Abstract
Live attenuated influenza vaccines (LAIV) offer significant advantages over subunit or split inactivated vaccines to mitigate an eventual influenza pandemic, including simpler manufacturing processes and more cross-protective immune responses. Using an established reverse genetics (rg) system for wild-type (wt) A/Leningrad/134/1957 and cold-adapted (ca) A/Leningrad/134/17/1957 (Len17) master donor virus (MDV), we produced and characterized three rg H5N1 reassortant viruses carrying modified HA and intact NA genes from either A/Vietnam/1203/2004 (H5N1, VN1203, clade 1) or A/Egypt/321/2007 (H5N1, EG321, clade 2) virus. A mouse model of infection was used to determine the infectivity and tissue tropism of the parental wt viruses compared to the ca master donor viruses as well as the H5N1 reassortants. All ca viruses showed reduced replication in lungs and enhanced replication in nasal epithelium. In addition, the H5N1 HA and NA enhanced replication in lungs unless it was restricted by the internal genes of the ca MDV. Mice inoculated twice 4 weeks apart with the H5N1 reassortant LAIV candidate viruses developed serum hemagglutination inhibition HI and IgA antibody titers to the homologous and heterologous viruses consistent with protective immunity. These animals remained healthy after challenge inoculation with a lethal dose with homologous or heterologous wt H5N1 highly pathogenic avian influenza (HPAI) viruses. The profiles of viral replication in respiratory tissues and the immunogenicity and protective efficacy characteristics of the two ca H5N1 candidate LAIV viruses warrant further development into a vaccine for human use.
INTRODUCTION
The A (H5N1) highly pathogenic avian influenza (HPAI) virus reemerged in 2003 in Asia and subsequently spread to Africa, Europe, and the Middle East, becoming endemic in some countries. To date, human-to-human transmission of H5N1 HPAI viruses has been very limited, and most cases of infection in humans have occurred through close contact with infected live or dead poultry (1, 2). The cumulative number of laboratory-confirmed human cases from 2003 to January 2014 is 648, with 384 deaths, resulting in a case-fatality ratio of nearly 60% (3). The virus is also highly pathogenic for poultry as defined by the World Organization for Animal Health (4).
While pandemic preparedness attention is divided among the A (H5N1), A (H2N2), A (H9N2), A (H7Nx), and A (H3N2)v subtypes in various continents, the endemicity of H5N1 viruses in poultry in parts of Asia and Africa (5, 6) poses a challenging threat to public health. The emergence of new reassortant variants between human viruses such as A (H1N1)pdm09 and H5N1 HPAI virus, potentially generating reassortants with the transmissibility of the 2009 H1N1 virus and the virulence of the HPAI H5N1 viruses, would pose a threat to public health (7). Therefore, research focused on the development of safe and effective vaccines against circulating A (H5N1) viruses for use in humans is needed to meet pandemic preparedness goals. A number of preclinical and clinical studies of pandemic vaccine candidate viruses prepared using different techniques are ongoing, and early results have been published (8–13). Some of these studies evaluate H5N1 candidate vaccine viruses representing recently emerged antigenic clusters and prepared in compliance with regulatory requirements for vaccine production (14).
Previous studies have shown that inactivated influenza vaccines delivered intramuscularly can efficiently elicit humoral neutralizing antibodies that are, however, generally restricted to viruses that are antigenically closely related (15–17). In contrast to inactivated vaccines, live attenuated influenza vaccines (LAIV) administered intranasally (i.n.) mimic natural infection and are capable of inducing a much broader immune response, as demonstrated in animal models and human trials (18–20). Besides eliciting humoral antibodies, LAIV elicit mucosal immunity that prevents virus entry and subsequent replication and spread in the respiratory tract. In addition to inducing neutralizing antibodies against circulating strains, live attenuated vaccines can also elicit viral epitope-specific cytotoxic CD8+ T lymphocytes and confer heterosubtypic immunity (18, 21–24).
Russian live attenuated influenza vaccines are produced by reassortment of genes from a cold-adapted, temperature-sensitive (abbreviated as ca/ts) master donor virus (MDV), A/Leningrad/134/17/57 (H2N2) (caLen17), and a currently circulating or potentially pandemic wild-type (wt) influenza A virus (21, 25, 26). A single dose is highly effective in preventing influenza-related disease as well as reducing bronchitis and pneumonia (21, 25, 27, 28). Millions of doses of this LAIV have been used in Russia, and similar vaccines have been used in the United States in recent years. Reassortant vaccine viruses derived from coinfection in embryonated eggs are selected by low-temperature (25 to 26°C) propagation followed by limiting dilution cloning to identify a reassortant virus that replicates efficiently at 25 to 26°C (cold-adapted [ca]) but is impaired at 39 to 40°C (i.e., has the ts phenotype). Cold adaptation enables the attenuated reassortant vaccine virus to replicate efficiently in the low-temperature regions of the upper respiratory tract to stimulate immune protection and memory, while the ts phenotype impairs replication at the higher temperature of the lower respiratory tract, where efficient replication would induce unwanted pathology.
The after-action review of the 2009 H1N1 pandemic response concluded that the current egg-based vaccine production system cannot meet the surge in demand to mitigate an eventual pandemic. Increasing the supply of fertile eggs by 1 order of magnitude to immunize at least 70 to 80% of the world population would require the construction of production facilities that are not sustainable in the postpandemic years. Cell-based influenza vaccine manufacturing can supplement the current egg-based system, expanding production capacity and potentially antigenic fidelity (29–31).
Here, we report the use of a reverse genetics (rg) system developed for cold-adapted master donor virus (MDV) caLen17 to generate two Madin-Darby canine kidney (MDCK) cell culture-derived H5N1 6:2 reassortants of the antigenically distinct clades 1 and 2.2 and a study of their immunogenicity and protective efficacy in a mouse model.
MATERIALS AND METHODS
Cells, viruses, and plasmids.
Madin-Darby canine kidney (MDCK) and 293T human embryonic kidney (HEK293T) cells were obtained from the American Type Culture Collection (ATCC) and were maintained in Dulbecco modified Eagle medium (DMEM) (Invitrogen, Carlsbad, CA) supplemented with 10% fetal bovine serum. Cold-adapted A/Leningrad/134/17/57 (H2N2) MDV (caLen17) was obtained from Nobilon International B.V. (The Netherlands). This virus was derived from an original egg-isolated caLen17 stock (32) and propagated in MDCK cells at a permissive temperature (32 to 34°C) followed by plaque purification. A working stock of caLen17 virus was prepared in MDCK cells by infection at a multiplicity of infection (MOI) of 0.0001 at a permissive temperature. Wild-type A/Leningrad/134/57 (H2N2) (Len134), A/Vietnam/1203/2004 (H5N1) clade 1 (VN1203), and A/Egypt/321/2007 (H5N1) clade 2.2 (EG321) viruses were from the CDC repository. These viruses were amplified in MDCK cells at 37°C to prepare working stock solutions. A/Vietnam/1203/2005(H5N1)PR8 (VN1203-PR8) and A/Egypt/2321-NAMRU3/2007(H5N1)PR8-IDCDC-RG11 (EG321-PR8) candidate vaccine viruses were propagated in eggs as described previously (33, 34).
A set of eight dual-promoter plasmids carrying all gene segments of caLen17 prepared at the CDC was used to rescue caLen17-rg virus (35, 36). Len134-rg virus was derived by reverting caLen17-specific mutations by reverse genetics (rg) as described previously (37). Site-directed mutagenesis of the plasmids was performed using the QuikChange XL multisite-directed mutagenesis kit (Stratagene, La Jolla, CA). Plasmids carrying modified HA and intact NA genes of VN1203 and EG321 viruses were described previously (33, 34).
All H5N1 reassortant viruses used in this study were engineered with a deletion of the polybasic cleavage site in the HA molecule. Wild-type H5N1 HPAI viruses with intact HA were used for challenge inoculation and for performing immunoassays.
Generation of reassortant viruses.
DNA from a set of eight plasmids was transfected into cocultured HEK293T/MDCK cells using TransIT LT-1 transfection reagent (Mirus, Madison, WI) according to the manufacturer's protocol. Four days after transfection, culture supernatants and cell lysates were collected and the recovered viruses were amplified twice in MDCK cells infected at an MOI of 0.0001 in the presence of 1 μg/ml tosylsulfonyl phenylalanyl chloromethyl ketone (TPCK)-treated trypsin (Sigma-Aldrich, St. Louis, MO). Culture supernatants were harvested, clarified by low-speed centrifugation, and stored at −80°C until use. Viruses were propagated at the permissive temperature (33°C) after transfections (HEK293T) or infections (MDCK).
Two H5N1 ca reassortant vaccine candidates, caVN-Len17rg and caEG-Len17rg, were generated, with six internal genes from MDV and polybasic-cleavage site-deleted H5 HA and intact N1 NA genes from VN1203 or from EG321, respectively. To control for the impact of attenuating mutations from the caLen17-rg genome on immunogenicity, one more reassortant virus, VN-Len134rg, was generated. This variant was rescued from plasmids carrying six internal genes of Len134-rg and modified HA and intact NA genes from VN1203.
All reverse genetics-derived viruses were fully sequenced to detect spontaneous mutations or quasispecies using a BigDye Terminator v3.1 cycle sequencing kit (Applied Biosystems) and a 3130xl Genetic Analyzer (Applied Biosystems) according to the instructions of the manufacturer.
Reassortant H2N2 viruses were generated in compliance with the CDC Institutional Biosafety Committee, the Institutional Biosecurity Board, and NIH Guidelines for Research Involving Recombinant DNA. H5N1 reassortants, as well as wild-type H2N2 viruses, were handled in biosafety level 3 containment facilities. Virus titers were determined by plaque assay in MDCK cells as described previously (37) and expressed in log10 PFU/ml.
MID50 determination.
Animal study protocols were approved by the CDC Animal Care and Use Committee. Groups of 5 female BALB/c mice (The Jackson Laboratories), 6 to 8 weeks of age, were anesthetized with isoflurane and inoculated with a volume of 50 μl of virus suspension containing the appropriate infectivity dose (101 to 105 PFU) by the intranasal (i.n.) route. Mice were euthanized with an overdose of isoflurane at 3 days postinoculation (dpi). Lungs and nasal turbinates were collected and stored frozen at −80°C until used for homogenization. Tissue homogenates were prepared using a bead disruptor (Roche MagNA Lyser instrument) in 1 ml of sterile phosphate-buffered saline (PBS), and the clarified supernatants were inoculated onto MDCK cells to determine the presence of infectious virus, as an indicator of infection. Virus titers in mouse organs were measured by plaque assay in MDCK cells as described in reference 37 and expressed in log10 PFU/ml. The limit of detection was 0.6 log10 PFU/ml. The median mouse intranasal infectious dose (MID50) was calculated as the median PFU dose required to infect 50% of the animals, using three approaches: (i) MID50 based on virus detection in lung, (ii) MID50 based on virus detection in nasal turbinates, and (iii) MID50 based on virus detection in any organ (i.e., the animal was considered infected if the virus was detected in either nasal turbinates or lung).
Virus replication kinetics and neuroinvasion.
Female BALB/c mice (The Jackson Laboratories), 6 to 8 weeks of age, were inoculated i.n. with 300 MID50s of each studied virus, and the viral loads were measured in respiratory (nasal turbinates and lung) and brain tissues collected at 3 and 6 dpi. Virus titers in nasal turbinates, lung, and brain were determined as described above.
Immunogenicity and protection studies.
To assess the immunogenicity of two H5N1 ca reassortant vaccine candidates, caVN-Len17rg and caEG-Len17rg, relative to control virus wtVN-Len134rg, groups of 18 animals were inoculated with 300 MID50s intranasally, after collection of a preimmune blood sample. A second blood sample was collected 28 dpi, and on the same day, animals received a second i.n. inoculation of the same virus used for priming. A third blood sample was collected on dpi 56. Serum samples were treated with receptor-destroying enzyme (RDE) per established protocol. Serum antibodies were quantified by hemagglutination inhibition (HI) assay against both homologous and heterologous viruses using horse red blood cells (38, 39).
An indirect enzyme-linked immunosorbent assay (ELISA) using egg-grown inactivated influenza virus was used to quantify IgG antibodies to influenza virus in serum samples from mice. In brief, ELISA plates were coated with sucrose gradient-purified VN1203-PR8 or EG321-PR8 virus at a concentration of 5 μg/ml (100 μl per well) in 0.05 M carbonate-bicarbonate buffer, pH 9.6, by overnight incubation at 4°C. Sera were RDE treated for 10 h at a 1:4 dilution. Sera were then heat inactivated at 56°C for 30 min and brought to a final volume of 1:10 with PBS, pH 7.4. Plates were washed 1 time with PBS with Tween 20 (0.1%), pH 7.4 (PBST). Plates were blocked with 0.1% bovine serum albumin (BSA)-PBS (200 μl/well) at 37°C for 1 h. The blocking solution was discarded. Sera were diluted 1:1,000 in 0.01% BSA-PBST and added to each plate, followed by serial 2-fold dilutions. Each serum sample was tested in duplicate. Plates were incubated for 1 h at 37°C. The test sera were removed, and the plates were washed 3 times with PBST. Anti-mouse IgG (goat)-horseradish peroxidase (HRP) conjugate (Alpha Diagnostic Intl., Inc., San Antonio, TX) (a 1:1,000 dilution; 100 μl) was added to each well, and the plates were incubated at 37°C for 1 h. The plates were washed 4 times with PBST. O-Phenylenediamine (OPD) with H2O2 was added to each well (100 μl). The plates were incubated at 37°C for 10 min, the color change was stopped by addition of 3 N HCl, and the plates were read by a plate spectrophotometer (490 nm, 0.1 s). The limit of detectable response for the ELISA was set as optical density (OD) values above average background plus 2 standard deviations.
To assess protection, all animals were infected on dpi 60 with 100 50% lethal doses (LD50) of either wild-type (wt) VN1203 or EG321 virus by the i.n. route as described above. Four mice in each group were euthanized with isoflurane at 3 days after challenge, and respiratory (lung and nasal turbinates) and systemic (spleen and brain) organs were harvested for virus titration. The remaining five animals in each group were weighed and monitored daily until 14 dpi.
Statistical analyses.
Data were analyzed with the Statistica software (version 6.0; Statsoft Inc.). Statistical significance of differences between viral titers in organs of mice infected with different viruses was determined by the Mann-Whitney U test. Differences in log2-transformed HI titers and ELISA antibody titers were also analyzed by the Mann-Whitney U test. P values of <0.05 were considered significant.
RESULTS
Generation and characterization of H5N1 reassortant viruses.
Using an established reverse genetics system for caLen17-rg MDV and reverted Len134-rg virus, we generated three rg H5N1 reassortant viruses carrying modified HA and intact NA genes from either VN1203 or EG321 HPAI viruses (Table 1). These viruses have distinct antigenic properties as determined by two-way HI tests with ferret antisera (40). The caVN-Len17rg and caEG-Len17rg reassortants were prepared as candidate vaccine viruses for use as LAIV, while VN-Len134rg virus served as a control for the impact of Len17-specific mutations on the properties of the caVN-Len17rg reassortant.
TABLE 1.
Genome composition of H5N1 reassortant viruses used in the study
| Reassortant | HA gene | NA gene | Internal genes |
|---|---|---|---|
| caEG-Len17rg | EG321, ΔHAa clade 2.2 | EG321, intact | caLen17-rg |
| caVN-Len17rg | VN1203, ΔHA clade 1 | VN1203, intact | caLen17-rg |
| VN-Len134rg | VN1203, ΔHA clade 1 | VN1203, intact | Len134-rg |
ΔHA, polybasic cleavage site deleted.
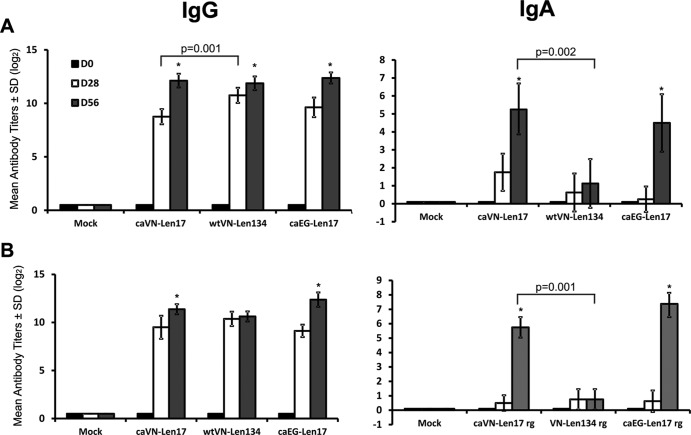
To assess the conditional replication phenotype of the candidate vaccine viruses, we used MDCK cells to compare the infectious viral titers of the rescued H5N1 reassortants to those of parental wt and ca H2N2 viruses at optimal (33°C) and restrictive (37°C and 38°C) temperatures. The two ca LAIV candidate vaccine viruses replicated efficiently at 33°C, but their replication at 38°C, and even at 37°C, was severely impaired, recapitulating the phenotype of the parental caLen17 virus (Fig. 1). In contrast, the infectious titers of the VN-Len134rg reassortant were essentially the same at all studied temperatures, resembling those of the wt Len134 virus (Fig. 1). These data indicated that the phenotypes of the H5N1 reassortant viruses were consistent with the origin of the six internal genes from either caLen17-rg or Len134-rg viruses.
FIG 1.
Infectious viral titers of parental and rg-derived H2N2 viruses, as well as H5N1 reassortants, at permissive and restrictive temperatures. Virus stocks propagated in MDCK cells at the permissive temperature (33°C) were titrated by plaque assay at the permissive or the restrictive temperatures (37°C and 38°C). The bars represent virus titers at the indicated temperature ± standard deviation (SD) (T lines).
Replication of original and rg-derived H2N2 viruses in mice.
The replication and tropism of the MDV parents of candidate vaccine viruses were assessed in the mouse model of infection (41). The reverse genetics-derived MDV caLen17-rg had an MID50 value similar to that of the original MDV caLen17 (Table 2). As was expected, cold-adapted viruses replicated better in nasal turbinates than in lung, and MID50 values were calculated based on virus detection in nasal turbinates. In contrast, wild-type H2N2 viruses replicated more efficiently in lungs than in nasal turbinates, and MID50 values were calculated from lung titers. Notably, the Len134-rg virus was somewhat less infectious for mice than was the original wt virus Len134, with a 6-fold lower MID50 value. These results could be due to lower heterogeneity in the HA sequence of the rg virus than in that of the wt virus. Mutation at codon 314 (H2 numbering) of the HA1 of caLen17 virus appeared as a result of virus adaptation to MDCK cells and therefore was not reverted during rescue of Len134-rg virus. In addition, sequencing of MDCK-grown original Len134 virus revealed a quasispecies at codon 316 of HA1 (data not shown).
TABLE 2.
Infectivity and replication of A/Leningrad/134/17/57 parent virus, its rg counterparts, and H5N1 reassortants in mice
| Virus | MID50a (log10 PFU) |
Vaccine virus doseb (log10 PFU) | Mean virus titer atc: |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 3 dpi |
6 dpi |
|||||||||
| Nasal turbinate | Lung | Total | Nasal turbinate | Lung | Braind | Nasal turbinate | Lung | Braind | ||
| caLen17 | 3.32 | ≥5.0 | 3.32 | 5.80 | 3.6 ± 0.1 | 1.0 ± 0.6 | <0.6 | 2.8 ± 0.4 | <0.6 | <0.6 |
| caLen17-rg | 3.5 | ≥5.5 | 3.50 | 5.98 | 3.4 ± 0.2 | 2.0 ± 0.1 | <0.6 | 2.5 ± 0.5 | 0.8 ± 0.5 | <0.6 |
| Len134 | 2.68 | 1.83 | 1.83 | 4.31 | 3.4 ± 1.1 | 5.1 ± 0.2 | <0.6 | 1.6 ± 0.8 | 3.8 ± 0.2 | <0.6 |
| Len134-rg | 3.37 | 2.62 | 2.62 | 5.10 | 3.8 ± 0.4 | 3.1 ± 0.2e | <0.6 | 1.2 ± 0.2 | 2.6 ± 0.5e | <0.6 |
| caEG-Len17rg | 2.17 | ≥5.0 | 2.17 | 4.65 | 2.7 ± 0.4 | 0.7 ± 0.2 | <0.6 | 0.9 ± 0.2 | <0.6 | <0.6 |
| caVN-Len17rg | 2.37 | 3.37 | 2.37 | 4.85 | 3.4 ± 0.4 | 1.1 ± 0.3 | <0.6 | 3.1 ± 0.9 | 0.7 ± 0.3 | <0.6 |
| VN-Len134rg | 2.62 | 0.83 | 0.83 | 3.31 | 2.5 ± 1.8 | 5.1 ± 0.2 | <0.6 | 0.6 ± 0.0 | 4.6 ± 0.3 | <0.6 |
To determine MID50, groups of 5 mice were infected with 101 to 105 PFU of each virus. Three days later, mice were euthanized and lung and nasal turbinates were collected and titrated by plaque assay in MDCK cells (limit of detection was 0.6 log10 PFU/ml). MID50 values were separately calculated based on virus detection in lung and nasal turbinates. Total MID50 value was calculated based on virus detection in any organ of the mice.
Infectious virus dose (in log10 PFU) used to inoculate groups of eight mice with the equivalent of 300 MID50s of each virus in a volume of 50 μl per mouse.
Nasal turbinates, lung, and brains were collected from four mice at 3 dpi and four mice at 6 dpi and titrated by plaque assay in MDCK cells. The virus titers are expressed as the mean log10 PFU/ml ± standard deviation from four mice per group (limit of detection was 0.6 log10). Tissues in which no virus was detected were given a value of 0.6 log10 to calculate the mean titer.
No virus was detected in the brain tissues of mice from any of the groups.
P < 0.05 compared to Len134 virus.
The relative replication of all H2N2 viruses in mice infected with equal mouse infectious doses of each virus (300 MID50s) confirmed that both cold-adapted viruses replicated efficiently in the upper respiratory tract with viral titers 3 days after infection of 3.4 to 3.6 log10, whereas lung titers did not exceed 2.0 log10 (Table 2). Moreover, the ca viruses were cleared from lungs of most animals by 6 dpi but were still recovered from nasal turbinates at titers of 2.5 to 2.8 log10. These data suggest a trend toward reduced replication of H2N2 ca viruses in lungs compared to that in nasal turbinates in the mouse model. In contrast to cold-adapted viruses, animals infected with wt H2N2 viruses demonstrated prolonged pulmonary replication, shedding the virus in lungs at relatively high titers, 2.6 to 3.8 log10, as late as 6 days postinoculation (Table 2). Despite similar virus titers being detected in nasal turbinates of mice infected with two wt viruses, Len134-rg virus was recovered from lung at significantly lower titers than was the Len134 original virus at both time points.
Replication of H5N1 reassortant candidate vaccine viruses in mice.
The MID50 of two LAIV candidate viruses, caVN-Len17rg and caEG-Len17rg, was approximately 10-fold lower than that of the parental virus caLen17-rg (Table 2). Importantly, these viruses, like ca H2N2 viruses, replicated in the upper respiratory tract more efficiently than in the lung, and therefore, MID50 calculations were based on virus detection in nasal turbinates. Infection of mice with 300 MID50s of ca H5N1 viruses resulted in efficient replication in the upper respiratory tract, reaching titers of 2.7 to 3.4 log10 at 3 dpi, whereas replication in lungs was severely impaired (0.7 to 1.1 log10) (Table 2). Notably, 6 days after inoculation nasal replication of the caEG-Len17rg virus was at a very low level, 0.9 log10, whereas caVN-Len17rg virus was still detected at a titer of 3.1 log10 at this site (P = 0.02). These findings suggest a contribution of viral HA and NA genes in mouse infectivity, considering that the three viruses share identical caLen17-rg virus internal genes and differ in the origin of HA and NA genes (i.e., caLen17-rg, caVN-Len17rg, and caEG-Len17rg).
Interestingly, the VN-Len134rg avian-human chimeric virus with wt internal genes had essentially an opposite pattern of virus replication in mouse organs compared to caVN-Len17rg. Although VN-Len134rg had the lowest MID50 (Table 2), animals inoculated with 300 MID50s showed the highest viral titers in lungs at both 3 and 6 days postinfection, whereas replication in the upper respiratory tract was less efficient than that of the cold-adapted counterpart (P = 0.02 at 6 dpi). These data further confirm that mutations within the internal genes of MDV caLen17 impart the attenuation phenotype to cold-adapted vaccine candidates. On the other hand, the impact of surface genes on virus replication in vivo can be noted from the comparison of VN-Len134rg (H5N1) and Len134-rg (H2N2) viruses. Indeed, the virus with HA and NA of avian origin replicated to 100-fold-higher titers in mouse lung than did the virus with human HA and NA, at both 3 and 6 dpi (Table 2).
Importantly, none of the viruses studied were detected in mouse brains at both time points. Altogether, the reduced replication of ca H5N1 vaccine candidate reassortants, as well as MDV, in the lower respiratory tract is consistent with virulence attenuation for mice (42).
Immunogenicity and protective efficacy of H5N1 vaccine candidate reassortants in mice.
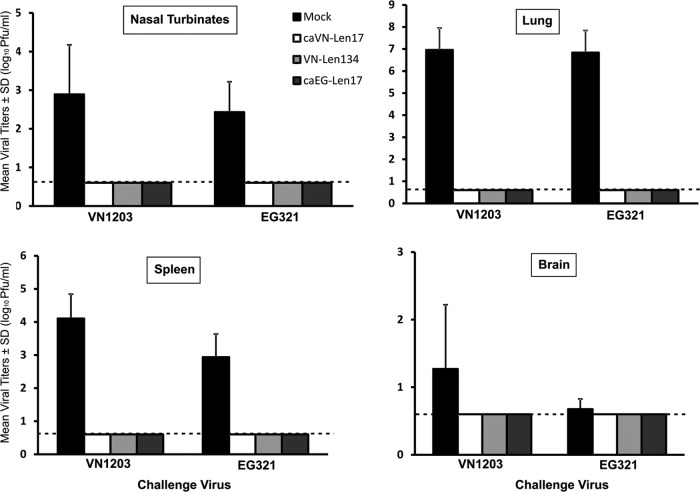
To study the performance of ca H5N1 vaccine viruses, we conducted a two-dose i.n. immunization and assessed the humoral immune response and the outcome of lethal challenge by infection with wt H5N1. One dose of either caVN-Len17rg or caEG-Len17rg H5N1 vaccine virus failed to elicit high serum HI geometric mean titers (GMT of <20, 3.6 to 4.2 log2), whereas the avian-human chimeric virus VN-Len134rg with wt internal genes was highly immunogenic even after a single dose (GMT of >50, or 5.6 log2; Fig. 2A). Nevertheless, a second i.n. immunization of mice with H5N1 vaccine viruses induced a strong immune response evidenced by serum HI titers nearing 6.0 log2 (caVN-Len17rg) and 6.7 log2 (caEG-Len17rg), indicating that boost immunization may be essential to induce the optimal levels of humoral immunity in mice. Interestingly, the caVN-Len17rg vaccine virus appeared to be more cross-immunogenic than was the caEG-Len17rg strain. Thus, EG321-specific HI antibodies were detected even after single immunization of mice with caVN-Len17rg (GMT, 3.2 log2), reaching 5.3 log2 after boost immunization. This is a threshold titer required by regulatory authorities in human clinical trials to support vaccine licensure (43) and often correlated with protection in the H5N1 model (41, 44). In contrast, caEG-Len17rg vaccine virus did not induce VN1203-specific antibodies after first immunization, and boost vaccination yielded HI titers of only 4.6 log2, which was below this threshold. Notably, comparison of caVN-Len17 reassortant virus with VN-Len134 virus, which has wt internal genes, revealed significant difference in their immunogenicity. While cold-adapted virus caVN-Len17 induced a weak response after single immunization (HI titer of 3.6 log2 with VN1203 antigen and 3.2 log2 with EG321 antigen), VN-Len134 virus was highly immunogenic even after a single dose (HI titer of 5.7 log2 with VN1203 antigen and 4.9 log2 with EG321 antigen, respectively; P ≤ 0.003). Boost immunization of mice with VN-Len134 virus resulted in the highest GMT levels of 123 (or 6.95 log2) with homologous antigen VN1203 and 80 (6.3 log2) with heterologous antigen EG321, which were comparable to the GMT level induced by two doses of caEG-Len17 vaccine virus (Fig. 2).
FIG 2.
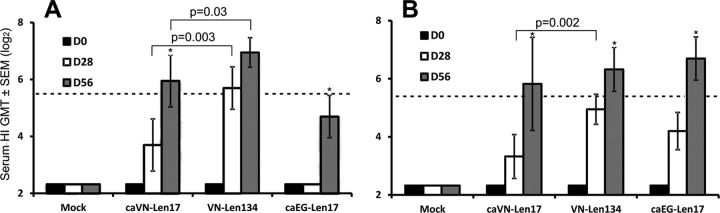
Anti-VN1203 and anti-EG321 specific HI antibody response from H5N1-vaccinated mice. Groups of 8 mice were inoculated i.n. with two doses of 300 MID50s of each virus 28 days apart or mock vaccinated. Mouse sera were collected 28 days after the first dose and 28 days after the second dose. The HI test was performed using MDCK-grown VN1203 (A) and EG321 (B) viruses. The bars represent mean serum HI titers calculated from log2-transformed HI titers of eight mice in each group ± standard deviations (T lines). HI titers below the detection limit (i.e., <10) were assigned a value of 5 (or 2.32 log2) for purposes of calculating the mean HI titer. A seroprotective level of antibody titer of ≥40 (or 5.32 log2) is indicated by the dashed line (43). Significantly higher (P < 0.05) HI titers detected after the second vaccination than after the first vaccination are indicated with an asterisk. SEM, standard error of the mean.
Serum IgG levels for wt VN1203 and EG321 in caH5N1-immunized mice revealed comparable levels of homologous antibody titers after first vaccination (8.8 and 9.1 log2 in caVN-Len17 and caEG-Len17-immunized mice, respectively) (Fig. 3). Levels of heterologous IgG titers after first vaccination were also similar (9.6 log2 for caEG-Len17-vaccinated mice against VN1203 antigen and 9.5 log2 for caVN-Len17-vaccinated mice against EG321 antigen). As observed in the HI test, VN-Len134 avian-human chimeric virus was more immunogenic than was caVN-Len17 virus after a single dose reaching homologous IgG antibody titers of ∼12 log2 (P = 0.001 compared to anti-VN1203 IgG levels after one dose of caVN-Len17) (Fig. 3). Boost immunization with cold-adapted H5N1 vaccine viruses significantly increased homologous and heterologous IgG titers, whereas for VN-Len134-immunized mice, a significant increase of IgG after boost immunization was noticed only for homologous antigen, but not for heterologous virus (P = 0.014 and P = 0.56, respectively).
FIG 3.
Serum IgG and IgA responses to VN1203 and EG321 whole-virus antigen following vaccination with ca H5N1 viruses. Groups of 8 mice were inoculated i.n. with two doses of 300 MID50s of each virus 28 days apart or mock vaccinated. Blood was collected 28 days after the first dose and 28 days after the second dose. ELISA was performed using MDCK-grown whole viruses VN1203 (A) and EG321 (B) as antigens. Shown are the mean antibody titers from eight mice in each group ± SD (T lines). Statistically significant (P < 0.05) higher antibody titers detected after the second vaccination than after the first vaccination are indicated with an asterisk.
Interestingly, the serum IgA responses to caVN-Len17 and VN-Len134 viruses after prime-boost were essentially opposite to those noted for IgG. Thus, anti-VN1203 IgA levels after two doses of caVN-Len17 virus reached 5.3 log2, whereas anti-VN1203 IgA levels after two doses of VN-Len134 virus did not exceed 2 log2 (P = 0.002). The same trend was noted for heterologous anti-EG321 IgA (5.8 log2 and 0.8 log2 after two doses of caVN-Len17 and VN-Len134 viruses, respectively; P = 0.001) (Fig. 3). Two doses of another cold-adapted H5N1 vaccine virus, caEG-Len17, also were able to induce high IgA levels to both homologous and heterologous antigens (7.4 log2 and 4.5 log2, respectively).
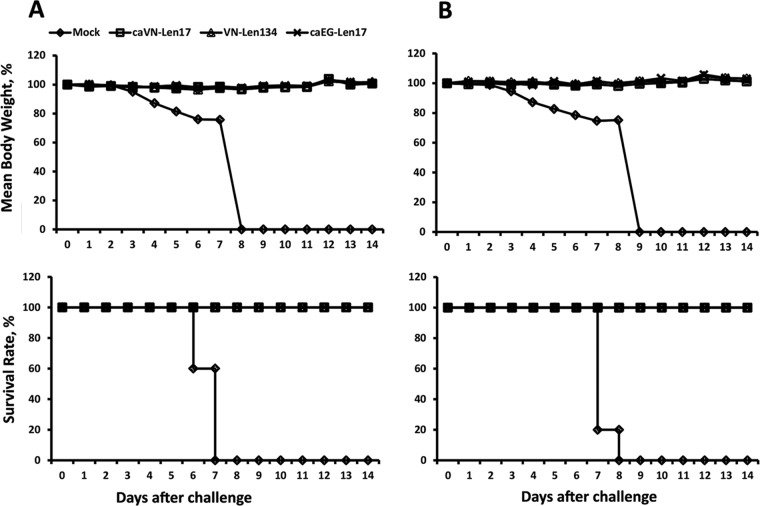
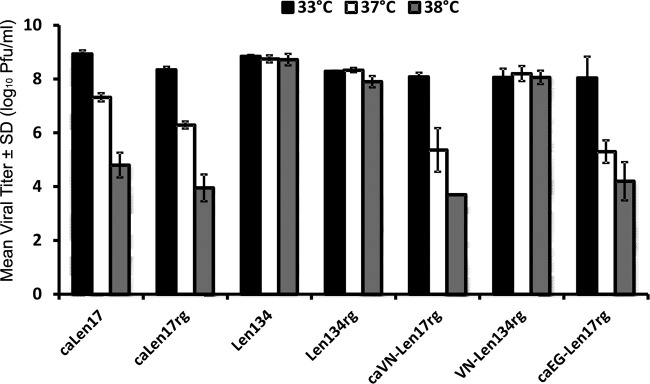
To assess homologous and cross-clade protection of H5N1 vaccine candidates, prime-boost-immunized mice from each immunization group were challenged with 100 LD50 of either VN1203 or EG321 HPAI virus by the i.n. route. As shown in Fig. 4, mice vaccinated with H5N1 LAIV candidates, as well as the VN-Len134 strain, were fully protected from infection with wt HPAI viruses. The challenge viruses were not detected in any of the tested organs, and there were no clinical signs of infection in both groups, whereas mock-immunized mice shed challenge virus at high titers in all studied organs and all mice succumbed to the infection by 7 to 8 dpi (Fig. 4 and 5). These data demonstrate the efficacy of LAIV against challenge with antigenically divergent H5N1 viruses, which correlated well with cross-reactive humoral immune responses to the vaccine viruses (Fig. 2 and 3).
FIG 4.
Infectious viral titers in vaccinated mice challenged with H5N1 homologous and heterologous viruses. Groups of 8 mice were inoculated i.n. with two doses of 300 MID50s of either caVN-Len17 or caEG-Len17 virus 28 days apart or mock vaccinated. Four weeks after the second vaccination, 4 mice from each group were challenged with 100 LD50 of either VN1203 or EG321 HPAI virus. Three days postchallenge, mouse organs were collected and homogenized, and viral titers were determined by plaque assay in MDCK cells. The virus titers are expressed as the mean log10 PFU/ml ± SD (T lines). The limit of virus detection was 0.6 log10 PFU/ml, indicated by a dashed line. Tissues in which no virus was detected were given a value of 0.6 log10 to calculate the mean titer.
FIG 5.
Weight loss and survival rates in mice challenged with H5N1 homologous and heterologous viruses. Groups of 18 mice were inoculated i.n. with two doses of 300 MID50s of each virus 28 days apart or mock vaccinated. Four weeks after the second vaccination, mice were challenged with 100 LD50 of HPAI virus VN1203 (A) or EG321 (B). Five mice per group were monitored daily for clinical signs (body weight) and survival rate for up to 14 days after challenge.
DISCUSSION
This study was designed to evaluate and characterize the immunogenic and protective attributes of H5N1 LAIV candidate vaccines derived from the Len17 master donor virus. Initial studies showed that caLen17-rg is substantially impaired in its ability to replicate in cell cultures or chicken embryos at temperatures above 35°C and can replicate efficiently at 26°C, i.e., it has a ts and ca phenotype virtually indistinguishable from that of the parental caLen17 (37) (data not shown for ca phenotype). Indeed, cold-adapted caLen17-rg virus derived by reverse genetics is phenotypically equivalent to the parental caLen17 virus with regard to replication efficiency in the upper and lower respiratory tracts of mice, as the two viruses had similar high viral titers in nasal turbinates 3 dpi (3.4 to 3.6 log10) and 6 dpi (2.5 to 2.8 log10), whereas their replication in the lower respiratory tract was 30 to 300 times less efficient than that in the upper respiratory tract. These data further support previous findings about restricted pulmonary replication of cold-adapted viruses based on the caLen17 backbone in a mouse model (45, 46), which is associated with the virus-attenuated phenotype.
In contrast to cold-adapted H2N2 viruses, wild-type Len134 virus was able to replicate in mouse lung to high titers (5.1 log10 at 3 dpi), which correlates with previous studies (45) showing that mice inoculated i.n. with wt Len134 had ∼4.5 log10 50% egg infective doses (EID50) in lungs at 3 dpi, whereas the caLen17 virus was below detection levels. We generated reverse genetics-derived Len134 virus (37), but despite similar temperature-sensitive profiles of Len134 and Len134-rg viruses in MDCK cells (Fig. 1), the latter virus replicated in mouse lung significantly less efficiently than did the authentic Len134 virus. The heterogeneous nature of Len134 virus may include a virus subpopulation with optimal replication capacity in mice that is missing in the Len134-rg virus derived from rg cDNA plasmids.
Despite the extensive use of the Len17 MDV for LAIV production, the replication of Len134 in nasal turbinates of mice in comparison to the reassortant LAIV viruses has not been reported. Here, we show that Len134 virus, as well as its rg copy, grew to similar titers in nasal turbinates at both 3 and 6 dpi. Interestingly, viral titers in nasal turbinates of all H2N2 viruses (ca and wt) were identical (3.4 to 3.8 log10) at 3 dpi, but the replication of cold-adapted viruses was more persistent than that of wt viruses (2.5 to 2.8 log10 for ca viruses versus 1.2 to 1.6 log10 for wt viruses at 6 dpi). In contrast, pulmonary replication of wt viruses was lengthier than that of ca viruses: at 6 dpi, viral titers of wt viruses in lung were 2.6 to 3.8 log10, whereas ca viruses were almost cleared at this time point (<0.6 to 0.8 log10) (Table 2). In summary, the MDV ca viruses were restricted in pulmonary replication as well as the period of replication in the upper respiratory tract relative to their parental wt viruses.
To evaluate and characterize the performance of the Len17 MDV for pandemic vaccine candidates, we derived candidate LAIV viruses from A/Vietnam/1203/2004 (H5N1) (VN1203) and Egypt/321/NAMRU-3/2007 (H5N1) (EG321). To date, there were no reports about the impact of mutations in internal genes of Len17 MDV on the virus properties in animal models, and all comparative studies of wt and ca H2N2 viruses always included viruses with slightly different HA and NA genes (i.e., nonisogenic pairs), which could contribute to viral growth characteristics.
Both caVN-Len17 and caEG-Len17 H5N1 reassortant viruses replicated in the upper respiratory tract more efficiently than in the lung, but the virus titers in nasal turbinates at 6 dpi were significantly different between caVN-Len17rg and caEG-Len17rg groups, suggesting that H5N1 surface antigens contributed to the duration of viral replication in the upper respiratory tract of mice. A recent study (20) also demonstrated the impact of different HA and NA genes on the replication characteristics of viruses derived from the cold-adapted caA/Ann Arbor/6/60 (H2N2) (caAA) master donor virus. A panel of viruses that shared the internal proteins of caAA with unique HA and NA genes of various subtypes were shown to differ in their replication efficiency in mouse lung. The ability of selected viruses to infect mice was correlated with the magnitude and quality of immune responses following vaccination. In our studies, rg viruses differing by surface genes (two groups: [i] caLen17-rg, caVN-Len17rg, and caEG-Len17rg and [ii] Len134-rg and VN-Len134rg) displayed distinct infectivity in mice. The differential infectivity of reassortant viruses for mice is determined by the HA and NA genes. Human and avian influenza viruses have different receptor specificities mediated by the HA receptors that engage the glycans in the respiratory tract (reviewed in reference 47). In vivo reassortment of avian H5N1 and human H3N2 viruses in a ferret model indicated that reassortants could be generated only in the upper respiratory tract, where both α2,3 and α2,6 types of receptors were present, whereas lung replication was detected only for H5N1 virus, consistent with the abundance of α2,3 receptors in the lower respiratory tract (48). Reassortants between avian H5N1 and human H3N2 viruses studied in a mouse model also indicated that HA and NA are the major determinants of reassortant virus tropism in mice. Thus, the wild-type A/Wyoming/3/2003 (H3N2) was undetectable in any organ studied, whereas reassortant virus bearing six internal genes from H3N2 virus and HA and NA genes from wild-type A/Thailand/16/2004 (H5N1) virus was recovered from lung and nasal turbinates at very high titers (49).
The internal genes that include the ca mutations were also major determinants of the phenotypic characteristics of caVN-Len17rg compared to VN-Len134rg parent virus, in agreement with the in vitro findings (37). Reversion of nine amino acid mutations from the cold-adapted virus dramatically shifted virus tropism in mouse respiratory organs. The cold-adapted virus replicated to higher titers and for longer times in nasal turbinates and failed to replicate efficiently in lungs, in agreement with the critical role of Len17-specific mutations in internal genes in vaccine virus attenuation.
Our analyses of the humoral immune response of mice to H5N1 reassortant viruses by HI and ELISA indicated that the antibody response to intranasal inoculation with LAIV is modulated by the functional properties of the HA and NA. Previous studies in mice and ferrets have shown that optimal protective responses to the homologous and heterologous H5 HA require two sequential immunizations with an H5N1 LAIV (44). This study demonstrated that the multiple differences in mutations leading to ca phenotypes of A/Ann Arbor/6/60 and Len17 MDV did not impact the two doses required to stimulate robust serum HI antibodies. Interestingly, two i.n. inoculations of the caVN-Len17rg virus given 28 days apart may elicit a more cross-reactive antibody response than may the caEG-Len17rg virus.
The caVN-Len17 virus induced serum IgA antibodies at a relatively high level after two immunizations. In contrast, the VN-Len134 avian-human chimeric virus was unable to stimulate serum IgA even after boost immunization. This suggests that despite extensive replication in the lower respiratory tract, the impaired viral replication in the upper respiratory tract was detrimental for the serum IgA response. Conversely, the strong IgA response to caVN-Len17 is correlated with superior replication in the nasal turbinates. Although we did not measure IgA levels in nasal secretions, a strong correlation between local and serum IgA levels was found for volunteers administered live attenuated or inactivated H1N1 or H3N1 influenza vaccine (50), which suggests the mucosal origin of systemic IgA in LAIV recipients. Interestingly, significant increases in serum IgA levels were detected in clinical trials of two pandemic LAIV (51, 52), prompting the authors to propose the use of serum IgA as a surrogate indicator of the mucosal immune response triggered by intranasal vaccine.
The two H5N1 LAIV provided extremely efficient neutralization of the homologous or heterologous clade challenge viruses, with neither being recovered from any organs of vaccinated mice, whereas mock-immunized mice had high titers of wt H5N1 viruses in all organs analyzed. Vaccinated mice remained healthy and showed no evidence of weight loss. Cross-clade protective immunity induced by caVN-Len17rg vaccine virus was previously evaluated in a ferret model (53) and compared to inactivated vaccines. Both vaccines were highly immunogenic and protective against homologous challenge following double immunization. However, LAIV demonstrated better cross-protection against EG321 wild-type virus infection than did inactivated influenza vaccines. Although the caEG-Len17rg virus was not evaluated in a ferret model, the findings reported here suggest that this candidate vaccine virus may have immunogenic and protective characteristics comparable, albeit not identical, to those of caVN-Len17rg virus in ferrets.
In summary, these data and previous studies (53) indicate that pandemic 6:2 reassortant vaccine virus based on caLen17 MDV generated through the established reverse genetics system provides candidate vaccine viruses with preclinical safety and immunogenicity profiles consistent with successful development of human vaccines for H5N1.
ACKNOWLEDGMENTS
We thank the National Institute of Hygiene and Epidemiology, Ministry of Health, People's Republic of Vietnam, and the Ministry of Health and Population, Egypt, for providing valuable specimens containing influenza virus A(H5N1).
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention or the Agency for Toxic Substances and Disease Registry.
Footnotes
Published ahead of print 19 March 2014
This paper is dedicated to the memory of Alexander “Sasha” Klimov, who inspired and supported live attenuated influenza vaccine research for decades.
REFERENCES
- 1. Peiris JS, de Jong MD, Guan Y. 2007. Avian influenza virus (H5N1): a threat to human health. Clin. Microbiol. Rev. 20:243–267. 10.1128/CMR.00037-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Abdel-Ghafar AN, Chotpitayasunondh T, Gao Z, Hayden FG, Nguyen DH, de Jong MD, Naghdaliyev A, Peiris JS, Shindo N, Soeroso S, Uyeki TM. 2008. Update on avian influenza A (H5N1) virus infection in humans. N. Engl. J. Med. 358:261–273. 10.1056/NEJMra0707279 [DOI] [PubMed] [Google Scholar]
- 3.WHO. 2014. Cumulative number of confirmed human cases of avian influenza A(H5N1) reported to WHO. World Health Organization, Geneva, Switzerland: http://www.who.int/influenza/human_animal_interface/EN_GIP_20131210CumulativeNumberH5N1cases.pdf?ua=1 Accessed January 2014 [Google Scholar]
- 4.OIE (World Organization for Animal Health). 2008. Manual of diagnostic tests and vaccines for terrestrial animals, 6th ed, vol 1, p 323–333 OIE (World Organization for Animal Health), Paris, France [Google Scholar]
- 5. Sims LD, Domenech J, Benigno C, Kahn S, Kamata A, Lubroth J, Martin V, Roeder P. 2005. Origin and evolution of highly pathogenic H5N1 avian influenza in Asia. Vet. Rec 157(6):159–164 [DOI] [PubMed] [Google Scholar]
- 6.OIE (World Organization for Animal Health). 6 June 2012. Outbreaks of highly pathogenic avian influenza (subtype H5N1) in poultry. OIE (World Organization for Animal Health), Paris, France: http://www.oie.int/fileadmin/Home/eng/Animal_Health_in_the_World/docs/pdf/graph_avian_influenza/graphs_HPAI_06_06_2012.pdf [Google Scholar]
- 7. Octaviani CP, Ozawa M, Yamada S, Goto H, Kawaoka Y. 2010. High genetic compatibility between swine-origin H1N1 and highly pathogenic avian H5N1 influenza viruses. J. Virol. 84:10918–10922. 10.1128/JVI.01140-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Leroux-Roels I, Leroux-Roels G. 2009. Current status and progress of prepandemic and pandemic influenza vaccine development. Expert Rev. Vaccines 8:401–423. 10.1586/erv.09.15 [DOI] [PubMed] [Google Scholar]
- 9. Rudenko L, Desheva J, Korovkin S, Mironov A, Rekstin A, Grigorieva E, Donina S, Gambaryan A, Katlinsky A. 2008. Safety and immunogenicity of live attenuated influenza reassortant H5 vaccine (phase I-II clinical trials). Influenza Other Respir. Viruses 2:203–209. 10.1111/j.1750-2659.2008.00064.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Svindland SC, Jul-Larsen A, Pathirana R, Andersen S, Madhun A, Montomoli E, Jabbal-Gill I, Cox RJ. 2012. The mucosal and systemic immune responses elicited by a chitosan-adjuvanted intranasal influenza H5N1 vaccine. Influenza Other Respir. Viruses 6:90–100. 10.1111/j.1750-2659.2011.00271.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Landry N, Ward BJ, Trepanier S, Montomoli E, Dargis M, Lapini G, Vezina LP. 2010. Preclinical and clinical development of plant-made virus-like particle vaccine against avian H5N1 influenza. PLoS One 5:e15559. 10.1371/journal.pone.0015559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yang P, Duan Y, Zhang P, Li Z, Wang C, Dong M, Tang C, Xing L, Gu H, Zhao Z, Liu X, Zhang S, Wang X. 2012. Multiple-clade H5N1 influenza split vaccine elicits broad cross protection against lethal influenza virus challenge in mice by intranasal vaccination. PLoS One 7:e30252. 10.1371/journal.pone.0030252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vesikari T, Forsten A, Herbinger KH, Cioppa GD, Beygo J, Borkowski A, Groth N, Bennati M, von Sonnenburg F. 2012. Safety and immunogenicity of an MF59((R))-adjuvanted A/H5N1 pre-pandemic influenza vaccine in adults and the elderly. Vaccine 30:1388–1396. 10.1016/j.vaccine.2011.12.009 [DOI] [PubMed] [Google Scholar]
- 14.WHO. 2012. Antigenic and genetic characteristics of influenza A(H5N1) and influenza A(H9N2) viruses and candidate vaccine viruses developed for potential use in human vaccines. WHO, Geneva, Switzerland: http://www.who.int/influenza/vaccines/virus/201202_h5_h9_vaccinevirusupdate.pdf [PubMed] [Google Scholar]
- 15. Cox RJ, Brokstad KA, Ogra P. 2004. Influenza virus: immunity and vaccination strategies. Comparison of the immune response to inactivated and live, attenuated influenza vaccines. Scand. J. Immunol. 59:1–15. 10.1111/j.0300-9475.2004.01382.x [DOI] [PubMed] [Google Scholar]
- 16. Lu X, Edwards LE, Desheva JA, Nguyen DC, Rekstin A, Stephenson I, Szretter K, Cox NJ, Rudenko LG, Klimov A, Katz JM. 2006. Cross-protective immunity in mice induced by live-attenuated or inactivated vaccines against highly pathogenic influenza A (H5N1) viruses. Vaccine 24:6588–6593. 10.1016/j.vaccine.2006.05.039 [DOI] [PubMed] [Google Scholar]
- 17. Belshe R, Lee MS, Walker RE, Stoddard J, Mendelman PM. 2004. Safety, immunogenicity and efficacy of intranasal, live attenuated influenza vaccine. Expert Rev. Vaccines 3:643–654. 10.1586/14760584.3.6.643 [DOI] [PubMed] [Google Scholar]
- 18. Tamura S, Tanimoto T, Kurata T. 2005. Mechanisms of broad cross-protection provided by influenza virus infection and their application to vaccines. Jpn. J. Infect. Dis. 58:195–207 [PubMed] [Google Scholar]
- 19. Jang YH, Byun YH, Lee YJ, Lee YH, Lee KH, Seong BL. 2012. Cold-adapted pandemic 2009 H1N1 influenza virus live vaccine elicits cross-reactive immune responses against seasonal and H5 influenza A viruses. J. Virol. 86:5953–5958. 10.1128/JVI.07149-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lau YF, Wright AR, Subbarao K. 2012. The contribution of systemic and pulmonary immune effectors to vaccine-induced protection from H5N1 influenza virus infection. J. Virol. 86:5089–5098. 10.1128/JVI.07205-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rudenko LG, Lonskaya NI, Klimov AI, Vasilieva RI, Ramirez A. 1996. Clinical and epidemiological evaluation of a live, cold-adapted influenza vaccine for 3-14-year-olds. Bull. World Health Organ. 74:77–84 [PMC free article] [PubMed] [Google Scholar]
- 22. Powell TJ, Strutt T, Reome J, Hollenbaugh JA, Roberts AD, Woodland DL, Swain SL, Dutton RW. 2007. Priming with cold-adapted influenza A does not prevent infection but elicits long-lived protection against supralethal challenge with heterosubtypic virus. J. Immunol. 178:1030–1038 [DOI] [PubMed] [Google Scholar]
- 23. Quan FS, Compans RW, Nguyen HH, Kang SM. 2008. Induction of heterosubtypic immunity to influenza virus by intranasal immunization. J. Virol. 82:1350–1359. 10.1128/JVI.01615-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cheng X, Eisenbraun M, Xu Q, Zhou H, Kulkarni D, Subbarao K, Kemble G, Jin H. 2009. H5N1 vaccine-specific B cell responses in ferrets primed with live attenuated seasonal influenza vaccines. PLoS One 4:e4436. 10.1371/journal.pone.0004436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rudenko LG, Slepushkin AN, Monto AS, Kendal AP, Grigorieva EP, Burtseva EP, Rekstin AR, Beljaev AL, Bragina VE, Cox N, et al. 1993. Efficacy of live attenuated and inactivated influenza vaccines in schoolchildren and their unvaccinated contacts in Novgorod, Russia. J. Infect. Dis. 168:881–887. 10.1093/infdis/168.4.881 [DOI] [PubMed] [Google Scholar]
- 26. Klimov AI, Egorov AY, Gushchina MI, Medvedeva TE, Gamble WC, Rudenko LG, Alexandrova GI, Cox NJ. 1995. Genetic stability of cold-adapted A/Leningrad/134/47/57 (H2N2) influenza virus: sequence analysis of live cold-adapted reassortant vaccine strains before and after replication in children. J. Gen. Virol. 76:1521–1525. 10.1099/0022-1317-76-6-1521 [DOI] [PubMed] [Google Scholar]
- 27. Rudenko LG, Ramirez A, Barro M, Gushchina MI, Armanda RE, Ermachenko TA, Romanova IR, Grigor'eva EP, Aleksandrova GI, Lonskaia NI. 1991. The inoculation properties of live recombinant influenza vaccine types A and B used separately and jointly in children 3 to 14. Vopr. Virusol. 36:472–474 (In Russian.) [PubMed] [Google Scholar]
- 28. Aleksandrova GI, Medvedeva TE, Polezhaev FI, Garmashova LM, Budilovskii GN. 1986. Reactogenicity, genetic stability and effectiveness of a live recombinant influenza vaccine for children designed on the base of a cold-adapted attenuation donor A/Leningrad/134/47/57. Vopr. Virusol. 31:411–414 (In Russian.) [PubMed] [Google Scholar]
- 29. Montomoli E, Khadang B, Piccirella S, Trombetta C, Mennitto E, Manini I, Stanzani V, Lapini G. 2012. Cell culture-derived influenza vaccines from Vero cells: a new horizon for vaccine production. Expert Rev. Vaccines 11:587–594. 10.1586/erv.12.24 [DOI] [PubMed] [Google Scholar]
- 30. Perdue ML, Arnold F, Li S, Donabedian A, Cioce V, Warf T, Huebner R. 2011. The future of cell culture-based influenza vaccine production. Expert Rev. Vaccines 10:1183–1194. 10.1586/erv.11.82 [DOI] [PubMed] [Google Scholar]
- 31. Liu K, Yao Z, Zhang L, Li J, Xing L, Wang X. 2012. MDCK cell-cultured influenza virus vaccine protects mice from lethal challenge with different influenza viruses. Appl. Microbiol. Biotechnol. 94:1173–1179. 10.1007/s00253-011-3860-8 [DOI] [PubMed] [Google Scholar]
- 32. Aleksandrova GI, Mikutskaia BA, Pleshanova RA, Panova NG, Smorodintsev AA. 1965. The reactive and immunogenic properties and epidemiological effectiveness of further attenuated influenza virus vaccinal strains (observed in preschool children). Vopr. Virusol. 10:67–73 (In Russian.) [PubMed] [Google Scholar]
- 33.WHO. 2009. Availability of a new recombinant H5N1 vaccine virus. World Health Organization, Geneva, Switzerland: http://www.who.int/influenza/vaccines/virus/H5N1virus26May/en/index.html [Google Scholar]
- 34.WHO. 2005. Evolution of H5N1 avian influenza viruses in Asia. Emerg. Infect. Dis. 11:1515–1521. 10.3201/eid1110.050644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hoffmann E, Neumann G, Kawaoka Y, Hobom G, Webster RG. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. U. S. A. 97:6108–6113. 10.1073/pnas.100133697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Subbarao K, Chen H, Swayne D, Mingay L, Fodor E, Brownlee G, Xu X, Lu X, Katz J, Cox N, Matsuoka Y. 2003. Evaluation of a genetically modified reassortant H5N1 influenza A virus vaccine candidate generated by plasmid-based reverse genetics. Virology 305:192–200. 10.1006/viro.2002.1742 [DOI] [PubMed] [Google Scholar]
- 37. Isakova-Sivak I, Chen LM, Matsuoka Y, Voeten JT, Kiseleva I, Heldens JG, den Bosch H, Klimov A, Rudenko L, Cox NJ, Donis RO. 2011. Genetic bases of the temperature-sensitive phenotype of a master donor virus used in live attenuated influenza vaccines: A/Leningrad/134/17/57 (H2N2). Virology 412:297–305. 10.1016/j.virol.2011.01.004 [DOI] [PubMed] [Google Scholar]
- 38.WHO. 2002. WHO manual on animal influenza diagnosis and surveillance. World Health Organization, Geneva, Switzerland: http://whqlibdoc.who.int/hq/2002/who_cds_csr_ncs_2002.5.pdf [Google Scholar]
- 39. Stephenson I, Wood JM, Nicholson KG, Charlett A, Zambon MC. 2004. Detection of anti-H5 responses in human sera by HI using horse erythrocytes following MF59-adjuvanted influenza A/Duck/Singapore/97 vaccine. Virus Res. 103:91–95. 10.1016/j.virusres.2004.02.019 [DOI] [PubMed] [Google Scholar]
- 40. Balish AL, Davis CT, Saad MD, El-Sayed N, Esmat H, Tjaden JA, Earhart KC, Ahmed LE, Abd El-Halem M, Ali AH, Nassif SA, El-Ebiary EA, Taha M, Aly MM, Arafa A, O'Neill E, Xiyan X, Cox NJ, Donis RO, Klimov AI. 2010. Antigenic and genetic diversity of highly pathogenic avian influenza A (H5N1) viruses isolated in Egypt. Avian Dis. 54:329–334. 10.1637/8903-042909-Reg.1 [DOI] [PubMed] [Google Scholar]
- 41. Matsuoka Y, Lamirande EW, Subbarao K. 2009. The mouse model for influenza. Curr. Protoc. Microbiol. Chapter 15:Unit 15G.3. 10.1002/9780471729259.mc15g03s13 [DOI] [PubMed] [Google Scholar]
- 42. Voeten JT, Kiseleva IV, Glansbeek HL, Basten SM, Drieszen-van der Cruijsen SK, Rudenko LG, van den Bosch H, Heldens JG. 2010. Master donor viruses A/Leningrad/134/17/57 (H2N2) and B/USSR/60/69 and derived reassortants used in live attenuated influenza vaccine (LAIV) do not display neurovirulent properties in a mouse model. Arch. Virol. 155:1391–1399. 10.1007/s00705-010-0719-8 [DOI] [PubMed] [Google Scholar]
- 43.Committee for Medicinal Products for Human Use. 2008. Guideline on dossier structure and content for pandemic influenza vaccine marketing authorisation application. EMEA/CPMP/VEG/4717/03-Rev.1. Committee for Medicinal Products for Human Use, European Medicines Agency, London, United Kingdom [Google Scholar]
- 44. Suguitan AL, Jr, McAuliffe J, Mills KL, Jin H, Duke G, Lu B, Luke CJ, Murphy B, Swayne DE, Kemble G, Subbarao K. 2006. Live, attenuated influenza A H5N1 candidate vaccines provide broad cross-protection in mice and ferrets. PLoS Med. 3:e360. 10.1371/journal.pmed.0030360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wareing MD, Watson JM, Brooks MJ, Tannock GA. 2001. Immunogenic and isotype-specific responses to Russian and US cold-adapted influenza A vaccine donor strains A/Leningrad/134/17/57, A/Leningrad/134/47/57, and A/Ann Arbor/6/60 (H2N2) in mice. J. Med. Virol. 65:171–177. 10.1002/jmv.2017 [DOI] [PubMed] [Google Scholar]
- 46. Desheva JA, Lu XH, Rekstin AR, Rudenko LG, Swayne DE, Cox NJ, Katz JM, Klimov AI. 2006. Characterization of an influenza A H5N2 reassortant as a candidate for live-attenuated and inactivated vaccines against highly pathogenic H5N1 viruses with pandemic potential. Vaccine 24:6859–6866. 10.1016/j.vaccine.2006.06.023 [DOI] [PubMed] [Google Scholar]
- 47. Ge S, Wang Z. 2011. An overview of influenza A virus receptors. Crit. Rev. Microbiol. 37:157–165. 10.3109/1040841X.2010.536523 [DOI] [PubMed] [Google Scholar]
- 48. Jackson S, Van Hoeven N, Chen LM, Maines TR, Cox NJ, Katz JM, Donis RO. 2009. Reassortment between avian H5N1 and human H3N2 influenza viruses in ferrets: a public health risk assessment. J. Virol. 83:8131–8140. 10.1128/JVI.00534-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Chen LM, Davis CT, Zhou H, Cox NJ, Donis RO. 2008. Genetic compatibility and virulence of reassortants derived from contemporary avian H5N1 and human H3N2 influenza A viruses. PLoS Pathog. 4:e1000072. 10.1371/journal.ppat.1000072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Clements ML, Murphy BR. 1986. Development and persistence of local and systemic antibody responses in adults given live attenuated or inactivated influenza A virus vaccine. J. Clin. Microbiol. 23:66–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Talaat KR, Karron RA, Callahan KA, Luke CJ, DiLorenzo SC, Chen GL, Lamirande EW, Jin H, Coelingh KL, Murphy BR, Kemble G, Subbarao K. 2009. A live attenuated H7N3 influenza virus vaccine is well tolerated and immunogenic in a phase I trial in healthy adults. Vaccine 27:3744–3753. 10.1016/j.vaccine.2009.03.082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Karron RA, Talaat K, Luke C, Callahan K, Thumar B, Dilorenzo S, McAuliffe J, Schappell E, Suguitan A, Mills K, Chen G, Lamirande E, Coelingh K, Jin H, Murphy BR, Kemble G, Subbarao K. 2009. Evaluation of two live attenuated cold-adapted H5N1 influenza virus vaccines in healthy adults. Vaccine 27:4953–4960. 10.1016/j.vaccine.2009.05.099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gustin KM, Maines TR, Belser JA, van Hoeven N, Lu X, Dong L, Isakova-Sivak I, Chen LM, Voeten JT, Heldens JG, van den Bosch H, Cox NJ, Tumpey TM, Klimov AI, Rudenko L, Donis RO, Katz JM. 2011. Comparative immunogenicity and cross-clade protective efficacy of mammalian cell-grown inactivated and live attenuated H5N1 reassortant vaccines in ferrets. J. Infect. Dis. 204:1491–1499. 10.1093/infdis/jir596 [DOI] [PubMed] [Google Scholar]