Abstract
Background:
This study was aimed to investigate the main and buffering effects of positive religious coping on the association between the number of chronic medical conditions and major depressive disorder (MDD) among African Americans, Caribbean Blacks and Non-Hispanic Whites.
Methods:
This cross-sectional study used data from the National Survey of American Life, 2001 and 2003. This study enrolled 3,570 African Americans, 1,438 Caribbean Blacks and 891 Non-Hispanic Whites. Number of chronic conditions and positive religious coping were independent variables, 12-month MDD was the outcome and socio-economic characteristics were controls. We fitted the following three ethnic-specific logistic regressions for data analysis. In Model I, we included the number of chronic conditions and controls. In Model II, we added the main effect of religious coping. In Model III, we included an interaction between religious coping and number of chronic conditions.
Results:
Based on Model I, number of chronic conditions was associated with higher odds of 12-month MDD among all race/ethnic groups. Model II showed a significant and negative association between religious coping and MDD among Caribbean Blacks (odds ratio [OR] =0.55, 95% confidence Interval [CI] =0.39-0.77), but not African Americans or Hispanic Whites. Model III suggested that, only among Caribbean Blacks, the effect of chronic medical conditions on MDD is smaller in the presence of high positive religious coping (OR for interaction = 0.73, 95% CI = 0.55-0.96).
Conclusions:
Although the association between multiple chronic conditions and MDD may exist regardless of race and ethnicity, race/ethnicity may shape how positive religious coping buffers this association. This finding sheds more light onto race and ethnic differences in protective effects of religiosity on mental health of populations.
Keywords: African Americans, Caribbean Blacks, chronic medical conditions, ethnicity, major depressive disorder, Non-Hispanic Whites, positive religious coping
INTRODUCTION
In the United States, 133 million adults-almost 1 out of every 2 persons over 18 years of age-have at least one chronic illness.[1] Chronic medical conditions affect individuals for prolonged periods of time placing significant limitations on their social lives. It is believed that about 25% of people with chronic conditions have at least one daily activity limitation.[2] Unfortunately, most patients with chronic medical conditions do not receive proper diagnosis and treatment of concurrent psychiatric comorbidities.[3]
Mental health comorbidities worsen outcomes of chronic medical diseases,[4] possibly due to influence of poor mental health on self-care[5] and disease management.[6] Among patients with chronic diseases, comorbid depression may influence a wide range of outcomes, from symptoms perception,[5] quality of life[7] and medication adherence[8] to service utilization and mortality.[9] Depression may have a negative impact on the outcome of medical illness through biological pathways such as inflammation.
It is well-known that chronic medical conditions of the cardiovascular system,[10,11,12] urinary system,[13] respiratory system,[14,15] gastrointestinal,[16,17] musculoskeletal[18] and endocrine[19] all put the patient at high risk for poor mental health. Although there are studies suggesting that mental health effects of somatic conditions may depend on the type of condition,[20,21] several investigators believe that mental health burden of chronic conditions may be independent of the type of chronic conditions.[22,23]
For a wide range of reasons, the link between chronic medical conditions and depression needs further investigation. Although the link between chronic medical diseases and depression in the clinical settings is already well-established, there is a dearth of knowledge about the same association in the community settings. Most of the available literature originates from studies, which are limited to only one or particular combinations of chronic conditions. Possible buffers of the link between chronic medical diseases and depression are also understudied. Finally, the link between medical conditions and mental health might be under the influence of race and ethnicity;[21,24,25] however, very few empirical studies have focused on race and ethnic differences in this link.
Based on the Transactional Model of Stress and Health, developed by Lazarus and Folkman, coping with stressors explains why mental health consequences associated with stressors may vary among populations. Individuals without functional coping may be at most risk of experiencing distress as a result of exposure to stress, here conceptualized as having multiple medical chronic conditions.[26,27]
Religious coping, defined as using religious behaviors and thoughts in dealing with stressful situations, may have different roles for different ethnic groups.[28,29,30,31,32] Religious coping includes but is not limited to prayer during stressful times and look to God for support, strength and guidance.[33] In some countries such as United States, up to 70% of patients with chronic conditions report use of religious coping to some degree.[34,35] Positive and negative religious coping styles have been reported to be correlated with the level of distress in stressful conditions such as having a chronic condition.[36,37] In general, positive religious coping has been shown to be associated with better well-being and less distress among patients with chronic conditions.[38,39,40] Religious coping may also influence the type of health care utilization.[41]
Race and ethnicity may shape choices of coping strategies that individuals use when they are faced with various stressors.[42] It can be hypothesized that race and ethnicity may shape use and benefits associated with positive and negative religious coping among patients with chronic medical conditions. We already know that use of religious coping is linked to race and ethnicity,[33] as the role of religious coping may be different among Blacks than Whites.[28,29,30,31,32,33]
The current study was conducted to test the main and buffering effects of positive religious coping on the associations between multiple chronic conditions and 12-month major depressive disorder (MDD). We also explored how these effects vary among African Americans, Caribbean Blacks and Non-Hispanic Whites.
METHODS
Data came from the National Survey of American Life (NSAL), 2001-2003. The survey received institutional approval by the Review Board of the University of Michigan. All participants provided consent to participate in the survey.
Participants
The NSAL had applied a national household probability sampling strategy. African Americans were sampled from large cities and other urban/rural areas; however, Caribbean Blacks were only sampled from large cities. A full description of methods, including sampling, has been described.[43,44,45]
Interview
About 86% of the interviews were face-to-face and the remaining 14% were telephone interviews. Each interview lasted about 2 hours and 20 minutes. All interviews were conducted in English and the final response rate was 72%.
Measures
Number of chronic medical conditions
Chronic medical conditions were measured using self-reported history of doctor-diagnosed chronic medical conditions, from 14 medical conditions. Respondents were asked about the following conditions: Arthritis/rheumatism, peptic ulcers, cancer, hypertension, diabetes, chronic liver disease, chronic kidney disease, stroke, asthma, other chronic lung diseases, atherosclerosis, sickle cell disease, heart disease and glaucoma. Self-reported history of doctor-diagnosed chronic medical conditions has been shown to be accurate.[46]
Positive religious coping
The current study used the following two indicators to measure religious coping: (1) How important is prayer when you deal with stressful situations? (2) How much do you look to God for strength, support and guidance? The first question provides an assessment of the significance of prayer in difficult circumstances and the second question reflects an overall orientation toward God as a resource. Responses to the first item included very important (4), fairly important (3), not too important (2) or not important at all (1). Responses to the second item included strongly agree (4), somewhat agree (3), somewhat disagree (2), or strongly disagree (1). Total scores ranged from 0 to 6, with a higher score indicating higher positive religious coping.[33,34]
Outcome
The 12-month MDD was measured using a modified version of the World Mental Health Composite International Diagnostic Interview (CIDI). CIDI is a fully structured diagnostic interview and evaluates a wide range of Diagnostic and Statistical Manual-IV (DSM-IV) mental disorders. CIDI has been used reliably on the World Mental Health project.[47]
Covariates
Socio-demographic characteristics including age, gender, educational level, income, marital status, employment and country region were measured.
Statistical analysis
Stata version 13 (Stata Corp., College Station, TX, USA) was used for data analysis. As the NSAL had a complex sampling design (a multistage sample design involving clustering and stratification), we applied appropriate statistical techniques, which account for the complex design. Weights were applied based on strata, clusters and non-response. Sub-population analyses for surveys were also applied.
Number of chronic conditions and positive religious coping were independent variables, 12-month MDD was the outcome and socio-economic characteristics were controls. We fitted the following three ethnic-specific logistic regressions for data analysis. In Model I, we included the number of chronic conditions and controls. In Model II, we added main effect of religious coping. In Model III, we included an interaction between religious coping and number of chronic conditions. Number of chronic medical conditions and religious coping were entered as a continuous variable. Adjusted odds ratios (or) and 95% confidence intervals (CI) were reported. P < 0.05 were considered to be statistically significant.
RESULTS
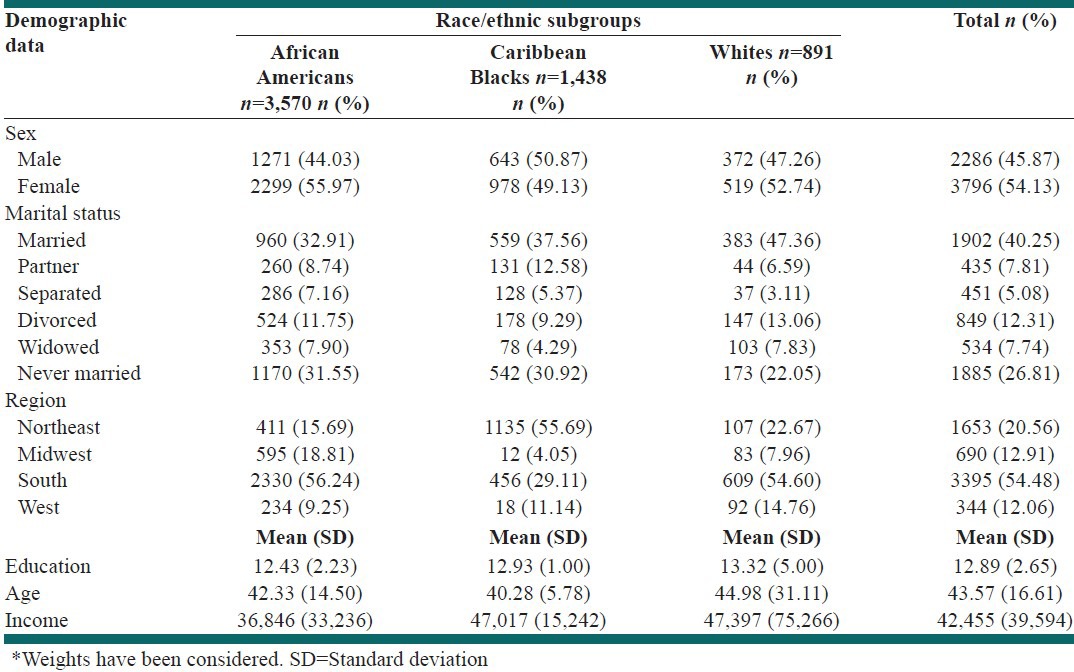
Out of all participants, 985 individuals did not have any chronic conditions, 948 had one chronic condition, 651 had two conditions, 413 had three conditions, 294 had four conditions, 172 had five conditions and 197 had six or more chronic conditions respectively. The socio-demographics of the participants of each race/ethnic group are presented in Table 1.
Table 1.
Socio-economic characteristics among African Americans, Caribbean Blacks and non-Hispanic Whites
Model I
Number of chronic conditions was associated with higher odds of MDD over the last 12 months among all racial and ethnic groups (OR = 1.34, 95% CI = 1.23-1.46 for African Americans, OR = 1.38, 95% CI = 1.02-1.87 for Caribbean Blacks and 1.42, 95% CI = 1.24-1.62 for Non-Hispanic Whites) [Tables 2-4].
Table 2.
Association between number of chronic medical conditions, positive religious coping and depression among African Americans
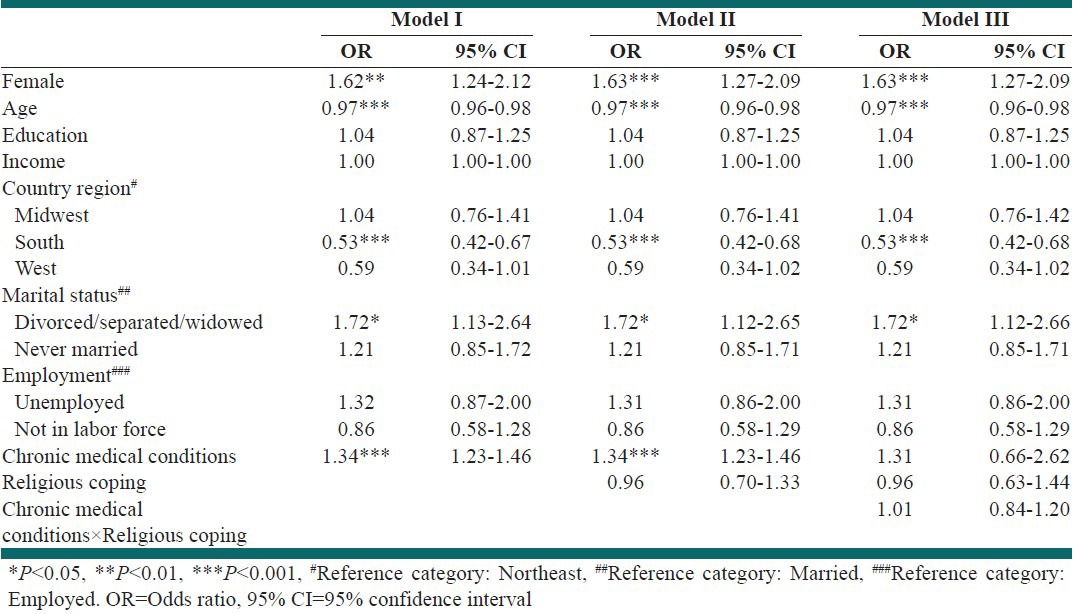
Table 4.
Association between number of chronic medical conditions, positive religious coping and depression among non-Hispanic Whites
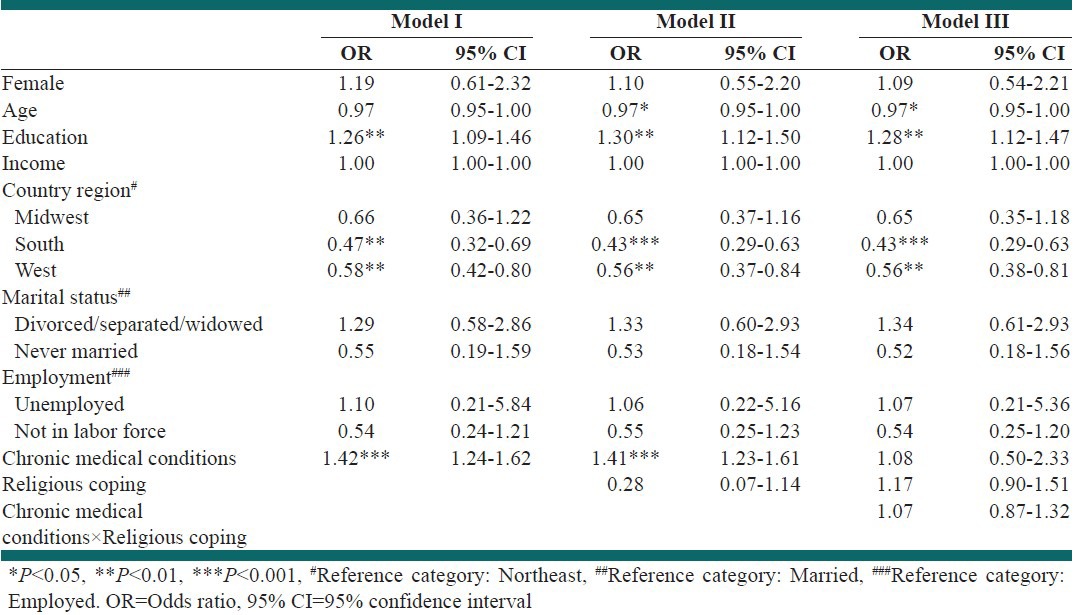
Table 3.
Association between number of chronic medical conditions, positive religious coping and depression among Caribbean Blacks
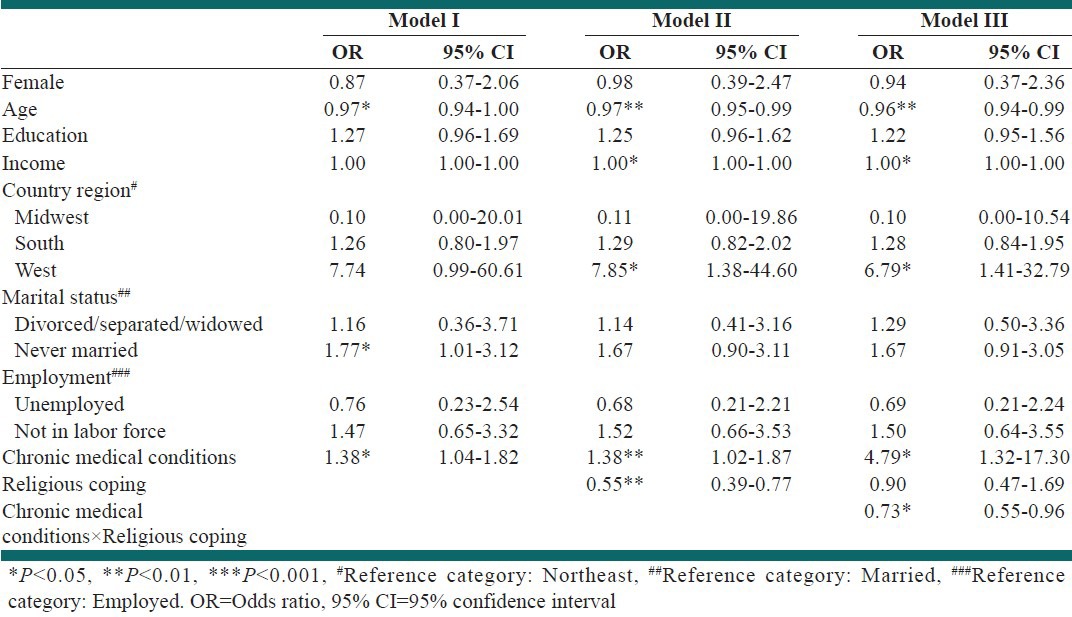
Model II: Main effect
After controlling for number of chronic medical conditions and socio-economic characteristics, religious coping did not have a statistically significant main effect among African Americans (OR = 0.96, 95% CI = 0.70-1.33) or non-Hispanic Whites (OR = 0.28, 95% CI = 0.07-1.14). Higher religious coping was, however, associated with lower odds of MDD over the last 12 months among Caribbean Blacks (OR = 0.55, 95% CI = 0.39-0.77) [Tables 2-4].
Model III: Stress-buffering effect
Interaction between religious coping and number of chronic conditions was significant only among Caribbean Blacks (OR for interaction = 0.73, 95% CI = 0.55-0.96), but not Whites and African Americans. This finding suggests that among Caribbean Blacks, the effect of chronic medical conditions on MDD is smaller in the presence of high religious coping [Tables 2-4].
DISCUSSION
Based on our study, among all race/ethnic groups, multiple chronic conditions were associated with higher odds of 12-month MDD. Religious coping was associated with lower rate of 12-month MDD among Caribbean Blacks but not African Americans and non-Hispanic Whites. Religious coping also showed a buffering effect against the effect of multiple chronic conditions on 12-month MDD among Caribbean Blacks.
Research has suggested that religious coping may be associated with maladaptive or avoidant coping strategies for some people but that it is closely related to problem-focused coping for some others.[48] In one study, positive religious coping was predictive of decreased cumulative health risk only among Hispanic Whites but not non-Hispanic Whites.[49] In another study, European Americans demonstrated a significant, positive relationship between negative religious coping and anxiety symptoms and an opposite trend related to anxiety and positive religious coping. However, no such relationships emerged among the African American sample.[50]
People of different races and ethnicities have different tendencies to use positive and negative religious coping.[51] African Americans and Caribbean Blacks have higher levels of religious coping than non-Hispanic Whites.[41,50] Among African Americans only, Southerners were more likely than respondents who resided in other regions to endorse religious coping. Among Caribbean Blacks, those who emigrated from Haiti were more likely than Jamaicans to utilize religious coping at stressful situations.[34]
Analysis of the NSAL has suggested that race and ethnicity determine which chronic condition is associated with 12-month MDD. That study showed that among African Americans, MDD is linked to hypertension, asthma and other chronic respiratory diseases, whereas among Caribbean Blacks, MDD is associated with arthritis/rheumatism and heart disease.[52] A cross-sectional study of 2,234 adults showed that coronary artery disease and chronic hemodialysis were associated with higher depression symptoms compared with rheumatoid or chronic hepatitis. These studies have suggested that different chronic conditions may require different psychological adjustment and may be dissimilar in terms of a patient's mental health need.[20]
This study reported a moderator of a moderator, by reporting that race/ethnicity moderates the moderating effect of religious coping on the link between medical conditions and MDD. The current study extends our current knowledge about the complex link between race and ethnicity, physical health and mental health. Although it is not advisable or ethical to prescribe religion as a tool for health promotion, our findings may have implications for reducing physical and mental health disparities related to race and ethnicity. Based on our findings, positive religious coping may reduce risk of depression associated with multiple medical conditions among Caribbean Blacks; such a protective effect cannot be found among their African American or non-Hispanic White counterparts. Promotion of positive religious coping as a strategy for prevention of depression may have implications for primary health care workers who provide services to patients of Caribbean countries.
Further research is needed to understand why the protective effect of positive religious coping varies based on race and ethnicity. Research may focus on how race and ethnicity interacts with the effect of positive religious coping on other mental and physical health outcomes, in the presence of stressors. This is especially important because religious coping might be a common coping approach among patients with medical conditions.
Our study had several limitations. The study did not control for other coping resources such as social support that may be associated with religious coping and MDD. This is very important because social support varies according to race and ethnicity. We measured chronic conditions using self-reported physician diagnosed conditions. We did not have data on the validity of self-reports of medical conditions among different race and ethnic groups.[53] Although reporting health may be similar among Blacks and Whites,[54] Whites may be more aware of their health problems due to a better access to health care and more frequent physician visits.
The cross-sectional nature of the data prevents us from establishing true causality between chronic diseases and depression. The sample size for non-Hispanic Whites was considerably smaller than that of African Americans and Caribbean Blacks in the sample; therefore, the results among Whites should be interpreted more cautiously. The study was also limited in not measuring medication for depression. Differential validity of the diagnosis of MDD among racial/ethnic groups may be another limitation of this study. Using the Structured Clinical Interview for DSM-IV as the gold standard, the CIDI diagnosis of MDD may have higher validity among African Americans than that of Caribbean Blacks. CIDI may result in over diagnosis of depression among Caribbean Blacks.[55,56] This study did not measure religious struggle or negative religious coping. In addition, type of medical condition was not entered to the study. Research is needed to understand if the effect of religious coping varies based on the type of medical condition. Finally, the data for this study came from interviews conducted in English.
Our study is one of very few studies that have investigated the moderating effects of race and ethnicity on the moderating effect of religious coping on the link between multiple chronic medical diseases and depression. It extends the literature on the role of religious coping in shaping mental health of patients who deal with chronic conditions[57,58] and also ethnic differences in the protective effect of religiosity on mental health.[28,29,30,31,32]
CONCLUSIONS
Based on our study, irrespective of race and ethnicity, there is a consistent association between number of chronic diseases and 12-month MDD. Positive religious coping may buffer this effect only among Caribbean Blacks but not African Americans or non-Hispanic Whites. This finding emphasizes the role of race and ethnicity in shaping the complex inter-relations between medical conditions, religiosity and mental health of populations.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Wu SY, Green A. Santa Monica, CA: RAND Health; 2000. Projection of Chronic Illness Prevalence and Cost Inflation. [Google Scholar]
- 2.Anderson G. Baltimore, MD: John Hopkins University; 2004. Chronic Conditions: Making the Case for Ongoing Care. [Google Scholar]
- 3.Mikkelsen RL, Middelboe T, Pisinger C, Stage KB. Anxiety and depression in patients with chronic obstructive pulmonary disease (COPD). A review. Nord J Psychiatry. 2004;58:65–70. doi: 10.1080/08039480310000824. [DOI] [PubMed] [Google Scholar]
- 4.Haarasilta L, Marttunen M, Kaprio J, Aro H. Major depressive episode and health care use among adolescents and young adults. Soc Psychiatry Psychiatr Epidemiol. 2003;38:366–72. doi: 10.1007/s00127-003-0644-1. [DOI] [PubMed] [Google Scholar]
- 5.Levenson JL. Psychosocial interventions in chronic medical illness. An overview of outcome research. Gen Hosp Psychiatry. 1992;14(6 Suppl):43S–9. doi: 10.1016/0163-8343(92)90117-s. [DOI] [PubMed] [Google Scholar]
- 6.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. Lancet. 2007;370:851–8. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 7.Gladis MM, Gosch EA, Dishuk NM, Crits-Christoph P. Quality of life: Expanding the scope of clinical significance. J Consult Clin Psychol. 1999;67:320–31. doi: 10.1037//0022-006x.67.3.320. [DOI] [PubMed] [Google Scholar]
- 8.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 9.Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, et al. The functioning and well-being of depressed patients. Results from the Medical Outcomes Study. JAMA. 1989;262:914–9. [PubMed] [Google Scholar]
- 10.Carney RM, Freedland KE, Miller GE, Jaffe AS. Depression as a risk factor for cardiac mortality and morbidity: A review of potential mechanisms. J Psychosom Res. 2002;53:897–902. doi: 10.1016/s0022-3999(02)00311-2. [DOI] [PubMed] [Google Scholar]
- 11.Hackett ML, Anderson CS. Predictors of depression after stroke: A systematic review of observational studies. Stroke. 2005;36:2296–301. doi: 10.1161/01.STR.0000183622.75135.a4. [DOI] [PubMed] [Google Scholar]
- 12.Davidson K, Jonas BS, Dixon KE, Markovitz JH. Do depression symptoms predict early hypertension incidence in young adults in the CARDIA study? Coronary Artery Risk Development in Young Adults. Arch Intern Med. 2000;160:1495–500. doi: 10.1001/archinte.160.10.1495. [DOI] [PubMed] [Google Scholar]
- 13.Kutner NG, Brogan D, Hall WD, Haber M, Daniels DS. Functional impairment, depression, and life satisfaction among older hemodialysis patients and age-matched controls: A prospective study. Arch Phys Med Rehabil. 2000;81:453–9. doi: 10.1053/mr.2000.3878. [DOI] [PubMed] [Google Scholar]
- 14.Wagena EJ, van Amelsvoort LG, Kant I, Wouters EF. Chronic bronchitis, cigarette smoking, and the subsequent onset of depression and anxiety: Results from a prospective population-based cohort study. Psychosom Med. 2005;67:656–60. doi: 10.1097/01.psy.0000171197.29484.6b. [DOI] [PubMed] [Google Scholar]
- 15.Goldney RD, Ruffin R, Fisher LJ, Wilson DH. Asthma symptoms associated with depression and lower quality of life: A population survey. Med J Aust. 2003;178:437–41. doi: 10.5694/j.1326-5377.2003.tb05408.x. [DOI] [PubMed] [Google Scholar]
- 16.Jones MP. The role of psychosocial factors in peptic ulcer disease: Beyond Helicobacter pylori and NSAIDs. J Psychosom Res. 2006;60:407–12. doi: 10.1016/j.jpsychores.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 17.Levenstein S, Kaplan GA, Smith MW. Psychological predictors of peptic ulcer incidence in the Alameda County Study. J Clin Gastroenterol. 1997;24:140–6. doi: 10.1097/00004836-199704000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Dickens C, McGowan L, Clark-Carter D, Creed F. Depression in rheumatoid arthritis: A systematic review of the literature with meta-analysis. Psychosom Med. 2002;64:52–60. doi: 10.1097/00006842-200201000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care. 2001;24:1069–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 20.Bayat N, Alishiri GH, Salimzadeh A, Izadi M, Saleh DK, Lankarani MM, et al. Symptoms of anxiety and depression: A comparison among patients with different chronic conditions. J Res Med Sci. 2011;16:1441–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Fisher L, Laurencin G, Chesla CA, Skaff MM, Mullan JT, Gardiner PS, et al. Depressive affect among four with type 2 diabetes. Diabetes Spectr. 2004;17:215–24.32. [Google Scholar]
- 22.Anderson GM, Grumbach K, Luft HS, Roos LL, Mustard C, Brook R. Use of coronary artery bypass surgery in the United States and Canada. Influence of age and income. JAMA. 1993;269:1661–6. [PubMed] [Google Scholar]
- 23.Alonso J, Ferrer M, Gandek B, Ware JE, Jr, Aaronson NK, Mosconi P, et al. Health-related quality of life associated with chronic conditions in eight countries: Results from the International Quality of Life Assessment (IQOLA) Project. Qual Life Res. 2004;13:283–98. doi: 10.1023/b:qure.0000018472.46236.05. [DOI] [PubMed] [Google Scholar]
- 24.Ferraro KF, Farmer MM. Double jeopardy to health hypothesis for African Americans: Analysis and critique. J Health Soc Behav. 1996;37:27–43. [PubMed] [Google Scholar]
- 25.Wee HL, Li SC, Cheung YB, Fong KY, Thumboo J. The influence of ethnicity on health-related quality of life in diabetes mellitus: A population-based, multiethnic study. J Diabetes Complications. 2006;20:170–8. doi: 10.1016/j.jdiacomp.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 26.Lazarus RS, Folkman S. New York: Springer; 1984. Stress, Appraisal, and Coping. [Google Scholar]
- 27.Lazarus RS. Theory-based stress measurement. Psychol Inq. 1990;1:3–13. [Google Scholar]
- 28.Taylor RJ, Chatters LM, Nguyen AW. Religious participation and DSM IV major depressive disorder among Black Caribbeans in the United States. J Immigr Minor Health. 2013;15:903–9. doi: 10.1007/s10903-012-9693-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor RJ, Chatters LM, Abelson JM. Religious involvement and DSM-IV 12-month and lifetime major depressive disorder among African Americans. J Nerv Ment Dis. 2012;200:856–62. doi: 10.1097/NMD.0b013e31826b6d65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ellison CG, Boardman JD, Williams DR, Jackson JS. Religious involvement stress and mental health: Findings from the 1995 detroit area study. Soc Forces. 2001;80:215–49. [Google Scholar]
- 31.Ellison CG, Musick MA, Henderson AK. Balm in Gilead: Racism religious involvement and psychological distress among African American Adults. J Sci Stud Relig. 2008;47:291–309. [Google Scholar]
- 32.Ellison CG, Flannelly KJ. Religious involvement and risk of major depression in a prospective nationwide study of African American adults. J Nerv Ment Dis. 2009;197:568–73. doi: 10.1097/NMD.0b013e3181b08f45. [DOI] [PubMed] [Google Scholar]
- 33.Chatters LM, Taylor RJ, Jackson JS, Lincoln KD. Religious coping among African Americans, Caribbean Blacks and Non-Hispanic Whites. J Community Psychol. 2008;36:371–86. doi: 10.1002/jcop.20202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thuné-Boyle IC, Stygall J, Keshtgar MR, Davidson TI, Newman SP. Religious coping strategies in patients diagnosed with breast cancer in the UK. Psychooncology. 2011;20:771–82. doi: 10.1002/pon.1784. [DOI] [PubMed] [Google Scholar]
- 35.Ai AL, Park CL, Huang B, Rodgers W, Tice TN. Psychosocial mediation of religious coping styles: A study of short-term psychological distress following cardiac surgery. Pers Soc Psychol Bull. 2007;33:867–82. doi: 10.1177/0146167207301008. [DOI] [PubMed] [Google Scholar]
- 36.Winter U, Hauri D, Huber S, Jenewein J, Schnyder U, Kraemer B. The psychological outcome of religious coping with stressful life events in a Swiss sample of church attendees. Psychother Psychosom. 2009;78:240–4. doi: 10.1159/000219523. [DOI] [PubMed] [Google Scholar]
- 37.Hebert R, Zdaniuk B, Schulz R, Scheier M. Positive and negative religious coping and well-being in women with breast cancer. J Palliat Med. 2009;12:537–45. doi: 10.1089/jpm.2008.0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vallurupalli M, Lauderdale K, Balboni MJ, Phelps AC, Block SD, Ng AK, et al. The role of spirituality and religious coping in the quality of life of patients with advanced cancer receiving palliative radiation therapy. J Support Oncol. 2012;10:81–7. doi: 10.1016/j.suponc.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ramirez SP, Macêdo DS, Sales PM, Figueiredo SM, Daher EF, Araújo SM, et al. The relationship between religious coping, psychological distress and quality of life in hemodialysis patients. J Psychosom Res. 2012;72:129–35. doi: 10.1016/j.jpsychores.2011.11.012. [DOI] [PubMed] [Google Scholar]
- 40.Olson MM, Trevino DB, Geske JA, Vanderpool H. Religious coping and mental health outcomes: An exploratory study of socioeconomically disadvantaged patients. Explore (NY) 2012;8:172–6. doi: 10.1016/j.explore.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 41.Greenawalt DS, Tsan JY, Kimbrel NA, Meyer EC, Kruse MI, Tharp DF, et al. Mental health treatment involvement and religious coping among African American, hispanic, and white veterans of the wars of Iraq and Afghanistan. Depress Res Treat 2011. 2011 doi: 10.1155/2011/192186. 192186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dohrenwend BS, Dohrenwend BP. Oxford, England: Wiley; 1974. Stressful Life Events: Their Nature and Effects. [Google Scholar]
- 43.Jackson JS, Neighbors HW, Nesse RM, Trierweiler SJ, Torres M. Methodological innovations in the National Survey of American Life. Int J Methods Psychiatr Res. 2004;13:289–98. doi: 10.1002/mpr.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jackson JS, Torres M, Caldwell CH, Neighbors HW, Nesse RM, Taylor RJ, et al. The National Survey of American Life: A study of racial, ethnic and cultural influences on mental disorders and mental health. Int J Methods Psychiatr Res. 2004;13:196–207. doi: 10.1002/mpr.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) Int J Methods Psychiatr Res. 2004;13:221–40. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lampe FC, Walker M, Lennon LT, Whincup PH, Ebrahim S. Validity of a self-reported history of doctor-diagnosed angina. J Clin Epidemiol. 1999;52:73–81. doi: 10.1016/s0895-4356(98)00146-2. [DOI] [PubMed] [Google Scholar]
- 47.Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen H. The World Health Organization composite international diagnostic interview short form (CIDI-SF) Int J Methods Psychiatr Res. 1998;7:171–85. [Google Scholar]
- 48.Krägeloh CU, Chai PP, Shepherd D, Billington R. How religious coping is used relative to other coping strategies depends on the individual's level of religiosity and spirituality. J Relig Health. 2012;51:1137–51. doi: 10.1007/s10943-010-9416-x. [DOI] [PubMed] [Google Scholar]
- 49.Rabinowitz YG, Hartlaub MG, Saenz EC, Thompson LW, Gallagher-Thompson D. Is religious coping associated with cumulative health risk? An examination of religious coping styles and health behavior patterns in Alzheimer's dementia caregivers. J Relig Health. 2010;49:498–512. doi: 10.1007/s10943-009-9300-8. [DOI] [PubMed] [Google Scholar]
- 50.Chapman LK, Steger MF. Race and religion: Differential prediction of anxiety symptoms by religious coping in African American and European American young adults. Depress Anxiety. 2010;27:316–22. doi: 10.1002/da.20510. [DOI] [PubMed] [Google Scholar]
- 51.Trevino KM, Archambault E, Schuster J, Richardson P, Moye J. Religious coping and psychological distress in military veteran cancer survivors. J Relig Health. 2012;51:87–98. doi: 10.1007/s10943-011-9526-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.First MB, Spitzer RL, Gibbon M, Williams JB. New York: Biometrics Research, New York State Psychiatric Institute; 1997. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-Patient ed. (SCID-1/NP) [Google Scholar]
- 53.Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness, treatment, and control: The role of neighborhood context. Soc Sci Med. 2007;65:1853–66. doi: 10.1016/j.socscimed.2007.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gibson RC. Race and the self-reported health of elderly persons. J Gerontol. 1991;46:S235–42. doi: 10.1093/geronj/46.5.s235. [DOI] [PubMed] [Google Scholar]
- 55.Williams DR, González HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64:305–15. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 56.Assari S, Moghani Lankarani M, Moazen B, Mokhtari MR, Hayman LW, Caldwell CH. Association between medical chronic diseases and anxiety/depression; Do African Americans, Caribbean Blacks and Non Hispanic Whites differ? J Health Dispar Res Pract. 2014 In Press. [Google Scholar]
- 57.Pargament KI. New York: Guilford; 1997. The Psychology of Religion and Coping: Theory, Research, Practice. [Google Scholar]
- 58.Cummings JP, Pargament KI. Medicine for the spirit: Religious coping in individuals with medical conditions. Religions. 2010;1:28–53. Doi:10.3390/rel1010028. [Google Scholar]


