Abstract
Background:
Prior studies have suggested that patient-rated hand function is impacted by depression and pain catastrophization. We studied the impact that these comorbidities have on treatment outcomes.
Methods:
Two hundred and fifty-six patients presenting to an orthopaedic hand clinic were followed in this prospective cohort investigation. Patients who were prescribed treatment for atraumatic hand/wrist conditions were eligible for inclusion. At enrollment, all patients completed the Center for Epidemiologic Studies Depression (CES-D) scale, the Pain Catastrophizing Scale (PCS), and the Michigan Hand Outcomes Questionnaire (MHQ; scale of 0 to 100, with 100 indicating the best hand performance). One month and three months after treatment, patients again completed the MHQ. Participants’ psychological comorbidity status was categorized as either affected (a CES-D score of ≥16, indicating depression, or a PCS score of ≥30, indicating catastrophization) or unaffected (a CES-D score of <16 and a PCS score of <30). Diagnoses and treatments for both the affected and unaffected groups were examined. The effect of time and patient status, and their interaction, on MHQ scores was evaluated by mixed modeling.
Results:
Fifty patients were categorized as affected and 206 as unaffected. Diagnoses and treatments differed minimally between the two groups. At the time of enrollment, the mean MHQ score of the unaffected group (64.9; 95% confidence interval [CI], 62.5 to 67.3) was significantly higher than that of the affected group (48.1; 95% CI, 43.3 to 53.0). Both groups demonstrated similar significant absolute improvement over baseline at three months after treatment (an increase of 12.5 points [95% CI, 7.5 to 17.4] in the affected group and 12.8 points [95% CI, 10.4 to 15.3] in the unaffected group). Thus, at the time of final follow-up, the rating of hand function by the affected patients (60.6 [95% CI, 55.0 to 66.2]) was still significantly poorer than the rating by the unaffected patients (77.7 [95% CI, 75.0 to 80.5]).
Conclusions:
Although patients affected by depression and/or pain catastrophization reported worse self-rated hand function at baseline and at the time of follow-up, these patients showed similar absolute improvement in self-rated hand function following treatment compared with patients with unaffected status.
Level of Evidence:
Prognostic Level I. See Instructions for Authors for a complete description of levels of evidence.
Depression affects 9.1% of individuals in the United States1. More concerning, the estimated prevalence of depression increased 60% from 2005 to 20082. Depression can affect people’s interpretation of pain and negatively influence their experience with physical health problems and physical function3-6. The prevalence of depression is believed to be even higher among all orthopaedic patients compared with the general population7-10. Furthermore, any orthopaedic patient is at substantial risk for depression—either its onset or its unmasking—regardless of the severity of the orthopaedic presentation7,11,12.
Often intermixed with depression is pain catastrophization, which also influences the perception of pain and function. Catastrophization is defined as an exaggerated or inappropriate response to nociception, including elements of rumination, magnification, and helplessness13-17, and it predicts the transformation of acute pain episodes into persisting, chronic issues18,19. With emotional distress playing a key role in both depression and pain catastrophization, it is not surprising that these two psychological morbidities have been correlated14,20-24. As coexisting conditions, depression and pain catastrophization are important psychological comorbidities among patients with disabling physical pain5,25 and have an additive and adverse effect on people’s interpretation of physical pain4. They are also predictive of persisting pain and general musculoskeletal complaints at the time of follow-up appointments six months after orthopaedic treatment3,26,27.
In orthopaedics, few studies have examined the effects of these psychological comorbidities—depression and pain catastrophization—on patient-rated outcome measures for upper-extremity musculoskeletal injuries. Depression and pain catastrophization scores, as measured with the Center for Epidemiologic Studies Depression (CES-D) scale and the Pain Catastrophizing Scale (PCS), are strongly and negatively correlated with patient-rated upper-extremity function as assessed with use of the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire3,5,25,28,29. However, prior investigations on this effect in hand surgery have mostly focused on cross-sectional data without considering change in patient-rated outcomes over time25,29-32.
This study was designed to determine the impact of depression (as measured with use of the CES-D) and pain catastrophization (measured with use of the PCS) on patient-rated hand function as assessed using a hand-specific measure (the Michigan Hand Outcomes Questionnaire [MHQ]) both before orthopaedic treatment and after (one and three months following treatment). Our primary hypothesis was that patients affected by these mental comorbidities would have a worse patient-rated assessment of their hand function at baseline and following treatment (one and three months) compared with unaffected patients. Our secondary aim was to determine the absolute effect of depression and pain catastrophization on patient-rated response to treatment for hand conditions. We hypothesized that patients who were affected by depression and pain catastrophization would demonstrate a response to treatment at three months, as measured by absolute change in MHQ score from baseline, that was equal to the response to treatment of unaffected patients.
Materials and Methods
We obtained institutional review board approval prior to conducting this prospective cohort study at our tertiary medical center. We recruited patients from four orthopaedic hand clinics at our institution. For inclusion, patients were required to be over the age of eighteen years and proficient in English and to have had an atraumatic diagnosis, regardless of prescribed treatment. Patients presenting with acute traumatic conditions or with expected follow-up outside our institution were excluded.
Patients were offered participation in this observational study after being assessed by the physician and were provided with appropriate orthopaedic treatment, which included bracing, medication, corticosteroid injection, referral to occupational therapy, or surgery. After providing written consent, participants completed three initial assessments, from which baseline data were obtained. To assess depression, patients completed the twenty-question CES-D scale (a scale of 0 to 60, with 60 indicating the highest depressive symptomatology)33-36. To assess pain catastrophization, subjects completed the thirteen-question PCS (a scale of 0 to 52, with 52 indicating the highest catastrophizing behavior)13,37. Both of these scales were chosen because they have been previously validated and used in similar studies5,25,28,34-39. To assess hand function, subjects completed the seventy-one-question MHQ (a scale of 0 to 100, with 100 indicating the best hand performance), which was chosen because it distinguishes the left and right hand and includes subscales40-50. Patient demographic information collected included date of birth, sex, ethnic and racial background, self-report of clinically diagnosed depression, whether the patient was currently receiving treatment for depression, and contact information.
All patients provided follow-up data at two time points: one-month (± one week) after receiving treatment and three months (± two weeks) after receiving treatment. At each of these time points, patients completed the MHQ. We also collected data regarding subjects’ diagnosis(es) and treatment(s). Study data were collected and managed using REDCap (Research Electronic Data Capture) tools hosted at our institution51,52.
Sample Size
The chosen sample size was determined a priori using the following data. We estimated a 20% prevalence of depression and pain catastrophization in our patients (based on other orthopaedic reports7-10). We planned to enroll all patients who met our inclusion criteria consecutively until fifty patients affected by depression and/or catastrophization were enrolled and then continue enrollment if needed to reach a case-control ratio of 1:4. The 1:4 subject-to-control ratio (fifty affected, 200 unaffected) was chosen because little additional power is gained from higher ratios53. Published data suggest that the average MHQ score (and standard deviation [SD]) for patients with a hand condition is 47.4 ± 18.743 and estimate a minimal clinically important difference in score, ranging from 6 to 23 points48,54. This sample size provided a power of 0.94 to detect a 10-point difference in the MHQ score, based on analysis by repeated-measures ANOVA (analysis of variance). This same sample size provided a power greater than 0.99 to detect a 20-point difference in the MHQ score by repeated-measures ANOVA. For our actual analysis methods (see below), we gained additional power by accounting for the unequal time periods between data collections by performing a mixed model, which makes the above power and effect size estimates slightly conservative.
Data Analysis
Participants were categorized into one of two groups defining their psychological comorbidity status according to baseline data. The affected group was defined as subjects who, at baseline, had either a CES-D score of ≥1635,36 or a PCS score of ≥3037. These cutoffs were determined by the creators of the scales and were subsequently validated as being indicative of depression and pain catastrophization, respectively34,36,37,55-57. Furthermore, these cutoffs are consistent with those presented elsewhere in the orthopaedic literature investigating this topic25. The unaffected group had, at baseline, both a CES-D score of <16 and a PCS score of <30. We anticipated moderate correlation between CES-D and PCS scores4.
Descriptive statistical analysis was performed on the demographic variables for both groups. Associations between groups and diagnosis, treatment, and the dichotomization of treatment into either surgical or nonsurgical treatment were assessed by Fisher exact tests. The correlation of CES-D and PCS scores was determined with use of the Spearman r value. A mixed model was fit to determine the effect that patient status (i.e., affected versus unaffected), time, and their potential interaction had on overall MHQ scores. This model took into account the repeated nature of the data and the unequal time intervals of data collection. All 95% confidence intervals (CIs) underwent a Bonferroni adjustment to account for multiple comparisons. A priori contrasts examined the difference in overall MHQ scores from three months to baseline for both groups as well as the difference in improvement during this duration between the two groups. Secondary analyses compared the MHQ subscale scores between groups as well as determined the impact of surgical versus nonsurgical treatment on overall MHQ scores with use of the same mixed-model methodology. For all comparisons, significance was defined as p < 0.05. There were no missing data among the final cohort contributing to our analyses.
Source of Funding
This work was supported by a grant from the Doris Duke Charitable Foundation to Washington University to fund Doris Duke Clinical Research Fellow Daniel London.
This publication was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448, sub-award TL1 TR000449, from the National Center for Advancing Translational Sciences.
Results
Three hundred and twenty-nine patients were initially approached to participate in this study. Of those patients, 279 fully completed the first set of measures—the CES-D, the PCS, and the MHQ. Two hundred and fifty-six of the 279 patients completed all follow-up assessments and were included in the final data analysis (a 92% retention rate) (Fig. 1). The twenty-three patients who dropped out were not disproportionately members of either patient group (affected versus unaffected, p = 0.07). As expected, CES-D and PCS scores were moderately correlated (rs = 0.54)58.
Fig. 1.

A flowchart depicting the number of patients who were assessed for eligibility, who were enrolled, who completed all measures, and who were included in the final analysis.
The distribution of demographic data, diagnoses, and treatments among the final 256 patients according to group status is presented in Table I. There was an association between a patient being classified as affected and both having a self-reported history of depression (p < 0.001) and being currently treated for depression (p < 0.001). However, these latter categorizations did not identify all patients with affected status. The diagnoses of the patients differed between groups, largely because of the lack of affected patients who were diagnosed with a cyst or mass (p = 0.028). However, there was no significant difference between the groups on the basis of treatment (p = 0.26). When the treatment variable was categorized as surgical versus nonsurgical intervention, a lack of a significant difference was maintained (p = 0.64).
TABLE I.
Demographic Characteristics
| Patient Status |
||
| Variable | Unaffected (N = 206) | Affected (N = 50) |
| Mean age ± SD at enrollment (yr) | 56.9 ± 12.8 | 53.8 ± 11.5 |
| Sex (no. [%]) | ||
| Female | 144 (69.9%) | 37 (74.0%) |
| Male | 62 (30.1%) | 13 (26.0%) |
| Race (no. [%]) | ||
| African-American | 36 (17.5%) | 8 (16.0%) |
| Caucasian | 166 (80.6%) | 42 (84.0%) |
| Native American | 2 (1.0%) | 0 (0.0%) |
| Other | 2 (1.0%) | 0 (0.0%) |
| Depression history (no. [%]) | ||
| History of depression | 31 (15.0%) | 33 (66.0%) |
| Current treatment for depression | 21 (10.2%) | 26 (52.0%) |
| Diagnosis (no. [%]) | ||
| Arthritis | 51 (24.8%) | 14 (28.0%) |
| Cyst/mass | 14 (6.8%) | 0 (0.0%) |
| Dupuytren disease | 10 (4.9%) | 2 (4.0%) |
| Nerve compression | 35 (17.0%) | 14 (28.0%) |
| Tendinitis | 74 (35.9%) | 9 (18.0%) |
| Ulnar-sided wrist pain | 5 (2.4%) | 2 (4.0%) |
| Arthritis and tendinitis | 5 (2.4%) | 2 (4.0%) |
| Nerve compression and tendinitis | 8 (3.9%) | 4 (8.0%) |
| Other | 4 (1.9%) | 3 (6.0%) |
| Treatment (no. [%]) | ||
| Aponeurotomy | 9 (4.4%) | 2 (4.0%) |
| Brace/medication/therapy | 52 (25.2%) | 19 (38.0%) |
| Injection | 97 (47.1%) | 16 (32.0%) |
| Surgery | 47 (22.8%) | 13 (26.0%) |
| Other | 1 (0.5%) | 0 (0.0%) |
Overall MHQ scores of the unaffected group were significantly higher than the MHQ scores of the affected group at all three time points (Table II). The unaffected group reported better function, with a significant increase of 12.8 points in overall MHQ score from baseline to three months (95% CI, 10.4 to 15.3, t = 10.41, p < 0.001). The affected group also reported better function, with a significant increase of 12.5 points in overall MHQ score from baseline to three months (95% CI, 7.5 to 17.4, t = 4.97, p < 0.001). Both groups equivalently improved their MHQ scores over time, as the difference in improvement between the groups was not significant (0.5 ± 2.8 points [standard error of the mean]; t = 0.15, p = 0.88). The interaction between psychological comorbidity status and time was not a significant predictor of overall MHQ score (F = 0.01, p = 0.99). This result can be seen in Figure 2, where the MHQ score trajectories are similar for both groups. However, both a patient’s status (F = 48.03, p < 0.001) and time (F = 39.87, p < 0.001) were each independently significant predictors of overall MHQ scores.
TABLE II.
Mean Overall MHQ Scores at the Three Time Points by Patient Status
| Unaffected |
Affected |
|||
| Mean | 95% CI | Mean | 95% CI | |
| Baseline | 64.9 | 62.5-67.3 | 48.1 | 43.3-53.0 |
| 1 mo. after treatment | 74.0 | 71.3-76.8 | 57.1 | 51.6-62.7 |
| 3 mo. after treatment | 77.7 | 75.0-80.5 | 60.6 | 55.0-66.2 |
Fig. 2.

Mean overall MHQ scores at baseline, one month after treatment, and three months after treatment according to patient status (unaffected or affected). Error bars represent the 95% confidence interval.
The patterns of improved function, stratified by group, were consistent for all six of the MHQ subscales. Table III reports the mean change in subscale scores from baseline to one month and from baseline to three months after treatment. Figure 3 depicts the similar pattern of change observed over time.
TABLE III.
Mean Change in Subscale Scores by Patient Status
| Change in Score from Baseline to One Month |
Change in Score from Baseline to Three Months |
|||
| Subscale | Unaffected | Affected | Unaffected | Affected |
| Overall hand function | 8.1 | 8.4 | 11.9 | 11.9 |
| Activities of daily living | 4.5 | 4.2 | 9.7 | 10.1 |
| Work performance | 2.6 | 1.9 | 8.3 | 9.7 |
| Pain | 13.3 | 13.6 | 20.8 | 20.0 |
| Aesthetics | 3.5 | 2.3 | 4.3 | 3.9 |
| Satisfaction | 22.1 | 21.3 | 25.1 | 24.6 |
Fig. 3.
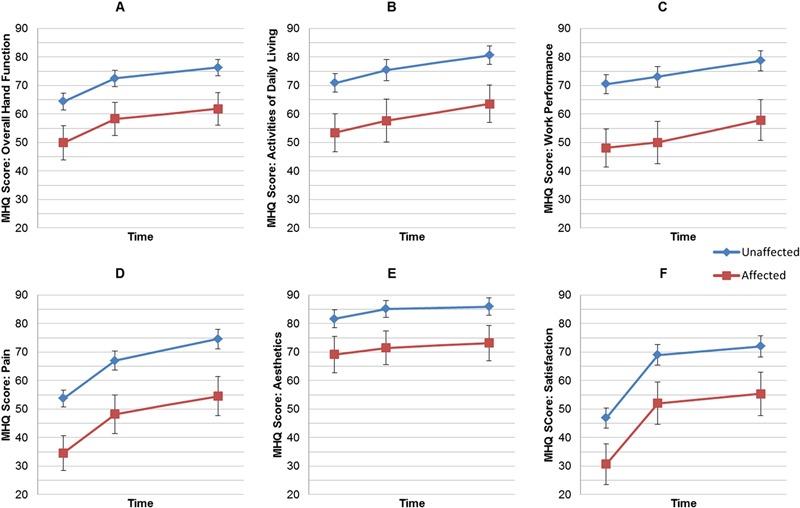
Mean MHQ subscale scores for overall hand function (Fig. 3-A), activities of daily living (Fig. 3-B), work performance (Fig. 3-C), pain (Fig. 3-D), aesthetics (Fig. 3-E), and satisfaction (Fig. 3-F) at baseline, one month after treatment, and three months after treatment according to patient status (unaffected = blue, and affected = red). Error bars represent the 95% confidence interval.
Regardless of psychological comorbidity status, nonsurgical patients showed significant improvement from baseline to one month but nonsignificant improvement from one month to three months. Among surgical patients who were unaffected by depression and/or pain catastrophization, the improvement from baseline to one month was not significant but it was significant from one month to three months. Due to the small sample size of patients who were both affected by depression and/or pain catastrophization and underwent surgery, there were no significant increases from baseline to three months in overall MHQ scores. Within each treatment modality, the overall MHQ scores of the unaffected group were significantly higher than the overall MHQ scores of the affected group at all three time points. Patterns of improvement, however, were similar for both the affected and unaffected groups (Table IV). For all patients, regardless of treatment type, mixed modeling demonstrated that time and patient status predicted overall MHQ scores (F ≥ 9.49, all p < 0.001), with no significant interaction between time and status (p ≥ 0.34).
TABLE IV.
Overall MHQ scores at the Three Time Points by Patient Status and Type of Treatment
| Time Point |
|||||||
| Baseline |
1 Mo. |
3 Mo. |
|||||
| Patient Status | Treatment | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI |
| Affected | Nonsurgical (n = 37) | 51.4 | 46.2-56.7 | 63.4 | 57.0-69.8 | 65.5 | 58.2-72.8 |
| Surgery (n = 13) | 38.8 | 27.4-50.2 | 39.4 | 28.6-50.1 | 46.6 | 31.2-62.0 | |
| Unaffected | Nonsurgical (n = 159) | 66.8 | 64.3-69.4 | 74.0 | 71.2-76.8 | 78.7 | 75.6-81.8 |
| Surgery (n = 47) | 58.2 | 53.3-63.2 | 62.5 | 57.1-67.9 | 74.6 | 69.2-80.0 | |
Discussion
Depression and pain catastrophization can negatively affect how patients perceive their hand function. Patients with relatively high scores on the depression or catastrophizing questionnaires reported clinically worse hand function compared with patients with relatively low scores on the depression and catastrophizing questionnaires, before and after treatment, and regardless of the treatment prescribed. However, both patient groups had equivalent improvement in patient-rated outcome scores following treatment. These results suggest that the psychological comorbidities of depression and pain catastrophization, as assessed by the questionnaires we employed, do not affect patients’ improvement three months after treatment of atraumatic conditions involving the hand.
When examining patient-rated function prior to treatment, the orthopaedic literature has demonstrated that psychological comorbidities, such as depression and pain catastrophization, impact patients’ perceptions of pain and function, and these comorbidities correlate with increased levels of pain and reduced function. Specifically, two prior studies noted that patients with carpal tunnel syndrome and other atraumatic hand conditions had increased pain intensity prior to treatment when depression and pain catastrophization were present25,32. Our data are consistent with these previous studies. However, unlike these prior investigations, our longitudinal data allowed for comparison over time, which demonstrated similar improvement following treatment among affected and unaffected patients over a three-month period.
Our findings also corroborate published data suggesting that depression and pain catastrophization can influence patient-rated outcomes after intervention for orthopaedic problems. For example, two weeks after minor hand surgery for carpal tunnel syndrome, trigger fingers, or benign tumors, patients with higher depressive symptomatology reported disproportionate levels of pain and had worse postoperative outcomes as measured with use of the DASH questionnaire28. Similarly, among patients with depression, psychological status was a predictor of self-reported dissatisfaction two years after carpal tunnel release30. Analogous results were seen in a cross-sectional examination of patients treated for trapeziometacarpal arthritis31. After total knee arthroplasty, patients demonstrating psychological comorbidities exhibited worse functional outcome scores and persistent postoperative pain, from time points that ranged from three months to five years after surgery59-64. While our data show similar outcomes, this is only true when three-month MHQ scores are reviewed in isolation. In contrast to prior studies, our findings indicated that when change in MHQ scores (overall and for the six subscales) was examined over time, the patients in the affected group and the patients in the unaffected group responded to treatment to a similar and clinically relevant extent, regardless of surgical or nonsurgical treatment. Furthermore, the change in satisfaction subscale scores did not differ between the two groups, suggesting that both groups were experiencing the same change in function based on their own perceptions and expectations.
While our data are similar to those suggested in the hand and knee arthroplasty literature, our finding is novel in that we sought to determine patient response to treatment after stratification based on psychological status. The existing hand literature, to our knowledge, focuses on correlational relationships and cross-sectional methods that do not account for a patient’s experienced change in function from before to after treatment. The existing knee arthroplasty literature investigating this topic focuses on modeling scenarios to determine what is predictive of poor outcomes, including depression. While both sets of information are useful, they can mislead readers into assuming that affected patients, in isolation, have poor outcomes after treatment, and therefore, physicians may want to modify which treatment options they offer to that select group. Our data however, indicated that patients who reported high levels of depression and pain catastrophization on questionnaires reported improvement in MHQ scores similar in magnitude to unaffected patients after receiving treatment. Such a finding has relevance when considering pretreatment counseling of patients. On the basis of our data, we expect that patients with depression and pain catastrophization can still anticipate experiencing clinically meaningful improvement in the months following initiation of treatment. However, when considering the greater degree of pain and impairment at baseline, the population affected by depression and pain catastrophization will, on average, fail to reach the absolute level of function reported by patients without those comorbid characteristics.
There are several strengths to our study. First, the large sample that was analyzed provided greater-than-appropriate power to test our hypothesis. Bias resulting from missing data was minimized by our high retention rate (92%) and complete data collection from the final cohort. Additionally, the inclusion of multiple diagnoses and treatments should allow broad applicability of our results across atraumatic hand conditions that present to an orthopaedic hand surgeon’s office.
Not surprisingly, patients’ self-reported history of depression did not perfectly coincide with CES-D scores categorizing patients as affected. The CES-D questionnaire states explicitly in its instructions to answer its questions on the basis of the last seven days. This means that temporal life events, such as an acute illness, or in the case of our cohort, hand pain, may impact patient responses such that the score may not correlate with clinically diagnosed depression. This highlights the limitations that are inherent in research that attempts to study the effect of depression via a questionnaire approach.
An additional limitation is that we defined all events—patient status, diagnosis, and treatment—on the basis of patient responses and care provided at or after the first office visit. We did not take into account a change in patient status, a new diagnosis, or additional treatment for either the original concern or a new problem. In doing so, we approached our analysis with a method akin to intention-to-treat. There was also no placebo group, and consequently, it is not possible to know if the improvement shown by both groups was due to treatment, the natural course of clinical presentations, placebo effect, or other unmeasured factors. Additionally, with three months of data collection, a response after treatment is observed; however, longer follow-up may have led to further differentiation between groups based on long-term impairment or recurrence rates. We also did not collect any objective data on patient function; instead, we relied on patient-rated outcomes, for which it is unclear what effect scaling may have had. Finally, we cannot be certain what effect, if any, the complexity of a presenting problem, the nature of previous treatment experiences, or the tertiary setting of our institution had on our findings.
It has been hypothesized that assessing patient depression and pain catastrophization, and treating it, may lead to improved surgical outcomes, limit unnecessary interventions, reduce pain, and increase quality of life5,11,65,66. Prior studies have demonstrated that treatment of depression and pain catastrophization with cognitive behavioral therapy has led to improved psychological outcomes and a reduction in pain scores for patients with chronic back pain, fibromyalgia, temporomandibular pain, and other chronic pain complaints67-75. Additional studies are warranted to determine if psychological treatment can result in even greater improvement in patient-rated hand function for affected patients.
Supplementary Material
Disclosure of Potential Conflicts of Interest
Footnotes
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Centers for Disease Control and Prevention (CDC). Current depression among adults—United States, 2006 and 2008. MMWR Morb Mortal Wkly Rep. 2010 Oct 1;59(38):1229-35 [PubMed] [Google Scholar]
- 2.Pratt LA, Brody DJ. Depression in the United States household population, 2005-2006. NCHS Data Brief. 2008 Sep;(7):1-8 [PubMed] [Google Scholar]
- 3.Karels CH, Bierma-Zeinstra SM, Burdorf A, Verhagen AP, Nauta AP, Koes BW. Social and psychological factors influenced the course of arm, neck and shoulder complaints. J Clin Epidemiol. 2007 Aug;60(8):839-48 Epub 2007 Mar 26 [DOI] [PubMed] [Google Scholar]
- 4.Linton SJ, Nicholas MK, MacDonald S, Boersma K, Bergbom S, Maher C, Refshauge K. The role of depression and catastrophizing in musculoskeletal pain. Eur J Pain. 2011 Apr;15(4):416-22 Epub 2010 Sep 29 [DOI] [PubMed] [Google Scholar]
- 5.Vranceanu AM, Barsky A, Ring D. Psychosocial aspects of disabling musculoskeletal pain. J Bone Joint Surg Am. 2009 Aug;91(8):2014-8 [DOI] [PubMed] [Google Scholar]
- 6.Wegener ST, Castillo RC, Haythornthwaite J, Mackenzie EJ, Bosse MJ; LEAP Study Group. Psychological distress mediates the effect of pain on function. Pain. 2011 Jun;152(6):1349-57 Epub 2011 Mar 10 [DOI] [PubMed] [Google Scholar]
- 7.Crichlow RJ, Andres PL, Morrison SM, Haley SM, Vrahas MS. Depression in orthopaedic trauma patients. Prevalence and severity. J Bone Joint Surg Am. 2006 Sep;88(9):1927-33 [DOI] [PubMed] [Google Scholar]
- 8.Husain N, Humail SM, Chaudhry IB, Rahman R, Robinson H, Creed F. Psychological distress among patients of an orthopaedic outpatient clinic: a study from a low-income country. Ann Gen Psychiatry. 2010 Feb 15;9:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosemann T, Laux G, Szecsenyi J. Osteoarthritis: quality of life, comorbidities, medication and health service utilization assessed in a large sample of primary care patients. J Orthop Surg Res. 2007 Jun 30;2:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCarthy ML, MacKenzie EJ, Edwin D, Bosse MJ, Castillo RC, Starr A; LEAP study group. Psychological distress associated with severe lower-limb injury. J Bone Joint Surg Am. 2003 Sep;85-A(9):1689-97 [DOI] [PubMed] [Google Scholar]
- 11.Vranceanu AM, Ring D. Value of psychological evaluation of the hand surgical patient. J Hand Surg Am. 2008 Jul-Aug;33(6):985-7 [DOI] [PubMed] [Google Scholar]
- 12.Dersh J, Mayer T, Theodore BR, Polatin P, Gatchel RJ. Do psychiatric disorders first appear preinjury or postinjury in chronic disabling occupational spinal disorders? Spine (Phila Pa 1976). 2007 Apr 20;32(9):1045-51 [DOI] [PubMed] [Google Scholar]
- 13.Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995 Dec;7(4):524-32 [Google Scholar]
- 14.Sullivan MJL, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001 Mar;17(1):52-64 [DOI] [PubMed] [Google Scholar]
- 15.Chaves JF, Brown JM. Spontaneous cognitive strategies for the control of clinical pain and stress. J Behav Med. 1987 Jun;10(3):263-76 [DOI] [PubMed] [Google Scholar]
- 16.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983 Sep;17(1):33-44 [DOI] [PubMed] [Google Scholar]
- 17.Spanos NP, Radtke-Bodorik HL, Ferguson JD, Jones B. The effects of hypnotic susceptibility, suggestions for analgesia, and the utilization of cognitive strategies on the reduction of pain. J Abnorm Psychol. 1979 Jun;88(3):282-92 [DOI] [PubMed] [Google Scholar]
- 18.Forsythe ME, Dunbar MJ, Hennigar AW, Sullivan MJ, Gross M. Prospective relation between catastrophizing and residual pain following knee arthroplasty: two-year follow-up. Pain Res Manag. 2008 Jul-Aug;13(4):335-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pavlin DJ, Sullivan MJ, Freund PR, Roesen K. Catastrophizing: a risk factor for postsurgical pain. Clin J Pain. 2005 Jan-Feb;21(1):83-90 [DOI] [PubMed] [Google Scholar]
- 20.Börsbo B, Peolsson M, Gerdle B. Catastrophizing, depression, and pain: correlation with and influence on quality of life and health - a study of chronic whiplash-associated disorders. J Rehabil Med. 2008 Jul;40(7):562-9 [DOI] [PubMed] [Google Scholar]
- 21.Edwards RR, Bingham CO, 3rd, Bathon J, Haythornthwaite JA. Catastrophizing and pain in arthritis, fibromyalgia, and other rheumatic diseases. Arthritis Rheum. 2006 Apr 15;55(2):325-32 [DOI] [PubMed] [Google Scholar]
- 22.Edwards RR, Smith MT, Kudel I, Haythornthwaite J. Pain-related catastrophizing as a risk factor for suicidal ideation in chronic pain. Pain. 2006 Dec 15;126(1-3):272-9 Epub 2006 Aug 22 [DOI] [PubMed] [Google Scholar]
- 23.Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007 Feb;30(1):77-94 Epub 2006 Dec 20 [DOI] [PubMed] [Google Scholar]
- 24.Drahovzal DN, Stewart SH, Sullivan MJ. Tendency to catastrophize somatic sensations: pain catastrophizing and anxiety sensitivity in predicting headache. Cogn Behav Ther. 2006;35(4):226-35 [DOI] [PubMed] [Google Scholar]
- 25.Ring D, Kadzielski J, Fabian L, Zurakowski D, Malhotra LR, Jupiter JB. Self-reported upper extremity health status correlates with depression. J Bone Joint Surg Am. 2006 Sep;88(9):1983-8 [DOI] [PubMed] [Google Scholar]
- 26.Severeijns R, Vlaeyen JW, van den Hout MA, Picavet HS. Pain catastrophizing and consequences of musculoskeletal pain: a prospective study in the Dutch community. J Pain. 2005 Feb;6(2):125-32 [DOI] [PubMed] [Google Scholar]
- 27.Severeijns R, Vlaeyen JW, van den Hout MA, Picavet HS. Pain catastrophizing is associated with health indices in musculoskeletal pain: a cross-sectional study in the Dutch community. Health Psychol. 2004 Jan;23(1):49-57 [DOI] [PubMed] [Google Scholar]
- 28.Vranceanu AM, Jupiter JB, Mudgal CS, Ring D. Predictors of pain intensity and disability after minor hand surgery. J Hand Surg Am. 2010 Jun;35(6):956-60 Epub 2010 Apr 9 [DOI] [PubMed] [Google Scholar]
- 29.Das De S, Vranceanu AM, Ring DC. Contribution of kinesophobia and catastrophic thinking to upper-extremity-specific disability. J Bone Joint Surg Am. 2013 Jan 2;95(1):76-81 [DOI] [PubMed] [Google Scholar]
- 30.Lozano Calderón SA, Paiva A, Ring D. Patient satisfaction after open carpal tunnel release correlates with depression. J Hand Surg Am. 2008 Mar;33(3):303-7 [DOI] [PubMed] [Google Scholar]
- 31.Lozano-Calderon SA, Souer JS, Jupiter JB, Ring D. Psychological differences between patients that elect operative or nonoperative treatment for trapeziometacarpal joint arthrosis. Hand (N Y). 2008 Sep;3(3):271-5 Epub 2008 Mar 29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nunez F, Vranceanu AM, Ring D. Determinants of pain in patients with carpal tunnel syndrome. Clin Orthop Relat Res. 2010 Dec;468(12):3328-32 Epub 2010 Sep 1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ensel WM. Measuring depression: The CES-D scale. In: Lin N, Dean A, Ensel WM, editors. Social support, life events, and depression. New York: Academic Press; 1986 [Google Scholar]
- 34.Zich JM, Attkisson CC, Greenfield TK. Screening for depression in primary care clinics: the CES-D and the BDI. Int J Psychiatry Med. 1990;20(3):259-77 [DOI] [PubMed] [Google Scholar]
- 35.Radloff LS. The CES-D scale. Appl Psychol Meas. 1977 Jun;1(3):385-401 [Google Scholar]
- 36.Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977 Sep;106(3):203-14 [DOI] [PubMed] [Google Scholar]
- 37.Sullivan JA. The Pain Catastrophizing Scale - User Manual. 5 ed. Montreal: McGill University; 2009. p. 36 [Google Scholar]
- 38.Ring D, Kadzielski J, Malhotra L, Lee SG, Jupiter JB. Psychological factors associated with idiopathic arm pain. J Bone Joint Surg Am. 2005 Feb;87(2):374-80 [DOI] [PubMed] [Google Scholar]
- 39.Vranceanu AM, Safren S, Zhao MJ, Cowan J, Ring D. Disability and psychologic distress in patients with nonspecific and specific arm pain. Clin Orthop Relat Res. 2008 Nov;466(11):2820-6 Epub 2008 Jul 18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chung KC, Hamill JB, Walters MR, Hayward RA. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg. 1999 Jun;42(6):619-22 [DOI] [PubMed] [Google Scholar]
- 41.Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg Am. 1998 Jul;23(4):575-87 [DOI] [PubMed] [Google Scholar]
- 42.McMillan CR, Binhammer PA. Which outcome measure is the best? Evaluating responsiveness of the Disabilities of the Arm, Shoulder, and Hand Questionnaire, the Michigan Hand Questionnaire and the Patient-Specific Functional Scale following hand and wrist surgery. Hand (N Y). 2009 Sep;4(3):311-8 Epub 2009 Mar 4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Horng YS, Lin MC, Feng CT, Huang CH, Wu HC, Wang JD. Responsiveness of the Michigan Hand Outcomes Questionnaire and the Disabilities of the Arm, Shoulder, and Hand questionnaire in patients with hand injury. J Hand Surg Am. 2010 Mar;35(3):430-6 Epub 2010 Feb 6 [DOI] [PubMed] [Google Scholar]
- 44.Kotsis SV, Chung KC. Responsiveness of the Michigan Hand Outcomes Questionnaire and the Disabilities of the Arm, Shoulder and Hand questionnaire in carpal tunnel surgery. J Hand Surg Am. 2005 Jan;30(1):81-6 [DOI] [PubMed] [Google Scholar]
- 45.Dias JJ, Rajan RA, Thompson JR. Which questionnaire is best? The reliability, validity and ease of use of the Patient Evaluation Measure, the Disabilities of the Arm, Shoulder and Hand and the Michigan Hand Outcome Measure. J Hand Surg Eur Vol. 2008 Feb;33(1):9-17 [DOI] [PubMed] [Google Scholar]
- 46.Kotsis SV, Lau FH, Chung KC. Responsiveness of the Michigan Hand Outcomes Questionnaire and physical measurements in outcome studies of distal radius fracture treatment. J Hand Surg Am. 2007 Jan;32(1):84-90 [DOI] [PubMed] [Google Scholar]
- 47. Malay S; SUN Study Group, Chung KC. The minimal clinically important difference after simple decompression for ulnar neuropathy at the elbow. J Hand Surg Am. 2013 Apr;38(4):652-9. Epub 2013 Mar 6. [DOI] [PMC free article] [PubMed]
- 48.Shauver MJ, Chung KC. The minimal clinically important difference of the Michigan hand outcomes questionnaire. J Hand Surg Am. 2009 Mar;34(3):509-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.University of Michigan Department of Surgery. MHQ - scoring. 2006. http://sitemaker.umich.edu/mhq/scoring. Accessed 2013 Jan 9
- 50.Badalamente M, Coffelt L, Elfar J, Gaston G, Hammert W, Huang J, Lattanza L, Macdermid J, Merrell G, Netscher D, Panthaki Z, Rafijah G, Trczinski D, Graham B; American Society for Surgery of the Hand Clinical Trials and Outcomes Committee. Measurement scales in clinical research of the upper extremity, part 2: outcome measures in studies of the hand/wrist and shoulder/elbow. J Hand Surg Am. 2013 Feb;38(2):407-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Obeid JS, McGraw CA, Minor BL, Conde JG, Pawluk R, Lin M, Wang J, Banks SR, Hemphill SA, Taylor R, Harris PA. Procurement of shared data instruments for Research Electronic Data Capture (REDCap). J Biomed Inform. 2013 Apr;46(2):259-65 Epub 2012 Nov 10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377-81 Epub 2008 Sep 30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Woodward M. Epidemiology: study design and data analysis. 1 ed. Boca Raton, FL: Chapman and Hall/CRC Press; 1999 [Google Scholar]
- 54.Jensen MP, Gammaitoni AR, Olaleye DO, Oleka N, Nalamachu SR, Galer BS. The pain quality assessment scale: assessment of pain quality in carpal tunnel syndrome. J Pain. 2006 Nov;7(11):823-32 [DOI] [PubMed] [Google Scholar]
- 55.Boyd JH, Weissman MM, Thompson WD, Myers JK. Screening for depression in a community sample. Understanding the discrepancies between depression symptom and diagnostic scales. Arch Gen Psychiatry. 1982 Oct;39(10):1195-200 [DOI] [PubMed] [Google Scholar]
- 56.Craig TJ, Van Natta PA. Current medication use and symptoms of depression in a general population. Am J Psychiatry. 1978 Sep;135(9):1036-9 [DOI] [PubMed] [Google Scholar]
- 57.Craig TJ, Van Natta PA. Influence of demographic characteristics on two measures of depressive symptoms: the relation of prevalence and persistence of symptoms with sex, age, education, and marital status. Arch Gen Psychiatry. 1979 Feb;36(2):149-54 [DOI] [PubMed] [Google Scholar]
- 58.Zou KH, Tuncali K, Silverman SG. Correlation and simple linear regression. Radiology. 2003 Jun;227(3):617-22 [DOI] [PubMed] [Google Scholar]
- 59.Brander V, Gondek S, Martin E, Stulberg SD. Pain and depression influence outcome 5 years after knee replacement surgery. Clin Orthop Relat Res. 2007 Nov;464:21-6 [DOI] [PubMed] [Google Scholar]
- 60.Domenech J, Sanchis-Alfonso V, López L, Espejo B. Influence of kinesiophobia and catastrophizing on pain and disability in anterior knee pain patients. Knee Surg Sports Traumatol Arthrosc. 2013 Jul;21(7):1562-8 Epub 2012 Oct 19 [DOI] [PubMed] [Google Scholar]
- 61.Faller H, Kirschner S, König A. Psychological distress predicts functional outcomes at three and twelve months after total knee arthroplasty. Gen Hosp Psychiatry. 2003 Sep-Oct;25(5):372-3 [DOI] [PubMed] [Google Scholar]
- 62.Fisher DA, Dierckman B, Watts MR, Davis K. Looks good but feels bad: factors that contribute to poor results after total knee arthroplasty. J Arthroplasty. 2007 Sep;22(6)(Suppl 2):39-42 Epub 2007 Jul 26 [DOI] [PubMed] [Google Scholar]
- 63.Fortin PR, Clarke AE, Joseph L, Liang MH, Tanzer M, Ferland D, Phillips C, Partridge AJ, Bélisle P, Fossel AH, Mahomed N, Sledge CB, Katz JN. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999 Aug;42(8):1722-8 [DOI] [PubMed] [Google Scholar]
- 64.Sullivan M, Tanzer M, Stanish W, Fallaha M, Keefe FJ, Simmonds M, Dunbar M. Psychological determinants of problematic outcomes following Total Knee Arthroplasty. Pain. 2009 May;143(1-2):123-9 Epub 2009 Mar 21 [DOI] [PubMed] [Google Scholar]
- 65.Asenlöf P, Denison E, Lindberg P. Individually tailored treatment targeting activity, motor behavior, and cognition reduces pain-related disability: a randomized controlled trial in patients with musculoskeletal pain. J Pain. 2005 Sep;6(9):588-603 [DOI] [PubMed] [Google Scholar]
- 66.Ring D. The role of science and psychology in optimizing care of hand illness. J Hand Ther. 2011 Apr-Jun;24(2):82-3 Epub 2011 Feb 9 [DOI] [PubMed] [Google Scholar]
- 67.Buhrman M, Nilsson-Ihrfeldt E, Jannert M, Ström L, Andersson G. Guided internet-based cognitive behavioural treatment for chronic back pain reduces pain catastrophizing: a randomized controlled trial. J Rehabil Med. 2011 May;43(6):500-5 [DOI] [PubMed] [Google Scholar]
- 68.Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. 2006 Jan;26(1):17-31 Epub 2005 Sep 30 [DOI] [PubMed] [Google Scholar]
- 69.Edwards RR, Cahalan C, Mensing G, Smith M, Haythornthwaite JA. Pain, catastrophizing, and depression in the rheumatic diseases. Nat Rev Rheumatol. 2011 Apr;7(4):216-24 Epub 2011 Feb 1 [DOI] [PubMed] [Google Scholar]
- 70.García-Campayo J, Serrano-Blanco A, Rodero B, Magallón R, Alda M, Andrés E, Luciano JV, del Hoyo YL. Effectiveness of the psychological and pharmacological treatment of catastrophization in patients with fibromyalgia: a randomized controlled trial. Trials. 2009 Apr 23;10:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gatchel RJ, Rollings KH. Evidence-informed management of chronic low back pain with cognitive behavioral therapy. Spine J. 2008 Jan-Feb;8(1):40-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain. 1999 Mar;80(1-2):1-13 [DOI] [PubMed] [Google Scholar]
- 73.Smeets RJ, Vlaeyen JW, Kester AD, Knottnerus JA. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. J Pain. 2006 Apr;7(4):261-71 [DOI] [PubMed] [Google Scholar]
- 74.Turner JA, Holtzman S, Mancl L. Mediators, moderators, and predictors of therapeutic change in cognitive-behavioral therapy for chronic pain. Pain. 2007 Feb;127(3):276-86 Epub 2006 Oct 27 [DOI] [PubMed] [Google Scholar]
- 75.Turner JA, Mancl L, Aaron LA. Short- and long-term efficacy of brief cognitive-behavioral therapy for patients with chronic temporomandibular disorder pain: a randomized, controlled trial. Pain. 2006 Apr;121(3):181-94 Epub 2006 Feb 21 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure of Potential Conflicts of Interest


