknown)?
For Hispanic/Latino background: Which of the following best describes your Hispanic/Latino heritage (Dominican or Dominican descent, Central American or Central American descent, Cuban or Cuban descent, Mexican or Mexican descent, Puerto Rican or Puerto Rican descent, South American or South American descent, more than one heritage, other)?
For education: What was the highest grade/level of education achieved (elementary/primary school (includes grades 1–5), middle school/junior high (includes grades 6–8), high school/preparatory school, trade school/vocational school, university/college, other)? If exact level is not listed, mark the closest equivalent.
For income: Counting the income of all the members of your household, was your household income for the year … (select from 10 categories from less than $10,000 to more than $100,000)?
For health insurance: Do you have health insurance or other healthcare coverage (no, yes)?
Variable definitions
Hypertension was defined as average measured blood pressure ≥140mm Hg systolic or 90mm Hg diastolic or self-reported use of medications for hypertension in the last 4 weeks.
Participants were defined as aware of hypertension if classified as having hypertension and reported being informed by medical provider that they had hypertension. Participants were defined as treated if classified as having hypertension and reported that they were taking medications for hypertension. Participants were defined as controlled if classified as having hypertension and the measured blood pressure was <140/90mm Hg.
Statistical methods
HCHS/SOL participants were recruited through a multistage probability sampling design.6 From a sample of households, members were screened, sampled, and requested to enroll in the study. Because some groups were sampled at a higher or lower rate than others (e.g., older and younger persons), sampling weights were needed in our analysis to make the estimates applicable to the population from which the HCHS/SOL sample was drawn. All analyses used SAS, version 9.2.1 (SAS Institute, Cary, NC), and SUDAAN version 10.0 (RTI International, Research Triangle Park, NC).
To specifically describe the HCHS/SOL cohort, unweighted frequencies of demographic variables were calculated. All other analyses were weighted by the sampling weights. These weighted estimates were for the target population, which consisted of all noninstitutionalized Hispanic/Latino adults aged 18–74 years and residing in the defined geographical areas (census block groups) across the 4 participating field centers. All unadjusted prevalence percentages were externally standardized to the US 2000 population age distribution in order to make these estimates comparable to those for NHANES 2009–2010 participants.11 Age- and gender-adjusted hypertension prevalence was calculated using a survey linear regression model. Homogeneity of the adjusted prevalence was tested using an F-statistic.
The percents aware, treated, and controlled were calculated for the target population using the weighted number of hypertensive participants as the denominator. The estimates were also externally standardized to the hypertensive population in NHANES when comparing to the NHANES results.12 Homogeneity of unadjusted awareness, treatment, and control rates was tested using an F-statistic.
RESULTS
Mexicans were the largest Hispanic/Latino group represented in this study (n = 6,422), but there are more than 2,000 in each of Cuban and Puerto Rican backgrounds and more than 1,000 in each of Central American, South American, and Dominican backgrounds (Table 1). A little more than a third of participants had less than a high school education, almost one-half had household incomes of ≤$20,000, and more than half of those aged <65 years had no health insurance (Table 1).
Table 1.
Characteristics of the Hispanic Community Health Study/Study of Latinos participants
| Men | Women | |||
|---|---|---|---|---|
| N | % | N | % | |
| Age group (years) | ||||
| 18–29 | 1,243 | 19 | 1,420 | 15 |
| 30–39 | 997 | 15 | 1,367 | 14 |
| 40–49 | 1,618 | 25 | 2,542 | 26 |
| 50–59 | 1,586 | 24 | 2,700 | 28 |
| 60–69 | 875 | 13 | 1,375 | 14 |
| 70–74 | 184 | 3 | 312 | 3 |
| Total | 6,503 | 100 | 9,716 | 100 |
| Hispanic background | ||||
| Central American | 675 | 10 | 1,034 | 11 |
| Cuban | 1,094 | 17 | 1,239 | 13 |
| Dominican | 505 | 8 | 947 | 10 |
| Mexican | 2,433 | 38 | 3,989 | 41 |
| Puerto Rican | 1,115 | 17 | 1,568 | 16 |
| South American | 434 | 7 | 628 | 6 |
| Mixed or other | 225 | 3 | 273 | 3 |
| Total | 6,481 | 100 | 9,678 | 100 |
| Education | ||||
| <High school completion | 2,386 | 37 | 3,660 | 39 |
| High school or more | 4,004 | 63 | 5,817 | 61 |
| Total | 6,390 | 100 | 9,477 | 100 |
| Income | ||||
| ≤$10,000 | 733 | 12 | 1,565 | 18 |
| $10,001–20,000 | 1,815 | 30 | 3,001 | 34 |
| $20,001–40,000 | 2,175 | 36 | 2,846 | 33 |
| $40,001–75,000 | 984 | 16 | 1,019 | 12 |
| >$75,000 | 360 | 6 | 283 | 3 |
| Total | 6,067 | 100 | 8,714 | 100 |
| Health insurance | ||||
| Aged <65 years | ||||
| No | 3,268 | 55 | 4,393 | 50 |
| Yes | 2,641 | 45 | 4,361 | 50 |
| Total | 5,909 | 100 | 8,754 | 100 |
| Aged 65+ years | ||||
| No | 53 | 11 | 145 | 18 |
| Yes | 427 | 89 | 652 | 82 |
| Total | 480 | 100 | 797 | 100 |
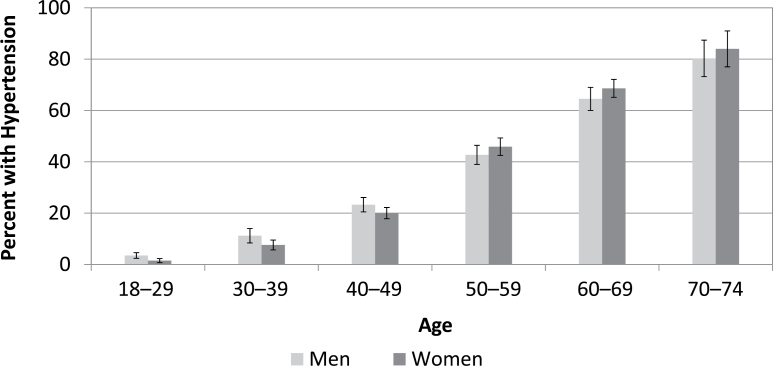
The overall age-adjusted prevalence of hypertension was 26.1% for men and 25.3% for women. Figure 1 illustrates the increase in hypertension prevalence across increasing age groups for both men and women. Though the confidence intervals overlap, in those aged <50 years, men had higher prevalence of hypertension than women, and in those aged >50 years, women had a higher prevalence than men.
Figure 1.
Prevalence of hypertension by age and sex.
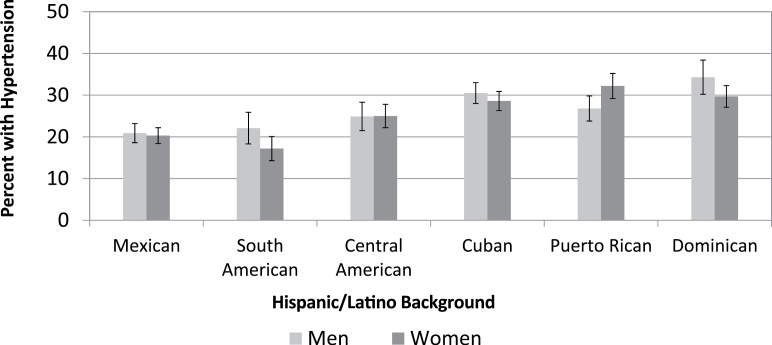
As shown in Figure 2, prevalence of hypertension varied among Hispanic groups, with the lowest in South American women (17.2%) and the highest in Dominican men (34.3%). Using a full model adjusting for age, sex, and site as main effects, Mexican participants had statistically significantly lower prevalence than each of the other background groups (P values <0.01) except South Americans. Since differences were observed among sites as well as by Hispanic/Latino background, model-based comparisons of site differences within Hispanic groups are shown in Table 2. Within background group, there were site differences (shown by the P values), with the Chicago site showing lower hypertension prevalence for several of the Hispanic/Latino background groups.
Figure 2.
Age-standardized prevalence of hypertension according to Hispanic/Latino background and sex.
Table 2.
Age-adjusted prevalence of hypertension within field site
| Background/site | Percent prevalence | 95% confidence interval | Site comparison | P value |
|---|---|---|---|---|
| Central American | ||||
| 1. Bronx | 26.6 | (21.3, 31.9) | 1 vs. 2 | 0.007 |
| 2. Chicago | 17.7 | (14.0, 21.4) | 2 vs. 3 | 0.004 |
| 3. Miami | 24.6 | (21.8, 27.5) | 1 vs. 3 | 0.524 |
| South American | ||||
| 1. Bronx | 18.4 | (13.3, 23.6) | 1 vs. 2 | 0.036 |
| 2. Chicago | 11.9 | (8.6, 15.1) | 2 vs. 3 | 0.004 |
| 3. Miami | 19.6 | (15.5, 23.8) | 1 vs. 3 | 0.713 |
| Mexican | ||||
| 1. Bronx | 13.3 | (9.9, 16.7) | 1 vs. 2 | 0.009 |
| 2. Chicago | 18.1 | (16.6, 19.5) | 2 vs. 4 | 0.007 |
| 4. San Diego | 21.2 | (19.4, 23.1) | 1 vs. 4 | <0.001 |
| Puerto Rican | ||||
| 1. Bronx | 28.6 | (25.6, 31.5) | 1 vs. 2 | 0.882 |
| 2. Chicago | 28.9 | (25.8, 32.1) | ||
| Dominican | ||||
| 1. Bronx | 29.5 | (27.1, 31.8) | ||
| Cuban | ||||
| 3. Miami | 28.9 | (27.0, 30.7) | ||
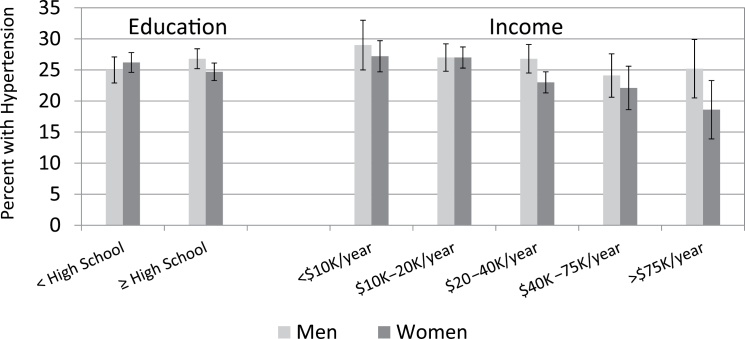
The prevalence of hypertension was compared across education and income levels (Figure 3). The percent with hypertension did not differ by either education or income levels as the confidence intervals overlapped.
Figure 3.
Age-standardized prevalence of hypertension by education and income.
Table 3 shows the proportion of hypertensive participants who were aware of having hypertension (A), under treatment (T), and had their hypertension under control (C) after model-based adjustment to the target population. For example, among men with hypertension aged 18–29 years, 48% were aware they had hypertension, 19% were under treatment with medications, and 17% were controlled with a blood pressure <140/90mm Hg. Participants aged <40 years were least likely to be both aware of and treated for their hypertension. The percent aware and treated increased steeply with age. Among men, control of hypertension was the lowest for those aged <40 years, while in women it was lowest in those aged ≥70 years. Differences in A/T/C by background group were seen in men but not in women. Control was as low as 12% in Central American men. There were no differences in A/T/C by education or income. However, higher proportions of hypertensive participants with health insurance reported being aware of their diagnosis, receiving treatment, and having their blood pressure levels adequately controlled compared with hypertensive individuals with no health insurance. The percent controlled in those who were treated can be calculated by dividing the percent controlled by the percent treated in Table 3. For example, in men aged 18–29 years, the percent controlled among those treated would be 17/19, or 89%. In some groups, the percent controlled in those treated is as low as 50%.
Table 3.
Percent of hypertensive participants who are aware, treated, and controlled
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Aware | Treated | Controlled | Aware | Treated | Controlled | |
| Age group (years) | ||||||
| 18–29 | 48 | 19 | 17 | 52 | 42 | 37 |
| 30–39 | 58 | 38 | 19 | 72 | 47 | 39 |
| 40–49 | 64 | 48 | 30 | 76 | 63 | 47 |
| 50–59 | 71 | 56 | 37 | 82 | 72 | 47 |
| 60–69 | 76 | 70 | 38 | 77 | 71 | 40 |
| 70–74 | 74 | 66 | 35 | 79 | 71 | 30 |
| Statistical testa | * | * | * | * | * | |
| Origin | ||||||
| Central American | 57 | 39 | 12 | 75 | 66 | 32 |
| Cuban | 78 | 65 | 40 | 79 | 68 | 38 |
| Dominican | 67 | 54 | 27 | 79 | 69 | 42 |
| Mexican | 62 | 49 | 31 | 77 | 67 | 45 |
| Puerto Rican | 71 | 58 | 35 | 78 | 69 | 46 |
| South American | 62 | 46 | 25 | 72 | 64 | 41 |
| Mixed/other | 57 | 49 | 19 | 86 | 79 | 57 |
| Statistical testa | * | * | * | |||
| Education | ||||||
| Less than high school | 65 | 53 | 32 | 76 | 68 | 38 |
| High school or more | 72 | 57 | 34 | 79 | 68 | 45 |
| Statistical testa | ||||||
| Income | ||||||
| ≤$10,000 | 71 | 56 | 34 | 79 | 71 | 44 |
| $10,001–20,000 | 74 | 59 | 33 | 77 | 66 | 40 |
| $20,001–40,000 | 65 | 51 | 30 | 80 | 72 | 48 |
| $40,001–75,000 | 63 | 51 | 35 | 83 | 66 | 42 |
| >$75,000 | 70 | 67 | 48 | 86 | 74 | 54 |
| Statistical testa | ||||||
| Health insurance | ||||||
| Aged <65 years | ||||||
| No | 59 | 39 | 22 | 74 | 61 | 39 |
| Yes | 73 | 62 | 39 | 80 | 70 | 50 |
| Aged 65+ years | ||||||
| No | 59 | 53 | 33 | 58 | 50 | 23 |
| Yes | 81 | 75 | 41 | 84 | 78 | 38 |
| Statistical testa | * | * | * | * | * | * |
a Test for homogeneity of percentages (* P < .01 indicating percentages differ).
The prevalence of hypertension and rates of awareness, treatment, and control in HCHS/SOL were compared with identical definitions in Hispanic and non-Hispanic whites in NHANES 2009–2010 (Table 4).13 To compare with published national estimates, the prevalence of hypertension in HCHS/SOL was age-standardized to the US 2000 age distribution and the percent of awareness, treatment, and control was age-standardized to the hypertensive NHANES population. The hypertension prevalence in HCHS/SOL (25.5) was very similar to that found in NHANES for Hispanic participants (26.1) and slightly lower than for non-Hispanic white participants (27.4). However, in HCHS/SOL, the percent aware, treated, and controlled was lower than in NHANES Hispanic and non-Hispanic white participants. Of particular concern was the percent controlled in HCHS/SOL (37.5) and NHANES Hispanics (40.7) as compared with non-Hispanic whites (56.3).
Table 4.
Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos and the National Health and Nutrition Examination Survey, men and women combined
| HCHS/SOL all Hispanics | NHANES all Hispanics | NHANES non-Hispanic Whites | ||||
|---|---|---|---|---|---|---|
| % | CI | % | CI | % | CI | |
| Hypertension | ||||||
| Prevalence | 25.5 | 24.6–26.4 | 26.1 | 24.2–28.0 | 27.4 | 24.8–30.0 |
| Aware | 74.1 | 72.1–76.1 | 77.7 | 73.5–81.9 | 81.4 | 77.1–85.7 |
| Treated | 63.4 | 61.3–65.5 | 69.6 | 65.3–73.9 | 76.6 | 71.9–81.3 |
| Controlled | 37.5 | 35.2–39.8 | 40.7 | 37.2–44.2 | 56.3 | 52.0–60.6 |
HCHS/SOL conducted in 2007–2011. NHANES conducted in 2009–2010. Prevalence is age-adjusted to the 2000 year standard. Awareness, treatment, and control adjusted to the age-distribution of hypertensive persons.
Abbreviations: CI, 95% confidence interval; HCHS/SOL, Hispanic Community Health Study/Study of Latinos; NHANES, National Health and Nutrition Examination Survey.
DISCUSSION
These results have important implications for cardiovascular health in Hispanics/Latinos living in the United States. Since hypertension is a major risk factor for cardiovascular disease, a first goal must be primary prevention and, for those with hypertension, the maximum use of effective control measures. This study showed significant differences in hypertension prevalence among Hispanic/Latino groups, as well as significant differences within these groups by geographic location. Educational attainment and household income were not associated with hypertension prevalence. The proportion of hypertensive individuals who were aware, treated, and controlled did differ by health insurance status.
Of critical concern is the overall low rate of awareness, treatment, and control among Hispanics/Latinos, particularly in younger men. In men aged <40 years with hypertension, slightly more than half were aware of their diagnosis and only 20% had their blood pressure levels under control. Among men of all ages, those with health insurance had higher rates of awareness, treatment, and control. In both men and women, blood pressure control is far from optimal even in those who have health insurance.
The existing literature on the hypertension prevalence among US Hispanics/Latinos is heavily concentrated on those of Mexican background, though there have been some smaller studies in other Hispanic/Latino background groups. A recent report compared hypertension prevalence among those of Mexican background in the Hispanic Health and Nutrition Survey (HHANES) conducted in 1982–1984 with those of Mexican background in the NHANES conducted in 1999–2004.14 Within each survey, US-born individuals of Mexican background had higher hypertension prevalence than those who were first-generation immigrants (i.e., born in Mexico). Comparing across surveys, first-generation immigrant NHANES participants of Mexican background had similar hypertension prevalence as first-generation immigrant HHANES participants of Mexican background. The authors concluded that longer residence in the United States adversely influences blood pressure, but that new immigrants in the 1980s were similar with respect to hypertension to new immigrants in the early 2000s. The Multi-Ethnic Study of Atherosclerosis (MESA) included US Hispanics aged 45–84 years of various ancestries.15 Among Hispanic MESA participants, the age-adjusted hypertension prevalence was 37.6% in Mexicans, 43.3% in Puerto Ricans, 52.9% in Dominicans, and 42.1 % in those of other Hispanic/Latino ancestries. These percentages were higher than those observed in the HCHS/SOL, likely because of the older ages of MESA participants, but the relative relationships among groups were similar. Hypertension prevalence was also evaluated in the 1993–1994 and 2004–2005 cohorts of Mexican background aged ≥75 years who participated in the Hispanic Established Population for the Epidemiology Study of the Elderly.16 This study showed a secular increase in the hypertension prevalence, from 73% in 1993–1994 to 78% in 2004–2005, but a significant improvement in awareness and control among treated hypertensive individuals during the same period.
The results of the HCHS/SOL raise many questions that will be addressed in future research. The variation in the hypertension prevalence by background or center could be explained by a variety of factors including variations in genetics, obesity, diet (e.g., sodium intake), acculturation, or behavioral factors such as activity levels. Diabetes and metabolic syndrome are quite prevalent in this population and constitute avenues for further research in relation to hypertension. As the Affordable Care Act17 is implemented, there will be potential for research in understanding how changes in health insurance availability impact hypertension prevention and treatment.
Limitations of the study include the smaller number within some of the background groups, for example, South Americans. Also, while none of the Hispanic background groups included were completely homogenous, participants of Central and South American backgrounds include individuals from many different countries, and it is likely that even greater heterogeneity exists within these groups. Hypertension is defined based on measures in a single visit. While this allows comparison with other surveys that use the same methodology, it is not equivalent to hypertension diagnosed in a medical care setting where measurements over a period of time are preferred. Finally, it is important to note that the HCHS/SOL study population is not a representative sample of all Hispanics/Latinos in the United States but only represents the specific communities from which they were drawn.
In conclusion, while the overall hypertension prevalence in HCHS/SOL was slightly lower than that seen in non-Hispanic whites in NHANES, some Hispanic/Latino groups were found to experience markedly higher rates of hypertension. For those who have hypertension, however, there is a substantial gap in diagnosis and adequate treatment and control of blood pressure levels.
The results presented here carry several important messages. First, the Hispanic/Latino population is not a single entity but a highly diverse population with widely varying hypertension prevalence, with some Hispanic/Latino groups lower and other groups higher than for non-Hispanic whites. Of most concern is the low proportion of persons with their hypertension under control. The healthcare community, Hispanic/Latino advocates, health policy makers, and the Hispanic/Latino community at large have a challenging task and responsibility to create tailored strategies to improve awareness, treatment, and control of this significant factor for coronary disease, stroke, and heart failure.
DISCLOSURE
The authors declared no conflict of interest.
ACKNOWLEDGMENTS
The authors thank the staff and participants of for their important contributions. The study website is http://www.cscc.unc.edu/hchs/. The HCHS/SOL was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following institutes/centers/offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Institute on Minority Health and Health Disparities, National Institute on Deafness and Other Communication Disorders, National Institute of Dental and Craniofacial Research, National Institute of Diabetes and Digestive and Kidney Diseases, National Institute of Neurological Disorders and Stroke, and National Institutes of Health, Office of Dietary Supplements.
REFERENCES
- 1. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., Jones DW, Materson BJ, Oparil S, Wright JT, Jr., Roccella EJ. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42:1206–1252 [DOI] [PubMed] [Google Scholar]
- 2. Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev 2010; CD005182. [DOI] [PubMed] [Google Scholar]
- 3. Vasan RS, Kannel WB. Are guidelines effectively guiding antihypertensive therapy? Am J Cardiol 2007; 100:143–144 [DOI] [PubMed] [Google Scholar]
- 4. Daviglus ML, Talavera GA, Avilés-Santa ML, Allison M, Cai J, Criqui MH, Gellman M, Giachello AL, Gouskova N, Kaplan RC, LaVange L, Penedo F, Perreira K, Pirzada A, Schneiderman N, Wassertheil-Smoller S, Sorlie PD, Stamler J. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse background in the United States. JAMA 2012; 308:1775–1784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, Kaplan RC, Daviglus ML, Giachello AL, Schneiderman N, Raij L, Talavera G, Allison M, Lavange L, Chambless LE, Heiss G. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol 2010; 20:629–641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lavange LM, Kalsbeek WD, Sorlie PD, Aviles-Santa LM, Kaplan RC, Barnhart J, Liu K, Giachello A, Lee DJ, Ryan J, Criqui MH, Elder JP. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol 2010; 20:642–649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. US Census Bureau. The Hispanic Population Census: 2010, 2010 Census Brief. 2013. www.census.gov/prod/cen2010/briefs/c2010br-04.pdf Accessed 28 October 2013.
- 8. US Census Bureau. Census 2010 SF1 Data File, Table P4. 2013. http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml Accessed 28 October 2013.
- 9. US Census Bureau. Census 2010 SF1 Data File, Table GCT-P3. 2013. http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml Accessed 28 October 2013.
- 10. Ostchega Y, Zhang G, Sorlie P, Hughes JP, Reed-Gillette DS, Nwankwo T, Yoon S. Blood pressure randomized methodology study comparing automatic oscillometric and mercury sphygmomanometer devices: National Health and Nutrition Examination Survey, 2009–2010. National Health Statistics Reports no. 59. Hyattsville, MD: National Center for Health Statistics; 2012; 1–16 [PubMed] [Google Scholar]
- 11. Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People 2010 Stat Notes 2001; 1–10 [PubMed]
- 12. Crim MT, Yoon SS, Ortiz E, Wall HK, Schober S, Gillespie C, Sorlie P, Keenan N, Labarthe D, Hong Y. National surveillance definitions for hypertension prevalence and control among adults. Circ Cardiovasc Qual Outcomes 2012; 5:343–351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yoon SS, Burt V, Louis T, Carroll MD. Hypertension among adults in the United States, 2009–2010. NCHS data brief, no. 107. Hyattsville, MD: National Center for Health Statistics; 2012; 1–7 [PubMed] [Google Scholar]
- 14. Morales LS, Leng M, Escarce JJ. Risk of cardiovascular disease in first and second generation Mexican-Americans. J Immigr Minor Health 2011; 13:61–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Allison MA, Budoff MJ, Wong ND, Blumenthal RS, Schreiner PJ, Criqui MH. Prevalence of and risk factors for subclinical cardiovascular disease in selected US Hispanic ethnic groups: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol 2008; 167:962–969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. AlGhatrif M, Kuo YF, Al SS, Raji MA, Ray LA, Markides KS. Trends in hypertension prevalence, awareness, treatment and control in older Mexican Americans, 1993–2005. Ann Epidemiol 2011; 21:15–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.US Department of Health and Human Services, HHS.Gov/HealthCare. http://www.hhs.gov/healthcare/rights/ Accessed 31 December 2013.