Abstract
More than 80% cardiovascular disease (CVD) is preventable despite the fact that it is currently the ultimate cause of disability in the world. Assessment of the nationwide prevalence of dyslipidemia as a major CVD risk factor is essential to efficiently conduct prevention programs. We extracted data according to the cut-off points of dyslipidemia used in each study. All published papers on this topic in Iranian and international journals with affiliation of “Iran” were reviewed using standard keywords up to September 2011. We included all available population-based studies and national surveys conducted in individuals aged ≥ 15 years. We excluded studies with < 300 individuals, non-population-based studies, or duplicated citations. We analyzed by random effect method due to between-study heterogeneity. The estimated prevalence and 95% confidence intervals in 29 eligible articles and one un-published data for hypercholesterolemia (≥200 mg/dl), hypertriglyceridemia (≥150 mg/dl), high levels of low density lipoprotein cholesterol ([LDL-C] [≥ 130 mg/dl]) and low levels of high density lipoprotein cholesterol ([HDL-C] <40 mg/dl in males, <50 mg/dl in females), in Iranian people were 41.6% (36.1-47.0), 46.0% (43.3-48.7), 35.5% (24.0-47.1) and 43.9% (33.4-54.4), respectively among both sexes and in both rural and urban areas. Hypercholesterolemia, high LDL-C and low HDL-C were more prevalent in women, whereas hypertriglyceridemia was more prevalent in men. All types of lipid component abnormalities were more prevalent in urban residents. Prevalence of dyslipidemia is considerable in Iran. It is necessary to enforce current measures of dyslipidemia control in the Iranian people to reduce CVD burden.
Keywords: Cardiovascular disease, dyslipidemia, Iran
INTRODUCTION
According to World Health Organization (WHO) statistics four non-communicable diseases (NCDs) including cardiovascular disease (CVD), cancer, chronic respiratory disease and diabetes were the major causes of mortality in the world in 2008.[1] 35 million deaths (60% of total global mortality) annually are due to these diseases.[1] It is anticipated that the mortality rate of NCDs will increase by 17% in the next 10 years.[1] Despite this increasing trend of NCDs throughout the world, fortunately more than 80% of heart disease, stroke and type 2 diabetes (and almost one-third of cancers) are preventable.[1]
CVD is a common in the general population. It is not only the ultimate cause of death in adults,[2] but also predictably the definitive cause of disability in the world between the years 2000 and 2025[3] due to increased life expectancy, consumption of western diets, physical inactivity and smoking.[4] As well as in Iran, the most of in-patient admissions for CVD (75%) were suffering from coronary heart disease (CHD).[5] In addition, the economic cost of CVD is high. In 2008, the direct and indirect economic costs of CVD in European Union were estimated at 192 billion Euros.[6] This figure was estimated at 475 billion $ in the US in the same year.[7]
Atherosclerosis of the arterial vessel walls is the most important underlying cause of CVD and dyslipidemia is a major and primary risk factor of atherosclerotic CVD. Plasma levels of lipids vary in normal individuals in different communities due to genetic and life-style differences including variations in dietary and physical activity habits.[8,9] For example, the average levels of total cholesterol (T-C) in western men is reported 202 mg/dl[10] compared to 165 mg/dl among Chinese men.[11]
In the WHO multinational monitoring of trends and determinants in cardiovascular disease (MONICA) project the mean of T-C in 30 countries varied from 158 mg/dl in China-Beijing to 246 mg/dl in Luxemburg among men and from 162 mg/dl in China-Beijing to 246 mg/dl in UK-Glasgow among the women.[12]
Dyslipidemia covers the broad spectrum of lipid abnormalities. However, elevations of T-C and low density lipoprotein cholesterol (LDL-C) have received the most attention. Besides the elevation of T-C and LDL-C levels, other types of lipid profile abnormalities such as low high density lipoprotein cholesterol (HDL-C) levels could also predispose to CVD. Overall, dyslipidemia is defined by T-C, LDL-C, triglyceride (TG), apolipoprotein B and lipoprotein (a) levels in upper the 90th percentile or HDL-C and apolipoprotein A1 levels below the 10th percentile of the general population.[13]
The value of reducing T-C and LDL-C in primary and secondary prevention of CVD is evident based on several epidemiological studies. The seven countries study, WHO MONICA project, multiple risk factor intervention trial, Framingham Heart Study, Migration and Stockholm studies have established the association of plasma cholesterol with risk of CVD.[14,15,16,17,18,19] The results of a meta-analysis study of 10 large cohort studies revealed that for each 0.6 mmol/l reduction of serum T-C levels in adults aged ≥ 60 years, the risk of CHD end points decreased by 27%.[20]
The national cholesterol education program adult treatment panel III (NCEP ATP III) 2001 guidelines defined hypercholesterolemia as T-C ≥ 240 mg/dl.[21] However, the evidence shows that the risk of CVD events increases with T-C levels > 150 mg/dl.[22] Hence, the precise cut-off value for definition of hypercholesterolemia is a formidable task. In addition according to NCEP ATP III approximately 20% of individuals with desired levels of T-C (150-250 mg/dl) suffering from CVD events; therefore it is crucial to recognize the high risk people in this range of cholesterol levels.[23] The relationship between low HDL-C and CVD risk and protective effect of HDL-C against atherosclerosis are also well-established.[22,24,25,26,27] Based on the above mentioned data the decline of the coronary events could be possible by modifying the serum lipid levels. For conducting programs to prevent CVD, first we should know the prevalence of CVD risk factors in the community. Hence, we decided to assess the prevalence of dyslipidemia as a major risk factor of CVD in Iran in a systematic review and meta-analysis study.
METHODS
To obtain all related studies, we searched in Persian databases; Iran Medex, Magiran, SID, Irandoc and also in English databases; Scopus, ISI web of Science and PubMed up to September 2011. The search terms were “lipid,” “dyslipidemia,” “CVD,” “hypercholesterolemia,” “hypertriglyceridemia,” “prevalence,” “public health” and “epidemiology,” with affiliation to “Iran” for searching in the English databases and also we used the Farsi equivalent of these terms for search in Persian databases. Moreover, the references of selected citations and non-published national surveys were hand-searched. In addition, we sent at least 3 E-mails to corresponding authors in cases that had incomplete data.
Inclusion and exclusion criteria
We included all available population-based studies including local, subnational studies and national surveys, which were carried out on individuals with age ≥ 15 years. We excluded studies with fewer than 300 individuals, non-population-based studies, or those with duplicate citation. When there were multiple publications from the same population, only the largest study was included.
Data extraction
Data were collected according to a standard protocol independently by two authors. Disagreement was resolved by discussion between them. In cases could not reach a consensus, a third author was consulted. The extracted information from literature included the name of the first author, the year of publication, the study region, type of study (local study or survey), total sample size, age and sex groups, urban/rural areas, cut-off point of prevalence, reported prevalence and its 95% confidence interval (CI).
Statistical analysis
Heterogeneity of reported prevalence was assessed by the Chi-square-based Q-test and was regarded to be statistically significant at P < 0.1. In order to gain better insight into the prevalence of dyslipidemia and its heterogeneity throughout Iran, we analyzed our findings using meta-analysis random effect methods model (using the DerSimonian and Laird method) analysis due to the presence of between-study heterogeneity by cut-off values of NCEP ATP III. The analyses were conducted with STATA software, version 11.0, Produced by StataCorp, USA.
RESULTS
In the primary search, we found 181 full text articles that were related to our topic. After considering inclusion and exclusion criteria, we selected 29 articles and 1 hand-searching (non-published, in press) data.[28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57] The number of the initial search results and included studies are shown in the Figure 1. The extracted data from these studies are shown separately in four tables [Tables 1-4]. This includes the prevalence of high levels of T-C, TG, LDL-C and also low levels of HDL-C, respectively according to the population-based studies in the cities of Iran. Due to severe heterogeneity of reported prevalence (P < 0.001), meta-analysis was performed by using a random effect method. We estimated the prevalence of each lipid component according to sex, which is observed in a separate table [Table 5]. We found 14 and 11 eligible studies for prevalence of hypercholesterolemia (≥200 mg/dl) and hypertriglyceridemia (≥150 mg/dl), respectively with a total sample size equal to 1,134,874 subjects for hypercholesterolemia and 44,958 subjects for hypertriglyceridemia. The eligible studies for estimation of the prevalence of high LDL-C (≥130 mg/dl) or low HDL-C levels (<40 among males, <50 among females) were 11 and 14 articles, respectively with a total sample size of 26,454 subjects for high LDL-C levels and 74,216 subjects for low HDL-C levels. Our estimated prevalence of hypercholesterolemia and hypertriglyceridemia in those aged > 19 years old among both sexes were 41.6% (CI: 95% 36.1-47.0) and 46.0% (CI: 95% 43.3-48.7), respectively. These figures for prevalence of high LDL-C and low HDL-C levels were 35.5% (CI: 95% 24.0-47.1) and 43.9% (CI: 95% 33.4-54.4), respectively.
Figure 1.
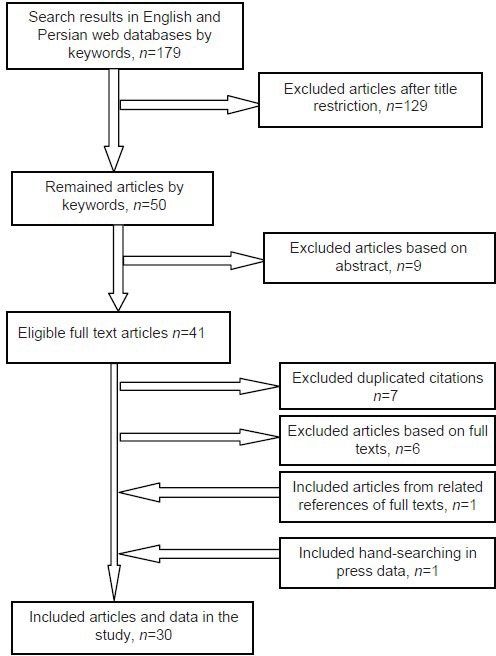
Flow diagram of the study selection process
Table 1.
The prevalence of hypercholesterolemia in population-based studies in cities of Iran
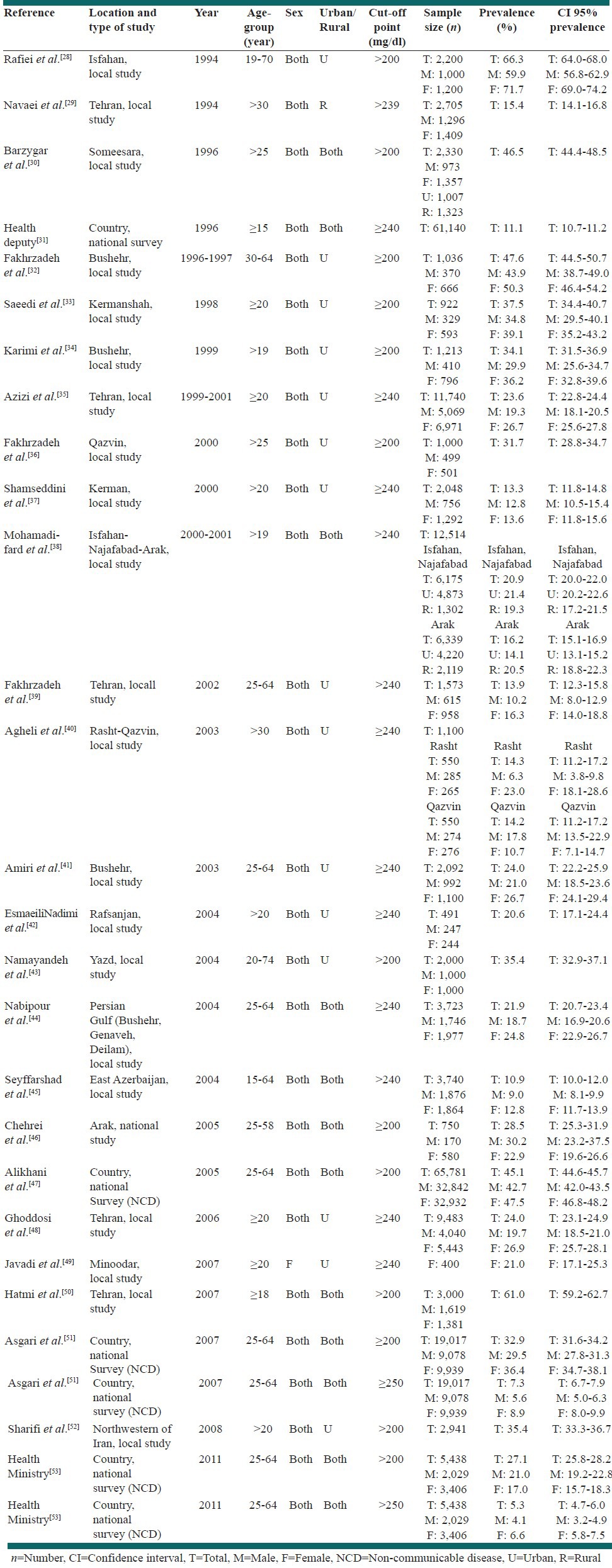
Table 4.
The prevalence of low level of HDL-C in population-based studies in cities of Iran
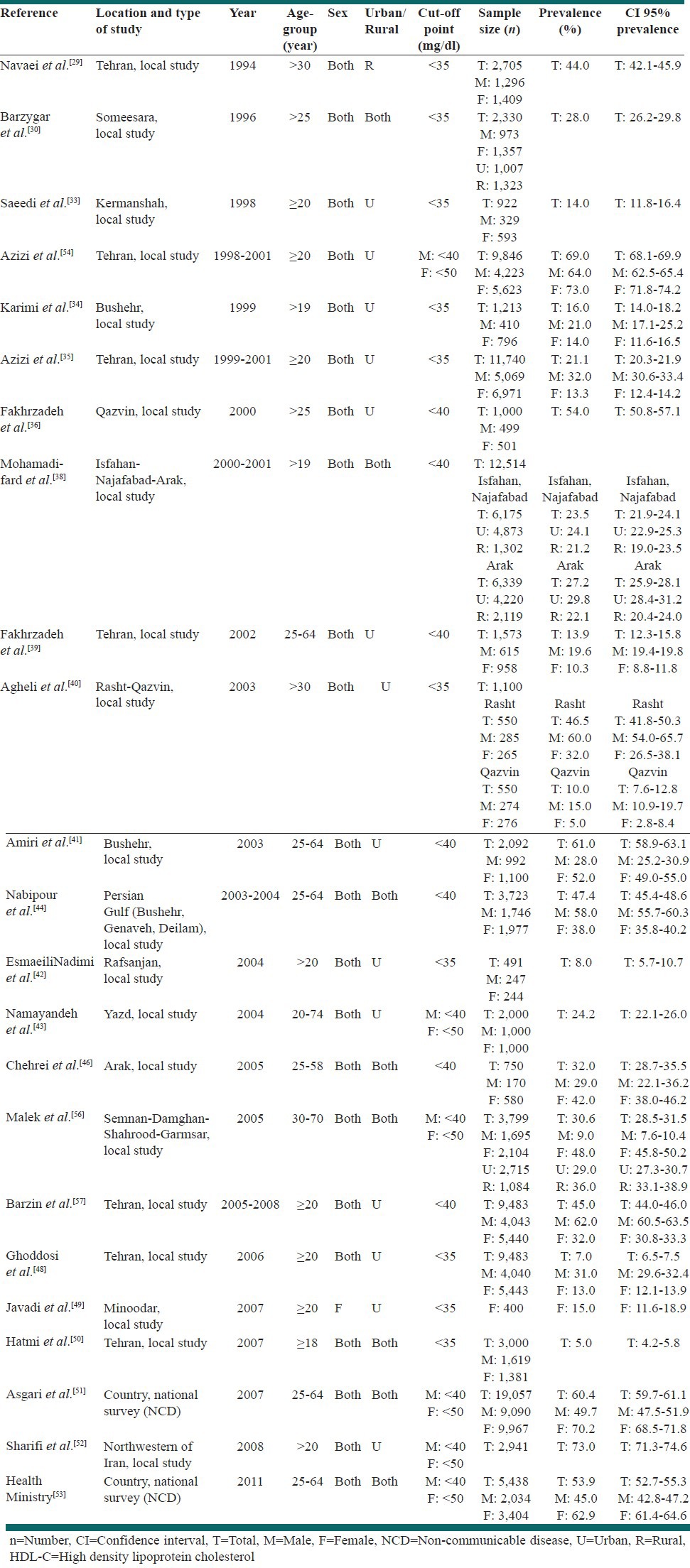
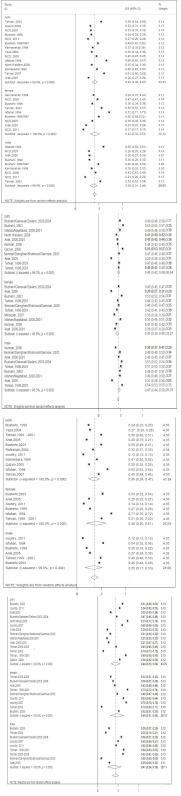
Table 5.
The overall prevalence of lipid components according to ATPIII cut-off among sex by random effect meta-analysis of data extracted from population-based studies in Iran
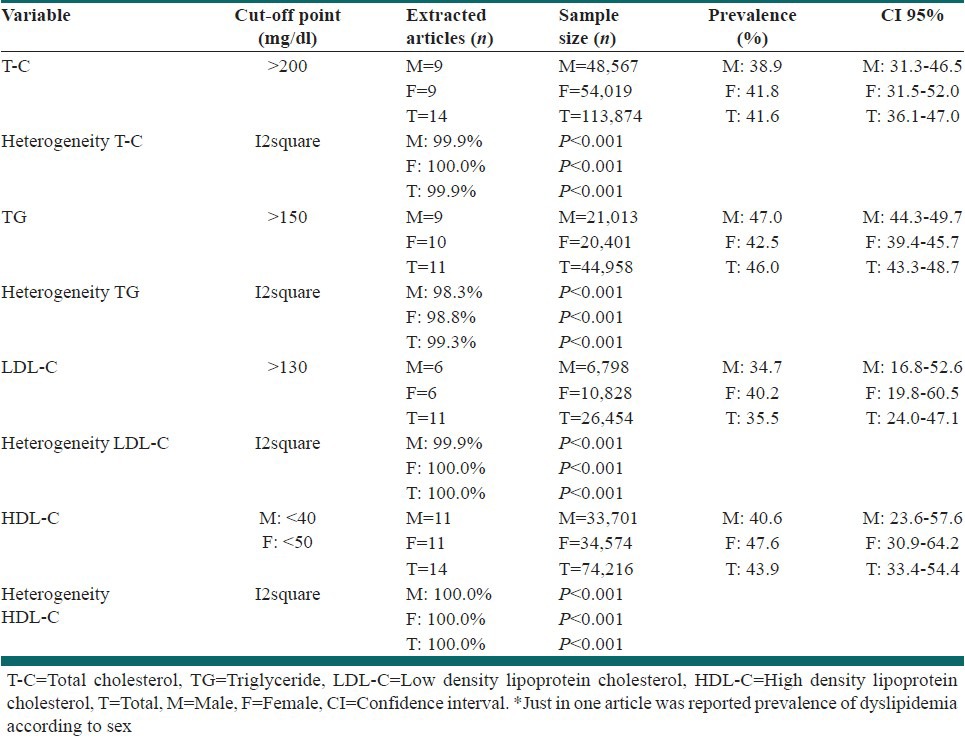
Table 2.
The prevalence of hypertriglyceridemia in population-based studies in cities of Iran
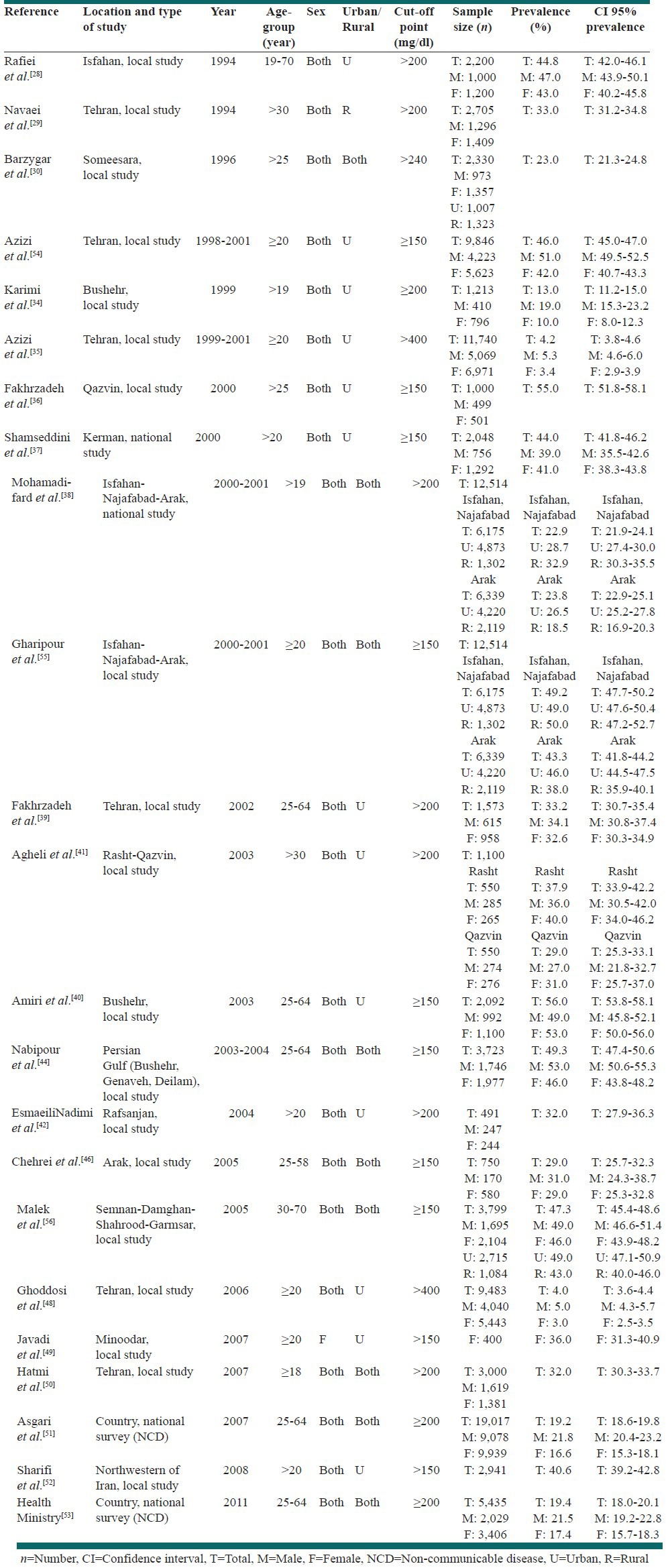
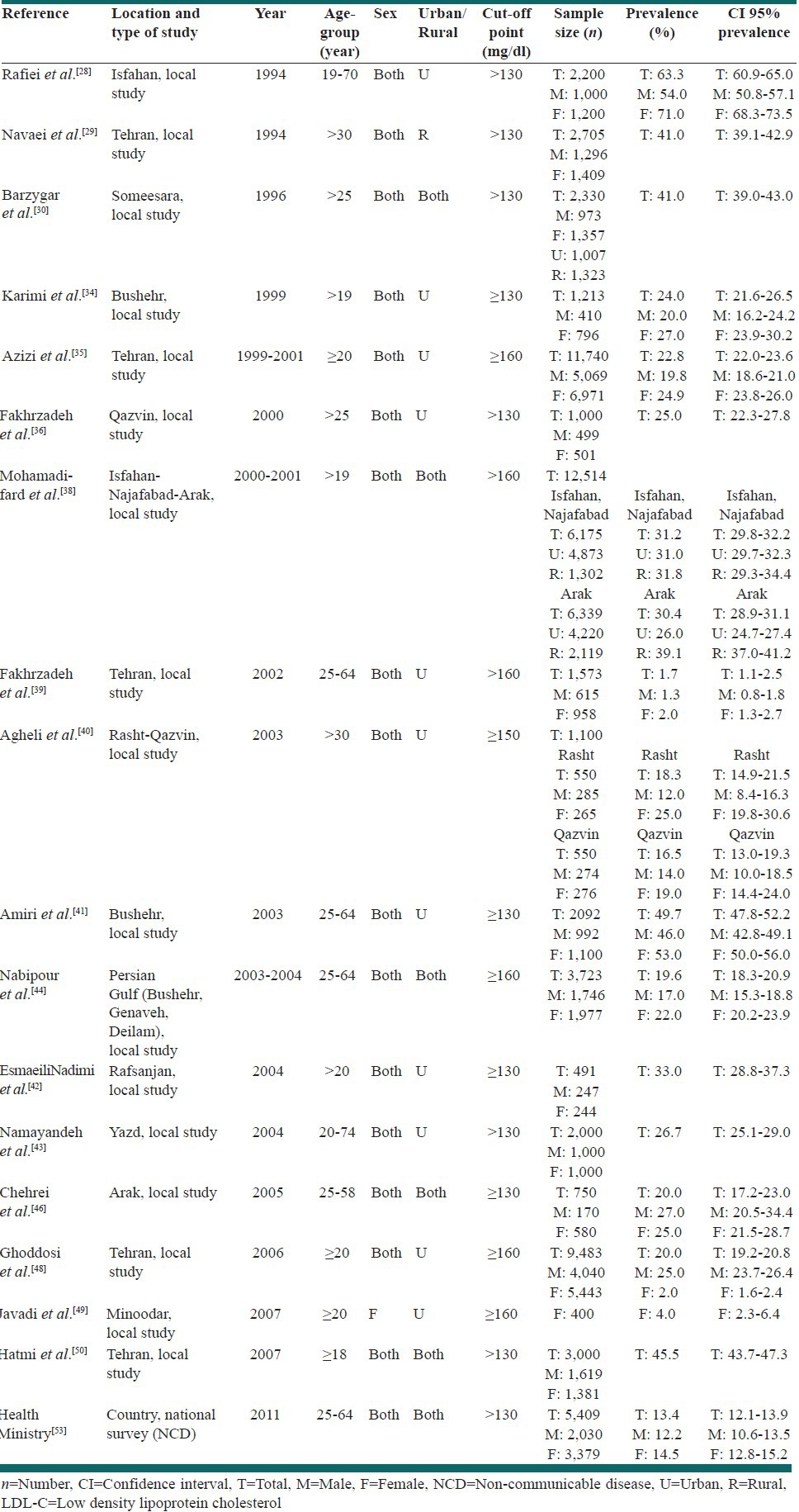
Table 3.
The prevalence of high level of LDL-C in population-based studies in cities of Iran
Women had a higher prevalence of hypercholesterolemia while men had a higher prevalence of hypertriglyceridemia. These figures for prevalence of hypercholesterolemia were 41.8% (CI: 95% 31.5-52.0) in women versus 38.9% (CI: 95% 31.3-46.5) in men. In hypertriglyceridemic status, the prevalence was 47.0% (CI: 95% 44.3-49.7) in men versus 42.5% (CI: 95% 39.4-45.7) in women.
In addition, hypercholesterolemia and hypertriglyceridemia were more common among urban than rural residents.
The prevalence of high LDL-C and low HDL-C levels were greater among women and urban residents. These figures for prevalence of high LDL-C were 40.2% (CI: 95% 19.8-60.5) in women versus 34.7% (CI: 95% 16.8-52.6) in men. The prevalence of low HDL-C were 47.6% (CI: 95% 30.9-64.2) in women versus 40.6% (CI: 95% 23.6-57.6) in men. The details of these estimations are shown in Table 5.
DISCUSSION
Our findings indicate that the prevalence of dyslipidemia regarding sex differences is considerable in Iran. Overall the abnormalities of lipid components were more common among men in urban areas. Speedy urbanization, unhealthy diet and inactivity are underlying reasons for the high prevalence of dyslipidemia in Iran.[58,59] Usually, in practice only T-C is measured, whilst low level of T-C may result in hiding the abnormal level of TG and HDL-C. So, we considered all components of lipid in our systematic search. In the following sections, we discuss and compare our findings with those of other countries.
Hypercholesterolemia
According to the report of Tehran Lipid Glucose Study which was held in the metropolitan city of Tehran among nearly half of Tehranian adults, mean T-C level was 210 mg/dl.[35] So, the prevalence of hypercholesterolemia in Iran was expected to be high. We estimated the overall prevalence of high T-C (≥200 mg/dl) levels in adult aged ≥ 18 years in our country to be 41.6% (36.1-47.0). This was according to the population-based studies in different cities of Iran among both sexes and in both rural and urban areas. This figure shows that the prevalence of hypercholesterolemia in Iran is higher relative to Eastern Asian countries. The corresponding figure was approximately 33% in Chinese aged 35-74 years,[60] 17.2% in Nepali people[61] and 23.2% in Eastern Indians.[62] On the other hand in western European countries, hypercholesterolemia is prevailing more relative to our country. The prevalence of high T-C was 48% in the UK adults aged 19-64 years[63] and 56.7% in adults aged 30-70 in Portugal.[64] In U.S, it was reported to be 40.5% and 45.8% among non-Hispanic white men and women, respectively aged ≥ 20 years by the American Heart Association in 2013.[65] The prevalence of hypercholesterolemia in our neighbouring countries in the middle east crescent varies from 54% in Saudi Arabians aged 30-70 years,[66] to 37.5% in Turkish people aged ≥ 20 years,[67] and 36.9% of Lebanese aged 18-65 years.[68] We found that similar to most of the other studies hypercholesterolemia was more prevalent in Iranian women.
Hypertriglyceridemia
In our study, the reported prevalence of adult hypertriglyceridemia (≥150 mg/dl) in both sexes and in both rural and urban areas was 46.0% (43.3-48.7). This figure shows that the prevalence of hypertriglyceridemia in Iran is higher relative to most other western or eastern countries. The corresponding figure is 27% in US,[65] 25% in Sweden,[69] 19.2%in Italy,[70] 26% in Portugal,[64] and 12.5% in Switzerland.[71] In Asia, the prevalence of high TG is reported to be 26.35% in Taiwanese aged 40-65 years,[72] 29.3% in Malaysia,[73] 37.7% in Eastern India[62] and 48.3% in Nepal.[61] The report from our neighbouring Middle Eastern countries vary from 40.3% in Saudi Arabia[66] and 41.6% in Iraq,[74] to 35.3% in Lebanon,[68] 30.4% in Turkey,[67] and 20.7% in Oman.[75] The higher prevalence of high TG in our country relative to most of the studies elsewhere might be due to higher intake simple carbohydrates and higher ratio of simple to complex carbohydrate consumption by the Persian people.[76] We observed higher prevalence of hypertriglyceridemia in Iranian males similar to findings in most other countries.
High LDL-C levels
The reported prevalence of high LDL-C (≥130 mg/dl) levels in adults of both sexes in both rural and urban areas was 35.5 (24.0-47.1) % in our study. The corresponding figure was 30.1% and 29.3%, respectively in adult US non-Hispanic white men and women,[65] 20.8% in Switzerland,[71] 24.8% in China,[60] and 46.9% among Indians aged ≥ 20 years.[62] The reports from our neighbouring countries in the middle East varied from 32.1% from Lebanon,[68] to 44.5% in Turkey.[67] These figures were higher among urban women in most of the studies.
Low HDL-C levels
The reported prevalence of low levels of HDL-C (<40 in males, <50 in females) among adults of both sexes and in both rural and urban areas was 43.9 (33.4-54.4) %. This figure was reported as 33.1% and 12.4%, respectively in adult US non-Hispanic white men and women[65] and 53.4% in Switzerland.[71] The corresponding figure in the East Asian region was 56.7% in Nepal,[61] 54.75% in Taiwan,[72] 37.2% in Malaysia,[73] 33.4% in Korea,[77] 22.5% in Eastern India,[62] and 19.2% in China.[60] The reports from our neighbouring countries were 49.9% in Iraq,[74] 49.3% in Lebanon,[68] 21.1% in Turkey,[67] and 75.4% in Oman.[75] In our study in contrast to others this figure among females was higher than males.
CONCLUSIONS
Based on the above study it can be concluded that although different population-based studies have been performed in Iran to define the prevalence of lipid profile abnormalities, we observed some heterogeneities in the data expressed by different authors. Although determining the definite prevalence of dyslipidemia is an arduous task by these population-based studies, it is obvious that abnormalities in lipid components are fairly prevalent in Iran.
So Health Care Organizations in Iran should execute well-defined programs to control of dyslipidemia in the general population more efficaciously. For example, lipid clinic can be effective in the management of lipid profile and cardiovascular risk of dyslipidemic patients.[78]
ACKNOWLEDGMENTS
The authors would like to thank of Endocrinology and Metabolism Clinical Sciences Institute and also Ministry of Health and Medical Education of Iran for helping in searching of published and non-published articles.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Alwan A. 2008-2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases. Report World Health Organization. Published. 2009. Available in http://www.who.int/nmh/publications/9789241597418/en .
- 2.Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349:1269–76. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- 3.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997;349:1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 4.Critchley J, Liu J, Zhao D, Wei W, Capewell S. Explaining the increase in coronary heart disease mortality in Beijing between 1984 and 1999. Circulation. 2004;110:1236–44. doi: 10.1161/01.CIR.0000140668.91896.AE. [DOI] [PubMed] [Google Scholar]
- 5.Fakhrzadeh H, Pourebrahim R, Akhlaghi MR. Direct medical cost of coronary heart disease in Iran oil industry. Iran S Med J. 2001;1:45–52. [Google Scholar]
- 6.Allender S, Scarborough P, Peto V, Leal J, Luengo-Fernandez R, Gray A. 2008 ed. European Heart Network; 2008. European Cardiovascular Disease Statistics. Available in http://www.healtheurope.org/index . [Google Scholar]
- 7.Williams KJ, Tabas I. Lipoprotein retention – And clues for atheroma regression. Arterioscler Thromb Vasc Biol. 2005;25:1536–40. doi: 10.1161/01.ATV.0000174795.62387.d3. [DOI] [PubMed] [Google Scholar]
- 8.Carroll MD, Lacher DA, Sorlie PD, Cleeman JI, Gordon DJ, Wolz M, et al. Trends in serum lipids and lipoproteins of adults, 1960-2002. JAMA. 2005;294:1773–81. doi: 10.1001/jama.294.14.1773. [DOI] [PubMed] [Google Scholar]
- 9.Wu Z, Yao C, Zhao D, Wu G, Wang W, Liu J, et al. Cardiovascular disease risk factor levels and their relations to CVD rates in China – Results of Sino-MONICA project. Eur J Cardiovasc Prev Rehabil. 2004;11:275–83. doi: 10.1097/01.hjr.0000136566.89429.63. [DOI] [PubMed] [Google Scholar]
- 10.Bennet A, Di Angelantonio E, Erqou S, Eiriksdottir G, Sigurdsson G, Woodward M, et al. Lipoprotein (a) levels and risk of future coronary heart disease: Large-scale prospective data. Arch Intern Med. 2008;168:598–608. doi: 10.1001/archinte.168.6.598. [DOI] [PubMed] [Google Scholar]
- 11.Erqou S, Kaptoge S, Perry PL, Di Angelantonio E, Thompson A, et al. Emerging Risk Factors Collaboration. Lipoprotein (a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA. 2009;302:412–23. doi: 10.1001/jama.2009.1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller NE, Thelle DS, Forde OH, Mjos OD. The Tromsø heart-study. High-density lipoprotein and coronary heart-disease: A prospective case-control study. Lancet. 1977;1:965–8. doi: 10.1016/s0140-6736(77)92274-7. [DOI] [PubMed] [Google Scholar]
- 13.Bostom AG, Cupples LA, Jenner JL, Ordovas JM, Seman LJ, Wilson PW, et al. Elevated plasma lipoprotein (a) and coronary heart disease in men aged 55 years and younger. A prospective study. JAMA. 1996;276:544–8. doi: 10.1001/jama.1996.03540070040028. [DOI] [PubMed] [Google Scholar]
- 14.Keys A. Cambridge, MA: Harvard University Press; 1980. Seven Countries: A Multivariate Analysis of Death and Coronary Heart Disease. [Google Scholar]
- 15.Keil U, Kuulasmaa K. The WHO MONICA project: Risk factors. Int J Epidemiol. 1989;18(3 Suppl 1):S46–55. [PubMed] [Google Scholar]
- 16.Stamler J, Wentworth D, Neaton JD. Is relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded? Findings in 356,222 primary screenees of the multiple risk factor intervention trial (MRFIT) JAMA. 1986;256:2823–8. [PubMed] [Google Scholar]
- 17.Kannel WB, Castelli WP, Gordon T. Cholesterol in the prediction of atherosclerotic disease. New perspectives based on the Framingham study. Ann Intern Med. 1979;90:85–91. doi: 10.7326/0003-4819-90-1-85. [DOI] [PubMed] [Google Scholar]
- 18.Robertson TL, Kato H, Rhoads GG, Kagan A, Marmot M, Syme SL, et al. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California. Incidence of myocardial infarction and death from coronary heart disease. Am J Cardiol. 1977;39:239–43. doi: 10.1016/s0002-9149(77)80197-5. [DOI] [PubMed] [Google Scholar]
- 19.Carlson LA, Rosenhamer G. Reduction of mortality in the stockholm ischaemic heart disease secondary prevention study by combined treatment with clofibrate and nicotinic acid. Acta Med Scand. 1988;223:405–18. doi: 10.1111/j.0954-6820.1988.tb15891.x. [DOI] [PubMed] [Google Scholar]
- 20.Law MR, Wald NJ, Thompson SG. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ. 1994;308:367–72. doi: 10.1136/bmj.308.6925.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harper CR, Jacobson TA. New perspectives on the management of low levels of high-density lipoprotein cholesterol. Arch Intern Med. 1999;159:1049–57. doi: 10.1001/archinte.159.10.1049. [DOI] [PubMed] [Google Scholar]
- 22.Rosenson RS. Low HDL-C: A secondary target of dyslipidemia therapy. Am J Med. 2005;118:1067–77. doi: 10.1016/j.amjmed.2004.12.021. [DOI] [PubMed] [Google Scholar]
- 23.Gordon DJ, Probstfield JL, Garrison RJ, Neaton JD, Castelli WP, Knoke JD, et al. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation. 1989;79:8–15. doi: 10.1161/01.cir.79.1.8. [DOI] [PubMed] [Google Scholar]
- 24.Abbott RD, Yano K, Hakim AA, Burchfiel CM, Sharp DS, Rodriguez BL, et al. Changes in total and high-density lipoprotein cholesterol over 10- and 20-year periods (the Honolulu Heart Program) Am J Cardiol. 1998;82:172–8. doi: 10.1016/s0002-9149(98)00310-5. [DOI] [PubMed] [Google Scholar]
- 25.Abbott RD, Wilson PW, Kannel WB, Castelli WP. High density lipoprotein cholesterol, total cholesterol screening, and myocardial infarction. The Framingham Study. Arteriosclerosis. 1988;8:207–11. doi: 10.1161/01.atv.8.3.207. [DOI] [PubMed] [Google Scholar]
- 26.Manninen V, Tenkanen L, Koskinen P, Huttunen JK, Mänttäri M, Heinonen OP, et al. Joint effects of serum triglyceride and LDL cholesterol and HDL cholesterol concentrations on coronary heart disease risk in the Helsinki Heart Study. Implications for treatment. Circulation. 1992;85:37–45. doi: 10.1161/01.cir.85.1.37. [DOI] [PubMed] [Google Scholar]
- 27.Barter P, Gotto AM, LaRosa JC, Maroni J, Szarek M, Grundy SM, et al. HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med. 2007;357:1301–10. doi: 10.1056/NEJMoa064278. [DOI] [PubMed] [Google Scholar]
- 28.Rafiei M, Boshtam M, Sarraf-Zadegan N. Lipid profiles in the Isfahan population: An Isfahan cardiovascular disease risk factor survey, 1994. East Mediterr Health J. 1999;5:766–77. [PubMed] [Google Scholar]
- 29.Navaei L, Mehrabi Y, Azizi F. Epidemiology of hyperlipidemia, obesity and increased blood pressure in rural areas of Tehran Province. Iran J Endocrinol Metab. 2000;2:253–62. [Google Scholar]
- 30.Barzygar A, Tehrani HS. Prevalence of atherosclerosis risk factors in the Some’esara city in 1996. J Kerman Univ Med Sci. 1997;4:182–9. [Google Scholar]
- 31.1st ed. East Azarbaijan, West Azarbaijan, Ardabil, Isfahan, Ilam, Bushehr, and Tehran: Health view University of Medical Sciences and Health Treatment Services; 2002. Health Deputy Secretariat of Applied Research, Vice Chancellor for Research and Technology, National Research Center of the Medical Sciences, Ministry of Health and Medical Education of Iran. [Google Scholar]
- 32.Fakhrzadeh H, Nabipour I, Rayani M, Vasiq A. Angina and myocardial infarction in patients with hyperlipidemia in Bushehr: A population-based study. Iran J Diabetes Lipid Disord. 2002;2:65–73. [Google Scholar]
- 33.Saeedi MR, Ray A, Rezaei M. Prevalence of hyperlipidemia among adult residents of Kermanshah in 1997-1998. Scientific Journal of Kurdistan University of Medical Sciences. 2003;3:49–54. [Google Scholar]
- 34.Karimi F, Rayani M, Akbarzadeh S, Khakzad M, Tahmasebi R, Arab J, et al. Prevalence of hyperlipidemias in adult population (>=19 years) of Bushehr Port; 1999. Iran S Med J. 2000;3:98–106. [Google Scholar]
- 35.Azizi F, Rahmani M, Emami H, Mirmiran P, Hajipour R, Madjid M, et al. Cardiovascular risk factors in an Iranian urban population: Tehran lipid and glucose study (phase 1) Soz Praventivmed. 2002;47:408–26. doi: 10.1007/s000380200008. [DOI] [PubMed] [Google Scholar]
- 36.Fakhrzadeh H, Larijani B, Bndarian F, Adibi H, Samavat T, Malek Afzali H, et al. Ischemic heart disease associated with coronary risk factors in the population over 25 years of Qazvin: Apopulation. based study. The Journal of Qazvin University of Medical Sciences and Health Services. 2005;35:26–34. [Google Scholar]
- 37.Shamseddini S, Zohor A, Vaji MB, Mirzaei F, Forod A, Kashani M. Blood lipid concentrations and its association with body mass index in the Kerman citizens. Armaghane Danesh. 2002;7:8–15. [Google Scholar]
- 38.Mohamadi-fard N, Sadri GH, Sarraf-zadegan N, Baghaie AM, Shahrokhi SH, Hoseini SH, et al. The prevalence of cardiovascular risk factors in rural and urban population of Isfahan and Markazi provinces. The Journal of Qazvin University of Medical Sciences and Health Services. 2003;7:5–14. [Google Scholar]
- 39.Fakhrzadeh H, Pourebrahim R, Nouri M, Nouri M, Shoushtarizadeh P, Pajouhi M. Distribution of risk factors for cardiovascular disease in the population covered Tehran's population laboratory. Iran J Diabetes Lipid Disord. 2004;3(Suppl 1):53–61. MONICA project. [Google Scholar]
- 40.Agheli N, AsifZadeh S, Rajabi M. Prevalence of risk factors for coronary heart disease in adults over 30 years of Rasht and Qazvin. The Journal of Qazvin University of Medical Sciences and Health Services. 2005;35:59–65. [Google Scholar]
- 41.Amiri M, Emami SR, Nabipour I, Nosraty A, Iranpour D, Soltanian A, et al. Risk factors of cardiovascular diseases in Bushehr port on the basis of the WHO Monica project: The Persian Gulf Healthy Heart Project. Iran S Med J. 2004;2:151–61. [Google Scholar]
- 42.EsmaeiliNadimi A, Kohanali JA. Lipid disorders in Rafsanjan urban population/phase I study of risk factors for coronary artery disease in Rafsanjan. Iran J Diabetes Lipid Disord. 2004;3:149–54. [Google Scholar]
- 43.Namayandeh SM, Sadr SM, Ansarin Z, Rafiei M. A cross-sectional study of the prevalence of coronary artery disease traditional risk factors in Yazd urban population, Yazd healthy heart project. Iran Cardiovasc Res J. 2011;5:7–13. [Google Scholar]
- 44.Nabipour I, Amiri M, Imami SR, Jahfari SM, Nosrati A, Iranpour D, et al. Unhealthy lifestyles and ischaemic electrocardiographic abnormalities: The Persian Gulf Healthy Heart Study. East Mediterr Health J. 2008;14:858–68. [PubMed] [Google Scholar]
- 45.Seyffarshad M, Kousha A, Pourdowlati S, Karamouz M, Farahbakhsh M, Hakimi S, et al. Cardiac risk factor analysis in East Azerbaijan, Iran. Cardiology. 2007;3:1–4. [Google Scholar]
- 46.Chehrei A, Sadrnia S, Keshteli AH, Daneshmand MA, Rezaei J. Correlation of dyslipidemia with waist to height ratio, waist circumference, and body mass index in Iranian adults. Asia Pac J Clin Nutr. 2007;16:248–53. [PubMed] [Google Scholar]
- 47.Alikhani S, Delavari A, Alaedini F, Kelishadi R, Rohbani S, Safaei A. A province-based surveillance system for the risk factors of non-communicable diseases: A prototype for integration of risk factor surveillance into primary healthcare systems of developing countries. Public Health. 2009;123:358–64. doi: 10.1016/j.puhe.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 48.Ghoddosi K, Ameli J, Saadat AR, Farziani VP, Poor FN, Karami GH, et al. Dyslipidemia and its relation with smoking in Tehran. Journal of Gorgan University of Medical Sciences. 2006;8:55–9. [Google Scholar]
- 49.Javadi HR, Azimian J, Rajabi M, Kalantari Z, Javadi M, Esmaiilzadeh H, et al. Prevalence of cardiovascular risk factors among women in Minoodar district of Qazvin; Interventional propositions. The Journal of Qazvin University of Medical Sciences and Health Services. 2009;13:35–43. [Google Scholar]
- 50.Hatmi ZN, Tahvildari S, Gafarzadeh Motlag A, Sabouri Kashani A. Prevalence of coronary artery disease risk factors in Iran: A population based survey. BMC Cardiovasc Disord. 2007;7:32. doi: 10.1186/1471-2261-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Asgari F, Mirzazadeh A, Miri AH. Iran, Tehran: Ministry of Health and Medical Education. Deputy for Health Center for Non-Communicable Disease Control and Management; 2007. Iran Non-Communicable Diseases Risk Factors Surveillance, Data Book for 2007; pp. 1–82. Available in: www.who.int/chp/steps/2007STEPSreportIran.pdf . [Google Scholar]
- 52.Sharifi F, Mousavinasab SN, Soruri R, Saeini M, Dinmohammadi M. High prevalence of low high-density lipoprotein cholesterol concentrations and other dyslipidemic phenotypes in an Iranian population. Metab Syndr Relat Disord. 2008;6:187–95. doi: 10.1089/met.2008.0007. [DOI] [PubMed] [Google Scholar]
- 53.Ministry of Health and Medical Education of Iran. NCD Survey. 2011 [Google Scholar]
- 54.Azizi F, Etemadi A, Salehi P, Zahedi S. Prevalence of metabolic syndrome in an urban population: Tehran lipid and glucose study. Tehran Univ M J. 2003;6:389–99. doi: 10.1016/s0168-8227(03)00066-4. [DOI] [PubMed] [Google Scholar]
- 55.Gharipour M, Bagheri A, Boshtam M, Rabiei K. Prevalence of metabolic syndrome among the adults of central of areas of Iran (as part of “Isfahan Healthy Heart Study”) Journal of Birjand University of Medical Sciences. 2006;13:56–63. [Google Scholar]
- 56.Malek M, Ghorbani R, Rashidipour A, Eskandarian R. Prevalence of low HDL-C cholesterol-high triglycerides in the province of semnan (2005) Iran J Diabetes Lipid. 2009;9:75–80. [Google Scholar]
- 57.Barzin M, Mirmiran P, Afghan M, Azizi F. Distribution of 10-year risk for coronary heart disease and eligibility for therapeutic approaches among Tehranian adults. Public Health. 2011;125:338–44. doi: 10.1016/j.puhe.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 58.Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran lipid and glucose study phase II. Trials. 2009;10:5. doi: 10.1186/1745-6215-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fakhrzadeh H, Tabatabaei-Malazy O. Dyslipidemia and cardiovascular disease. In: Kelishadi R, editor. Dyslipidemia: From Prevention to Treatment. 1st ed. Croatia: InTech; 2012. pp. 303–20. [Google Scholar]
- 60.He J, Gu D, Reynolds K, Wu X, Muntner P, Zhao J, et al. Serum total and lipoprotein cholesterol levels and awareness, treatment, and control of hypercholesterolemia in China. Circulation. 2004;110:405–11. doi: 10.1161/01.CIR.0000136583.52681.0D. [DOI] [PubMed] [Google Scholar]
- 61.Sharma SK, Ghimire A, Radhakrishnan J, Thapa L, Shrestha NR, Paudel N, et al. Prevalence of hypertension, obesity, diabetes, and metabolic syndrome in Nepal. Int J Hypertens 2011. 2011 doi: 10.4061/2011/821971. 821971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Prasad DS, Kabir Z, Dash AK, Das BC. Coronary risk factors in South Asians: A prevalence study in an urban populace of Eastern India. CVD Prev Control. 2010;5:125–32. [Google Scholar]
- 63.United Kingdom Food Standard Agency: The National Diet and Nutrition Survey: Adults aged 19-64 years (Summary Report) [Last accessed on 2004]. Available from: http://www.food.gov.uk/multimedia/pdfs/ndns5full.pdf .
- 64.Costa J, Borges M, Oliveira E, Gouveia M, Carneiro AV. Incidence and prevalence of hypercholesterolemia in Portugal: A systematic review. Part III. Rev Port Cardiol. 2003;22:829–36. [PubMed] [Google Scholar]
- 65.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics - 2013 update: A report from the American Heart Association. Circulation. 2013;127:e6–245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Al-Nozha MM, Arafah MR, Al-Maatouq MA, Khalil MZ, Khan NB, Al-Marzouki K, et al. Hyperlipidemia in Saudi Arabia. Saudi Med J. 2008;29:282–7. [PubMed] [Google Scholar]
- 67.Erem C, Hacihasanoglu A, Deger O, Kocak M, Topbas M. Prevalence of dyslipidemia and associated risk factors among Turkish adults: Trabzon lipid study. Endocrine. 2008;34:36–51. doi: 10.1007/s12020-008-9100-z. [DOI] [PubMed] [Google Scholar]
- 68.Sibai AM, Obeid OA, Batal M, Adra N, El Khoury D, Hwalla N. Prevalence and correlates of metabolic syndrome in an adult Lebanese population. Prev Control. 2008;3:83–90. [Google Scholar]
- 69.Hollman G, Kristenson M. The prevalence of the metabolic syndrome and its risk factors in a middle-aged Swedish population - Mainly a function of overweight? Eur J Cardiovasc Nurs. 2008;7:21–6. doi: 10.1016/j.ejcnurse.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 70.Miccoli R, Bianchi C, Odoguardi L, Penno G, Caricato F, Giovannitti MG, et al. Prevalence of the metabolic syndrome among Italian adults according to ATP III definition. Nutr Metab Cardiovasc Dis. 2005;15:250–4. doi: 10.1016/j.numecd.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 71.Firmann M, Mayor V, Vidal PM, Bochud M, Pécoud A, Hayoz D, et al. The CoLaus study: A population-based study to investigate the epidemiology and genetic determinants of cardiovascular risk factors and metabolic syndrome. BMC Cardiovasc Disord. 2008;8:6. doi: 10.1186/1471-2261-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lin CC, Liu CS, Lai MM, Li CI, Chen CC, Chang PC, et al. Metabolic syndrome in a Taiwanese metropolitan adult population. BMC Public Health. 2007;7:239. doi: 10.1186/1471-2458-7-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rampal S, Mahadeva S, Guallar E, Bulgiba A, Mohamed R, Rahmat R, et al. Ethnic differences in the prevalence of metabolic syndrome: Results from a multi-ethnic population-based survey in Malaysia. PLoS One. 2012;7:e46365. doi: 10.1371/journal.pone.0046365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mula-Abed WA, Chilmeran SK. Prevalence of dyslipidemia in the Iraqi adult population. Saudi Med J. 2007;28:1868–74. [PubMed] [Google Scholar]
- 75.Al-Lawati JA, Mohammed AJ, Al-Hinai HQ, Jousilahti P. Prevalence of the metabolic syndrome among Omani adults. Diabetes Care. 2003;26:1781–5. doi: 10.2337/diacare.26.6.1781. [DOI] [PubMed] [Google Scholar]
- 76.Bahreynian M, Esmaillzadeh A. Quantity and quality of carbohydrate intake in Iran: A target for nutritional intervention. Arch Iran Med. 2012;15:648–9. [PubMed] [Google Scholar]
- 77.Lee MH, Kim HC, Ahn SV, Hur NW, Choi DP, Park CG, et al. Prevalence of dyslipidemia among Korean adults: Korea National Health and Nutrition Survey 1998-2005. Diabetes Metab J. 2012;36:43–55. doi: 10.4093/dmj.2012.36.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ghayour-Mobarhan M, Kazemi-Bajestani SM, Ferns G. Lipid clinics are urgently required in the Iranian public health system. Int J Prev Med. 2010;1:172–5. [PMC free article] [PubMed] [Google Scholar]


