Abstract
Using data (n=60,775 women) from the Women’s Health Initiative Clinical Trial (WHI CT)— a national study of postmenopausal women aged 50 to 79 years — we analyzed cross-sectional associations between the availability of different types of food outlets in the 1.5 miles surrounding a woman’s residence, census tract neighborhood socioeconomic status (NSES), body mass index (BMI) and blood pressure (BP).
We simultaneously modeled NSES and food outlets using linear and logistic regression models, adjusting for multiple socio-demographic factors, population density and random effects at the tract and metropolitan statistical area (MSA) level.
We found significant associations between NSES, availability of food outlets and individual-level measurements of BMI and BP. As grocery store/supermarket availability increased from the 10th to the 90th percentile of its distribution, controlling for confounders, BMI was lower by 0.30 kg/m2. Conversely, as fast-food outlet availability increased from the 10th to the 90th percentile, BMI was higher by 0.28 kg/m2. When NSES increased from the 10th to the 90th percentile of its distribution, BMI was lower by 1.26 kg/m2. As NSES increased from the 10th to the 90th percentile, systolic and diastolic BP were lower by 1.11 mm and 0.40 mm Hg, respectively. As grocery store/supermarket outlet availability increased from the 10th and 90th percentiles diastolic BP was lower by 0.31 mm Hg.
In this national sample of post-menopausal women, we found important independent associations between the food and socioeconomic environments and BMI and BP. These findings suggest that changes in the neighborhood environment may contribute to efforts to control obesity and hypertension.
INTRODUCTION
A growing body of research has assessed the influence of social and physical characteristics of the environment on obesity and obesity-related conditions, including hypertension, in the United States (1–2). By addressing the role of such features as neighborhood safety and walkability, social services, and especially the local availability of retail outlets that offer healthy food choices—all of which may contribute to obesity or obesity-related behaviors, including diet and exercise—this research has encouraged a more comprehensive assessment of the underlying causes of the obesity epidemic (2–3).
Studies of the local food environment have found associations with poor diet, lack of access to nutritious, affordable food and increased risk of obesity. Compared with other types of food stores, grocery stores and supermarkets tend to offer a large variety of high-quality, healthy food products at lower prices (4–5). Residing near grocery stores or supermarkets has been linked to better quality of diet as well as lower risk of obesity and other risk factors for chronic disease (5–6). Additionally, several studies have shown that consuming food from fast food outlets is associated with higher caloric intake, greater fat intake, higher body mass index (BMI) and weight gain (7–8). Whether individuals who live closer to fast-food restaurants eat more fast food remains uncertain, however; some analyses have found such an association (9), while others have not (10–12).
Studies that have examined the association between neighborhood characteristics, including the local food environment, and the risk of hypertension have yielded analogous results. For example, an analysis of data from the Chicago Community Adult Health Study found that living in an affluent or gentrified neighborhood was associated with a lower rate of hypertension, even after adjusting for individual sociodemographic factors (13). Using data from the Multi-Ethnic Study of Atherosclerosis (MESA) for six communities across the United States, Mujahid and colleagues found that residents of neighborhoods with a higher perceived availability of healthy foods (including high-quality fruits and vegetables and low-fat products), walkability, safety and social cohesion were less likely to have hypertension (14). A recent study of 1,221 middle-aged and older adults living in the Portland, Oregon area, who were followed for one year, found smaller increases in systolic and diastolic blood pressure (BP) among residents of highly walkable neighborhoods (15).
Despite a variety of intriguing findings, however, the existing research linking the local food environment with BMI and hypertension has shortcomings. Most studies have analyzed a single type of food outlet (e.g., grocery stores or fast-food outlets) at one time. Only two studies have examined multiple dimensions of the food environment (i.e., fast food outlets and supermarkets) simultaneously, and both found presence of a grocery store to be associated with reduced obesity risk (12, 16). Further, no study to date has used national data or examined these relationships specifically in women. Focusing on women is important because there is evidence that the effects of neighborhood on women differ from the effects on men (17).
Our study addresses these and other gaps in the literature using data from the Women’s Health Initiative Clinical Trial (WHI CT), a national study of postmenopausal women, to examine the association between the availability of different types of food outlets near a woman’s residence and key health outcomes related to BMI and blood pressure. In our analyses, we simultaneously consider the availability of grocery stores and supermarkets, where there are likely to be numerous healthy food choices; major fast-food restaurants, where many menu options are less healthy; and neighborhood socioeconomic status.
Conceptual Framework
We base this research on a social ecological framework, which proposes that individual health is influenced by biological and genetic functioning, social and familial relationships, environmental contingencies, and broader social and economic trends (18).
Our analyses focus on the influence of neighborhood factors and individual characteristics. There are a variety of mechanisms through which neighborhood factors, including neighborhood socioeconomic status (NSES) and the food environment could impact BMI and blood pressure. These mechanisms include, but are not limited to, exposure, convenience, variety of choices, and cues. Thus NSES could affect BMI and blood pressure through the association of NSES with access to resources conducive to healthy lifestyles (e.g., availability of healthy foods, walking environment) and with the level of neighborhood stressors (e.g., crime, violence and social cohesion). The neighborhood food environment could similarly affect BMI and blood pressure through its association with geographic access and availability of different types of foods and the resulting influence on food purchasing patterns and diet. Since healthy foods can be found in grocery stores and supermarkets, more grocery stores/supermarkets per person may increase the purchase of healthy foods. Similarly, more fast food establishments per person may increase the purchase of the inexpensive, energy dense foods that are typically sold in those establishments (19). The fast food environment may also affect obesity indirectly if one believes that there may be unhealthful cues associated with the fast food environment (20).
METHODS AND PROCEDURES
Data Sources
Our main source of data was the WHI CT, a cohort study of 68,132 women ages 50 – 79 years at baseline, recruited between 1993 and 1998 in areas surrounding 76 clinical centers, satellites and remote examination sites. To optimize the match between the dates of the data on the food environment (see below) and on the health outcomes of interest, we used the BMI and blood pressure (BP) data from the assessment that occurred between October 2004 and March 2005 or the visit closest to that. We geocoded each participant’s residential address in order to obtain the exact longitude and latitude.
WHI CT participants were enrolled in one or more of three randomized controlled trials: dietary modification (DM), hormone therapy (HT), and calcium/vitamin D (CaD) supplementation. The DM trial was designed to evaluate the effect of a low-fat eating pattern on breast cancer, colorectal cancer and coronary heart disease. The HT trial examined the effects of estrogen alone (E) or estrogen plus progestin (E+P) versus placebo on coronary heart disease, osteoporotic fractures and breast cancer. The E+P and E trials were stopped early in July 2002 and March 2004, respectively, but all HT participants were followed without additional intervention until March 31, 2005. The CaD trial, which began 1 to 2 years after women joined one or both of the HT and DM trials, evaluated the effect of calcium and vitamin D supplementation on osteoporotic fractures and colorectal cancer. Additional information about the study design, recruitment and enrollment has been published elsewhere (21).
We developed the food environment measures using 2006 data purchased from InfoUSA, a leading compiler of information on businesses from yellow pages, white pages, newspapers, incorporation records, real estate deed transfers and other sources. The 2006 database contained information on 14 million companies in the United States and included key attributes such as business name, street address, yellow page heading, sales volume and detailed North American Industry Classification System (NAICS) codes. According to InfoUSA, 90 percent of businesses are geocoded to their exact street address and more than 99 percent are geocoded to a census block group. InfoUSA has been used frequently in the literature to compile information regarding the food environment. Particularly with respect to data on fast food restaurants and supermarkets/grocers, when compared with direct observation, the number, type and location of outlets listed in InfoUSA databases has demonstrated to be high (22).
The third source of data, used to create our neighborhood socioeconomic status (NSES) index as well as population density was the 2000 U.S. Census Summary file (23).
Study Population
Women eligible for our study included 68,132 WHI CT participants living in urban or suburban areas. We excluded women who lived in census tracts with a population count of less than 500 (n=62) and women living outside MSAs or in rural census tracts (n=6,679) because we were concerned that our measures of the food environment would not be comparable in urban and rural areas. We also excluded participants who were missing data on the study outcomes (n =117) or whose residential address could not be geocoded (n=499). After these exclusions, the final analytic sample included 60,775 women (92.5 percent of all urban/suburban women in the WHI CT) who resided in 268 different MSAs and 18,186 different census tracts.
Of note, we were initially concerned that BMI and BP outcomes for women in the intervention arm of the DM trial, which was designed to change the diet of its participants, might exhibit associations with the local food environment and neighborhood socioeconomic status that differed from those found in other WHI CT participants. We conducted analyses that excluded DM intervention participants to address this concern, however, and found that the betas and p-values in associations were nearly identical. Therefore, all WHI CT participants who met the other inclusion criteria were included in our analyses.
Study Outcomes
Our analyses were based on estimating multivariate regression models with random effects, as described later, to assess cross-sectional associations between health outcomes of interest and a series of independent variables. The study outcomes included BMI, calculated as the weight in kilograms divided by the square of the height in meters (kg/m2), systolic blood pressure (SBP), and diastolic blood pressure (DBP). Body weight (in kg), height (in cm) and blood pressure (in mm Hg) were measured by trained and certified technicians following standardized protocols. Weight was recorded to the nearest one-tenth kilogram, and height was measured to the nearest one-tenth centimeter using a wall-mounted stadiometer. Blood pressure was measured twice, separated by a 30-second rest. We used the mean of the two readings in our analyses.
We also used standard criteria to develop two binary outcome variables: obesity, defined as BMI ≥ 30, and hypertension, defined as SBP ≥ 140, DBP ≥ 90, or self-reported use of medication for high blood pressure at the baseline visit or any subsequent follow-up visit (41, 42).
Neighborhood Variables
The key independent variables in the models were measures of the local availability of different types of food outlets and neighborhood socioeconomic status. We constructed measures of the availability of different types of food outlets using the following steps. First, we categorized mid-size markets (North American Industry Classification System ([NAICS] code 445110), supermarkets (NAICS code 445110), specialty stores (NAICS codes 44521, 44522), and vegetable and produce markets (NAICS code 44523) as “grocery stores and supermarkets.” We also categorized 10 major limited-service restaurant/fast-food food chains—McDonald’s, Subway, Burger King, Taco Bell, Pizza Hut, Little Caesars, Kentucky Fried Chicken, Wendy’s, Dominos Pizza, and Jack in the Box—as “fast-food restaurants.”
Next, we used the geocoded latitudes and longitudes for participants’ residential addresses and for the addresses of food establishments to calculate the numbers of “grocery store and supermarkets” and “fast-food restaurants” within circular areas, or “buffers,” around each woman’s residence using three alternative radii: 0.75, 1.5, and 3.0 miles. We considered these three buffered areas, based on the urban planning literature, aiming to capture (i) a walkable distance (0.75 miles) (24), (ii) a distance commonly or usually travelled by individuals by car and/or public transport (up to 1.5 miles) (25), and (iii) a larger distance that encompasses majority of a person’s daily activities for the population of interest (3.0 miles) (26–27). We present results for 1.5 miles because most errands and short transportation trips have been shown to be within this distance. We show results for all three buffers in the appendix. Prior studies have examined buffers of varying sizes (e.g., census tracts, as well as up to approximately 2 miles).
We constructed a measure of availability based on the number of outlets per 1,000 persons in the circular buffers. Ideally, to compute this ratio, we would have used the count of food outlets and persons in a buffer. Unfortunately, we were only able to generate the number of food outlets of each type in the buffers, as described in the preceding paragraph; due the restricted nature of the data we used, we were unable to obtain exact population counts for the buffers. Consequently, we approximated the population within each buffer by identifying all the census tracts whose centroids were within the buffer and summing the tract populations. Because the areas encompassed by these tracts and by the buffer were not identical, however, we corrected the ratio of food outlets to population using the respective areas as follows:
where Noutlets is the number of food outlets within the buffer, PTracts is the sum of the population of the tracts, and ABuffer and ATracts are the areas of the buffer and the union of tracts, respectively. Of note, for a woman who lives in a residential setting with smaller tracts (e.g., Manhattan), the buffer would include many other tract centroids. For a woman who lives in a residential setting with larger tracts (e.g., suburban setting), the buffer would include fewer tract centroids. Because the food environment variables were highly skewed, we log-transformed them for analysis.
We measured neighborhood socioeconomic status (NSES) at the level of census tracts using an index of six variables collected in the 2000 Census: (1) percent of adults older than 25 with less than a high school education; (2) percent of males who were unemployed; (3) percent of households with income below the poverty line; (4) percent of households receiving public assistance; (5) percent of households with children headed by a woman; and (6) median household income. The variables for the index were identified through confirmatory factor analysis. This NSES index has been demonstrated in prior studies to be an important neighborhood-level predictor of a variety of health outcomes (28–30). The index ranges from 0 to 100 across U.S. census tracts, with higher scores indicating more affluent tracts. We assigned the NSES index to the participants based on their tract of residence.
Covariates
Several individual characteristics of participants collected at WHI enrollment were included as covariates, including year of randomization, birth cohort, race/ethnicity, educational attainment, household income, marital status, indicator of urban or suburban residence, and indicators for enrollment in the control or intervention arms of the HT, DM or CaD trials. We included population density, which we constructed by computing buffers (i.e., 1.5 mile radii) around each residential address and identifying all of the tract centroids that fall within that specific buffer. We averaged the population densities of these tracts to obtain a smoothed estimate to approximate the population density in a woman’s buffer. For a woman who lives in a residential setting with smaller tracts (e.g., Manhattan), the buffer would include many other tract centroids. For a woman who lives in a residential setting with larger tracts (e.g., suburban setting), the buffer would include fewer tract centroids. Note that this buffer boundary is individualized for every woman. While 80% of our analytic sample is urban and 20% is suburban, we feel this measure is better employing tract-level population density. Yet we recognize that ideally we would have calculated population density based on population size estimates at a smaller census level than a tract (e.g., block and block group) and spatially joined these. Due to the restricted nature of the data we were unable to employ these computations.
Theoretically, neighborhood-level population density may independently affect health outcomes such as blood pressure and BMI. For example, in areas with high population density, people may walk more, transportation facilities may differ, pollution and other aspects of the environment may change with population density, and population density may be correlated with land use mix. We also think that a different definition of buffer may apply to urban versus suburban women. Population density may partly capture this effect because urban and suburban areas will have different levels of population density. Thus, population density can have its own effect through a number of mechanisms, and also serve as a control for many potentially correlated factors.
On average, individual-level covariates were missing in 1.9 percent of cases. We imputed missing values using IVEware in SAS (31).
Estimation
We used linear models for the continuous outcomes (BMI, SBP, and DBP) and logistic models for the binary outcomes (obesity and hypertension). We included multiple random effects, for MSA and for tracts nested within MSA, to allow for correlations among women living in the same tract, and among tracts in the same MSA. We assumed an exchangeable correlation structure within units in a cluster. All tests of significance were conducted with adjusted standard errors. The hierarchical random effects models were estimated using the LME and NLME routines in R (32). We chose a p-value of .05 or less as the criterion for statistical significance in analyses.
Sensitivity Analyses
In our main analyses, we used the measures of availability of different types of food outlets based on the 1.5-mile radius around women’s residences. However, we tested the sensitivity of our results to the choice of radius using the measures developed using the 0.75 and 3.0 mile radii.
We also conducted a sensitivity analysis in which we included total energy expenditure (total METs per week), a measure of physical activity, as a covariate in the regression models. While physical activity is likely to be correlated with both the study outcomes and the neighborhood variables, it is less clear whether physical activity should be considered a confounder of the associations of interest or a mediator of the effects of neighborhood characteristics on the study outcomes. In the former case, it would be appropriate to include it as a covariate in the models; in the latter, it would be more appropriate to exclude it, since we did not intend to conduct a mediation analysis.
Our main analyses did not control for whether women were taking medications that reduce blood pressure because access to high quality medical care may mediate the effects of NSES on the study outcomes and we were interested in the full effect sizes associated with NSES (i.e., the effect sizes without accounting for mediators). Nonetheless, we conducted sensitivity analyses in which we also controlled for taking of anti-hypertensive medication. Results of all of these analyses can be found in Table 6 (Appendix 1 Table 3).
Simulations
To make the effect sizes in our study easier to interpret, we predicted each outcome for a woman at the 10th, 25th, 50th, 75th, and 90th percentile of each neighborhood variable of interest—grocery store and supermarket availability, fast-food restaurant availability and NSES—setting all other covariates at their means. We computed the 95 percent confidence limits for the predicted values of the outcomes using standard methods (33).
RESULTS
Descriptive Data
The mean age of women in the study sample was 68.2 years (Table 1). The women were generally well educated—76.5 percent had at least some college—and fell into middle income brackets. Nearly two-thirds of the women were either married or in a marriage-like relationship. 80.4 percent of the women were non-Hispanic white, 11 percent were Black and 4.5 percent were Hispanic. Also, 80 percent of the women lived in an urban area.
Table 1.
Characteristics of the Women's Health Initiative Study Population n=60,775
| Mean (SD) | |
|---|---|
| Age | 68.21 (7.26) |
| n (%) | |
| Educational Attainment | |
| Less than High School | 3,403 (5.6%) |
| Some High School or GED | 10,879 (17.9%) |
| Some college | 24,128 (39.7%) |
| College degree and beyond | 22,365 (36.8%) |
| Household Income | |
| Less than $10,000 | 2,856 (4.7%) |
| $10,000 to $19,999 | 7,779 (12.8%) |
| $20,000 to $34,999 | 15,133 (24.9%) |
| $35,000 to $49,999 | 12,884 (21.2%) |
| $50,000 to $74,999 | 12,033 (19.8%) |
| $75,000 to $99,999 | 5,409 (8.9%) |
| $100,000 to $149,999 | 3,282 (5.4%) |
| $150,000 or more | 1,459 (2.4%) |
| Marital Status | |
| Never married | 2,553 (4.2%) |
| Divorced or separated | 10,332 (17.0%) |
| Widowed | 10,514 (17.3%) |
| Presently married | 36,343 (59.8%) |
| Marriage-like relationship | 1,033 (1.7%) |
| Race/ethnicity | |
| Black | 6,685 (11.0%) |
| Hispanic | 2,735 (4.5%) |
| White | 48,863 (80.4%) |
| Other | 2,492 (4.1%) |
| Urban (versus suburban) | 48,620 (80.0%) |
The mean BMI of the women in the study sample was 29.1 and 38.1 percent were obese (Table 2). Mean systolic (diastolic) blood pressure was 125.2 mm Hg (71.1 mm Hg), and over half of the women had hypertension.
Table 2.
Main Outcomes of Interest of the Women's Health Initiative Study Population n=60,775
| Mean (SD) | |
|---|---|
| Obesity | |
| BMI | 29.10 (6.12) |
| Blood Pressure | |
| Systolic BP, mmHg | 125.15 (16.75) |
| Diastolic BP, mmHg | 71.13 (9.66) |
| n (%) | |
| Obesea | 23,155.28 (38.1%) |
| Not Obese | 37,619.73 (61.9%) |
| Hypertensionb | 34,580.98 (56.9%) |
Obese is defined as BMI ≥ 30.
Hypertension is defined as having been prescribed hypertension medications by a doctor at baseline or any follow-up visit or having mean systolic BP ≥ 140 mm Hg, diastolic BP ≥90 mm Hg at a woman’s last visit.
Table 3 presents descriptive data for the neighborhood variables of interest. On average, there were 3.9 grocery stores and supermarkets and 3.2 fast-food restaurants per 10,000 persons within a 1.5-mile radius around participants’ residences. (Data for the measures based on the 0.75 and 3.0 mile radii are reported in Table 3.) The mean NSES was 75.4, with a range from 20.0 to 99.6.
Table 3.
Descriptive Statistics of Neighborhood Characteristics - the Women's Health Initiative Study Population n=60,775
| Mean (S.D.) | 10th percentile |
Median | 90th percentile |
|
|---|---|---|---|---|
| Food Environment | ||||
| .75 mile Buffer | ||||
| Fast food restaurants in .75 mile buffer per 1000 persons | 0.68 (14.68) | 0.06 | 0.23 | 1.13 |
| Grocery stores/supermarkets in .75 mile buffer per 1000 persons | 0.72 (8.86) | 0.09 | 0.31 | 1.15 |
| 1.5 mile Buffer | ||||
| Fast food restaurants in 1.5 mile buffer per 1000 persons | 0.32 (1.07) | 0.07 | 0.21 | 0.54 |
| Grocery stores/supermarkets in 1.5 mile buffer per 1000 persons | 0.39 (2.48) | 0.09 | 0.28 | 0.66 |
| 3.0 mile Buffer | ||||
| Fast food restaurants in 3.0 mile buffer per 1000 persons | 0.25 (0.36) | 0.09 | 0.22 | 0.40 |
| Grocery stores/supermarkets in 3.0 mile buffer per 1000 persons | 0.33 (1.49) | 0.13 | 0.28 | 0.53 |
| Neighborhood Socioeconomic Statusa | 75.36 (9.25) | 62.72 | 77.25 | 84.96 |
| Population Density in 0.75 mile buffer | 5,674.91 (8,390.10) | 433.33 | 3,738.00 | 11,034.00 |
| Population Density in 1.5 mile buffer | 5,130.16 (6,695.33) | 552.00 | 3,567.00 | 9,757.60 |
| Population Density in 3.0 mile buffer | 4,518.53 (5,529.06) | 640.00 | 3,135.00 | 8,607.60 |
| Population Density in Census Tract | 6,188.54 (12,221.40) | 419.84 | 3,450.69 | 11,409.68 |
Neighborhood Socioeconomic Status (NSES) is comprised of six census variables: 1) percentage of adults older than 25 with less than a high school education; 2) percentage of males above 16 who are unemployed; 3) percentage of households with an income below the poverty line; 4) percentage of households receiving public assistance; 5) percentage of female-headed households with children; and 6) the median household income. The index ranges from 0 – 100 across U.S. census tracts, with higher scores indicating more affluent tracts.
Regression Results
Our detailed presentation focuses on the findings for the neighborhood variables and on the main analyses, which used the measures of food outlet availability based on a 1.5-mile radius around each participant’s residence. We discuss the results for additional buffers with 0.75 and 3.0 radii at the end of the Results section and present full regression results in the Appendix (Tables 4 and 5).
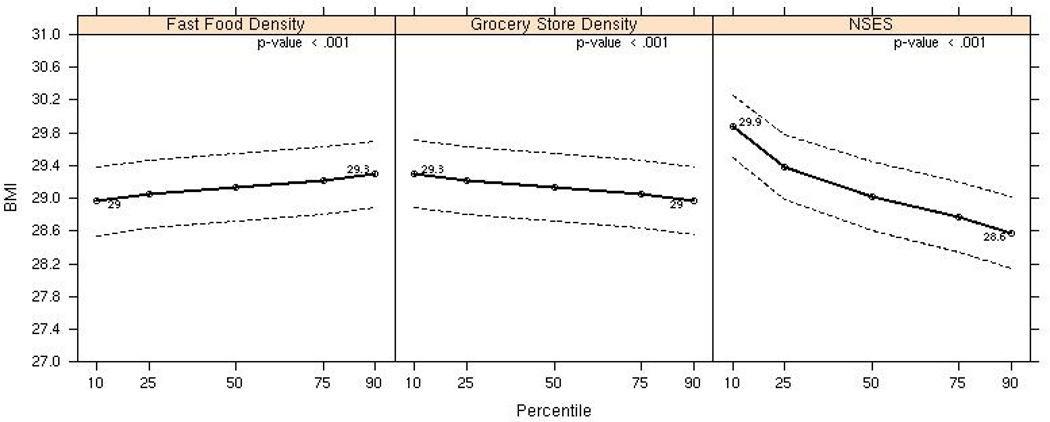
BMI and Obesity
We found a significant negative association between the availability of grocery stores and supermarkets and BMI (coefficient (β)= −.15; 95 percent confidence interval [95% CI]=(−.23, −.08); p<.001), a positive association between the availability of fast-food restaurants and BMI (β=.13; 95% CI= (.06, .21); p<.001), and a negative association between NSES and BMI (β=−.06; 95% CI=(−.06, −.05); p<.001). Figure 1 illustrates the effect sizes. As the availability of grocery stores and supermarkets increased from the 10th to the 90th percentile of the distribution, adjusting for all individual and neighborhood-level covariates, BMI was lower by 0.30 kg/m2, from 29.3 to 29.0. For a 5’6” woman who weighs 177 pounds (BMI = 29.1), this corresponds to a difference of 1 to 2 pounds. Conversely, as the availability of fast-food restaurants increased from the 10th to the 90th percentile, BMI was higher by .28 kg/ m2, from 29.00 to 29.28. Thus the effect size for the availability of fast-food restaurants was similar to the effect size for grocery stores and supermarkets, but opposite in direction. The third panel in Figure 1 shows that, as NSES increased from the 10th to the 90th percentile of the distribution, BMI was lower by 1.26 1.30 kg/ m2 from 29.86 to 28.60. For a 5’6” woman who weighs 177 pounds, this corresponds to a difference of 7 to 8 pounds.
Figure 1.
Associations between Fast Food Density at 1.5 miles, Grocery Store/Supermarket Density at 1.5 miles, NSES and BMI*
*Adjusted for birth cohort, race/ethnicity, educational attainment, marital status, income, urban (vs suburban), population density, availability of fast food outlets, availability of grocery store/supermarkets, NSES.
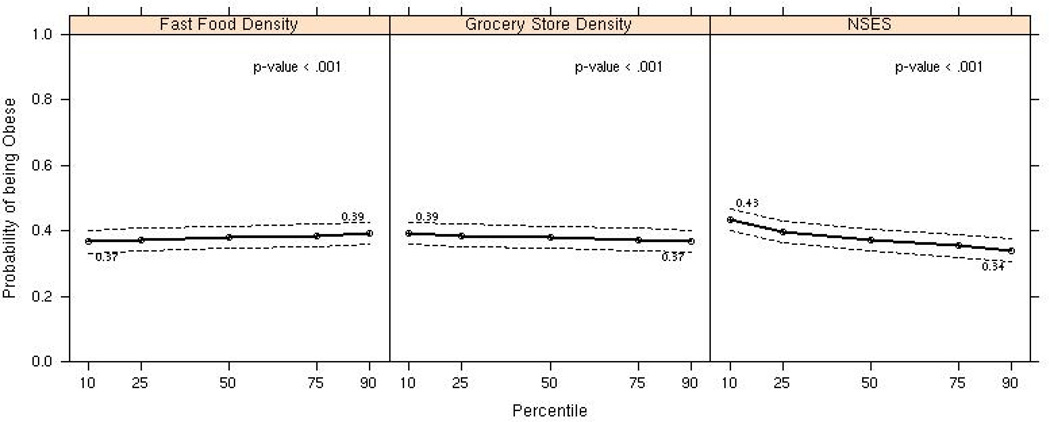
Similarly, we observed a negative association between the availability of grocery stores and supermarkets and the odds of being obese (odds ratio [OR]=.95; 95% CI=(.93, .98); p<.001), a positive association between the availability of fast-food restaurants and the odds of being obese (OR= 1.04; 95% CI =(1.02, 1.07); p<.001), and a negative association between NSES and the odds of obesity (OR=.983; 95% CI= (.980, .985); p<.001). As shown in Figure 2, as the availability of grocery stores and supermarkets increased from the 10th to the 90th percentile, other things being equal, the prevalence of obesity fell from 39 percent to 37 percent. However, the obesity prevalence rose from 37 percent to 39 percent as the availability of fast-food restaurants increased from the 10th to the 90th percentile. The obesity prevalence decreased from 43 percent to 34 percent as NSES increased from the 10th to the 90th percentile.
Figure 2.
Associations between Fast Food Density at 1.5 miles, Grocery Store/Supermarket Density at 1.5 miles, NSES and Obesity (dichotomous) *
*Adjusted for birth cohort, race/ethnicity, educational attainment, marital status, income, urban (vs suburban), population density, availability of fast food outlets, availability of grocery store/supermarkets, NSES.
Blood Pressure and Hypertension
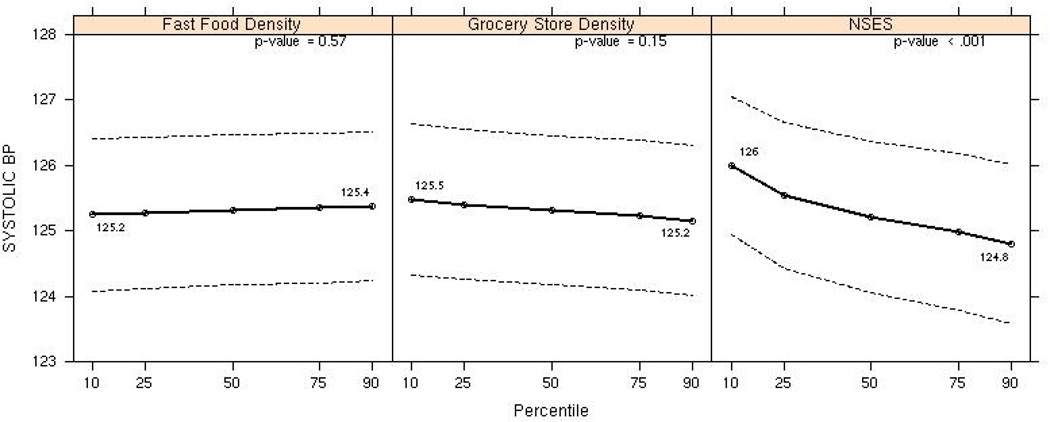
The availability of grocery stores and supermarkets and the availability of fast-food restaurants were not associated with SBP. However, we found a significant negative association between NSES and SBP (β =−.05; 95% CI = (−.07, −.03); p<.001). As NSES increased from the 10th to the 90th percentile of the distribution, other things being equal, SBP was lower by 1.11 mm Hg, from 125.98 to 124.87 (Figure 3).
Figure 3.
Associations between Fast Food Density at 1.5 miles, Grocery Store/Supermarket Density at 1.5 miles, NSES and SBP*
*Adjusted for birth cohort, race/ethnicity, educational attainment, marital status, income, urban (vs suburban), population density, availability of fast food outlets, availability of grocery store/supermarkets, NSES.
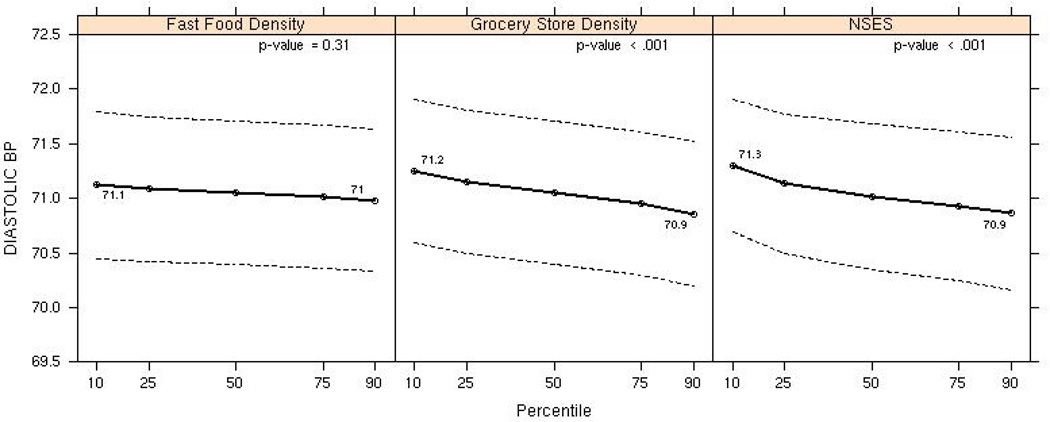
Although the availability of fast-food restaurants was unassociated with DBP, the availability of grocery stores and supermarkets was negatively associated with this outcome (β=−.162; 95% CI =(−.29, −.04); p 0.01). We also found a negative association between NSES and DBP (β=−.02; 95% CI = (−.03, −.01); p 0.002). Αs shown in Figure 3, as grocery store availability increased from the 10th to the 90th percentile, other things being equal, DBP was lower by 0.31 mm Hg, from 71.21 to 70.90. Similarly, as NSES increased from the 10th to the 90th percentile, DBP was lower by 0.40 mm Hg, from 71.27 to 70.87.
Finally, while the availability of fast food restaurants was not associated with the risk of hypertension, the availability of grocery stores/supermarkets showed a significant inverse association with hypertension (OR=0.97; 95% CI=(0.944, 0.995); p < .05). Also, NSES was negatively associated with odds of hypertension (OR=0.994; 95% CI=(0.991, 0.996); p<.001). The prevalence of hypertension decreased from 59 percent to 56 percent as NSES increased from the 10th to the 90th percentile of the distribution (data not shown).
Sensitivity Analyses
The findings of our analyses were similar when we measured the availability of food outlets using a 0.75, 1.5, or 3.0-mile radius around participants’ residences. There were few differences with regard to the statistical significance of associations. Effect sizes differed slightly when we used the alternative radii, but there was no consistent pattern.
We also found that our results (i.e., coefficients and p-values) were almost identical even after adding physical activity to the regression models. Physical activity was negatively and significantly associated with BMI, SBP and DBP, as well as with the dichotomous outcomes of obesity and hypertension.
Finally, controlling for hypertension medication in our fully adjusted models also made virtually no difference in the coefficients or p-values. Compared with the analyses which did not control for hypertension medication, we found that effect sizes and statistical significance were nearly identical to those in the main analyses.
DISCUSSION
Using data from the Women’s Health Initiative Clinical Trial, we found that greater availability of grocery stores and supermarkets within a short distance of women’s homes was associated with lower BMI, lower rates of obesity and lower DBP, other things being equal. Conversely, greater availability of fast food restaurants was associated with higher BMI and higher obesity rates. Additionally, women who lived in more affluent census tracts (i.e., tracts with higher NSES) had lower BMI and obesity rates, lower SBP and DBP, and lower rates of hypertension. Our findings were robust to a variety of sensitivity analyses including using alternative radii around women’s homes to measure the availability of different types of food outlets and adjusting the results for a measure of women’s physical activity.
Evidence suggesting that the “built” environment (i.e., a person’s surroundings that are human-made or modified) influences dietary intake and physical activity has emerged in recent years (34). Studies have also found that access to food outlets with healthy food options may reduce obesity rates (35). Our study supports the hypothesis that the built environment affects BMI and related outcomes, and builds on the existing literature by focusing exclusively on women; using national data; and simultaneously considering the availability of grocery stores and supermarkets, which provide access to fruits and vegetables and other healthy food options; fast-food restaurants, where many menu options are less healthy; and neighborhood socioeconomic status.
A noteworthy observation from our study is that the food environment had a much more consistent association with BMI and obesity than with BP outcomes. By contrast, NSES was strongly and consistently associated with BMI, obesity and all three BP outcomes. This pattern of findings may not be surprising. Published studies suggest that the local availability of different types of food outlets is associated with the quality of people’s diets, and the quality of the diet is a key determinant of total energy balance and consumption of obesogenic food products, which in turn have a direct influence on BMI. However, BP and hypertension are affected by numerous factors in addition to diet and weight including stress, alcohol use, exercise, and access to quality medical care. Our NSES index is likely to capture multiple aspects of neighborhoods that are relevant for both our BMI and BP outcomes including safety, noise, social services, the presence of venues for exercise and recreation, and the availability of medical care providers.
The effect sizes we estimated are consistent with appreciable impacts of the neighborhood characteristics we studied on public health. The prevalence of obesity among women residing in neighborhoods with availability of grocery stores and supermarkets at the 10th to the 90th percentiles differed by 2 percentage points. The obesity rate among women residing in neighborhoods with availability of fast food restaurants at the 10th and 90th percentiles differed by 2 percentage points as well, although in the opposite direction. The obesity rate among women residing in census tracts with NSES at the 10th and 90th percentiles differed by 9 percentage points, and mean BMI differed by 1.26 kg/m2. This difference is similar to the typical weight gain seen in women aged 50–59 at WHI enrollment over 7 years of follow-up (36).
Additionally, mean SBP among women residing in neighborhoods with NSES at the 10th and 90th percentiles differed by 1.11 mm Hg, and the prevalence of hypertension differed by 3 percentage points, other things being equal. An individual-level meta-analysis of randomized trials has shown that SBP differences as small as 2 mm Hg can have a substantial impact on stroke and major cardiovascular events (37).
Limitations
Our study has several limitations. First, the analysis was cross-sectional, which limits our ability to draw causal inferences. An important potential threat to the validity of causal inferences is the selection of individuals and food outlets into neighborhoods. Unhealthy people may disproportionately reside in neighborhoods with a higher availability of fast-food restaurants for reasons that we could not capture—or adjust for—using our data. Although individuals balance multiple goals when moving and are unlikely to have their location decisions driven primarily by a single neighborhood attribute, such as the food environment, unmeasured attributes of individuals, such as assets and proximity of children, may be correlated with both their health and the characteristics of the neighborhoods in which they live. Alternatively, fast-food restaurants may preferentially locate in neighborhoods with unhealthy residents who have a high demand for their menu options. Similarly, grocery stores may situate in neighborhoods with health-conscious residents who demand healthy food choices, or healthy people may disproportionately reside in neighborhoods with high concentrations of grocery stores.
Second, because our findings are based on the WHI data, they pertain to a specific population—women over the age of 50 who reside in metropolitan areas and who do not live in the poorest neighborhoods. Nonetheless, obesity and related conditions are leading causes of morbidity and mortality for this population.
Third, there may be question around how major an issue fast food consumption is among women of postmenopausal age. To clarify, fast food consumption, per se, among this population was not measured. Although much research has demonstrated that fast food consumption has increased dramatically over the past three decades (6–10), no research to our knowledge has focused specifically on older and/or postmenopausal women. Prior research among postmenopausal women, however, has shown that diet is associated with weight gain and incidence of certain cancers (11). Further, our main associations of interest (the effect of the food environment and neighborhood SES on BMI and blood pressure) are relevant for postmenopausal women for a host of reasons including the relevance of weight gain, diet and blood pressure to chronic disease among older women. Our study examined the fast food environment and we note there could be multiple hypothesized mechanisms by which the neighborhood environment may be associated with BMI and hypertension across the United States, that don’t necessarily include fast food consumption as a necessary mediator (e.g., the fast food environment may be associated with other suboptimal health risk behaviors which affect BMI or hypertension).
Fourth, due to limitations of the data, we were unable to account for certain characteristics of women that may influence how and the degree to which they interact with their residential neighborhood environment. These characteristics include employment status, type of work, and use of transportation. In a related vein, we were unable to account for other local environments that may affect women’s health, such as the characteristics of the neighborhoods around their places of work or land use mix, which has been found to be associated with BMI. However, measuring land use mix nationally is not possible. All studies that have demonstrated an association between land use mix and BMI are limited geographically and thus there is no way we can include this in our models. Yet, population density has commonly been used as a land use variable and we did include population density in all models.
Fifth, while we looked at geographic areas of .75, 1.5 and 3.0 miles respectively, our results are based on models with equal buffer radii for fast food establishments and grocery stores. We also examined models that used different buffer radii for fast food establishments and grocery stores and found that our results were consistent in terms of direction, although in a small number of cases the effects did not achieve statistical significance. In particular, in the models for BMI we used a fast food radius of .75 miles and varied the grocery store radius, the effect of fast food outlet availability was smaller than in other models and statistically nonsignificant in two cases. We underscore that we cannot be certain of the best radius and that, in fact, the correct radius may vary across communities. Nonetheless, a radius of .75 miles is in the low range of the radii used in other studies of fast food availability, so it seems likely that the larger radii that we used are more appropriate in most cases.
Next, interpreting associations between neighborhood characteristics and SBP and DBP is complicated by the use of blood-pressure-lowering medications in a substantial proportion of women who had hypertension. As discussed earlier, access to quality medical care may be an important determinant of BP among persons with hypertension. To account for this, we also analyzed a binary variable indicating the presence of hypertension and found no difference in our results.
Finally, our measures of the availability of different types of food outlets are subject to measurement error. Our approach of enumerating food outlets within circular buffers around women’s residences weighted all outlets inside a buffer equally and assigned a weight of zero to all outlets outside the buffer. In fact, food outlets are likely to diminish in importance to women as the distance from their homes increases, but gradually rather than abruptly. Also, although the three alternative radii that we chose for the buffers—0.75, 1.5, and 3.0 miles—were based on information from other studies on how far people travel to buy food, the appropriate radius is likely to vary across communities based on such characteristics as urbanicity, street design and traffic.
Another source of measurement error stems from the fact that, in constructing the availability measures, we were unable to ascertain the true population counts of buffers and instead used the population counts for an overlapping area constructed by joining census tracts whose centroids lie within the circular buffers. Measurement error from this source is likely to be smallest for the 0.75 mile radius and largest for the 3.0 mile radius. The last source of measurement error is the quality of the InfoUSA data on food outlets, which may miss some outlets and may contain errors in addresses, names, and NAICS/SIC codes.
We addressed concerns about measurement error by using alternative radii to conduct sensitivity analyses and found little difference in the results, although this is not a definitive test. We also included population density as a covariate in the models to capture urbanicity and crowding. Of note, in the classical measurement error model, the error biases regression coefficients toward zero, suggesting that our analyses may understate the effect sizes for the food outlet variables. However, the results for the classical model depend on the measurement error being uncorrelated with other independent variables; we have no way of assessing this assumption.
Despite these limitations, our study makes an important and novel contribution to the literature on the association between neighborhood characteristics and health outcomes. Most important, our findings provide strong evidence for an association between the local availability of different types of food outlets and obesity.
Conclusions and Policy Implications
The postmenopausal years are an especially important time for women’s cardiovascular health. Reducing rates of obesity and hypertension in women is important because these conditions are risk factors for comorbidities and complications—such as stroke, myocardial infarction and heart failure—that have serious implications for women’s health. While our results cannot be interpreted as identifying causal effects, they do support the hypothesis that modifying the food environment to encourage healthy eating may have a beneficial impact on obesity and related outcomes. A growing number of communities are developing policies that aim to curb obesity. For example, communities and municipalities have moved to require nutritional information on food in restaurants (38), ban trans fats in restaurant food, and limit or prohibit additional fast-food restaurants (39). Our findings provide support for policies to attract grocery stores and limit increases in the number of fast-food restaurants in residential areas. Continued examination of different aspects of the food environment, geographic areas and population subgroups would be useful avenues in the context of the current efforts to address the obesity epidemic in the United States.
Supplementary Material
Figure 4.
Associations between Fast Food Density at 1.5 miles, Grocery Store/Supermarket Density at 1.5 miles, NSES and DBP*
*Adjusted for birth cohort, race/ethnicity, educational attainment, marital status, income, urban (vs suburban), population density, availability of fast food outlets, availability of grocery store/supermarkets, NSES.
ACKNOWLEDGMENTS
This work was funded by the National Heart, Lung and Blood Institute (40 R01HL084425). The work was carried out in RAND's Center for Population Health and Health Disparities. The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts N01WH22110, 24152, 32100–2, 32105–6, 32108–9, 32111–13, 32115, 32118–32119, 32122, 42107–26, 42129–32, and 44221. We acknowledge WHI investigators including: Program Office: (National Heart, Lung, and Blood Institute, Bethesda, Maryland) Jacques Rossouw, Shari Ludlam, Joan McGowan, Leslie Ford, and Nancy Geller. Clinical Coordinating Center: (Fred Hutchinson Cancer Research Center, Seattle, WA) Ross Prentice, Garnet Anderson, Andrea LaCroix, Charles L. Kooperberg; (Medical Research Labs, Highland Heights, KY) Evan Stein; (University of California at San Francisco, San Francisco, CA) Steven Cummings. Clinical Centers: (Albert Einstein College of Medicine, Bronx, NY) Sylvia Wassertheil-Smoller; (Baylor College of Medicine, Houston, TX) Haleh Sangi-Haghpeykar; (Brigham and Women's Hospital, Harvard Medical School, Boston, MA) JoAnn E. Manson; (Brown University, Providence, RI) Charles B. Eaton; (Emory University, Atlanta, GA) Lawrence S. Phillips; (Fred Hutchinson Cancer Research Center, Seattle, WA) Shirley Beresford; (George Washington University Medical Center, Washington, DC) Lisa Martin; (Los Angeles Biomedical Research Institute at Harbor- UCLA Medical Center, Torrance, CA) Rowan Chlebowski; (Kaiser Permanente Center for Health Research, Portland, OR) Erin LeBlanc; (Kaiser Permanente Division of Research, Oakland, CA) Bette Caan; (Medical College of Wisconsin, Milwaukee, WI) Jane Morley Kotchen; (MedStar Research Institute/Howard University, Washington, DC) Barbara V. Howard; (Northwestern University, Chicago/Evanston, IL) Linda Van Horn; (Rush Medical Center, Chicago, IL) Henry Black; (Stanford Prevention Research Center, Stanford, CA) Marcia L. Stefanick; (State University of New York at Stony Brook, Stony Brook, NY) Dorothy Lane; (The Ohio State University, Columbus, OH) Rebecca Jackson; (University of Alabama at Birmingham, Birmingham, AL) Cora E. Lewis; (University of Arizona, Tucson/Phoenix, AZ) Cynthia A. Thomson; (University at Buffalo, Buffalo, NY) Jean Wactawski-Wende; (University of California at Davis, Sacramento, CA) John Robbins; (University of California at Irvine, CA) F. Allan Hubbell; (University of California at Los Angeles, Los Angeles, CA) Lauren Nathan; (University of California at San Diego, LaJolla/Chula Vista, CA) Robert D. Langer; (University of Cincinnati, Cincinnati, OH) Margery Gass; (University of Florida, Gainesville/Jacksonville, FL) Marian Limacher; (University of Hawaii, Honolulu, HI) J. David Curb; (University of Iowa, Iowa City/Davenport, IA) Robert Wallace; (University of Massachusetts/Fallon Clinic, Worcester, MA) Judith Ockene; (University of Medicine and Dentistry of New Jersey, Newark, NJ) Norman Lasser; (University of Miami, Miami, FL) Mary Jo O’Sullivan; (University of Minnesota, Minneapolis, MN) Karen Margolis; (University of Nevada, Reno, NV) Robert Brunner; (University of North Carolina, Chapel Hill, NC) Gerardo Heiss; (University of Pittsburgh, Pittsburgh, PA) Lewis Kuller; (University of Tennessee Health Science Center, Memphis, TN) Karen C. Johnson; (University of Texas Health Science Center, San Antonio, TX) Robert Brzyski; (University of Wisconsin, Madison, WI) Gloria E. Sarto; (Wake Forest University School of Medicine, Winston-Salem, NC) Mara Vitolins; (Wayne State University School of Medicine/Hutzel Hospital, Detroit, MI) Michael S. Simon. Women’s Health Initiative Memory Study: (Wake Forest University School of Medicine, Winston-Salem, NC) Sally Shumaker.
Footnotes
DISCLOSURE
The authors of this manuscript have no conflicts of interest to declare.
Contributor Information
T. Dubowitz, RAND Corporation
B. Ghosh-Dastidar, RAND Corporation
C. Eibner, RAND Corporation
M.E. Slaughter, RAND Corporation
M. Fernandes, RAND Corporation
E.A. Whitsel, Departments of Epidemiology and Medicine, University of North Carolina Gillings School of Global Public Health and School of Medicine
C.E. Bird, RAND Corporation
A. Jewell, RAND Corporation
K. L. Margolis, University of Minnesota and Health Partners Research Foundation
W. Li, Preventive and Behavioral Medicine, University of Massachusetts Medical School
Y. Michael, Epidemiology and Biostatistics, Drexel University School of Public Health
R. Shih, RAND Corporation
J. Manson, Department of Preventive Medicine, Brigham and Women’s Hospital, Harvard Medical School
J.J. Escarce, RAND Corporation and University of California Los Angeles
REFERENCES
- 1.Lake A, Townshend T. Obesogenic environments: Exploring the built and food environments. J R Soc Promot Health. 2006 Nov;126(6):262–267. doi: 10.1177/1466424006070487. [DOI] [PubMed] [Google Scholar]
- 2.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117(2):417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 3.Kirk SFL, Penney TL, McHugh TLF. Characterizing the obesogenic environment: The state of the evidence with directions for future research. Obes Rev. 2009;11(2):109–117. doi: 10.1111/j.1467-789X.2009.00611.x. [DOI] [PubMed] [Google Scholar]
- 4.Block D, Kouba J. A comparison of the availability and affordability of a market basket in two communities in the chicago area. Public Health Nutr. 2006 Oct;9(7):837–845. doi: 10.1017/phn2005924. [DOI] [PubMed] [Google Scholar]
- 5.Bodor JN, Rose D, Farley TA, Swalm C, Scott SK. Neighbourhood fruit and vegetable availability and consumption: The role of small food stores in an urban environment. Public Health Nutr. 2008;11(4):413–420. doi: 10.1017/S1368980007000493. [DOI] [PubMed] [Google Scholar]
- 6.Morland K, Wing S, Roux AD. The contextual effect of the local food environment on residents' diets: The atherosclerosis risk in communities study. Am. J. Public Health. 2002;92(11):1761–1768. doi: 10.2105/ajph.92.11.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bowman SA, Vinyard BT. Fast food consumption of US adults: Impact on energy and nutrient intakes and overweight status. J. Am. Coll. Nutr. 2004;23(2):163–168. doi: 10.1080/07315724.2004.10719357. [DOI] [PubMed] [Google Scholar]
- 8.Jeffery R, Baxter J, McGuire M, Linde J. Are fast food restaurants an environmental risk factor for obesity? Int J Behav Nutr Phys Act. 2006;3(1):2. doi: 10.1186/1479-5868-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu GC, Wilson JS, Qi R, Ying J. Green neighborhoods, food retail and childhood overweight: Differences by population density. Am. J. Health Promot. 2007;21(4):317–325. doi: 10.4278/0890-1171-21.4s.317. [DOI] [PubMed] [Google Scholar]
- 10.Currie J, DellaVigna S, Moretti E, Pathania V. The effect of fast food restaurants on obesity. NBER Working Paper, w14721. 2009 [Google Scholar]
- 11.Li F, Harmer P, Cardinal BJ, Bosworth M, Johnson-Shelton D. Obesity and the built environment: Does the density of neighborhood fast-food outlets matter? Am. J. Health Promot. 2009;23(3):203–209. doi: 10.4278/ajhp.071214133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rundle A, Neckerman KM, Freeman L, et al. Neighborhood food environment and walkability predict obesity in new york city. Environ. Health Perspect. 2009;117(3):442–447. doi: 10.1289/ehp.11590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness, treatment, and control: The role of neighborhood context. Soc. Sci. Med. 2007;65(9):1853–1866. doi: 10.1016/j.socscimed.2007.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mujahid MS, Roux D, Ana V, et al. Neighborhood characteristics and hypertension. Epidemiology. 2008 Jul;19(4):590–598. doi: 10.1097/EDE.0b013e3181772cb2. [DOI] [PubMed] [Google Scholar]
- 15.Li F, Harmer P, Cardinal BJ, Vongjaturapat N. Built environment and changes in blood pressure in middle aged and older adults. Prev. Med. 2009 Mar;48(3):237–241. doi: 10.1016/j.ypmed.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lopez RP. Neighborhood risk factors for obesity. Obesity. 2007;15(8):2111–2119. doi: 10.1038/oby.2007.251. [DOI] [PubMed] [Google Scholar]
- 17.Grafova I, Freedman V, Kumar R, Rogowski J. Neighborhoods and obesity in later life. Am. J. Public Health. 2008;98(11):2065. doi: 10.2105/AJPH.2007.127712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smedley BD, Syme SL. Promoting health: Intervention strategies from social and behavioral research. Am. J. Health Promot. 2001 Jan-Feb;15(3):149–166. doi: 10.4278/0890-1171-15.3.149. [DOI] [PubMed] [Google Scholar]
- 19.Farley TA, Rice J, Bodor JN, Cohen DA, Bluthenthal RN, Rose D. Measuring the food environment: Shelf space of fruits, vegetables, and snack foods in stores. J. Urban Health. 2009 Sep;86(5):672–682. doi: 10.1007/s11524-009-9390-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paquet C, Daniel M, Knauper B, Gauvin L, Kestens Y, Dube L. Interactive effects of reward sensitivity and residential fast-food restaurant exposure on fast-food consumption. Am. J. Clin. Nutr. 2010 Mar;91(3):771–776. doi: 10.3945/ajcn.2009.28648. [DOI] [PubMed] [Google Scholar]
- 21.Anderson GL, Manson J, Wallace R, et al. Implementation of the Women's Health Initiative study design. Ann. Epidemiol. 2003 Oct;13(9S):S5–S17. doi: 10.1016/s1047-2797(03)00043-7. [DOI] [PubMed] [Google Scholar]
- 22.Bader M, Ailshire J, Morenoff J, House J. Measurement of the local food environment: A comparison of existing data sources. Am. J. Epidemiol. 2010 doi: 10.1093/aje/kwp419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.U.S. Census Bureau. Census 2000 summary file 4: Household and families 2000. [Accessed October 2004];2000 http://factfinder.census.gov.
- 24.Agrawal AW, Schlossberg M, Irvin K. How far, by which route and why? A spatial analysis of pedestrian preference. Journal of Urban Design. 2008;13(1):81–98. [Google Scholar]
- 25.Vitaliano PP, Scanlan JM, Zhang J, et al. Are the salutogenic effects of social supports modified by income? A test of an "Added value" Hypothesis. Health Psychol. 2001;20:155–165. [PubMed] [Google Scholar]
- 26.Hu PS, Young JR. Summary of travel trends: 1995 nationwide personal transportation survey. Knoxville TN: 1999. [Google Scholar]
- 27.Frank LD, Engelke P, Hourigan D. How land use and transportation systems impact public health: An annotated bibliography. Atlanta, GAND: [Google Scholar]
- 28.Bird CE, Seeman TE, Escarce JJ, et al. Neighborhood socioeconomic status and biological "Wear & tear" In a nationally representative sample of u.S. Adults. J. Epidemiol. Community Health. 2009 Sep 16; doi: 10.1136/jech.2008.084814. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dubowitz T, Heron M, Bird CE, et al. Neighborhood socioeconomic status and fruit and vegetable intake among whites, blacks, and mexican americans in the United States. Am. J. Clin. Nutr. 2008;87(6):1883–1891. doi: 10.1093/ajcn/87.6.1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Merkin S, Basurto-Dávila R, Karlamangla A, et al. Neighborhoods and cumulative biological risk profiles by race/ethnicity in a national sample of US adults: Nhanes III. Ann. Epidemiol. 2009;19(3):194–201. doi: 10.1016/j.annepidem.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raghunathan T, Solenberger P, Van Hoewyk J. Iveware: Imputation and variance estimation software: Survey Research Center, Survey Methodology Program, Institute for Social Research. University of Michigan; 2002. [Google Scholar]
- 32.R Development Core Team. R. Vienna, Austria: R Foundation for Statistical Computing; 2009. A language and environment for statistical computing. http://cran.r-project.org/doc/manuals/refman.pdf. [Google Scholar]
- 33.Wooldridge J. Econometric analysis of cross section and panel data. The MIT Press; 2002. [Google Scholar]
- 34.Popkin BM, Duffey K, Gordon-Larsen P. Environmental influences on food choice, physical activity and energy balance. Physiol. Behav. 2005;86(5):603–613. doi: 10.1016/j.physbeh.2005.08.051. [DOI] [PubMed] [Google Scholar]
- 35.Rao M, Prasad S, Adshead F, Tissera H. The built environment and health. Lancet. 2007;370(9593):1111–1113. doi: 10.1016/S0140-6736(07)61260-4. [DOI] [PubMed] [Google Scholar]
- 36.Caan B, Neuhouser M, Aragaki A, et al. Calcium plus vitamin d supplementation and the risk of postmenopausal weight gain. Arch. Intern. Med. 2007;167(9):893. doi: 10.1001/archinte.167.9.893. [DOI] [PubMed] [Google Scholar]
- 37.Turnbull F, Neal B, Algert C. Effects of different blood-pressure-lowering regimens on major cardiovascular events: Results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527–1535. doi: 10.1016/s0140-6736(03)14739-3. [DOI] [PubMed] [Google Scholar]
- 38.Elbel B, Kersh R, Brescoll VL, Dixon LB. Calorie labeling and food choices: A first look at the effects on low-income people in new york city. Health Aff (Project Hope) 2009 doi: 10.1377/hlthaff.28.6.w1110. [DOI] [PubMed] [Google Scholar]
- 39.Bibbins-Domingo K, Chertow GM, Coxson PG, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N. Engl. J. Med. 2010 Feb 18;362(7):590–599. doi: 10.1056/NEJMoa0907355. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gonzalez JS, Safren SA, Delahanty LM, et al. Symptoms of depression prospectively predict poorer self-care in patients with type 2 diabetes. Diabetic medicine: a journal of the British Diabetic Association. 2008;25(9):1102. doi: 10.1111/j.1464-5491.2008.02535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.