Abstract
Evaluation and treatment of concomitant intra-articular pathology may be beneficial before periacetabular osteotomy (PAO) is performed. Hip arthroscopy before PAO allows the surgeon to perform full inspection of the hip joint and can be used to treat hip pathology before osteotomy. The indications for hip arthroscopy before PAO are presented in this article. The combined surgical procedure is described, along with potential complications. The advantages and disadvantages of this technique are outlined.
Hip dysplasia and femoroacetabular impingement are now recognized as the most common morphologic abnormalities that lead to hip osteoarthritis. Advances in our understanding of these conditions have provided treatment strategies to preserve the hip joint in young patients. Multiple studies have shown improved clinical outcomes after surgical correction of the abnormal anatomy found in patients with dysplasia and femoroacetabular impingement.1-3
Periacetabular osteotomy (PAO) has been popularized by Reinhold Ganz for the treatment of symptomatic hip dysplasia. The osteotomy addresses the underlying bony abnormality but does not correct concomitant intra-articular pathology. Recent studies have found a high incidence of labral tears, cartilage lesions, and soft-tissue disorders in dysplastic hips.4-6 In an effort to improve clinical outcomes, attention has been given to addressing intra-articular pathology at the time of PAO.7,8
In this article we describe our rationale and technique for combined hip arthroscopy and PAO. This approach allows the surgeon to effectively identify and address intra-articular pathology at the time of extra-articular correction.
Rationale for Combined Hip Arthroscopy and PAO
Patients with hip dysplasia frequently have intra-articular pathology in addition to bony under-coverage.8,9 The typical chondrolabral injury in the setting of dysplasia frequently lies along the anterosuperior rim. The labrum is torn in greater than 65% of these patients, and chondral lesions are also frequently observed.4,8,9
Hip arthroscopy prior to PAO is beneficial for 2 reasons (Table 1). First, it allows the surgeon to identify intra-articular pathology. Labral tears, cartilage flaps, and chondromalacia can be visually inspected. This may have important prognostic value for patients undergoing PAO and in some circumstances may lead the surgeon to terminate the procedure before PAO. If the chondral damage is more severe than predicted preoperatively, the osteotomy may be of little value. In this setting it may be preferable to avoid PAO in favor of arthroplasty. Second, hip arthroscopy allows treatment of intra-articular pathology before PAO. Prior to PAO, many concomitant procedures may be beneficial; chondroplasty, microfracture, labral repair, and ligamentum teres debridement are all amenable to arthroscopic treatment.
Table 1.
Rationale for Combined Approach
| 1. Identification of chondral damage before PAO |
| 2. Treatment of intra-articular pathology in conjunction with PAO |
The labrum plays an important role in maintaining normal hip biomechanics, including joint stability, load bearing, synovial fluid regulation, and maintenance of the suction seal.10-13 An intact labrum is necessary for proper regulation of fluid flow. Ferguson et al.12 have shown that a functional labrum preserves normal hydrostatic pressure in the hip, which may be important for cartilage health. Multiple studies have now shown improved clinical outcomes when the labrum is repaired, rather than debrided.3,14-16
Given the high prevalence of labral tears in the setting of dysplasia and evidence that the labrum plays a protective role in the hip, it stands to reason that labral repair at the time of PAO may improve short- and long-term clinical outcomes. An arthrotomy at the time of PAO can be performed; however, arthroscopy may provide more complete access and visualization of the entire joint. In 1 study, in which a second-look arthroscopy was performed at a mean of 18 months after PAO, labral tears either persisted or worsened.4 The labrum may be an important pain generator before PAO, as well as afterward if left untreated. In a group of 135 patients who underwent PAO, 15 patients had pain that led to arthroscopic labral treatment.7 Eleven of those patients reported resolution of symptoms.
Patient Selection
Patients are considered for PAO with concomitant hip arthroscopy based on history, clinical examination, radiographs, and delayed gadolinium-enhanced magnetic resonance imaging of cartilage (dGEMRIC). Nonoperative treatment is initially trialed for patients with mild dysplasia (lateral center-edge angle of 20° to 25°) and consists of physical therapy, activity restrictions, and nonsteroidal anti-inflammatory medications. Patients with symptomatic dysplasia are considered for surgery. A positive response to intra-articular diagnostic injection, using local anesthetic, aids in confirming that the pain is originating from the hip joint.
Radiographic analysis includes anteroposterior pelvis, false-profile, Dunn lateral, and Von Rosen views. Radiographs are used to calculate the degree of dysplasia using the lateral center-edge angle, acetabular index, and anterior center-edge angle.17,18 The amount of joint space narrowing, sclerosis, and osteophyte formation is also scrutinized. Radiographs and magnetic resonance imaging should be used to determine whether a cam lesion on the femoral head or neck exists. The dGEMRIC is evaluated for labral tears, chondral flaps, bony edema, and the dGEMRIC index.
Patients with joint space narrowing or significant chondral injury are not considered for PAO. Patients with mild dysplasia, a lateral center-edge angle of 20° to 25°, may be considered for arthroscopy alone.
Surgical Technique
Surgeons
A critical principle in the treatment of the dysplastic hip is a multidisciplinary approach that permits understanding and treatment of both the bony and soft-tissue aspects of the pathology. The procedure is performed by 2 attending surgeons working in concert: a specialist in arthroscopic and open hip preservation (B.D.) and a specialist in PAO and open hip preservation (J.L.) (Video 1). Although one surgeon could perform both the arthroscopic and open parts of this procedure, we believe that the team approach yields better decision making, technical expertise in all parts of the procedure, and a faster operative time (Table 2).
Table 2.
Benefits of Team Approach
| 1. Better decision making |
| 2. Technical expertise in arthroscopic and open techniques |
| 3. Faster operative time |
Operating Room Preparation
Two operating tables are used during the course of the procedure. Hip arthroscopy is performed first on a traction table, and the patient is then transferred to a flat-top radiolucent table for PAO. A standard fluoroscope is used for both procedures and is positioned on the side opposite the affected hip.
Anesthesia
An epidural catheter is placed before the procedure for postoperative pain control. The patient is placed under general anesthesia. Skeletal muscle relaxation is preferred for distraction during hip arthroscopy. This can be accomplished by infusing anesthetic through the epidural catheter or by intravenous paralysis. If the epidural catheter is used during the procedure, it can prevent possible recognition of nerve injury during PAO and may compromise the postoperative neurological examination. The epidural catheter can be titrated to have a sensory blockade but still allow motor function. Hypotensive anesthesia is helpful for minimizing the pump pressure needed for hip arthroscopy and preventing complications due to fluid extravasation.19-21 This is particularly important during this combined procedure because fluid extravasation can cause increased difficulty with surgical dissection during PAO.
Hip Arthroscopy
The patient is transferred to the fracture table with a well-padded perineal post.22 Arthroscopy in this setting is typically performed with an anterolateral portal and mid-anterior portal. The standard anterolateral portal is placed 1 to 2 cm superior and 1 to 2 cm anterior to the greater trochanter with the hip distracted.23 In dysplastic hips the labrum is typically hypertrophied, and care should be taken to avoid iatrogenic injury during insertion of the arthroscope. This is accomplished by aiming toward the most distal part of the air arthrogram with a 14-gauge spinal needle under fluoroscopy. Joint access is achieved as previously described by Domb et al.24 The joint is vented and then re-entered with the spinal needle. A wire is passed into the joint, and a cannulated obturator and arthroscopic sheath are introduced. A 70° arthroscope is then introduced, and a spinal needle is used to create a mid-anterior portal. The mid-anterior portal is the apex of a triangle created by the standard anterolateral portal and anterior portal. This portal is created before infusion of fluid into the joint to prevent poor visualization due to bleeding. Diagnostic arthroscopy is performed using the mid-anterior and anterolateral portals. Most intra-articular pathology is anterosuperior in dysplastic hips, and these portals can typically be used for all central- and peripheral-compartment procedures. Complete diagnostic arthroscopy of the central compartment is then carried out with treatment as indicated.
Labral Treatment
Labral tears are frequently identified before PAO and should be repaired if satisfactory labral tissue remains. The labrum is often hypertrophied and amenable to refixation. We prefer to use a labral base stitch as previously described (Fig 1).25 In some cases the labrum will not be amenable to repair, and in these cases debridement or reconstruction is preferred to leaving the torn labrum.
Fig 1.
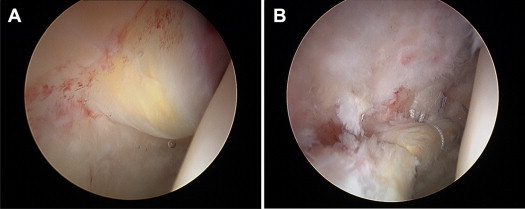
A 26-year-old woman presented with a 7-month duration of groin pain and mechanical symptoms. She was treated with combined hip arthroscopy and PAO. (A) At the time of arthroscopy, she was noted to have a hypertrophied and torn labrum. (B) She underwent labral repair before PAO.
Chondral Treatment
The anterosuperior aspect and, occasionally, the posterosuperior aspect of the acetabulum frequently show signs of chondral pathology before PAO.4 Unstable cartilage flaps are treated with chondroplasty, and full-thickness defects are treated with microfracture.
Less frequently, the femoral head will have evidence of chondral injury. In our experience these lesions are typically partial thickness and treated with chondroplasty when indicated.
Ligamentum Teres
Inspection of the ligamentum teres during arthroscopy will often show full- or partial-thickness tearing.26 It is our preference to debride these tears. All degenerative and torn tissue is debrided with an arthroscopic shaver and radiofrequency device.
Iliopsoas
Internal snapping is a common finding among patients with dysplastic hips.27 This can be treated arthroscopically or during PAO with fractional iliopsoas lengthening. However, the iliopsoas may function as an anterior stabilizer of the hip, and therefore a thoughtful approach to its treatment is necessary in the setting of dysplasia.
Peripheral Compartment
After the lesions in the central compartment have been addressed, traction is released and the hip is flexed to 45°. The head and neck junction of the femur is inspected and compared with preoperative imaging. Cam lesions are identified, and femoroplasty is performed when indicated.
Periacetabular Osteotomy
After completion of the arthroscopic procedure, the portals are closed and the patient is transferred to a radiolucent table. Capsular closure and possible advancement are addressed at the completion of the open procedure. The technique for PAO has been described by Ganz and modified by Millis and colleagues.7 A modified iliofemoral approach is used for exposure. The skin incision begins proximally along the iliac crest and extends distally and medially, just caudal to the inguinal crease. Subcutaneous flaps are raised to allow similar deep tissue dissection. Proximally, the fascia overlying the iliac crest between the external obliques and gluteus medius is incised. The external obliques and iliacus are elevated subperiosteally from the inner table of the pelvis. The anterior superior iliac spine (ASIS) then undergoes osteotomy to allow reflection of the sartorius. Subperiosteal dissection can be continued to the anterior inferior iliac spine. The direct and reflected heads of the rectus femoris are incised to expose the hip capsule. The capsular insertion of the iliacus is gently elevated to enhance visualization.
The hip is flexed and adducted to remove tension on the anterior musculature. The interval between the medial joint capsule and iliopsoas is then developed in preparation for the ischial osteotomy. Once entered, the interval is established with blunt elevators and dilated. The ischium is bluntly palpated, and overlying soft tissue is elevated. Angled or curved osteotomes are passed through this prepared interval. The surgeon uses fluoroscopy to confirm the position of a Ganz or Mast osteotome for the ischial cut, checking instrument position on anteroposterior, false-profile, and 50° cephalad views. The osteotomy is frequently carried out in 3 stages, first the medial portion, then the lateral portion, and finally, the central portion of the ischium.
Attention is then turned to the pubic osteotomy. Exposure of the pubis is also aided by flexion and adduction of the hip. The psoas tendon is retracted anteromedially with a small Hohmann retractor gently impacted into the pubis. The periosteum overlying the pubis is incised longitudinally and retracted. A Gigli saw is passed around the pubis by use of a curved Satinsky or vascular clamp. Care is taken to identify the iliopectineal eminence and pass the saw medial to it to reduce the risk of intra-articular extension during pubic osteotomy. The Gigli saw is placed in a superomedial-to-inferolateral direction, with care taken to remain perpendicular to the long axis of the pubis. This facilitates fragment mobilization. Once completed, an osteotome is inserted in the pubic osteotomy to ensure mobility and completion of the cut.
The leg is abducted and extended to protect the sciatic nerve. The ilium is exposed just distal below the ASIS because this is used as a starting point. The osteotomy is marked with Bovie electrocautery, typically originating just distal to the ASIS and terminating 1 cm proximal to the brim of the true pelvis. The osteotomy should also terminate at the mid portion of the posterior column, with care taken to remain posterior to the hip joint but anterior to the sciatic notch. The ilium then undergoes osteotomy from an anterior-to-posterior direction with a power saw.
The posterior column is then exposed through elevation of the iliacus off the inner table. A deep retractor is advanced to the quadrilateral surface to aid in exposure. A long straight osteotome is used under fluoroscopic guidance to initially score the posterior column. A Ganz osteotome is then used to deepen the cut and connect existing cuts in the ilium and ischium.
A Schanz screw is placed using fluoroscopy in the fragment that has undergone osteotomy. The screw is placed 5 to 10 mm proximal to the articular surface. The fragment is mobilized and repositioned to improve coverage. Fluoroscopy is used to visualize the correction. Once the fragment is positioned correctly, it is fixed with 4.5- and 3.5-mm screws.
The anterior hip capsule is exposed, and the previous capsulotomy created during the arthroscopy is closed. The capsule is plicated to improve hip stability when necessary. During closure, the ASIS osteotomy is repaired with a 4.0-mm cancellous screw with a washer or heavy nonabsorbable suture (Fig 2).
Fig 2.
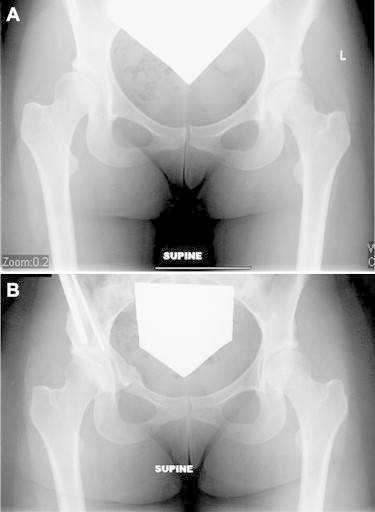
A 21-year-old woman presented with longstanding activity-related right groin pain. (A) An anteroposterior pelvic radiograph shows acetabular dysplasia. (B) She underwent combined hip arthroscopy and PAO.
Postoperative Rehabilitation
The epidural catheter is used for the first 24 to 48 hours after surgery. A continuous passive motion machine is used starting on postoperative day 1, continuing for 6 weeks. Weight bearing is restricted to one-sixth of normal body weight for 6 to 8 weeks. Subsequent physical therapy is focused first on achieving range of motion, second on strengthening hip stabilizers and core muscles, and third on functional rehabilitation.
Discussion
PAO has become accepted treatment for hip dysplasia, with good results seen at midterm follow-up.2,28 Treatment of concomitant intra-articular pathology at the time of pelvic osteotomy has the potential to improve outcomes, although this is debatable. Many authors have reported compromised long-term outcomes after PAO with labral tears, whereas others have not seen this association.2,29,30 The literature may also be compromised with respect to treating labral pathology because many reports consist of debridement rather than repair.
There are advantages and disadvantages to hip arthroscopy before PAO. Intra-articular treatment can be performed in an open manner through an arthrotomy or arthroscopically (Table 3). An anterior arthrotomy provides access to a limited window within the joint, whereas arthroscopy allows access to the entire central compartment and acetabular rim. The ability to fully access the central compartment allows the surgeon to identify and treat all concomitant pathology in this setting. It allows inspection of the joint, which in some circumstances may deter the surgeon from proceeding with an osteotomy. Labral tears can be repaired along the entire rim. Chondral injuries can be addressed in the anterosuperior and posterosuperior region. Rim trimming, chondroplasty, and microfracture can be performed in an effort to treat chondral injury. Ligamentum teres tears are treatable arthroscopically. Further long-term outcome studies will be necessary to determine whether complete treatment of the intra-articular findings will yield improved results.
Table 3.
Advantages and Disadvantages to Arthroscopy Before PAO
| Advantages | Disadvantages |
|---|---|
| Identification of intra-articular pathology | Increased operative time |
| Treatment of intra-articular pathology | Fluid extravasation before PAO |
| Potential to create instability | |
| Complications from secondary procedure |
There are drawbacks to performing arthroscopy before PAO. The need to transfer the patient from a traction table to a radiolucent table adds to the surgical time. Fluid extravasation can be problematic during the osteotomy by complicating soft-tissue anatomy and surgical dissection. This can be minimized by limiting the arthroscopy time, using a lower pump pressure, and maintaining adequate outflow. Often, this procedure will require 2 surgical teams: one team proficient in hip arthroscopy and another team adept at pelvic osteotomy.
The treatment of hip dysplasia is evolving over time. PAO is often the treatment of choice in a young patient with symptomatic hip dysplasia. In addition to treating the structural pelvic deformity, treatment of coexisting intra-articular pathology has the potential to improve outcomes. Hip arthroscopy may be preferable to open capsulotomy to address the intra-articular pathology.
Footnotes
The authors report the following potential conflict of interest or source of funding: B.D. receives support from Arthrex and MAKO Surgical; and J.L. receives support from Arthrex.
Supplementary Data
Combined hip arthroscopy and PAO.
References
- 1.Steppacher S.D., Tannast M., Ganz R., Siebenrock K.A. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matheney T., Kim Y.J., Zurakowski D., Matero C., Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–2123. doi: 10.2106/JBJS.G.00143. [DOI] [PubMed] [Google Scholar]
- 3.Larson C.M., Giveans M.R., Stone R.M. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: Mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015–1021. doi: 10.1177/0363546511434578. [DOI] [PubMed] [Google Scholar]
- 4.Fujii M., Nakashima Y., Jingushi S. Intraarticular findings in symptomatic developmental dysplasia of the hip. J Pediatr Orthop. 2009;29:9–13. doi: 10.1097/BPO.0b013e318190a0be. [DOI] [PubMed] [Google Scholar]
- 5.Ilizaliturri V.M., Jr., Chaidez P.A., Valero F.S., Aguilera J.M. Hip arthroscopy after previous acetabular osteotomy for developmental dysplasia of the hip. Arthroscopy. 2005;21:176–181. doi: 10.1016/j.arthro.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 6.Klein S.E., Morgan P., Schoenecker P.L., Clohisy J.C. Arthroscopic treatment of labral tears after a previous Pemberton osteotomy. J Pediatr Orthop. 2010;30:549–553. doi: 10.1097/BPO.0b013e3181e4f575. [DOI] [PubMed] [Google Scholar]
- 7.Matheney T., Kim Y.J., Zurakowski D., Matero C., Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome: Surgical technique. J Bone Joint Surg Am. 2010;92(suppl 1 pt 2):115–129. doi: 10.2106/JBJS.J.00646. [DOI] [PubMed] [Google Scholar]
- 8.Ross J.R., Zaltz I., Nepple J.J., Schoenecker P.L., Clohisy J.C. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med. 2011;39(suppl):72S–78S. doi: 10.1177/0363546511412320. [DOI] [PubMed] [Google Scholar]
- 9.McCarthy J.C., Lee J.A. Acetabular dysplasia: A paradigm of arthroscopic examination of chondral injuries. Clin Orthop Relat Res. 2002;(405):122–128. doi: 10.1097/00003086-200212000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Field R.E., Rajakulendran K. The labro-acetabular complex. J Bone Joint Surg Am. 2011;93(suppl 2):22–27. doi: 10.2106/JBJS.J.01710. [DOI] [PubMed] [Google Scholar]
- 11.Ferguson S.J., Bryant J.T., Ganz R., Ito K. The acetabular labrum seal: A poroelastic finite element model. Clin Biomech (Bristol, Avon) 2000;15:463–468. doi: 10.1016/s0268-0033(99)00099-6. [DOI] [PubMed] [Google Scholar]
- 12.Ferguson S.J., Bryant J.T., Ganz R., Ito K. The influence of the acetabular labrum on hip joint cartilage consolidation: A poroelastic finite element model. J Biomech. 2000;33:953–960. doi: 10.1016/s0021-9290(00)00042-7. [DOI] [PubMed] [Google Scholar]
- 13.Ferguson S.J., Bryant J.T., Ganz R., Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36:171–178. doi: 10.1016/s0021-9290(02)00365-2. [DOI] [PubMed] [Google Scholar]
- 14.Larson C.M., Giveans M.R. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369–376. doi: 10.1016/j.arthro.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 15.Schilders E., Dimitrakopoulou A., Bismil Q., Marchant P., Cooke C. Arthroscopic treatment of labral tears in femoroacetabular impingement: A comparative study of refixation and resection with a minimum two-year follow-up. J Bone Joint Surg Br. 2011;93:1027–1032. doi: 10.1302/0301-620X.93B8.26065. [DOI] [PubMed] [Google Scholar]
- 16.Philippon M.J., Briggs K.K., Yen Y.M., Kuppersmith D.A. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: Minimum two-year follow-up. J Bone Joint Surg Br. 2009;91:16–23. doi: 10.1302/0301-620X.91B1.21329. [DOI] [PubMed] [Google Scholar]
- 17.Peelle M.W., Della Rocca G.J., Maloney W.J., Curry M.C., Clohisy J.C. Acetabular and femoral radiographic abnormalities associated with labral tears. Clin Orthop Relat Res. 2005;441:327–333. doi: 10.1097/01.blo.0000181147.86058.74. [DOI] [PubMed] [Google Scholar]
- 18.Wenger D.E., Kendell K.R., Miner M.R., Trousdale R.T. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;(426):145–150. doi: 10.1097/01.blo.0000136903.01368.20. [DOI] [PubMed] [Google Scholar]
- 19.Morrison D.S., Schaefer R.K., Friedman R.L. The relationship between subacromial space pressure, blood pressure, and visual clarity during arthroscopic subacromial decompression. Arthroscopy. 1995;11:557–560. doi: 10.1016/0749-8063(95)90131-0. [DOI] [PubMed] [Google Scholar]
- 20.Clarke M.T., Arora A., Villar R.N. Hip arthroscopy: Complications in 1054 cases. Clin Orthop Relat Res. 2003;406:84–88. doi: 10.1097/01.blo.0000043048.84315.af. [DOI] [PubMed] [Google Scholar]
- 21.Fowler J., Owens B.D. Abdominal compartment syndrome after hip arthroscopy. Arthroscopy. 2010;26:128–130. doi: 10.1016/j.arthro.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 22.Byrd J.W. Hip arthroscopy. The supine position. Clin Sports Med. 2001;20:703–731. [PubMed] [Google Scholar]
- 23.Kelly B.T., Weiland D.E., Schenker M.L., Philippon M.J. Arthroscopic labral repair in the hip: Surgical technique and review of the literature. Arthroscopy. 2005;21:1496–1504. doi: 10.1016/j.arthro.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 24.Domb B., Hanypsiak B., Botser I. Labral penetration rate in a consecutive series of 300 hip arthroscopies. Am J Sports Med. 2012;40:864–869. doi: 10.1177/0363546512437152. [DOI] [PubMed] [Google Scholar]
- 25.Fry R., Domb B. Labral base refixation in the hip: Rationale and technique for an anatomic approach to labral repair. Arthroscopy. 2010;26(suppl):S81–S89. doi: 10.1016/j.arthro.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 26.Botser I.B., Martin D.E., Stout C.E., Domb B.G. Tears of the ligamentum teres: Prevalence in hip arthroscopy using 2 classification systems. Am J Sports Med. 2011;39(suppl):117S–125S. doi: 10.1177/0363546511413865. [DOI] [PubMed] [Google Scholar]
- 27.Clohisy J.C., St John L.C., Nunley R.M., Schutz A.L., Schoenecker P.L. Combined periacetabular and femoral osteotomies for severe hip deformities. Clin Orthop Relat Res. 2009;467:2221–2227. doi: 10.1007/s11999-009-0810-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garras D.N., Crowder T.T., Olson S.A. Medium-term results of the Bernese periacetabular osteotomy in the treatment of symptomatic developmental dysplasia of the hip. J Bone Joint Surg Br. 2007;89:721–724. doi: 10.1302/0301-620X.89B6.18805. [DOI] [PubMed] [Google Scholar]
- 29.Sambandam S.N., Hull J., Jiranek W.A. Factors predicting the failure of Bernese periacetabular osteotomy: A meta-regression analysis. Int Orthop. 2009;33:1483–1488. doi: 10.1007/s00264-008-0643-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Siebenrock K.A., Leunig M., Ganz R. Periacetabular osteotomy: The Bernese experience. Instr Course Lect. 2001;50:239–245. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Combined hip arthroscopy and PAO.


