Abstract
Background
Patients with retinitis pigmentosa are motivated to try complementary or integrative therapies to slow disease progression. Basic science, clinical research and retinitis pigmentosa patients' self-reports support the hypothesis that acupuncture may improve visual function.
Methods
A prospective, case series, pilot study enrolled 12 adult patients with RP treated at an academic medical centre with a standardised protocol that combined electroacupuncture to the forehead and below the eyes and acupuncture to the body, at 10 half-hour sessions over two weeks. Pre- and post-treatment tests included Early Treatment Diabetic Retinopathy Study visual acuity (VA), Pelli-Robson contrast sensitivity (CS), Goldmann visual fields, and dark-adapted full-field stimulus threshold (FST)(n = 9). Scotopic Sensitivity Tester-1 (SST-1) dark-adaptometry was performed on the last two subjects.
Results
Six of 12 subjects had measurable, significant visual function improvements after treatment. Three of nine subjects tested with the FST had a significant 10.3 to 17.5 dB (that is, 13- to 53-fold) improvement in both eyes at one week after acupuncture, maintained for at least 10 to 12 months, which was well outside typical test-retest variability (95% CI: 3–3.5 dB) previously found in retinitis pigmentosa. SST-1 dark-adaptation was shortened in both subjects tested on average by 48.5 per cent at one week (range 36 to 62 per cent across 10 to 30 dB), which was outside typical coefficients of variation of less than 30 per cent previously determined in patients with retinitis pigmentosa and normals. Four of the five subjects with psychophysically measured scotopic sensitivity improvements reported subjective improvements in vision at night or in dark environments. One subject had 0.2 logMAR improvement in VA; another had 0.55 logCS improvement. Another subject developed more than 20 per cent improvement in the area of the Goldmann visual fields. The acupuncture protocol was completed and well tolerated by all, without adverse events or visual loss.
Conclusions
Acupuncture entails minimal risk, if administered by a well-trained acupuncturist and may have significant, measurable benefits on residual visual function in patients with retinitis pigmentosa, in particular scotopic sensitivity, which had not previously been studied. These preliminary findings support the need for future controlled studies of potential mechanisms.
Keywords: acupuncture, low vision, retinitis pigmentosa
After being diagnosed with a disabling and chronic disease, such as retinitis pigmentosa, it is extremely disheartening to the patient to hear that nothing can be done to treat it. Because of the lack of current management options beyond nutritional supplements attempting to slow disease progression, many patients with retinitis pigmentosa are motivated to try complementary and/or integrative therapies to attempt to slow, halt or reverse the disease process.1 In 2006–07, our survey of complementary therapy usage in 96 patients with retinitis pigmentosa found that 42 per cent of respondents had tried acupuncture, of whom 61 per cent indicated a subjective improvement in vision.1
Both basic science research2 and clinical studies3–4 support the hypothesis that electroacupuncture and/or acupuncture may have a potentially beneficial effect on visual function in patients with retinitis pigmentosa. In RCS rats with retinitis pigmentosa-like retinal degeneration, increased retinal nerve growth factor and brain-derived neurotrophic factor proteins, as well as outer nuclear layer retinal thickness were measured following electroacupuncture.2 From the clinical perspective, two published case series indicate that most retinitis pigmentosa patients treated with acupuncture had improvements in visual acuity (VA), with younger and earlier stage patients more likely to improve,3 or had improvements in visual field (VF) area and sensitivity.4 While these findings are intriguing, more rigorous research methods involving a sham control group have not been employed and the potential mechanisms that may play a role have not been explored in patients with retinitis pigmentosa. Previous research using functional magnetic resonance imaging (fMRI) has demonstrated physiological changes in the eye and/or cortical activation in response to stimulation of vision-related acupoints in normally sighted patients.5–7
In the past 15 years, over 400 patients with retinitis pigmentosa have received acupuncture treatments at the private practice of a licensed naturopathic physician and acupuncturist (AR) with expertise in Chinese medicine for ocular disease.8,9 Rather than relying solely on self-reporting by patients with retinitis pigmentosa of improved VF and night vision following treatment by a single highly trained practitioner, we felt it was important to better document the effects, to inform patients interested in this potential treatment and to explore whether a different, well-trained acupuncturist could obtain demonstrable results with a standardised treatment procedure. The goal of this project was to collect preliminary data on this established acupuncture protocol, administered by a Johns Hopkins University (JHU) credentialed acupuncturist (JG) to subjects with retinitis pigmentosa extensively tested by a JHU credentialed optometrist (AKB). We aimed to determine whether such a study would support the hypothesis that visual function can improve after treatment with a standardised acupuncture protocol.
METHODS
This was a prospective case series in which all subjects received acupuncture to determine preliminary efficacy or proof of principle with the standardised protocol. This acupuncture protocol was specifically developed for retinitis pigmentosa based on the extensive clinical experience of a naturopathic physician and licensed acupuncturist and has an acceptable safety profile but only if administered by a qualified, well-trained acupuncturist. A placebo control group was not included in this early research as selection of a control intervention in acupuncture research remains controversial.10 Specifically, placebo acupuncture (that is, needles inserted into non-acupoints or use of a blunt tip sham needle) may not necessarily represent an inert and valid control. All procedures took place at JHU between April and December, 2012. The protocol for the study was approved by the Institutional Review Board of JHU, School of Medicine and followed the tenets of the Declaration of Helsinki. Informed consent was obtained from the subjects after explanation of the nature and possible consequences of the study.
Subjects
A total of 12 subjects with retinitis pigmentosa confirmed by previous diagnostic tests and ocular examination were enrolled and all 12 completed the acupuncture protocol. Eligible subjects with retinitis pigmentosa had no previous history of acupuncture for retinitis pigmentosa, VA better than 6/120, demonstrated VF loss and did not smoke cigarettes in the past six months. Current or recent smokers were excluded since ocular blood flow11 and vasodynamic responses to changes in light12 in the central retinal artery are reduced among smokers with normal vision and the toxic effects of nicotine may damage the retina and retinal pigment epithelium (RPE).13 Subjects continued to take all nutritional supplements they considered useful for retinitis pigmentosa (for example, lutein, vitamin A) and had been taking prior to participation. An ocular history determined whether subjects had ever seen stars at night and their age at first onset of visual loss at night and in their periphery. An open-ended interview was conducted at the beginning of each post-treatment follow-up visit (by AKB) prior to any vision testing to determine subjective changes in visual function.
Test frequency/duration
All subjects completed baseline vision and ocular assessments at a single visit within 90 days prior to initiating the acupuncture intervention and the tests were repeated within one week and one month after intervention. In subjects with significant improvements in the visual function at both one week and one month after treatment, the tests were repeated every 1.0 to 1.5 months for up to 10 to 12 months after treatment to assess the duration of positive longitudinal effects. Each visit took about three to four hours to complete.
Vision measures
The battery of visual function tests included the dark-adapted full-field stimulus threshold (FST; Diagnosys Espion),14,15 dark-adaptometry (Scotopic Sensitivity Tester [SST]-1; LKC Technologies),16 kinetic perimetry (Goldmann visual field), VA (Early Treatment Diabetic Retinopathy Study [ETDRS] chart) and contrast sensitivity (CS with the Pelli-Robson chart). The vision testing was conducted by a single, well-trained examiner (AKB) according to her previously published methods for VA,17 CS,17 Goldmann visual field,18 SST-1 dark-adaptometry16 and dark-adapted full-field stimulus threshold.14,15 VA and CS were measured in each eye with trial lenses as indicated by a refraction at each visit. FST was determined three times within a visit for each eye with a white light stimulus after 45 minutes of dark-adaption and with dilated pupils.
SD-OCT
Spectral domain optical coherence tomography (SD-OCT; Heidelberg Spectralis) was obtained at the screening visit to determine the presence of cystoid macular oedema (CME) and help correlate the extent of retinal degeneration (that is, photoreceptor and retinal pigment epithelial loss) with disease progression or treatment response. SD-OCT was repeated for the same segmentation locations after treatment, if cystoid macular oedema was noted pre-treatment.
Acupuncture
Modern clinical research in China and Dr Rosenfarb's experience suggests that adding electroacupuncture to an acupuncture protocol improves the probability of positive results in retinitis pigmentosa.9 The protocol consists of 10 sessions in a two-week period (five 30-minute sessions per week). We used an electroacupuncture device, namely the transcutaneous electrical nerve stimulator unit (TENS, Lhasa OMS Inc, Weymouth, MA, USA) to deliver 15 Hz continuous wave stimulation and attached the leads to four of the acupuncture points located on the forehead and below the eye. The established protocol indicates the specific pre-selected points for all participants, needling depths and manipulation techniques. The standard points for all subjects are located around the eyes (that is, forehead/temples), on the head, ears, abdomen, hands, arms, lower legs and toes. The acupuncture points are: GV-20, GV-24, yin tang, tai yang, BL-2 to yu yao with electrostimulation, qiu hou to yi ming with electrostimulation, ST-2, GB-20, ear (Eye 1, Eye 2, Eye, Liver), CV-12, CV-6, ST-25, LI-12, LI-3, HT-8 and BL-67. Additionally, the following proximate point combinations were palpated and of each pair, the one that was more sensitive was selected for needling: LV-8/KD-10, SP-6/KD-7, LV-2/LV-3. An IR 3000 heat lamp was placed over the abdomen to warm acupuncture points in that area, which is thought to increase the response of the overall treatment. The heat lamp was used in nine of 12 subjects for five to 30 minutes per session, depending on varying individual sensitivities to the heat.
Data analyses
Changes in vision were considered significant and a sign of improvement, if the change after treatment exceeded previously published values for test variability in retinitis pigmentosa,14–18 that is, 3.0 to 3.6 dB 95% confidence interval (CI) for dark-adapted full-field stimulus threshold, greater than 30 per cent coefficients of variation (CoV) for SST-1 dark-adaptometry, greater than 20 per cent at two consecutive tests for Goldmann visual field area, more than seven letters for ETDRS VA or more than six letters for Pelli-Robson contrast sensitivity. Goldmann visual field results were digitised to determine the seeing retinal areas.19 Two-sample t-tests were used to explore differences between subjects who did and those who did not improve significantly in the scotopic sensitivity tests (that is, FST or SST-1 dark-adaptometry), using Stata/IC version 10.0 (Stata Corp, College Station, TX, USA).
RESULTS
Each subject's age, gender, ocular history and baseline visual function measures are listed in Table 1. The acupuncture procedures were well tolerated without adverse events or loss of vision. All 12 subjects indicated they would be willing to repeat the treatment series in the future.
Table 1.
Listing of subjects' ages, gender, ocular history, baseline visual function measures and maximum improvement in either eye from one week to one month after treatment
| ID | Age | Gender | logMAR VA better eye | Max logMAR VA improvement improvement | logCS better eye | Max logCS improvement | V4e log GVF area better eye | III4e log GVF area better eye | GVF % improvement at 1 week. | FST improvement | Peak FST improvement (dB) | Baseline mean FST better eye | Ever saw stars at night | Age of first night vision loss | Age of first visual field loss | Years of night vision loss | years of visual field loss | RP genetic mutation |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1† | 50 | F | 0.26 | −0.06 | 1.25 | 0.10 | 2.32 | 20.2% | Yes | −24.3 | −45.0 | Yes | 40 | 40 | 10 | 10 | X-linked:RPGR | |
| 2 | 52 | M | 0.08 | −0.08 | 1.6 | 0.30 | 2.45 | 41.3% | No | −2.2 | −41.1 | Yes | 9 | 51 | 43 | 1 | AD: TOPORS | |
| 3† | 54 | F | 0.48 | −0.06 | 1.40 | 0.55† | 1.5 | 1.07 | 23.0% | Yes | −13.0 | −22.8 | Yes | 23 | 26 | 31 | 28 | AR: Usher 2A |
| 4 | 50 | M | 1.02 | −0.10 | 0.55 | 0.20 | 1.68 | 1.24 | 20.2% | No | −4.7 | −19.9 | Yes | 8 | 10 | 42 | 40 | AR |
| 5† | 26 | M | 0.46 | −0.08 | 0.90 | 0.00 | 2.68 | 2.05 | 28.8% | Yes | −11.6 | −15.2 | Yes | 12 | 19 | 14 | 7 | adopted |
| 6 | 18 | M | 0.08 | −0.02 | 1.60 | 0.05 | 2.21 | 31.8% | No | −2.9 | −43.4 | 1–2 | 0 | 0 | 18 | 18 | AR | |
| 7 | 31 | M | 0.76 | 0.04 | 0.45 | 0.00 | 2.57 | 4.7% | Unreliable | −49.5 | Yes | 22 | 26 | 9 | 5 | AR | ||
| 8 | 49 | F | 0.00 | −0.12 | 1.80 | 0.05 | 2.4 | 2.15 | 7.2% | No | 0.1 | −39.6 | 1–2 | 0 | 25 | 49 | 24 | AD |
| 9 | 40 | M | 0.20 | −0.04 | 1.10 | 0.05 | 1.26 | 1.09 | 0.0% | No | 0.4 | −22.8 | No | 0 | 0 | 40 | 40 | AD |
| 10 | 34 | M | 0.28 | −0.08 | 1.05 | 0.10 | 2.22 | 1.06 | −15% | No | 0.3 | −43.1 | Yes | 17 | 15 | 17 | 19 | X-linked:RPGR |
| 11† | 78 | F | 0.54 | −0.20† | 0.85 | 0.00 | 2.29 | 2.06 | 20.2% | No | 1.0 | −63.2 | Yes | 53 | 68 | 25 | 10 | AD |
| 12† | 40 | M | 0.18 | 0.00 | 1.40 | 0.10 | 2.79 | 2.69 | 9.6% | Normal baseline | Yes | 33 | 38 | 7 | 2 | AR |
indicates subjects with significant improvement in scotopic sensitivity measures (FST or SST-1) or significant VA or contrast sensitivity improvement.
AD: autosomal dominant, AR: autosomal recessive, GVF:Goldmann visual field, FST: dark-adapted full-field stimulus threshold.
Three of nine subjects with reliably measurable dark-adapted full-field stimulus thresholds experienced a significant 10.3 to 17.5 dB (that is, 13- to 53-fold) improvement in full-field stimulus thresholds dark-adapted sensitivity in both eyes at one week after treatment (subjects 1, 3 and 5), which is outside the typical test-retest variability (95% CI) of 3.0 to 3.6 dB for the full-field stimulus thresholds in retinitis pigmentosa14,15 and was maintained for at least 10 to 12 months. Figure 1 shows the results for dark-adapted sensitivity using the full-field stimulus threshold displayed as means and 95% CIs based on three within-session measures for each subject. The previously reported range for normally sighted subjects without retinitis pigmentosa14 is indicated in the grey-shaded area of Figure 1. Subject 1's post-treatment improved sensitivities are in this normal range.
Figure 1.
Line graph indicating full-field stimulus threshold (FST) dark-adapted sensitivity for each subject across visits, with the mean and 95% confidence intervals (CI) for three measures at each time. Subject ID numbers are indicated to the right of their corresponding results. The previously reported normal range is indicated in the grey shaded area
After finding that three of the first nine subjects had improvements in FST scotopic sensitivity (subject 7 was not able to provide reliable FST results due to interference from spontaneously occurring photopsias), we determined the rate or time course for dark-adaptation in our last two subjects using the SST-1. We found a mean improvement of 43 per cent (range 36 to 53 per cent across intensities; that is, more rapid dark-adaptation) in subject 11 and mean improvement of 54 per cent (range 43 to 62 per cent from 10 to 30 dB) in subject 12 at one week after treatment in Figure 2. These changes reflect reductions in the time required to reach a certain level of intensity when comparing before and after treatment and were outside the typical coefficient of variation of less than 30 per cent for the SST-1 that we previously determined for patients with retinitis pigmentosa and normal subjects.16 Subject 12's improvements in dark-adapted sensitivity in the first 10 minutes from 30 to 15 dB were still maintained six weeks after treatment. Previously published data16 from normally sighted controls are indicated in thin black lines in Figure 2.
Figure 2.
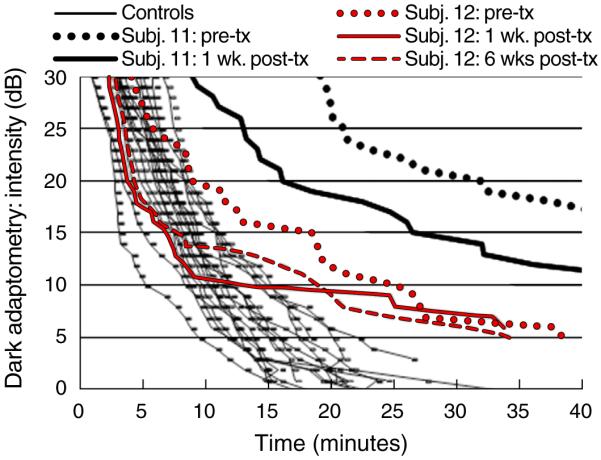
Scotopic Sensitivity Tester (SST)-1 dark-adaptation curve data for subjects 11 and 12, drawn with black and red lines, respectively. Each curve represents the detection time at the pre-treatment or one or six weeks after treatment, at the stimulus intensities plotted along the ordinate. Data from normally sighted controls are drawn with thin black lines; each curve represents one individual's mean detection time across four visits
When comparing subjects who did (n = 5) or did not (n = 6) have a significant improvement in scotopic sensitivity with the FST or SST-1 dark-adaptometry, there was no statistically significant difference in the baseline FST (p = 0.49), GVF log retinal area for the III4e target (p = 0.39), VA in the better eye (p = 0.55), CS in the better eye (p = 0.60), age of onset for VF loss (p = 0.10) or current age (p = 0.40). The age of onset for loss of night vision was statistically significantly greater in subjects who had a significant improvement in scotopic sensitivity after treatment, compared to subjects who did not improve (32 versus 6.0 years) (p = 0.016).
Subject 12 had full Goldmann visual fields with pericentral scotomas with the V4e stimulus that were reduced by 64.4 and 59.4 per cent in the right and left eyes, respectively, one week after treatment. By six weeks, his pericentral scotomas were reduced by only 18.1 and 20.4 per cent in the right and left eyes, respectively, indicating that the effects measured with Goldmann visual fields were not persisting. Improvements in Goldmann visual field area of more than 20 per cent were not noted beyond one week after treatment in other subjects, except in subject 6, whose improvements ranged between 59 to 99 per cent in each eye for the II4e isopter at one, two and three months post-treatment. This subject had previous experience with completing Goldmann visual fields in clinical practice, prior to his study participation.
Significant improvements for ETDRS VA or Pelli-Robson contrast sensitivity occurred in one subject (subject 11) with 0.2 logMAR or two lines of improvement and another subject (subject 3) with 0.55 logCS or four steps of improvement. The only subject with a significant change in contrast sensitivity also developed a reduction in cystoid macular oedema observed with SD-OCT post-treatment and shown in Figure 3. We are unable to state whether the improvements in contrast sensitivity and cystoid macular oedema were a result of the acupuncture treatment, as there is a possibility that the cystoid macular oedema may have spontaneously resolved. The non-significant improvement in VA subjects 3 and 8 by 0.04 and 0.12 logMAR, respectively, was correlated with reductions in cystoid macular oedema observed with SD-OCT after treatment. Differences in the magnitude of the VA change appear to be related to the position of the reduced cystoid macular oedema relative to the fovea, that is, closer in subject 8 than subject 3, as shown in Figure 3. These were the only two subjects with cystoid macular oedema at the pre-treatment assessment and a larger sample with cystoid macular oedema would be needed to establish whether changes are related to acupuncture treatment or spontaneous resolution. The baseline qualitative amount of RPE dysfunction measured with fundus autofluorescence (FAF; Heidelberg Spectralis, Carlsbad, CA, USA) did not predict the subjects who developed a significant improvement in visual function.
Figure 3.

Spectral domain optical coherence tomography (SD-OCT) images from subjects 3 (left panels) and 8 (right panels) with a cross-section obtained through the fovea, demonstrating intraretinal cystoid macular oedema at the pre-treatment visit (top panels) that diminished after treatment (lower panels)
Table 2 lists the subjectively reported improvements in visual function noted by participants during their activities of daily living at one week to one month after treatment. The largest proportion of subjects reported improvement in vision in dim or dark environments. There was a statistically significant correlation between subjects who had significantly improved results during scotopic sensitivity testing with the FST or SST-1 (n = 5), and subjects who reported improved vision at night in dark areas (χ2 = 4.4; p = 0.036). Four of five with improved scotopic testing noted subjective improvements in real-world situations and activities and only one (subject 6), who did not improve on the FST noted a subjective improvement. Although subject 5 had a significant improvement in scotopic sensitivity with the FST, his night vision still remained well below normal, which may have limited impact on daily activities and may explain why he did not notice any improvements in everyday life.
Table 2.
Subjectively reported improvements in visual function at one week to one month post-treatment
| ID | Glare | Distance clarity | Near reading or computer | Contrast sensitivity | Visual field area | Visual field clarity/brightness | Colour vision | Vision in dim areas/dusk (mesopic) | Vision at night in dark (scotopic) | Bright to dim transition/adaptation | Photopsias dec. intensity and area | Reduced eye strain/fatigue |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1† | − | − | − | − | − | − | − | + | + | + | + | − |
| 2 | − | − | − | − | − | − | + | + | − | − | − | − |
| 3† | − | − | − | + | − | − | − | + | + | + | − | − |
| 4 | − | + | + | − | + | + | + | + | − | − | − | − |
| 5† | − | − | − | − | − | + | + | − | − | − | + | − |
| 6 | − | − | − | + | − | + | + | + | + | + | − | − |
| 7 | − | − | − | − | − | − | − | + | + | + | − | − |
| 8 | − | − | − | − | + | − | − | − | − | − | − | − |
| 9 | − | − | − | − | − | − | − | − | − | − | − | − |
| 10 | − | − | − | − | + | − | − | − | − | − | − | + |
| 11† | − | + | + | − | − | − | − | + | + | − | + | − |
| 12† | − | − | − | − | − | + | − | + | + | + | − | − |
| Total | 0 | 2 | 2 | 2 | 3 | 4 | 4 | 8 | 6 | 5 | 3 | 1 |
Key: − = no change; + = improved.
subjects with significant improvement in scotopic sensitivity measures (FST or SST-1) or significant VA or CS improvement.
CS: contrast sensitivity, FST: dark-adapted full-field stimulus threshold.
DISCUSSION
The current pilot study describes the quantifiable changes in visual function that patients with retinitis pigmentosa exhibited after receiving a standardised acupuncture protocol. We found that the most robust improvements in visual function for the largest proportion of subjects (five of 11) were measured by the scotopic sensitivity tests. Previous case series studies of acupuncture for retinitis pigmentosa did not measure this aspect of visual function and instead focused on measurements of VA and VF,6,7 which did not change significantly in the vast majority of our subjects (10 of 12). Visual loss at night is a hallmark of retinitis pigmentosa and the subjectively reported improvements after treatment appear to be clinically meaningful for subjects with significant measurable changes in the psychophysical tests of scotopic sensitivity.
Not all subjects developed a significant improvement in visual function following the acupuncture protocol but the current sample was too small to draw any conclusions regarding factors that may influence individual differences in treatment response. Our data hint that age of onset of loss of night vision may predict improvements in dark-adapted visual function. Future research will need to identify specific patient-related factors that may predict responses in visual function following acupuncture, for example, systemic medications or lifestyle choices (diet, exercise), which may be modifiable and/or could be used as inclusion/exclusion criteria for future clinical trials. Not all of the subjects in our study had a confirmed genetic mutation for retinitis pigmentosa but it is noteworthy that the two unrelated subjects with X-linked RPGR mutations listed in Table 1 had different responses to acupuncture despite similar baseline FSTs; that is, the affected female carrier developed a significant improvement (subject 1), while the affected male did not have a significant change (subject 10). The roles of retinitis pigmentosa genotypes and other patient-specific factors (for example, epigenetic changes) on responsiveness to acupuncture should be further explored with a larger sample.
In our previously published studies18 of test-retest variability in retinitis pigmentosa, we examined whether learning effects were present during four sessions at monthly intervals for tests of VA, contrast sensitivity and dark-adaptation, as well as for two repeated tests of Goldmann visual fields, and did not find evidence of a systematic learning effect across subjects with retinitis pigmentosa for any of these tests. Therefore, we do not believe that learning effects played a significant role in the improvements noted during this study. We found that seven of 12 subjects had a greater than 20 per cent improvement in field area one week after treatment that was not sustained at one month. Our experience is that typical variability in field area is less than 20 per cent for subjects with retinitis pigmentosa with a visual field radius greater than seven degrees.18 Goldmann visual field variability may be influenced by many patient-related factors that are difficult to quantify; however, we have no reason to believe that the subjects with retinitis pigmentosa in this study would be significantly more variable than those enrolled in our previous research and tested by the same operator.
To provide a scientific rationale for future clinical trials involving acupuncture for retinitis pigmentosa and to guide their design, it is necessary to obtain further evidence of plausible physiological mechanisms that could be responsible for improvements in visual function in patients with retinitis pigmentosa following acupuncture. Although basic research with animal models indicates that neurotrophic factors increase in response to electroacupuncture,5 it is not possible to assess these factors directly in patients with retinitis pigmentosa. Ciliary neurotrophic factor regenerates cone outer segments in animal models20 and may reduce cone photoreceptor loss21 and improve cone function22 in patients with retinitis pigmentosa. Thus, the cone contrast test23 might serve as an indirect measure of neurotrophic factor changes. In fact, one-third of our subjects (subjects 2, 4, 5 and 6) reported improved colour vision after treatment. One third of the subjects (4, 5, 6 and 12) reported that the entire visual field appeared brighter, more vibrant and crisper after treatment. Subject 12 said that this change was `as if the world looked like it had a glossy photo finish, whereas previously it had a matte finish.' While none of our tests for vision were appropriate to capture this aspect of vision, perhaps static threshold visual fields or microperimetry may be better suited to assess this type of visual change in future studies.
In healthy human volunteers without retinitis pigmentosa, an immediate increase in ophthalmic artery (OA) blood velocity24 or a decreased vascular resistance in the posterior ciliary arteries (PCAs)25 has been reported following needling of vision-related acupoints, while such changes were not found for non-vision related acupoints. Significantly reduced vascular resistance in the central retinal artery (CRA) and PCAs was found following acupuncture in open-angle glaucoma subjects.25 Electroacupuncture increases blood fluidity by decreasing platelet aggregation in the systemic vascular system of normal subjects, and may involve an endogenous adrenergic mechanism.26 Successful treatment of other chronic diseases, such as lower back pain, with electroacupuncture has been attributed to increased blood flow to surrounding nerves (for example, sciatic).27 Ocular blood flow as a potential mechanism and indicator of physiological changes that occur in response to electroacupuncture has not been reported previously for patients with retinitis pigmentosa and is a potential area to explore in future studies. Several groups have documented reduced velocity of ocular blood flow in both early and late stage retinitis pigmentosa compared to normal controls;28–32 however, no previous longitudinal or experimental studies have adequately explored the relationship between changes in ocular blood flow velocity and either improvements or reductions in visual function in retinitis pigmentosa. The relationship between vascular and visual function in retinal ischaemia has been described previously33 and it might also play a role in patients with retinitis pigmentosa after acupuncture.
In a disease such as retinitis pigmentosa, the management options of which are extremely limited, it is important to examine the potential for integrative therapies to improve visual function. Acupuncture is a relatively inexpensive treatment modality that is minimally invasive and involves minimal risk when administered by an acupuncturist with appropriate training. Continued studies should examine the potential for this treatment to improve visual function, thus improving the quality of life of patients with retinitis pigmentosa, while other promising treatments such as stem cells, gene therapies and pharmacologic agents are being developed. Additional studies would provide the necessary groundwork to help justify a randomised controlled trial, by identifying which visual and physiological measures, such as ocular or retinal blood flow, are responsive to acupuncture, demonstrating the feasibility of the methodology, validity of proposed mechanisms and providing improved estimates of the effect.
IMPORTANT NOTE TO READERS
This acupuncture protocol must be administered by a qualified and licensed acupuncturist, preferably with hands-on training and experience with specific needling techniques for treating patients with retinitis pigmentosa. It is important to caution patients that the risks if treated by some-one without appropriate expertise include serious injuries such as nerve damage, cellulitis and other infections or haematomas. A randomised, controlled trial is needed to determine the efficacy of this protocol. We strongly recommend preliminary vision testing by the patient's eye-care provider before commencing treatment and retesting after 10 treatments to assess measurable improvements. Any recommendations regarding continued treatment should be based on changes in visual function.
ACKNOWLEDGEMENT
This research was supported by National Institutes of Health Grant K23EY018356 (AKB).
REFERENCES
- 1.Kiser AK, Dagnelie G. Reported effects of non-traditional treatments and complementary and alternative medicine by retinitis pigmentosa patients. Clin Exp Optom. 2008;91:166–176. doi: 10.1111/j.1444-0938.2007.00224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pagani L, Manni L, Aloe L. Effects of electroacupuncture on retinal nerve growth factor and brain-derived neurotrophic factor expression in a rat model of retinitis pigmentosa. Brain Res. 2006;1092:198–206. doi: 10.1016/j.brainres.2006.03.074. [DOI] [PubMed] [Google Scholar]
- 3.Wong S, Ching R. The use of acupuncture in ophthalmology. Am J Chin Med. 1980;8:104–153. doi: 10.1142/s0192415x80000098. [DOI] [PubMed] [Google Scholar]
- 4.Dabov S, Goutoranov G, Ivanova R, Petkova N. Clinical application of acupuncture in ophthalmology. Acupunct Electrother Res. 1985;10:79–93. doi: 10.3727/036012985816714577. [DOI] [PubMed] [Google Scholar]
- 5.Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D, Fazekas F, Ebner F. Acupuncture using laser needles modulates brain function: first evidence from functional transcranial Doppler sonography and functional magnetic resonance imaging. Lasers Med Sci. 2004;19:6–11. doi: 10.1007/s10103-004-0291-0. [DOI] [PubMed] [Google Scholar]
- 6.Li G, Cheung RT, Ma QY, Yang ES. Visual cortical activations on fMRI upon stimulation of the vision-implicated acupoints. Neuroreport. 2003;14:669–673. doi: 10.1097/00001756-200304150-00002. [DOI] [PubMed] [Google Scholar]
- 7.Siedentopf CM, Golaszewski SM, Mottaghy FM, Ruff CC, Felber S, Schlager A. Functional magnetic resonance imaging detects activation of the visual association cortex during laser acupuncture of the foot in humans. Neurosci Lett. 2002;327:53–56. doi: 10.1016/s0304-3940(02)00383-x. [DOI] [PubMed] [Google Scholar]
- 8.Rosenfarb A. Healing Your Eyes with Chinese Medicine. North Atlantic Books; Berkeley, California: 2007. [Google Scholar]
- 9.Rosenfarb A. Ophthalmology in Chinese Medicine. People's Medical Publishing House; Beijing, China: 2011. [Google Scholar]
- 10.Lin JG, Chen CH, Huang YC, Chen YH. How to design the control group in randomized controlled trials of acupuncture? Evid Based Complement Alternat Med. 2012;2012:875284. doi: 10.1155/2012/875284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steigerwalt RD, Jr, Laurora G, Incandela L, Cesarone MR, Belcaro GV, De Sanctis MT. Ocular and orbital blood flow in cigarette smokers. Retina. 2000;20:394–397. doi: 10.1097/00006982-200007000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Havelius U, Hansen F. Ocular vasodynamic changes in light and darkness in smokers. Invest Ophthalmol Vis Sci. 2005;46:1698–1705. doi: 10.1167/iovs.04-0756. [DOI] [PubMed] [Google Scholar]
- 13.Yang L, Gong H, Wang Y, Wang Y, Yin H, Chen P, Zhang H, et al. Nicotine alters morphology and function of retinal pigment epithelial cells in mice. Toxicol Pathol. 2010;38:560–567. doi: 10.1177/0192623310368983. [DOI] [PubMed] [Google Scholar]
- 14.Klein M, Birch DG. Psychophysical assessment of low visual function in patients with retinal degenerative diseases (RDDs) with the Diagnosys full-field stimulus threshold (D-FST) Doc Ophthalmol. 2009;119:217–224. doi: 10.1007/s10633-009-9204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roman AJ, Cideciyan AV, Aleman TS, Jacobson SG. Full-field stimulus testing (FST) to quantify visual perception in severely blind candidates for treatment trials. Physiol Meas. 2007;28:N51–N56. doi: 10.1088/0967-3334/28/8/N02. [DOI] [PubMed] [Google Scholar]
- 16.Kiser AK, Mladenovich D, Eshraghi F, Bourdeau D, Dagnelie G. Reliability and consistency of dark-adapted psychophysical measures in advanced eye disease. Invest Ophthalmol Vis Sci. 2006;47:444–452. doi: 10.1167/iovs.04-1146. [DOI] [PubMed] [Google Scholar]
- 17.Kiser AK, Mladenovich D, Eshraghi F, Bourdeau D, Dagnelie G. Reliability and consistency of visual acuity and contrast sensitivity measures in advanced eye disease. Optom Vis Sci. 2005;82:946–954. doi: 10.1097/01.opx.0000187863.12609.7b. [DOI] [PubMed] [Google Scholar]
- 18.Bittner AK, Iftikhar MH, Dagnelie G. Test-retest, within-visit variability of Goldmann visual fields in retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2011;52:8042–8046. doi: 10.1167/iovs.11-8321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dagnelie G. Conversion of planimetric visual field data into solid angles and retinal areas. Clin Vis Sci. 1990;5:95–100. [Google Scholar]
- 20.Wen R, Tao W, Luo L, Huang D, Kauper K, Stabila P, LaVail MM, et al. Regeneration of cone outer segments induced by CNTF. Adv Exp Med Biol. 2012;723:93–99. doi: 10.1007/978-1-4614-0631-0_13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Talcott KE, Ratnam K, Sundquist SM, Lucero AS, Lujan BJ, Tao W, Porco TC, et al. Longitudinal study of cone photoreceptors during retinal degeneration and in response to ciliary neurotrophic factor treatment. Invest Ophthalmol Vis Sci. 2011;52:2219–2226. doi: 10.1167/iovs.10-6479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sieving PA, Caruso RC, Tao W, Coleman HR, Thompson DJ, Fullmer KR, Bush RA. Ciliary neurotrophic factor (CNTF) for human retinal degeneration: phase I trial of CNTF delivered by encapsulated cell intraocular implants. Proc Natl Acad Sci USA. 2006;103:3896–3901. doi: 10.1073/pnas.0600236103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rabin J, Gooch J, Ivan D. Rapid quantification of color vision: the cone contrast test. Invest Ophthalmol Vis Sci. 2011;52:816–820. doi: 10.1167/iovs.10-6283. [DOI] [PubMed] [Google Scholar]
- 24.Litscher G. Computer-based quantification of traditional chinese-, ear- and Korean hand acu-puncture: needle-induced changes of regional cerebral blood flow velocity. Neurol Res. 2002;24:377–380. doi: 10.1179/016164102101200177. [DOI] [PubMed] [Google Scholar]
- 25.Takayama S, Watanabe M, Kusuyama H, Nagase S, Seki T, Nakazawa T, Yaegashi N. Evaluation of the effects of acupuncture on blood flow in humans with ultrasound color Doppler imaging. Evid Based Complement Alternat Med. 2012;2012:513638. doi: 10.1155/2012/513638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ishikawa S, Suga H, Fukushima M, Yoshida A, Yoshida Y, Sunagawa M, Hisamitsu T. Blood fluidity enhancement by electrical acupuncture stimulation is related to an adrenergic mechanism. J Acupunct Meridian Stud. 2012;5:21–28. doi: 10.1016/j.jams.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 27.Inoue M, Kitakoji H, Yano T, Ishizaki N, Itoi M, Katsumi Y. Acupuncture treatment for low back pain and lower limb symptoms—the relation between acupuncture or electroacupuncture stimulation and sciatic nerve blood flow. Evid Based Complement Alternat Med. 2008;5:133–143. doi: 10.1093/ecam/nem050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Akyol N, Kükner S, Celiker U, Koyu H, Lüleci C. Decreased retinal blood flow in retinitis pigmentosa. Can J Ophthalmol. 1995;30:28–32. [PubMed] [Google Scholar]
- 29.Beutelspacher SC, Serbecic N, Barash H, Burgansky-Eliash Z, Grinvald A, Krastel H, Jonas JB. Retinal blood flow velocity measured by retinal function imaging in retinitis pigmentosa. Graefes Arch Clin Exp Ophthalmol. 2011;249:1855–1858. doi: 10.1007/s00417-011-1757-y. [DOI] [PubMed] [Google Scholar]
- 30.Cellini M, Strobbe E, Gizzi C, Campos EC. ET-1 plasma levels and ocular blood flow in retinitis pigmentosa. Can J Physiol Pharmacol. 2010;88:630–635. doi: 10.1139/Y10-036. [DOI] [PubMed] [Google Scholar]
- 31.Grunwald JE, Maguire AM, Dupont J. Retinal hemodynamics in retinitis pigmentosa. Am J Ophthalmol. 1996;122:502–508. doi: 10.1016/s0002-9394(14)72109-9. [DOI] [PubMed] [Google Scholar]
- 32.Zhang Y, Harrison JM, Nateras OS, Chalfin S, Duong TQ. Decreased retinal-choroidal blood flow in retinitis pigmentosa as measured by MRI. Doc Ophthalmol. 2013;126:187–197. doi: 10.1007/s10633-013-9374-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shoshani YZ, Harris A, Rusia D, Spaeth GL, Siesky B, Pollack A, Wirostko B. Contrast sensitivity, ocular blood flow and their potential role in assessing ischaemic retinal disease. Acta Ophthalmol. 2011;89:e382–e395. doi: 10.1111/j.1755-3768.2011.02130.x. [DOI] [PubMed] [Google Scholar]



