Abstract
Background:
Malaria is one of the most serious diseases in pregnant women as well as children less than 5 years around the world. The present study aimed to investigate the effect of health education based on the protection motivation theory on malaria preventive behaviors in the households of Ghale Ganj, Kerman, Iran in 2011.
Methods:
The present quasi-experimental study was conducted on 144 households covered by 8 health centers of Ghale Ganj, Kerman. The study samples were selected through systematic random sampling and the study data were collected using a questionnaire including demographic information, the constructs of the protection motivation theory, and a checklist for assessing the malaria preventive behaviors. After the pre-test, the intervention group underwent an educational intervention and after two months, the post-test was performed through the same questionnaire. Then, the data were entered into the SPSS statistical software (v. 18) and analyzed using Chi-square and Wilcoxon non-parametric tests. Besides, P < 0.05 was considered as statistically significant.
Results:
Before the intervention, no significant difference was found between the two study groups regarding perceived vulnerability, perceived severity, response costs, self-efficacy, response efficacy, and malaria preventive behaviors. After the intervention, however, a significant increase was observed in the intervention group's mean scores of all the constructs of the protection motivation theory as well as malaria preventive behaviors (P < 0.01).
Conclusions:
According to the findings of the study, educational intervention based on the protection motivation theory is highly effective in promoting malaria preventive behaviors.
Keywords: Health education, malaria, protection motivation theory
INTRODUCTION
Today, almost 3.3 Billion individuals, i.e. half of the world's population, are at risk of malaria. In fact, malaria, as the most important parasitic disease, is one of the major health problems in some parts of Iran[1,2] and one of the main factors of morbidity in the world.[3]
Based on the annual report of malaria by the World Health Organization (WHO) in 2011, 216 million cases of malaria have occurred in 106 countries around the world in 2010 and 86% of the victims were children below 5 years of age. Of course, the number of the malaria-related deaths in 2010 was reported as 655,000 cases which showed a 5% (36,000 cases) decrease in comparison to 2009. Although this seems to be a significant improvement, these measures are quite alarming for a disease which can be completely prevented and treated.[4]
In general, malaria is considered as a major barrier to the development as well as economic improvement of human communities. In the same line, malaria affects the individual's lives by increasing poverty, limiting education opportunities, and resulting in their being absent from school or work.[5]
Nowadays, malaria is the most important parasitic disease in Iran and mainly involves the southern areas,[4] including Sistan and Baluchistan province, Hormozgan province, and southern part of Kerman province. These areas have been limited by Persian Gulf and Oman Sea in the south and Afghanistan as well as Pakistan in the East. Overall, these provinces comprise 12% of Iran's population and account for 62% of the country's malaria cases.[6]
Furthermore, malaria is one of the major health problems of seven tropical cities in southern Kerman among which, Ghale Ganj has shown the highest rate of both indigenous and imported malaria cases over years. With the annual parasite incidence (API >5 case in 1,000 person), Ghale Ganj is still at the control stage and has not entered the pre-elimination stage,[7] which might be due to the city's being adjacent to some areas of Sistan and Baluchistan and Hormozgan provinces.
Malaria control programs have not been highly successful in tropical as well as subtropical developed countries. Moreover, lack of resources for management of the disease, occurrence of drug-resistance in parasites, and the mosquitoes’ resistance to insecticides has led to the failure of some malaria eradication programs around the world.[8] Overall, due to the epidemiological as well as entomological features, lack of technical success, occurrence of drug resistance in parasites,[9] mosquitoes’ resistance to insecticides, environmental problems, difficulty of biological control,[10] organizational deficiencies, insufficient access to effective healthcare services, urbanization and transfer of human population,[11] the involved countries’ social, cultural, political, economic, and ecological factors, and the economic burden of the disease, the possibility of controlling the disease has been limited.[9] Meanwhile, drug resistance is considered as the greatest challenge against malaria. In fact, resistance to the previous anti-malaria drugs has been shown in all the countries around the world and has resulted in an increase in the mortality of the children.[12] Therefore, malaria prevention educational program is highly essential[13] and more efficient programs have to be designed and conducted. Effective malaria programs consist of multiple interventions with the purpose of control as well as prevention and more emphasis on health education.[14] It has been proved that knowledge, attitude, and malaria-related behaviors in the residents of high-risk areas can increase the awareness as well as the probability of cooperation and acceptance of preventive actions against the disease.[15] Evidence also shows that malaria control programs accompanied by the society members’ cooperation are more effective than those which have been designed and carried out by the government alone. Besides, educational interventions on increasing the preventive actions in the residents of malaria risk areas can play an effective role in planning for controlling as well as preventing the disease.[16]
In general, educational skill is of utmost importance; in a way that educational intervention must be accompanied by planning before, presenting models and patterns during, and assessment after the education.[17] Thus, novel educational methods and theories of health education whose efficiency has been proved should be utilized in order to teach health issues. Considering health education, theory refers to the instruments which help health trainers to develop a better understanding of what has affected the individual's or the group's health as well as basic behaviors and, consequently, design more effective interventions.[18] In the present study, protection motivation theory has been utilized in order to investigate the preventive behaviors against the disease. This theory includes both behavioral and non-behavioral factors[19] involved in the disease. It was developed in 1975 in order to explain the effect of fear from health dangers (e.g. malaria) on health attitudes and behaviors (e.g. protection behavior against the disease) and that fear can affect the selection of behaviors to a great extent. Rogers stated that fear affects the protection motivation through 5 constructs of perceived vulnerability, perceived severity, response efficacy, response costs, and self efficacy;[20] and finally, protection motivation leads to the stimulation of healthy behaviors.
According to this theory (Graph 1),[21] individuals develop a considerable tendency toward accepting the suggested behavior in case their perceived threat is high, i.e. they consider themselves vulnerable to a disease (high vulnerability), they consider a disease as severe and with a great number of complications (high-perceived severity), believe that the suggested behavior can be effective and prevent the disease (high efficiency), consider the costs of performing the behavior low (low response costs), and consider doing the preventive behaviors easy (high self-efficacy).[22]
Graph 1.
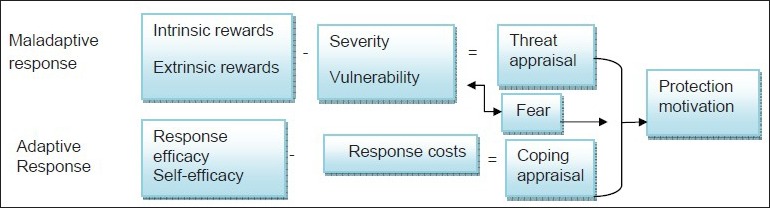
Protection motivation theory
Overall, in order to prevent malaria, both behavioral and environmental factors must be taken into account and on the contrary to some health education theories which only focus on behavioral factors, the protection motivation theory considers both behavioral and environmental factors which the individuals can use in order to protect themselves against diseases and accidents.
Up to now, no educational interventional studies have been conducted on malaria or any other issues in Ghale Ganj, Kerman, Iran. Therefore, the present study aims to investigate the effect of health education based on the protection motivation theory on malaria preventive behaviors in the rural households of this area.
METHODS
The study population of the present interventional, quasi-experimental research included all the households of Ghale Ganj who were selected through cluster and systematic random sampling. Among the 8 health centers of the city, 4 health centers with the highest incidence and prevalence of malaria in the recent years were selected from which, 2 were randomly selected as the control and 2 as the intervention group. According to the sample size formula, i.e., 2δ2(Z1-α/2+Z1-β)2/(μ1-μ2)2, δ=2.1, Z1-α=1.96, CI = 95%, Z1-β=0.84, μ1-μ2=1, and power of 80%, 70 households were selected for each study group. The required households were selected through systematic random sampling by referring to the health houses (n = 22). Of course, considering the probability of loss, this trend was continued in all the health centers until 80 households were selected for each group. The inclusion criteria of the study were being above 15 years old and living in Ghale Ganj. On the other hand, the exclusion criteria of the study were failure in cooperation and not being home after 3 times referring to their houses. At first, 160 households took part in the study (79 in the intervention group and 81 in the control group); however, 16 (7 in the intervention group and 9 in the control group) were excluded due to failure in cooperation and not being home after 3 times referring to their houses. Finally, 144 households (72 in each group) were enrolled into the study.
The study data were gathered through a researcher-made questionnaire including the constructs of the protection motivation theory as well as a checklist of malaria preventive behaviors based on the questionnaire utilized by Rostami[23] and Morovati.[20] In order to determine the content validity of the questionnaire, it was given to the health education as well as medical entomology professors and they were asked to give their opinions through choosing the options of not related, weakly related, related, and strongly related. In case a question was considered as not related or weakly related, it was omitted from the questionnaire (overall, 12 question were omitted). Furthermore, in order to determine the reliability of the questionnaire, it was given to 32 household members similar to the study participants who were not taking part in the study with a 12-day time interval. Using the test-retest method, the correlation coefficients of perceived vulnerability (0.83), perceived severity (0.80), response costs (0.80), self-efficacy (0.80), and response efficacy (0.73) were all at the optimum level. The questions regarding perceived vulnerability (3 questions, score range from 5 to 15), perceive severity (2 questions, score range from 5 to 10), response costs (3 questions, score range from 5 to 15), self-efficacy (3 questions, score range from 5 to 15), and response efficacy (3 questions, score range from 5 to 15) were assessed through the 5-option Likert scale ranging from “completely agree” to “completely disagree”. The items of the checklist of malaria preventive behaviors (7 questions, score range from 7 to 14) had 2 (1 = undesirable, 2 = desirable) options. The ethical considerations of this study included respecting the study participants, explaining the study objectives to the participants before completing the questionnaires, obtaining their consent for participation in the study, not applying personal opinions when completing the questionnaires, and training the control households after accomplishment of the study.
After establishing the coordination with Jiroft University of Medical Sciences, Jiroft, Iran as well as Ghale Ganj health and treatment network and obtaining the households’ consent, the questionnaires were completed for one of the above 15-year-old members of the households by the researcher and two other individuals helping him. This was due to the fact that most of the study participants were illiterate. Then, an educational program on malaria as well as its preventive actions, i.e. filling pits and pools, using bed nets, using nets on doors and windows, and protection against being bitten by anopheles mosquitoes, was conducted by 16 trained health workers for the subjects of the intervention group. This program was performed through group discussion and question and answer methods in at least two hours for each 15 individuals in a period of one month. On the other hand, the members of the control group did not receive any educational interventions. Two months after the end of training by the health workers, the questionnaires were completed again and the data were analyzed using the SPSS statistical software and Chi-square and Wilcox on tests.
RESULTS
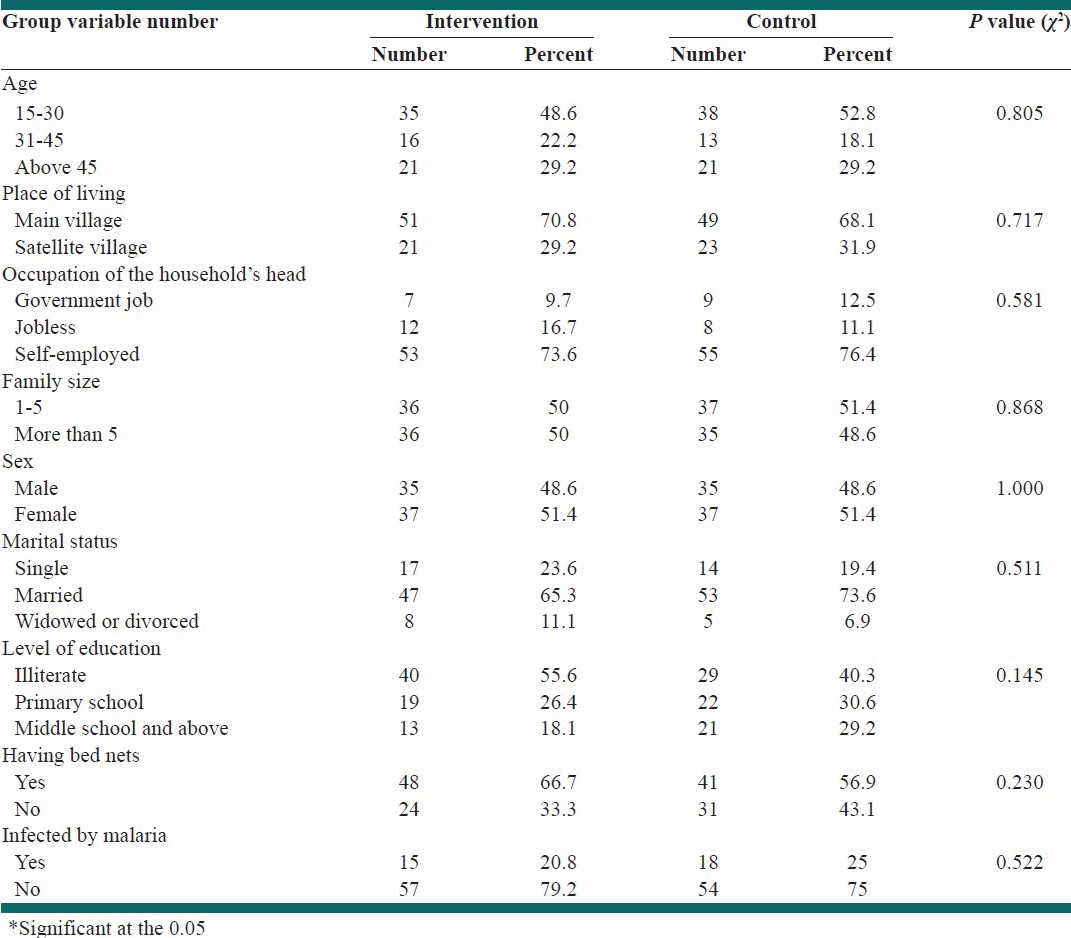
A total of 144 individuals from the study households answered the questions in the present study. According to the results, 50.7%, 20.1%, and 29.2% of the study subjects were in 15-30, 31-45, and above 45 years age groups, respectively. In addition, 69.4% lived in the main village, while 30.6% lived in Satellite village. Furthermore, 11.1%, 13.9%, and 75% of the household heads had government jobs, were jobless, and were self-employed, respectively. The results also revealed that 50.7% of the households had 1-5 members, while 49.3% had more than 5 members. Besides, 48.6% of the study subjects were male and 51.4% were female. In addition, 21.5%, 49.4%, and 9% of the participants were single, married, and widowed or divorced, respectively. Moreover, 61.8% of the households had bed nets at home, while 38.2% did not. Finally, 22.9% of the respondents had got infected by malaria in the past. The results of Chi-square test did not show any significant difference between the two study groups regarding the demographic variables. Results are expressed as significant at P < 0.05 [Table 1].
Table 1.
Relative distribution of the study subjects based on the demographic variables (by Chi-square test)
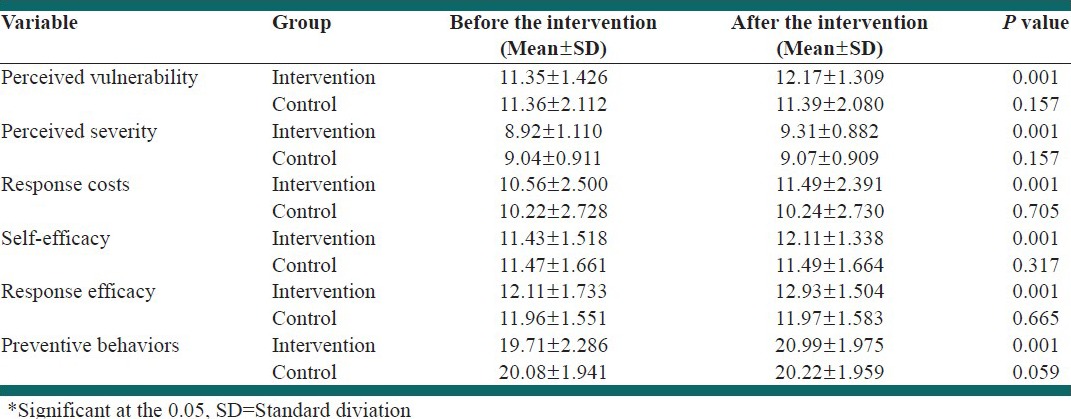
The results of the study revealed no significant difference between the two groups regarding their mean scores of the constructs of the protection motivation theory and malaria preventive behaviors before the intervention. However, the results of Wilcoxon non-parametric test showed a statistically significant difference in the intervention group's perceived vulnerability, perceived severity, response costs, self-efficacy, response efficacy, and malaria preventive behaviors before and after the intervention; results are expressed as significant at P < 0.05 [Table 2].
Table 2.
Comparison of the two groups’ means of the constructs of the protection motivation theory and malaria preventive behaviors before and after the intervention (by Wilcoxon test)
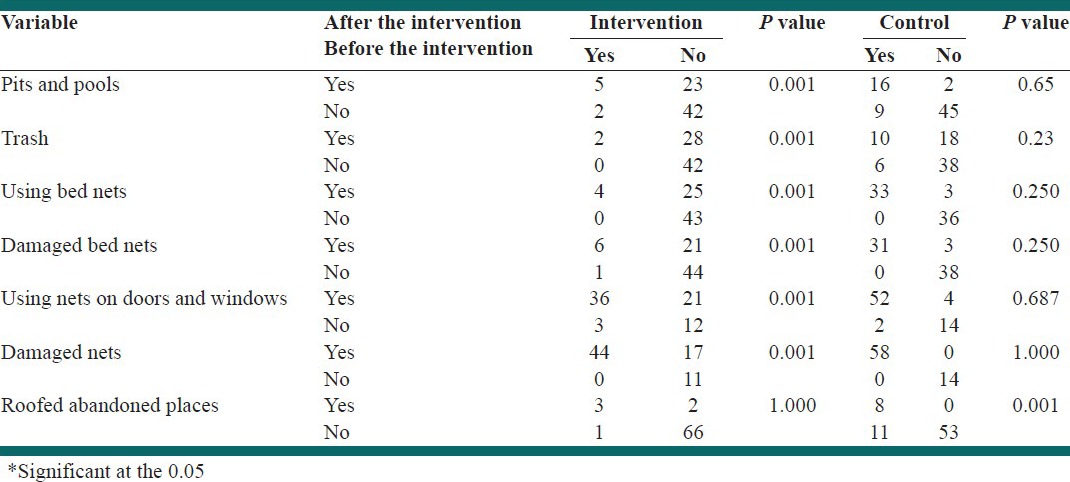
The comparison of the scales of malaria preventive behaviors checklist in the two study groups before and after the intervention (by McNemar test) is presented in Table 3 with significant result at P < 0.05.
Table 3.
Comparison of the frequency and percentage of the constructs of malaria preventive behaviors before and after the intervention in the two study groups (by McNemar test)
DISCUSSION
The present study investigated the effect of education based on the protection motivation theory on malaria preventive behaviors. Till now, the constructs of the protection motivation theory have predicted the preventive behaviors in a great number of studies whose results are going to be discussed in comparison to those of the current research in this section.
In this study, no statistically significant difference was observed between the two groups’ perceived vulnerability scores before the intervention; however, a significant difference was found in the intervention group after the educational intervention. This is in line with a study conducted in Yazd using the protection motivation theory in order for the students to protect themselves against sunrays and prevent skin cancer (P < 0.05).[24] Moreover, McMath conducted a study on the role of individual differences based on the protection motivation theory and the risk of skin cancer and revealed that in comparison to the subjects with low-threat messages, those who had received high-threat messages had gained higher perceived vulnerability scores (P < 0.01).[25,26] The findings of the present study are also consistent with those of the study by McClendon on the effect of intervention based on the protection motivation theory on reducing the risk of skin cancer as well as the ones performed by McGowana[27] and Bassett.[28]
Overall, each individual has a unique understanding of experiencing a particular situation which might be in the opposite direction from one's health. In fact, the individuals’ sensitivity in understanding a situation or disease is highly varied.[29] If the individuals do not feel that they are vulnerable against a health threat, most probably they will not accept the suggested healthy behavior. Thus, perceived vulnerability can play a critical role in the individuals’ intention to accept and continue the healthy behavior.
Regarding perceived severity, a statistically significant difference was observed between the two groups’ scores before and after the intervention, which is in line with the studies performed by baghianimoghadam, McMath, McClendon, McGowana, and Bassett.[24,25,26,27,28] Perceived severity refers to the individuals’ beliefs and the mental effects of a disease or situation as well as the impacts it may have on their life affaires. In fact, these effects can be considered the problems they may create for the individuals.[29] If the individuals believe that being exposed to health threats will be accompanied by average or high complications, the probability of accepting the healthy behaviors might increase to a great extent.
The findings of the current study revealed a statistically significant difference between the two groups’ response costs scores before and after the intervention, which is in agreement with the studies performed by McMath, McClendon, and Lotfi.[25,26,30] In fact, if the individuals believe that they are vulnerable against a health threat, the health threat is serious and accompanied by severe complications, and the costs of doing the health recommendations are quite inappreciable; they will most probably accept the healthy behavior.
Considering the self-efficacy scores, a statistically significant difference was found between the two groups before and after the intervention, which is consistent with the results of the studies conducted by baghianimoghadam, McClendon, Lin, and Mahler,[24,26,31,32] but in contrast with those by Bassett and Bastani.[28,33]
Bandura defines self-efficacy as the individuals’ judgment of their capabilities for doing a particular task and according to his studies, since perceived self-efficacy acts as an independent part of the individuals’ basic skills, it is an important component in their performance. Perceived self-efficacy is in fact the individuals’ beliefs about their capabilities to act in the fields which empower them to control the events affecting their lives; therefore, perceived self-efficacy forms the foundation of the peoples’ deeds.[34]
The findings of the present study showed a statistically significant difference between the intervention group's response efficacy scores before and after the educational intervention, which is in agreement with the results of the studies by baghianimoghadam, McClendon, McGowana, and Lin,[23,24,25,26,30] but on the contrary to those of the research by Bassett.[28]
In general, individuals have limited stimulants for their behaviors unless they believe that desirable outcomes are obtained through what they do.[34] This is in fact response efficacy which is considered as a major component in accepting the healthy behaviors. Considering the results of this study in comparison to those of the other studies, the present research has been quite successful in changing the scores of the constructs of the protection motivation theory in the intervention group.
In this study, no statistically significant difference was observed between the two groups’ malaria preventive behavior scores before the intervention, while a significant difference was found in the intervention group after the educational intervention. Also, the difference between the two groups revealed to be statistically significant (P < 0.001). These results are in line with those obtained by Baghiani Moghaddam as well as Ayi.[24,35]
In general, reducing the exposure to anopheles mosquitoes as well as their bites is one of the protective measures against being infected by malaria,[36] which can be achieved by several preventive behaviors. The results of the present study also showed education based on this theory to be highly effective in malaria preventive behaviors. Overall, healthy behavior is the main focus of health education, in a way that health education is not complete without providing appropriate healthy behaviors.[37] The findings of this study showed the positive effects of the protection motivation theory on changing malaria preventive behaviors in the intervention group.
Considering the items of malaria preventive behaviors checklist, a significant difference was observed in the intervention group regarding using bed nets (P < 0.001), using nets on doors as well as windows (P < 0.001), lack of pits and pools around the house (P < 0.001), lack of trash around the house (P < 0.001), undamaged bed nets (P < 0.001), and undamaged nets on doors and windows (P < 0.001) before and after the intervention. However, non-significant difference was observed in existence of roofed abandoned places in both groups, before and after the intervention. These differences are due to the effect of the educational intervention based on the protection motivation theory on malaria preventive behaviors. Nevertheless, no significant difference was found in the intervention group regarding the existence of roofed abandoned places near the place of living before and after the intervention, which might result from spending considerable financial resources for destroying the roofed abandoned places and constructing new buildings instead of the old ones. These findings are in line with those of the studies conducted by Rostamipour Dolatabad[23] and Geounuppakul;[38] of course, a statistically significant difference was observed in the intervention group regarding the lack of roofed abandoned places and not keeping animals near the house in the study by Rostamipour Dolatabad. According to the evidence, the present study has been successful in changing the majority of the variables of malaria preventive behaviors checklist.
Considering the results of the present study, other similar interventional studies, and Homusou's research,[39] one can conclude that in the people who do not perform malaria preventive behaviors, the goal of malaria preventive behaviors and controlling as well as eliminating the disease can be achieved by health education based on the scientific evidences, through appropriate models and theories, and strengthening as well as full support of the individuals.
A limitation of the present study was that written educational aids could not be used since most of the subjects’ were illiterate. Also, follow up was just 2 months and not followed up in long periods of time for the durable measuring.
CONCLUSIONS
Since the findings of the current study showed a significant difference between the intervention group's mean scores of preventive behaviors and the constructs of the protection motivation theory before and after the intervention, the educational intervention based on the protection motivation theory has been effective in the rural households of Ghale Ganj. The study results suggest that protection motivation theory could be used in order to attract the cooperation of the individuals living in malaria risk areas in doing malaria preventive actions and train such individuals to do environmental actions as well as personal protections for preventing malaria. Further studies are also recommended to be performed on using this theory for preventing malaria in other groups, such as students.
ACKNOWLEDGEMENTS
The present article was adapted from proposal No. 90-5569 which was approved and financially supported by Shiraz University of Medical Sciences, Shiraz, Iran. Hereby, the authors would like to thank the deputy of health of Jiroft University of Medical Sciences as well as the authorities of the health and treatment network of Ghale Ganj for their cooperating in the study. Research Improvement Center of Shiraz University of Medical Sciences and Ms. A. Keivanshekouh are also appreciated for improving the use of English in the manuscript.
Footnotes
Source of Support: Shiraz University of Medical Sciences and Jiroft University of Medical Sciences
Conflict of Interest: None declared
REFERENCES
- 1.World Health Organization (WHO) [Last accessed on 2012 Apr]. Available from: http://www.who.int/features/factfiles/malaria/en/ . Fact sheet N°94.
- 2.Nahravanian H, Asmar M, Raeisi A, Farahmand M, Farzanehnezhad Z, Arshi SH, et al. Seroparasitological evaluation of Plasmodium vivax malaria and stability of the anti-plasmoddial antibodies in Parsabad, Ardabil Province. Shahrekord Univ Med Sci J. 2010;11:57–62. [Google Scholar]
- 3.Geneva: World Health Organization. March; 2010. World Health Organization (WHO): Policy recommendation on intermittent preventive treatment during infancy with sulphadoxine-pyrimethamine (SP-IPTi) for Plasmodium falciparum malaria control in Africa. [Google Scholar]
- 4.Geneva: World Health Organization; 2011. World Health Organization (WHO): World Malaria Report 2011. [Google Scholar]
- 5.Van Damme-Ostapowicz K, Krajewska-Kułak E, Rozwadowska E, Nahorski WL, Olszański R. Quality of life and satisfaction with life of malaria patients in context of acceptance of the disease: Quantitative studies. Malar J. 2012;11:171. doi: 10.1186/1475-2875-11-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mehravaran A, Oshaghi MA, Vatandoost H, Abai MR, Ebrahimzadeh A, Roodi AM, et al. First report on Anopheles fluviatilis U in southeastern Iran. Acta Trop. 2011;117:76–81. doi: 10.1016/j.actatropica.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 7.Tehran (Iran): Ministry of Health; 2008. Ministery of health. Islamic Republic of Iran: Ministry of health strategic program for elimination of malaria (Until 1404) 2008. [Google Scholar]
- 8.Song J, Socheat D, Tan B, Dara P, Deng C, Sokunthea S, et al. Rapid and effective malaria control in Cambodia through mass administration of artemisinin-piperaquine. Malar J. 2010;9:57. doi: 10.1186/1475-2875-9-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hatami H, Razavi M, Eftekharardebili H, Majlesi F, Seiednozadi M, Parizadeh M. Tehran: Arjmand Publication; 2004. Text book of Public health. [Google Scholar]
- 10.Soltani A, Vatandoost H, Jabbari H. Implication of expanded polystyrene and shredded waste polystyrene to control Anopheles spp, Bandar Abbas and Chabahar Iran. Hormozgan Med J. 2009;13:149–57. [Google Scholar]
- 11.Unnikrishnan B, Jaiswal A, Reshmi B. Awareness and treatment seeking behavior of people affected with Malaria in Coastal South India. Iran J Pub Health. 2008;37:119–23. [Google Scholar]
- 12.Geneva: World Health Organization; 2011. World Health Organization (WHO). Global Plan For artemisin in resistance Containment (GPARC) [Google Scholar]
- 13.Hamedi Y. Malaria Drug Resistance in Iran. Hormozgan Med J. 2006;10:93–9. [Google Scholar]
- 14.Cropley L. The effect of health education interventions on child malaria treatment-seeking practices among mothers in rural refugee villages in Belize, Central America. Health Promot Int. 2004;19:445–52. doi: 10.1093/heapro/dah406. [DOI] [PubMed] [Google Scholar]
- 15.Tagliaferri L, Prunotto G, Hakizimana J, Rios WP, Pelucchi C, Principi N, et al. Knowledge of Malaria Among Women of Burundi and its Impact on the Incidence of the Disease. J Trop Pediatr. 2012;58:258–62. doi: 10.1093/tropej/fmr089. [DOI] [PubMed] [Google Scholar]
- 16.Basseri HR, Halakoie Naaini HR, Raeisi A, Shahandeh K. Comparison of knowledge, attitude and practice of Afghan refugees and Iranian, related to transmission and prevention of malaria, in Iranshahr City in 2005-2006. Iran J Epidemiol. 2007;3:7–13. [Google Scholar]
- 17.Fatahi Bafghi A, Karimi H, Anvari MH, Barzegar K. Comparison of lecture and group disscution methods on lerning rate of laboratory students. J Dev Steps Med Sci. 2007;4:51–6. [Google Scholar]
- 18.Safari M, Eftekhar H, Sayed Emami R, Mahmoudi M. Tehran: Asaresobhan Publicaton; 2009. Health education and promotion research methods. [Google Scholar]
- 19.Moravatisharifabad MA, Momeni SM, Barkhordari FA, Fallahzadh H. Predictors of unsafe driving in Yazd City, Based on protection motivation theory in 2010. Horizon Med Sci. 2012;17:49–59. [Google Scholar]
- 20.Morowatisharifabad M, Jowzi F, Barkhordi A, Falahzadeh H. Related factors to workers’ use of hearing protection device in knitting and spinning factories of Yazd city based on Protection Motivation Theory. Iran Occup Health J. 2009;6:50–9. [Google Scholar]
- 21.McClendon BT, Prentice-Dunn S. Reducing Skin Cancer Risk: An Intervention Based on Protection Motivation Theory. J Health Psychol. 2001;6:321–28. doi: 10.1177/135910530100600305. [DOI] [PubMed] [Google Scholar]
- 22.Naito M, O’Callaghan FV, Morrissey S. Understanding Women's mammography intentions: A Theory-Based Investigation. Women Health. 2009;49:101–18. doi: 10.1080/03630240902915119. [DOI] [PubMed] [Google Scholar]
- 23.Rostamipor A. Tehran: Tarbiat Modarres University; 1999. Applicaton of the Health Belief Model in Preventive behaviors to malaria in villages of Kahnooj; p. 182. [Google Scholar]
- 24.Baghianimoghadam MH, Mohammadi S, Noorbala MT, Mazloomy Mahmoodabad SS. An intervention based on protection motivation theory in reducing skin cancer risk. J Pak Assoc Dermatol. 2011;21:141–8. [Google Scholar]
- 25.McMath BF, Prentice-Dunn S. Protection Motivation Theory and Skin Cancer Risk: The Role of Individual Differences in Responses to Persuasive Appeals. J Appl Soc Psychol. 2005;35:621–43. [Google Scholar]
- 26.McClendon BT, Prentice-Dunn S, Blake R, McMath B. The role of appearance concern in responses to intervention to reduce skin cancer risk. Health Educ. 2002;102:76–83. [Google Scholar]
- 27.McGowana EL, Prapavessis H. Colon cancer information as a source of exercise motivation for relatives of patients with colon cancer. Psychol Health Med. 2010;15:729–41. doi: 10.1080/13548506.2010.507771. [DOI] [PubMed] [Google Scholar]
- 28.Bassett SF, Prapavessis H. A test of an adherence-enhancing adjunct to physiotherapy steeped in the protection motivation theory. Physiother Theory Pract. 2011;27:360–72. doi: 10.3109/09593985.2010.507238. [DOI] [PubMed] [Google Scholar]
- 29.Mohammadi N, Rafiaifar SH, Aghamolayie T, Akbari M, Aminshokravi . Tehran: Mehrravash Publication; 2006. Comprehensive program of Health education curriculum. [Google Scholar]
- 30.Lotfi B, Hashemi SZ, Ansari-Moghadam A. Investigation of the Impact of HBM-Based Training on BSE in Women Referred to Health Centers in Zahedan in 2010-2011. J Health Scope. 2012;1:39–43. [Google Scholar]
- 31.Lin D, Li X, Stanton B, Fang X, Lin X, Xu X, et al. Theory-Based HIV-related sexual risk reduction prevention for Chinese Female Rural-to-Urban Migerants. AIDS Educ Prev. 2010;22:344–55. doi: 10.1521/aeap.2010.22.4.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mahler HI, Kulik JA, Harrell J, Correa A, Gibbons FX, Gerrard M. Effects of UV Photographs, Photoaging Information, and Use of Sunless Tanning Lotion on Sun Protection Behaviors. Arch Dermatol. 2005;141:372–80. doi: 10.1001/archderm.141.3.373. [DOI] [PubMed] [Google Scholar]
- 33.Bastani F. The Effect of Education on Nutrition Behavioral Intention and Self- Efficacy in Women. J Health Scope. 2012;1:12–7. [Google Scholar]
- 34.Peyman N, Heidarnia A, Ghofranipour F, Kazemnejad A, Hossein Khodaee G, Amin Shokravi F. The relationship between perceived self-efficacy and contraceptive behaviors among Iranian women referring to health centers in Mashad in order to decrease unwanted pregnancies. J Reprod Fertil. 2007;8:78–90. [Google Scholar]
- 35.Ayi I, Nonaka D, Adjovu JK, Hanafusa S, Jimba M, Bosompem KM, et al. Schoo-based participatory health education for malaria control in Ghana: Engaging children as health messengers. Malar J. 2010;9:1–12. doi: 10.1186/1475-2875-9-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization WHO. [Last accessed on 2012 Apr]. Available from: http://www.who.int/mediacentre/factsheets/fs094/en/, Fact sheet N°94 .
- 37.Sharifi GR, Baghianimoghadam MH, Shamsi M, Rezaaian M. Tehran: Asaresobhan Publicaton; 2009. Research in health education. [Google Scholar]
- 38.Geounuppakul M, Butraporn P, Kunstadter P, Leemingsawat S, Pacheun Ora. An Empowerment Program to Enhance Women's Ability to Prevent and Control malaria in the community, changing Mal Province, Thailand, Southeast Asian. J Tro Med Public Health. 2007;38:546–59. [PubMed] [Google Scholar]
- 39.Houmsou RS, Amuta EU, Sar TT. Malaria Prevention during pregnancy: Awareness and factors contributing to disease occurring among pregnant women in Gboko Metropolis, Benue State, Nigeria. J Med Biomed Sci. 2010;1:36–40. [Google Scholar]


