Abstract
Introduction:
Increasedlife expectancy in populations has brought along specific new scenarios in the fields of medicine for the elderly; prevalence of physical complications such as edentulism and patients with dentures is growing. Management of anesthesia and ventilation in this group of patients has turned into a great challenge. Some researchers suggest dentures to be left in place during bag-mask ventilation; yet, no unanimous agreement exists in this regard.
Methods:
In a single blind randomized clinical trial, we studied 300 patients with ASA class I, II (American Society of Anesthesiologists), Mallampati class (I, II) and aged over 55 years in three groups. After induction of anesthesia, in group G dentures were removed and in each buccal space an eight-layer 10 × 10 cm gauze and an oral airway were placed. In group D, the dentures and an oral airway were left in place. In group C (control), after removing dentures just an appropriate oral airway was placed. Then, each three group underwent bag-mask ventilation. Success of bag-mask ventilation (BMV) was considered as increase in end-tidal carbon dioxide to more than 20 mmHg and back to baseline with fresh gas flow of 3 L/min and adjustable pressure limiting valve pressure of 20 cm H2O. Success rates were evaluated between groups.
Results:
Effective BMV was possible in 91 (91%), 64 (64%) and 41 (41%) patients in groups G, D and C respectively. The differences were statistically significant. Successful BMV rate was significantly higher in female patients in group G compared to group C; 43/44 versus 25/46 individuals, P = 0.0001, odds ratio = 0.03, 95% confidence interval (0.00, 0.22).
Conclusions:
Leaving dentures in place in edentulous patients after inducing anesthesia improves bag-mask ventilation. However, placing folded compressed gauze in buccal space leads to more significant improvement in BMV compared to leaving dentures in place.
Keywords: Bag-mask ventilation, dentures, edentulous patients, end-tidal carbon dioxide, folded gauze
INTRODUCTION
Establishing a secure airway has always been of ultimate priority in providing care and treatment for patients for millennia.[1,2,3,4,5] Bag-mask ventilation, as an undeniable part of airway management, plays a major role in establishing airway not only in patients undergoing general anesthesia but also in those with emergency airway requirements.[6,7,8,9,10,11] Edentulous patients with dentures and required to be intubated are considered a challenge for most anesthesiologists.[3] Routinely in most centers, their dentures are removed prior to being transferred to the operating room. This mostly has been due to the belief that the dentures inside patients’ mouth could cause airway obstruction and compromise the sterility of the surgical field. Although, bag-mask ventilation (BMV) in edentulous patients or those having their dentures removed is difficult, prevalence of edentulism is high among individuals over 65 years (60%) and due to the problem of proper covering of mask in patients with hollow cheeks (caused by edentulism) BMV has turned into a great challenge in these patients.[3,12,13] To overcome this problem various techniques have been introduced including smaller-size oral masks, intraoral Rendell-Baker-Saucek Mask, special anatomical masks, oral airway or nasal mask or even approaches for not removing the dentures.[3,12,13]
Another rarely-reported yet simple way of improving ventilation in edentulous patients is using oral gauze.[3,13] In the present study, we aimed to compare the efficacy of three methods (leaving dentures in place, insertion of folded gauze in buccal space and placing just an appropriate oral airway after removing dentures) in establishing proper airway.
METHODS
In a single blind prospective randomized clinical trial, edentulous patients (n = 300, all over 55 years old) with ASA class I and II referring to the operating room of a referral hospital who were scheduled to undergo cataract surgery under general anesthesia were recruited. The project was approved by the University Ethics Committee and informed written consents were obtained prior to the study. Sample size was calculated based on the following formula and a total of 300 individuals (100 for each group) were calculated:
N = 2 (1.96 + 0.84) 2 * 0.2625 (1 − 0.2625)/(0.35 − 0.175) 2
N = 99.11 ≠ 100(for each group)
Patients not having the criteria for difficult bag mask ventilation, i.e., body mass index ≥31 kg/m2, history of snoring or sleep apnea, thick neck circumference, limited thyromental distance, Mallmapati class III and IV and long beard or mustache were arrived into the study. All patients were edentulous and aged over 55 years old. In addition, patients with nasogastric tube or facial anomalies were not included. Later, patients were randomly divided into three groups of 100 patients by picking a ballot:
Group gauze (G): Patients with removed dentures; in each buccal space, an eight-layer gauze 10 * 10 cm which was quadrupled and an appropriate size oral airway was selected measuring the distance from the corner of the mouth to the tip of the ear and placed between gauzes [Figure 1].
Figure 1.

Placing a folded gauze in the buccal cavities (on the both sides of the airway) in edentulous patients is performed to improve bag.mask.ventilation
Group denture (D): Patients with their dentures in place without oral gauzes; an appropriate size oral airway was placed in the oral cavity.
Group control (C): Patients with their dentures removed; an appropriate size oral airway was placed in order to maintain the airway without placing gauzes in the oral cavity.
BMV of patients was performed by a skilled anesthesiologist who was not a project member. All patients were preoxygenated by oxygen (3 L/min for 5 min). Premedication was performed with fentanyl (1 μg/kg) and midazolam (0.02 mg/kg) 5 min prior to anesthesia induction. All patients were hydrated before anesthesia induction by Ringer's solution 5 ml/kg. Anesthesia induction was performed by propofol (2 mg/kg) and atracurium (0.5 mg/kg). Ventilator was set to the following values: Fresh gas flow = 3 L/min and valve pressure adjustable pressure limiting (APL valve) =20 cm H2O.
The exact time for the evaluation of BMV was determined by a zero TOF using a nerve stimulator following anesthesia induction, i.e., administration of propofol and muscle relaxant; patients being connected to a mainstream capnogram device (Respironics model number: 7100, Respironics California Inc., California) were bag-mask ventilated for 10 times by a skilled anesthesiologist. At the end of each time of ventilation, patients’ end-tidal carbon dioxide (ETCO2) was recorded. Successful BMV was determined as a return to the baseline ETCO2 following increased ETCO2 to more than 20 mmHg at FGF = 3 L/min and APL valve pressure of 20 Cm H2O.
Statistical analysis
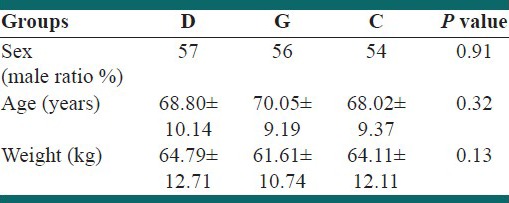
Chi-square test was used for analyzing categorical variables. Odds ratio (OR) and 95% confidence interval (CI) was calculated for point estimations of OR. One-way analysis of variance was used for analyzing age and weight variables for groups of study [Table 1]. P < 0.05 was considered to be significant.
Table 1.
Demographic characteristics of the patients
RESULTS
No significant difference was observed between the three studied groups regarding gender, age and weight distribution [Table 1]. Successful BMV rate was significantly higher in female patients compared with male patients in group C, P = 0.01, OR = 2.827, 95% CI (1.241, 6.441) [Graph 1]. In spite of great success in BMV in female patients of the control group (25 out of 46 patients), the ratio was lower compared with the females in group G (43/44 patients); the difference between two groups was statistically significant [Graph 2]; P = 0.0001, OR = 0.03 CI 95% (0.00, 0.22). The overall success rate was significantly higher in patients of the group D compared to the group C (64% vs. 40%; P = 0.001). On the other hand, successful BMV rate in group G (91/100 patients) was higher comparing to the group D (64/100 patients); the difference between two groups was statistically significant (P = 0.01) [Graph 3].
Graph 1.
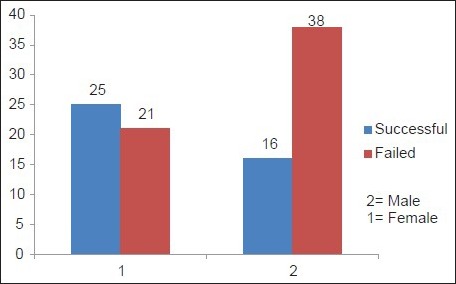
Successful bag-mask ventilation in patients of the control group according to gender distribution (P = 0.01)
Graph 2.
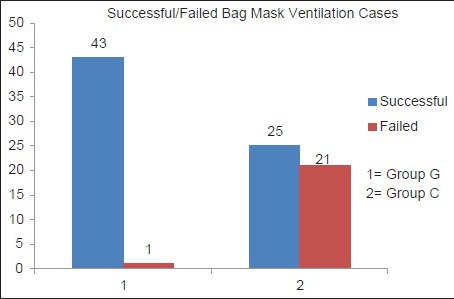
Successful bag-mask ventilation in female patients of the groups C and G (P = 0.0001)
Graph 3.
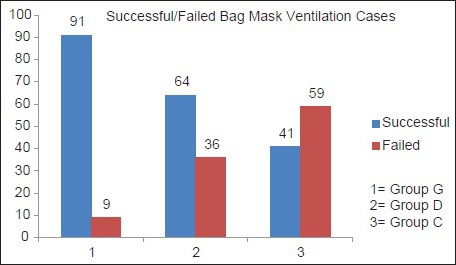
Successful bag-mask ventilation in patients of all groups (G, D and C) (P = 0.01)
DISCUSSION
BMV, as a main essential technique in controlling airway, provides oxygenation and ventilation before securing a stable airway. Thanks to its life-saving properties, BMV is of special importance to the rescuers.[3] Weiss and Lutes showed that endotracheal intubation in traumatic patients does not increase the survival rate compared to BMV.[14] To perform proper BMV the mask should be kept firmly and appropriately in place followed by positive pressure ventilation; this is of so great importance that lack of qualification in BMV is a relative contraindication to its performance. BMV is often used along with oral or nasal airways. To perform effective BMV proper coverage of mouth and nose by mask is essential because there are three major problems in performing sufficient BMV: Insufficient volume of air, poor oxygenation, stomach distention. The two former concerns could be eliminated by full coverage of mouth and nose by mask.[15]
Throughout general anesthesia, muscle tone reduces in oropharynx leading to collapse of the tongue, soft palate and epiglottis contributing to airway obstruction as a factor of difficult BMV in anesthetized patients. Edentulous patients are at increased risk of the obstruction and difficult BMV comparing to patients with teeth.[16,17] Furthermore, these patients have relatively big tongues due to jaw bones cavity and collapse of the tongue in edentulous patients’ mouth.[18] In fact, during anesthesia induction tongue tends to be placed laterally in patients without dentures causing more airway obstruction.[19] The importance of the above-mentioned factors were highlighted in our study; firstly placing compressed folded gauze in buccal space would prohibit the soft-tissue from obstructing the airway and secondly improved mask coverage of patient mouth would contribute to more proper ventilation.
The positioning throughout ventilation is also of importance. Weiss and Lutes in a study showed that BMV whereas the patient is in the supine position and external auditory meatus is aligned with the sternal notch is better compared with sniffing position.[14] Using denture adhesive in patients with nasogastric tube increases expiratory volume comparing to patients without using adhesive.[20] Lack of teeth can be considered a major factor in difficult BMV while very few studies have been conducted to address this concern. In a study carried out by Kheterpal et al., risk factors for difficult BMV were evaluated amongst which lack of teeth also was stated as a significant risk factor.[9] Using dentures and long tubed gauzes packing vestibular cavities in edentulous patients has been reported to improve BMV.[12,13,21,22] Unlike the study of Conlon et al., results of our study demonstrated that placing folded gauze in buccal space was more successful (91% vs. 73%)[12] which could be due to the more accurate exclusion criteria and utilization of skilled anesthesiologists rather than various individuals with various experience and skills in our study as well.
In our study, females without dentures and without folded gauze in their buccal spaces were ventilated better than edentulous males in similar conditions; this major finding has not been mentioned in similar studies. In addition, complete dentures (upper and lower jaws) were used in our study; however, in Colon's study partial dentures (only upper jaw or only lower jaw) were used probably contributing to the differences in the success rates between groups (73% in Colon's vs. 64% in our study). Although using partial dentures, the rest of the teeth are natural and consequently in such cases anatomical changes of tongue and jaw will be less. Therefore, despite associated increased risk of swallowing the dentures, it is expected that the success chance in patients with partial dentures would be higher.[12]
Similar to the study of Kheterpal et al., being male was a prognostic factor in difficult BMV and females without dentures and without folded gauze in their buccal space were ventilated better than males with similar conditions.[9]
Limited alveolar tissue in upper and lower jaws would consequently decrease the volume of the oral cavity and place pressure on the tongue leading to tongue swelling in edentulous patients. This could be prevented by insertion of dentures in patient mouth.[22] However, dentures place pressure on the submandibular soft-tissue and push tongue toward palate causing airway obstruction; especially, in edentulous individuals in which this space is expected to be smaller than those with teeth.[23] Therefore, removal of the dentures and placement of oral gauze throughput BMV seems quite rational as it would be with more appropriate ventilation and less undesirable complications.
Limitations
Our study was a single-center study performed on patients undergoing ophthalmic surgeries. Therefore, further multi-center studies on patients undergoing different surgeries are recommended.
CONCLUSIONS
Findings of our study revealed that leaving dentures in place improves BMV; furthermore, placing folded gauze in buccal space in edentulous patients considerably facilitates BMV. In addition, females without dentures and without any folded gauze in their buccal space are better ventilated than males with similar conditions.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Soleimanpour H, Gholipouri C, Panahi JR, Afhami MR, Ghafouri RR, Golzari SE, et al. Role of anesthesiology curriculum in improving bag-mask ventilation and intubation success rates of emergency medicine residents: A prospective descriptive study. BMC Emerg Med. 2011;11:8. doi: 10.1186/1471-227X-11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soleimanpour H, Panahi JR, Mahmoodpoor A, Ghafouri RR. Digital intubation training in residency program, as an alternative method in airway management. Pak J Med Sci. 2011;27:401–4. [Google Scholar]
- 3.Soleimanpour H, Sarahrudi K, Hadju S, Golzari SE. How to overcome difficult-bag-mask-ventilation: Recents approaches. Emerg Med. 2012;2:e116. [Google Scholar]
- 4.Mahmoodpoor A, Soleimanpour H, Nia KS, Panahi JR, Afhami M, Golzari SE, et al. Sensitivity of palm print, modified mallampati score and 3-3-2 rule in prediction of difficult intubation. Int J Prev Med. 2013;4:1063–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Soleimanpour H, Khoshnudi F, Movaghar MH, Ziapour B. Improvement of decerebrate status in a hanged child following emergent tracheostomy. Pak J Biol Sci. 2010;13:1164–5. doi: 10.3923/pjbs.2010.1164.1165. [DOI] [PubMed] [Google Scholar]
- 6.Soleimanpour H, Shams Vahdati S, Mahmoodpoor A, Panahi JR, Afhami MR, Pouraghaei M, et al. Modified cricothyroidotomy in skill laboratory. J Cardiovasc Thorac Res. 2012;4:73–6. doi: 10.5681/jcvtr.2012.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Golzari SE, Khan ZH, Ghabili K, Hosseinzadeh H, Soleimanpour H, Azarfarin R, et al. Contributions of Medieval Islamic physicians to the history of tracheostomy. Anesth Analg. 2013;116:1123–32. doi: 10.1213/ANE.0b013e3182884313. [DOI] [PubMed] [Google Scholar]
- 8.Soleimanpour H, Gholipouri C, Golzari SE, Rahmani F, Sabahi M. Capnography in the emergency department. Emerg Med. 2012;2:e123. [Google Scholar]
- 9.Kheterpal S, Han R, Tremper KK, Shanks A, Tait AR, O’Reilly M, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006;105:885–91. doi: 10.1097/00000542-200611000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Sokouti M, Montazeri V. Acute nonpenetrating tracheobronchial injuries: What is important in the mortality? J Cardiovasc Thorac Res. 2009;1:5–8. [Google Scholar]
- 11.Mahmoodpoor A, Golzari SE, Hamidi M, Hamidi M, Parish M, Soleimanpour H, et al. Comparison of three methods for laryngeal mask airway insertion in adults: Standard, lateral and rotational. J Clin Anal Med. 2014 In Press. [Google Scholar]
- 12.Conlon NP, Sullivan RP, Herbison PG, Zacharias M, Buggy DJ. The effect of leaving dentures in place on bag-mask ventilation at induction of general anesthesia. Anesth Analg. 2007;105:370–3. doi: 10.1213/01.ane.0000267257.45752.31. [DOI] [PubMed] [Google Scholar]
- 13.Susheela T, Anju G, Reeta S, Kirti K. Edentulous patient and face mask ventilation. Indian J Anesth. 2008;52:347–8. [Google Scholar]
- 14.Weiss AM, Lutes M. ACEP News; 2008. Sep, [Last accessed on 2014 Mar 13]. Focus on-bag-valve mask ventilation. Available from: http://www.acep.org/contentaspx?id=40992 . [Google Scholar]
- 15.Roberts JR, Hedges JR. 5th ed. Philadelphia: Saunders; 2010. Clinical Procedures in Emergency Medicine; pp. 46–8. [Google Scholar]
- 16.Boidin MP. Airway patency in the unconscious patient. Br J Anaesth. 1985;57:306–10. doi: 10.1093/bja/57.3.306. [DOI] [PubMed] [Google Scholar]
- 17.Nandi PR, Charlesworth CH, Taylor SJ, Nunn JF, Doré CJ. Effect of general anaesthesia on the pharynx. Br J Anaesth. 1991;66:157–62. doi: 10.1093/bja/66.2.157. [DOI] [PubMed] [Google Scholar]
- 18.Vogel JE, Mulliken JB, Kaban LB. Macroglossia: A review of the condition and a new classification. Plast Reconstr Surg. 1986;78:715–23. [PubMed] [Google Scholar]
- 19.Cohen AM, Vig PS. Lateral tongue spreading. J Dent. 1973;2:32–4. doi: 10.1016/s0300-5712(73)80007-7. [DOI] [PubMed] [Google Scholar]
- 20.Noguchi T, Shiga Y, Koga K, Shigematsu A. A method to improve a gas leak on mask ventilation in the patient with a nasogastric tube. Anesthesiology. 2001;94:545. doi: 10.1097/00000542-200103000-00041. [DOI] [PubMed] [Google Scholar]
- 21.Sugiyama I, Kazuna S, Aikao W, Tomoko K, Tetsuro I. Use of a denture adhesive for facilitation of mask ventilation in a patient with mandibular protrusion. J Clin Anesth. 2002;26:691–2. [Google Scholar]
- 22.Tan WK, Liu EH, Thean HP. A clinical report about an unusual occurrence of post-anesthetic tongue swelling. J Prosthodont. 2001;10:105–7. doi: 10.1111/j.1532-849x.2001.00105.x. [DOI] [PubMed] [Google Scholar]
- 23.Caruso LJ, Sungur M. Bag and mask ventilation. N Engl J Med. 2007;357:2090–2. doi: 10.1056/NEJMc072473. [DOI] [PubMed] [Google Scholar]


