Abstract
Chronic kidney disease is one of the most common complication of systemic lupus erythematosus, which if untreated can lead to the end-stage renal disease (ESRD). Early diagnosis and adequate treatment of lupus nephritis (LN) is critical to prevent the chronic kidney disease incidence and to reduce the development of ESRD. The treatment of LN has changed significantly over the past decade. In patients with active proliferative LN (Classes III and IV) intravenous methylprednisolone 1 g/m2/day for 1-3 days then prednisone 0.5-1.0 mg/kg/day, tapered to <0.5 mg/kg/day after 10-12 weeks of treatment plus mycophenolate mofetile (MMF) 1.2 g/m2/day for 6 months followed by maintenance lower doses of MMF 1-2 g/day or azathioprine (AZA) 2 mg/kg/day for 3 years have proven to be efficacy and less toxic than cyclophosphamide (CYC) therapy. Patients with membranous LN (Class V) plus diffuse or local proliferative LN (Class III and Class IV) should receive either the standard 6 monthly pulses of CYC (0.5-1 g/m2/month) then every 3rd month or to a shorter treatment course consisting of 0.5 g/m2 IV CYC every 2 weeks for six doses (total dose 3 g) followed by maintenance therapy with daily AZA (2 mg/kg/day) or MMF (0.6 g/m2/day) for 3 years. Combination of MMF plus rituximab or MMF plus calcineurin inhibitors may be an effective co-therapy for those refractory to induction or maintenance therapies. This report introduces a new treatment algorithm to prevent the development of ESRD in children with LN.
Keywords: End-stage renal disease, lupus, nephritis, treatment algorithm
INTRODUCTION
End-stage renal disease (ESRD) is one of the most serious complication of systemic lupus erythematosus (SLE) and caries significant short- and long-term morbidity.[1,2,3,4] Approximately, 50% of SLE patients have clinical evidence of lupus nephritis (LN) at the time of diagnosis, with an even greater incidence of ESRD among children and adolescents.[4,5]
Even with aggressive therapy, some patients with active proliferative LN will have a decline in renal function leading to ESRD.
Recent clinical studies including a number of randomized controlled treatment trials of SLE patients with renal disease have clarified the therapeutic role of a variety of immunosuppressive regimens both in proliferative and membranous LN.[6,7,8,9] The goal of each of these trials has been to achieve clinical efficacy with a remission of the nephritis while minimizing deleterious side effects of treatment.[10,11,12,13,14,15,16,17] The histopathologic classification of LN continues to guide therapy, and treatment for all major classes of LN has seen some shift in management during this time.
The treatment of LN today is markedly different that it was a decade ago.
In this report, we are introducing a newly designed treatment algorithm on how to most effectively prevent the ESRD in children with LN.
Pathogenesis
Genetics and environmental and hormonal factors all play a role in the predilection to SLE and perhaps to LN.[18,19] Autoimmunity is important in the pathogenesis of SLE.[20] The disease process, including a breakdown in self-tolerance, polyclonal hyperactivity of B cells along with defective auto-regulation of T cells that leads to autoantibody production, and deposition of immune deposits with a subsequent inflammatory responses.[18,19,20,21] There is evidence that increased apoptosis and impaired clearance and defective clearance of apoptotic cells facilitate the emergence of anti-DNA antibodies and immune complex formation. The deposition of circulating immune complexes, the in situ formation of others and the activation of complement are major components of glomerular involvement in LN.[21,22] Many factors influence the localization of glomerular immune complexes. These include the size, charge, and avidity of the immune complexes as well as the clearing ability by the mesangium and local hemodynamics.[21] The glomerular localization of immune complexes activates complement-mediated damage, procoagulant factors, leukocyte chemo-attraction, and release of cytokines associated with cellular proliferation and matrix formation. In some patients, vascular and tubulointerstitial damage are prominent.[20,21]
Clinical manifestations
The presentation of childhood LN can be quite variable, often few signs or symptoms exist.[22,23,24,25] From 30% to 50% of patients have clinically evident renal disease at presentation,[23,24] but renal involvement occurs in as many as 60-80% of patients during the disease course and the risk of progression to ESRD is 18-50%.[23,24,25] LN is manifested by proteinuria, micro hematuria with dysmorphic erythrocytes and erythrocyte casts. In some, development of LN is associated with high serum creatinine level and a decline in glomerular filtration rate. Other patients, including those with proliferative disease and some with membranous lupus nephropathy, develop the nephrotic syndrome, hypertension, and anemia. Nephrotic patients with membranous lupus and lupus patients with anti-phospholipid antibodies are particularly pre-disposed to thrombotic complications such as deep vein thrombophlebitis, renal vein thrombosis, and pulmonary emboli.[26] Clinical risk factors at the time of initial presentation include elevated serum creatinine, hypertension, nephrotic range proteinuria, anemia and black and hispanic race and ethinicity.[11]
Renal pathology
All patients with clinical and laboratory evidence of active LN should undergo renal biopsy in order to determine the type and severity of glomerular lesion according to International Society of Nephrology/Renal Pathology Society (ISN/RPS) Classification of LN.[27,28] Biopsy is most highly recommended in patients with SLE who present with abnormal serum creatinine, hematuria, proteinuria >0.5 g/24 h or spot urine protein/creatinine ratio of >0.5 and active urine sediment. In general, clinical renal manifestations correlate well with ISN biopsy classification. With treatment or over time, serial biopsies often show transformation from one histological class to another.
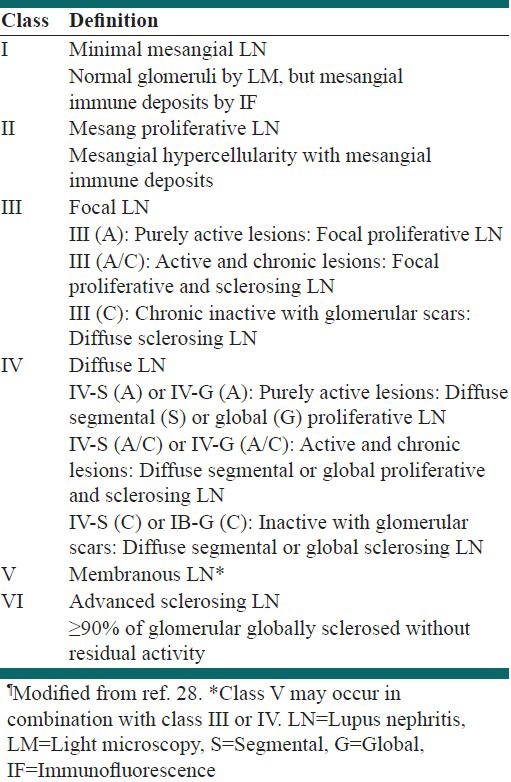
ISN/RPS Class I denotes normal glomeruli by light microscopy but with mesangial immune deposits by immunofluorescence (IF) and electron microscopy. ISN/RPS Class II, which is mesangial proliferative LN, is characterized by mesangial hypercellularity demonstrated by LM, with greater than three mesangial cells in areas away from the vascular pole by LM as well as mesangial immune deposits. ISN/RPS Class III is focal LN, defined as focal segmental and/or global endocapillary and/or extra-capillary glomerulonephritis affecting less than 50% of the glomeruli. ISN/RPS Class IV is diffuse LN. It is characterized by segmental and/or global endocapillary and/or extra-capillary glomerulonephritis affecting more than 50% of glomeruli [Table 1]. Both Class III and IV have sub-endothelial immune deposits. LN Class IV is subdivided into diffuse segmental versus diffuse global proliferation, and both Class III and IV may have active A (proliferative), and inactive chronic C (sclerosing) lesions. ISN Class V is membranous LN defined by sub-epithelial immune deposits. SLE patients may have combined lesions noted as Class III plus V or IV plus V. Class VI is defined as advanced sclerosing LN with more than 90% global glomerular sclerosis. In LN, IgG staining on IF is almost always present and C1q is particularly common. “Full house staining” (the presence of IgG, IgA, IgM, and C3 and C1q) is very suggestive of LN as is IF deposition along the tubular basement membranes and the glomerular basement membranes [Table 1].
Table 1.
International Society of Nephrology/Renal Pathology Society classification of lupus nephritis¶
Treatment
Prompt diagnosis after the onset of LN and subsequent initiation of appropriate therapy are associated with improved outcomes regardless of the histologic subclass.[29] Patients with active proliferative LN (Class III and Class IV) should receive intravenous methylprednisolon (MP) 1.0 g/m2/day for 1-3 days then prednisone 0.5-1.0 mg/kg/day tapered to <0.5 mg/kg/day after 8-12 weeks of treatment plus mycophenolate mofetil (MMF) 1.2 g/m2/day for 6 months followed by maintenance lower doses of MMF 0.6 g/m2/day or azathioprine (AZA) 2 mg/kg/day for 3 years.[30,31]
Kidney disease improving global outcomes (KDIGO) recent guideline for glomerulonephritis recommends cyclophosphamide (CYC) induction therapy for patients with severe proliferative (Class III/IV) LN, with respect to level of proteinuria, and decline in renal function.[32] Furthermore, based on the KDIGO guideline one cannot conclude that induction therapy with MMP is equal or superior to CYC therapy in terms of future renal function and numbers of flares as the long-term follow-up in the randomized clinical trials reported with MMF therapy are shorter than the CYC containing regimen.
Patients with membranous LN (Class V) plus diffuse or local proliferative LN (Class III and Class IV) should receive either the standard 6 monthly pulses of CYC (0.5-1 g/m2/month) followed by infusion every 3rd month or to a shorter treatment course consisting of 0.5 g/m2 IV CYC every 2 weeks for six doses (total dose 3 g) followed by maintenance therapy with daily AZA (2 mg/kg/day) or MMF (0.6 g/m2/day) for 3 years. Both regimens are equally effective, but the shorter regimen is less toxic with fewer severe and total infections.[33,34] Controlled clinical trials and meta-analyses compared treatment with CYC to MMF found that MMF-treated patients had greater reductions in proteinuria, improved renal histology with fewer adverse effects. With the results of these clinical trials, MMF is considered as a first-line induction agent for severe LN.[34,35]
Patients with membranous LN (pure Class V) and subnephrotic proteinuria do extremely well regardless the treatment and may be treated with low doses MMF (1.2 g/m2/day) and prednisone 0.5 mg/kg/day. In Class V LN with nephrotic syndrome both MMF and IV CYC proved equivalent in inducing partial or complete remission of the nephrotic syndrome.[26] Patients with Class VI LN generally do not response to immunosuppression and should be prepared for renal replacement therapy. In a large randomized controlled trial of 86 patients with diffuse proliferative LN (Classes III and IV) with or without membranous LN (Class V) showed that treatment with plasmapheresis, prednisone, and short-term oral CYC led to a more rapid decline in circulating autoantibody levels, but no difference in outcome when compared with prednisone and CYC alone.[36]
In patients fail to respond adequately to induction therapy within 6 months, a switch from either CYC to MMF or from MMF to CYC plus pulse MP followed by daily low dose prednisone is probably more effective than no change in their medications. Combination of MMF plus rituximab or MMF plus calcineurin inhibitors may be an effective co-therapy for those refractory to induction or maintenance therapies.[9,36] [Figure 1]. There are limited data on the use of repeated dosing of rituximab either every 6 months or when the CD19-20 B cell count rises.
Figure 1.
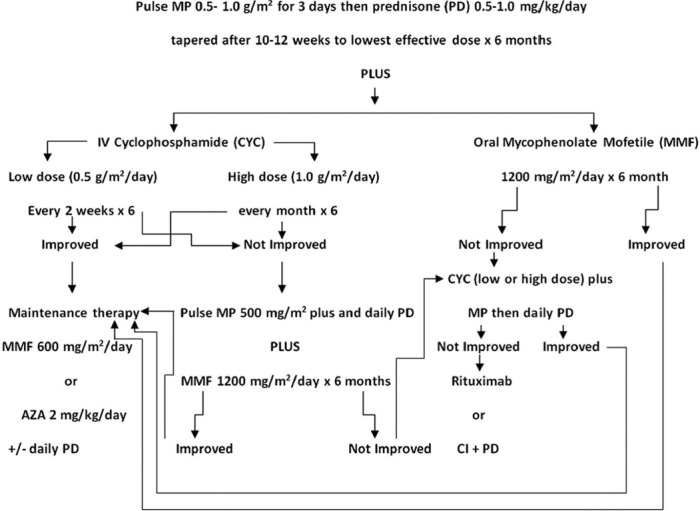
Treatment algorithm for proliferative lupus nephritis (Class III and Class IV). AZA = Azathioprine, CI = Calcineurin inhibitors, CYC = Cyclophosphamide, MP = Methylprednisolone, PD = Prednisone
A number of adjunctive agents have proved helpful in treating LN patients including angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers. Use of hydroxychloroquine is recommended for all patients with LN regardless of the type or severity of glomerular lesions.[5] The use of hydoxychloroquine may help with extra-renal symptoms, but there are only limited data on their effect in renal involvement.
CONCLUSIONS
The treatment of LN has changed significantly over the past decade because of new data from well-conducted randomized clinical trials on how to best treat LN by achieving favorable outcomes with the least amount of therapy-associated toxicities. The current approach to treating LN has largely been guided by histologic findings by ISN/SPN classification with appropriate consideration of presenting clinical parameters and degree of renal impairment. New regimens using lower doses and shorter treatment durations of intravenous CYC have been advanced to reduce toxicity without sacrificing efficacy of therapy. MMF has emerged as a viable alternative to CYC for induction therapy for both proliferative and membranous LN. Large controlled clinical studies using the MMF and AZA for maintenance therapy have been approved.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Bomback AS, Appel GB. Updates on the treatment of lupus nephritis. J Am Soc Nephrol. 2010;21:2028–35. doi: 10.1681/ASN.2010050472. [DOI] [PubMed] [Google Scholar]
- 2.Kasitanon N, Magder LS, Petri M. Predictors of survival in systemic lupus erythematosus. Medicine (Baltimore) 2006;85:147–56. doi: 10.1097/01.md.0000224709.70133.f7. [DOI] [PubMed] [Google Scholar]
- 3.Appel GB, Radhakrishnan J, D’Agati V. Secondary glomerular diseases. In: Taal MW, Chertow GM, Marsden PA, Skorecki K, Yu ASL, Brenner BM, editors. The Kidney. 9th ed. Philadelphia, PA: Elsevier; 2011. pp. 1192–202. [Google Scholar]
- 4.Papadimitraki ED, Isenberg DA. Childhood- and adult-onset lupus: An update of similarities and differences. Expert Rev Clin Immunol. 2009;5:391–403. doi: 10.1586/eci.09.29. [DOI] [PubMed] [Google Scholar]
- 5.Costenbader KH, Desai A, Alarcón GS, Hiraki LT, Shaykevich T, Brookhart MA, et al. Trends in the incidence, demographics, and outcomes of end-stage renal disease due to lupus nephritis in the US from 1995 to 2006. Arthritis Rheum. 2011;63:1681–8. doi: 10.1002/art.30293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gourley MF, Austin HA, 3rd, Scott D, Yarboro CH, Vaughan EM, Muir J, et al. Methylprednisolone and cyclophosphamide, alone or in combination, in patients with lupus nephritis. A randomized, controlled trial. Ann Intern Med. 1996;125:549–57. doi: 10.7326/0003-4819-125-7-199610010-00003. [DOI] [PubMed] [Google Scholar]
- 7.Ranchin B, Fargue S. New treatment strategies for proliferative lupus nephritis: Keep children in mind! Lupus. 2007;16:684–91. doi: 10.1177/0961203307079810. [DOI] [PubMed] [Google Scholar]
- 8.Sundel R, Solomons N, Lisk L aspreva lupus management study (ALMS) group. Efficacy of mycophenolate mofetil in adolescent patients with lupus nephritis: Evidence from a two-phase, prospective randomized trial. Lupus. 2012;21:1433–43. doi: 10.1177/0961203312458466. [DOI] [PubMed] [Google Scholar]
- 9.Nwobi O, Abitbol CL, Chandar J, Seeherunvong W, Zilleruelo G. Rituximab therapy for juvenile-onset systemic lupus erythematosus. Pediatr Nephrol. 2008;23:413–9. doi: 10.1007/s00467-007-0694-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Illei GG, Austin HA, Crane M, Collins L, Gourley MF, Yarboro CH, et al. Combination therapy with pulse cyclophosphamide plus pulse methylprednisolone improves long-term renal outcome without adding toxicity in patients with lupus nephritis. Ann Intern Med. 2001;135:248–57. doi: 10.7326/0003-4819-135-4-200108210-00009. [DOI] [PubMed] [Google Scholar]
- 11.Contreras G, Pardo V, Leclercq B, Lenz O, Tozman E, O’Nan P, et al. Sequential therapies for proliferative lupus nephritis. N Engl J Med. 2004;350:971–80. doi: 10.1056/NEJMoa031855. [DOI] [PubMed] [Google Scholar]
- 12.Houssiau FA, Vasconcelos C, D’Cruz D, Sebastiani GD, Garrido Ed Ede R, Danieli MG, et al. Immunosuppressive therapy in lupus nephritis: The Euro-Lupus Nephritis Trial, a randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum. 2002;46:2121–31. doi: 10.1002/art.10461. [DOI] [PubMed] [Google Scholar]
- 13.Pereira T, Abitbol CL, Seeherunvong W, Katsoufis C, Chandar J, Freundlich M, et al. Three decades of progress in treating childhood-onset lupus nephritis. Clin J Am Soc Nephrol. 2011;6:2192–9. doi: 10.2215/CJN.00910111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Niaudet P. Treatment of lupus nephritis in children. Pediatr Nephrol. 2000;14:158–66. doi: 10.1007/s004670050034. [DOI] [PubMed] [Google Scholar]
- 15.Mak A, Cheak AA, Tan JY, Su HC, Ho RC, Lau CS. Mycophenolate mofetil is as efficacious as, but safer than, cyclophosphamide in the treatment of proliferative lupus nephritis: A meta-analysis and meta-regression. Rheumatology (Oxford) 2009;48:944–52. doi: 10.1093/rheumatology/kep120. [DOI] [PubMed] [Google Scholar]
- 16.Baskin E, Ozen S, Cakar N, Bayrakci US, Demirkaya E, Bakkaloglu A. The use of low-dose cyclophosphamide followed by AZA/MMF treatment in childhood lupus nephritis. Pediatr Nephrol. 2010;25:111–7. doi: 10.1007/s00467-009-1291-x. [DOI] [PubMed] [Google Scholar]
- 17.Hahn BH, Mc Mahon MA, Wilkinson A, Wallace WD, Daikh DI, Fitzgerald JD, et al. American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res (Hoboken) 2012;64:797–808. doi: 10.1002/acr.21664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harley JB, Alarcón-Riquelme ME, Criswell LA, Jacob CO, Kimberly RP, et al. International Consortium for Systemic Lupus Erythematosus Genetics (SLEGEN) Genome-wide association scan in women with systemic lupus erythematosus identifies susceptibility variants in ITGAM, PXK, KIAA1542 and other loci. Nat Genet. 2008;40:204–10. doi: 10.1038/ng.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clatworthy MR, Smith KG. Systemic lupus erythematosus: Mechanism. In: Mason J, Pusey C, editors. The Kidney in Systemic Autoimmune Disease. Amsterdam, Netherlands: Elsevier; 2008. pp. 285–309. [Google Scholar]
- 20.Tsokos GC. Systemic lupus erythrematosus. N Eng J Med. 2011;365:2110–21. doi: 10.1056/NEJMra1100359. [DOI] [PubMed] [Google Scholar]
- 21.D’Agati V, Appel GB. Lupus nephritis: Pathology and pathogenesis. In: Wallace DJ, Hahn BH, editors. Dubois's Lupus Erythematous. 7th ed. Philadelphia, PA: Lippincott and Williams; 2007. pp. 1094–111. [Google Scholar]
- 22.Ataei N, Haydarpour M, Madani A, Esfahani ST, Hajizadeh N, Moradinejad MH, et al. Outcome of lupus nephritis in Iranian children: Prognostic significance of certain features. Pediatr Nephrol. 2008;23:749–55. doi: 10.1007/s00467-007-0713-x. [DOI] [PubMed] [Google Scholar]
- 23.Lee BS, Cho HY, Kim EJ, Kang HG, Ha IS, Cheong HI, et al. Clinical outcomes of childhood lupus nephritis: A single center's experience. Pediatr Nephrol. 2007;22:222–31. doi: 10.1007/s00467-006-0286-0. [DOI] [PubMed] [Google Scholar]
- 24.Hobbs DJ, Barletta GM, Rajpal JS, Rajpal MN, Weismantel DP, Birmingham JD, et al. Severe paediatric systemic lupus erythematosus nephritis: A single-centre experience. Nephrol Dial Transplant. 2010;25:457–63. doi: 10.1093/ndt/gfp481. [DOI] [PubMed] [Google Scholar]
- 25.Appel GB, Contreras G, Dooley MA, Ginzler EM, Isenberg D, Jayne D, et al. Mycophenolate mofetil versus cyclophosphamide for induction treatment of lupus nephritis. J Am Soc Nephrol. 2009;20:1103–12. doi: 10.1681/ASN.2008101028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weening JJ, D’Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, et al. The classification of glomerulonephritis in systemic lupus erythematosus revisited. Kidney Int. 2004;65:521–30. doi: 10.1111/j.1523-1755.2004.00443.x. [DOI] [PubMed] [Google Scholar]
- 27.Markowitz GS, D’Agati VD. The ISN/RPS 2003 classification of lupus nephritis: An assessment at 3 years. Kidney Int. 2007;71:491–5. doi: 10.1038/sj.ki.5002118. [DOI] [PubMed] [Google Scholar]
- 28.Faurschou M, Starklint H, Halberg P, Jacobsen S. Prognostic factors in lupus nephritis: Diagnostic and therapeutic delay increases the risk of terminal renal failure. J Rheumatol. 2006;33:1563–9. [PubMed] [Google Scholar]
- 29.Dooley MA, Jayne D, Ginzler EM, Isenberg D, Olsen NJ, Wofsy D, et al. Mycophenolate versus azathioprine as maintenance therapy for lupus nephritis. N Engl J Med. 2011;365:1886–95. doi: 10.1056/NEJMoa1014460. [DOI] [PubMed] [Google Scholar]
- 30.Walsh M, James M, Jayne D, Tonelli M, Manns BJ, Hemmelgarn BR. Mycophenolate mofetil for induction therapy of lupus nephritis: A systematic review and meta-analysis. Clin J Am Soc Nephrol. 2007;2:968–75. doi: 10.2215/CJN.01200307. [DOI] [PubMed] [Google Scholar]
- 31.Radhakrishnan J, Cattran DC. The KDIGO practice guideline on glomerulonephritis: Reading between the (guide) lines: Application to the individual patient. Kidney Int. 2012;82:840–56. doi: 10.1038/ki.2012.280. [DOI] [PubMed] [Google Scholar]
- 32.Houssiau FA, Vasconcelos C, D’Cruz D, Sebastiani GD, de Ramon Garrido E, Danieli MG, et al. The 10-year follow-up data of the Euro-Lupus Nephritis Trial comparing low-dose and high-dose intravenous cyclophosphamide. Ann Rheum Dis. 2010;69:61–4. doi: 10.1136/ard.2008.102533. [DOI] [PubMed] [Google Scholar]
- 33.Ginzler EM, Dooley MA, Aranow C, Kim MY, Buyon J, Merrill JT, et al. Mycophenolate mofetil or intravenous cyclophosphamide for lupus nephritis. N Engl J Med. 2005;353:2219–28. doi: 10.1056/NEJMoa043731. [DOI] [PubMed] [Google Scholar]
- 34.Radhakrishnan J, Moutzouris DA, Ginzler EM, Solomons N, Siempos II, Appel GB. Mycophenolate mofetil and intravenous cyclophosphamide are similar as induction therapy for class V lupus nephritis. Kidney Int. 2010;77:152–60. doi: 10.1038/ki.2009.412. [DOI] [PubMed] [Google Scholar]
- 35.Lewis EJ, Hunsicker LG, Lan SP, Rohde RD, Lachin JM. A controlled trial of plasmapheresis therapy in severe lupus nephritis. The Lupus Nephritis Collaborative Study Group. N Engl J Med. 1992;326:1373–9. doi: 10.1056/NEJM199205213262101. [DOI] [PubMed] [Google Scholar]
- 36.Edelbauer M, Jungraithmayr T, Zimmerhackl LB. Rituximab in childhood systemic lupus erythematosus refractory to conventional immunosuppression: Case report. Pediatr Nephrol. 2005;20:811–3. doi: 10.1007/s00467-004-1760-1. [DOI] [PubMed] [Google Scholar]


