Abstract
Background:
The current study examined race and ethnic differences in the separate and combined (additive) effects of anxiety, depression and problem drinking on the baseline and trajectory of subjective health among adult men in the United States.
Methods:
This longitudinal study used data from the Fragile Families and Child Well-being Study. We included 4,655 men, composed of 2,407 Blacks, 1,354 Hispanic Whites and 894 non-Hispanic Whites. The dependent variable was subjective health, measured four times (i.e., baseline, year 1, year 3 and year 5). Latent growth curve modeling was used for data analysis. When controlling for socio-economics, we tested separate effects of anxiety and depression. Then we tested combined effects of anxiety, depression and problem drinking.
Results:
Among all race and ethnic groups, anxiety and problem drinking were associated with baseline and trajectory of subjective health. Combined (additive) effects of anxiety and depression, however, varied based on race and ethnicity. Among Blacks, depression and anxiety were associated with a worse trajectory of subjective health. Among non-Hispanic Whites, anxiety was associated with a better baseline and worse trajectory of subjective health, while depression was associated with worse baseline subjective health. Among Hispanic Whites, anxiety was associated with a worse trajectory of subjective health, while depression was not associated with subjective health.
Conclusions:
Although separate effects of anxiety and problem drinking were similar among race and ethnic groups, race and ethnicity seemed to modify the combined effects of different mental health problems. These results warrant further exploration of these complex links.
Keywords: Anxiety disorder, blacks, depressive disorder, Hispanic Whites, non-hispanic Whites, problem alcohol use, subjective health
INTRODUCTION
Mental health problems and psychiatric disorders are associated with lower levels of subjective health and quality of life among individuals.[1,2,3] Studies among diverse samples have consistently shown that the presence of anxiety,[4,5,6] depression,[7,8,9] and problem alcohol use[10] are all inversely correlated with perceived well-being, self-rated health and life satisfaction. Most of this literature, however, has not controlled for the effect of comorbid psychiatric disorders.
Individuals with high anxiety symptoms report poor general health, physical distress and activity limitations.[11] Among patients with chronic medical conditions, depressive symptoms predict health related quality of life (HRQOL) after controlling for functional status, demographics and clinical variables.[10] Problem drinking also predicts low life satisfaction, less frequent positive affect and more frequent negative affect.[10]
Mental health problems may, however, differ in their effects on subjective well-being. For instance, a study on a community sample in the United States showed that while anxiety, depression and alcohol use all adversely influence the quality of life, the patterns of their effects vary. The study showed similar adverse effects of anxiety and depression on psychological, physical and social functioning, whereas alcohol use disorder affected role functioning but not other domains of life.[12]
There are various reasons why further research is needed on race and ethnic differences in the complex relations between psychiatric disorders and subjective health. First, literature on the association between mental health and subjective health has provided mixed results. For instance, negative linear,[13,14] curvilinear (inverse J shaped),[15] and positive linear[16] association between consumption of alcohol and perceived health has been found in different countries and cultures.
In addition, most of the studies that have shown a link between poor mental health and subjective health have had a cross-sectional design. There are very few studies measuring the influence of baseline risk and protective factors on the trajectory of subjective health.[11] In addition, most of the studies in this field have been conducted in the clinical setting and limited information exists on the same associations in the community setting.[11,17] Most longitudinal studies that have investigated the association between mental health problems and trajectory of subjective health[17] have assumed a linear change of subjective health over time. In other words, most studies have used traditional statistical techniques for longitudinal data analysis that only models the average slope. Latent growth curve modeling (LGCM), however, has enabled us to also estimate the non-linear change of an outcome. Availability of modeling packages, such as Mplus[18] and analysis of moment structures (AMOS)[19] have recently facilitated the testing of non-linear trajectories of health outcomes. These techniques have only recently been applied to examine HRQOL trajectories,[20,21] and authors are not aware of any study on the association between mental health problems and linear and non-linear trajectories of subjective health.
Finally, there is a need to study these associations among men and women, separately.[16] Female binge drinkers, for instance, have reported more physically and mentally unhealthy days than male binge drinkers.[22] Similar gender differences may exist for the effect of other mental health problems on well-being.
The current study aimed to examine race and ethnic differences in separate and combined (additive) effects of anxiety, depression and problem drinking on the baseline and trajectory of subjective health. In this regard, we used LGCM that enables us to model both linear and nonlinear trajectories of subjective health over time.
METHODS
For this study, we used data from the first four waves of the Fragile Families and Child Well-being Study (FFCWS). This is an ongoing large population-based cohort, started in 1998. The study has randomly sampled families in 20 U.S. cities with population of 200,000 or more. A detailed description of sampling and interview protocol of this study has been published elsewhere.[23]
We included 4,655 male adults (2,407 Blacks, 1,354 Hispanic Whites and 894 non-Hispanic Whites). The FFCWS has oversampled non-married couples[23] and is not representative of the United States. As non-marital unions are less stable than marital unions, a large number of cohabiting couples at baseline do not live together in subsequent waves. For instance, by Wave II, fewer than half of male partners were residing in the home with their female partner.
Data were collected at baseline (Wave I) and then 1 year later (Wave II), 3 years later (Wave III) and 5 years later (Wave IV) later. Socio-economic factors were measured at Wave I, anxiety, depression and problem drinking were measured at Wave II and subjective health was measured at Waves I - IV.
Measures
Major depressive disorder
The Composite International Diagnostic Interview-Short Form (CIDI-SF), Section A[24,25,26,27] was used to measure major depressive disorder. The CIDI-SF is a standardized instrument that is consistent with DSM-III-R (American Psychiatric Association, 1994) to determine the probability that the respondent would be diagnosed with major depressive disorder if given the full CIDI interview. Major depressive disorder is indicated by feelings of depression or anhedonia experienced for most of the day, every day, for at least 2 weeks. Participants were classified as likely to have major depressive disorder if they endorsed the screening items and 3 or more depressive symptoms (e.g., losing interest, feeling tired, change in weight) (0 = no, 1 = yes).
Generalized anxiety disorder
The CIDI-SF was used to measure generalized anxiety disorder.[24,25,26,27] The diagnosis is based on DSM-III-R (American Psychiatric Association, 1994). The CIDI-SF has good reliability and validity.[24,25,26,27] Generalized Anxiety Disorder is indicated by a period of 6 months or more when an individual feels excessively worried or anxious about more than one thing, more days than not and has difficulty controlling their worries. Common symptoms include being keyed up or on edge, irritability, restlessness, having trouble falling asleep, tiring easily, difficulty concentrating and tense or aching muscles. Subjects were classified as having generalized anxiety disorder if they met full diagnostic criteria based on the CIDI-SF (0 = no, 1 = yes).
Problem alcohol use
Problem alcohol use was defined as five or more drinks (coded “1”) or less (coded “0”) during the past month. This measure approximates the National Institute on Alcohol and Alcoholism definition of heavy drinking days (i.e., five or more drinks in a single day for men; NIAAA, 2005).
Covariates
Control variables in this study included age, education level, income and relationship status, measured at baseline interview (Wave 1).
Main outcome
We used the following single item to measure subjective health: How is your health? Five scale responses including Great, Good, Fair and Poor were used.[28,29,30,31] Single item measures of subjective health have been used frequently in the literature.[32,33,34,35] Test retest reliability for single items range from 0.7 to 0.8 for the brief time intervals.[28] Validity results commonly have shown surprisingly high correlations between single-item indicators and much longer scales. These single-item scales are very attractive for national surveys because they are cost-effective and simple to apply.[36]
Analysis plan
We used SPSS 21.0 (IBM Corporation, Armonk, NY, USA) for univariate and bivariate analysis. We used Pearson's correlation to test for our bivariate associations between control variables, problem alcohol use, depression, anxiety and perceived health.
We used AMOS for multivariable analysis. We fitted multi-group LGCM, which is a type of structural equation modeling. We defined our groups based on race and ethnicity. In our models, we tested paths from depression, anxiety and problem alcohol use and control variables to intercept, linear slope and quadratic slope of subjective health. A comparative fit index (CFI) of higher than 0.90 was indicative of acceptable fit.[37] Although variables measured at baseline data did not have missing values, variables measured at Wave II data had a missing value in <10% of cases.
We run a series of models for our data analysis. Models I-III tested separate effects of anxiety, depression and problem drinking. Model I included anxiety and socio-economic status as possible predictors of baseline and trajectory of self-rated health. Model II included depression and socio-economic status as possible predictors of baseline and trajectory of self-rated health. Model III included problem alcohol use and socio-economic status as possible predictors of baseline and trajectory of self-rated health. Model IV measured combined effects of these predictors and included anxiety, depression, problem alcohol use and socio-economic status to the model [Figure 1a-d].
Figure 1.
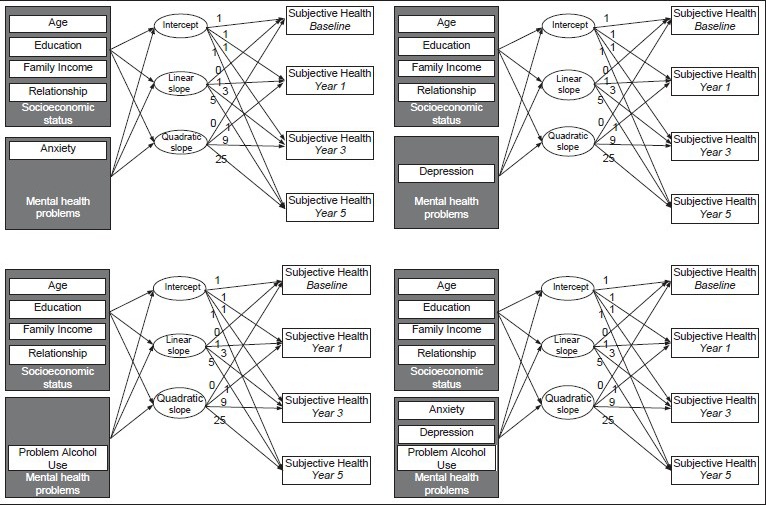
Diagram of the modeling approach. Models I-III tested the separate associations of anxiety, depression, and problem alcohol use with baseline and trajectory of subjective health. Model IV tested the combined effects of anxiety, depression, and problem alcohol use. Multi-group analysis has been used in all cases, where group is based on race and ethnicity
RESULTS
2,407 (49.1%) were Blacks, 1,354 (27.6%) were Hispanic Whites and 894 (18.3%) were non-Hispanic Whites.
Model I
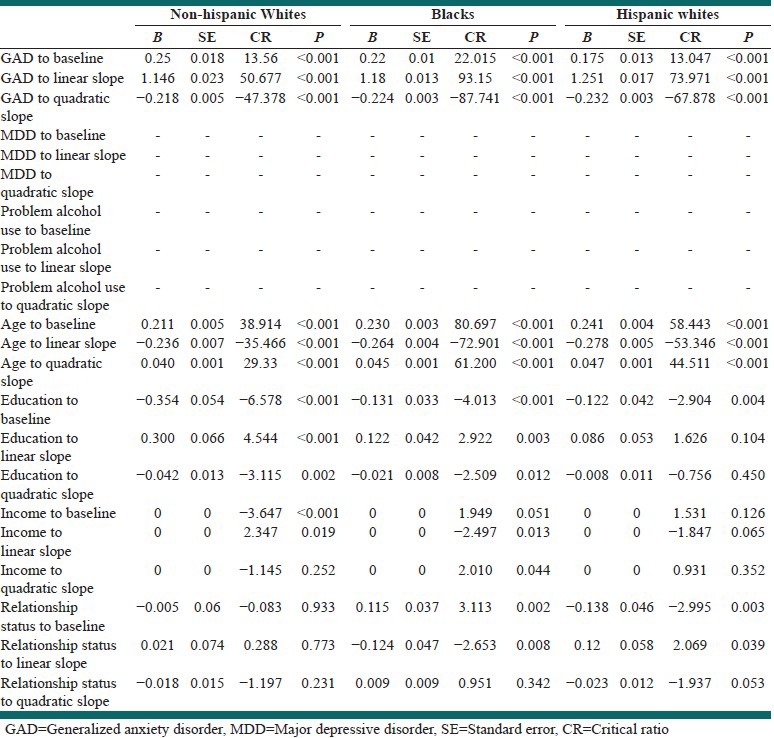
The Model I which measured separate effect of anxiety on the baseline and trajectory of self-rated health did not fit the data very well (Chi-square = 3970.234, P < 0.001, CFI = 0.882). Based on this model, among all three race/ethnic groups, anxiety was associated with a worse baseline and a better trajectory of self-rated health over time [Table 1, Figure 1a].
Table 1.
Results of Model I to test separate effect of anxiety on the baseline and trajectory of poor subjective health among men in the United States
Model II
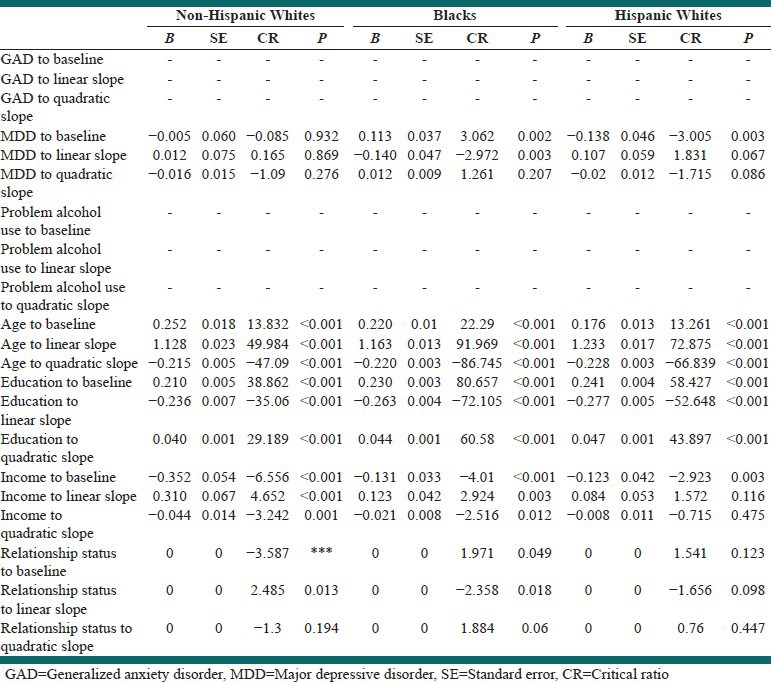
Model II which included depression and socio-economic status did not fit data very well, either (Chi-square = 188.318, P < 0.001, CFI = 0.882). Based on this model, among Blacks and Hispanic Whites, depression was associated with baseline and trajectory of self-rated health over time [Table 2, Figure 1b].
Table 2.
Results of Model II to test the separate effect of depression on the baseline and trajectory of poor subjective health among men in the United States
Model III
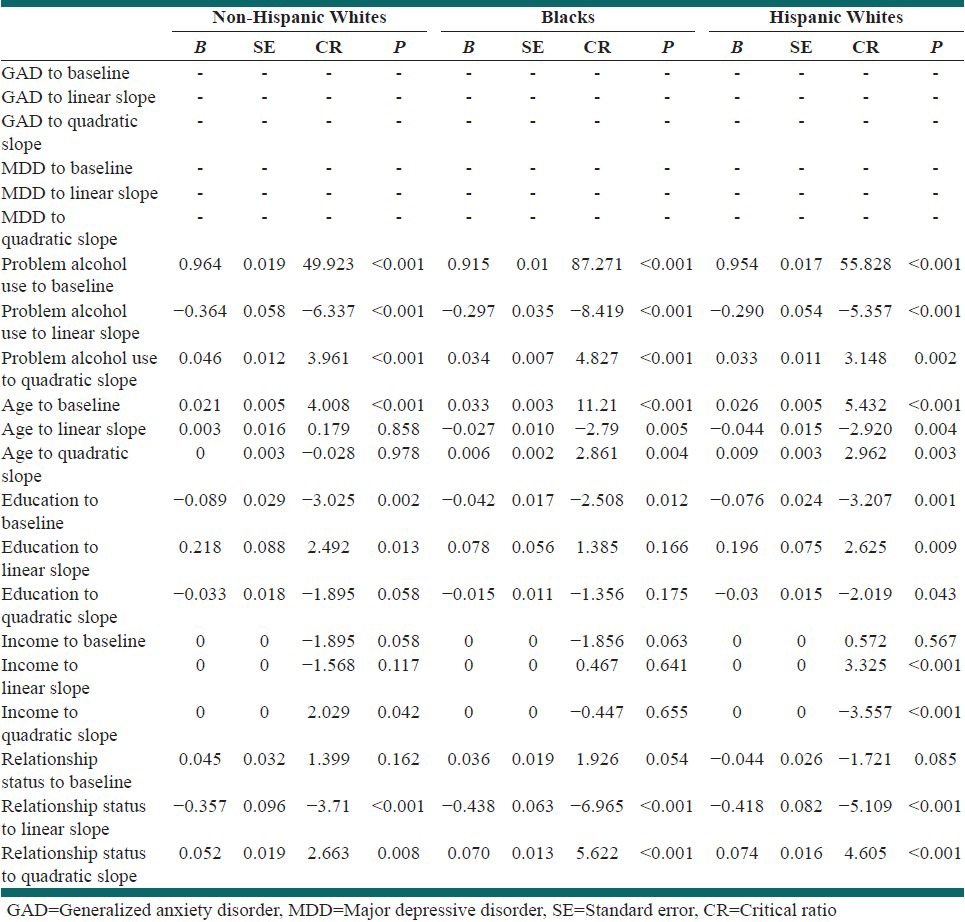
Although Model III only included problem alcohol use and socio-economic status, the model showed acceptable fit (Chi-square = 357.542, P < 0.001, CFI = 0.989). Based on this model, among all three race/ethnic groups, problem alcohol use was associated with a worse baseline and also a worse trajectory of self-rated health over time [Table 3, Figure 1c].
Table 3.
Results of Model III which tests the separate effects of problem alcohol use on the baseline and trajectory of poor subjective health among men in the United States
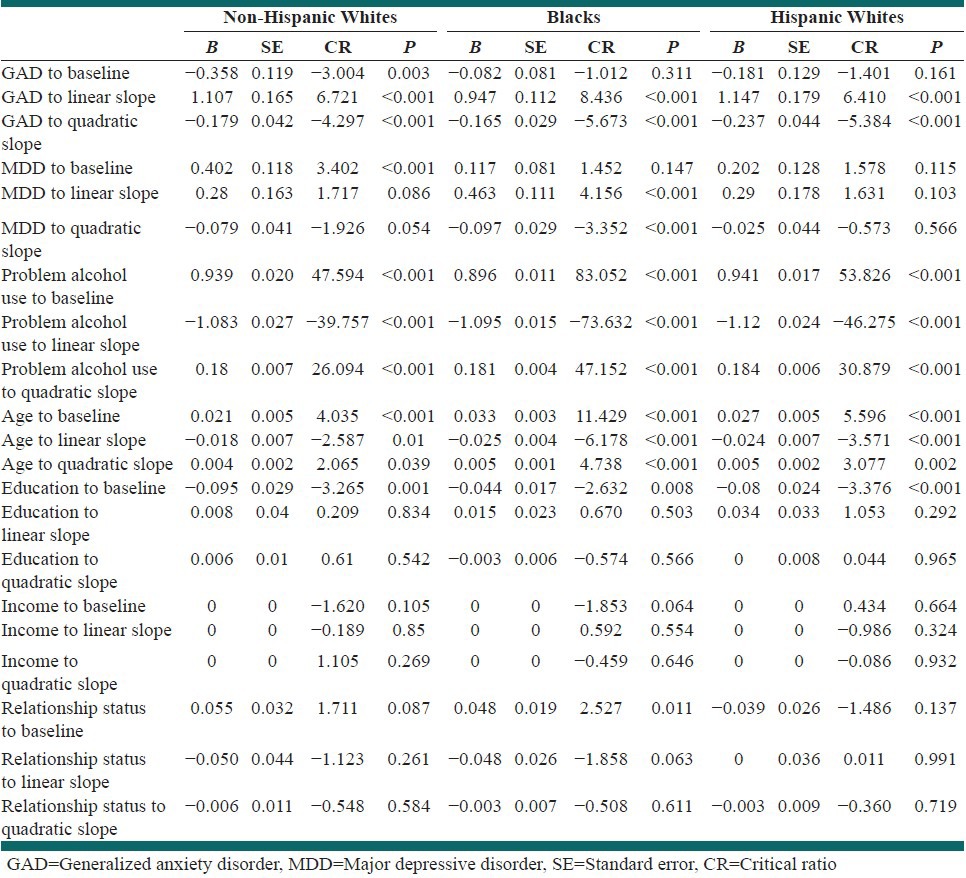
Model IV
Model IV that tested the combined effects of anxiety, depression, problem alcohol use and socio-economic status on the baseline and trajectory of self-rated health showed acceptable fit (Chi-square = 4344.716, P < 0.001, CFI = 0.943). Based on this model, the associations between anxiety and depression with subjective health varied based on race and ethnicity, while the effect of problem drinking remained stable across race and ethnic groups. Among Blacks, depression and anxiety were associated with a worse trajectory of subjective health. Among non-Hispanic Whites, anxiety was associated with a better baseline and worse trajectory of subjective health, while depression was associated with a worse baseline subjective health. Among Hispanic Whites, depression was associated with a worse trajectory of subjective health, while anxiety was not associated with subjective health. Among all race/ethnic groups, problem alcohol use was associated with worse baseline and trajectory of subjective health [Table 4, Figure 1d].
Table 4.
Results of Model IV which tests the combined (additive) effects of anxiety disorder, depressive disorder, and problem alcohol use on the baseline and trajectory of poor subjective health among men in the United States
DISCUSSION
The current study tested race and ethnic differences in the separate and combined effects of anxiety, depression and problem alcohol use on the baseline and trajectory of subjective health over 5 years among adult men in the United States. The study was unique in the following two ways; it enrolled a diverse sample of community population and modeled both linear and non-linear change of the outcome over time. In short, separate effects of anxiety and problem alcohol use on the baseline and trajectory of subjective health were similar across all race and ethnic groups. The combined effect of problem alcohol use was also similar amongst non-Hispanic and Hispanic Whites and Blacks. The combined effects of anxiety and depression showed race and ethnic differences, however. Surprisingly, when the effect of depression and problem drinking is controlled, baseline subjective health shows a positive association with anxiety among non-Hispanic Whites, a finding which is not seen among Blacks and Hispanic Whites.
Interestingly, our findings suggest that race and ethnicity modify the combined effects of anxiety, depression and problem drinking. Although the effect of problem alcohol use and subjective health was stable among all ethnic groups, previous studies have suggested that health effects of alcohol use and abuse may vary by culture. For instance, Guallar-Castillón et al., argued that the shape of association between alcohol use and subjective health may depend on culture or country of study. Literature has shown a “J shaped” relation between total alcohol use and subjective health in Nordic countries, however, this association might be positive and linear in some other countries.[14]
Another study on a large and representative sample of non-institutionalized Spanish adults showed a negative association between total consumption of alcohol and perceived health.[14] A survey among 4,472 adults in two large European cities found a curvilinear relationship (inverse J shaped) between alcohol consumption and all subscales of the SF-36, except role limitation due to physical health.[15] One study tested the association between several drinking patterns (i.e. drinking intensity and frequency, frequency of intoxication, drinking outside of meals and beverage type) and subjective health among a random sample of 3,586 in the United States showed that intoxication and liquor drinking are associated with poorer perceived health status than regular, moderate consumption of other alcoholic beverages. The study also suggested gender differences in the association between drinking and subjective health.[13] In another study of 12,037 adults in Spain, occasional, moderate and excessive consumption of alcohol were associated with better self-rated health, even after adjustment for drinking pattern and alcohol abuse. Former-drinking, frequent binge drinking and alcohol abuse were, however, associated with suboptimal self-rated health.[16]
Based on our study, problem drinking was associated with poor subjective health among non-Hispanic and Hispanic Whites and Blacks. Research has shown that although the quality of life of alcohol-dependent subjects is very poor, it may show considerable improvements as a result of abstinence, controlled or minimal drinking.[38] One study suggested that severe impairment of quality of life among alcohol misusers might be even worse than that of patients with cancer. Impairment due to alcohol misuse, however, improves with abstinence and deteriorates with relapse.[39]
The current study was limited to men. Comparison of subjective well-being in men and women has indicated that for almost all domains, quality of life of women might be worse than men. A study showed such gender differences after adjustment for level of alcohol dependency: For instance, disturbance in sleep with depression is believed to happen only among female alcohol misusers.[39] In another study in the U.S., among binge drinkers, the highest-intensity binge drinkers were more likely to report poor HRQOL than binge drinkers with lower levels of intensity. In this study, female binge drinkers reported a higher number of physically and mentally unhealthy days than their male counterparts.[22]
Our study showed that race and ethnicity also moderate the effect of socio-economic status on the baseline and change of subjective health. Race and ethnicity have not been frequently conceptualized as effect modifiers for the association between socio-economic status and trajectory of health and well-being. Ross et al., conducted growth curve analysis of seven waves of 13,682 Canadian adults and showed that quality of life is consistently highest for the most affluent and the most highly educated men and women. The study showed a consistent low quality of life for individuals with middle and low levels of income and education. The study showed that quality of life declines with age among both men and women, but the decline might be sharper for high-income women.[40]
Another cohort followed a nationally representative sample of 7,915 community-dwelling adults for 10 years and showed that quality of life remains generally stable until approximately age 70, when it starts to decline.[41] One study assessed trajectory of self-reported health among middle age African-Americans over a 4-year period. The study showed that factors such as pre-existing conditions at baseline and socio-economic status influence the baseline self-rated health. Authors argued that the pattern of decline in quality of life among African Americans look similar to that of Whites.[42]
Our study had a few limitations. We measured perceived health using a single item. Only men were included in the study, while gender differences may exist in our associations of interest. Our sample was not representative of U.S. adults and validity of our measures may differ among racial and ethnic groups. We only measured anxiety, depression and problem drinking at baseline, however, mental health is subjected to change over time. Despite the limitations, our study has two strengths: Enrolling a diverse community population sample and modeling nonlinear change of the outcome. Race and ethnic groups in the current study were the three major racial groups in the United States.
Among all three race/ethnic groups in this study, when the effects of depression and alcohol use are not controlled, anxiety is negatively associated with baseline subjective health. Surprisingly, among all ethnic groups, controlling for depression and alcohol use reverses the direction of association between anxiety and baseline subjective health. Interestingly, this reverse effect becomes significant among non-Hispanic Whites. Future research is needed to examine possible reasons for this phenomenon. The suppression effect may explain this finding,[43,44] however mediation, moderation and confounding effects should also be considered to understand why complex interrelation between anxiety, depression and alcohol use depend on race and ethnicity. Different patterns of comorbidity of anxiety, depression and problem alcohol use may be another possible explanation for this finding and warrants further investigation.
The study also has important implications. As we showed that problem alcohol use is consistently associated with low subjective health among Hispanic and non-Hispanic Whites and non-Hispanic Blacks, racial groups’ well-being may benefit similarly from diagnosis and treatment of problem drinking. As the combined effects of anxiety, depression and problem drinking varied based on race and ethnicity, screening, diagnosis and treatment of these disorders may need to take into account race and ethnicity. For instance, diagnosis of anxiety disorder among patients with depression or problem drinking may not have the same importance for promotion of well-being among non-Hispanic Whites. Depression or problem drinking may mask the effect of anxiety on perceived health among non-Hispanic Whites and Blacks.
CONCLUSIONS
Race and ethnicity modified the links between anxiety disorder, depressive disorder, and subjective health, only when both these disorders are in the model. The link between problem alcohol use and subjective health may be similar for Blacks, non-Hispanics and Hispanic Whites. While the effect of depression is controlled, anxiety is positively associated with baseline subjective health among non-Hispanic Whites. This finding was not found among Blacks or Hispanic Whites.
ACKNOWLEDGMENT
The FFCWS is funded by the National Institute of Child Health and Human Development (grant R01HD36916), the California Healthcare Foundation, the Center for Research on Religion and Urban Civil Society at the University of Pennsylvania, the Commonwealth Fund, the Ford Foundation, the Foundation for Child Development, the Fund for New Jersey, the William T. Grant Foundation, the Health care Foundation of New Jersey, the William and Flora Hewlett Foundation, the Hogg Foundation, the Christina A. Johnson Endeavor Foundation, the Kronkosky Charitable Foundation, the Leon Lowenstein Foundation, the John D. and Catherine T. MacArthur Foundation, the A. L. Mailman Family Foundation, the Charles S. Mott Foundation, the National Science Foundation, the David and Lucile Packard Foundation, the Public Policy Institute of California, the Robert Wood Johnson Foundation, the St. David's Hospital Foundation, the St. Vincent Hospital and Health Services and the US Department of Health and Human Services.
Footnotes
Source of Support: The Fragile Families and Child Well-being Study is funded by the National Institute of Child Health and Human Development (grant R01HD36916), the California Healthcare Foundation, the Center for Research on Religion and Urban Civil Society at the University of Pennsylvania, the Commonwealth Fund, the Ford Foundation, the Foundation for Child Development, the Fund for New Jersey, the William T. Grant Foundation, the Healthcare Foundation of New Jersey, the William and Flora Hewlett Foundation, the Hogg Foundation, the Christina A. Johnson Endeavor Foundation, the Kronkosky Charitable Foundation, the Leon Lowenstein Foundation, the John D. and Catherine T. MacArthur Foundation, the A. L. Mailman Family Foundation, the Charles S. Mott Foundation, the National Science Foundation, the David and Lucile Packard Foundation, the Public Policy Institute of California, the Robert Wood Johnson Foundation, the St. David's Hospital Foundation, the St. Vincent Hospital and Health Services, and the US Department of Health and Human Services
Conflict of Interest: None declared
REFERENCES
- 1.Cairney J, Corna LM, Veldhuizen S, Herrmann N, Streiner DL. Comorbid depression and anxiety in later life: Patterns of association, subjective well-being, and impairment. Am J Geriatr Psychiatry. 2008;16:201–8. doi: 10.1097/JGP.0b013e3181602a4a. [DOI] [PubMed] [Google Scholar]
- 2.Werner S. Subjective well-being, hope, and needs of individuals with serious mental illness. Psychiatry Res. 2012;196:214–9. doi: 10.1016/j.psychres.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 3.Kalman D, Lee A, Chan E, Miller DR, Spiro A, 3rd, Ren XS, et al. Alcohol dependence, other psychiatric disorders, and health-related quality of life: A replication study in a large random sample of enrollees in the Veterans health administration. Am J Drug Alcohol Abuse. 2004;30:473–87. doi: 10.1081/ada-120037389. [DOI] [PubMed] [Google Scholar]
- 4.Mauriño J, Sanjúan J, Haro JM, Díez T, Ballesteros J. Impact of depressive symptoms on subjective well-being: The importance of patient-reported outcomes in schizophrenia. Patient Prefer Adherence. 2011;5:471–4. doi: 10.2147/PPA.S24479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim JH, Ann JH, Kim MJ. The relationship between depressive symptoms and subjective well-being in newly admitted patients with schizophrenia. Compr Psychiatry. 2010;51:165–70. doi: 10.1016/j.comppsych.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 6.Evans CC, Sherer M, Nick TG, Nakase-Richardson R, Yablon SA. Early impaired self-awareness, depression, and subjective well-being following traumatic brain injury. J Head Trauma Rehabil. 2005;20:488–500. doi: 10.1097/00001199-200511000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Wetherell JL, Palmer BW, Thorp SR, Patterson TL, Golshan S, Jeste DV. Anxiety symptoms and quality of life in middle-aged and older outpatients with schizophrenia and schizoaffective disorder. J Clin Psychiatry. 2003;64:1476–82. doi: 10.4088/jcp.v64n1212. [DOI] [PubMed] [Google Scholar]
- 8.Strine TW, Chapman DP, Kobau R, Balluz L. Associations of self-reported anxiety symptoms with health-related quality of life and health behaviors. Soc Psychiatry Psychiatr Epidemiol. 2005;40:432–8. doi: 10.1007/s00127-005-0914-1. [DOI] [PubMed] [Google Scholar]
- 9.Rapaport MH, Clary C, Fayyad R, Endicott J. Quality-of-life impairment in depressive and anxiety disorders. Am J Psychiatry. 2005;162:1171–8. doi: 10.1176/appi.ajp.162.6.1171. [DOI] [PubMed] [Google Scholar]
- 10.Molnar DS, Busseri MA, Perrier CP, Sadava SW. A longitudinal examination of alcohol use and subjective well-being in an undergraduate sample. J Stud Alcohol Drugs. 2009;70:704–13. doi: 10.15288/jsad.2009.70.704. [DOI] [PubMed] [Google Scholar]
- 11.Dekker RL, Lennie TA, Albert NM, Rayens MK, Chung ML, Wu JR, et al. Depressive symptom trajectory predicts 1-year health-related quality of life in patients with heart failure. J Card Fail. 2011;17:755–63. doi: 10.1016/j.cardfail.2011.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clark DB, Kirisci L. Posttraumatic stress disorder, depression, alcohol use disorders and quality of life in adolescents. Anxiety. 1996;2:226–33. doi: 10.1002/(SICI)1522-7154(1996)2:5<226::AID-ANXI4>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 13.Stranges S, Notaro J, Freudenheim JL, Calogero RM, Muti P, Farinaro E, et al. Alcohol drinking pattern and subjective health in a population-based study. Addiction. 2006;101:1265–76. doi: 10.1111/j.1360-0443.2006.01517.x. [DOI] [PubMed] [Google Scholar]
- 14.Guallar-Castillón P, Rodríguez-Artalejo F, Díez Gañán LD, Banegas Banegas JR, Lafuente Urdinguio PL, Herruzo Cabrera RH. Consumption of alcoholic beverages and subjective health in Spain. J Epidemiol Community Health. 2001;55:648–52. doi: 10.1136/jech.55.9.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van Dijk AP, Toet J, Verdurmen JE. The relationship between health-related quality of life and two measures of alcohol consumption. J Stud Alcohol. 2004;65:241–9. doi: 10.15288/jsa.2004.65.241. [DOI] [PubMed] [Google Scholar]
- 16.Valencia-Martín JL, Galán I, Rodríguez-Artalejo F. Alcohol and self-rated health in a Mediterranean country: The role of average volume, drinking pattern, and alcohol dependence. Alcohol Clin Exp Res. 2009;33:240–6. doi: 10.1111/j.1530-0277.2008.00826.x. [DOI] [PubMed] [Google Scholar]
- 17.Le Grande MR, Elliott PC, Murphy BM, Worcester MU, Higgins RO, Ernest CS, et al. Health related quality of life trajectories and predictors following coronary artery bypass surgery. Health Qual Life Outcomes. 2006;4:49. doi: 10.1186/1477-7525-4-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muthen LK, Muthen BO. Los Angeles, CA: Muthen and Muthen; 2004. Mplus Version 3.11. [Google Scholar]
- 19.Clayton MF, Pett MA. AMOS versus LISREL: One data set, two analyses. Nurs Res. 2008;57:283–92. doi: 10.1097/01.NNR.0000313487.64412.be. [DOI] [PubMed] [Google Scholar]
- 20.Chen H, Cohen P. Using individual growth model to analyze the change in quality of life from adolescence to adulthood. Health Qual Life Outcomes. 2006;4:10. doi: 10.1186/1477-7525-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De Berardis G, Pellegrini F, Franciosi M, Belfiglio M, Di Nardo B, Greenfield S, et al. Longitudinal assessment of quality of life in patients with type 2 diabetes and self-reported erectile dysfunction. Diabetes Care. 2005;28:2637–43. doi: 10.2337/diacare.28.11.2637. [DOI] [PubMed] [Google Scholar]
- 22.Wen XJ, Kanny D, Thompson WW, Okoro CA, Town M, Balluz LS. Binge drinking intensity and health-related quality of life among US adult binge drinkers. Prev Chronic Dis. 2012;9:E86. doi: 10.5888/pcd9.110204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reichman N, Teitler J, Garfinkel I, McLanahan S. Fragile families: Sample and design. Child Youth Serv Rev. 2001;32:303–26. [Google Scholar]
- 24.Kessler RC, Wittchen HU, Abelson JM, McGonagle KA, Schwarz N, Kendler KS, et al. Methodological studies of the composite international diagnostic interview (CIDI) in the US National Comorbidity Survey. Int J Methods Psychiatr Res. 1998;7:33–55. [Google Scholar]
- 25.Kessler RC, Andrews G, Mroczek D, Ustun TB, Wittchen HU. The World Health Organization composite international diagnostic interview short form (CIDI-SF) Int J Methods Psychiatr Res. 1998;7:171–85. [Google Scholar]
- 26.Wittchen HU, Hofler M, Gander F, Pfister H, Storz S, Ustun TB, et al. Screening for mental disorders: Performance of the composite international diagnostic-screener (CID-S) Int J Methods Psychiatr Res. 1999;8:59–70. [Google Scholar]
- 27.Wittchen HU, Kessler RC, Ustun TB. Properties of the composite international diagnostic interview (CIDI) for measuring mental health outcome. In: Thornicroft G, Tansella M, editors. Mental Health Outcome Measures. 2nd ed. London: Gaskell; 2001. pp. 212–27. [Google Scholar]
- 28.McDowell I. 3rd ed. New York: Oxford University Press; 2006. Measuring Health: A Guide to Rating Scales and Questionnaires. [Google Scholar]
- 29.Bélanger A, Berthelot JM, Guimond E, Houle CA. Ottawa, Canada: Statistics Canada Report; 2002. Head-to-head comparison of two generic health status measures in the household population: McMaster Health Utilities Index (Mark3) and the EQ-5D; pp. 1–62. [Google Scholar]
- 30.McDowell I. Measures of self-perceived well-being. J Psychosom Res. 2010;69:69–79. doi: 10.1016/j.jpsychores.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 31.Hunt MO. The individual, society, or both? A comparison of black, Latino, and white beliefs about the causes of poverty. Soc Forces. 1996;75:293–332. [Google Scholar]
- 32.Andrews FM. Social indicators of perceived life quality. Soc Indic Res. 1974;1:279–99. [Google Scholar]
- 33.Andrews FM, Crandall R. The validity of measures of self-reported well-being. Soc Indic Res. 1976;3:1–19. [Google Scholar]
- 34.Knäuper B, Turner PA. Measuring health: Improving the validity of health assessments. Qual Life Res. 2003;12(Suppl 1):81–9. doi: 10.1023/a:1023589907955. [DOI] [PubMed] [Google Scholar]
- 35.Verbrugge LM. A global disability indicator. J Aging Stud. 1997;11:337–62. [Google Scholar]
- 36.Assari S. Race and ethnicity, religion involvement, church-based social support and subjective health in United States: A case of moderated mediation. Int J Prev Med. 2013;4:208–17. [PMC free article] [PubMed] [Google Scholar]
- 37.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 38.Foster JH, Powell JE, Marshall EJ, Peters TJ. Quality of life in alcohol-dependent subjects – A review. Qual Life Res. 1999;8:255–61. doi: 10.1023/a:1008802711478. [DOI] [PubMed] [Google Scholar]
- 39.Peters TJ, Millward LM, Foster J. Quality of life in alcohol misuse: Comparison of men and women. Arch Womens Ment Health. 2003;6:239–43. doi: 10.1007/s00737-003-0012-x. [DOI] [PubMed] [Google Scholar]
- 40.Ross NA, Garner R, Bernier J, Feeny DH, Kaplan MS, McFarland B, et al. Trajectories of health-related quality of life by socio-economic status in a nationally representative Canadian cohort. J Epidemiol Community Health. 2012;66:593–8. doi: 10.1136/jech.2010.115378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Orpana HM, Ross N, Feeny D, McFarland B, Bernier J, Kaplan M. The natural history of health-related quality of life: A 10-year cohort study. Health Rep. 2009;20:29–35. [PubMed] [Google Scholar]
- 42.Wolinsky FD, Miller TR, Malmstrom TK, Miller JP, Schootman M, Andresen EM, et al. Self-rated health: Changes, trajectories, and their antecedents among African Americans. J Aging Health. 2008;20:143–58. doi: 10.1177/0898264307310449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1:173–81. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hicks BM, Patrick CJ. Psychopathy and negative emotionality: Analyses of suppressor effects reveal distinct relations with emotional distress, fearfulness, and anger-hostility. J Abnorm Psychol. 2006;115:276–87. doi: 10.1037/0021-843X.115.2.276. [DOI] [PMC free article] [PubMed] [Google Scholar]


