Abstract
This article describes an innovative method to disseminate the Acute Care for Elders (ACE) model of care for hospitalized older patients implemented at 11 community hospitals in Wisconsin. The ACE Tracker is a computer-generated checklist of all older patients in a facility that takes information from multiple areas of the electronic medical record to identify the older patients’ risk factors for functional decline and poor outcomes. The ACE Tracker report was validated against in-person observation of the older patients and found to be accurate. Interdisciplinary teams on medical–surgical units use this summary report to review each patient’s plan of care and to efficiently assess the patients who are vulnerable to poor hospital outcomes. The ACE Tracker is also used during regular consultation provided through teleconferencing between an off-site geriatrician (e-Geriatrician) and the local ACE team. The effect of the ACE Tracker and e-Geriatrician models was assessed by measuring use of urinary catheters, physical restraints, high-risk medications, and social service evaluation at a single hospital for the 6 months before and after implementation of the models. There were significant improvements in urinary catheter and physical therapy referrals but no significant changes in the other outcomes. There was no change in the length of stay or in the rate of hospital readmission within 30 days.
Keywords: ACE units, hospitalized older patients, interdisciplinary team, care management, electronic medical record
The Acute Care for Elders (ACE) unit was developed in the early 1990s as a model of care to lessen the chance of functional decline in older hospitalized patients.1,2 ACE units emphasize early and repeated assessments to identify risk factors for functional decline and other hospital complications and an interdisciplinary approach to interventions that minimize risk of poor hospital outcomes.3 Two randomized controlled studies4,5 found that older adults treated on an ACE unit were less likely to experience functional declines during hospitalization and after discharge. Fewer older adults were discharged to a nursing home or were residing in a nursing facility 3 months after their hospitalization than of those who received standard care. Two additional randomized controlled studies6,7 have shown mixed results in decreasing length of stay and costs of health services.
In spite of the evidence of the effectiveness of this model of care, ACE is not the standard for older hospitalized adults in the United States (unpublished data). Barriers to dissemination include the capital investment to start the program, a scarcity of geriatricians to serve as medical directors, and the fact that an ACE unit benefits only those patients on the unit and not older patients on other hospital units (e.g., a cardiac unit).8
This article will describe methods of disseminating ACE concepts to hospitals that do not have special ACE units or geriatricians on staff. The first is a computer-generated spreadsheet listing all older patients in a facility and their risk factors for functional decline or poor outcomes (the ACE Tracker). The second component is regular consultation through teleconferencing between an off-site geriatrician and a local ACE team (the e-Geriatrician). How these models were implemented and evaluated on an interdisciplinary team at each participating hospital is discussed.
DESCRIPTION OF AURORA HEALTH CARE
Aurora Health Care is a not-for-profit integrated healthcare system serving eastern Wisconsin comprising 12 acute care hospitals, one psychiatric hospital, 100 clinics, 130 community pharmacies, a home care agency, and a hospice service. Three of the Aurora hospitals are located in rural counties.
The healthcare system provided care for approximately 30,000 hospitalized patients aged 65 and older in 2008. There are 16 board-certified geriatricians on the medical staff of Aurora’s hospitals, predominantly located at one hospital. Six of the 12 hospitals do not have a geriatrician on staff. Aurora’s providers use a single electronic medical record (EMR) at all hospital and clinic sites. Two of the hospitals have ACE units. There was a desire to disseminate ACE concepts to the other 10 hospitals in the system, but the facilities had no geriatrician on staff, lacked the capital budget for renovation, or both. In addition, it was desired to disseminate ACE concepts in the two hospitals with ACE units to older patients cared for on other units.
DESCRIPTION OF THE ACE TRACKER PROGRAM
ACE Tracker is a software program that uses data from the EMR to create a daily report on all patients aged 65 and older on a medical or surgical unit. The goal is to develop an efficient and effective method of reviewing multiple older patients without having to ask the same questions repeatedly. The report pulls information from various parts of the EMR, including admission and daily nursing assessments, pharmacy data, social service charting, and physician orders. The content of the report includes patient identifiers, length of stay, history of cognitive impairment, assessment for delirium, bed rest, use of restraints, serum albumin level, total number of prescribed medications, assessments for risk of falls and for risk of pressure ulcers, activities of daily living, use of urinary catheters, and use of high-risk medications. Also included is whether physical and occupational therapy and social service assessments have been ordered. Information on admission diagnosis and comorbidities are not included. The data are updated every 15 minutes. The nursing staff collects the majority of information during their admission and daily assessments of their patients. Additional information about medications and orders is also retrieved from the electronic record. The Confusion Assessment Method (CAM) is currently scored on the ACE Tracker system without a formal cognitive assessment by the nursing staff.
THE ACE TEAM
Interdisciplinary teams at 11 hospitals use the ACE Tracker. Clinical nurse specialists typically lead these teams, which include a social worker, a pharmacist, and a physical or occupational therapist. The team can be unit based or hospital based; that is, some hospitals have formed separate teams for each adult inpatient unit, whereas others have one team that works across several units. These teams meet 5 days a week for 30 minutes. The ACE Tracker instrument serves as a guide for discussion of each patient. Information from the ACE Tracker is presented in a spreadsheet (Table 1) that serves as the basis for a discussion of the patient by the interdisciplinary team. For example, in Table 1, Patient H has a high risk of falls (Morse score ≥45) and had a fall before hospitalization. This would precipitate a discussion of interventions to lower risk of falls. Similarly, the list would precipitate a discussion of the use of a potential inappropriate medication (per the Beers criteria9) in Patient C and of pressure ulcer prevention techniques for Patient B. This list of all older patients on a medical or surgical unit, in essence, becomes a “virtual ACE unit.” Two times a week, a geriatrician attends the interdisciplinary team meetings. At the six hospitals without a geriatrician on staff, the teams use an “e-Geriatrician.”
Table 1.
Example of Printout from ACE Tracker Summarizing Risk Factor for Patients Aged of 65 or Older on a Hospital Unit
| Patient Room/ Bed |
Age | Length of Stay |
History of Dementia |
CAM | Number of Meds |
Beers | Morse | HX of Falls |
Bed Rest |
P/T | O/T | RES | ADL | Cath | Press Ulcer |
Wound Care |
Braden Scale |
Albumin | Social Services |
Advance Directives |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient A | 76 | 2 | N | N | 13 | N | 60 | Y | N | Y | Y | N | 8 | Y | Y | Y | 17 | ND | Y | N |
| Patient B | 74 | 1 | Y | N | 7 | N | 50 | Y | Y | N | N | N | 6 | Y | Y | Y | 9 | 2.9 | N | Y |
| Patient C | 78 | 12 | Y | Y | 10 | Y | 50 | Y | N | Y | Y | N | 7 | N | N | Y | 14 | 3.9 | Y | Y |
| Patient D | 72 | 1 | N | N | 5 | N | 50 | N | N | N | N | N | 12 | N | N | N | 15 | ND | N | N |
| Patient E | 91 | 6 | Y | N | 8 | N | 60* | N | N | Y | Y | N | 6* | N | N | N | 14 | ND | Y | N |
| Patient F | 78 | 1 | N | N | 7 | N | 70 | Y | Y | N | N | N | 6 | Y | N | N | 16 | ND | N | N |
| Patient G | 75 | 1 | N | N | 0 | N | 45 | N | N | Y | Y | N | 12 | N | N | N | 14 | 4.3 | N | N |
| Patient H | 93 | 1 | Y | N | 12 | N | 65 | Y | N | Y | Y | N | 6 | N | N | N | 15 | ND | Y | Y |
| Patient I | 91 | 1 | Y | N | 1 | N | 95 | Y | N | Y | Y | N | 7 | N | N | N | 12 | 3.5 | N | Y |
| Patient J | 74 | 5 | N | N | 20 | N | 45 | Y | N | Y | Y | N | 7 | Y | Y | Y | 12* | ND | Y | Y |
| Patient K | 72 | 6 | N | Y | 14 | N | 20 | N | N | Y | Y | N | 8 | N | N | N | 17 | 3.2 | Y | Y |
| Patient L | 83 | 3 | N | Y | 12 | N | 80* | Y | Y | Y | Y | N | 8 | Y | N | N | 12 | 2.3 | N | Y |
| Patient Totals | 5 | 3 | 11 | 1 | 8 | 3 | 9 | 9 | 0 | 5 | 3 | 4 | 6 | 7 |
Report Date: 02/27/08.
Report Time: 17:17.
History of Dementia = Cognition as defined by nursing admission assessment of history of dementia or Alzheimer’s disease.
CAM = Confusion Assessment Method10 as performed by nursing staff on admission and repeated daily on high-risk patients.
Meds = Number of total prescribed medications given to the patient on a scheduled basis.
Beers = Administration of potentially inappropriate medications for use in older adults within the prior 48-hours.9
Morse = Morse falls risk from calculated on admission and daily by nursing staff. A score >45 indicates an increased risk of in hospital falls.11
Hx of Falls = Any history of falls prior to hospitalization as recorded on nursing admission assessment.
Bed Rest = Bed rest as determined by daily nursing database describing the patient’s activity level.
PT = Physical therapy consultation ordered.
OT = Occupational therapy consultation ordered.
Res = Current use of a physical restraint device as recorded on nursing daily assessment.
ADL = Activity of daily living score for bathing, dressing, transferring, walking, using the toilet and eating. 0 score for requiring total assistance; 1 score for requiring some assistance; 2 score of independent. These data from nursing admission assessment are repeated every other day.
Cath = Urinary catheter in place as noted on nursing daily assessment
Press Ulcer = Pressure ulcer noted on nursing daily assessment.
Wound Care = Wound care consultation ordered.
Braden Scale = Calculated Braden Scale: 15–18 at risk, 13–14 at moderate risk, 10–12 at high risk, and 9 or below at very high risk.12 These data are from nursing daily assessment.
Albumin = The most recent serum albumin value with an asterisk noting a value of 3.5 mg/dL or lower.
Social Services = Any documentation of a social service assessment.
Advance Directives = Any documentation of the presence of the patient’s advance directives.
Y = Yes.
N = No.
ND = Not drawn.
This score is less favorable than the admission score.
DESCRIPTION OF THE E-GERIATRICIAN MODEL
This program was developed to allow a healthcare system to bring ACE unit care to hospitals that had no ACE unit and no geriatrician on medical staff. The e-Geriatrician is an off-site geriatrician who participates in the interdisciplinary team meetings through teleconference. The off-site geriatrician discusses high-risk cases with the team to help develop a plan of care in response to geriatric problems. Because the EMR is systemwide, the e-Geriatrician can access the ACE Tracker checklist for the patients to be covered in the meeting, as well as the individual medical records (e.g., to determine specific medications prescribed). After the team discusses patients on one unit, they move to a different nursing unit of the same hospital, re-establish the conference call with the geriatrician, and proceed with a discussion of the next group of older patients. The total time spent with the geriatrician on the conference call is 30 to 45 minutes. The geriatricians are reimbursed at an hourly rate for their participation.
OUTCOMES OF THE ACE MEETINGS
For approximately 30% to 50% of patients discussed in any ACE meeting, the team will make a recommendation, such as initiating physical therapy, removing a urinary catheter, or questioning the use of a specific medication. The staff nurse or clinical nurse specialist typically conveys these recommendations to the attending physician the next time the physician sees the patient. In some cases, an attending physician is called after the meeting with a specific request or suggestion. The ACE team receives feedback on responses of the physicians to the recommendations at the next meeting.
DEVELOPING THE ACE MODEL AT THE AURORA HOSPITALS
An outline of steps taken in developing the ACE model at Aurora hospitals is given in Appendix A. An important step was the development of an ACE advisory committee at each hospital composed of representatives from the departments of rehabilitation therapy, pharmacy, nursing, dietary, and the hospital administration. A local medical staff member with an interest in geriatrics was also asked to join the ACE advisory committee. This committee then identified individuals who would constitute the ACE interdisciplinary team. The top management at each institution approved the formation and functions of the ACE team. Geriatricians involved in the e-Geriatrician program attended medical staff meetings at all of the hospitals to explain the program, answer questions, and receive feedback. Two of the authors (MV and JS) taught the interdisciplinary teams at each hospital how to print out, interpret, and use the ACE Tracker software report. An internal Web site provided instructions on how to use the report, and teams were given demonstrations on how to work with the e-Geriatrician.”
In training, to function as an e-Geriatrician, geriatricians were instructed one on one and observed other colleagues during the telemedicine rounds. They met regularly to discuss their technique and approach. The geriatricians also met initially approximately six times with each ACE team at the distant hospitals to develop a professional relationship and rapport with the team members. The supervisors of the ACE teams provided feedback to the geriatricians as well. The nurses on each ACE team were given training on their approach to physicians at nursing staff meetings and during team meetings. The primary care physicians were given an update on the ACE model and their role in discussing the plan of care with nurses at medical staff meetings.
DEVELOPMENT OF THE ACE TRACKER
This effort started with a retrospective chart review of the quality of care of older patients on a medical unit.5 A team of software programmers, geriatricians, nurses, and pharmacists then defined several quality measures of care that formed the basis of a real-time report of the quality of care for older patients. The components of the ACE Tracker have been refined in an iterative process over 24 months with input from the team. For example, a method was developed to define whether an older patient had received a high-risk medication within the prior 48 hours, unlike with early versions of the software, which simply indicated whether the patient had taken a high-risk medication at any time during their hospital care. The most recent version of the ACE Tracker also identifies declines in function during hospital stay. For the Morse fall scale, the activity of daily living score, and the Braden pressure ulcer score, the ACE Tracker notes with an asterisk if there has been any worsening in the score during hospitalization.
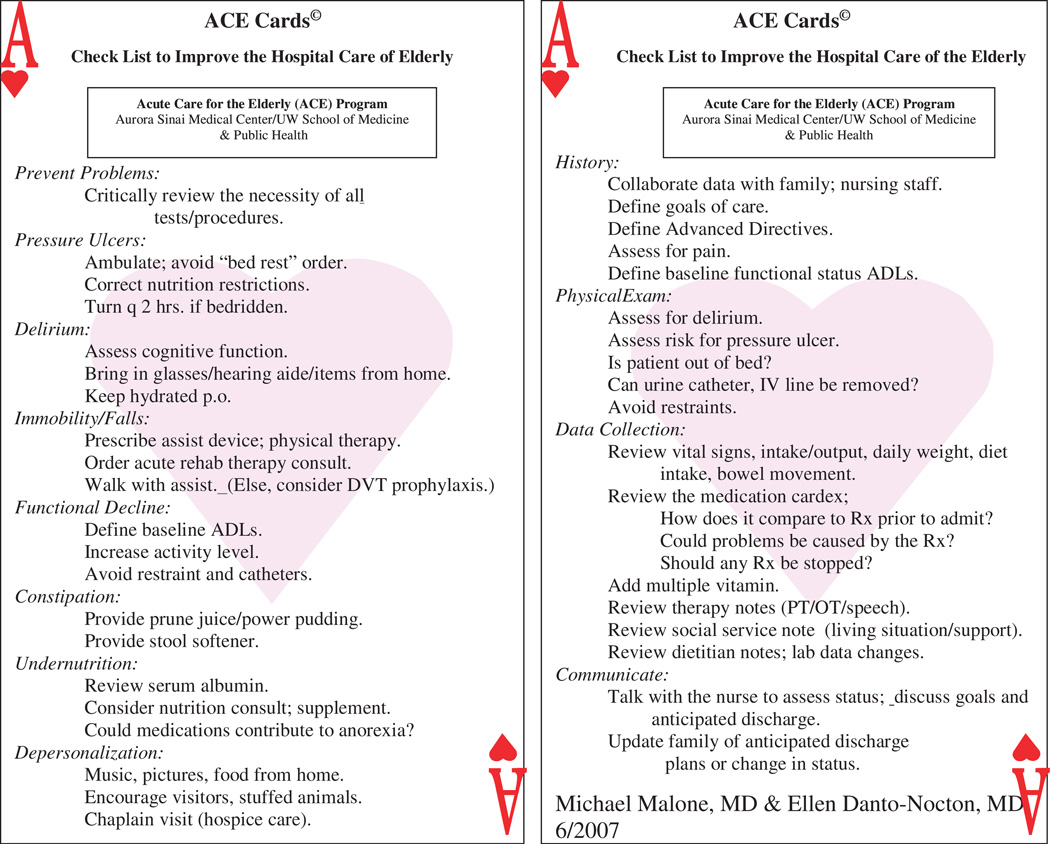
Other refinements to the ACE program include routine nurse-initiated admission orders and ACE cards. The admission orders empower the nursing and rehabilitation staff to initiate appropriate interventions without a specific physician order. The ACE cards (Figure 1) are distributed to the medical and nursing staff of the Aurora hospitals to raise visibility of the ACE program and to serve as pocket reminders of important ACE concepts.
Figure 1.
Front and back of Acute Care for Elders Cards, given to physicians and nurses of participating hospitals. P.O. = per os (oral); DVT = deep vein thrombosis; ADLs = activities of daily living; IV = intravenous; Rx = medication; PT = physical therapy; OT = occupational therapy; lab = laboratory
USE OF ACE TRACKER SOFTWARE TO ASSESS PRACTICE PATTERNS IN THE CARE OF HOSPITALIZED OLDER PATIENTS
An additional benefit of the ACE Tracker is a description of the patterns of care of older patients at each hospital in a healthcare system. ACE Tracker data for several key processes (use of urinary catheter, use of high-risk medications for older adults, use of physical restraint, physical therapy assessment, and social service assessment) are obtained for the second hospital day for each older hospitalized patient at each hospital throughout the system, producing a “snap-shot” of these processes of care for each hospital. The data are reported on the health system care management Web site on a 6-month basis. Table 2 shows an example of cumulative data from 12 hospitals. These processes of care can then be followed over time at each facility to determine whether the ACE interventions and other changes are having affecting the processes of care.
Table 2.
Acute Care for Elders Tracker Data for Key Processes of Care at 12 Aurora Health Care Hospitals: August 2007–January 2008
| Hospital | A | B | C | D | E | F | G | H | I | J | K | L | Average |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients for indicators 1 through 7, n | 896 | 569 | 741 | 576 | 575 | 652 | 549 | 402 | 813 | 2,025 | 6,470 | 755 | |
| 1. Beer’s list medication ordered, % | 12.1 | 12.1 | 8.8 | 12.2 | 9.9 | 6.3 | 11.3 | 8.2 | 8.0 | 6.8 | 12.6 | 8.9 | 9.1 |
| 2. Beer’s medication administered, % | 5.0 | 6.3 | 4.3 | 4.5 | 6.3 | 2.5 | 5.3 | 4.5 | 3.9 | 2.7 | 4.1 | 2.6 | 4.0 |
| 3. Physical therapy consultation, % | 39.2 | 49.4 | 64.6 | 68.4 | 71.5 | 55.4 | 45.9 | 57.5 | 71.8 | 65.5 | 55.3 | 72.2 | 58.7 |
| 4. Restraints ordered, % | 2.5 | 1.9 | 2.4 | 2.8 | 3.5 | 0.6 | 1.5 | 0.5 | 0.2 | 3.2 | 7.8 | 3.7 | 2.5 |
| 5. Urinary catheter ordered, % | 35.2 | 25.6 | 28.9 | 30.8 | 26.5 | 27.0 | 31.7 | 26.8 | 18.2 | 29.0 | 29.3 | 33.2 | 28.8 |
| 6. Social services consultation, % | 85.6 | 72.4 | 82.7 | 84.5 | 77.0 | 88.2 | 85.1 | 66.4 | 66.8 | 71.8 | 50.2 | 84.1 | 79 |
| 7. Pressure ulcer, % | 3.8 | 5.8 | 11.1 | 9.0 | 8.0 | 7.2 | 4.9 | 5.2 | 8.1 | 5.3 | 4.7 | 5.6 | 6.5 |
| 8. Wound consultation ordered if pressure ulcer present, % | 50.0 | 43.9 | 44.2 | 50.0 | 48.1 | 28.6 | 51.5 | 45.8 | 57.1 | 52.4 | 49.9 |
ADOPTION OF THE ACE TRACKER AND E-GERIATRICIAN
There was variation in the speed of adoption of the ACE program at the 12 hospitals. One indicator is the number of ACE Tracker reports generated each month at each hospital. Each ACE Tracker report (Table 1) contains information on approximately 10 patients. In 2007, there were more than 800 ACE Tracker reports generated per month across the 12 hospitals. Two hospitals averaged fewer than 30 reports per month (< daily), whereas the other 10 hospitals were generating more than one report daily. By November 2008, this had increased to more than 1,000 ACE Tracker reports generated throughout the 12 hospitals. Currently 28 of the 50 medical–surgical units at 12 Aurora hospitals have ACE programs. Patients in intensive care or specialty units are typically not covered. This results in the ACE Tracker reviewing approximately one-third of all older inpatients daily.
Several of the geriatricians have worked on a traditional geographically defined ACE unit and as e-Geriatricians. The innovative aspects of the model attract the geriatricians and the e-Geriatrician team members. Another positive aspect is the ability to access patients who are on many different units in a hospital. The geriatricians occasionally express frustration at not being able to perform an in-person evaluation on some patients. Another limitation of the model is the strict time limitations, which preclude comprehensive evaluation. One geriatrician described his role as thinking out loud about the most vulnerable features of the patient discussed without attempting any synthesis.
EVALUATION OF THE ACE TRACKER SOFTWARE
To determine the validity of the ACE Tracker report, a research nurse observed all patients aged 65 and older (n = 93) on 1 day at each of six hospitals. The 93 patients were receiving their care on two ACE units and six medical–surgical units participating with the ACE Tracker and e-Geriatrician models. The institutional review board at Aurora Health Care approved the study. The nurse assessed the use of an indwelling urinary catheter and physical restraints and reviewed the patients’ EMRs to determine the number of medications given to the patients, use of high-risk medications, fall risk assessment scores, and pressure ulcer risk. Nursing observations were compared with the ACE Tracker results. The 65 older women and 28 older men who were evaluated had a mean age of 79.9 ± 8.3). Nineteen patients (20.4%) had an indwelling urinary catheter, and no patient was restrained. The positive predictive value (PPV) and negative predictive value (NPV) of the ACE Tracker are given in Table 3. ACE Tracker agreed with the nurses’ documentation of the number of scheduled medications (τ = 0.95, 95% confidence interval (CI) = 0.91–0.99), the risk of in-hospital fall (τ = 0.94, 95% CI = 0.87–0.99), and the risk of pressure ulcer (τ = 0.93, 95% CI = 0.86–0.99). Overall, this preliminary evaluation suggests that the ACE Tracker software is valid when compared with an in-person observation of the care of older hospitalized patients at multiple hospitals.
Table 3.
Acute Care for Elders Tracker Compared with Nursing Observations of 93 Older Patients at Six Hospitals
| Variable | Positive Predictive Value |
Negative Predictive Value |
|---|---|---|
| Urinary catheter use | 94.7 | 95.9 |
| Physical therapy consultation | 96.7 | 84.8 |
| Restraint use | * | 100.0 |
| High-risk medication | 86.7 | 100.0 |
None of the 93 patients was restrained.
PRELIMINARY EVALUATION OF THE E-GERIATRICIAN
The e-Geriatrician model was launched as a quality improvement initiative on a surgical urology unit in February 2007 and then on a general medical unit in July 2007 at one hospital. Twice-per-week consultation was provided between an off-site geriatrician (40 miles away) and the local interdisciplinary team. To test the effect of the e-Geriatrician model, a quasi-experimental method was used of comparing the care for the 6 months before and after the initiative at one hospital. The Aurora Health Care institutional review board approved the project. Table 4 shows the processes and outcomes before and after the start of the e-Geriatrician program. The percentage of patients with urinary catheters decreased from 26.2% to 20.1%, and the prevalence of patients with consultations for physical therapy increased from 27.0% to 39.1%. There were no significant changes in the use of physical restraints, social service assessments, or high-risk medications. The length of hospital stay and the 30-day readmission rate were also unchanged on the two units where this program was implemented. These results are similar to the outcomes reported previously5 in a randomized trial of ACE in a community hospital.
Table 4.
Comparison of Processes and Outcomes in the 6-Month Periods Before and After Institution of e-Geriatrician and Acute Care for Elders (ACE) Tracker at One Hospital
| Before n = 478† |
After n = 406§ |
P- Value‡ |
|
|---|---|---|---|
| Urinary catheter, %* | 26.2 | 20.1 | .03 |
| Physical therapy, %* | 27.0 | 39.1 | <.001 |
| Restraints, %* | 0.6 | 0.8 | >.99 |
| High-risk medications, %* | 4.4 | 4.0 | .78 |
| Social work evaluation, %* | 86.0 | 83.2 | .25 |
| Pressure ulcer, %* | 7.9 | 5.0 | .11 |
| Length of stay, mean ± standard deviation | 3.7 ± 2.8 | 3.6 ± 3.2 | .76 |
| 30-day readmission, % | 14.5 | 12.7 | .40 |
These processes were used on Day 2 of hospitalization.
Before values were obtained by reviewing the electronic medical records for all patients aged 65 and older on the hospital units for the 6 months before the e-Geriatrician program was initiated.
After results came from the ACE Tracker.
Chi-square was performed. Fisher exact test was performed when a cell was <5. T-test was performed to compare the mean difference in length of stay. All statistical analyses were performed using SAS 9.1 (SAS Institute, Inc., Cary, NC).
LIMITATIONS OF THE ACE TRACKER AND THE E-GERIATRICIAN MODELS
There are many limitations to the ACE Tracker program as currently implemented. The level of control over the processes of care is less with the ACE Tracker than in a real ACE unit. For example, there is currently no formal tracking in the ACE Tracker report of whether recommendations to physicians are followed. Another limitation is data quality. For example, the ACE Tracker does not use objective indicators of cognition, because that information is not in the EMR. Instead, it assesses whether the patient has a history of dementia (taken from the admission nursing assessment). In addition, the nursing staff scores the CAM without a formal cognitive assessment, and thus, underrecognition of delirium may be a problem with the ACE Tracker system as it is currently used. Another important limitation of this model is that it does not include an indicator of pain severity. Also, in contrast to “real” ACE units,4–7 there is no evidence that application of the ACE Tracker or e-Geriatrician improves patient outcomes. Finally, individual sites implementing this system may need to adapt the ACE Tracker elements to suit their local needs and priorities.
CONCLUSION
The purpose of this study has been to describe steps in the development of a program to improve care of older patients in hospitals where a geographically distinct ACE unit is not feasible. Such a program benefits from an EMR and cooperation between hospitals with geriatricians on staff and those without. An analogous model of off-site evaluation by geriatrician was recently described in rural Australia.13 Preliminary outcomes of the ACE Tracker and e-Geriatrician model deployed at a distant hospital without a geriatrician on staff show that the model improves processes of care for older patients. ACE Tracker provides a reliable report of patients’ care. Given the dwindling numbers of geriatricians in the United States and Canada,14 ACE Tracker and e-Geriatrician may represent a method to disseminate geriatric concepts with efficient use of a geriatrician’s time. This new model of care has several features consistent with the vision for care in the future described in the Institute of Medicine Report on Retooling for an Aging America.14 The e-Geriatrician program uses health information technology and remote monitoring to support the healthcare workforce by promoting interdisciplinary patient care and care coordination. Future evaluation of these models of care should examine outcomes such as readmission rate and nursing home use. Evaluation of the effectiveness and the cost-effectiveness of these models is also needed.
ACKNOWLEDGMENTS
The authors would like to acknowledge Aurora Health Care for their support and collaboration in piloting and launching the ACE Tracker and e-Geriatrician models and Jeff Stephenson, Aurora Health Care, for technical support related to managing this program.
The authors would like to thank the following colleagues for assistance in developing and implementing this project: Dr. Ariba Khan, Dr. Dennis Baumgardner, Katherine Claxton, PharmD, Amy Onsager, RN, Amy Olson, Carla Oman, Barbara Paegelow, Naoyo Mori, Han-Yang Chen, MS, Patricia Maloney and Kelley Prevou.
APPENDIX A: STEPS TO SUCCESSFULLY DISSEMINATE ACUTE CARE FOR ELDERS (ACE) THROUGHOUT A HEALTHCARE SYSTEM
| (1) Obtain highest leadership acceptance of the model. |
| (2) Define the ACE financial and clinical outcomes and review performance quarterly. |
| (3) Meet with nurses and physicians at each hospital to identify their most difficult problems in caring for older hospitalized patients. |
| (4) Develop philanthropic support and relationships to assist with ACE dissemination. |
| (5) Develop information technology tools (ACE Tracker). |
| (6) Develop standardized ACE order sets for older adults admitted to all hospitals and standardized nursing care plans for care of older hospitalized patients. |
| (7) Develop ACE champions at each hospital to serve on each hospital’s ACE advisory team. |
| (8) Place future ACE program leaders on current ACE advisory teams to act as seeds for future expansion. |
| (9) Communicate regularly to leadership groups, departments, and medical staff using evidence-based approach to ACE. |
| (10) Develop tools to communicate ACE concepts (ACE Cards). |
| (11) Bring all ACE teams together twice per year for continuing education with national expert speakers. |
Footnotes
Author Contributions: Michael Malone, Marsha Vollbrecht, and Jeff Stephenson: conception and implementation of the ACE Tracker. Michael Malone, James Goodwin, Marsha Vollbrecht, Patti Pagel, Laura Burke, and Jeff Stephenson: study design, analysis and interpretation of the data, and preparation of the manuscript. Michael Malone, Patti Pagel, Laura Burke, and Jeff Stephenson: acquisition of data.
Sponsor’s Role: None.
REFERENCES
- 1.Palmer RM, Counsell S, Landefeld CS. Clinical intervention trials: The ACE unit. Clin Geriatr Med. 1998;14:831–849. [PubMed] [Google Scholar]
- 2.Sager MA, Rudberg MA. Functional decline associated with hospitalization for acute illness. Clin Geriatr Med. 1998;14:669–679. [PubMed] [Google Scholar]
- 3.Palmer RM, Landefeld CS, Kresevic D, et al. A medical unit for the acute care of the elderly. J Am Geriatr Soc. 1994;42:545–552. doi: 10.1111/j.1532-5415.1994.tb04978.x. [DOI] [PubMed] [Google Scholar]
- 4.Landefeld CS, Palmer RM, Kresevic D, et al. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338–1344. doi: 10.1056/NEJM199505183322006. [DOI] [PubMed] [Google Scholar]
- 5.Counsell SR, Holder CM, Liebenauer LL, et al. Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older adults: A randomized controlled trial of Acute Care for Elders (ACE) in a community hospital. J Am Geriatr Soc. 2000;48:1572–1581. doi: 10.1111/j.1532-5415.2000.tb03866.x. [DOI] [PubMed] [Google Scholar]
- 6.Covinsky KE, King JT, Jr, Quinn LM, et al. Do acute care for elders units increase hospital costs? A cost analysis using the hospital perspective. J Am Geriatr Soc. 1997;45:729–734. doi: 10.1111/j.1532-5415.1997.tb01478.x. [DOI] [PubMed] [Google Scholar]
- 7.Asplund K, Gustafson Y, Jacobsson C, et al. Geriatric-based versus general wards for older acute medical patients: A randomized comparison of outcomes and use of resources. J Am Geriatr Soc. 2000;48:1381–1388. doi: 10.1111/j.1532-5415.2000.tb02626.x. [DOI] [PubMed] [Google Scholar]
- 8.Rogers EM. Diffusion of Innovations. 5th ed. Washington, DC: Free Press; 2003. [Google Scholar]
- 9.Fick DM, Cooper JW, Wade WE, et al. Updating the Beers criteria for potentially inappropriate medications use in older adults: Results of a US concensus panel of experts. Arch Intern Med. 2003;163:2714–2716. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 10.Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: The confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 11.Morse JM. Preventing Patient Falls. Thousand Oaks, CA: SAGE Publications; 1997. [Google Scholar]
- 12.Bergstrom N, Braden BJ, Laguzza A, et al. The Braden Scale for predicting pressure ulcer risk. Nurs Res. 1987;36:205–210. [PubMed] [Google Scholar]
- 13.Gray L, Wootton R. Innovative in aged care—Comprehensive geriatric assessment “online.”. Aust J Aging. 2008;27:205–208. doi: 10.1111/j.1741-6612.2008.00309.x. [DOI] [PubMed] [Google Scholar]
- 14.Institute of Medicine (IOM) Retooling for an Aging American. Washington, DC: The National Academies Press; 2008. [Google Scholar]