Abstract
Background:
Considering the increased production of free radicals and inflammatory factors in rheumatoid arthritis (RA) and the effects of bioflavonoid quercetin on reducing oxidative stress, inflammation and blood pressure, the present study examined the effects of bioflavonoid quercetin on total antioxidant capacity (TAC) of plasma, lipid peroxidation and blood pressure in women with RA.
Methods:
The current study was a randomized double-blind clinical trial in which 51 women with RA aged 19-70 years, were participated. Patients were assigned into quercetin (500 mg/day) or placebo groups for 8 weeks. Dietary intake was recorded using 24-h dietary recall questionnaire and the physical activity was assessed through an international short questionnaire of physical activity at the beginning and end of the study. Plasma TAC and malondialdehyde (MDA) using colorimetric method, oxidized low density lipoprotein (ox-LDL) and high sensitivity C-reactive protein (hs-CRP) using enzyme-linked immunosorbent assay method and also blood pressure were measured at the beginning and end of intervention.
Results:
After 8 weeks there were no significant differences in TAC of plasma, ox-LDL, MDA, hs-CRP, systolic and diastolic blood pressure between quercetin and placebo groups and in each group comparing before and after.
Conclusions:
In this study, quercetin had no effect on oxidative and inflammatory status of plasma and blood pressure in patients with RA. Further studies are needed to ensure the effect of quercetin on oxidative stress and inflammation in human.
Keywords: Blood pressure, lipid peroxidation, quercetin, rheumatoid arthritis, total antioxidant capacity
INTRODUCTION
Rheumatoid arthritis (RA) is an autoimmune disease which affects joint and other organs. In many cases, the disease is associated with respiratory and cardiovascular complications so that cardiovascular diseases are the cause of 40-50% of all deaths in these patients.[1,2] Hypertension as a risk factor for cardiovascular diseases is prevalent in patients with RA.[3] The immune and inflammatory responses toward viral, genetic and environmental factors in these patients lead to stimulation of immune system and release of reactive oxygen species (ROS) by neutrophils and macrophages. Increased ROS will lead to further stimulation of immune responses and inflammation.[4] According to previous studies, the level of oxidative stress and lipid peroxidation in patients with RA is high and their antioxidant defense enzyme activity is low.[5,6] Thus, the use of antioxidant supplements beside medications may be useful in these patients. Bioflavonoids are important antioxidant compounds. In fact, these molecules are phenolic compounds that naturally exist in many fruits and vegetables. Nowadays, the role of bioflavonoids in preventing chronic diseases such as cancer, cardiovascular disease and atherosclerosis is well known.[7,8] Quercetin is one of the most important bioflavonoid, which is more abundant than other flavonoids.[9] In many studies, quercetin has shown antioxidant effects.[10,11,12] It is found that quercetin intake had an inverse correlation with serum C-reactive protein (CRP) in US adults.[13] This factor, along with blood cholesterol could be indicative of future risk of cardiovascular disease.[14,15] Quercetin has also shown some effects on protecting the cell wall and low density lipoprotein (LDL) against oxidation.[16,17] It also has shown beneficial effects on blood pressure in animals and human.[18,19] Quercetin is effective in reducing cardiovascular risk through different approaches, such as reducing oxidative stress and preventing platelet adhesion.[20] Considering the anti-inflammatory and antioxidant effects of quercetin and recommendations of previous studies to investigate the effect of this supplement in inflammatory diseases with high oxidative stress, quercetin may be useful in patients with RA, because quercetin like other antioxidants will show its effects better in the case of higher level of oxidation and inflammation.[21]
Previous studies showed that quercetin intake to 1,000 mg daily are well tolerated in human.[19,22] Despite the effect of quercetin on reducing oxidative stress in animal studies,[23,24] human studies have shown contradictory results.[19,21] To our knowledge, the effect of quercetin on oxidative stress in patients with RA has not been studied before. So far, only one study has investigated the effects of quercetin in patients with RA, that apart from the combined effect of vitamin C and quercetin, the effect of quercetin on oxidative stress in these patients has not been investigated.[25] The present study was conducted to investigate the effects of quercetin on total antioxidant capacity (TAC) of plasma, lipid peroxidation, and blood pressure in patients with RA.
METHODS
Subjects
The present study was a randomized double-blind clinical trial in which 51 patients with a diagnosis of RA, according to American College of Rheumatology 1987 criteria,[26] were recruited from two medical centers of Tehran (Loghman Hakim and Firouzgar hospitals) in 2010. Written informed consent was obtained from all patients and the study has been approved by the ethics committee of Tehran University of Medical Sciences and has been registered in the Iranian Registry of Clinical Trial (no. IRCT138807252394N2). Inclusion criteria were: Age 19-70 years old, unchanged type and dose of medications from previous month and no pregnancy or lactation. Patients were excluded from the study if changing each above mentioned criteria, affecting with other diseases that may require special treatment or increasing the severity of arthritis, smoking, acute illnesses and unwillingness to continue the study. Patients were using conventional medications for the treatment of RA, including disease modifying anti-rheumatic drugs and corticosteroids. The patients continued treatment during the intervention with the same type and dose of medication.
Design
The patients were assigned to two groups, quercetin supplement and placebo, using blocked randomization method. The supplement group used 500 mg/day quercetin (Solaray, USA) and the placebo group used one identical placebo capsule containing lactose (Daroupakhsh, pharmaceutical co.) for 8 weeks. Patients were advised not to change their diet and physical activity during the study. At the beginning of intervention, patient characteristics, dose and type of medications, and the history of previous diseases were asked. Weight and height were measured using standard protocol with light clothes and without shoes to the nearest 0.5 kg and 0.5 cm and body mass index were calculated. The blood pressure was measured twice in the sitting position and after 5-10 min resting with an analog sphygmomanometer (Omron Random Zero Blood Pressure Analyzer) and the average of two stages was recorded. The severity of disease was determined by a rheumatologist with joints examination and disease activity score (DAS28) was calculated. DAS28 higher than 2.6 was defined as active disease.[27]
Micronutrients and macronutrients intake, were estimated using 24-h recall questionnaire for 2 days and the data were analyzed using Nutritionist IV (Version 4.1, First Data Bank Division, Hearst Corporation) software. The physical activity was evaluated using the international physical activity questionnaire[28] and it was determined as the mean met-min/week.
Biochemical analysis
Before and after intervention, the venous blood samples of patients after at least 8-10 h fasting were drawn. The plasma was obtained after 10 min centrifuging at 2000 g, and it was stored at −80ºC until biochemical analyses. During the intervention, the patients were regularly monitored. At the end of the study, compliance was assessed by counting the number of capsules. Patients who had used less than 80% of supplements were excluded. TAC of plasma was measured by colorimetric method using Antioxidant Assay Kit (Cayman Chemical Company USA) with assay range of (0.044-0.33 mmol/L) according to company instructions. Malondialdehyde (MDA) was assessed by colorimetric method using Thiobarbituric Acid Reactive Substances (TBARS) Assay Kit (Cayman Chemical Company USA) with a dynamic range of (0-50 μmol/L) for the colorimetric method at the standard condition according to manufacturer's protocol. Plasma oxidized low density lipoprotein (ox-LDL) was measured by enzyme-linked immunosorbent assay (ELISA) method using ox-LDL enzyme immunoassay kit (Mercodia, Sweden) with the detection limit of (<1 mU/L) according to manufacturer's protocol. Plasma high sensitivity C-reactive protein (hs-CRP) was assessed by ELISA high sensivity CRP kit (dbc Diagnostic Biochem Canada) with sensitivity of (10 ng/mL) according to company instructions.
Statistical methods
All values are reported as mean ± SD Kolmogorov Smirnov test was performed to check whether distribution of quantitative variables is normal. In the case of normal distribution of quantitative variables, independent t test and analysis of covariance (ANOCVA) were used to compare two groups at the beginning and after intervention with adjusting the baseline values, respectively. Paired t test was used to compare the mean values at the beginning and after intervention. If the distribution of variable was not normal, Mann-Whitney U test was used to compare the differences between two groups. Wilcoxon signed-rank test was performed for each group to compare mean values before and after intervention. If confounding factors have significant differences between two groups and have linear correlation with a dependent variable (Pearson correlation coefficient <0.3), it was adjusted in the subsequent analyses. ANOCVA and repeated measures covariance were used to adjust the effect of confounding factors, comparing two groups and before and after in each group, respectively. SPSS statistical software (version 15; SPSS Inc.) was used for data analysis. The level of P ≤ 0.05 was considered statistically significant.
RESULTS
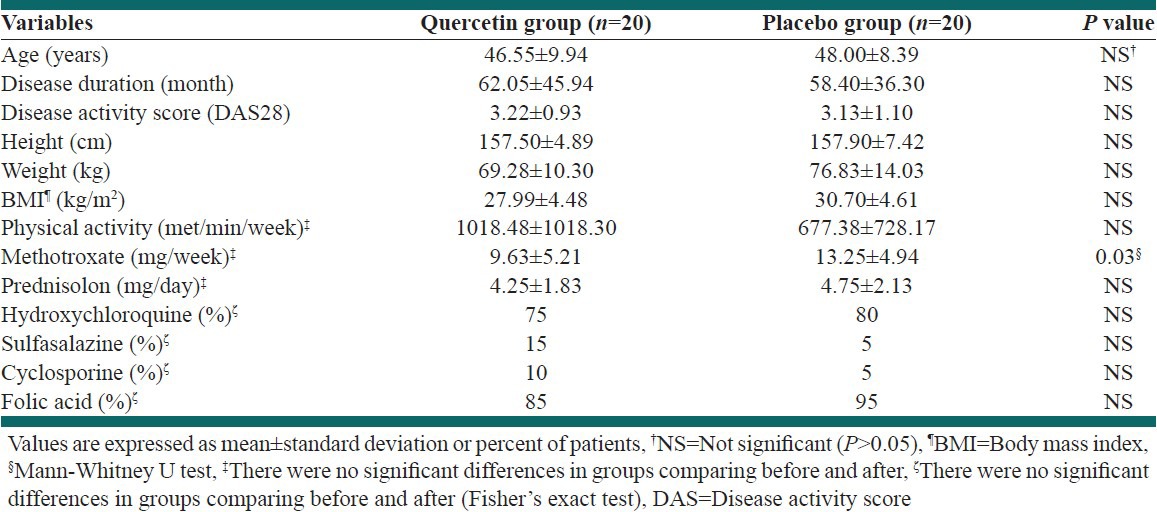
Among 51 patients who participated in the study, five subjects from quercetin group (four patients because of the need to increase and change medications and one patient because of supplement consumption less than 80%) and six patients from placebo group (five subjects because of changing the type and dose of medication and one due to unwillingness to continue the study) were excluded. Finally, 40 patients (20 patients in each group) completed the study and perprotocol statisticlal analyses were performed. Patients with active disease in quercetin and placebo groups were 15 and 14 patients, respectively. The remaining subjects had inactive disease. Distribution of patients with active disease in both groups was identical and DAS-28 was not significantly different between two groups. Weight, body mass index (BMI), age, disease duration and physical activity were not significantly different between quercetin and placebo groups. There was no significant difference between two groups in terms of medications at the beginning and end of the study, except for the average of methotrexate consumption. Methotrexate consumption was higher in quercetin group than placebo group at the beginning of the study, so it was adjusted in the analyses of dependent variables [Table 1].
Table 1.
Baseline characteristics of patients
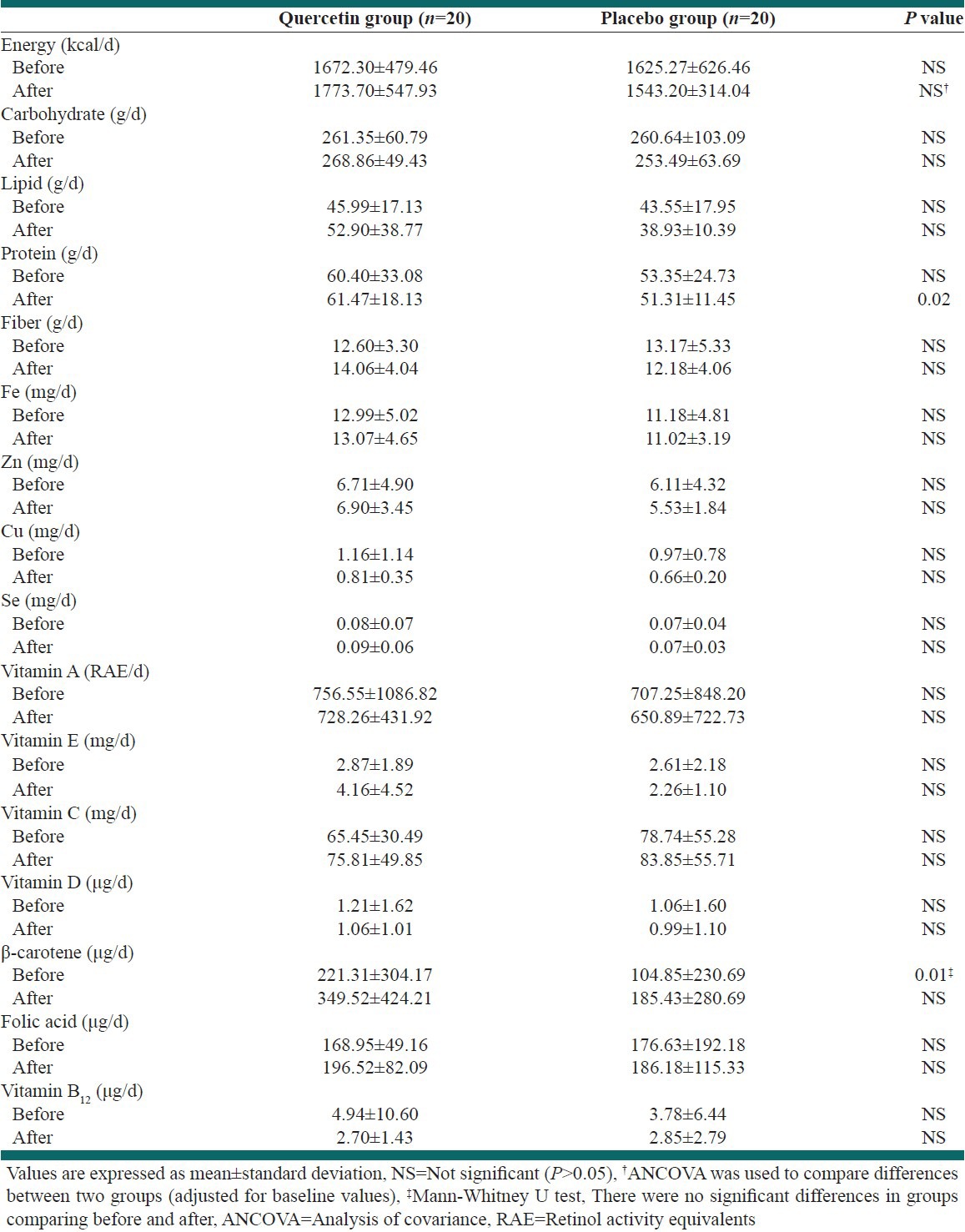
Daily macro and micronutrients intake are shown in Table 2. Among the dietary variables, only β-carotene at beginning and protein at the end of study showed statistically significant differences between groups and were adjusted in the analysis of dependent variables.
Table 2.
Daily energy and nutrient intake, before and after supplementation in both groups
Quercetin supplementation for 8 weeks, had no significant effect on plasma TAC (P = 0.35). A small decrease in TAC was observed in quercetin group at the end of intervention, but it was not statistically significant (P = 0.39). The ox-LDL and hs-CRP were not significantly different between groups (P = 0.52 and P = 0.66, respectively) after intervention. A slight increase in ox-LDL was observed in both groups at the end of the study which was not statistically significant (P = 0.58 and P = 0.48 for quercetin and placebo groups, respectively). Although hs-CRP decreased at the end of the study in both groups, but this change was not statistically significant (P = 0.13 and P = 0.062 for quercetin and placebo groups, respectively). Plasma MDA in the placebo group was higher than quercetin group (P = 0.01) at the beginning of study, but there was no significant difference between two groups at the end of the study after adjusting for baseline value (P = 0.14). The mean systolic and diastolic blood pressures increased in both groups at the end of the study, but it was not statistically significant (P = 0.44 and P = 0.16 for quercetin group and P = 0.51 and P = 0.85 for placebo group, respectively). After adjusting for baseline values, systolic blood pressure was not significantly different between two treatment groups (P = 0.48). Diastolic blood pressure was lower in quercetin group than placebo at the beginning of study (P = 0.01), but at the end of the study no significant change was shown after adjusting for baseline value (P = 0.77) [Table 3].
Table 3.
Biochemical outcomes and blood pressure before and after 8 week supplementation

DISCUSSION
According to our knowledge, the current study seems to be the first study examined the effect of quercetin supplement (500 mg/day) on oxidative stress and factors related to cardiovascular disease in patients with RA. In our study, quercetin supplement showed no statistically significant effect on plasma TAC. The in vitro studies have shown that quercetin inhibited the oxidative stress in animal organs.[29,30,31] The dose of quercetin in those studies was higher than its does in our study. Boots et al. have examined the effect of 4 × 500 mg quercetin within 24 h in patients with sarcoidosis and blood samples were obtained 3 h after the last dose.[21] This short term use of quercetin caused a significant increase in total equivalent antioxidant capacity in quercetin group compared to placebo. The daily quercetin dose was four times more than that of our study. However, various doses of 730 mg supplementation in hypertensive patients,[19] 150 mg in obese patients with metabolic syndrome[32] and 1000 mg in athletes after sport matches[33] showed no significant effect on the antioxidant capacity of plasma, which are in good agreement with our study.
In our study, quercetin showed no significant effect on MDA. The effects of quercetin on MDA are inconsistent in animal studies[23,29] and human clinical studies on the effect of quercetin on MDA are very scarce. To our knowledge, only Boots et al.[21] showed a significant decrease in plasma MDA as a marker of lipid peroxidation. They stated that the beneficial effect of quercetin could better appear when the level of oxidative stress and inflammation are enhanced. The duration of intervention and the dose of quercetin in these studies are not comparable with that of our study. The blood concentration of quercetin may also be different. Because of high level of oxidative stress and inflammation of the patients in Boots study and using quercetin as the only treatment (with no medication), the supplement could better reflect its beneficial effects.
In our study, quercetin had no effect on ox-LDL. Benito et al.[34] have studied the effect of quercetin and its metabolites, i.e., catechin and alcohol-free red wine on healthy rats for 10 days. They were not able to show the antioxidant effects of these polyphenols which is in good agreement with our results. They did not observe any significant change in lipid peroxidation. LDL lag phase or ex vivo LDL oxidation in rats showed no change compared to control group and no flavonoid metabolites were observed in LDL particles. Thus, since the flavonoid metabolites are not present in lipoproteins, they could not have any effect on their oxidation. Egert et al.[32] showed that consumption of 150 mg quercetin in patients with metabolic syndrome was able to reduce the mean ox-LDL significantly within 6 weeks. The presence of quercetin glucuronide in atherosclerotic lesions indicates that quercetin is fully available to prevent LDL oxidation in the body.[35] The number of participants in Egert's study was much higher than our study and yet the dose of supplement was one-third of our study which may suggest the probable pro-oxidative effect of supplement in our study due to higher dose of quercetin. Given the contradictory results of existing studies in this field, the direct effect of quercetin, its antioxidant role in the body and its appropriate dose in humans are still controversial and more researches are needed.
In the present study, quercetin supplementation showed no significant effect on hs-CRP as an acute phase protein. Chun et al.[13] found that CRP concentration is higher in women, the elderly, sedentary subjects and those who use non-steroidal anti-inflammatory drugs. At the same time, the total intake of flavonoids including isoflavones, anthocyanidins and quercetin from foods are inversely associated with CRP concentration. Garcia-Mediavilla et al.[31] found that quercetin and kaempferol are able to inhibit mRNA associated with CRP, inducible Nitric oxide synthase (iNOS) and cyclooxygenase-2 in the liver through the effect of quercetin and kaempferol on human liver cells. They found that, the inhibitory effect was done through the nuclear factor (NF-κB) transcription factor and the highest inhibitory effect of quercetin on NF-κB concentration happened at 100 μmol/L and its highest inhibitory effect on CRP took place at 5-50 μmol/L. These doses are much more than the dose of quercetin used in our study. The results of these studies were not consistent with other clinical studies like our study. The consumption of 1000 mg quercetin in marathon athletes had no significant effect on inflammatory factors such as CPR, cytokines, Monocyte chemoattrctant protein-1 and Macrophage inflammatory protein-1.[36] Also, quercetin and glucosamine chondroitin sulfate[37] or quercetin and vitamin C[25] had no significant effect on CRP and other inflammatory factors in patients with RA. One study conducted on patients with metabolic syndrome who received 150 mg/day quercetin showed no significant difference on CRP concentration between two study groups.[32] In that study, the initially low level of inflammation at baseline and low supplement does were interpreted as lack of effect of quercetin on CRP. The effect of quercetin in controlling inflammation such as CRP is still limited to in vitro and animal studies. Low bioavailability of quercetin and its conjugation in the body are other reasons for the lack of quercetin effect. Also in our study, hs-CRP level was not high and patients were in stable condition due to medication therapy, while quercetin shows its effects better when the level of inflammation is high.[21]
In our study, there was no significant effect on blood pressure which is consistent with Conquer et al.[38] that investigated the effects of queretin on blood pressure and some other cardiovascular risk factors in healthy subjects. Egert et al.[32] found that quercetin lead to significant decrease of systolic blood pressure of all participants with obesity and hypertension. Edwards et al.[19] found that quercetin had no significant effect on blood pressure in pre-hypertensive subjects. Only subjects in stage one hypertension showed a significant decrease in systolic and diastolic blood pressure. Furthermore, in our study, quercetin showed no effect on blood pressure, probably because patients did not suffer from hypertension.
CONCLUSIONS
The present study on the effects of quercetin on plasma oxidative status, hs-CRP and blood pressure in patients with RA, shown no significant effect on markers of oxidative stress including MDA, TAC, ox-LDL and cardiovascular risk factors including hs-CRP and blood pressure. It seems that further studies are required to measure the cellular and tissue oxidative stress beside its blood level, with various doses of quercetin, in order to determine the effect of this supplement on oxidative stress more extensively.
ACKNOWLEDGMENTS
This research was funded by the Vice Chancellor of Tehran University of Medical Sciences for research affairs (grant no. 960). We are grateful of Dr. Kavosh Rahimi for providing the supplement. The Biochemistry Laboratory staffs of the Institute of Endocrinology and metabolism of Shahid Beheshti University of Medical Sciences are highly appreciated for biochemical analyses.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Lipsky PE. Rheumatoid arthritis. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, editors. Harrison's principle of internal medicine. 17th ed. New York: McGraw Hill; 2008. pp. 2083–92. [Google Scholar]
- 2.Turesson C, Matteson EL. Cardiovascular risk factors, fitness and physical activity in rheumatic diseases. Curr Opin Rheumatol. 2007;19:190–6. doi: 10.1097/BOR.0b013e3280147107. [DOI] [PubMed] [Google Scholar]
- 3.Panoulas VF, Douglas KM, Milionis HJ, Stavropoulos-Kalinglou A, Nightingale P, Kita MD, et al. Prevalence and associations of hypertension and its control in patients with rheumatoid arthritis. Rheumatology (Oxford) 2007;46:1477–82. doi: 10.1093/rheumatology/kem169. [DOI] [PubMed] [Google Scholar]
- 4.Geronikaki AA, Gavalas AM. Antioxidants and inflammatory disease: Synthetic and natural antioxidants with anti-inflammatory activity. Comb Chem High Throughput Screen. 2006;9:425–42. doi: 10.2174/138620706777698481. [DOI] [PubMed] [Google Scholar]
- 5.Okamoto T. Oxidative stress in rheumatoid arthritis. In: Surh YJ, Packer l, editors. Oxidative Stress, Inflammation and Health. Boca Raton, FL: Taylor and Francis; 2005. pp. 245–61. [Google Scholar]
- 6.Kamanli A, Naziroğlu M, Aydilek N, Hacievliyagil C. Plasma lipid peroxidation and antioxidant levels in patients with rheumatoid arthritis. Cell Biochem Funct. 2004;22:53–7. doi: 10.1002/cbf.1055. [DOI] [PubMed] [Google Scholar]
- 7.Knekt P, Kumpulainen J, Järvinen R, Rissanen H, Heliövaara M, Reunanen A, et al. Flavonoid intake and risk of chronic diseases. Am J Clin Nutr. 2002;76:560–8. doi: 10.1093/ajcn/76.3.560. [DOI] [PubMed] [Google Scholar]
- 8.Huxley RR, Neil HA. The relation between dietary flavonol intake and coronary heart disease mortality: A meta-analysis of prospective cohort studies. Eur J Clin Nutr. 2003;57:904–8. doi: 10.1038/sj.ejcn.1601624. [DOI] [PubMed] [Google Scholar]
- 9.Bischoff SC. Quercetin: Potentials in the prevention and therapy of disease. Curr Opin Clin Nutr Metab Care. 2008;11:733–40. doi: 10.1097/MCO.0b013e32831394b8. [DOI] [PubMed] [Google Scholar]
- 10.Young JF, Nielsen SE, Haraldsdóttir J, Daneshvar B, Lauridsen ST, Knuthsen P, et al. Effect of fruit juice intake on urinary quercetin excretion and biomarkers of antioxidative status. Am J Clin Nutr. 1999;69:87–94. doi: 10.1093/ajcn/69.1.87. [DOI] [PubMed] [Google Scholar]
- 11.Molina MF, Sanchez-Reus I, Iglesias I, Benedi J. Quercetin, a flavonoid antioxidant, prevents and protects against ethanol-induced oxidative stress in mouse liver. Biol Pharm Bull. 2003;26:1398–402. doi: 10.1248/bpb.26.1398. [DOI] [PubMed] [Google Scholar]
- 12.Galisteo M, García-Saura MF, Jiménez R, Villar IC, Wangensteen R, Zarzuelo A, et al. Effects of quercetin treatment on vascular function in deoxycorticosterone acetate-salt hypertensive rats. Comparative study with verapamil. Planta Med. 2004;70:334–41. doi: 10.1055/s-2004-818945. [DOI] [PubMed] [Google Scholar]
- 13.Chun OK, Chung SJ, Claycombe KJ, Song WO. Serum C-reactive protein concentrations are inversely associated with dietary flavonoid intake in U.S. adults. J Nutr. 2008;138:753–60. doi: 10.1093/jn/138.4.753. [DOI] [PubMed] [Google Scholar]
- 14.Ridker PM. High-sensitivity C-reactive protein: Potential adjunct for global risk assessment in the primary prevention of cardiovascular disease. Circulation. 2001;103:1813–8. doi: 10.1161/01.cir.103.13.1813. [DOI] [PubMed] [Google Scholar]
- 15.Scirica BM, Morrow DA. Is C-reactive protein an innocent bystander or proatherogenic culprit.? Circulation. 2006;113:2128–51. doi: 10.1161/CIRCULATIONAHA.105.611350. [DOI] [PubMed] [Google Scholar]
- 16.Gong M, Garige M, Varatharajalu R, Marmillot P, Gottipatti C, Leckey LC, et al. Quercetin up-regulates paraoxonase 1 gene expression with concomitant protection against LDL oxidation. Biochem Biophys Res Commun. 2009;379:1001–4. doi: 10.1016/j.bbrc.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 17.Chopra M, Fitzsimons PE, Strain JJ, Thurnham DI, Howard AN. Nonalcoholic red wine extract and quercetin inhibit LDL oxidation without affecting plasma antioxidant vitamin and carotenoid concentrations. Clin Chem. 2000;46:1162–70. [PubMed] [Google Scholar]
- 18.Mackraj I, Govender T, Ramesar S. The antihypertensive effects of quercetin in a salt-sensitive model of hypertension. J Cardiovasc Pharmacol. 2008;51:239–45. doi: 10.1097/FJC.0b013e318162011f. [DOI] [PubMed] [Google Scholar]
- 19.Edwards RL, Lyon T, Litwin SE, Rabovsky A, Symons JD, Jalili T. Quercetin reduces blood pressure in hypertensive subjects. J Nutr. 2007;137:2405–11. doi: 10.1093/jn/137.11.2405. [DOI] [PubMed] [Google Scholar]
- 20.Lakhanpal P, Rai DK. Role of quercetin in cardiovascular diseases. Internet Journal of Medical Update. 2008;3:31–49. [Google Scholar]
- 21.Boots AW, Drent M, de Boer VC, Bast A, Haenen GR. Quercetin reduces markers of oxidative stress and inflammation in sarcoidosis. Clin Nutr. 2011;30:506–12. doi: 10.1016/j.clnu.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 22.Nieman DC, Henson DA, Davis JM, Angela Murphy E, Jenkins DP, Gross SJ, et al. Quercetin's influence on exercise-induced changes in plasma cytokines and muscle and leukocyte cytokine mRNA. J Appl Physiol. 2007;103:1728–35. doi: 10.1152/japplphysiol.00707.2007. [DOI] [PubMed] [Google Scholar]
- 23.Duarte J, Pérez-Palencia R, Vargas F, Ocete MA, Pérez-Vizcaino F, Zarzuelo A, et al. Antihypertensive effects of the flavonoid quercetin in spontaneously hypertensive rats. Br J Pharmacol. 2001;133:117–24. doi: 10.1038/sj.bjp.0704064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Galisteo M, García-Saura MF, Jiménez R, Villar IC, Zarzuelo A, Vargas F, et al. Effects of chronic quercetin treatment on antioxidant defence system and oxidative status of deoxycorticosterone acetate-salt-hypertensive rats. Mol Cell Biochem. 2004;259:91–9. doi: 10.1023/b:mcbi.0000021360.89867.64. [DOI] [PubMed] [Google Scholar]
- 25.Bae SC, Jung WJ, Lee EJ, Yu R, Sung MK. Effects of antioxidant supplements intervention on the level of plasma inflammatory molecules and disease severity of rheumatoid arthritis patients. J Am Coll Nutr. 2009;28:56–62. doi: 10.1080/07315724.2009.10719762. [DOI] [PubMed] [Google Scholar]
- 26.Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- 27.Guillemin F. How to assess musculoskeletal conditions. Assessment of disease activity. Best Pract Res Clin Rheumatol. 2003;17:415–26. doi: 10.1016/s1521-6942(03)00026-3. [DOI] [PubMed] [Google Scholar]
- 28.Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 29.Duarte J, Galisteo M, Ocete MA, Pérez-Vizcaino F, Zarzuelo A, Tamargo J. Effects of chronic quercetin treatment on hepatic oxidative status of spontaneously hypertensive rats. Mol Cell Biochem. 2001;221:155–60. doi: 10.1023/a:1010956928584. [DOI] [PubMed] [Google Scholar]
- 30.Amália PM, Possa MN, Augusto MC, Francisca LS. Quercetin prevents oxidative stress in cirrhotic rats. Dig Dis Sci. 2007;52:2616–21. doi: 10.1007/s10620-007-9748-x. [DOI] [PubMed] [Google Scholar]
- 31.García-Mediavilla V, Crespo I, Collado PS, Esteller A, Sánchez-Campos S, Tuñón MJ, et al. The anti-inflammatory flavones quercetin and kaempferol cause inhibition of inducible nitric oxide synthase, cyclooxygenase-2 and reactive C-protein, and down-regulation of the nuclear factor kappaB pathway in Chang Liver cells. Eur J Pharmacol. 2007;557:221–9. doi: 10.1016/j.ejphar.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 32.Egert S, Bosy-Westphal A, Seiberl J, Kürbitz C, Settler U, Plachta-Danielzik S, et al. Quercetin reduces systolic blood pressure and plasma oxidised low-density lipoprotein concentrations in overweight subjects with a high-cardiovascular disease risk phenotype: A double-blinded, placebo-controlled cross-over study. Br J Nutr. 2009;102:1065–74. doi: 10.1017/S0007114509359127. [DOI] [PubMed] [Google Scholar]
- 33.Quindry JC, McAnulty SR, Hudson MB, Hosick P, Dumke C, McAnulty LS, et al. Oral quercetin supplementation and blood oxidative capacity in response to ultramarathon competition. Int J Sport Nutr Exerc Metab. 2008;18:601–16. doi: 10.1123/ijsnem.18.6.601. [DOI] [PubMed] [Google Scholar]
- 34.Benito S, Buxaderas S, Mitjavila MT. Flavonoid metabolites and susceptibility of rat lipoproteins to oxidation. Am J Physiol Heart Circ Physiol. 2004;287:H2819–24. doi: 10.1152/ajpheart.00471.2004. [DOI] [PubMed] [Google Scholar]
- 35.Kawai Y, Nishikawa T, Shiba Y, Saito S, Murota K, Shibata N, et al. Macrophage as a target of quercetin glucuronides in human atherosclerotic arteries: Implication in the anti-atherosclerotic mechanism of dietary flavonoids. J Biol Chem. 2008;283:9424–34. doi: 10.1074/jbc.M706571200. [DOI] [PubMed] [Google Scholar]
- 36.Nieman DC, Henson DA, Davis JM, Dumke CL, Gross SJ, Jenkins DP, et al. Quercetin ingestion does not alter cytokine changes in athletes competing in the Western States endurance run. J Interferon Cytokine Res. 2007;27:1003–11. doi: 10.1089/jir.2007.0050. [DOI] [PubMed] [Google Scholar]
- 37.Matsuno H, Nakamura H, Katayama K, Hayashi S, Kano S, Yudoh K, et al. Effects of an oral administration of glucosamine-chondroitin-quercetin glucoside on the synovial fluid properties in patients with osteoarthritis and rheumatoid arthritis. Biosci Biotechnol Biochem. 2009;73:288–92. doi: 10.1271/bbb.80418. [DOI] [PubMed] [Google Scholar]
- 38.Conquer JA, Maiani G, Azzini E, Raguzzini A, Holub BJ. Supplementation with quercetin markedly increases plasma quercetin concentration without effect on selected risk factors for heart disease in healthy subjects. J Nutr. 1998;128:593–7. doi: 10.1093/jn/128.3.593. [DOI] [PubMed] [Google Scholar]


