Abstract
PURPOSE
Statins reduce the risk of mortality and coronary artery disease in individuals at high cardiovascular risk. Using nationally representative data, we examined the relationships between statin use and cardiovascular risk, diagnosis of hyperlipidemia, and other risk factors.
METHODS
We analyzed data from the 2010 Medical Expenditure Panel Survey, a nationally representative survey of the US civilian noninstitutionalized population. The study sample had a total of 16,712 individuals aged 30 to 79 years. Those who reported filling at least 2 statin prescriptions were classified as statin users. We created multiple logistic regression models for statin use as the dependent variable, with cardiovascular risk factors and sociodemographic factors as independent variables.
RESULTS
Overall, 58.2% (95% CI, 54.6%–61.7%) of individuals with coronary artery disease and 52.0% (95% CI, 49.4%–54.6%) of individuals with diabetes aged older than 40 years were statin users. After adjusting for cardiovascular risk factors and sociodemographic factors, the probability of being on a statin was significantly higher among individuals with both hyperlipidemia and coronary artery disease, at 0.44 (95% CI, 0.40–0.48), or hyperlipidemia only, at 0.32 (95% CI, 0.30–0.33), than among those with coronary artery disease only, at 0.11 (95% CI, 0.07–0.15). A similar pattern was seen in people with diabetes.
CONCLUSIONS
In this nationally representative sample, many people at high risk for cardiovascular events, including those with coronary artery disease, diabetes, or both, were not receiving statins despite evidence that these agents reduce adverse events. This undertreatment appears to be related to placing too much emphasis on hyperlipidemia and not enough on cardiovascular risk. Recently released guidelines from the American College of Cardiology and the American Heart Association offer an opportunity to improve statin use by focusing on cardiovascular risk instead of lipid levels.
Keywords: cardiovascular: coronary artery disease, cardiovascular: hyperlipidemia, endocrinology: diabetes, primary care issues
INTRODUCTION
The recently released cholesterol guidelines from the American College of Cardiology (ACC) and the American Heart Association (AHA)1 represent a shift away from a focus on treating to a target low-density lipoprotein (LDL) level2 and toward a focus on minimizing global cardiovascular risk. These changes are driven by the evidence that the benefits of statins accrue to those at high cardiovascular risk regardless of their cholesterol level.3–8 Statins, also known as 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors, are effective medications for reducing the risk of death and future cardiovascular disease in those with known coronary heart disease.9 In individuals aged more than 40 years with diabetes mellitus, the use of statins has been shown to decrease cardiovascular events and likely reduce mortality.7,8
The new ACC-AHA guidelines substantially broadened the number of individuals for whom statins are recommended, primarily by broadening the eligible population to lower levels of cardiovascular risk.10 Most newly eligible individuals in the guidelines are those who do not have a diagnosis of coronary artery disease. Benefits from statins in this primary prevention population in terms of a reduction in adverse cardiovascular events and in mortality are controversial and at best small.11–14 Although the risks of treatment are similar, individuals with high cardiovascular risk have a much lower number needed to treat than individuals with low risk regardless of cholesterol values. This marked difference in treatment effect according to baseline risk15 suggests that cardiovascular risk rather than the results of a cholesterol test should be the driving force behind the decision to prescribe statins.
Previous studies have shown increasing use of statins in the US population.16 Others have demonstrated suboptimal statin use among high-risk populations.17–20 Many of these studies have been limited in generalizability, however.18–20 A recent national study provided evidence that physicians give great consideration to patients’ lipid levels and little to their cardiovascular risk when recommending treatment.21 That study was limited, however, by its hypothetical case scenario methodology as well as its 30% response rate. A previous study did identify a lack of prescribing to high-risk patients, especially those without a diagnosis of hyperlipidemia, but used data that were more than 10 years old.17 A more recent study of patients with coronary heart disease cared for in cardiology clinics identified a large number of patients with LDL levels of less than 100 mg/dL who were not treated with statins.18 No recent trials have investigated how cardiovascular risk and specific risk factors contribute to actual statin prescribing in a nationally representative sample. We therefore set out to estimate the relationships between statin use and cardiovascular risk, diagnosed hyperlipidemia, and other specific risk factors in a nationally representative sample.
METHODS
Study Design
We used data from the Medical Expenditure Panel Survey (MEPS) from 2010 in this cross-sectional analysis. MEPS is a nationally representative survey of the civilian noninstitutionalized population of the United States conducted by the Agency for Healthcare Research and Quality (AHRQ) and the National Center for Health Statistics.22 MEPS is a subsample of the National Health Interview Survey and includes about 15,000 households. There are 2 concurrent panels included yearly in the survey, which consists of 5 interviews over 2 years. MEPS uses a complex survey design including an oversampling of minorities and captures data on demographics, expenditures by payer and type, medical conditions, insurance coverage, and prescription drug information.
Study Population
The study population consisted of adults aged 30 to 79 years who did not have a contraindication to statin therapy (pregnancy or severe liver disease). We chose the upper age cutoff because of less clear evidence of clinical benefit after that age23,24 and more accurate risk prediction before that age.25
Study Measures
Primary Outcome
Statin users were defined as individuals who reported filling 2 or more statin prescriptions from a pharmacy during 2010. Prescription drug information is collected by surveyors during interviews and confirmed with pharmacy data. We selected 2 or more prescriptions to increase the likelihood of identifying people who regularly used statins. Statins were identified by both generic and trade names along with combination products. This analysis accounts for only reported prescriptions. The survey’s drug data has been found to have validity regardless of sociodemographics, especially for medications taken longer term.26
Diagnoses
MEPS identifies medical conditions through self-report or in association with a medical event such as a prescription or medical expenditure. Previous reports of national survey data have shown varying levels of agreement with the medical record,27 but agreement seems to be highest for chronic conditions.28 Conditions that are considered to be important in terms of expenditure, policy, or prevalence are considered priority conditions and are identified with the question, “Has person ever been told by a doctor or other healthcare professional that they have (condition)?”29 All conditions considered in this analysis were priority conditions with the exception of severe liver disease, peripheral arterial disease, and pregnancy. Additionally, condition information was identified from medical events using clinical classification codes, which are groupings of International Classification of Diseases, 9th Revision (ICD-9) codes. Severe liver disease, peripheral arterial disease, and pregnancy were identified with these codes. Women who reported a history of diabetes that was not associated with a medical event nor considered current were not considered to have diabetes given the risk of false-positives related to gestational diabetes. A comparison of MEPS medical condition estimates with population estimates30 is given in Supplemental Table 1.
Modified Cardiovascular Disease Risk Index
We used Framingham point scores31 to assign cardiovascular risk to individuals without coronary artery disease or diabetes. Points were assigned based on the known values for an individual’s sex, age, and tobacco use. As data showed only diagnosis of hypertension, not actual blood pressure, we assumed conservative values for systolic blood pressure. Individuals without a diagnosis were assumed to have a systolic blood pressure of less than 120 mm Hg, while those with a history of hypertension were assumed to be treated and have a systolic blood pressure between 130 and 139 mm Hg. Lipid values were not estimated, but instead added to the model that predicted statin use as an independent dichotomous covariate of hyperlipidemia.
Covariates
Sociodemographic data included age, race/ethnicity (white, black, Hispanic, Asian, or other), poverty category (poor, near poor, and low, middle, or high income), tobacco use, and insurance coverage (any private, public, or uninsured).
Statistical Analysis
We conducted 2 sets of analyses: 1 for the entire sample including individuals with high and low cardiovascular risk and 1 restricted to those without a diagnosis of heart disease or diabetes. We refer to the first set of analyses as the all-eligible analyses and to the second set as the primary prevention analyses. For each, we estimated a logistic regression model with statin use as the dichotomous outcome variable and controlling for potential confounding by age, sex, race/ethnicity, insurance status, poverty category, tobacco use, hyperlipidemia, hypertension, peripheral arterial disease, and history of a cerebrovascular accident. The all-eligible model also included diabetes and coronary artery disease as well as their respective interactions with hyperlipidemia as additional independent variables. Because the interaction terms were significant, we ran 2 logistic regression models, one each for individuals with and without hyperlipidemia. The first primary prevention model included the same covariates as the all-eligible model with the exception of the exclusion of coronary artery disease and diabetes. The second primary prevention model included the modified cardiovascular risk index described above as a predictor as well as 2 factor interaction terms between risk index and hyperlipidemia. This analysis controlled for race/ethnicity, insurance coverage, and poverty category, and included separate models for men and women because the risk indexes are not equivalent.
We used Stata version 12 (StataCorp) for analyses. Postprediction average marginal effects were used to determine the probability that individuals within certain subpopulations were statin users. Complex survey weighting was used in all statistical analyses with the exception of Hosmer-Lemeshow testing.
This study was judged to be exempt from ethical review by the University of Michigan Medical Investigational Review Board.
RESULTS
Study Sample and Bivariate Comparisons
The MEPS sample aged 30 to 79 years included 16,712 individuals. Hyperlipidemia had been diagnosed in 38.4% (95% CI, 37.5%–39.3%) of the sample, of whom 46.9% (95% CI, 45.2%–48.6%) were using a statin. Coronary artery disease was present in 8.1% (95% CI, 7.5%–8.7%) of the sample, of whom 58.2% (95% CI, 54.6%–61.7%) were using a statin. In individuals with coronary artery disease without a diagnosis of hyperlipidemia, 15.5% (95% CI, 10.9%–21.6%) were on a statin. Overall, 11.2% (95% CI, 10.6%–11.9%) of the sample had diabetes and were aged older than 40 years, and 52.0% (95% CI, 49.3%–54.6%) of those individuals were using a statin. Among individuals aged older than 40 years with diabetes who did not have a diagnosis of hyperlipidemia, 12.0% (95% CI, 8.8%–16.2%) were on a statin.
The unadjusted characteristics of the whole sample as well as among those with coronary heart disease and diabetes by statin use are given in Table 1. On a national level, an estimated 5.6 million (95% CI, 4.9–6.3 million) individuals with coronary artery disease and about 9.0 million (95% CI, 8.2–9.8 million) individuals with diabetes aged older than 40 years were not regularly using statins.
Table 1.
Characteristics of Study Sample and Subsamples of Individuals Aged 30 to 79 Years
| Characteristic | Overall Sample | Coronary Artery Disease | Diabetes and Aged >40 Years | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Total | On Statin | Not on Statin | Total | On Statin | Not on Statin | Total | On Statin | Not on Statin | |
| Individuals, No. | 16,712 | 2,799 | 13,913 | 1,304 | 694 | 608 | 2,016 | 992 | 1,019 |
| Weighted proportion, % | – | 18.8 (18.0–19.7) |
81.2 (80.3–82.0) |
– | 58.2 (54.6–61.7) |
41.8 (38.3–45.4) |
– | 52.0 (49.4–54.6) |
48.0 (45.4–50.6) |
| Population in millions, No. | 166 (159–173) |
31.2 (29.2–33.2) |
135 (129–140) |
13.4 (12.3–14.5) |
7.8 (7.0–8.6) |
5.6 (4.9–6.3) |
18.7 (17.3–20.0) |
9.7 (8.9–10.6) |
9.0 (8.2–9.8) |
| Age, y | 51.3 (51.0–51.6) |
61.1 (60.6–61.6)a |
49.0 (48.7–49.3)a |
62.9 (62.3–63.6) |
64.9 (64.1–65.7)a |
60.2 (59.1–61.4)a |
60.3 (59.6–60.9) |
61.8 (61.1–62.6)a |
58.5 (57.6–59.4)a |
| Sex, female, % | 50.8 (50.2–51.4) |
46.7 (44.8–48.7)b |
51.7 (50.9–52.5)b |
41.4 (38.4–44.5) |
37.8 (33.6–42.3)b |
46.4 (41.9–51.1)b |
49.3 (46.8–51.8) |
49.8 (46.0–53.6) |
48.8 (44.8–52.8) |
| Tobacco users, % | 18.6 (17.7–19.5) |
16.4 (14.8–18.2)b |
19.1 (18.1–20.1)b |
21.7 (18.5–25.3) |
19.7 (15.9–24.0)b |
24.7 (20.5–29.4)b |
17.0 (15.1–19.0) |
15.7 (13.4–18.4) |
18.3 (15.5–21.5) |
| Hypertension, % | 39.2 (38.1–40.3) |
70.7 (68.2–72.7)b |
31.9 (30.8–33.1)b |
80.3 (77.6–82.8) |
84.2 (80.6–87.4)b |
74.8 (70.7–78.5)b |
81.1 (78.8–83.1) |
86.0 (83.1–88.6)b |
75.7 (72.1–78.9)b |
| Hyperlipidemia, % | 38.4 (37.5–39.3) |
95.8 (94.8–96.6)b |
25.1 (24.3–26.0)b |
78.7 (76.2–81.1) |
94.3 (92.0–96.0)b |
57.1 (52.7–61.4)b |
77.4 (75.0–79.5) |
94.8 (92.7–96.3)b |
58.5 (54.7–62.3)b |
| Race/ethnicity, % | |||||||||
| White | 69.5 (67.6–71.3) |
77.8 (76.0–80.3)b |
67.5 (65.5–69.5)b |
74.9 (71.8–77.7) |
80.3 (76.7–83.4)b |
67.3 (62.1–72.1)b |
62.8 (59.4–66.1) |
67.3 (63.3–71.0)b |
58.0 (53.3–62.5)b |
| Black | 11.2 (10.1–12.5) |
9.4 (8.0–11.0) |
11.6 (10.4–13.0) |
11.5 (9.6–13.6) |
9.1 (6.9–12.1) |
14.8 (11.9–18.2) |
16.4 (14.0–19.0) |
14.4 (11.9–17.4) |
18.4 (15.2–21.5) |
| Hispanic | 12.8 (11.4–14.3) |
7.2 (6.1–8.5) |
14.1 (12.6–15.8) |
8.2 (6.4–10.5) |
5.4 (4.0–7.3) |
12.2 (8.9–16.3) |
13.0 (11.0–15.3) |
10.2 (8.1–12.7) |
16.9 (14.0–22.2) |
| Asian | 4.7 (3.9–5.6) |
3.6 (2.6–4.9) |
4.9 (4.2–5.9) |
2.7 (1.8–4.0) |
3.2 (2.1–4.9) |
1.9 (1.0–3.7) |
4.4 (3.4–5.7) |
4.9 (3.5–6.7) |
3.9 (2.8–5.5) |
| Other | 1.8 (1.4–2.3) |
2.0 (1.3–3.0) |
1.8 (1.4–2.2) |
2.7 (1.8–4.2) |
1.9 (1.0–3.8) |
3.9 (2.3–6.3) |
3.5 (2.4–4.8) |
3.2 (2.1–4.9) |
3.7 (2.4–5.8) |
| Insurance, % | |||||||||
| Any private | 70.7 (67.6–72.0) |
69.9 (67.4–72.3)b |
70.9 (69.5–72.3)b |
55.1 (51.3–58.9) |
59.7 (55.0–64.1)b |
48.8 (43.5–54.1)b |
60.6 (57.8–63.3) |
62.2 (58.4–65.9)b |
58.8 (54.9–62.6)b |
| Public | 15.6 (14.7–16.6) |
25.7 (23.6–27.9) |
13.3 (12.4–14.3) |
37.3 (34.0–40.8) |
35.8 (31.7–40.1) |
39.4 (34.9–44.2) |
30.5 (27.9–33.3) |
32.5 (29.2–36.0) |
28.4 (24.7–32.4) |
| None | 13.7 (12.8–14.6) |
4.4 (3.6–5.5) |
15.8 (14.8–16.9) |
7.6 (6.1–9.3) |
4.5 (3.1–6.7) |
11.8 (9.1–15.1) |
8.9 (7.5–10.6) |
5.3 (3.6–7.7) |
12.8 (10.7–15.3) |
Note: Values are mean (95% CI) or percentage (95% CI).
Difference between those on a statin and not on a statin was significant (P <.05) with the adjusted Wald test.
Difference between those on a statin and not on a statin was significant (P <.05) with the χ2 test.
Multivariate Comparisons
In the all-eligible models, stratified by hyperlipidemia, analyses showed that age, coronary artery disease, diabetes mellitus, and hypertension were significant predictors of statin use regardless of the presence of hyperlipidemia (Table 2). Peripheral arterial disease was significant only in the model restricted to individuals without hyperlipidemia, whereas sex was significant only in the model restricted to individuals with hyperlipidemia. Cerebrovascular disease and tobacco use were not significant in either model. The odds associated with coronary artery disease, diabetes, peripheral arterial disease, and hypertension were all lower among individuals with hyperlipidemia compared with those without hyperlipidemia.
Table 2.
Odds Ratios for Statin Use by Hyperlipidemia Status
| Characteristic | With Hyperlipidemia Odds Ratio (95% CI) | P Value | Without Hyperlipidemia Odds Ratio (95% CI) | P Value |
|---|---|---|---|---|
| Coronary artery disease | 1.94 (1.58–2.40) | <.001 | 11.10 (5.51–22.80) | <.001 |
| Diabetes | 1.90 (1.59–2.28) | <.001 | 8.56 (4.35–16.87) | <.001 |
| Hypertension | 1.35 (1.14–1.60) | .001 | 2.30 (1.29–4.11) | .005 |
| Cerebrovascular disease | 0.87 (0.64–1.17) | .36 | 0.59 (0.17–2.01) | .40 |
| Peripheral arterial disease | 1.04 (0.60–1.81) | .88 | 8.38 (2.71–25.93) | <.001 |
| Tobacco use | 0.98 (0.82–1.16) | .76 | 1.26 (0.60–2.65) | .53 |
| Sex (male) | 1.19 (1.04–1.37) | .01 | 1.47 (0.81–2.66) | .21 |
| Age (per year) | 1.05 (1.04–1.05) | <.001 | 1.06 (1.03–1.09) | <.001 |
Notes: An odds ratio exceeding 1 indicates higher likelihood of statin use. Odds ratios are adjusted for insurance status, race, and poverty category.
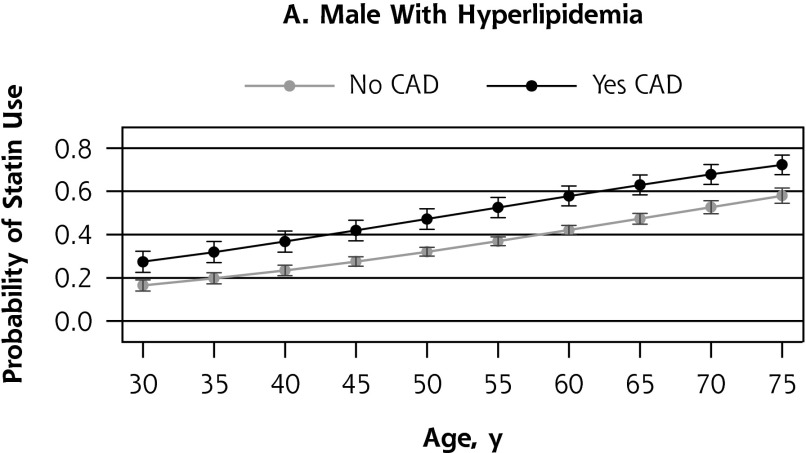
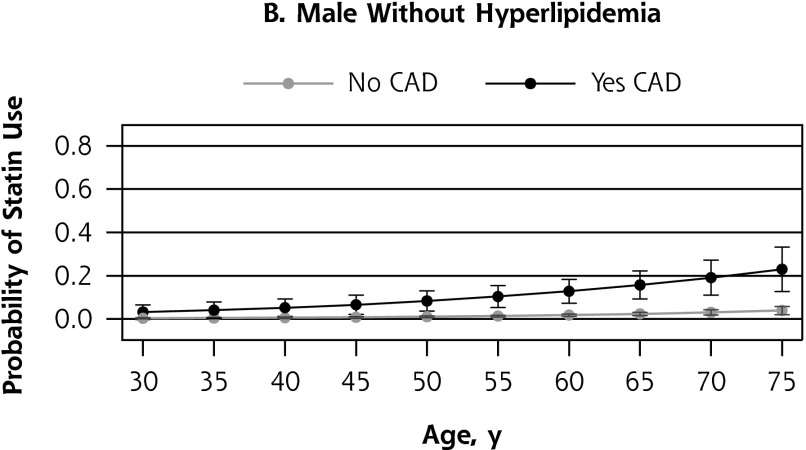
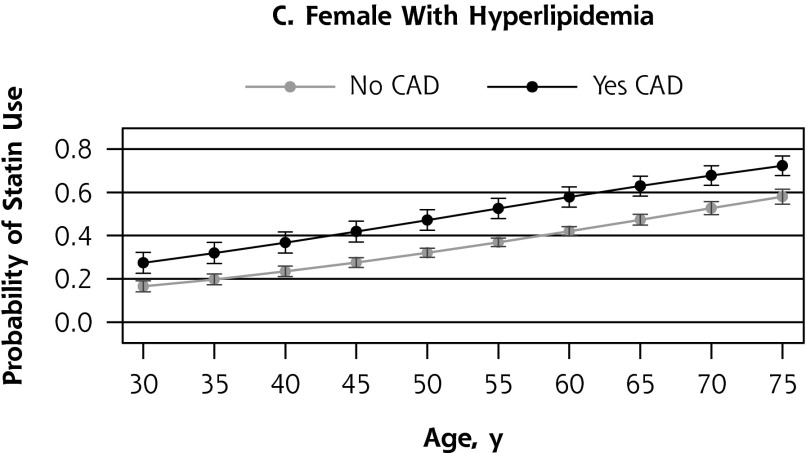
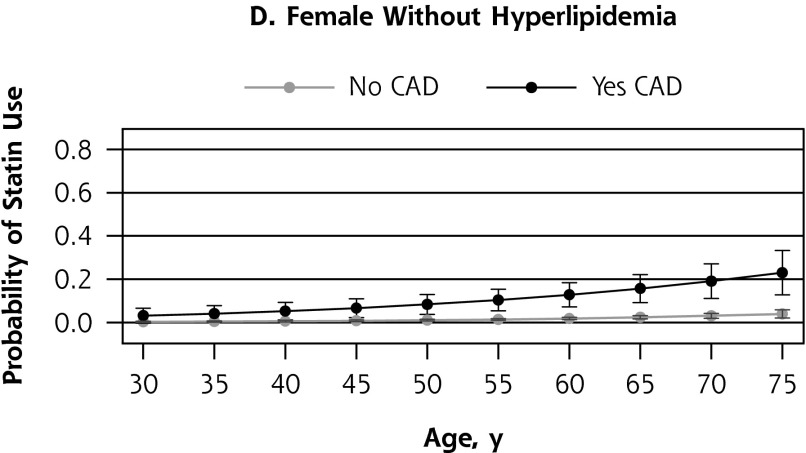
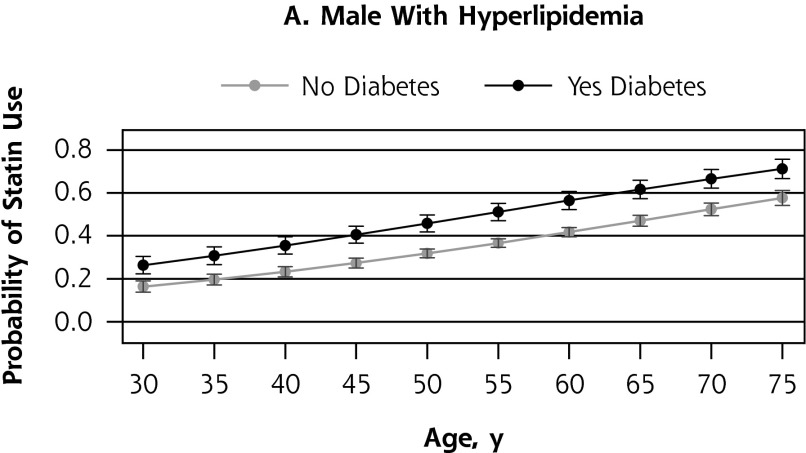
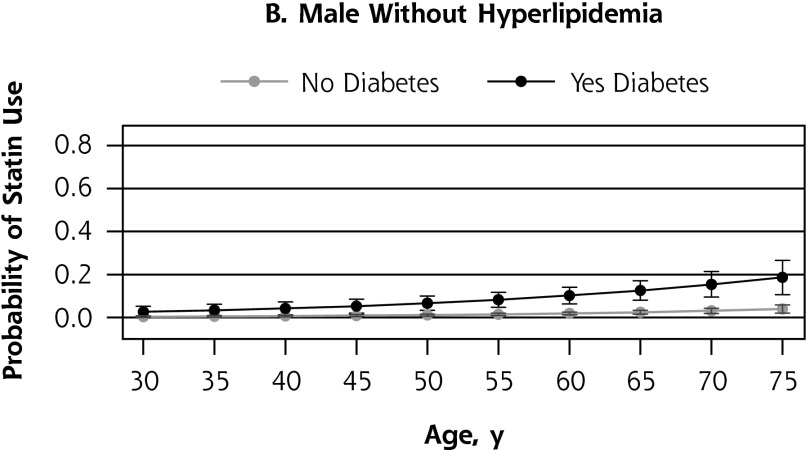
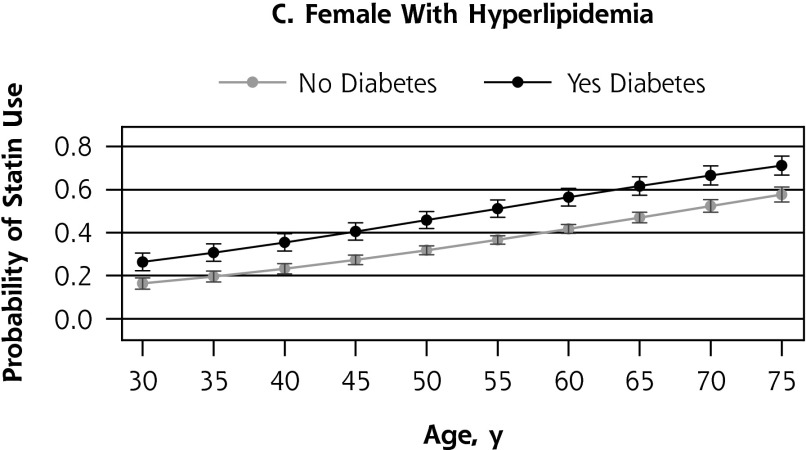
The model-predicted probability of statin use was 0.44 (95% CI, 0.40–0.48) for individuals with hyperlipidemia and coronary artery disease, compared with 0.32 (95% CI, 0.30–0.33) for those with only hyperlipidemia (P <.001). Individuals with coronary artery disease without hyperlipidemia had a probability of 0.11 (95% CI, 0.07–0.15) of being on a statin, which was significantly less than that of people with hyperlipidemia with or without coronary artery disease (P <.001) (Figure 1). Individuals with diabetes had similar findings to those with coronary artery disease (Figure 2).
Figure 1.
Probability of statin use by presence of coronary artery disease, according to sex and presence of hyperlipidemia.
CAD = coronary artery disease.
Figure 2.
Probability of statin use by presence of diabetes after age 40, according to sex and presence of hyperlipidemia.
In the first primary prevention logistic model, which included only individuals without a history of coronary artery disease or diabetes, while controlling for medical conditions and sociodemographics, results showed that increasing age, hyperlipidemia, hypertension, male sex, and history of cerebrovascular disease increased the likelihood of statin use (Table 3). Of the predictors of statin use, hyperlipidemia had a much greater association with statin use than the other predictors. Peripheral arterial disease and tobacco use were not significant. In the primary prevention cohort, individuals with a diagnosis of hyperlipidemia had a higher probability of being on a statin, at 0.30 (95% CI, 0.28–0.31), than individuals without a diagnosis of hyperlipidemia, at 0.006 (95% CI, 0.004–0.008) (P <.001).
Table 3.
Odds Ratios for Statin Use in Individuals Without Coronary Artery Disease or Diabetes
| Characteristic | Odds Ratio (95% CI) | P Value |
|---|---|---|
| Hyperlipidemia | 91.65 (60.27–139.36) | <.001 |
| Age (per year) | 1.06 (1.05–1.07) | <.001 |
| Hypertension | 1.35 (1.12–1.64) | .001 |
| Sex (male) | 1.33 (1.12–1.59) | .002 |
| Cerebrovascular disease | 1.52 (1.01–2.29) | .047 |
| Peripheral arterial disease | 1.59 (0.61–4.16) | .34 |
| Tobacco use | 1.00 (0.79–1.27) | .99 |
Notes: An odds ratio exceeding 1 indicates higher likelihood of statin use. Odds ratios are adjusted for insurance status, race, and poverty category.
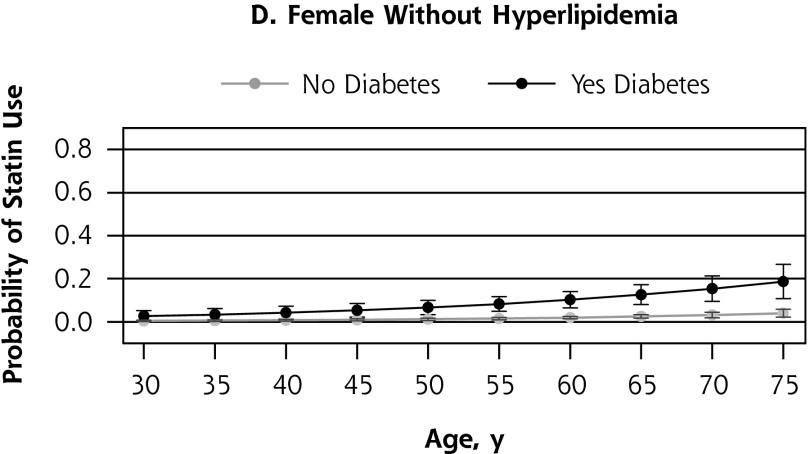
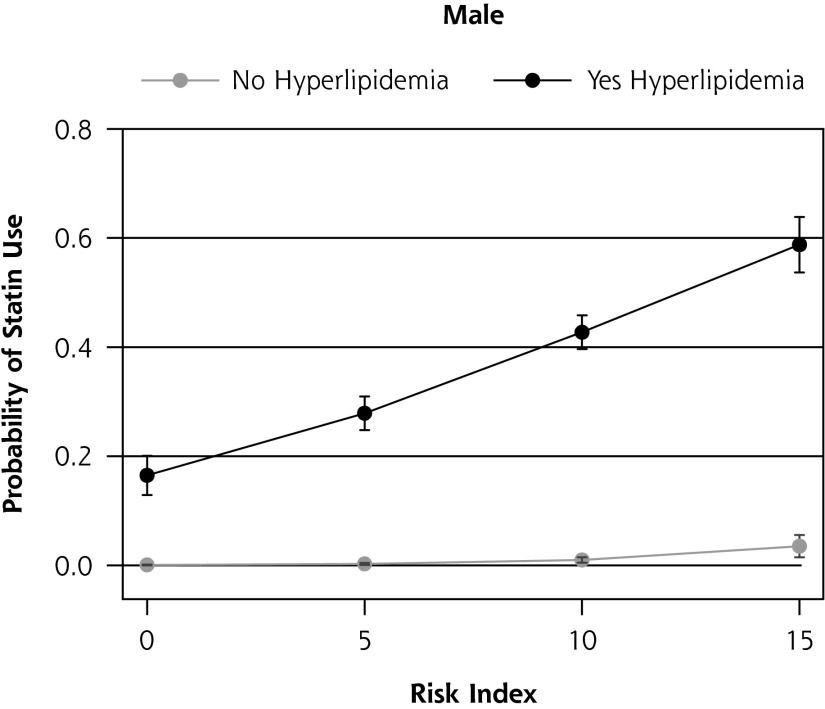
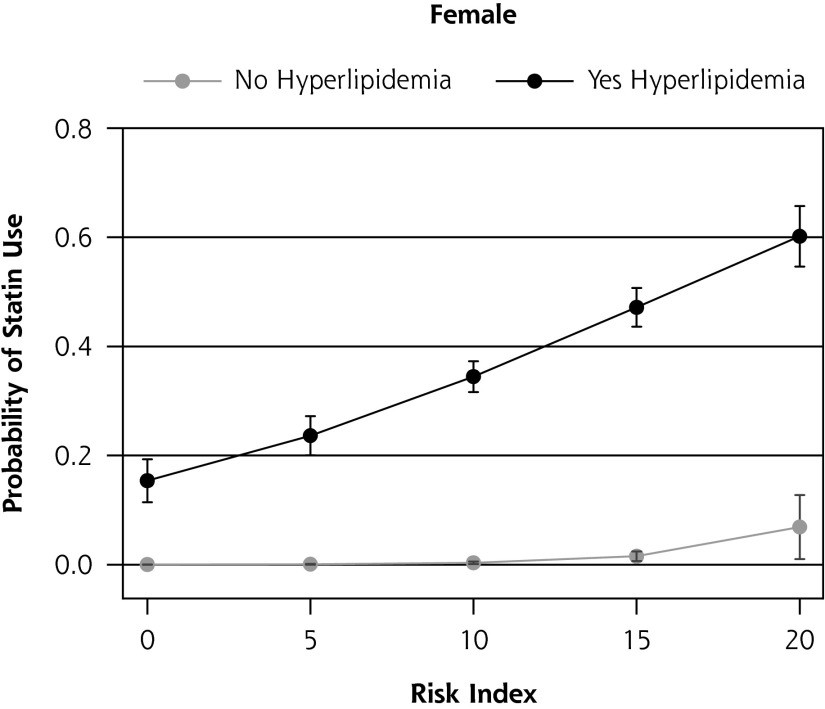
When examining the population without coronary artery disease or diabetes using a modified cardiovascular risk index, statin use generally increased with risk (Figure 3). Among men at high risk for cardiovascular disease because of risk factors other than hyperlipidemia, coronary artery disease, or diabetes, those with a diagnosis of hyperlipidemia had a probability of 0.59 (95% CI, 0.54–0.64) of being on a statin, while those without the diagnosis had a probability of just 0.04 (95% CI, 0.02–0.06) (P <.001). Similar results were found in women.
Figure 3.
Probability of statin use in an individual without diabetes or coronary artery disease by modified cardiovascular risk index, according to sex.
DISCUSSION
Key Findings
This study of a nationally representative sample documents significant underuse of statins in individuals with high cardiovascular disease risk aged 30 to 79 years. Nationally, within the study population, an estimated 9.0 million people with diabetes aged older than 40 years and 5.6 million people with coronary artery disease were not on statins. The identified populations have clearly been shown to benefit from statins. People with coronary artery disease have an approximate 16% reduction in overall mortality,9 while people aged older than 40 years with diabetes have a more than 30% reduction in cardiovascular disease outcomes and likely a reduced risk of death.7 Importantly, statins have benefit irrespective of cholesterol levels.3–5,7
Despite this benefit, hyperlipidemia appears to be the driving force behind statin use in both primary and secondary prevention. For years, guidelines,2 general public health messages, and direct-to-consumer advertising have anchored statins to cholesterol reduction rather than cardiovascular risk reduction. This overreliance on cholesterol levels is best illustrated in Figures 1 and 2, which show that those with hyperlipidemia but without diabetes or heart disease are more likely to be on statins than those without hyperlipidemia who have diabetes or heart disease. Given that individuals with heart disease or diabetes are at considerably higher cardiovascular risk, this pattern strongly supports the notion that statin use is being driven by hyperlipidemia instead of by overall cardiovascular risk. Given that the absolute benefit of statins is related to a patient’s overall risk, this finding is problematic.
The recently released ACC-AHA guidelines changed the focus from treating to a target LDL cholesterol level to treating based on an individual’s cardiovascular risk. Our study shows low levels of use among those with diabetes and heart disease who do not have hyperlipidemia, while a previous study shows low rates of use among those with LDL cholesterol values below goal.17 In addition, our study shows strong risk factors such as cerebrovascular disease, peripheral arterial disease, and tobacco use are frequently not significant predictors of statin use when controlling for other variables. There is evidence that statins benefit those with a history of cerebrovascular disease32 and peripheral arterial disease,33 but the evidence base is weaker than that supporting statin benefits for those with diabetes and heart disease. Both of these populations are included in the ACC-AHA guidelines’ high-risk category along with coronary artery disease and diabetes after age 40. There is potential benefit from decreasing the focus on hyperlipidemia and replacing it with cardiovascular risk when deciding to prescribe a statin.
The new guidelines substantially increase the recommended use of statins by including individuals with a 10-year cardiovascular risk as low as 7.5%. This risk level is substantially lower than that of other guidelines34 and incorporates less robust evidence than that for higher-risk groups.12–14 Given the substantial undertreatment of high-risk groups in our analysis, focusing resources on improving rates of use among those at high risk would likely have a greater impact in terms of morbidity and mortality than simply expanding use. This impact is especially true among individuals with coronary artery disease or with diabetes and age older than 40 years and likely among those with cerebrovascular disease and peripheral arterial disease.
In designing societal interventions to increase statin use, it is important to consider the risks of treatment, inability of some patients to tolerate statins, and personal choice not to use these agents. A previous study identified a discontinuation rate of 10.3% in patients with a documented statin-related event.34 Several potential adverse effects have been identified as causing noncompliance, including myalgia, fatigue, transaminitis, and memory problems, among others; however, when rechallenged, a number of affected patients are on a statin a year later.35 Assuming that 10% of the population cannot or will not take statins, that value still suggests that roughly 40% of diabetic individuals and 30% of individuals with cardiovascular disease would see improved outcomes if they were using a statin.
Our study shows lower levels of statin use than a recent 2011 study.17 The previous study’s population was a cardiology practice network and was composed of people with obstructive cardiovascular disease without age restriction. An estimated 77.8% of patients were being treated with statins, compared with the 58.2% in our study. Our lower rate of statin use is likely due to several factors, including differences in the subspecialty referral population vs the more generalizable MEPS population and our more conservative definition of statin use requiring at least 2 prescriptions. The latter factor would likely result in lower estimates of use. For instance, had we broadened the definition of a user to an individual with any statin prescription, use among those with coronary artery disease would have increased to 66.6% (95% CI, 62.9%–70.2%). Other estimates of statin use in a secondary prevention population are more than 5 years old and have varied between 50% and 68%.16,18,19
Limitations
The most noteworthy limitation of the study is that MEPS identifies medical conditions and prescription drug information by self-report. It does not include laboratory data such as lipid values or blood pressures. It is also unclear to what extent the prescribing of a statin could have influenced the diagnosis of hyperlipidemia. In one regard, it is reassuring that only one-half of people reporting a diagnosis of hyperlipidemia were using a statin. If individuals underreport or overreport a diagnosis of hyperlipidemia based on whether they are using a cholesterol-lowering drug, hyperlipidemia’s predictive strength for statin use could be overestimated in regression models.
Conclusions
In this nationally representative sample, a considerable number of individuals—especially those with coronary artery disease, diabetes, or both—who would potentially benefit from statins were not receiving this therapy. Our findings suggest that the most likely explanation is an overreliance on hyperlipidemia instead of cardiovascular risk when deciding whether to prescribe a statin. The recently released ACC-AHA guidelines offer an opportunity to reframe statins as medications that reduce cardiovascular risk rather than as medications that lower cholesterol. This change could lead to substantial societal benefits.
Acknowledgments
We acknowledge the contribution of Elizabeth (Lisa) Jackson, MD MPH, of the University of Michigan, who provided detailed comments on an earlier version of the manuscript. She did not receive compensation for her efforts.
Footnotes
Conflicts of interest: authors report none.
Michael Johansen had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Supplementary materials: Available at http://www.AnnFamMed.org/content/12/3/215/suppl/DC1/
References
- 1.Stone NJ, Robinson J, Lichtenstein AH, et al. 2013. ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;S0735-1097(13):06028-2 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25): 3143–3421 [PubMed] [Google Scholar]
- 3.Baigent C, Keech A, Kearney PM, et al. Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366(9493): 1267–1278 [DOI] [PubMed] [Google Scholar]
- 4.Hayward RA, Hofer TP, Vijan S. Narrative review: lack of evidence for recommended low-density lipoprotein treatment targets: a solvable problem. Ann Intern Med. 2006;145(7):520–530 [DOI] [PubMed] [Google Scholar]
- 5.Collins R, Armitage J, Parish S, Sleigh P, Peto RHeart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet. 2003;361(9374): 2005–2016 [DOI] [PubMed] [Google Scholar]
- 6.Mihaylova B, Emberson J, Blackwell L, et al. Cholesterol Treatment Trialists’ (CTT) Collaborators. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012; 380(9841):581–590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Colhoun HM, Betteridge DJ, Durrington PN, et al. CARDS investigators. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet. 2004;364(9435):685–696 [DOI] [PubMed] [Google Scholar]
- 8.Vijan S, Hayward RAAmerican College of Physicians. Pharmacologic lipid-lowering therapy in type 2 diabetes mellitus: background paper for the American College of Physicians. Ann Intern Med. 2004;140(8):650–658 [DOI] [PubMed] [Google Scholar]
- 9.Wilt TJ, Bloomfield HE, MacDonald R, et al. Effectiveness of statin therapy in adults with coronary heart disease. Arch Intern Med. 2004;164(13):1427–1436 [DOI] [PubMed] [Google Scholar]
- 10.Ioannidis JP. More than a billion people taking statins? Potential implications of the new cardiovascular guidelines. JAMA. 2014;311(5):463–464 [DOI] [PubMed] [Google Scholar]
- 11.Ray KK, Seshasai SR, Erqou S, et al. Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants. Arch Intern Med. 2010;170(12):1024–1031 [DOI] [PubMed] [Google Scholar]
- 12.Taylor F, Ward K, Moore TH, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2011;(1): CD004816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mihaylova B, Emberson J, Blackwell L, et al. Cholesterol Treatment Trialists’ (CTT) Collaborators. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380(9841):581–590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Redberg RF, Katz MH. Healthy men should not take statins. JAMA. 2012;307(14):1491–1492 [DOI] [PubMed] [Google Scholar]
- 15.Kent DM, Rothwell PM, Ioannidis JP, Altman DG, Hayward RA. Assessing and reporting heterogeneity in treatment effects in clinical trials: a proposal. Trials. 2010;11:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mann D, Reynolds K, Smith D, Muntner P. Trends in statin use and low-density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. Ann Pharmacother. 2008;42(9):1208–1215 [DOI] [PubMed] [Google Scholar]
- 17.Ma J, Sehgal NL, Ayanian JZ, Stafford RS. National trends in statin use by coronary heart disease risk category. PLoS Med. 2005;2(5): e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arnold SV, Spertus JA, Tang F, et al. Statin use in outpatients with obstructive coronary artery disease. Circulation. 2011;124(22): 2405–2410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cooke CE, Hammerash WJ., Jr Retrospective review of sex differences in the management of dyslipidemia in coronary heart disease: an analysis of patient data from a Maryland-based health maintenance organization. Clin Ther. 2006;28(4):591–599 [DOI] [PubMed] [Google Scholar]
- 20.Goff DC, Jr, Gu L, Cantley LK, Sheedy DJ, Cohen SJ. Quality of care for secondary prevention for patients with coronary heart disease: results of the Hastening the Effective Application of Research through Technology (HEART) trial. Am Heart J. 2003;146(6):1045–1051 [DOI] [PubMed] [Google Scholar]
- 21.Johansen ME, Gold KJ, Sen A, Arato N, Green LA. A national survey of the treatment of hyperlipidemia in primary prevention. JAMA Intern Med. 2013;173(7):586–588, discussion 588 [DOI] [PubMed] [Google Scholar]
- 22.Medical Expenditure Panel Survey. 2010 Consolidated Data File. http://meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h138/h138doc.pdf Accessed Jan 7, 2014
- 23.Shepherd J, Blauw GJ, Murphy MB, et al. PROSPER study group. PROspective Study of Pravastatin in the Elderly at Risk. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360(9346):1623–1630 [DOI] [PubMed] [Google Scholar]
- 24.Petersen LK, Christensen K, Kragstrup J. Lipid-lowering treatment to the end? A review of observational studies and RCTs on cholesterol and mortality in 80+-year olds. Age Ageing. 2010;39(6):674–680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koller MT, Steyerberg EW, Wolbers M, et al. Validity of the Framingham point scores in the elderly: results from the Rotterdam study. Am Heart J. 2007;154(1):87–93 [DOI] [PubMed] [Google Scholar]
- 26.Hill SC, Zuvekas SH, Zodet MW. Implications of the accuracy of MEPS prescription drug data for health services research. Inquiry. 2011;48(3):242–259 [DOI] [PubMed] [Google Scholar]
- 27.Edwards WS, Winn DM, Kurlantzick V, et al. Evaluation of national health interview survey diagnostic reporting. National Center for Health Statistics. Vital Health Stat. 1994;2(120). DHHS Publication No. (PHS)94-1394 [Google Scholar]
- 28.Johnson AE, Sanchez ME. Household and medical reports on medical conditions: National Medical Expenditure Survey. J Econ Soc Meas. 1993;19:199–223 [Google Scholar]
- 29.Medical Expenditure Panel Survey. 2010 Medical Conditions File http://meps.ahrq.gov/mepsweb/ Accessed Jun 3, 2013
- 30.Roger VL, Go AS, Lloyd-Jones DM, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–e220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.NHLBI. Estimate of 10-Year Risk for CHD. http://www.nhlbi.nih.gov/guidelines/cholesterol/risk_tbl.htm Accessed May 27, 2013
- 32.Manktelow BN, Potter JF. Interventions in the management of serum lipids for preventing stroke recurrence. Cochrane Database Syst Rev. 2009;(3):CD002091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aung PP, Maxwell HG, Jepson RG, Price JF, Leng GC. Lipid-lowering for peripheral arterial disease of the lower limb. Cochrane Database Syst Rev. 2007;(4):CD000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Institute for Health and Clinical Excellence. Lipid modification: Cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. London, England: NICE; 2008. http://guidance.nice.org.uk/cg67 Accessed Mar 22, 2014 [PubMed] [Google Scholar]
- 35.Zhang H, Plutzky J, Skentzos S, et al. Discontinuation of statins in routine care settings: a cohort study. Ann Intern Med. 2013;158(7):526–534 [DOI] [PMC free article] [PubMed] [Google Scholar]