Abstract
Background:
The different duration of delay to first contact with a psychiatrist in depressive disordered patients has been observed in western and non western cultures. This study aimed to examine the duration and predictive factors of delay in contact with a psychiatrist in depressive patients in Isfahan city of Iran.
Methods:
In This cross sectional study 156 depressive patients were recruited from various outpatient clinics in Isfahan city between January 2013 and February 2013. We used the Anderson Socio-Behavioral Model (ASBM) for examine the role of various factors influencing delay in help seeking. In this models there were three categories variables (predisposing, enabling and need factors). Quintile regression model was used to study the predictors.
Results:
The median duration between symptom onset and first contact with a psychiatrist was 1 year. In the first step (predisposing model), age at onset of depressive symptoms and never married were negative predictors for delay, but widowed or divorced statues was positive predictors for delay. In the enabling model past contact with health provider was positively associated with duration of delay. In the need model, neither variable had a significant effect on duration of delay. In the full model, younger age at onset, widowed or divorced statues and past contact with health provider increased duration of delay.
Conclusions:
More delay of help seeking by children and adolescence and probability of maladaptive coping style such as substance use and complicating of situation need to earlier diagnosis of depression in young group and earlier treatment for decrease DALLY for MDD, Therefore we suggest the mental health awareness programs for adolescent in school, and more ever for the influenced roles of parent and other family members and teachers on teen and young person's life, the education for families and teachers on adolescent mental health problems can be effective. First help seeking contact with non-psychiatric medical professionals enhance the delay of contact with a psychiatrist. Appropriate training of non-psychiatric medical professionals and developing a referral system would lead to better provision of mental health care.
Keywords: Delay, depression, predictive factors, psychiatrist
INTRODUCTION
Depression is the most common medical problems seen today.[1] Although there are a number of effective treatments for these disorders, a substantial number of people do not seek treatment for depressive episodes.[2]
Considerably less is known about the speed of treatment contact with a psychiatrist among incident psychiatric cases over a longer time periods, with the exception of research on the treatment lag following first episodes of schizophrenia in the developed countries. Therefore, the timing between the onset of a first depressive episode and an individual's entry into serious treatment represents a significant interval that has been largely ignored in the researches.[3] Hence we were going to assess the duration and determinants of treatment delay in depressive disorders in Isfahan, Iran.
METHODS
Subjects
A total of 156 Participants were recruited from outpatient psychiatric units of 2 public hospitals and 7 private out-patient psychiatric clinics who were diagnosed as a major depressive disorder by a psychiatrist, between January and February 2013. The exclusion criteria included current alcohol or drug dependence and previous history of schizophrenia, bipolar disorder, manic disorders or organic brain disorders.
Assessments
The outcome variable in this study, duration of delay in the initial treatment contact is defined as the time from disorder onset to the time of first contact with a psychiatrist. Measurement unit for this variables was year.
This study used Anderson's socio-behavioral model as the theoretical basis to study the role of various factors influencing delay in help-seeking. Current help-seeking literature guided the selection of predisposing, enabling and need variables.
Predisposing variables
Including age at the first depressive episode, Sex, Marital status, Education and Perceived Stigma (at the first contact with a psychiatrist).
Enabling variables
Including: Per capita income per household member, home ownership, perceived social support (PSS) and Health Insurance (at the first contact to a psychiatrist), previous contact with a health care provider (non-medical professional and non-psychiatric medical professionals) “prior to the first contact with a psychiatrist.
Need variables
Including Disability function and having a history of suicide thoughts, plans or attempts, at the time of seeking care.
The survey tool (questionnaire) adapted from WMH-CIDI and CCHS 1.2, Multidimensional PSS Scale and Stigma Module of Family Experience Schedule.[1]
Analysis
Quantile regression used for analysis roles of predictors factors on duration delay in treatment. In this model, we considered nine quantiles, that is, P = (0.10-0.90). Potential predictors were entered in this model in four steps. In the first step, predisposing variables and in three other steps, enabling, need and all variables were included. The statistical analysis was performed using the SPSS 15 and STATA 10.
RESULTS
Length of the total delay ranged from 4 day to 30 years. The mean standard deviation and median were 3.43 (5.26) and 1 years respectively. The pattern of delay was a positively skewed J-shape curve (skewness value = 2.33).
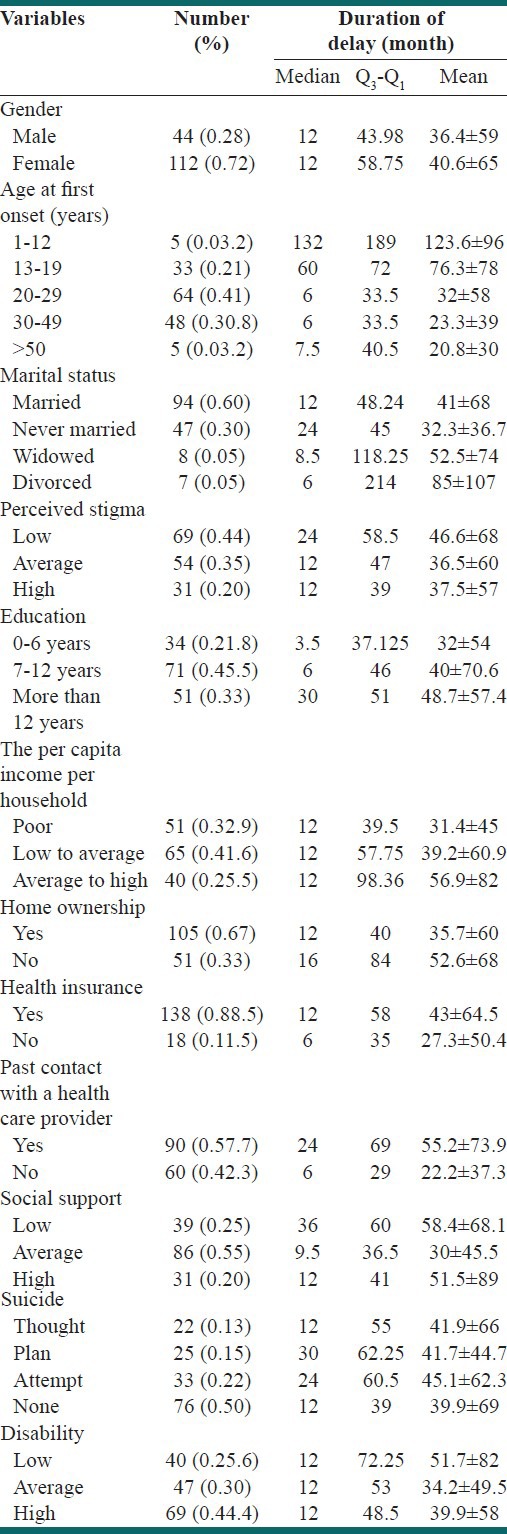
Descriptive statistics for predictor variables and duration delay according to these variables is presented in Table 1.
Table 1.
Demographic and clinical variable (predictors variable) in the total sample and duration of delay according predictor variables
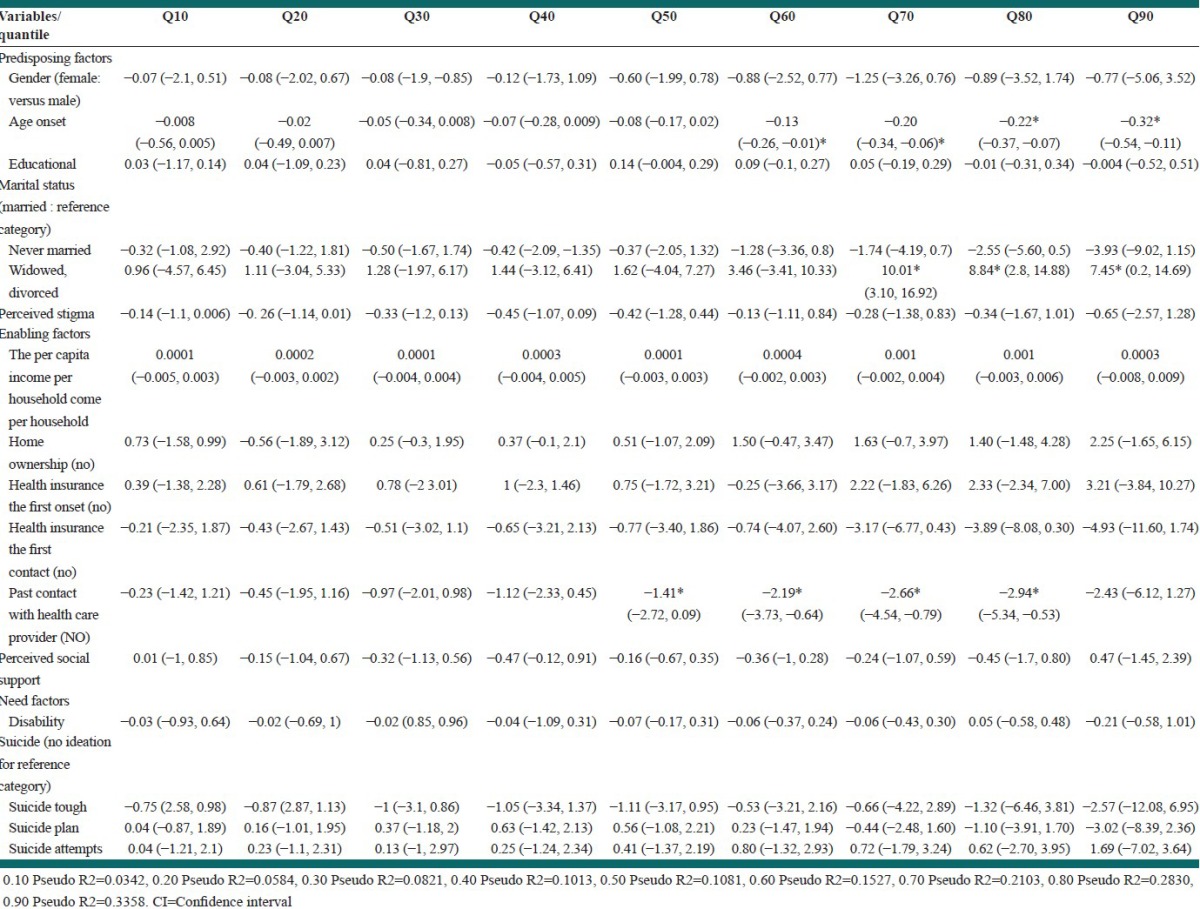
In predisposing model: Age at the first depressive episode in quantiles 60, 70, 80, 90 (β = −0.12, −0.19, −0.32, −0.26 respectively), never married in quantiles 80 (β = −4.42) and 90 (β = −5.71) and widowed or divorced in quantiles 70, 80, 90 (β = 9.88, 8.94, 8.58, respectively) were significantly predictor for delay.
In Enabling model: Previous contact with a health Care provider in quantiles 50, 60 and 70 had a negative correlation with delay (β = −1.52, −1.94, −3 respectively).
In need model: Neither variable had a significant effect on delay.
In the final model: Age at the first onset, widowed or divorced and past contact with a health care provider remained as significant correlates of delay and never married was no longer associated with delay [Table 2].
Table 2.
Quantile regression coefficients (standardized β [95% CI] for analysis roles of all factors on duration delay in first contact with psychiatric
Except for the small correlation (β = 174) between education and income, among other variables, there was no relation with each other.
DISCUSSION
The duration of delay in our study was lower when compared to more other countries.[4]
If mental disorders be started an early age will have less likely to mental health service utilization and have longer delay[1,4,5] as we found in the current study. One of the explanations for this effects is that symptoms emerging earlier in life are more likely tolerated as normal. Children with early-onset mental disorders may develop maladaptive coping strategies that ultimately interfere with treatment seeking later in life.[4,5]
Research in utilization of mental health services shown that greater utilization between females in contrast males. However most of studies on treatment delay consistently failed to find any association between gender and treatment delay in mental disorders[2] Similar most of previous study, we did not find a significant association between gender and delay, that suggested to be related greater perceived stigma attached to male mental health complains and greater PSS for female.[6] However in our study, there was no relationship between stigma and social support with gender and also between stigma and social support with treatment seeking delay.
In our study, single people had a shorter lag period than married people (in predisposing model). This may be due to receiving more advises about help-seeking from peer groups. Moreover, being widowed or divorced were predisposing to more delay of treatment seeking, that may be because low social support.
Despite previous studies, we found previous contact with non-psychiatric medical professionals leads to longer delay of contact with a psychiatrist.[7,8]
Our study found no association between of duration of treatment seeking delay and socio-economic status. In the U.S inadequately, Income and lack of health insurance acts as two significant barriers to treatment seeking, but in New Zealand income played no role in early or late into care.[6]
Our study did not find any association between need variables and delay. In some studies, there was no relationship between the need variables and delay, but other studies found two different association (in some of them negative and in other of them positive association).[1]
CONCLUSIONS
Earlier onset of depression is associated with more delay of refer to psychiatry that may have significant implications for productivity, substance use, suicide and interpersonal or relational problems. More people make their first contact with general medical practitioners (GP) and GPs are more reluctant to refer patients to psychiatrists.
Suggestions
we suggest the mental health awareness programs for adolescent in school, and more ever for the influenced roles of parent and other family members and teachers on teen and young person's life for on time referring of affected person to a doctor and educational program for GP for effective management of depressed patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Sadruddin S. PHD Theses. Department of Health Policy, Management and Evalution University of Toronto; 2007. Predictors of Treatment Delay in Depressive Disorder in Pakistan. [Google Scholar]
- 2.Blumenthal R, Endicott J. Barriers to seeking treatment for major depression. Depress Anxiety. 1996;4:273–8. doi: 10.1002/(SICI)1520-6394(1996)4:6<273::AID-DA3>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Olfson M, Berglund PA. Patterns and predictors of treatment contact after first onset of psychiatric disorders. Am J Psychiatry. 1998;155:62–9. doi: 10.1176/ajp.155.1.62. [DOI] [PubMed] [Google Scholar]
- 4.Wang PS, Angermeyer M, Borges G, Bruffaerts R, Tat Chiu W, DE Girolamo G, et al. Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry. 2007;6:177–85. [PMC free article] [PubMed] [Google Scholar]
- 5.Thampson A, Issikadis C, Hunt C. Delay to seek treatment for anxiety and mood disorders in an Australian clinical sample. Behav Change. 2008;25:71–84. [Google Scholar]
- 6.Carragher N, Adamson G, Bunting B, McCann S. Treatment-seeking behaviours for depression in the general population: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Affect Disord. 2010;121:59–67. doi: 10.1016/j.jad.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 7.Lincoln C, Harrigan S, McGorry PD. Understanding the topography of the early psychosis pathways. An opportunity to reduce delays in treatment. Br J Psychiatry Suppl. 1998;172:21–5. [PubMed] [Google Scholar]
- 8.Skeate A, Jackson C, Birchwood M, Jones C. Duration of untreated psychosis and pathways to care in first-episode psychosis. Investigation of help-seeking behaviour in primary care. Br J Psychiatry Suppl. 2002;43:s73–7. doi: 10.1192/bjp.181.43.s73. [DOI] [PubMed] [Google Scholar]


