Abstract
Objective
To determine whether the presence and extent of severe lumbar facet joint osteoarthritis (OA) is associated with back pain in older adults, accounting for disc height narrowing and other covariates.
Design
252 older adults from the Framingham Offspring Cohort (mean age 67 years) were studied. Participants received standardized CT assessments of lumbar facet joint OA and disc height narrowing at the L2-S1 interspaces using 4-grade semi-quantitative scales. Severe facet joint OA was defined according to the presence and/or degree of joint space narrowing, osteophytosis, articular process hypertrophy, articular erosions, subchondral cysts, and intraarticular vacuum phenomenon. Severe disc height narrowing was defined as marked narrowing with endplates almost in contact. Back pain was defined as participant report of pain on most days or all days in the past 12 months. We used multivariable logistic regression to examine associations between severe facet joint OA and back pain, adjusting for key covariates including disc height narrowing, sociodemographics, anthropometrics, and health factors.
Results
Severe facet joint OA was more common in participants with back pain than those without (63.2% vs. 46.7%;p=0.03). In multivariable analyses, presence of any severe facet joint OA remained significantly associated with back pain (odds ratio[OR]2.15 (95% confidence interval [CI]1.13-4.08). Each additional joint with severe OA conferred greater odds of back pain (OR per joint 1.20 (95% CI;1.02-1.41).
Conclusions
The presence and extent of severe facet joint OA on CT imaging is associated with back pain in community-based older adults, independent of sociodemographics, health factors, and disc height narrowing.
Keywords: zygapophyseal, lumbar, arthritis, intervertebral disc, spondylosis
INTRODUCTION
Back pain is a common reason prompting older adults to seek medical care, and a leading cause of disability in developed countries [1-5]. The spinal facet (‘zygapophyseal’) joints are a widely treated source of back pain, and rates of nonoperative yet invasive percutaneous facet joint procedures in older adults have increased more than 4-fold over the past decade[6]. Facet joint osteoarthritis (OA) is often presumed to be the cause of pain in some older adults with facet-mediated pain confirmed by anesthetic blocks[7]. Nevertheless, some patients with facet joint OA may have no back pain at all, and patients without facet joint OA may have substantial back pain[8-10]. This discordance between the appearance of facet joint OA on imaging and the symptom of pain is analogous to the high prevalence of asymptomatic radiographic findings observed in the setting of knee OA[11, 12].
Cross-sectional imaging using CT or MRI is necessary for complete evaluation of facet joint morphology in multiple planes, including the axial plane. Remarkably few population-based studies have examined relationships between facet joint OA on cross-sectional spinal imaging and the presence of back pain[8-10] (Table 1), and no studies have found significant associations. However, characteristics of these earlier works may explain why relevant associations between facet joint OA and back pain might not have been detected. Prior studies used either mild or moderate facet joint OA at any spinal level as the threshold for defining prevalent facet joint OA. It is possible that more advanced (severe) facet joint OA would be more strongly associated with back pain, such as is seen in the context of knee OA[11]. Also, prior studies did not examine the number of levels affected by severe facet joint OA, ignoring this important aspect of disease burden. Furthermore, earlier studies examined younger and middle-aged samples. This largely excludes older adults, in whom advanced facet joint OA on imaging as well as facet-mediated pain is most prevalent[13, 14], and in whom facet joint interventions are most commonly performed[6]. Last, some prior studies have not utilized well-described and reliable scales for facet joint OA[8, 9].
Table 1. Prior Studies of Lumbar Facet Joint Osteoarthritis and Back Pain.
| Imaging modality |
Mean age (years) |
Sample size |
Country | Year | Use of a well- characterized scale for facet joint OA*? |
Threshold for facet joint OA severity |
Association with Back Paint† |
|
|---|---|---|---|---|---|---|---|---|
| Kjaer et al. [8] | MRI | 40 | 412 | Denmark | 2005 | No | Mild | 1.1 (0.7-1.6) |
| Savage et al. [9] | MRI | 36 | 149 | United Kingdom |
1997 | No | Unclear | 4.4 (0.9-21) |
| Kalichman et al. [10] | CT | 53 | 188 | United States |
2008 | Yes | Moderate | 1.0 (0.5- 2.1) |
OA= Osteoarthritis
Odds ratio (95% confidence interval)
We attempted to overcome these limitations by conducting a study to examine associations between lumbar facet joint OA on imaging and back pain in a sample representative of community-based older US adults. The aim of this study was to determine whether definitions of facet joint OA incorporating the presence and extent of severe facet joint OA are associated with back pain in older adults, with and without adjustment for other sociodemographic factors, clinical factors, and disc height narrowing.
METHODS
Participants
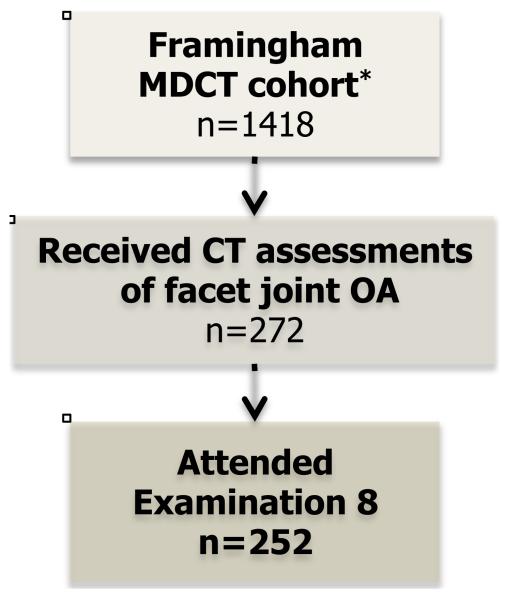
This study was an ancillary investigation to the Framingham Heart Study, and was approved by the Institutional Review Board of New England Baptist Hospital. The Offspring cohort of the Framingham Heart Study was initiated in 1971 as a prospective epidemiologic study of 5124 young adults [15]. 1418 individuals from the Offspring cohort underwent computed tomography (CT) scanning as part of the multidetector CT (MDCT) substudy of Framingham, which has been described elsewhere [16, 17]. Two hundred and seventy-two participants randomly selected from the MDCT cohort study received standardized CT assessments of facet joint OA as part of this ancillary study (Figure 1). Of this subgroup, 252 participants also attended Framingham Examination 8, and comprised our study sample. This represents a separate study sample from that reported in an earlier publication on facet joint OA by our research group [10]. Whereas the earlier study examined participants from both the Offspring and Generation 3 cohorts of Framingham, the present study sample is drawn from the Offspring cohort only, enriching the sample for older adults. Furthermore, the present study includes separate CT assessments conducted by different readers, and different pain assessments. In addition, our a priori analytic approach is distinct from that taken in our earlier work in that it examines the presence and extent of severe facet joint OA, rather than the finding of any moderate FJ facet joint OA.
Figure 1.
Flowchart of participation
MDCT= multi-detector computed tomography
Assessment of Facet Joint Osteoarthritis
All CT imaging assessments were performed using eFilm Workstation (Version 2.0.0) software, with blinding to sociodemographic and health-related factors, and pain information. Facet joint OA was graded at both the left and the right side at the spinal levels L2-L3, L3-L4, L4-L5, and L5-S1. We applied the Framingham Scale for grading of facet joint OA, a semi-quantitative measure we designed for these research purposes, based on earlier scales by Pathria et al.[18] and Weishaupt et al.[19] The Framingham Scale grades facet joint OA according to the degree of pathoanatomic change in the separate subcategories of joint space narrowing, osteophytosis, articular process hypertrophy, sclerosis, subarticular erosion, subchondral cystic change, and presence of vacuum phenomenon (Appendix 1). Because we were specifically focused on examining associations with severe or advanced facet joint OA, we considered the presence of severe facet joint OA to be at least grade IV facet joint OA in either the left or right facet joints at one or more lumbar spinal levels L2-S1 (Appendix 1). We defined the extent of severe facet joint OA as the number of joints with severe facet joint OA at the lumbar spinal levels L2-S1 (range 0-8). The Framingham CT scans did not consistently include the L1-L2 level, and this level therefore was not read as part of these structured assessments.
Assessment of Disk Height Narrowing
Disc height narrowing was graded at spinal levels L2-L3, L3-L4, L4-L5, and L5-S1, using grading criteria developed for research purposes by Videman et al., that have been used previously in studies of spinal degeneration on MRI[20-22]. Using sagittal CT reformatting, the midsagittal plane was identified at each level, and measurements of disc height narrowing were made at the midpoint of the anteroposterior diameter of the disk. This method was intended to account for degenerative scoliosis, which is common in older adults and may influence interpretations of disc height. These measurements were then used in applying the grading system of Videman: disc height narrowing was graded as ‘normal’ (disk height greater than level immediately superior), ‘mild’ (disk height equal to level immediately superior), ‘moderate’ (disk height narrowed as compared to level immediately superior), and ‘severe’ (endplates almost in contact)[23]. In instances where the reference level exhibited apparent disc height narrowing, the first ‘normal’ interspace superior to the index level was used as a reference. Since there is greater variability in disk height at the L5-S1 level as compared to L4-L5 [24], L5-S1 was graded based on reader experience, but was generally considered normal if comparable to, or slightly narrowed, as compared to L4-L5. Further details of the disc grading methods employed are provided elsewhere[23].
Quality and Reliability of CT Assessments
CT assessments of facet joint OA and disc height narrowing were performed by a board-certified, fellowship-trained nonoperative spine care specialist (PS), who was trained by a musculoskeletal radiologist (AG). Assessments of facet joint OA and disc height narrowing were performed at separate periods in time (i.e. disc height narrowing assessments were completed for all participants in the sample prior to the start of facet joint OA assessments), and participants were blinded to the results of these assessments. A reference atlas for each degenerative parameter was used throughout the reading process. The spine specialist reader calibrated to the standard of the radiologist prior to the start of formal reads using training sets of CT scans, and inter-observer reliability was calculated between the radiologist and spine specialist at the start of the reading process. All CT scans were interpreted by the spine specialist in a blinded fashion. Recalibration of the spine specialist was repeated during the reading process, either by direct interactions with the radiologist, or by review of images previously interpreted by the radiologist. To evaluate for reader-drift, reliability was reassessed periodically. Inter-observer reliability using the weighted κ statistic ranged between 0.68 and 0.84 for facet joint OA, and 0.70 and 0.84 for disc height narrowing, representing moderate to excellent reproducibility.
Assessment of Back Pain
All participants in the Framingham Offspring cohort underwent a standardized interview as part of the recurring Framingham clinical examinations. Participants were asked the question, ‘Have you had back pain in the past 12 months?’ Response categories included ‘no back pain’, or back pain on ‘a few days’, ‘some days’, ‘most of the days’, or ‘all days’. Because most individuals reported having at least some back pain, and we were interested in associations with frequent or persistent back pain specifically, individuals who reported having back pain on ‘all days’ or ‘most of the days’ were considered to have frequent back pain, and individuals who reported having no back pain, back pain on ‘a few days’, or ‘some days’ were considered to be without frequent back pain. Back pain and covariate data were taken from the Framingham examination that best coincided with the timing of the CT scan (Examination 8); this examination was conducted an average of 20 months after the CT scan (range: −1 to 58 months).
Covariates
Covariates examined in this study included those of particular relevance to older adults at or beyond retirement age[25-27]. Data were collected on participant age calculated according to birth date, and participant-reported sex, race, ethnicity, and educational background. Participants reported on current employment or volunteering activities, retirement from primary occupation or career, marital status, and whether or not they currently lived alone. Height and weight were measured at each clinical examination, and body mass index (BMI) was calculated as weight (kg) divided by height (meters2). Participants who reported smoked regularly within the past year were defined as current smokers.
Statistical analysis
We characterized the sample using descriptive statistics. We compared sociodemographics, health-related factors, and prevalence of facet joint OA and disc height narrowing between participants with and without frequent back pain, using the Student’s t-test for continuous variables or the chi-square test for categorical variables. We used a series of logistic regression models to determine unadjusted associations between single independent variables, including facet joint OA, and the outcome of frequent back pain. We examined correlations between independent variables using Spearman correlation coefficients. Next, we created a ‘core’ multivariable logistic regression model that included those sociodemographic and health-related factors that demonstrated at least a statistical trend towards an association with frequent back pain in the unadjusted regression models (p ≤ 0.15). We then added the variables of any severe facet joint OA and any severe disc height narrowing to the core multivariable model. We then repeated this process, treating the facet joint OA and disc height narrowing variables as the number of joints with severe OA or the number of disc levels with severe narrowing, rather than as dichotomous variables. We also conducted secondary multivariable analyses choosing covariates based on conceptual importance, adjusting for the factors of age, sex, BMI, and education. All analyses were performed using SPSS software, version 20.0.0) (IBM Corporation, Armonk, NY).
RESULTS
Two hundred and fifty-two participants comprised the study sample (Table 2). The mean age of participants was 67.4 ± 9.1 years and approximately half of participants were female. Reflecting the demographics of Framingham, Massachusetts at the time of the Offspring cohort’s inception, almost all participants were of white race and of non-Latino ethnicity. Roughly half of the sample were neither working nor volunteering, or had retired from their primary career occupation, reflecting the older age of the study sample. The study sample was slightly older than the main MDCT cohort (67.4 vs. 65.9 years; p=0.02), but otherwise without significant differences with respect to sociodemographic factors or back pain (data not shown).
Table 2. Study Sample (n=252).
| n (%) or mean (SD)* |
|
|---|---|
| Sociodemographics | |
|
| |
| Age (yrs.) | 67.4 (9.1) |
| Female sex | 122 (48.4%) |
| White race | 245 (97.2%) |
| Hispanic or Latino ethnicity | 1 (0.4%) |
| College education† | 104 (41.9%) |
| Working or volunteering†‡ | 159 (63.3%) |
| Retired (irrespective of whether working or volunteering)† |
132 (52.6%) |
| Married or living with a partner† | 161 (65.2%) |
| Live alone | 55 (21.8%) |
|
| |
| Health Factors | |
|
| |
| Body mass index (kg/m2) | 28.3 (4.8) |
| Smoked regularly in last year | 16 (6.3%) |
|
| |
| Spinal Degeneration on CT Imaging | |
|
| |
| Any moderate facet joint OA | 216 (85.7%) |
| Any severe facet joint OA | 127 (50.4%) |
| No joints with severe OA | 125 (49.6) |
| 1-2 joints with severe OA | 71 (28.2%) |
| 3-8 joints with severe OA | 56 (22.2%) |
| Any moderate disc height narrowing† | 175 (70.3%) |
| Any severe disc height narrowing† | 98 (39.4%) |
| No levels with severe narrowing | 151 (60.6%) |
| 1 level with severe narrowing | 68 (27.3%) |
| 2-4 levels with severe narrowing | 30 (12.0% |
|
| |
|
Back pain on most or all of the days
in the past 12 months |
57 (22.6%) |
n=number, SD= standard deviation
missing data in <1-2% of participants
homemakers defined as working
Table 3 presents a comparison of individuals with and without frequent back pain. Individuals with back pain were significantly older than those without (69.6 vs. 66.7 years; p=0.03); this association was driven mainly by a higher prevalence of back pain in those adults age ≥75 years. Self-report of neither working nor volunteering currently, and retirement from usual occupation, were significantly associated with a higher prevalence of back pain, and individuals with back pain were also somewhat more likely to live alone. Other sociodemographic and health factors, including higher BMI, were not associated with back pain. The presence of moderate facet joint OA was not associated with back pain, but both the presence of any severe facet joint OA (46.7% vs. 63.2%; p=0.03), and the number of joints with severe facet joint OA (p=0.006), were significantly associated with back pain. No associations were seen between disc height narrowing and back pain, regardless of the severity or extent of disc height narrowing.
Table 3. Characteristics of Older Adults With and Without Back Pain* (n=252).
| Back pain on none/few/some days (n=195) |
Back pain on most/all days (n=57) |
p-value | |
|---|---|---|---|
| Sociodemographic and Health Factors | |||
|
| |||
| Age (yrs.) | 66.7 (9.0) | 69.6 (9.1) | 0.03† |
| Female Sex | 91 (46.7%) | 31 (54.4%) | 0.31 |
| College Education | 81 (42.2%) | 23 (41.1%) | 0.96 |
| Working or volunteering (homemakers defined as working) |
130 (66.7%) | 29 (51.8%) | 0.04† |
| Retired from usual occupation or otherwise not employed |
95 (48.7%) | 37 (66.1%) | 0.02† |
| Married | 125 (65.1%) | 36 (65.5%) | 0.96 |
| Live alone | 38 (19.5%) | 17 (29.8%) | 0.10 |
| Body Mass Index (kg/m2) | 28.0 (4.6) | 29.0 (5.5) | 0.23 |
| Smoked regularly in last year | 14 (7.7%) | 5 (8.8%) | 0.79 |
|
| |||
| Spinal Degeneration on CT Imaging | |||
|
| |||
| Any moderate facet joint OA | 164 (84.1%) | 52 (91.2%) | 0.18 |
| Any severe facet joint OA | 91 (46.7%) | 36 (63.2%) | 0.03† |
| No joints with severe OA | 104 (53.3%) | 21 (36.8%) | |
| 1-2 joints with severe OA | 55 (28.2%) | 16 (28.1%) | 0.006†‡ |
| 3-8 joints with severe OA | 36 (18.5%) | 20 (35.1%) | |
| Any moderate DHL | 135 (70.3%) | 40 (70.2%) | 0.98 |
| Any severe DHL | 76 (39.6%) | 22 (38.6%) | 0.89 |
| No levels with severe DHL | 116 (60.4%) | 35 (61.4%) | |
| 1 level with severe DHL | 55 (28.6%) | 13 (22.8%) | 0.72‡ |
| 2-4 levels with severe DHL | 21 (10.9%) | 9 (15.8%) | |
Mean (standard deviation) or N (%)
Statistically significant (p ≤ 0.05)
chi-square test for trend
Table 4 presents odds ratios (ORs) and 95% confidence intervals (95% CI) for associations between predictor variables and frequent LBP. Retirement and working/volunteering status were highly intercorrelated, and therefore only retirement status was included in the multivariable analyses. In the core multivariable model including the sociodemographic factors of age ≥75, retirement, and living alone, retirement showed a weak and non-significant trend towards an association with back pain (odds ratio [OR] 1.82 [95% confidence interval [95% CI] 0.95-3.48]), but other variables showed no independent association with back pain (data not shown). When the variables of any severe facet joint OA and any severe disc height narrowing were added to the core model, the presence of any severe facet joint OA was significantly and independently associated with back pain (OR 2.15 [95% CI 1.13-4.08]), but no association was seen for disc height narrowing. When the variables of number of joints with severe facet joint OA and number of spinal levels with severe disc height narrowing were added to the core model, the number of joints with severe OA was significantly and independently associated with back pain (OR 1.22 [95% CI 1.04-1.42]), but no such association was seen for number of spinal levels with severe disc height narrowing. In secondary multivariable analyses, when adjusting for factors based on conceptual importance alone (age, sex, BMI, and education), any severe facet joint OA (OR 1.96 [95% CI 1.01-3.77]), and number of joints with severe OA (OR 1.21 [95% CI 1.03-1.42]), were significantly associated with back pain, although the corresponding measures for disc height narrowing were not. Last, in sensitivity analyses to examine the effects of imprecise temporal concordance between the date of the CT scans and the clinical examination (during which back pain frequency in the prior 12 months was assessed), we found no material differences in the association between facet joint OA and back pain when including the covariate of time delay between CT scan and clinical examination, or when restricting the analyses to those participants with less than a 20 month (mean) delay between the CT scan and the clinical examination (data not shown).
Table 4. Multivariable Analysis of Associations Between Spinal Degeneration on CT Imaging and Frequent Back Pain.
| Model 1- Severity of Facet Joint OA and Disc Height Narrowing |
Model 2- Extent of Facet Join OA and Disc Height Narrowing |
|
|---|---|---|
| Odds Ratio (95% Confidence Interval) | ||
|
| ||
| Sociodemographics | ||
|
| ||
| Age ≥ 75 years | 1.50 (0.74-3.04) | 1.42 (0.70-2.88) |
| Living alone | 1.82 (0.79-4.21) | 1.71 (0.74-3.96) |
| Retired | 1.88 (0.97-3.66) | 1.80 (0.93-3.47) |
|
| ||
| Spinal Degeneration on CT Imaging | ||
|
| ||
| Any severe facet joint OA | 2.15 (1.13-4.08)* | - |
| # of joints with severe OA | - | 1.22 (1.04-1.42)* |
| Any severe disc height narrowing |
0.69 (0.36-1.33) | - |
| # of levels with severe narrowing |
- | 0.89 (0.59-1.34) |
statistically significant (p ≤ 0.05)
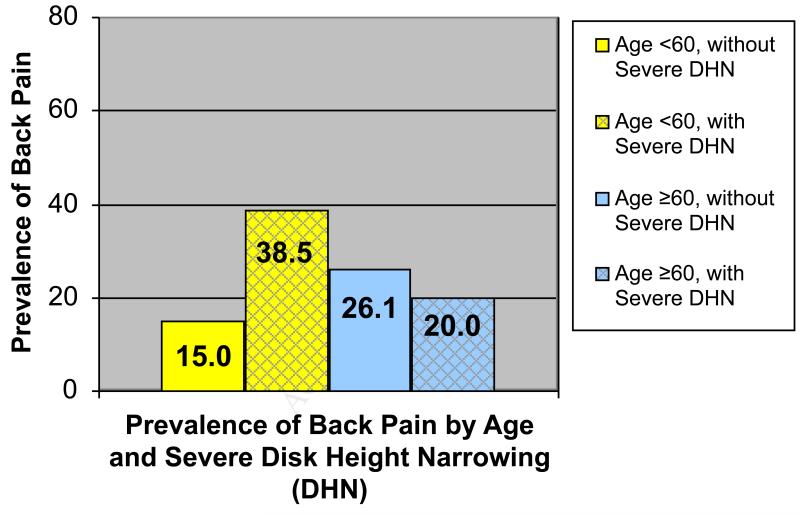
In post-hoc analyses, we examined relevant interactions between age and features of severe spinal degeneration by addition of interaction terms to the multivariable models from Table 3. In order to examine whether relationships between facet joint OA and back pain would be stronger in older adults, we tested for an interaction between facet joint OA and age ≥ 75 years. We found no interaction between age and the presence of any severe facet joint OA, or the number of joints with severe facet joint OA (data not shown), indicating that facet joint OA was associated with back pain across the age spectrum of the sample. In order to examine whether relationships between disc height narrowing and back pain would be stronger in younger and middle-aged adults, we tested for an interaction between disc height narrowing and age ≥ 60 years. We found a statistically significant interaction between any severe disc height narrowing and age ≥ 60 (p=0.02), with a main effect for any severe disc height narrowing of OR 3.72 (95% CI 0.85-16.3). This interaction is depicted graphically in Figure 2, which shows that disc height narrowing is associated with back pain in participants < 60 years, but not in participants ≥ 60 years. We found a similar interaction between the number of spinal levels with severe disc height narrowing and age ≥ 60 (p=0.04), with disc height narrowing associated with back pain only in the younger group. Severe facet joint OA remained significantly associated with back pain in all models including an interaction term (data not shown).
Figure 2.
Prevalence of Back Pain by Age and Severe Disk Height Narrowing (DHN)
DISCUSSION
Severe facet joint OA was significantly associated with frequent back pain in this study of community-based US older adults, adjusting for sociodemographics and health factors, and disc height narrowing. Furthermore, a greater number of joints with severe facet joint OA conferred greater odds of having frequent back pain. Disc height narrowing was independently associated with back pain in younger adults < age 60 years, but not in older adults.
To our knowledge, this is the first study demonstrating a clear association between facet joint OA on advanced spinal imaging and the presence of back pain. Prior studies examining this relationship have either found no association[8, 10], or associations that were not statistically significant[9]. Our study had various distinguishing features from prior work that may explain our positive findings and our ability to detect an association between facet joint OA and back pain. First and most importantly is the substantially older age of our study sample, including participants of mean age 67 years, as compared to prior studies where mean age ranged between 36 to 53 years. Since OA is an age-related degenerative process, it follows logically that advanced OA might be associated with pain in older adults, but not in younger adults[28, 29]. Indeed, prior studies using comparative diagnostic anesthetic blocks to identify the source of back pain have demonstrated that the proportion of back pain attributable to the facet joints is high in older adults, and low in younger adults [13, 14]. Second, our study applied thresholds for facet joint OA severity that identified severe OA in particular, inspired by findings from the knee OA literature, where a closer association between radiographic OA and pain is often seen in the setting of more severe radiographic changes[11, 30, 31]. Earlier studies, including work from our group conducted in another sample of Framingham participants[10], used thresholds of mild or moderate facet joint OA[8, 9]. This is likely inappropriate, since mild facet joint OA is essentially ubiquitous by middle age[32-34], and moderate facet joint OA is nearly so[10, 34]. Third, our study used a well-characterized and reliable scale for facet joint OA, in contrast to some earlier studies[8, 9].
Various prior studies have reported associations between disc height narrowing on advanced spinal imaging and back pain, and these have largely included samples of younger and middle-aged adults [35-37]. A noteworthy finding of this study was the association between disc height narrowing and back pain in adults < 60 years, but not in older adults. This observation supports the view held by some clinicians that discogenic back pain predominates in the young and middle-aged, but may become less symptomatic (or ‘burn out’) for individuals over the course of time[38]. This hypothesis has been difficult to test empirically due to the paucity of prior longitudinal imaging studies of back pain that include both middle-age and elderly persons. Furthermore, the overwhelming majority of prior cross-sectional studies using advanced spinal imaging such as CT or MRI examine only the anterior spinal structures of the intervertebral discs and endplates in young to middle-aged adults-not including older individuals [39]. Our data suggest the possibility that nonspecific back pain may shift from being discogenic-predominant in middle age to facetogenic-predominant in older adults, and this speculation warrants examination in future research.
Our study has other features that distinguish it from earlier works. Studies attempting to link spinal pain to specific posterior spinal structures on imaging (such as facet joint OA) generally come in two categories: 1) examinations of associations between imaging findings and spinal pain (including subjects with and without pain[8-10]), or 2) examinations of associations between imaging findings and the results of diagnostic anesthetic blocks to spinal structures (including only subjects with pain, usually from clinical convenience samples[7, 40]). Our study falls into the former category. We view this as a study strength, in light of continuing controversy regarding the validity of comparative diagnostic blocks[41]. In addition, we included both assessments of posterior spinal structure degeneration (facet joint OA) and anterior spinal structure degeneration (disc height narrowing) in the same multivariable models. Such an approach has been suggested since disc height narrowing might serve as a surrogate for facet joint OA when only the anterior structures are taken into account[42, 43].
Our study detected a modest magnitude association between facet joint OA and back pain (OR 2.2), which is generally comparable to odds ratio point estimates ranging from 2.0 – 2.5 for the most commonly studied parameters of intervertebral disk degeneration on imaging, including disc height narrowing, anular tears, and others[35, 39]. Similar to the case of both disc degeneration and extremity OA, however, the presence of any severe facet joint OA has limited discriminatory capability: many people with severe facet joint OA have no back pain, and some with back pain have no severe facet joint OA. This does not mean, however, that facet joint OA is not a potential cause of back pain. In fact, modest associations between spinal pathoanatomy and back pain should be expected due to the myriad confounding factors also contributing to the highly subjective experience of pain, including genetics, sociocultural factors, pain beliefs, mood, and other factors[44-47]. Our study, like the majority of prior imaging studies of back pain[48], accounted for only some of these potential confounding factors. On the contrary, our results showing significant associations between both severity and extent of facet joint OA and back pain provide some preliminary support for a causal link worthy of further examination in longitudinal studies.
Some limitations of our study are worthy of mention. First, we used a general back pain question which did not specify locations of lumbar pain corresponding to the levels that were imaged by CT (L2-S1). Therefore, our definition of frequent back pain may include not only lumbar pain, but also thoracic pain, which is prevalent in 2-6% of older adults[49]. Second, our study lacked precise concordance between the timing of CT scans and assessment of back pain frequency. Given that quantitative changes in lumbar spinal degeneration on advanced imaging are less than 1-2 % per year[50], we would expect any delay between CT scan and assessment of back pain to result in low rates of misclassification, which is supported by the results of our sensitivity analyses. Importantly, any misclassification in back pain locations or delays between imaging and pain assessments would be expected to bias towards the null, and would not explain the positive associations between facet joint OA and back pain detected in this study. Third, our imaging assessments utilized CT, a modality which is optimal for the cardinal features of facet joint OA (joint space narrowing, articular process hypertrophy, osteophytosis, and sclerosis) [13], but may be inferior for visualization of secondary features of facet joint OA, including joint effusions and articular process bone marrow lesions[51]. However, CT is currently not recommended as the first choice for advanced spinal imaging in situations where MRI is available, due in part to the known risks of ionizing radiation. MRI assessments of facet joint OA show moderate agreement with CT assessments of facet joint OA[19], but it remains to be seen whether severe facet joint OA on MRI associates with back pain in older adults in the manner seen here when using CT. Of note, our CT reads did not assess the L1-L2 spinal level, in contrast to most prior lumbar imaging studies, which include the entire lumbar region. Fourth, sample size in this study was not determined in advance based on power calculations related to the main research question pursued here. Nevertheless, the fact that we detected statistically significant results would suggest against type II error. Fifth, the cross-sectional nature of our study makes identifying potential confounding factors on conceptual grounds especially challenging, since temporal order between many of our measures cannot be determined. Future longitudinal studies of severe facet joint OA and associations with back pain are needed.
In conclusion, the results of this study demonstrate a significant but modest association between the presence and extent of severe facet joint OA on CT imaging and back pain in a sample of community-based older adults, independent of sociodemographics, health factors, and disc height narrowing. Further research is needed to determine whether imaging of facet joint OA may have a role in refining back pain case definition or directing back pain treatment for older adults.
ACKNOWLEDGEMENTS
We would like to thank the participants of the Framingham Heart Study. This manuscript was not prepared in collaboration with investigators of the Framingham Heart Study and does not necessarily reflect the opinions or conclusions of the Framingham Heart Study or the NHLBI.
ROLE OF FUNDING SOURCES:
From the Framingham Heart Study of the National Heart Lung and Blood Institute of the National Institutes of Health and Boston University School of Medicine. The National Heart, Lung and Blood Institute’s Framingham Heart Study contract (No. N01-HC-25195) supported the recruitment, enrollment, and examination of the Offspring and Third Generation Cohorts and the computed tomography scans. Dr. Suri and this research were funded by the Rehabilitation Medicine Scientist Training Program (RMSTP) and the National Institutes of Health (K12 HD 01097), with supplemental funding from the New England Baptist Hospital Research Funding Award and the Elizabeth Stent Fund. Dr. Katz was funded in part by NIH/NIAMS K24 AR 02123 and NIH/NIAMS P60 AR 47782. Dr. Hunter is funded by an Australian Research Council Future Fellowship.
Appendix 1. Framingham Scale for Lumbar Facet Joint Osteoarthritis*
| Joint space narrowing (JSN) |
Osteophytosis of articular processes |
Hypertrophy of articular processes |
Sclerosis | Subchondral erosions |
Subchondral cysts |
Joint space vacuum phenomenon |
|
|---|---|---|---|---|---|---|---|
| Grade I (Normal) | Joint space >2mm (no JSN) |
None or possible small osteophytes |
None | None or doubtful |
None | None | None |
| Grade II (Mild) | Joint space 1-2 mm |
Definite small osteophytes |
Mild | Definite | None | None | None |
| Grade III (Moderate) | Joint space <1 mm |
Moderate osteophytes |
Moderate | Definite | Mild | Mild | Any |
| Grade IV (Severe) | Bone-on-bone | Large osteophytes | Severe | Definite | Severe | Severe | Any |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONTRIBUTIONS
PS was involved with study concept and design, acquisition of data, analysis of data, interpretation of data, and drafting of the manuscript. DJH was involved with study concept and design and manuscript preparation. JR was involved with study concept, design, and manuscript preparation. AG was involved with study design, acquisition of data, and manuscript preparation. JNK was involved with study design, analysis of data, interpretation of data, and manuscript preparation. All authors were involved with critical revision of the manuscript for important intellectual content and approved the final version of the manuscript.
COMPETING INTERESTS:
None of the authors have received any financial support or other benefits from commercial sources for the work reported on in the manuscript, or have any other financial interests, which could create a potential conflict of interest or the appearance of a conflict of interest with regard to the work.
REFERENCES
- 1.Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine. 2006;31:2724–2727. doi: 10.1097/01.brs.0000244618.06877.cd. [DOI] [PubMed] [Google Scholar]
- 2.Deyo RA, Mirza SK, Turner JA, Martin BI. Overtreating chronic back pain: time to back off? J Am Board Fam Med. 2009;22:62–68. doi: 10.3122/jabfm.2009.01.080102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88(Suppl 2):21–24. doi: 10.2106/JBJS.E.01273. [DOI] [PubMed] [Google Scholar]
- 4.Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain. 2000;84:95–103. doi: 10.1016/S0304-3959(99)00187-6. [DOI] [PubMed] [Google Scholar]
- 5.van Tulder MW, Koes BW, Bouter LM. A cost-of-illness study of back pain in The Netherlands. Pain. 1995;62:233–240. doi: 10.1016/0304-3959(94)00272-G. [DOI] [PubMed] [Google Scholar]
- 6.Manchikanti L, Pampati V, Singh V, Boswell MV, Smith HS, Hirsch JA. Explosive growth of facet joint interventions in the Medicare population in the United States: a comparative evaluation of 1997, 2002, and 2006 data. BMC Health Serv Res. 2010;10:84. doi: 10.1186/1472-6963-10-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carrera GF, Williams AL. Current concepts in evaluation of the lumbar facet joints. Crit Rev Diagn Imaging. 1984;21:85–104. [PubMed] [Google Scholar]
- 8.Kjaer P, Leboeuf-Yde C, Korsholm L, Sorensen JS, Bendix T. Magnetic resonance imaging and low back pain in adults: a diagnostic imaging study of 40-year-old men and women. Spine. 2005;30:1173–1180. doi: 10.1097/01.brs.0000162396.97739.76. [DOI] [PubMed] [Google Scholar]
- 9.Savage RA, Whitehouse GH, Roberts N. The relationship between the magnetic resonance imaging appearance of the lumbar spine and low back pain, age and occupation in males. Eur Spine J. 1997;6:106–114. doi: 10.1007/BF01358742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalichman L, Li L, Kim DH, Guermazi A, Berkin V, O’Donnell CJ, et al. Facet joint osteoarthritis and low back pain in the community-based population. Spine (Phila Pa 1976) 2008;33:2560–2565. doi: 10.1097/BRS.0b013e318184ef95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord. 2008;9:116. doi: 10.1186/1471-2474-9-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duncan R, Peat G, Thomas E, Hay E, McCall I, Croft P. Symptoms and radiographic osteoarthritis: not as discordant as they are made out to be? Ann Rheum Dis. 2007;66:86–91. doi: 10.1136/ard.2006.052548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gellhorn AC, Katz JN, Suri P. Osteoarthritis of the spine: the facet joints. Nat Rev Rheumatol. 2012 doi: 10.1038/nrrheum.2012.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manchikanti L, Pampati V, Rivera J, Fellows B, Beyer C, Damron K. Role of facet joints in chronic low back pain in the elderly: a controlled comparative prevalence study. Pain Pract. 2001;1:332–337. doi: 10.1046/j.1533-2500.2001.01034.x. [DOI] [PubMed] [Google Scholar]
- 15.Feinleib M, Kannel WB, Garrison RJ, McNamara PM, Castelli WP. The Framingham Offspring Study. Design and preliminary data. Prev Med. 1975;4:518–525. doi: 10.1016/0091-7435(75)90037-7. [DOI] [PubMed] [Google Scholar]
- 16.Hoffmann U, Siebert U, Bull-Stewart A, Achenbach S, Ferencik M, Moselewski F, et al. Evidence for lower variability of coronary artery calcium mineral mass measurements by multi-detector computed tomography in a community-based cohort--consequences for progression studies. Eur J Radiol. 2006;57:396–402. doi: 10.1016/j.ejrad.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 17.Parikh NI, Hwang SJ, Larson MG, Cupples LA, Fox CS, Manders ES, et al. Parental occurrence of premature cardiovascular disease predicts increased coronary artery and abdominal aortic calcification in the Framingham Offspring and Third Generation cohorts. Circulation. 2007;116:1473–1481. doi: 10.1161/CIRCULATIONAHA.107.705202. [DOI] [PubMed] [Google Scholar]
- 18.Pathria M, Sartoris DJ, Resnick D. Osteoarthritis of the facet joints: accuracy of oblique radiographic assessment. Radiology. 1987;164:227–230. doi: 10.1148/radiology.164.1.3588910. [DOI] [PubMed] [Google Scholar]
- 19.Weishaupt D, Zanetti M, Boos N, Hodler J. MR imaging and CT in osteoarthritis of the lumbar facet joints. Skeletal Radiol. 1999;28:215–219. doi: 10.1007/s002560050503. [DOI] [PubMed] [Google Scholar]
- 20.Raininko R, Manninen H, Battie MC, Gibbons LE, Gill K, Fisher LD. Observer variability in the assessment of disc degeneration on magnetic resonance images of the lumbar and thoracic spine. Spine (Phila Pa 1976) 1995;20:1029–1035. doi: 10.1097/00007632-199505000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Videman T, Battie MC, Gill K, Manninen H, Gibbons LE, Fisher LD. Magnetic resonance imaging findings and their relationships in the thoracic and lumbar spine. Insights into the etiopathogenesis of spinal degeneration. Spine. 1995;20:928–935. doi: 10.1097/00007632-199504150-00009. [DOI] [PubMed] [Google Scholar]
- 22.Videman T, Battie MC, Ripatti S, Gill K, Manninen H, Kaprio J. Determinants of the progression in lumbar degeneration: a 5-year follow-up study of adult male monozygotic twins. Spine. 2006;31:671–678. doi: 10.1097/01.brs.0000202558.86309.ea. [DOI] [PubMed] [Google Scholar]
- 23.Suri P, Hunter DJ, Rainville J, Guermazi A, Katz JN. Quantitative assessment of abdominal aortic calcification and associations with lumbar intervertebral disc height loss: the Framingham Study. Spine J. 2012;12:315–323. doi: 10.1016/j.spinee.2012.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Schepper EI, Damen J, van Meurs JB, Ginai AZ, Popham M, Hofman A, et al. The association between lumbar disc degeneration and low back pain: the influence of age, gender, and individual radiographic features. Spine (Phila Pa 1976) 2010;35:531–536. doi: 10.1097/BRS.0b013e3181aa5b33. [DOI] [PubMed] [Google Scholar]
- 25.Docking RE, Fleming J, Brayne C, Zhao J, Macfarlane GJ, Jones GT. Epidemiology of back pain in older adults: prevalence and risk factors for back pain onset. Rheumatology. 2011;50:1645–1653. doi: 10.1093/rheumatology/ker175. [DOI] [PubMed] [Google Scholar]
- 26.Peat G, Thomas E, Handy J, Croft P. Social networks and pain interference with daily activities in middle and old age. Pain. 2004;112:397–405. doi: 10.1016/j.pain.2004.09.029. [DOI] [PubMed] [Google Scholar]
- 27.Helliwell JF, Putnam RD. The social context of well-being. Philosophical transactions of the Royal Society of London. Series B, Biological sciences. 2004;359:1435–1446. doi: 10.1098/rstb.2004.1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lethbridge-Cejku M, Scott WW, Jr., Reichle R, Ettinger WH, Zonderman A, Costa P, et al. Association of radiographic features of osteoarthritis of the knee with knee pain: data from the Baltimore Longitudinal Study of Aging. Arthritis Care Res. 1995;8:182–188. doi: 10.1002/art.1790080311. [DOI] [PubMed] [Google Scholar]
- 29.Borenstein D. Does osteoarthritis of the lumbar spine cause chronic low back pain? Curr Pain Headache Rep. 2004;8:512–517. doi: 10.1007/s11916-004-0075-z. [DOI] [PubMed] [Google Scholar]
- 30.Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30:914–918. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 31.Hochberg MC, Lawrence RC, Everett DF, Cornoni-Huntley J. Epidemiologic associations of pain in osteoarthritis of the knee: data from the National Health and Nutrition Examination Survey and the National Health and Nutrition Examination-I Epidemiologic Follow-up Survey. Semin Arthritis Rheum. 1989;18:4–9. doi: 10.1016/0049-0172(89)90008-5. [DOI] [PubMed] [Google Scholar]
- 32.Simon P, Orias AA, Andersson GB, An HS, Inoue N. In Vivo Topographic Analysis of Lumbar Facet Joint Space Width Distribution in Healthy and Symptomatic Subjects. Spine (Phila Pa 1976) 2012 doi: 10.1097/BRS.0b013e3182552ec9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li J, Muehleman C, Abe Y, Masuda K. Prevalence of facet joint degeneration in association with intervertebral joint degeneration in a sample of organ donors. J Orthop Res. 2011;29:1267–1274. doi: 10.1002/jor.21387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tischer T, Aktas T, Milz S, Putz RV. Detailed pathological changes of human lumbar facet joints L1-L5 in elderly individuals. Eur Spine J. 2006;15:308–315. doi: 10.1007/s00586-005-0958-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Videman T, Battie MC, Gibbons LE, Maravilla K, Manninen H, Kaprio J. Associations between back pain history and lumbar MRI findings. Spine. 2003;28:582–588. doi: 10.1097/01.BRS.0000049905.44466.73. [DOI] [PubMed] [Google Scholar]
- 36.Livshits G, Popham M, Malkin I, Sambrook PN, Macgregor AJ, Spector T, et al. Lumbar disc degeneration and genetic factors are the main risk factors for low back pain in women: the UK Twin Spine Study. Ann Rheum Dis. 2011;70:1740–1745. doi: 10.1136/ard.2010.137836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cheung KM, Karppinen J, Chan D, Ho DW, Song YQ, Sham P, et al. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine (Phila Pa 1976) 2009;34:934–940. doi: 10.1097/BRS.0b013e3181a01b3f. [DOI] [PubMed] [Google Scholar]
- 38.Bendix T, Kjaer P, Korsholm L. Burned-out discs stop hurting: fact or fiction? Spine (Phila Pa 1976) 2008;33:E962–967. doi: 10.1097/BRS.0b013e31818804b3. [DOI] [PubMed] [Google Scholar]
- 39.Chou D, Samartzis D, Bellabarba C, Patel A, Luk KD, Kisser JM, et al. Degenerative magnetic resonance imaging changes in patients with chronic low back pain: a systematic review. Spine (Phila Pa 1976) 2011;36:S43–53. doi: 10.1097/BRS.0b013e31822ef700. [DOI] [PubMed] [Google Scholar]
- 40.Schwarzer AC, Wang SC, O’Driscoll D, Harrington T, Bogduk N, Laurent R. The ability of computed tomography to identify a painful zygapophysial joint in patients with chronic low back pain. Spine (Phila Pa 1976) 1995;20:907–912. doi: 10.1097/00007632-199504150-00005. [DOI] [PubMed] [Google Scholar]
- 41.Carragee EJ, Haldeman S, Hurwitz E. The pyrite standard: the Midas touch in the diagnosis of axial pain syndromes. Spine J. 2007;7:27–31. doi: 10.1016/j.spinee.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 42.Hassett G, Hart DJ, Manek NJ, Doyle DV, Spector TD. Risk factors for progression of lumbar spine disc degeneration: the Chingford Study. Arthritis Rheum. 2003;48:3112–3117. doi: 10.1002/art.11321. [DOI] [PubMed] [Google Scholar]
- 43.Scheele J, de Schepper EI, van Meurs JB, Hofman A, Koes BW, Luijsterburg PA, et al. Association between spinal morning stiffness and lumbar disc degeneration: the Rotterdam Study. Osteoarthritis Cartilage. 2012;20:982–987. doi: 10.1016/j.joca.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 44.Battie MC, Videman T, Levalahti E, Gill K, Kaprio J. Heritability of low back pain and the role of disc degeneration. Pain. 2007;131:272–280. doi: 10.1016/j.pain.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 45.Chou R, Shekelle P. Will this patient develop persistent disabling low back pain? Jama. 2010;303:1295–1302. doi: 10.1001/jama.2010.344. [DOI] [PubMed] [Google Scholar]
- 46.Rainville J, Smeets RJ, Bendix T, Tveito TH, Poiraudeau S, Indahl AJ. Fear-avoidance beliefs and pain avoidance in low back pain--translating research into clinical practice. Spine J. 2011;11:895–903. doi: 10.1016/j.spinee.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 47.Neogi T, Felson D, Niu J, Nevitt M, Lewis CE, Aliabadi P, et al. Association between radiographic features of knee osteoarthritis and pain: results from two cohort studies. Bmj. 2009;339:b2844. doi: 10.1136/bmj.b2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hancock MJ, Maher CG, Laslett M, Hay E, Koes B. Discussion paper: what happened to the ‘bio’ in the bio-psycho-social model of low back pain? Eur Spine J. 2011;20:2105–2110. doi: 10.1007/s00586-011-1886-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hartvigsen J, Nielsen J, Kyvik KO, Fejer R, Vach W, Iachine I, et al. Heritability of spinal pain and consequences of spinal pain: a comprehensive genetic epidemiologic analysis using a population-based sample of 15,328 twins ages 20-71 years. Arthritis Rheum. 2009;61:1343–1351. doi: 10.1002/art.24607. [DOI] [PubMed] [Google Scholar]
- 50.Videman T, Battie MC, Parent E, Gibbons LE, Vainio P, Kaprio J. Progression and determinants of quantitative magnetic resonance imaging measures of lumbar disc degeneration: a five-year follow-up of adult male monozygotic twins. Spine (Phila Pa 1976) 2008;33:1484–1490. doi: 10.1097/BRS.0b013e3181753bb1. [DOI] [PubMed] [Google Scholar]
- 51.Suri P, Dharamsi AS, Gaviola G, Isaac Z. Association of Facet Joint Bone Marrow Lesions and Other Features with Low Back Pain: A Pilot Study. PM&R. 2012 doi: 10.1016/j.pmrj.2012.09.002. [DOI] [PubMed] [Google Scholar]