Abstract
A constellation of related genetic diseases are caused by defects in the telomere maintenance machinery. These disorders, often referred to as telomeropathies, share symptoms and molecular mechanisms, and mounting evidence indicates they are points along a spectrum of disease. Several new causes of these disorders have been recently discovered, and a number of related syndromes may be unrecognized telomeropathies. Progress in the clinical understanding of telomeropathies has in turn driven progress in the basic science of telomere biology. In addition, the pattern of genetic anticipation in some telomeropathies generates thought-provoking questions about the way telomere length impacts the course of these diseases.
Introduction
Human telomeres are composed of thousands of hexameric TTAGGG nucleotide repeats and the protein components that bind to and associate with them, including the shelterin complex (de Lange, 2010). These proteins recruit DNA repair factors to the telomeres and modify them so they mask rather than stimulate DNA repair. Thus, shelterin proteins protect telomeres from being recognized as DNA double-strand breaks. In the absence of such protection, catastrophic chromosome fusions occur (Sfeir and de Lange, 2012). Because of the “end replication” lagging strand synthesis problem and certain less-well defined end replication–processing events, telomeres shorten by 50–100 base pairs per cell division in vitro (Levy et al., 1992; Wu et al., 2012) and ∼20–30 base pairs per year in peripheral blood mononuclear cells during adulthood, which is modifiable by environmental factors (Daniali et al., 2013). This progressive shortening eventually interferes with the telomeres’ ability to suppress the DNA damage recognition machinery, triggering telomere-induced foci (TIFs) that lead to a p53/p21-mediated cell growth arrest called replicative senescence (Chin et al., 1999; Takai et al., 2003). Proliferating germline and certain adult somatic transit-amplifying stem-like cells express telomerase, a ribonucleoprotein reverse transcription; in general this telomerase activity only slows down the rate of progressive telomere shortening. The catalytic component of telomerase, TERT (telomerase reverse transcriptase), utilizes the telomerase RNA component (TERC) as a template to add new telomere repeats to the ends of existing telomeres in order to maintain telomere integrity (Wright et al., 1996). Telomere maintenance requires TERT, TERC, and a number of other gene products required for telomerase assembly and recruitment, as well as gene products necessary for the correct protection of the telomeres and processing before telomerase activity (Fig. 1; Palm and de Lange, 2008). Defects in these genes cause a spectrum of disorders leading to proliferative failure of a variety of tissues (Dokal, 2011).
Figure 1.
Molecular biology of telomeropathies. The processes required to correctly replicate and extend telomeres are outlined; genes with known disease-causing mutations are denoted in red. Telomeres are packaged in a “T-loop” configuration characterized by G-strand invasion of the centromere-proximal double-stranded DNA. The T-loop must be dissociated before replication of the telomere can take place, which is accomplished by the RTEL1 helicase. DNA replication after T-loop resolution yields blunt-ended (from leading-strand synthesis) and RNA primer–ended (from lagging strand synthesis) telomere ends, which must be processed by the CST complex (composed of CTC1, STN1, and TEN1) and Apollo before telomerase activity. Telomerase is a complex containing TERT, TERC, and a dimer of the Dyskerin complex (Dyskerin, NOP10, NHP2, GAR1), and its assembly is promoted by TCAB1 in the Cajal body. After assembly, telomerase is localized to the replicated and processed telomere by TCAB1 and TPP1, where it can add 50–100 base pairs of new telomere repeats to the G-overhang. After telomerase activity, the CST complex and DNA polymerase-α perform a fill-in reaction and nucleolytic processing that yields an extended telomere closed to further action by telomerase.
New syndromes characterized by impaired telomere maintenance, referred to as “telomeropathies,” “telomere disorders,” or “telomere syndromes” are increasingly being identified. Telomere length measurement or telomere dysfunction (measured by colocalization of shelterin components and DNA damage signals) are often used to identify a disorder of telomere maintenance in the laboratory (Touzot et al., 2010; Anderson et al., 2012; Ballew et al., 2013), whereas in the clinic telomeres are measured generally by flow cytometry or fluorescent in situ hybridization (FISH). This review focuses on the causes and symptoms of these syndromes with an emphasis on mutations recently linked to disorders of telomere biology. We also present a number of diseases not previously considered telomeropathies that have recently been shown to be related to telomere biology. Lastly, we discuss several models that may explain the heterogeneity of tissue failure in these disorders.
Telomerase, telomeres, and telomere maintenance
The telomerase holoenzyme adds new TTAGGG repeats via reverse transcription to the G-rich single-strand telomere overhang during DNA replication (Nakamura et al., 1997). In addition to the catalytic protein component (TERT) and the RNA component that provides the template (TERC) for telomere repeat addition, the telomerase holoenzyme complex contains a number of accessory proteins including dyskerin, NHP2, NOP10, and GAR1 (Egan and Collins, 2010). Assembly of telomerase requires recruitment to the Cajal body by the protein TCAB1 (Stern et al., 2012). It remains unclear how the complex is assembled in the Cajal body when all components are present, but several chaperone proteins, including HSP70, p23, and HSP90 are required for telomerase activity, and dyskerin can bind to the H/ACA box of TERC (Forsythe et al., 2001; Trahan and Dragon, 2009). Recent reports have shown that Coilin, a Cajal body protein with RNase activity, processes the 3′ end of TERC, and that this is required for proper telomerase assembly (Stern et al., 2012; Broome and Hebert, 2013). Mutations in TERT and TERC (Vulliamy et al., 2001, 2002; Armanios et al., 2005, 2007; Yamaguchi et al., 2005; Tsakiri et al., 2007; Calado et al., 2009a,b), Dyskerin (Heiss et al., 1998), NOP10 (Walne et al., 2007), NHP2 (Vulliamy et al., 2008), and TCAB1 (Zhong et al., 2011) have been detected in families with telomeropathies.
The shelterin complex is composed of six core proteins: telomere repeat–binding factor 1 and 2 (TRF1 and TRF2), TRF1-interacting nuclear protein 2 (TIN2), repressor/activator protein 1 (Rap1), TIN2-interacting protein 1 (TPP1), and protection of telomeres 1 (POT1; Palm and de Lange, 2008). TRF1 and TRF2 bind double-stranded telomeric DNA and nucleate the assembly of the shelterin complex via the TRF homology domains present on both factors, which bind to F/YxLxP motifs present on TIN2 and Rap1 (Chen et al., 2008). Homodimers of TRF1 and TRF2 can bind telomeres independently without being part of the full six-member complex (Lin et al., 2014). TIN2 recruits TPP1 (Houghtaling et al., 2004), and TPP1 in turn recruits POT1 to the complex (Xin et al., 2007). Assembly of a functional shelterin complex is absolutely critical for genome stability, and disruption of any shelterin component can lead to disastrous consequences for the cell (Sfeir and de Lange, 2012). Because mutations in shelterin components often result in embryonic or perinatal lethality in mice (Tejera et al., 2010; Beier et al., 2012), it is not surprising that only mutations in TIN2 of the shelterin complex have been identified in humans. Because of their extremely vital core functions, pathological mutations in shelterin components would be subject to strong negative selection, leading to their rapid loss from the population. Indeed, TIN2 mutants often present with especially severe, early-onset forms of telomeropathies (Hoyeraal-Hreidersson syndrome [HHS] and Revesz syndrome; Savage et al., 2008; Sasa et al., 2012; Vulliamy et al., 2012).
Part of the mechanism by which telomere ends are hidden from the DNA repair machinery is via a structure known as a T-loop (Doksani et al., 2013), in which intramolecular invasion of the telomeric duplex DNA by the telomeric single-stranded G-overhang creates a structure reminiscent of a Holliday recombination intermediate. This has no free 3′ end, and thus does not resemble a double-strand break (Fig. 1; Griffith et al., 1999). The T-loop must be dissociated during DNA replication, which is accomplished by RTEL1 or other helicases. In the absence of RTEL1, the T-loop is excised by the SLX4 nuclease, which causes rapid telomere loss (Vannier et al., 2012). Recent reports have identified RTEL1 mutations in HHS (Ballew et al., 2013; Le Guen et al., 2013; Walne et al., 2013b).
Apollo is a PSO2/SNM1 family interstrand cross-link repair nuclease that is recruited to the telomere by TRF2 (Chen et al., 2008). Depletion of Apollo, removal of its nuclease activity, or abrogation of its interaction with TRF2 results in loss of the 3′ telomeric G-overhang. This leads to deprotection of the telomere in mice and ATM-mediated telomere fusions. This suggests that Apollo is required to resect the blunt ends of the leading-strand telomere replication product after replication (Wu et al., 2012). A dominant-negative alternative splice form of Apollo has been identified in a patient with HHS (Touzot et al., 2010). Although this splice form was not derived from a mutation in the Apollo gene itself, introduction of the aberrant form into fibroblasts induces telomere fusions, suggesting that the Apollo splice variant may have been responsible for the patient’s symptoms.
Telomeres are difficult to replicate because they are repetitive and prone to forming secondary structures such as G-quadruplexes (Tang et al., 2008). This can lead to fork stalling during replication. The CST complex, which is composed of CTC1, STN1, and TEN1, is involved in restarting stalled replication forks during telomeric DNA replication, as well as promoting telomere C-strand fill-in after telomerase activity during DNA replication (Stewart et al., 2012; Wang et al., 2012). Mice deficient in CTC1 show rapid C-strand loss, leading to bone marrow failure (Gu et al., 2012). Mutations in CTC1 have been identified in Coats Plus syndrome (Anderson et al., 2012; Keller et al., 2012; Polvi et al., 2012; Walne et al., 2013a).
Telomere disorders
Defects in genes involved in telomere maintenance result in a large overlapping spectrum of symptoms (Kirwan and Dokal, 2008). The “diagnostic triad” of oral leukoplakia, skin hyperpigmentation, and nail dystrophy were originally used to identify families with dyskeratosis congenita (DKC; Heiss et al., 1998). Recently, an increasing number of reports have identified syndromes that do not include the diagnostic triad but are still caused by mutations in core telomere maintenance proteins (Tsangaris et al., 2008).
The symptoms of these disorders are extensive and the age of onset is highly variable; however, the disorders share similar underlying molecular mechanisms and have overlapping, incompletely penetrant phenotypes (Armanios et al., 2007). Individuals within the same family with the same mutation can present with different phenotypes (Walne et al., 2013b), and the severe telomeropathies, such as Revesz syndrome and Coats Plus syndrome, are extremely rare. Mutations in the same regions of the same genes can cause different disorders (Carroll and Ly, 2009), but impaired telomere maintenance appears to be present for all of the disorders. See Box 1 for a discussion of the changing understanding of these diseases.
Box 1.Telomeropathies are a spectrum disorder
The complexity of telomeropathies poses obvious challenges for their classification. The currently used nomenclature has several weaknesses, such as the use of symptoms that are not fully penetrant, like the classic triad, to classify patients. For example, within a cohort of TIN2 mutants from different families with mutation in the same residue of TIN2 (Arg282), the classic triad does not always appear, and classification of these patients ranges from aplastic anemia to Hoyeraal-Hreidarsson syndrome; as a whole, only 35% of TIN2 mutants showed the classic triad (Walne et al., 2008). Atypical timing or absence of the appearance of the classic triad despite impaired telomere maintenance is also apparent from careful analysis of the literature (Vulliamy et al., 2002; Yamaguchi et al., 2005; Savage et al., 2008; Sasa et al., 2012). Overall, it seems that the use of these symptoms to classify patients into different groups is flawed.
The picture becomes even more complicated for severe telomeropathies. Hoyeraal-Hreidarsson syndrome, Revesz syndrome, and Coats Plus are rare enough that virtually all reports can be considered anecdotes, and the symptoms used to distinguish between them (exudative retinopathy for Revesz syndrome and cerebral calcifications for Coats Plus) have been documented within patients diagnosed with all three disorders (Scheinfeld et al., 2007; Ramasubramanian and Shields, 2012). Further, because reports of the severe forms are distributed globally and investigation methods vary, certain symptoms, such as cerebral calcifications (determined via MRI), may not be observed even if they are present, leading to misclassification of patients.
Many groups have noted that the telomeropathies resemble a spectrum disorder much more than distinct diseases (Carroll and Ly, 2009; Diaz de Leon et al., 2010; Armanios and Blackburn, 2012); however, the current nomenclature does not reflect this property of telomeropathies. We would like to suggest the use of the term “impaired telomere maintenance spectrum disorder” (ITM), which highlights the underlying molecular cause of the syndromes without making inferences based on incompletely penetrant symptoms.
Consequences of impaired telomere maintenance.
In adulthood, idiopathic pulmonary fibrosis (IPF) is the most common symptom of a telomeropathy (Armanios and Blackburn, 2012). IPF is characterized by progressive failure of the lung coincident with fibrosis and inflammation (Armanios et al., 2007). Inherited mutations in TERC and TERT explain ∼8–20% of familial cases of IPF, as well as a small proportion of sporadic IPF cases (Tsakiri et al., 2007). 37% of familial cases and 25% of sporadic cases are associated with telomere lengths lower than the 10th percentile of the general population, suggesting that there is a significant number of IPF cases associated with impaired telomere maintenance with as-yet undiscovered genetic or environmental causes (Cronkhite et al., 2008). Familial IPF cases show autosomal-dominant inheritance consistent with haploinsufficiency of telomerase, with IPF appearing in mutation carriers in middle to old age, with median age of incidence at 51 years (Parry et al., 2011).
Other adult-onset manifestations of impaired telomere maintenance include familial liver cirrhosis (Calado et al., 2009b), aplastic anemia in adulthood (Fogarty et al., 2003), and sporadic acute myelogenous leukemia (AML), in which both somatic and germline mutations have been found (Calado et al., 2009a). Some patients with mutations in TERT also present with liver cirrhosis and IPF concurrently (Carulli et al., 2012); additionally, IPF, aplastic anemia, and liver cirrhosis occur frequently in the same patient at different times (Parry et al., 2011), showing that telomere shortening occurs throughout the body even in patients that display failure of a single organ. Because the common underlying cause of these organ failures is impaired telomere maintenance, it may be appropriate to consider them a single clinical spectrum disorder.
Dyskeratosis congenita (DKC) was the first disorder linked to impaired telomere maintenance (Mitchell et al., 1999). Aside from the diagnostic triad, it is associated with a host of other symptoms that appear less frequently. Most prominently, individuals with DKC display organ failure, usually in the bone marrow (Dokal, 2011; Young, 2012) and present with aplastic anemia or specific lymphopenias. In these patients, pulmonary toxicity due to bone marrow transplant conditioning (ablation of the existing stem cell compartment) can induce pulmonary fibrosis, and a subset of individuals with DKC will encounter pulmonary fibrosis before bone marrow failure (Goldfarb et al., 2013). Less commonly, DKC involves failure of a variety of endothelial and epithelial compartments, including enterocolitis, emphysema, liver cirrhosis, premature hair graying, short stature, dental caries, osteoporosis, and esophageal stricture (Dokal, 2011). DKC overlaps significantly in pathology and genetic cause with HHS, Coats Plus syndrome, and Revesz syndrome.
Hoyeraal-Hreidersson syndrome (HHS) is an especially severe form of DKC, with the addition of intrauterine growth retardation, cerebellar hypoplasia, and microcephaly (Aalfs et al., 1995). HHS patients typically present with strikingly short telomeres and have a higher mortality rate (Walne et al., 2013b). Revesz syndrome is also exceptionally rare, and is characterized by symptoms of HHS with the addition of exudative retinopathy (Kajtár and Méhes, 1994). Coats Plus syndrome has recently been linked to mutations in the CTC1 gene (Anderson et al., 2012), and patients with CTC1 mutation-derived Coats Plus syndrome may exhibit symptoms of HHS and Revesz syndrome, with the addition of cerebral calcifications. Despite these distinctions, cerebral calcifications and exudative retinopathy have been observed in patients with all three severe forms of DKC (Scheinfeld et al., 2007; Ramasubramanian and Shields, 2012).
Depending on the mutation responsible for HHS, genotypically identical individuals in the same pedigree may show dramatically different symptoms to such a degree that full siblings of HHS patients with the same alleles may manifest only bone marrow failure or classical DKC symptoms, whereas their sibling suffers the entire course of HHS (Walne et al., 2013b). Presently, it is difficult to establish guidelines distinguishing the three disorders due to the incomplete penetrance of the symptoms and very small numbers of HHS, Coats Plus, and Revesz syndrome patients. Because of the overlapping symptoms and causes of these disorders, it is likely that they represent a single disease entity with multiple genetic mechanisms for the same pathological conditions, not three distinct disorders.
The only curative therapy for the life-threatening symptoms of telomeropathies at the present time is tissue or organ transplant; bone marrow transplant in the case of bone marrow failure or via lung transplant in IPF patients (Young, 2012; Isoda et al., 2013). However, many patients with bone marrow failure will show improvement when treated with androgen therapy, such as danazol or oxymetholone (Armanios, 2013). In the future, it may be possible to perform autologous stem cell transplantation after in vitro transient lengthening of telomeres, either through gene therapy or by as-yet undiscovered small-molecule telomerase activators.
Telomere length is heritable.
In normal individuals, the estimates of the heritability of telomere length vary widely, from 0.36 to 0.84 (Goldman et al., 2005; Diaz de Leon et al., 2010; Aviv, 2012). Estimating telomere length heritability is complicated by the increasing importance of the environment with increased age, which is difficult to normalize across multiple studies. However, there are well-established correlations between parental telomere length, paternal telomere length in particular, and offspring leukocyte telomere length (De Meyer et al., 2007; Eisenberg et al., 2012). The heritability of telomere length is important because families with telomeropathies can display genetic anticipation—a decrease in age of onset and increase in severity of symptoms—in later generations. The anticipation of symptoms correlates with telomere length in the individuals, with the most severely affected individuals displaying the shortest telomere lengths (Armanios, 2012). Even wild-type offspring of heterozygous TERT mutation carriers have telomeres shorter than the age-matched general population (Chiang et al., 2010), suggesting that the exceptionally short telomeres inherited cannot be fully extended during embryonic development.
Severity of telomeropathies may increase by generation.
Anticipation in telomeropathies not only reduces the age of onset of symptoms, but can lead to increased severity of symptoms. For example, older generations of many families with TERT or TERC mutations display adult-onset symptoms such as IPF and aplastic anemia, whereas younger generations display DKC symptoms (Armanios, 2012). The rate at which this anticipation occurs varies depending on the extent of impaired telomere maintenance, inheritance mode of the responsible mutation, initial telomere length in each individual, and poorly defined environmental factors (Armanios et al., 2005).
Though individuals with childhood-onset telomeropathies (such as DKC-like symptoms) rarely reproduce, there are indications that further anticipation is possible. For example, one individual who suffered bone marrow failure and underwent a hematopoietic stem cell transplant at age 13 had two children who inherited his mutation in TIN2; the oldest child displayed bone marrow failure and retinal vasculopathy at age 3, and both children were below the first percentile in telomere length for their age (Gleeson et al., 2012).
Telomere length can be affected by the environment.
An enormous variety of environmental exposures and disease states correlate with shorter lymphocyte telomere lengths (Zhang et al., 2013), which may partially explain the incompletely penetrant phenotypes of telomeropathies. For example, environmental air pollution (Grahame and Schlesinger, 2012), tobacco exposure (Theall et al., 2013), stress (Parks et al., 2009), asthma, and chronic obstructive pulmonary disease (COPD; Albrecht et al., 2014) have all been linked to shorter telomere lengths. In addition, environmental influences may explain why pulmonary fibrosis precedes bone marrow failure in some DKC patients. The “multiple hit” model, which has been proposed elsewhere (Alder et al., 2011; Armanios and Blackburn, 2012), suggests collaboration between a genetic predisposition to impaired telomere maintenance, inherited short telomeres, and environmental exposures that drive further telomere shortening, leading to IPF. This model and the heterogeneity in environmental exposures could explain the highly variable age of onset of IPF in cohorts with telomeropathies.
Environmental insult-driven accelerated telomere shortening may also explain why the diagnostic triad symptoms of DKC may appear at widely varying ages, both before and after bone marrow failure (Vulliamy et al., 2002; Yamaguchi et al., 2005; Savage et al., 2008; Tsangaris et al., 2008; Walne et al., 2008; Sasa et al., 2012), and in some cases fail to appear at all. Heterogeneity in environmental exposures could provoke tissue failure asynchronously, resulting in a unique order of symptom onset for each patient.
Secondary telomeropathies.
In addition to classically linked disorders of impaired telomere maintenance, a number of diseases not typically associated with telomere biology have been reported that include dysfunction at the telomeres. These include defects in DNA repair machinery that may interact with telomere components, such as FANCD2 and RECQL4, as well as mutations in genes with poorly characterized telomere function, such as MPN1 and DNMT3B. We refer to these as peripheral or secondary telomeropathies because it is unresolved if the reported telomere dysfunction in these contexts is the cause or just one of the effects of the diseases.
Recent observations have shown short telomeres and TIFs in primary lymphocytes obtained from Fanconi anemia (FA) patients with mutations in the FANCD2 gene (Joksic et al., 2012). In vitro studies have shown direct interactions between FANCD2, telomeric DNA, and tankyrase I (a known regulator of TRF1 binding; Smith et al., 1998), as well as down-regulation of TRF1 in FANCD2 mutant cells (Lyakhovich et al., 2011). Apollo has been shown to localize FANCD2 to the telomeres, suggesting that FANCD2 may be an Apollo mediator and that the HHS shown in the patients with the Apollo splice variant may have been partially FANCD2 mediated (Mason and Sekiguchi, 2011). It is unknown if the short telomere phenotype observed in these patients contributes to their disease state because of the overlap in symptoms of FA and telomeropathies, as well as the genome-wide perturbation in DNA repair, a feature of FA. However, only a subset of FA patients analyzed in Pavesi et al. (2009) showed abnormally short telomeres, and FA as a whole exhibits telomere length closer to that of nontelomere-mediated inherited bone marrow failure syndromes (Gadalla et al., 2010), suggesting that this impaired telomere maintenance is a feature of FANCD2-mediated FA, not FA in general.
Rothmund-Thomson syndrome (RT) is caused by mutations in the RECQL4 gene, and shares some symptoms with DKC, including poikiloderma (hyper- or hypo-pigmentation), hyperkeratotic lesions, dental abnormalities, and short stature (Wang and Plon, 1993). Cell lines derived from patients with RECQL4 mutations showed a marked increase in TIFs, as well as increased rates of telomere fusions and telomeric DNA breaks. RECQL4 also interacts with both TRF1 and TRF2, suggesting that RT syndrome may be one manifestation of impaired telomere maintenance (Ghosh et al., 2012).
MPN1 (also known as USB1 or C16orf57) mutations that segregate with the disease were identified in families with symptoms of DKC. No obvious problems with patient telomeres were detected, although the investigators did not examine TIF frequency (Shchepachev et al., 2012). Yeast studies examining the role of MPN1 have shown telomere shortening in yeast lines with MPN1 deletions, as well as an increase in telomeric RNA transcripts (TERRA). However, it remains unclear how MPN1 is involved in telomere biology because its known activities involve regulating the stability of the U6 snRNA by removing uridine tracts from the 3′ end (Shchepachev et al., 2012). MPN1 may have other targets, such as TERRA, which may explain the symptoms that indicate impaired telomere maintenance.
ICF (immunodeficiency, centromeric region instability, and facial anomalies syndrome type I) is a disorder caused by mutations in DNMT3B. Fibroblasts from ICF patients have short telomeres, as well as marked reductions in subtelomeric methylation (Yehezkel et al., 2013). Cultured fibroblasts from ICF patients exhibit premature senescence that can be circumvented via overexpression of telomerase, suggesting telomere length is limiting.
These examples illustrate that the telomere/telomerase regulatory network is very large and quite sensitive to exogenous perturbations. Because of this molecular complexity, it is likely that there is an extensive group of peripheral or secondary telomeropathies that act on telomeres in an indirect fashion; the mutations outlined above may be among the first of these recognized.
Unanswered questions about telomere disorders.
Though much is already known about the biology of telomeropathies, important unanswered questions remain. The mechanism through which successive generations in families with telomere disorders exhibit different symptoms is not yet determined. Though inherited short telomeres can explain the age of onset, they do not independently explain why earlier generations manifest adult-onset symptoms (IPF, liver cirrhosis, AML) whereas younger generations show DKC/HH symptoms (bone marrow failure, mucocutaneous abnormalities). Roughly half of the families with DKC still have no identifiable causative mutation, implying that undiscovered biology remains. Lastly, the well-established cancer predisposition in DKC families somewhat contradicts the conventional interpretation of telomere length as a limit on cellular proliferation.
Mechanisms for the generational differences in telomere disorder symptoms
Families with telomere disorders display both anticipation in age of onset as well as generational changes in which symptoms appear (Armanios, 2012). Because of limited information about telomere-shortening rates in the tissues affected by telomeropathies, it is uncertain if the disease threshold for telomere length is consistent from tissue to tissue. Nevertheless, some difference in telomere biology of the most relevant tissues (lung and bone marrow) may help explain the differences. Either the tissues must shorten at different rates or they must be differentially sensitive to shortened telomeres, though some mix of the two possibilities is entirely possible.
Telomere shortening is proposed to be synchronous in adulthood between lymphocytes, skin, muscle, and adipose tissue (Daniali et al., 2013), though data from primate models suggests that lung telomeres shorten considerably faster compared with skeletal muscle (Gardner et al., 2007). The observations are further complicated by differences in telomere measurement methods and an unknown extent of lymphocyte contamination of the nonlymphocyte samples via blood present in tissue during DNA extraction.
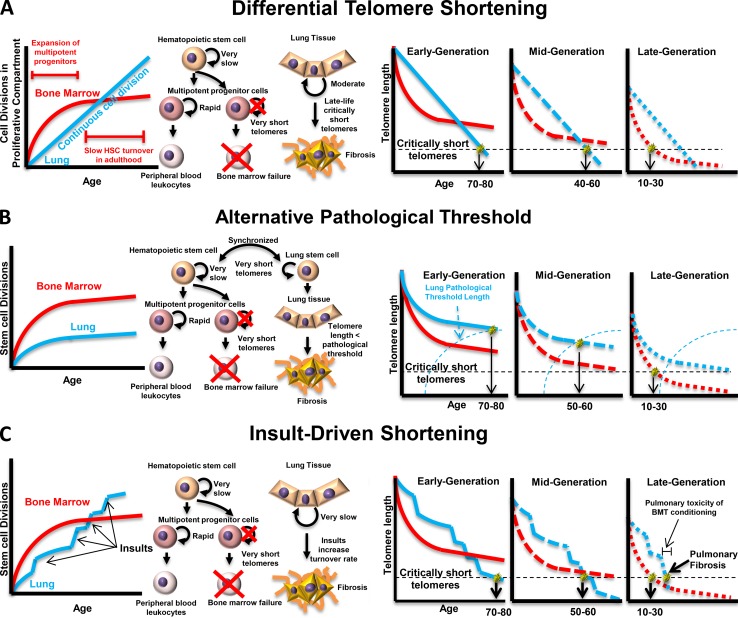
Here we put forward three models to explain the generational differences in symptoms of telomere disorders based on differing interpretations of the data about tissue telomere dynamics (Fig. 2). One model relies on differential telomere shortening based on the different developmental and maintenance systems of the two most important tissues (Fig. 2 A). Another assumes synchronous telomere shortening but infers some alternative pathological threshold that occurs before critically short telomeres (Fig. 2 B). The third model attempts to merge both possibilities by assuming synchronous telomere shortening punctuated by rapid telomere loss during insult-driven proliferation in specific tissues such as the lung (Fig. 2 C).
Figure 2.
Three models for the genetic anticipation observed in telomeropathies. Models that explain the anticipation observed in impaired telomere maintenance rely on different assumptions about the behavior of organ-specific stem cells. (A) If lung tissue stem cells have a constant cell division rate that is slower than hematopoietic stem cells during expansion of the multipotent progenitor (MPP) cell compartment but slower than the maintenance HSC division rate after the MPP pool is established, a point will exist in middle age when lung telomere lengths are shorter than MPP/HSC telomere lengths; if the patient started with an initial telomere length sufficient to avoid critically short telomeres until after this point, the patient will experience IPF, whereas patients with initial telomere lengths short enough that they encounter the critical length before that point will experience bone marrow failure. (B) If stem telomere attrition rates are synchronized after development, lung tissue must be subject to an alternative pathological threshold for telomere length that may be age dependent. In this case, patients with longer initial telomere lengths will never encounter critically short telomeres in their bone marrow, while their lung tissue will encounter the alternative threshold, leading to IPF. Patients with shorter initial telomere lengths will encounter critically short telomeres in their bone marrow before the critical threshold for the lungs, leading to bone marrow failure. (C) If telomere attrition rates are synchronous under normal conditions but lung tissue is differentially sensitive to environmental insults, an alternative pathological threshold is not necessary to explain the anticipation. Patients with longer initial telomeres will eventually be driven into IPF by environmental insults while never encountering the critically short telomere length in the HSC compartment, whereas patients with shorter initial telomere length will encounter the critical threshold before insult-driven lung failure. This model is further supported by observations of pulmonary fibrosis after pulmonary toxicity from bone marrow transplant conditioning.
Differential telomere shortening.
Lung tissue and hematopoietic stem cells (HSCs) have remarkably different developmental and regulatory environments, so it is reasonable to expect some differences in their telomere dynamics. Lymphocytes are the most-studied primary human tissue with regard to telomere length, and so the telomere dynamics of HSCs are much better understood compared with cells in the lung. During development and early childhood there is comparatively rapid cell division in HSCs and a corresponding rise in the number of multipotent progenitor (MPP) cells, which are partially committed progenitor cells with limited self-renewal capacity; the MPP cells expand asymmetrically to give rise to differentiated blood cells (Kondo, 2010). Once this pool of MPP cells is established, the more primitive HSCs slow to roughly one division per year in adulthood, with a corresponding drop in telomere shortening rate (Catlin et al., 2011). This is documented by the more rapid telomere shortening observed in lymphocytes in childhood, followed by a long plateau of gradual shortening in adulthood (Sidorov et al., 2009).
In contrast, lung tissue is replenished by a spatially constrained self-renewing stem cell population (Asselin-Labat and Filby, 2012). There is little data on turnover rate in human lung, but in mouse models turnover is roughly 2% per week (Alder et al., 2011). Though human lung telomere dynamics are not fully understood, telomeres in lung tissue shorten with age (Gardner et al., 2007). This suggests that if there is a telomerase-positive stem cell compartment, it does not have sufficient telomerase activity to maintain telomeres indefinitely.
The observation of faster telomere shortening in Macaque lung compared with muscle may be used along with the known HSC/bone marrow telomere dynamics to explain the generational differences in telomere disorder symptoms (Fig. 2 A). If telomere shortening is faster in childhood for HSCs compared with lung tissue, but faster in lung in adulthood owing to a reduction in shortening rate in HSCs, there will be a “crossing point” that occurs in middle age to late life when telomeres are shorter in the lung than they are in the HSCs. If initial telomere length is long enough that the shortest compartment encounters a critically short telomere length after this crossing point, the patient will exhibit IPF, whereas if the initial telomere length was short enough that this occurs before the crossing point, the patient will present with bone marrow failure.
Alternative pathological thresholding.
If lung and HSC telomeres shorten synchronously in adulthood, an age-dependent difference in response to short telomeres may explain the generational changes in telomeropathy symptoms. There are recent discoveries demonstrating that the telomere position effect (TPE), a change in gene expression in telomere-proximal genes driven by changes in telomere length, is more widespread in humans than previously believed (Wright and Shay, 1992; Baur et al., 2001; Lou et al., 2009; Stadler et al., 2013). TPE-driven changes in gene expression could be differentially harmful to different tissues, resulting in tissue-specific pathological thresholds for telomere length.
Differential sensitivity to short telomeres, which has been proposed elsewhere (Armanios, 2013), is one way to explain the generational differences in telomeropathy symptoms (Fig. 2 B). In earlier generations HSCs never become short enough to trigger bone marrow failure, whereas they may encounter the pathological threshold for lung tissue in middle age to late life. Younger generations would encounter critically short telomeres in their HSC compartment during the expansion of transient amplifying cells, leading to bone marrow failure.
Insult-driven shortening.
In contrast to lymphocytes, lung tissue likely exhibits substantial heterogeneity in environmental insult exposure due to the constrained environment of a solid organ. Because of this heterogeneity, spatially delimited sections of the lung will be under greater proliferative and oxidative stress compared with the organ as a whole. Measurements of lung telomere length may miss pockets of especially short telomeres, such that length of the shortest telomeres present in the lung is substantially overestimated.
This insult-driven shortening could explain the generational differences in telomere disorder symptoms (Fig. 2 C); in earlier generations, HSC telomeres never become critically short, but pockets of damaged cells in the lung are driven into critical telomere length ranges by environmental stresses, leading to local failure that would spread from these initial foci to adjoining areas as those cells divide in an attempt to repair the tissue.
Undiscovered telomeropathies
A substantial portion (∼40%) of DKC has no proven monogenic cause (Armanios and Blackburn, 2012). Based on the recent discoveries of very rare mutations (such as TIN2 mutations and a nonmutation-linked pathological alternative splice form of Apollo), the suite of genes required for adequate telomere maintenance has expanded. Thus, it is likely that the network of genes required for normal telomere maintenance is large. This is further supported by the fact that although telomere length is partially heritable, well-powered studies attempting to establish genetic linkage to telomere length have met with little success. These studies reveal small numbers of loci that have extremely modest effects on telomere length (on the order of 200 bases per allele for the strongest effects detected, such as variants in the TERT locus; Levy et al., 2010; Bojesen et al., 2013). This suggests that the vast majority of heritable variation in telomere length is accomplished by the integrated action of a very large number of mostly undiscovered weak single nucleotide polymorphisms in a large number of genes. Because of this diversity, next-generation sequencing-based approaches may have more success in identifying the causes of uncharacterized telomeropathies compared with the candidate gene approaches applied in the past.
However, many investigations of DKC-like disorders use a candidate gene approach to identify the responsible mutation, generally by sequencing the genes with mutations known to cause telomere disorders. This approach cannot identify genes that have not been shown to cause telomeropathies in the past but are likely to impair telomere maintenance when defective, and so to improve the success rate of such an approach we have included a list of all genes known to cause telomeropathies when defective, as well as a list of their primary interaction partners with the aim of expanding the list of viable candidate genes (Table 1).
Table 1.
Candidate genes and complexes in telomere disorders
| Genes that cause telomere disorders when defective | Process/complex | Diseases | Process/complex including genes that cause telomeropathies | Candidate genes |
| TIN2 | Shelterin, inhibits TRF1 PARsylation | DKC/HHS/Revesz syndrome | Shelterin | TRF1, TRF2, TIN2, RAP1, TPP1, POT1 |
| RTEL1 | T-loop dissociation, target of cytosolic iron–sulfur protein assembly (CIA) complex | DKC/HHS | CST complex | CTC1, STN1, TEN1 |
| CTC1 | CST complex | Coats Plus | Telomerase | TERT, TERC, Dyskerin, NHP2, NOP10, GAR1 |
| Apollo | Overhang processing | HHS | CIA complex | MMS19, MIP18, CIAO1, IOP1, RTEL1 |
| TERT, TERC, Dyskerin, NHP2, NOP10 | Telomerase | IPF, DKC, aplastic anemia | Apollo | TRF2, FANCD2, Apollo |
| TCAB1 | Cajal body, telomerase assembly | DKC | Cajal body | Coilin, HOT1, TCAB1, Telomerase complex |
| TRF1 regulation | TRF1, TNKS1, TIN2, TNKS1BP1 |
All genes known to cause telomeropathies when defective are listed, as well as the telomere/telomerase-relevant complexes they participate in. Bold indicates a gene known to cause telomeropathies; genes listed without bold are putative candidate genes due to their known interactions. References for complexes not already discussed in the text: CIA complex (Seki et al., 2013), Cajal body proteins (Kappei et al., 2013), and TRF1 regulation (Seimiya and Smith, 2002; Ye and de Lange, 2004). PARsylation, poly(ADP-ribosyl)ation.
It is also possible that some telomeropathies are not monogenic, and so defy conventional linkage analysis. For example, a family with three siblings afflicted by HHS had a rare paternally transmitted missense variant in POT1 present in 2.5% of the population in which each affected sibling inherited the same combination of maternal and paternal alleles, but the unaffected sibling did not (Lamm et al., 2009). The rare variant was clearly not independently causative of the disorder because of its frequency in the general population, but it is possible that there was a reciprocal mutation present in the maternal background that resulted in a context-dependent telomere defect.
Malignancy induced by telomere dysfunction
The observation that DKC families display increased cancer incidence, particularly AML and myelodysplastic syndrome (Alter et al., 2010), is counterintuitive given that telomere length, and the limit on cellular proliferation it imposes, is considered an initial block to oncogenesis (Shay and Wright, 2005). However, telomeropathies are characterized by persistent DNA damage signals at the telomeres, telomere fusions, and genomic rearrangements driven by telomere repair-mediated recombination (Gramatges and Bertuch, 2013). The prolonged action of this genotoxic stress may result in a pool of cells with deranged genomes.
Indeed, spontaneous reversion to the functional TERC allele in haploinsufficient DKC patients via isodisomy of chromosome 3 has been observed (Jongmans et al., 2012), illustrating that both the predisposition to genomic rearrangement is present and that HSCs that obtain a proliferative advantage (in this case by recapitulating adequate telomere maintenance) can take over the depopulated niche. Depopulation of the HSC niche followed by strong selection for HSCs still capable of division may explain why DKC patients are especially predisposed to hematological malignancy and myelodysplastic syndrome (Kirwan et al., 2009; Dokal, 2011).
Presumably, telomere length in normal individuals has been selected into a range that strikes a balance between premature shortening-mediated genomic instability (or immune surveillance deficiencies) observed in DKC cohorts and an unexplored fitness penalty encountered in individuals with constitutively active telomerase or extremely long telomeres. Inappropriate activation of telomerase would logically result in an increased tumor incidence by circumventing crisis, the proliferative limit imposed by telomere shortening. A cancer syndrome has been observed recently in a family with an activating mutation in TERT; a mutation in the upstream promoter region of telomerase created a novel ETS transcription factor–binding site, resulting in approximately twofold up-regulation of telomerase in vitro. The family suffered from an early-onset melanoma tumor syndrome with multiple co-morbid cancers, including one individual afflicted by six different primary tumors (Horn et al., 2013).
Because the frequency of malignancy increases in both DKC as well as in individuals with inappropriately high telomerase activity, it is likely that telomere length in normal individuals remains centered around a “malignancy valley,” which on the whole minimizes the rate of cancer.
Summary
In this review we have given an overview of the causes and symptoms of the disorders caused by defects in telomere maintenance. In addition, we have reviewed a number of related syndromes that may be unrecognized telomeropathies. The symptoms of these disorders are extensive; the age of onset is highly variable with genetic anticipation being involved. However, the disorders share a similar underlying molecular mechanism, premature telomere shortening, leading to a spectrum of diseases that are only recently being recognized. We expect new human syndromes will be revealed in the future that correlate with telomere syndromes, which will be informative in terms of the basic science of telomere biology but also in correctly describing the spectrum disorder that these diseases represent.
Acknowledgments
We would like to thank Sin (Sabrina) Mak for contributing the electron microscopy image of a T-loop used in Figure 1.
The laboratory was supported by NASA grants NNX11AC15G, NNJ05HD36G, and NNX09AU95G; National Cancer Institute SPORE P50CA70907 and CA154805; and the Simmons Cancer Center Support grant 5P30 CA142543. J.W. Shay and W.E. Wright hold the Southland Financial Corporation Distinguished Chair in Geriatric Research. This work was performed in space constructed with support from National Institutes of Health grant C06 RR30414. B. Holohan was supported by a pre-doctoral fellowship from the Simmons Cancer Center.
The authors declare no competing financial interests.
Footnotes
Abbreviations used in this paper:
- AML
- acute myelogenous leukemia
- DKC
- dyskeratosis congenita
- HHS
- Hoyeraal-Hreidersson syndrome
- HSC
- hematopoietic stem cell
- IPF
- idiopathic pulmonary fibrosis
- POT1
- protection of telomeres 1
- TERC
- telomerase RNA component
- TERT
- telomerase reverse transcriptase
- TIF
- telomere-induced foci
- TIN2
- TRF1-interacting nuclear protein 2
- TPP1
- TIN2-interacting protein 1
- TRF
- telomere repeat–binding factor
References
- Aalfs C.M., van den Berg H., Barth P.G., Hennekam R.C. 1995. The Hoyeraal-Hreidarsson syndrome: the fourth case of a separate entity with prenatal growth retardation, progressive pancytopenia and cerebellar hypoplasia. Eur. J. Pediatr. 154:304–308 10.1007/BF01957367 [DOI] [PubMed] [Google Scholar]
- Albrecht E., Sillanpää E., Karrasch S., Alves A.C., Codd V., Hovatta I., Buxton J.L., Nelson C.P., Broer L., Hägg S., et al. 2014. Telomere length in circulating leukocytes is associated with lung function and disease. Eur. Respir. J. 43:983–992 10.1183/09031936.00046213 [DOI] [PubMed] [Google Scholar]
- Alder J.K., Guo N., Kembou F., Parry E.M., Anderson C.J., Gorgy A.I., Walsh M.F., Sussan T., Biswal S., Mitzner W., et al. 2011. Telomere length is a determinant of emphysema susceptibility. Am. J. Respir. Crit. Care Med. 184:904–912 10.1164/rccm.201103-0520OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alter B.P., Giri N., Savage S.A., Peters J.A., Loud J.T., Leathwood L., Carr A.G., Greene M.H., Rosenberg P.S. 2010. Malignancies and survival patterns in the National Cancer Institute inherited bone marrow failure syndromes cohort study. Br. J. Haematol. 150:179–188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson B.H., Kasher P.R., Mayer J., Szynkiewicz M., Jenkinson E.M., Bhaskar S.S., Urquhart J.E., Daly S.B., Dickerson J.E., O’Sullivan J., et al. 2012. Mutations in CTC1, encoding conserved telomere maintenance component 1, cause Coats plus. Nat. Genet. 44:338–342 10.1038/ng.1084 [DOI] [PubMed] [Google Scholar]
- Armanios M. 2012. Telomerase and idiopathic pulmonary fibrosis. Mutat. Res. 730:52–58 10.1016/j.mrfmmm.2011.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armanios M. 2013. Telomeres and age-related disease: how telomere biology informs clinical paradigms. J. Clin. Invest. 123:996–1002 10.1172/JCI66370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armanios M., Blackburn E.H. 2012. The telomere syndromes. Nat. Rev. Genet. 13:693–704 10.1038/nrg3246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armanios M., Chen J.L., Chang Y.P., Brodsky R.A., Hawkins A., Griffin C.A., Eshleman J.R., Cohen A.R., Chakravarti A., Hamosh A., Greider C.W. 2005. Haploinsufficiency of telomerase reverse transcriptase leads to anticipation in autosomal dominant dyskeratosis congenita. Proc. Natl. Acad. Sci. USA. 102:15960–15964 10.1073/pnas.0508124102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armanios M.Y., Chen J.J., Cogan J.D., Alder J.K., Ingersoll R.G., Markin C., Lawson W.E., Xie M., Vulto I., Phillips J.A., III, et al. 2007. Telomerase mutations in families with idiopathic pulmonary fibrosis. N. Engl. J. Med. 356:1317–1326 10.1056/NEJMoa066157 [DOI] [PubMed] [Google Scholar]
- Asselin-Labat M.L., Filby C.E. 2012. Adult lung stem cells and their contribution to lung tumourigenesis. Open Biol. 2:120094 10.1098/rsob.120094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aviv A. 2012. Genetics of leukocyte telomere length and its role in atherosclerosis. Mutat. Res. 730:68–74 10.1016/j.mrfmmm.2011.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballew B.J., Joseph V., De S., Sarek G., Vannier J.B., Stracker T., Schrader K.A., Small T.N., O’Reilly R., Manschreck C., et al. 2013. A recessive founder mutation in regulator of telomere elongation helicase 1, RTEL1, underlies severe immunodeficiency and features of Hoyeraal Hreidarsson syndrome. PLoS Genet. 9:e1003695 10.1371/journal.pgen.1003695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baur J.A., Zou Y., Shay J.W., Wright W.E. 2001. Telomere position effect in human cells. Science. 292:2075–2077 10.1126/science.1062329 [DOI] [PubMed] [Google Scholar]
- Beier F., Foronda M., Martinez P., Blasco M.A. 2012. Conditional TRF1 knockout in the hematopoietic compartment leads to bone marrow failure and recapitulates clinical features of dyskeratosis congenita. Blood. 120:2990–3000 10.1182/blood-2012-03-418038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bojesen S.E., Pooley K.A., Johnatty S.E., Beesley J., Michailidou K., Tyrer J.P., Edwards S.L., Pickett H.A., Shen H.C., Smart C.E., et al. 2013. Multiple independent variants at the TERT locus are associated with telomere length and risks of breast and ovarian cancer. Nat. Genet. 45:371–384: e1–e2 10.1038/ng.2566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broome H.J., Hebert M.D. 2013. Coilin displays differential affinity for specific RNAs in vivo and is linked to telomerase RNA biogenesis. J. Mol. Biol. 425:713–724 10.1016/j.jmb.2012.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calado R.T., Regal J.A., Hills M., Yewdell W.T., Dalmazzo L.F., Zago M.A., Lansdorp P.M., Hogge D., Chanock S.J., Estey E.H., et al. 2009a. Constitutional hypomorphic telomerase mutations in patients with acute myeloid leukemia. Proc. Natl. Acad. Sci. USA. 106:1187–1192 10.1073/pnas.0807057106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calado R.T., Regal J.A., Kleiner D.E., Schrump D.S., Peterson N.R., Pons V., Chanock S.J., Lansdorp P.M., Young N.S. 2009b. A spectrum of severe familial liver disorders associate with telomerase mutations. PLoS ONE. 4:e7926 10.1371/journal.pone.0007926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll K.A., Ly H. 2009. Telomere dysfunction in human diseases: the long and short of it! Int. J. Clin. Exp. Pathol. 2:528–543 [PMC free article] [PubMed] [Google Scholar]
- Carulli L., Dei Cas A., Nascimbeni F. 2012. Synchronous cryptogenic liver cirrhosis and idiopathic pulmonary fibrosis: a clue to telomere involvement. Hepatology. 56:2001–2003 10.1002/hep.26089 [DOI] [PubMed] [Google Scholar]
- Catlin S.N., Busque L., Gale R.E., Guttorp P., Abkowitz J.L. 2011. The replication rate of human hematopoietic stem cells in vivo. Blood. 117:4460–4466 10.1182/blood-2010-08-303537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Yang Y., van Overbeek M., Donigian J.R., Baciu P., de Lange T., Lei M. 2008. A shared docking motif in TRF1 and TRF2 used for differential recruitment of telomeric proteins. Science. 319:1092–1096 10.1126/science.1151804 [DOI] [PubMed] [Google Scholar]
- Chiang Y.J., Calado R.T., Hathcock K.S., Lansdorp P.M., Young N.S., Hodes R.J. 2010. Telomere length is inherited with resetting of the telomere set-point. Proc. Natl. Acad. Sci. USA. 107:10148–10153 10.1073/pnas.0913125107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin L., Artandi S.E., Shen Q., Tam A., Lee S.L., Gottlieb G.J., Greider C.W., DePinho R.A. 1999. p53 deficiency rescues the adverse effects of telomere loss and cooperates with telomere dysfunction to accelerate carcinogenesis. Cell. 97:527–538 10.1016/S0092-8674(00)80762-X [DOI] [PubMed] [Google Scholar]
- Cronkhite J.T., Xing C., Raghu G., Chin K.M., Torres F., Rosenblatt R.L., Garcia C.K. 2008. Telomere shortening in familial and sporadic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 178:729–737 10.1164/rccm.200804-550OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniali L., Benetos A., Susser E., Kark J.D., Labat C., Kimura M., Desai K., Granick M., Aviv A. 2013. Telomeres shorten at equivalent rates in somatic tissues of adults. Nat Commun. 4:1597 10.1038/ncomms2602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Lange T. 2010. How shelterin solves the telomere end-protection problem. Cold Spring Harb. Symp. Quant. Biol. 75:167–177 10.1101/sqb.2010.75.017 [DOI] [PubMed] [Google Scholar]
- De Meyer T., Rietzschel E.R., De Buyzere M.L., De Bacquer D., Van Criekinge W., De Backer G.G., Gillebert T.C., Van Oostveldt P., Bekaert S. 2007. Paternal age at birth is an important determinant of offspring telomere length. Hum. Mol. Genet. 16:3097–3102 10.1093/hmg/ddm271 [DOI] [PubMed] [Google Scholar]
- Diaz de Leon A., Cronkhite J.T., Katzenstein A.L., Godwin J.D., Raghu G., Glazer C.S., Rosenblatt R.L., Girod C.E., Garrity E.R., Xing C., Garcia C.K. 2010. Telomere lengths, pulmonary fibrosis and telomerase (TERT) mutations. PLoS ONE. 5:e10680 10.1371/journal.pone.0010680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dokal I. 2011. Dyskeratosis congenita. Hematology (Am Soc Hematol Educ Program). 2011:480–486 10.1182/asheducation-2011.1.480 [DOI] [PubMed] [Google Scholar]
- Doksani Y., Wu J.Y., de Lange T., Zhuang X. 2013. Super-resolution fluorescence imaging of telomeres reveals TRF2-dependent T-loop formation. Cell. 155:345–356 10.1016/j.cell.2013.09.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan E.D., Collins K. 2010. Specificity and stoichiometry of subunit interactions in the human telomerase holoenzyme assembled in vivo. Mol. Cell. Biol. 30:2775–2786 10.1128/MCB.00151-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg D.T., Hayes M.G., Kuzawa C.W. 2012. Delayed paternal age of reproduction in humans is associated with longer telomeres across two generations of descendants. Proc. Natl. Acad. Sci. USA. 109:10251–10256 10.1073/pnas.1202092109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fogarty P.F., Yamaguchi H., Wiestner A., Baerlocher G.M., Sloand E., Zeng W.S., Read E.J., Lansdorp P.M., Young N.S. 2003. Late presentation of dyskeratosis congenita as apparently acquired aplastic anaemia due to mutations in telomerase RNA. Lancet. 362:1628–1630 10.1016/S0140-6736(03)14797-6 [DOI] [PubMed] [Google Scholar]
- Forsythe H.L., Jarvis J.L., Turner J.W., Elmore L.W., Holt S.E. 2001. Stable association of hsp90 and p23, but Not hsp70, with active human telomerase. J. Biol. Chem. 276:15571–15574 10.1074/jbc.C100055200 [DOI] [PubMed] [Google Scholar]
- Gadalla S.M., Cawthon R., Giri N., Alter B.P., Savage S.A. 2010. Telomere length in blood, buccal cells, and fibroblasts from patients with inherited bone marrow failure syndromes. Aging (Albany, N.Y. Online). 2:867–874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner J.P., Kimura M., Chai W., Durrani J.F., Tchakmakjian L., Cao X., Lu X., Li G., Peppas A.P., Skurnick J., et al. 2007. Telomere dynamics in macaques and humans. J. Gerontol. A Biol. Sci. Med. Sci. 62:367–374 10.1093/gerona/62.4.367 [DOI] [PubMed] [Google Scholar]
- Ghosh A.K., Rossi M.L., Singh D.K., Dunn C., Ramamoorthy M., Croteau D.L., Liu Y., Bohr V.A. 2012. RECQL4, the protein mutated in Rothmund-Thomson syndrome, functions in telomere maintenance. J. Biol. Chem. 287:196–209 10.1074/jbc.M111.295063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gleeson M., O’Marcaigh A., Cotter M., Brosnahan D., Vulliamy T., Smith O.P. 2012. Retinal vasculopathy in autosomal dominant dyskeratosis congenita due to TINF2 mutation. Br. J. Haematol. 159:498. [DOI] [PubMed] [Google Scholar]
- Goldfarb S., Sullivan K.E., Jyonouchi S. 2013. A patient with X-linked dyskeratosis congenita presenting with bronchiolitis obliterans requiring lung transplantation and immunodeficiency. Pediatr. Pulmonol. 48:91–93 10.1002/ppul.22528 [DOI] [PubMed] [Google Scholar]
- Goldman F., Bouarich R., Kulkarni S., Freeman S., Du H.Y., Harrington L., Mason P.J., Londoño-Vallejo A., Bessler M. 2005. The effect of TERC haploinsufficiency on the inheritance of telomere length. Proc. Natl. Acad. Sci. USA. 102:17119–17124 10.1073/pnas.0505318102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grahame T.J., Schlesinger R.B. 2012. Oxidative stress-induced telomeric erosion as a mechanism underlying airborne particulate matter-related cardiovascular disease. Part. Fibre Toxicol. 9:21 10.1186/1743-8977-9-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gramatges M.M., Bertuch A.A. 2013. Short telomeres: from dyskeratosis congenita to sporadic aplastic anemia and malignancy. Transl. Res. 162:353–363 10.1016/j.trsl.2013.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith J.D., Comeau L., Rosenfield S., Stansel R.M., Bianchi A., Moss H., de Lange T. 1999. Mammalian telomeres end in a large duplex loop. Cell. 97:503–514 10.1016/S0092-8674(00)80760-6 [DOI] [PubMed] [Google Scholar]
- Gu P., Min J.N., Wang Y., Huang C., Peng T., Chai W., Chang S. 2012. CTC1 deletion results in defective telomere replication, leading to catastrophic telomere loss and stem cell exhaustion. EMBO J. 31:2309–2321 10.1038/emboj.2012.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heiss N.S., Knight S.W., Vulliamy T.J., Klauck S.M., Wiemann S., Mason P.J., Poustka A., Dokal I. 1998. X-linked dyskeratosis congenita is caused by mutations in a highly conserved gene with putative nucleolar functions. Nat. Genet. 19:32–38 10.1038/ng0598-32 [DOI] [PubMed] [Google Scholar]
- Horn S., Figl A., Rachakonda P.S., Fischer C., Sucker A., Gast A., Kadel S., Moll I., Nagore E., Hemminki K., et al. 2013. TERT promoter mutations in familial and sporadic melanoma. Science. 339:959–961 10.1126/science.1230062 [DOI] [PubMed] [Google Scholar]
- Houghtaling B.R., Cuttonaro L., Chang W., Smith S. 2004. A dynamic molecular link between the telomere length regulator TRF1 and the chromosome end protector TRF2. Curr. Biol. 14:1621–1631 10.1016/j.cub.2004.08.052 [DOI] [PubMed] [Google Scholar]
- Isoda T., Mitsuiki N., Ohkawa T., Kaneko S., Endo A., Ono T., Aoki Y., Tomizawa D., Kajiwara M., Araki S., et al. 2013. Irreversible leukoencephalopathy after reduced-intensity stem cell transplantation in a dyskeratosis congenita patient with TINF2 mutation. J. Pediatr. Hematol. Oncol. 35:e178–e182 10.1097/MPH.0b013e318279e5ca [DOI] [PubMed] [Google Scholar]
- Joksic I., Vujic D., Guc-Scekic M., Leskovac A., Petrovic S., Ojani M., Trujillo J.P., Surralles J., Zivkovic M., Stankovic A., et al. 2012. Dysfunctional telomeres in primary cells from Fanconi anemia FANCD2 patients. Genome Integr. 3:6 10.1186/2041-9414-3-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jongmans M.C., Verwiel E.T., Heijdra Y., Vulliamy T., Kamping E.J., Hehir-Kwa J.Y., Bongers E.M., Pfundt R., van Emst L., van Leeuwen F.N., et al. 2012. Revertant somatic mosaicism by mitotic recombination in dyskeratosis congenita. Am. J. Hum. Genet. 90:426–433 10.1016/j.ajhg.2012.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kajtár P., Méhes K. 1994. Bilateral coats retinopathy associated with aplastic anaemia and mild dyskeratotic signs. Am. J. Med. Genet. 49:374–377 10.1002/ajmg.1320490404 [DOI] [PubMed] [Google Scholar]
- Kappei D., Butter F., Benda C., Scheibe M., Draškovič I., Stevense M., Novo C.L., Basquin C., Araki M., Araki K., et al. 2013. HOT1 is a mammalian direct telomere repeat-binding protein contributing to telomerase recruitment. EMBO J. 32:1681–1701 10.1038/emboj.2013.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller R.B., Gagne K.E., Usmani G.N., Asdourian G.K., Williams D.A., Hofmann I., Agarwal S. 2012. CTC1 mutations in a patient with dyskeratosis congenita. Pediatr. Blood Cancer. 59:311–314 10.1002/pbc.24193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirwan M., Dokal I. 2008. Dyskeratosis congenita: a genetic disorder of many faces. Clin. Genet. 73:103–112 10.1111/j.1399-0004.2007.00923.x [DOI] [PubMed] [Google Scholar]
- Kirwan M., Vulliamy T., Marrone A., Walne A.J., Beswick R., Hillmen P., Kelly R., Stewart A., Bowen D., Schonland S.O., et al. 2009. Defining the pathogenic role of telomerase mutations in myelodysplastic syndrome and acute myeloid leukemia. Hum. Mutat. 30:1567–1573 10.1002/humu.21115 [DOI] [PubMed] [Google Scholar]
- Kondo M. 2010. Lymphoid and myeloid lineage commitment in multipotent hematopoietic progenitors. Immunol. Rev. 238:37–46 10.1111/j.1600-065X.2010.00963.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamm N., Ordan E., Shponkin R., Richler C., Aker M., Tzfati Y. 2009. Diminished telomeric 3′ overhangs are associated with telomere dysfunction in Hoyeraal-Hreidarsson syndrome. PLoS ONE. 4:e5666 10.1371/journal.pone.0005666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Guen T., Jullien L., Touzot F., Schertzer M., Gaillard L., Perderiset M., Carpentier W., Nitschke P., Picard C., Couillault G., et al. 2013. Human RTEL1 deficiency causes Hoyeraal-Hreidarsson syndrome with short telomeres and genome instability. Hum. Mol. Genet. 22:3239–3249 10.1093/hmg/ddt178 [DOI] [PubMed] [Google Scholar]
- Levy D., Neuhausen S.L., Hunt S.C., Kimura M., Hwang S.J., Chen W., Bis J.C., Fitzpatrick A.L., Smith E., Johnson A.D., et al. 2010. Genome-wide association identifies OBFC1 as a locus involved in human leukocyte telomere biology. Proc. Natl. Acad. Sci. USA. 107:9293–9298 10.1073/pnas.0911494107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy M.Z., Allsopp R.C., Futcher A.B., Greider C.W., Harley C.B. 1992. Telomere end-replication problem and cell aging. J. Mol. Biol. 225:951–960 10.1016/0022-2836(92)90096-3 [DOI] [PubMed] [Google Scholar]
- Lin J., Countryman P., Buncher N., Kaur P., e L., Zhang Y., Gibson G., You C., Watkins S.C., Piehler J., et al. 2014. TRF1 and TRF2 use different mechanisms to find telomeric DNA but share a novel mechanism to search for protein partners at telomeres. Nucleic Acids Res. 42:2493–2504 10.1093/nar/gkt1132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lou Z., Jun W., Riethman H., Baur J.A., Voglauer R., Shay J.W., Wright W.E. 2009. Endogenous genes near telomeres regulated by telomere length in human cells. Aging. 1:608–621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyakhovich A., Ramirez M.J., Castellanos A., Castella M., Simons A.M., Parvin J.D., Surralles J. 2011. Fanconi anemia protein FANCD2 inhibits TRF1 polyADP-ribosylation through tankyrase1-dependent manner. Genome Integr. 2:4 10.1186/2041-9414-2-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason J.M., Sekiguchi J.M. 2011. Snm1B/Apollo functions in the Fanconi anemia pathway in response to DNA interstrand crosslinks. Hum. Mol. Genet. 20:2549–2559 10.1093/hmg/ddr153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell J.R., Wood E., Collins K. 1999. A telomerase component is defective in the human disease dyskeratosis congenita. Nature. 402:551–555 10.1038/990141 [DOI] [PubMed] [Google Scholar]
- Nakamura T.M., Morin G.B., Chapman K.B., Weinrich S.L., Andrews W.H., Lingner J., Harley C.B., Cech T.R. 1997. Telomerase catalytic subunit homologs from fission yeast and human. Science. 277:955–959 10.1126/science.277.5328.955 [DOI] [PubMed] [Google Scholar]
- Palm W., de Lange T. 2008. How shelterin protects mammalian telomeres. Annu. Rev. Genet. 42:301–334 10.1146/annurev.genet.41.110306.130350 [DOI] [PubMed] [Google Scholar]
- Parks C.G., Miller D.B., McCanlies E.C., Cawthon R.M., Andrew M.E., DeRoo L.A., Sandler D.P. 2009. Telomere length, current perceived stress, and urinary stress hormones in women. Cancer Epidemiol. Biomarkers Prev. 18:551–560 10.1158/1055-9965.EPI-08-0614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parry E.M., Alder J.K., Qi X., Chen J.J., Armanios M. 2011. Syndrome complex of bone marrow failure and pulmonary fibrosis predicts germline defects in telomerase. Blood. 117:5607–5611 10.1182/blood-2010-11-322149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavesi E., Avondo F., Aspesi A., Quarello P., Rocci A., Vimercati C., Pigullo S., Dufour C., Ramenghi U., Dianzani I. 2009. Analysis of telomeres in peripheral blood cells from patients with bone marrow failure. Pediatr. Blood Cancer. 53:411–416 10.1002/pbc.22107 [DOI] [PubMed] [Google Scholar]
- Polvi A., Linnankivi T., Kivelä T., Herva R., Keating J.P., Mäkitie O., Pareyson D., Vainionpää L., Lahtinen J., Hovatta I., et al. 2012. Mutations in CTC1, encoding the CTS telomere maintenance complex component 1, cause cerebroretinal microangiopathy with calcifications and cysts. Am. J. Hum. Genet. 90:540–549 10.1016/j.ajhg.2012.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramasubramanian A., Shields C.L. 2012. Bevacizumab for Coats’ disease with exudative retinal detachment and risk of vitreoretinal traction. Br. J. Ophthalmol. 96:356–359 10.1136/bjophthalmol-2011-300141 [DOI] [PubMed] [Google Scholar]
- Sasa G.S., Ribes-Zamora A., Nelson N.D., Bertuch A.A. 2012. Three novel truncating TINF2 mutations causing severe dyskeratosis congenita in early childhood. Clin. Genet. 81:470–478 10.1111/j.1399-0004.2011.01658.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage S.A., Giri N., Baerlocher G.M., Orr N., Lansdorp P.M., Alter B.P. 2008. TINF2, a component of the shelterin telomere protection complex, is mutated in dyskeratosis congenita. Am. J. Hum. Genet. 82:501–509 10.1016/j.ajhg.2007.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheinfeld M.H., Lui Y.W., Kolb E.A., Engel H.M., Gomes W.A., Weidenheim K.M., Bello J.A. 2007. The neuroradiological findings in a case of Revesz syndrome. Pediatr. Radiol. 37:1166–1170 10.1007/s00247-007-0592-0 [DOI] [PubMed] [Google Scholar]
- Seimiya H., Smith S. 2002. The telomeric poly(ADP-ribose) polymerase, tankyrase 1, contains multiple binding sites for telomeric repeat binding factor 1 (TRF1) and a novel acceptor, 182-kDa tankyrase-binding protein (TAB182). J. Biol. Chem. 277:14116–14126 10.1074/jbc.M112266200 [DOI] [PubMed] [Google Scholar]
- Seki M., Takeda Y., Iwai K., Tanaka K. 2013. IOP1 protein is an external component of the human cytosolic iron-sulfur cluster assembly (CIA) machinery and functions in the MMS19 protein-dependent CIA pathway. J. Biol. Chem. 288:16680–16689 10.1074/jbc.M112.416602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sfeir A., de Lange T. 2012. Removal of shelterin reveals the telomere end-protection problem. Science. 336:593–597 10.1126/science.1218498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shay J.W., Wright W.E. 2005. Senescence and immortalization: role of telomeres and telomerase. Carcinogenesis. 26:867–874 10.1093/carcin/bgh296 [DOI] [PubMed] [Google Scholar]
- Shchepachev V., Wischnewski H., Missiaglia E., Soneson C., Azzalin C.M. 2012. Mpn1, mutated in poikiloderma with neutropenia protein 1, is a conserved 3′-to-5′ RNA exonuclease processing U6 small nuclear RNA. Cell Rep. 2:855–865 10.1016/j.celrep.2012.08.031 [DOI] [PubMed] [Google Scholar]
- Sidorov I., Kimura M., Yashin A., Aviv A. 2009. Leukocyte telomere dynamics and human hematopoietic stem cell kinetics during somatic growth. Exp. Hematol. 37:514–524 10.1016/j.exphem.2008.11.009 [DOI] [PubMed] [Google Scholar]
- Smith S., Giriat I., Schmitt A., de Lange T. 1998. Tankyrase, a poly(ADP-ribose) polymerase at human telomeres. Science. 282:1484–1487 10.1126/science.282.5393.1484 [DOI] [PubMed] [Google Scholar]
- Stadler G., Rahimov F., King O.D., Chen J.C., Robin J.D., Wagner K.R., Shay J.W., Emerson C.P., Jr, Wright W.E. 2013. Telomere position effect regulates DUX4 in human facioscapulohumeral muscular dystrophy. Nat. Struct. Mol. Biol. 20:671–678 10.1038/nsmb.2571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern J.L., Zyner K.G., Pickett H.A., Cohen S.B., Bryan T.M. 2012. Telomerase recruitment requires both TCAB1 and Cajal bodies independently. Mol. Cell. Biol. 32:2384–2395 10.1128/MCB.00379-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart J.A., Wang F., Chaiken M.F., Kasbek C., Chastain P.D., II, Wright W.E., Price C.M. 2012. Human CST promotes telomere duplex replication and general replication restart after fork stalling. EMBO J. 31:3537–3549 10.1038/emboj.2012.215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takai H., Smogorzewska A., de Lange T. 2003. DNA damage foci at dysfunctional telomeres. Curr. Biol. 13:1549–1556 10.1016/S0960-9822(03)00542-6 [DOI] [PubMed] [Google Scholar]
- Tang J., Kan Z.Y., Yao Y., Wang Q., Hao Y.H., Tan Z. 2008. G-quadruplex preferentially forms at the very 3′ end of vertebrate telomeric DNA. Nucleic Acids Res. 36:1200–1208 10.1093/nar/gkm1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tejera A.M., Stagno d’Alcontres M., Thanasoula M., Marion R.M., Martinez P., Liao C., Flores J.M., Tarsounas M., Blasco M.A. 2010. TPP1 is required for TERT recruitment, telomere elongation during nuclear reprogramming, and normal skin development in mice. Dev. Cell. 18:775–789 10.1016/j.devcel.2010.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theall K.P., McKasson S., Mabile E., Dunaway L.F., Drury S.S. 2013. Early hits and long-term consequences: tracking the lasting impact of prenatal smoke exposure on telomere length in children. Am. J. Public Health. 103(S1, Suppl 1):S133–S135 10.2105/AJPH.2012.301208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Touzot F., Callebaut I., Soulier J., Gaillard L., Azerrad C., Durandy A., Fischer A., de Villartay J.P., Revy P. 2010. Function of Apollo (SNM1B) at telomere highlighted by a splice variant identified in a patient with Hoyeraal-Hreidarsson syndrome. Proc. Natl. Acad. Sci. USA. 107:10097–10102 10.1073/pnas.0914918107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trahan C., Dragon F. 2009. Dyskeratosis congenita mutations in the H/ACA domain of human telomerase RNA affect its assembly into a pre-RNP. RNA. 15:235–243 10.1261/rna.1354009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsakiri K.D., Cronkhite J.T., Kuan P.J., Xing C., Raghu G., Weissler J.C., Rosenblatt R.L., Shay J.W., Garcia C.K. 2007. Adult-onset pulmonary fibrosis caused by mutations in telomerase. Proc. Natl. Acad. Sci. USA. 104:7552–7557 10.1073/pnas.0701009104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsangaris E., Adams S.L., Yoon G., Chitayat D., Lansdorp P., Dokal I., Dror Y. 2008. Ataxia and pancytopenia caused by a mutation in TINF2. Hum. Genet. 124:507–513 10.1007/s00439-008-0576-7 [DOI] [PubMed] [Google Scholar]
- Vannier J.B., Pavicic-Kaltenbrunner V., Petalcorin M.I., Ding H., Boulton S.J. 2012. RTEL1 dismantles T loops and counteracts telomeric G4-DNA to maintain telomere integrity. Cell. 149:795–806 10.1016/j.cell.2012.03.030 [DOI] [PubMed] [Google Scholar]
- Vulliamy T., Marrone A., Goldman F., Dearlove A., Bessler M., Mason P.J., Dokal I. 2001. The RNA component of telomerase is mutated in autosomal dominant dyskeratosis congenita. Nature. 413:432–435 10.1038/35096585 [DOI] [PubMed] [Google Scholar]
- Vulliamy T., Marrone A., Dokal I., Mason P.J. 2002. Association between aplastic anaemia and mutations in telomerase RNA. Lancet. 359:2168–2170 10.1016/S0140-6736(02)09087-6 [DOI] [PubMed] [Google Scholar]
- Vulliamy T., Beswick R., Kirwan M., Marrone A., Digweed M., Walne A., Dokal I. 2008. Mutations in the telomerase component NHP2 cause the premature ageing syndrome dyskeratosis congenita. Proc. Natl. Acad. Sci. USA. 105:8073–8078 10.1073/pnas.0800042105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vulliamy T., Beswick R., Kirwan M.J., Hossain U., Walne A.J., Dokal I. 2012. Telomere length measurement can distinguish pathogenic from non-pathogenic variants in the shelterin component, TIN2. Clin. Genet. 81:76–81 10.1111/j.1399-0004.2010.01605.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walne A.J., Vulliamy T., Marrone A., Beswick R., Kirwan M., Masunari Y., Al-Qurashi F.H., Aljurf M., Dokal I. 2007. Genetic heterogeneity in autosomal recessive dyskeratosis congenita with one subtype due to mutations in the telomerase-associated protein NOP10. Hum. Mol. Genet. 16:1619–1629 10.1093/hmg/ddm111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walne A.J., Vulliamy T., Beswick R., Kirwan M., Dokal I. 2008. TINF2 mutations result in very short telomeres: analysis of a large cohort of patients with dyskeratosis congenita and related bone marrow failure syndromes. Blood. 112:3594–3600 10.1182/blood-2008-05-153445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walne A.J., Bhagat T., Kirwan M., Gitiaux C., Desguerre I., Leonard N., Nogales E., Vulliamy T., Dokal I.S. 2013a. Mutations in the telomere capping complex in bone marrow failure and related syndromes. Haematologica. 98:334–338 10.3324/haematol.2012.071068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walne A.J., Vulliamy T., Kirwan M., Plagnol V., Dokal I. 2013b. Constitutional mutations in RTEL1 cause severe dyskeratosis congenita. Am. J. Hum. Genet. 92:448–453 10.1016/j.ajhg.2013.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F., Stewart J.A., Kasbek C., Zhao Y., Wright W.E., Price C.M. 2012. Human CST has independent functions during telomere duplex replication and C-strand fill-in. Cell Rep. 2:1096–1103 10.1016/j.celrep.2012.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L.L., Plon S.E. 1993. Rothmund-Thomson Syndrome. GeneReviews. Pagon R.A., Adam M.P., Bird T.D., Dolan C.R., Fong C.T., Stephens K., Seattle, WA: 1–27 [Google Scholar]
- Wright W.E., Shay J.W. 1992. Telomere positional effects and the regulation of cellular senescence. Trends Genet. 8:193–197 10.1016/0168-9525(92)90232-S [DOI] [PubMed] [Google Scholar]
- Wright W.E., Piatyszek M.A., Rainey W.E., Byrd W., Shay J.W. 1996. Telomerase activity in human germline and embryonic tissues and cells. Dev. Genet. 18:173–179 [DOI] [PubMed] [Google Scholar]
- Wu P., Takai H., de Lange T. 2012. Telomeric 3′ overhangs derive from resection by Exo1 and Apollo and fill-in by POT1b-associated CST. Cell. 150:39–52 10.1016/j.cell.2012.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xin H., Liu D., Wan M., Safari A., Kim H., Sun W., O’Connor M.S., Songyang Z. 2007. TPP1 is a homologue of ciliate TEBP-beta and interacts with POT1 to recruit telomerase. Nature. 445:559–562 10.1038/nature05469 [DOI] [PubMed] [Google Scholar]
- Yamaguchi H., Calado R.T., Ly H., Kajigaya S., Baerlocher G.M., Chanock S.J., Lansdorp P.M., Young N.S. 2005. Mutations in TERT, the gene for telomerase reverse transcriptase, in aplastic anemia. N. Engl. J. Med. 352:1413–1424 10.1056/NEJMoa042980 [DOI] [PubMed] [Google Scholar]
- Ye J.Z., de Lange T. 2004. TIN2 is a tankyrase 1 PARP modulator in the TRF1 telomere length control complex. Nat. Genet. 36:618–623 10.1038/ng1360 [DOI] [PubMed] [Google Scholar]
- Yehezkel S., Shaked R., Sagie S., Berkovitz R., Shachar-Bener H., Segev Y., Selig S. 2013. Characterization and rescue of telomeric abnormalities in ICF syndrome type I fibroblasts. Front Oncol. 3:35 10.3389/fonc.2013.00035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young N.S. 2012. Bone marrow failure and the new telomere diseases: practice and research. Hematology. 17(Suppl 1):S18–S21 [DOI] [PubMed] [Google Scholar]
- Zhang X., Lin S., Funk W.E., Hou L. 2013. Environmental and occupational exposure to chemicals and telomere length in human studies. Occup. Environ. Med. 70:743–749 10.1136/oemed-2012-101350 [DOI] [PubMed] [Google Scholar]
- Zhong F., Savage S.A., Shkreli M., Giri N., Jessop L., Myers T., Chen R., Alter B.P., Artandi S.E. 2011. Disruption of telomerase trafficking by TCAB1 mutation causes dyskeratosis congenita. Genes Dev. 25:11–16 10.1101/gad.2006411 [DOI] [PMC free article] [PubMed] [Google Scholar]