Abstract
Eating pathology in Seasonal Affective Disorder (SAD) may be more severe than hyperphagia during winter. Although research has documented elevated rates of subclinical binge eating in women with SAD, the prevalence and correlates of BED in SAD remain largely uncharacterized. We examined the prevalence and correlates of binge eating, weekly binge eating with distress, and BED as defined by the DSM-IV-TR in SAD. We also tested whether binge eating exhibits a seasonal pattern among individuals with BED. Two samples were combined to form a sample of individuals with SAD (N = 112). A third sample included non-depressed adults with clinical (n=12) and subclinical (n=11) BED. All participants completed the Questionnaire of Eating and Weight Patterns-Revised (QEWP-R) and modified Seasonal Pattern Assessment Questionnaire (M-SPAQ). In the SAD sample, 26.5% reported binge eating, 11.6% met criteria for weekly binge eating with distress, and 8.9% met criteria for BED. Atypical symptom severity predicted binge eating and BED. In the BED sample, 30% endorsed seasonal worsening of mood, and 26% reported a winter pattern of binge eating. The spectrum of eating pathology in SAD includes symptoms of BED, which are associated with atypical depression symptoms, but typical depression symptoms.
Keywords: seasonality, affective disorders, binge eating disorder, atypical depression
1. Introduction
Winter seasonal affective disorder (SAD) is a subtype of Major Depressive Disorder characterized by annual onset of symptoms beginning in the fall-winter months, with full remission occurring in spring (American Psychiatric Association (APA), 2013). Atypical vegetative symptoms of depression, including hyperphagia (i.e. increased appetite and food consumption) and carbohydrate craving during depressive episodes, are more common in SAD than non-seasonal depression (Rosenthal et al., 1984a; Rosenthal et al., 1987). Moreover, the severity of atypical symptoms like hyperphagia may exceed simply overeating, with some data suggesting that hyperphagia during winter depressive episodes may occur in discrete binge eating episodes (Levitan et al., 2004), during which large amounts of food are consumed accompanied by a sense of loss of control over eating during the episode (APA, 2013). Specifically, Levitan et al. (2004) reported that 24.4% of women with SAD met criteria for sub-threshold binge eating behavior. Thus, it is possible that hyperphagia in SAD may not only include elevated rates of binge eating, but may also meet the diagnostic threshold for BED. Studies have documented elevated rates of BED in other mood disorder populations (e.g. Bipolar Disorder; Wildes et al., 2008; McElroy et al., 2011), and it is clear that BED is associated with a high degree of psychiatric comorbidity (Grilo et al., 2007; Javaras et al., 2008; Grucza et al., 2007; Hudson et al., 2007). However, previous studies have not reported the percentage of individuals meeting full diagnostic criteria for BED in both men and women with SAD. Further, the demographic and clinical correlates of binge eating symptomatology and threshold BED in SAD have yet to be characterized. Doing so will help to identify those individuals vulnerable to comorbid BED and SAD, and may inform treatment approaches to both disorders.
Several clinical characteristics of SAD may be associated with risk for binge eating and BED. For instance, previous research has demonstrated that atypical vegetative symptoms predict binge eating and loss of control among individuals with Bipolar Disorder (Wildes et al., 2008), and rates of binge eating are elevated in depressed individuals with atypical symptom presentations (Kendler et al., 1996; Benazzi et al., 1999; Angst et al., 2002), suggesting that atypical vegetative symptoms and binge eating may also be correlated in SAD. Seasonality, a core feature of SAD, is another potential risk factor for binge eating and BED in SAD. Seasonality is a dimensional measure of the degree to which mood, sleep, appetite, and weight vary seasonally, and is associated with specific vulnerability for atypical vegetative symptoms like hyperphagia (Young et al., 1991; Lam et al., 2001a). SAD, eating disorders, bipolar disorder, and non-seasonal depression are all associated with weight gain in the winter (Hardin et al., 1991), suggesting that eating behavior may vary seasonally among multiple psychiatric populations. Indeed, winter weight gain experienced by individuals with SAD is partially mediated by subclinical binge eating behavior (Levitan et al., 2004). Therefore, it is possible that seasonality may be related to risk for binge eating, as was recently suggested by Davis (2013), and BED.
Prior research exploring the relationship between seasonality and eating disorders has focused on Bulimia Nervosa (BN; Lam et al., 1996). Although the prevalence of BN in SAD has not been reported, there is evidence that SAD is highly comorbid with BN; 35% of individuals with BN met criteria for a presumptive SAD diagnosis in one report (Lam et al., 1996). In addition, individuals with BN experience worsening of mood and weight gain, and an exacerbation of binge eating and purging, during the fall-winter months (Fornari et al., 1994; Blouin et al., 1992). Given that binge eating is a cardinal feature of both BN and BED, there is reason to predict that clinically significant binge eating and SAD may be related. Therefore, the primary aims of this study are to determine the prevalence and correlates of binge eating and BED in a sample of adults with SAD. To this end, two hypotheses will be tested: (1) The percentage of individuals with SAD meeting criteria for binge eating and BED will exceed that expected based population data, and (2), Seasonality and atypical symptom severity will predict risk for binge eating and BED among individuals with SAD, but typical symptom severity will not. Finally, given that symptoms of BN show a seasonal pattern, it is possible that binge eating and BED may also become exacerbated in the winter months. As such, this study included the ancillary aim to determine whether mood and BED symptoms worsen during winter in a second sample of individuals with clinical and subclinical BED.
2. Method
2.1. Procedures: study 1
2.1.1 Participants
Two samples, one from Bethesda, MD, USA, (latitude: 38.9847° N) and one from Pittsburgh, PA, USA (latitude: 40.4417° N) were combined to form a single sample of adults with SAD (N = 112). Participants were either recruited by researchers at the Uniformed Services University of the Health Sciences (USUHS; n = 64) from Bethesda, MD and the surrounding regions, or by researchers at the University of Pittsburgh (n = 48) from the Pittsburgh metro area via flyers, media advertisements, and research registry listings. Individuals were not included if they met criteria for Anorexia Nervosa or BN, or if they endorsed symptoms of Bipolar Disorder, psychosis, or substance abuse. Individuals in the Bethesda sample were recruited to participate in a clinical trial comparing the efficacy of light therapy to that of cognitive behavior therapy for SAD. For the purposes of the present study, only data collected at baseline were included in the analyses. Individuals in the Pittsburgh sample were recruited to participate in a study assessing biological, physiological, behavioral, and affective predictors of SAD using a case-control design. All procedures were approved by the Institutional Review Boards of the participating universities. All participants read and signed an informed consent document prior to participation.
2.1.2 Measures
Participants were administered the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID; First et al., 1996). To meet inclusion criteria for SAD, a diagnosis of recurrent Major Depressive Disorder, With Seasonal Pattern was required. Additionally, individuals in the SAD group met criteria for a current SAD episode based on the Structured Interview Guide for the Hamilton Rating Scale for Depression-Seasonal Affective Disorder version (SIGH-SAD; Williams et al., 1992). The SIGH-SAD includes two subscales designed to establish the presence of typical (e.g. guilt; suicidal ideation) and atypical symptoms (e.g. hyperphagia; weight gain) of depression frequently associated with SAD (see Table 1 for a list of typical and atypical symptoms). In order to meet criteria for a current SAD episode, participants must have scored a total of 20 or greater on the overall scale, at least a 15 on the typical symptoms subscale, and at least a 5 on items measuring atypical depressive symptoms according to established criteria (Terman et al., 1990).
Table 1.
Typical and atypical symptoms of depression as assessed by the Structured Interview Guide for Hamilton Rating Scale for Depression-Seasonal Affective Disorder version (SIGH-SAD).
| Typical Symptoms | Atypical Symptoms |
|---|---|
| H1. Depressed mood | A1. Social Withdrawal |
| H2. Difficulty in work and activities | A2. Weight gain |
| H3. Genital symptoms (e.g. loss of libido, menstrual disturbances) | A3. Appetite increase |
| A4. Increased eating | |
| H4. Loss of appetite/gastrointestinal symptoms | A5. Carbohydrate craving or eating |
| H5. Loss of weight | |
| H6. Insomnia early (initial insomnia) | A6. Hypersomnia |
| H7. Insomnia middle | A7. Fatigability (i.e. low energy, feelings of being heavy or leaden) |
| H8. Insomnia late (terminal insomnia) | |
| H9. Fatigue and/or aches and pains | A8. Mood and/or energy slump in the afternoon or evening |
| H10. Feelings of guilt | |
| H11. Suicidality | |
| H12. Anxiety (psychic) | |
| H13. Anxiety (somatic) | |
| H14. Hypochondriasis | |
| H15. Poor insight | |
| H16. Psychomotor retardation | |
| H17. Psychomotor agitation | |
| H18. Diurnal variation in mood | |
| H19. Depersonalization and derealization | |
| H20. Paranoid symptoms | |
| H21. Obsessional and compulsive symptoms |
Participants completed the Modified Seasonal Pattern Assessment Questionnaire (MSPAQ; Lam et al., 1996), a self-report measure of clinical and subclinical seasonal fluctuations in mood and behavior. In epidemiological SAD research, the original SPAQ (Rosenthal et al., 1984b) has been used to identify a winter or summer mood pattern and to place respondents into presumptive diagnostic categories, including winter- and summer-type SAD and subsyndromal SAD (S-SAD). The SPAQ has demonstrated high test-retest and inter-item reliability (Rohan & Sigmon, 2000). Winter mood pattern is defined as responding to the question, “At what time of year do you feel the worst?” with January, and/or February (with or without endorsement of other affected months). Conversely, a summer mood pattern is defined as responding with July and/or August (with or without endorsement of other affected months; Kasper et al., 1989). A global seasonality score (GSS) is then calculated by summing responses to six SPAQ items asking respondents to rate the degree to which mood, energy, sleep length, weight, appetite, and social activity change with the seasons. SAD criteria require that an individual meet the above winter or summer mood pattern, answer affirmatively to the question, “If you experience changes with the seasons, do you feel that these are a problem for you?” and endorse at least moderate severity on this item, and have a GSS greater than 11 (Kasper et al., 1989).
To determine the presence and severity of binge eating behavior, participants completed the Questionnaire on Eating and Weight Patterns-Revised (QEWP-R; Spitzer et al., 1993), a self-report assessment of the DSM-IV-TR research diagnostic criteria for BED (APA, 2000). Diagnostic criteria for BED as defined by the DSM-IV-TR required that binge eating (episodic overeating accompanied by loss of control) be present for at least six months and occur two or more times per week. However, based on evidence that there are few differences between individuals who binge eat once per week and those who binge eat twice per week (Garfinkel et al., 1995; Striegel-Moore et al., 1998; Striegel-Moore et al., 2000), the diagnostic criteria for BED have been revised in the fifth edition of the DSM to reflect this understanding (APA, 2013). The revised DSM-5 criteria for BED now require that binge eating only be present for three months and occur one or more times per week (APA, 2013). Because the QEWP-R focuses on binge eating symptomatology in the last six months, it is not possible to derive a BED diagnosis that is fully consistent with the revised DSM-5 criteria. However, it is possible to utilize QEWPR responses to approximate the DSM-5 criteria for BED by reducing the frequency criterion for binge eating from two or more times per week to one or more times per week. Therefore, we categorized individuals who endorsed binge eating with distress at least once per week for the duration of six months into the group “weekly binge eating with distress” in an effort to be more consistent with DSM-5 criteria for BED. We then compared the symptom presentation in the weekly binge eating with distress group to that of individuals who met criteria for subthreshold binge eating (any episodic overeating with loss of control over the amount of food consumed) in the last six months and those who met criteria for BED as defined by the DSM-IV-TR (i.e. binge eating occurring at least twice per week for the last six months that is associated with significant distress).
2.2. Procedures: study 2
2.2.1 Participants
Participants (n=23) were adults recruited by researchers at the University of Mississippi Medical Center in Jackson, MS, USA (latitude: 32.2989° N) through media advertisements for participation in a study examining behavioral and clinical features of a binge episode (Johnson et al., 2003). Interested individuals were screened using the QEWP-R (Spitzer et al., 1993). Those who received a QEWP-R-derived diagnosis of possible BN (n = 6) or no diagnosis (n = 6) were not included in the study. The QEWP-R diagnostic categories of interest included BED as defined by the DSM-IV-TR (i.e., binge eating and associated distress without compensatory purging behavior; APA, 2000) and subclinical binge eating (i.e., met a subset of DSM-IV-TR BED criteria and engaged in at least episodic overeating). Given that this was an archival sample, data were not available to retrospectively define subclinical binge eating in a way that is consistent with research indicating that loss of control is necessary to assign a diagnosis of binge eating (Neigo et al., 1997; Pratt et al., 1998; Keel et al., 2001; Mond et al., 2006; Colles et al., 2008).
2.2.2. Assessment of seasonal variation in mood and behavior
After being screened with the QEWP-R, participants completed the M-SPAQ. The question, “At what time of the year do you binge most?” was used to identify seasonality in binge eating behavior. Currently, there are no established criteria for defining a seasonal binge pattern. For the purposes of this study, a Winter Binge Pattern was defined as reporting the most frequent binge eating behavior during at least one winter month (i.e., December, January, and/or February) with or without endorsement of other affected months. Defining a Winter Binge Pattern in this way is consistent with evidence that winter worsening of binge/purge symptoms peaks in December and is highest during December, January, and February among individuals with BN (Lam et al., 1996). A Summer Binge Pattern was defined as most frequent binge eating behavior in July and/or August. Although participants were not formally evaluated for depression, the M-SPAQ was also used to estimate prevalence of SAD according to the same MSPAQ criteria (Kasper et al., 1989) described above for the Bethesda and Pittsburgh samples. The prevalence of S-SAD was also assessed. In order to meet criteria for S-SAD, an individual must have a GSS of at least 10 but deny that they experience this as a problem, or have a GSS of eight or nine and experience this as at least a mild problem (Kasper et al., 1989).
2.3. Statistical approach
Within the SAD sample, data from the QEWP-R were used to calculate the prevalence of binge eating symptomatology and BED. Three logistic regression analyses were conducted to determine whether demographic characteristics such as age, gender, ethnicity, or latitude were associated with the likelihood of meeting criteria for binge eating, BED as defined by the DSMIV-TR, and weekly binge eating with distress. To assess primary hypotheses about whether clinical characteristics such as atypical symptom severity, typical symptom severity, and GSS, were predictive of binge eating, DSM-IV-TR BED, or weekly binge eating with distress, three logistic regression analyses were conducted, one analysis per binge eating outcome. Age and gender were designated as covariates for these three analyses. To correct for possible alpha inflation due to multiple comparisons, the significance threshold was adjusted for all 3 primary analyses utilizing the Bonferroni method, yielding an adjusted p-value of 0.02 (i.e. p <0.05/m, where m = 3 comparisons). Finally, across the SAD and binge eating samples, the percentage of individuals endorsing binge eating most during each month was calculated to depict the frequency of binge eating across the year, based on responses to the question “At what time of the year do you binge most” on the M-SPAQ.
3. Results
3.1. Study 1
In the combined SAD sample, participants (N = 112) were largely middle-aged (M = 41.8, SD = 13), female (85%), and Caucasian (87%). Self-reported race/ethnicity of non-Caucasian participants included African American (6.3%), Hispanic (1.8%), Asian or Pacific Islander (2.7%), and other (0.9%). Age, ethnicity, and latitude were not associated with any binge eating outcome (Tables 2–4). Given that there were no males in the SAD sample who met criteria for BED as defined by the DSM-IV-TR, a Fisher’s exact test was conducted to statistically estimate the effect of gender on the likelihood of having BED rather than logistic regression. No effect of gender was observed for binge eating (OR (4, 109) = 1.359, p = 0.629), DSM-IV-TR BED (χ2 (1, 112) = 1.965, p = 0.355, two-tailed Fisher’s Exact Test), or weekly binge eating with distress (OR (4, 109) = 2.841, p = 0.340; Tables 2–4).
Table 2.
Study 1: Demographic and clinical characteristics of SAD participants with and without binge eating.
| Binge Eating (n = 31) | No Binge Eating (n = 81) | ORB | p | |
|---|---|---|---|---|
| Age, (years) M (SD)A | 43.6 (13.32) | 41.14 (12.90) | 1.017 | 0.328 |
| Gender, n (%) | 1.359 | 0.629 | ||
| Female | 27 (87.1) | 68 (84.0) | ||
| Ethnicity, n (%) | 0.795 | 0.546 | ||
| White | 28 (90.3) | 71 (87.7) | ||
| Recruitment site, n (%) | 0.697 | 0.437 | ||
| Pittsburgh | 15 (48.4) | 33 (40.7) | ||
| Bethesda | 16 (51.6) | 48 (59.3) | ||
| Atypical symptom score, M (SD) | 12.74 (4.25) | 10.05 (3.30) | 1.246 | 0.002 |
| Typical symptom score, M (SD) | 17.57 (5.13) | 17.37 (5.24) | 1.036 | 0.460 |
| GSS, M (SD) | 16.32 (3.61) | 14.91 (4.18) | 1.057 | 0.395 |
Age data were missing for one participant in the No Binge Eating Group
OR = odds ratio.
Table 4.
Study 1: Demographic and clinical characteristics of SAD participants with and without weekly binge eating with distress.
| Weekly Binge Eating With Distress (n = 13) |
No Weekly Binge Eating With Distress (n = 99) |
ORB | p | |
|---|---|---|---|---|
| Age, (years) M (SD)A | 38.00 (13.02) | 42.32 (12.98) | 0.976 | 0.312 |
| Gender, n (%) | 2.841 | 0.340 | ||
| Female | 12 (9.23) | 83 (83.8) | ||
| Ethnicity, n (%) | 0.884 | 0.788 | ||
| White | 11 (84.6) | 88 (88.9) | ||
| Recruitment site, n (%) | 0.690 | 0.570 | ||
| Pittsburgh | 7 (53.8) | 41 (41.4) | ||
| Bethesda | 6 (46.2) | 58 (58.6) | ||
| Atypical symptom score, M (SD) | 14.31 (6.12) | 11.03 (3.85) | 1.194 | 0.037 |
| Typical symptom score, M (SD) | 18.23 (5.70) | 17.31 (5.14) | 1.030 | 0.650 |
| GSS, M (SD) | 17.46 (3.27) | 15.02 (4.09) | 1.146 | 0.180 |
Age data were missing for one participant in the No Weekly Binge Eating With Distress Group
OR = odds ratio.
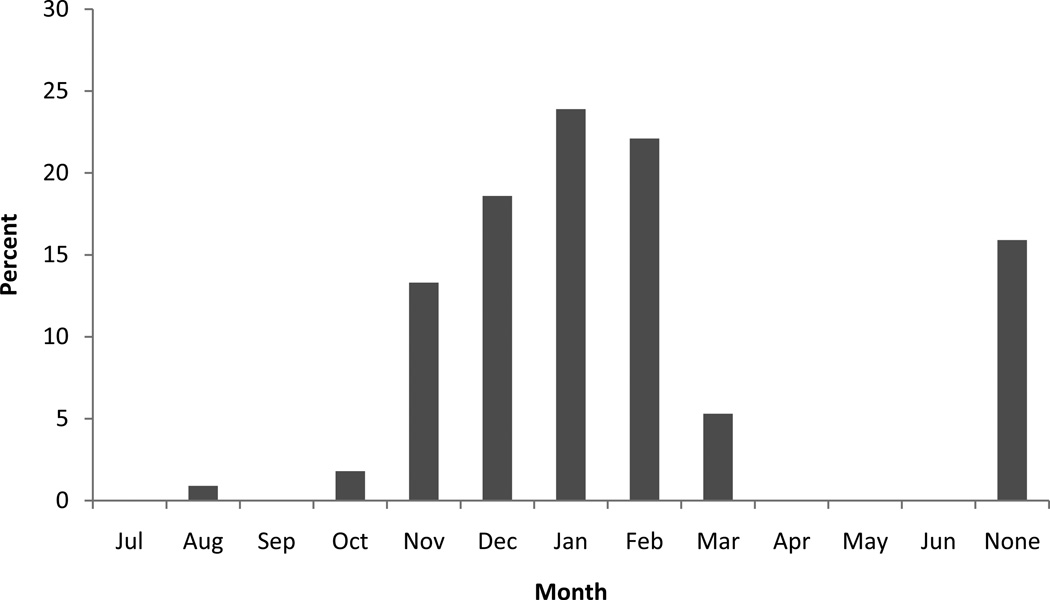
Thirty-one participants (27.4%) reported binge eating during the six months prior to participation, with 10 participants (8.9%) meeting full diagnostic criteria for BED as defined by the DSM-IV-TR. When the frequency criterion for number of binge episodes was reduced from two or more to one or more per week to be more consistent with DSM-5 diagnostic criteria for BED, 13 participants (11.6%) met criteria for clinically significant binge eating with distress. On the M-SPAQ, 30 (26.5%) individuals with SAD met criteria for a Winter Binge Pattern (i.e., increased binge frequency during December, January, and/or February). Of those with a Winter Binge Pattern, most reported increased binge eating in December (70%), January (90%), and February (83.3%). This pattern, therefore, cannot be explained solely by holiday eating, because months other than November (U. S. Thanksgiving Holiday) and December (Christmas and Hanukkah holidays) were elevated (i.e., January and February). Only one participant met criteria for a Summer Binge Pattern (i.e., increased binge frequency during July and/or August; See Figure 1), although this participant still met criteria for winter SAD.
Figure 1.
Study 1: Percentage of participants with Seasonal Affective Disorder (SAD) endorsing “binge most” by month on the Modified Seasonal Pattern Assessment Questionnaire (M-SPAQ).
A considerable proportion of individuals in the sample reported experiencing eating and weight related atypical vegetative symptoms on the SIGH-SAD, including noticeable weight gain (50.9%), increased appetite (40.2%), hyperphagia (48.2%), and increased craving and/or consumption of carbohydrates (79.5%) during winter. The severity of atypical symptoms, as indexed by the total atypical score on the SIGH-SAD (M = 11.42, SD = 4.29), was significantly associated with binge eating and with weekly binge eating with distress, but not with BED as defined by the DSM-IV-TR. Typical depressive symptoms were not predictive of binge eating, BED as defined by the DSM-IV-TR, or weekly binge eating with distress. Seasonality scores (M = 16.00, SD = 3.44) were not significantly associated with binge eating or weekly binge eating with distress, and were only marginally associated with BED as defined by the DSM-IV-TR. Tables 2–4 depict statistical associations between demographic and clinical variables and binge eating outcomes.
Follow-up analyses were conducted to determine whether removal of eating related questions from atypical symptoms scores affected any of the observed associations. After the removal of the hyperphagia question (question A4 on the SIGH-SAD) from the atypical scores, they were no longer associated with BED as defined by the DSM-IV-TR (OR (1, 111) = 1.209, p = 0.08). However, atypical scores continued to be a significant predictor of binge eating (OR (1, 111) = 1.224, p = <0.01) and weekly binge eating with distress (OR (1, 111) = 1.215, p = 0.05). No associations between atypical scores and any index of binge eating remained significant after the removal of all of the questions assessing eating related symptoms (questions A2, A4, and A5 on the SIGH-SAD).
3.2. Study 2 (Individuals with Clinical and Subclinical BED)
Participants with BED (n = 11) and subclinical binge eating symptomatology (n = 13) were combined to form a sample of binge eaters due to the small size of each group. Binge eaters were middle-aged (M = 45.3 years; SD = 10.7), female (95.8%), and obese on average (M BMI = 39.7; SD = 11.4). Participants’ race and ethnicity were not recorded in this archival sample. BED diagnosis was not associated with age (OR (1, 23) = 0.956, p = 0.260). Similar to the SAD sample, the lack of male representation in the binge eating groups necessitated the use of the Fisher’s Exact Test to statistically estimate the effect of gender on group membership (BED vs. subclinical binge eating). No statistical effect of gender was observed (χ2 (1, 23) = 1.233, p = 0.458, two-tailed Fisher’s Exact Test). The single male in the sample was in the subclinical binge eating group.
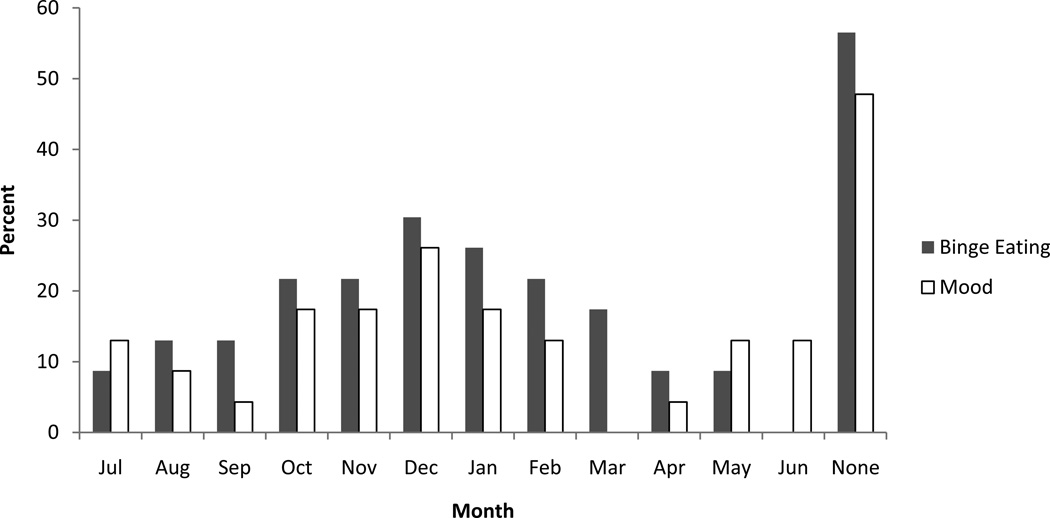
1. Seven (30%) participants reported seasonal worsening of mood. Four individuals met criteria for summer mood pattern (17%), while a winter mood pattern was observed in three individuals (13%). No participants met M-SPAQ severity criteria for SAD or S-SAD. In contrast to seasonal patterns in mood, a winter binge eating pattern (n = 6; 26%) was more common than a summer binge eating pattern (n = 0). Interestingly, all of those who endorsed a seasonal pattern to their binge eating demonstrated a pattern of more frequent binge eating during the winter months or a mixed pattern with peaks of binge eating in both summer and winter (see Figure 2). Participants endorsing a winter binge eating pattern were no more likely to meet criteria for a winter than a summer mood pattern (OR (1, 23) = 0.458, p = 0.531).
Figure 2.
Study 2: Percentage of participants with clinical and subclinical binge eating endorsing “binge most” and “feel worst” by month on the Modified Seasonal Pattern Assessment Questionnaire (M-SPAQ).
4. Discussion
The present study demonstrated that over one-quarter (27.4%) of men and women with SAD reported binge eating in the six months prior to participation, similar to the percentage reported by Levitan et al. (2004) in their sample of women with SAD. Moreover, the prevalence of BED as defined by the DSM-IV-TR in participants with SAD was 8.9%, comparable to the prevalence of BED in other psychiatric populations (e.g. Wildes et al., 2008; Grilo et al., 2007; Javaras et al., 2008). When the criteria for BED were adjusted to be more consistent with the DSM-5, the percentage of individuals with SAD meeting criteria for weekly binge eating with distress increased to 11.6%. The observation that the prevalence of BED in SAD is greater than previously appreciated and similar to the prevalence of BED in other affective disorders suggests that BED, SAD, and affective disorders generally may share some underlying susceptibility.
To identify potential factors that may be related to susceptibility to both SAD and BED, we examined the relationship between seasonality, atypical depression symptoms, and binge eating among individuals with SAD. Interestingly, severity of atypical depressive symptoms was associated with binge eating and weekly binge eating with distress, while typical depressive symptoms were not related to any index of binge eating. This distinction between atypical and typical symptoms and their prediction of BED suggests that atypical depression and BED might share a common etiology, which could be driving the documented association between MDD and BED, as well as the association between SAD and BED observed in the present study. Although hyperphagia is common to both binge eating and atypical depression, hyperphagia can occur in the absence of loss of control, a feature that is essential to the diagnosis of binge eating. Further, the most frequently reported atypical symptoms among individuals with SAD who engaged in binge eating were fatigue (96.8%), social withdrawal (93.5%), and carbohydrate craving (90.3%), followed by hypersomnia (74.2%) and hyperphagia (71.0%). Removal of the item assessing hyperphagia from atypical symptoms scores also did not eliminate the association between atypical symptoms and binge eating and weekly binge eating with distress. Therefore, the association between atypical depressive symptoms and binge eating may be explained by shared liability rather than measurement artifact, a hypothesis supported by the observation that body mass index and rates of BN are higher in co-twins of women with atypical depression (Kendler et al., 1996). It is important to note that the relationship between atypical depressive symptoms and binge eating outcomes were no longer significant after excluding items on the SIGH-SAD assessing eating related symptoms. It may be argued that this finding further supports the hypothesis that binge eating and atypical depressive symptomatology share a common etiology, insofar as changes in appetitive behavior in the context of a depressive episode appear to be related to the likelihood of meeting criteria for binge eating. Together, these findings suggest that atypical depressive symptoms may represent important risk factors for binge eating and BED in both SAD and other psychiatric populations, which could have important implications for our understanding of the etiology and treatment of both SAD and BED
Seasonality was not a significant predictor of binge eating or BED above and beyond the effects of age, gender, and atypical symptom severity. Nevertheless, more than one-quarter of participants with SAD met criteria for a Winter Binge Pattern, which might suggest that sensitivity to seasonal changes in light availability is associated with risk for binge eating and BED. Indeed, recent evidence indicates that greater seasonality significantly predicts binge eating symptomatology among generally healthy community volunteers (Davis, 2013). Further, transmission of both serotonin (Lambert et al., 2002; Praschak-Rieder et al., 2008) and dopamine (Eisenberg et al., 2010; Karson et al., 1984) vary seasonally, and have been linked to eating disorders (Frieling et al., 2010; Jimerson et al., 1997; Kaye et al., 2005), binge eating (Kuikka et al., 2001; Davis et al., 2009; Levitan et al., 2004), and SAD (Lam et al., 2001; Neumeister et al., 1998). Additional investigation of the impact of seasonality on binge eating is needed to further clarify this relationship.
Similar to BN samples, we found preliminary evidence to suggest that individuals with full and subclinical BED experience significant seasonal variation in their mood and eating patterns, even at lower latitudes. Specifically, 30% of binge eating participants endorsed seasonal worsening of mood as ‘problematic,’ compared to the population rate of 13.4% endorsing problematic seasonal worsening of mood at similar latitudes (i.e. Sarasota, FL, USA; Rosen et al., 1990). Previous research at Northern latitudes has demonstrated that a pattern of worsened bingeing and purging during the winter months was more common in individuals with BN than a summer pattern (Lam et al., 1996). In the present study, the prevalence of increased binge eating during winter (26%) is consistent with these earlier findings and supports our hypothesis that BED symptomatology may vary across the seasons.
This study has several limitations, which should be considered when interpreting the findings. First, BED was not diagnosed by clinical interview in the two SAD samples, but rather was based on self-reported symptomatology on the QEWP-R questionnaire. Research has demonstrated that agreement between the QEWP-R and structured clinical interviews for the diagnosis of BED is satisfactory (Celio et al., 2004). However, specificity of the QEWP-R was low (0.35; Celio et al., 2004), indicating that the measure generates many false-positive BED diagnoses. Therefore, it is possible that the prevalence of BED described in the present samples may be overestimated. Second, no data were collected on the number of depressive episodes experienced by participants, precluding the assessment of whether chronicity of depression was associated with binge eating or BED. This is an interesting question that warrants further attention. Third, binge eating symptomatology was reported retrospectively, and may have therefore been influenced by recall bias. Fourth, the term “binge” on the M-SPAQ was not defined for participants. This leaves open the possibility that the way in which individuals determined what constitutes a binge was not consistent with how it is defined clinically. Finally, the preliminary results of study 2 should be interpreted with caution given the small sample size (N = 24). In the future, it will be necessary to evaluate the relationship between binge eating and seasonality in a larger sample of adults diagnosed with BED, as well as at higher latitudes where seasonal variation in mood and behavior may be more prevalent.
Our data suggest that the degree of binge eating pathology associated with SAD may be more significant than previously known. For those with comorbid SAD and BED, treatment outcomes may be improved through a dual focus approach targeting both SAD and BED symptoms. Preliminary evidence suggests that light therapy may be efficacious for the treatment of BN (Braun et al., 1999; Shapiro et al., 2007) and that light exposure may reduce sensitivity to sweet tasting foods (Srivastava et al., 2013) that are often consumed during binge eating episodes (Coole, et al., 1997; Rosen et al., 1986; Yanovski et al., 1992). Future intervention studies may consider examining the efficacy of light therapy for the treatment of winter binge eating. It is possible that treatment outcome for the “seasonal” binge eater may be improved through tailoring existing interventions by providing more intense treatment coinciding with the most difficult months and identifying season-specific cues for binge eating (Rohan et al., 2004; Rohan et al., 2007). In the research setting, studies could assess for seasonal variations in binge eating and mood to account for possible confounding effects of season on treatment outcome.
Finally, high rates of co-occurrence between binge eating and SAD suggest that there may be common etiological pathways underlying susceptibility to both conditions. For example, dopamine signaling is hypothesized to affect the emergence of binge eating behavior across various disorders, including SAD (Levitan et al., 2004; Levitan, 2007) and BED (Davis et al., 2009). Dopamine is thought to participate in the reinforcement of behaviors such as eating that enhance subjective pleasure (Bello & Hajal, 2010). Individual differences in dopamine signaling may promote winter binge eating by strengthening the coupling of palatable foods such as carbohydrates to their hedonic effect. Therefore, it is possible that abnormalities in dopaminergic processing may increase risk for binge eating in both SAD (Levitan et al., 2004; Lam et al., 2001b) and BED (Davis et al., 2009).
The alarming public health costs posed by mental health comorbidities, as well as those associated with weight gain, highlight the importance of research in this area. The present study has demonstrated that the prevalence of BED in SAD is comparable to that of other psychiatric conditions and is correlated with the severity of atypical depression symptoms. These findings suggest that SAD and BED may share a common etiology, and support the idea of integrated treatment for individuals who exhibit seasonal variation in their mood and binge eating behavior. Future research should focus on further developing tailored interventions that will improve quality of life and reduce the negative health consequences associated with seasonal depression, binge eating, and weight gain. Further, exploration of shared etiological mechanisms underlying both BED and SAD may improve our understanding of these conditions.
Table 3.
Study 1: Demographic and clinical characteristics of SAD participants with and without binge eating disorder (BED) as defined by the DSM-IV-TR.
| BED (n = 10) | No BED (n = 102) | ORB | p | |
|---|---|---|---|---|
| Age, (years) M (SD)A | 35.10 (13.21) | 42.48 (12.85) | 0.957 | 0.135 |
| Gender, n (%) | 0.355C | |||
| Female | 10 (100) | 85 (83.3) | ||
| Ethnicity, n (%) | 0.996 | 0.993 | ||
| White | 8 (80.0) | 91 (89.2) | ||
| Recruitment site, n (%) | 0.532 | 0.407 | ||
| Pittsburgh | 6 (60.0) | 42 (41.2) | ||
| Bethesda | 4 (40.0) | 60 (58.8) | ||
| Atypical symptom score, M (SD) | 14.30 (6.29) | 11.13 (3.96) | 1.166 | 0.102 |
| Typical symptom score, M (SD) | 18.20 (6.44) | 17.34 (5.07) | 1.003 | 0.969 |
| GSS, M (SD) | 18.00 (2.62) | 15.04 (4.09) | 1.246 | 0.097 |
Age data were missing for one participant in the No BED Group.
OR = odds ratio.
Given that there were no males in the SAD sample who met criteria for BED as defined by the DSM-IV-TR, a Fisher’s exact test was conducted to statistically estimate the effect of gender on the likelihood of having BED rather than logistic regression. No effect of gender was observed (χ2 (1, 112) = 1.965, p = 0.355, two-tailed Fisher’s Exact Test).
Acknowledgements
This study was supported by a competitive intramural grant project number C072EJ (Uniformed Services University of the Health Sciences; Rohan, K. J.), and NIH Grant Numbers UL1 RR024153 and UL1TR000005 (University of Pittsburgh, CTSI), and NIH R03 MH096119 01A1 (Roecklein, K. A.). These sponsors had no role in the development of the protocol, execution of the study, data analysis, or manuscript preparation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: Text revision. 4th ed. Washington, DC: APA; 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: APA; 2013. [Google Scholar]
- Angst J, Gamma A, Sellaro R, Zhang H, Merikangas K. Toward a validation of atypical depression in the community: Results of the Zurich cohort study. Journal of Affective Disorders. 2002;72:125–138. doi: 10.1016/s0165-0327(02)00169-6. [DOI] [PubMed] [Google Scholar]
- Bello NT, Hajnal A. Dopamine and eating behaviors. Pharmacology Biochemistry and Behavior. 2010;97:25–33. doi: 10.1016/j.pbb.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benazzi F. Prevalence and clinical features of atypical depression in depressed outpatients: a 467-case study. Psychiatry Research. 1999;86:259–265. doi: 10.1016/s0165-1781(99)00035-9. [DOI] [PubMed] [Google Scholar]
- Blouin A, Blouin J, Aubin P, Carter J, Goldstein C, Boyer H, Perez E. Seasonal patterns in bulimia nervosa. American Journal of Psychiatry. 1992;149:73–81. doi: 10.1176/ajp.149.1.73. [DOI] [PubMed] [Google Scholar]
- Braun DL, Sunday SR, Fornari VM, Halmi KA. Bright light therapy decreases winter binge frequency in women with bulimia nervosa: A double-blind, placebo-controlled study. Comprehensive Psychiatry. 1999;40:442–448. doi: 10.1016/s0010-440x(99)90088-3. [DOI] [PubMed] [Google Scholar]
- Celio AA, Wilfley DE, Crow SJ, Mitchell J, Walsh TA. Comparison of the binge eating scale, questionnaire for eating and weight patterns-revised, and the eating disorder examination in the assessment of binge eating disorder and its symptoms. International Journal of Eating Disorders. 2004;36:434–444. doi: 10.1002/eat.20057. [DOI] [PubMed] [Google Scholar]
- Colles SL, Dixon JB, O’Brien PE. Loss of control is central to psychological disturbance associated with binge eating disorder. Obesity. 2008;16:608–614. doi: 10.1038/oby.2007.99. [DOI] [PubMed] [Google Scholar]
- Coole EA, Guss JL, Kissileff HR, Devlin MJ, Walsh BT. Patterns of food selection during binges in women with binge eating disorder. International Journal of Eating Disorders. 1997;11:111–120. doi: 10.1002/(sici)1098-108x(199709)22:2<187::aid-eat11>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Davis CA. A narrative review of binge eating and addictive behaviors: Shared associations with seasonality and personality factors. Advanced online publication. Frontiers in Psychiatry. 2013;4 doi: 10.3389/fpsyt.2013.00183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis CA, Levitan RD, Reid C, Carter JC, Kaplan AS, Patte KA, King N, Curtis C, Kennedy JL. Dopamine for “wanting” and opioids for liking: A comparison of obese adults with and without binge eating. Obesity. 2009;17:1220–1225. doi: 10.1038/oby.2009.52. [DOI] [PubMed] [Google Scholar]
- Eisenberg DP, Kohn PD, Baller EB, Bronstein JA, Masdeu JC, Berman KF. Seasonal effects on human striatal presynaptic dopamine synthesis. Journal of Neuroscience. 2010;3:14691–14694. doi: 10.1523/JNEUROSCI.1953-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams J. Biometrics Research Department. New York: New York State Psychiatric Institute; 1996. Structured clinical interview for DSM-IV axis I disorders – patient edition (SCID-I/P version 2.0) [Google Scholar]
- Fornari V, Braun D, Sunday S, Sandberg D, Matthews M, Chen I, Mandel FS, Halmi KA, Katz JL. Seasonal patterns in eating disorders subgroups. Comprehensive Psychiatry. 1994;35:450–456. doi: 10.1016/0010-440x(94)90228-3. [DOI] [PubMed] [Google Scholar]
- Frieling H, Romer KD, Scholz S, Mittelbach F, Wilhelm J, De Zwaan M, Jacoby GE, Kornhuber J, Hillemacher T, Bleich S. Epigenetic dysregulation of dopaminergic genes in eating disorders. International Journal of Eating Disorders. 2010;43:577–583. doi: 10.1002/eat.20745. [DOI] [PubMed] [Google Scholar]
- Gendall KA, Sullivan PE, Joyce PR, Carter FA, Bulik CM. The nutrient intake of women with bulimia nervosa. International Journal of Eating Disorders. 1997;21:115–127. doi: 10.1002/(sici)1098-108x(199703)21:2<115::aid-eat2>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Grilo CM, White MA, Masheb RM. DSM-IV Psychiatric disorder comorbidity and its correlates in binge eating disorder. International Journal of Eating Disorders. 2008;42:228–234. doi: 10.1002/eat.20599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grucza RA, Przybeck TR, Cloninger CR. Prevalence and correlates of binge eating disorder in a community sample. Comprehensive Psychiatry. 2007;48:124–131. doi: 10.1016/j.comppsych.2006.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardin TA, Wehr TA, Brewerton T, Kasper S, Berrettini W, Rabkin J, Rosenthal NE. Evaluation of seasonality in six clinical and two normal populations. Journal of Psychiatric Research. 1991;25:75–87. doi: 10.1016/0022-3956(91)90001-q. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javaras KN, Pope HG, Jr, Lalonde JK, Roberts JL, Nillni YI, Laird NM, Bulik CM, Crow SJ, McElroy SL, Walsh BT, Tsuang MT, Rosenthal NE, Hudson JI. Co-occurrence of binge eating disorder with psychiatric and medical disorders. Journal of Clinical Psychiatry. 2008;69:266–273. doi: 10.4088/jcp.v69n0213. [DOI] [PubMed] [Google Scholar]
- Jimerson DC, Wolfe BE, Metzger ED, Finkelstein DM, Cooper TB, Levine JM. Decreased serotonin function in bulimia nervosa. Archives of General Psychiatry. 1997;54:529–534. doi: 10.1001/archpsyc.1997.01830180043005. [DOI] [PubMed] [Google Scholar]
- Johnson WG, Roberson-Nay R, Rohan KJ, Torgrud L. An experimental investigation of DSM-IV binge-eating criteria. Eating Behavior. 2003;4:295–303. doi: 10.1016/S1471-0153(03)00028-X. [DOI] [PubMed] [Google Scholar]
- Karson CN, Berman KF, Kleinman J, Karoum F. Seasonal variation in human central dopamine activity. Psychiatry Research. 1984;11:111–117. doi: 10.1016/0165-1781(84)90094-5. [DOI] [PubMed] [Google Scholar]
- Kasper S, Wehr TA, Bartko JJ, Gaist PA, Rosenthal NE. Epidemiological findings of seasonal changes in mood and behavior: A telephone survey of Montgomery County, Maryland. Archives of General Psychiatry. 1989;46:823–833. doi: 10.1001/archpsyc.1989.01810090065010. [DOI] [PubMed] [Google Scholar]
- Kaye WH, Frank GK, Bailer UF, Henry SE, Meltzer CC, Price JC, Mathis CA, Wagner A. Serotonin alteration in anorexia and bulimia nervosa: New insights from imaging studies. Physiology & Behavior. 2005;85:73–81. doi: 10.1016/j.physbeh.2005.04.013. [DOI] [PubMed] [Google Scholar]
- Keel PK, Mayer SA, Harnden-Fischer JH. Importance of size in defining a binge episode in bulimia nervosa. International Journal of Eating Disorders. 2001;29:294–301. doi: 10.1002/eat.1021. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Eaves LJ, Walters EE, Neale MC, Heath AC, Kessler RC. The identification and validation of distinct depressive syndromes in a population-based sample of female twins. Archives of General Psychiatry. 1996;53:391–399. doi: 10.1001/archpsyc.1996.01830050025004. [DOI] [PubMed] [Google Scholar]
- Kuikka JT, Tammela L, Karhunen L, Rissanen A, Bergstrom KA, Naukkarinen H, Vanninen E, Karhu J, Lappalainen R, Repo-Tiihonen E, Tiihonen J, Uusitupa M. Reduced serotonin transporter binding in binge eating women. Psychopharmacology. 2001;155:310–314. doi: 10.1007/s002130100716. [DOI] [PubMed] [Google Scholar]
- Lam R, Goldner E, Grewal A. Seasonality of symptoms in anorexia and bulimia nervosa. International Journal of Eating Disorders. 1996;19:35–44. doi: 10.1002/(SICI)1098-108X(199601)19:1<35::AID-EAT5>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- Lam RW, Tam EM, Grewal A, Yatham LN. Effects of alpha-methyl-para tyrosine-induced catecholamine depletion in patients with seasonal affective disorder in summer remission. Neuropsychopharmacology. 2001;25:s97–s101. doi: 10.1016/S0893-133X(01)00337-2. [DOI] [PubMed] [Google Scholar]
- Lam RW, Tam EM, Yatham LN, Shiah IS, Zis AP. Seasonal depression: The dual vulnerability hypothesis. Journal of Affective Disorders. 2001;63:123–132. doi: 10.1016/s0165-0327(00)00196-8. [DOI] [PubMed] [Google Scholar]
- Lambert GW, Reid C, Kaye DM, Jennings GL, Esler MD. Effect of sunlight and season on serotonin turnover in the brain. Lancet. 2002;360:1840–1842. doi: 10.1016/s0140-6736(02)11737-5. [DOI] [PubMed] [Google Scholar]
- Levitan RD. The chronobiology and neurobiology of winter seasonal affective disorder. Dialogues in Clinical Neuroscience. 2007;9:315–324. doi: 10.31887/DCNS.2007.9.3/rlevitan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitan RD, Masellis M, Basile VS, Lam RW, Kaplan AS, Davis C, Muglia P, Mackenzie B, Tharmalingam S, Kennedey SH, Macciardi F, Kennedy JL. The dopamine-4 receptor gene associated with binge eating and weight gain in women with seasonal affective disorder: An evolutionary perspective. Biological Psychiatry. 2004;56:665–669. doi: 10.1016/j.biopsych.2004.08.013. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Frye MA, Hellemann G, Altshuler L, Leverich GS, Suppes T, Keck PE, Nolen WA, Kupka R, Post RM. Prevalence and correlates of eating disorders in 875 patients with bipolar disorder. Journal of Affective Disorders. 2011;128:191–198. doi: 10.1016/j.jad.2010.06.037. [DOI] [PubMed] [Google Scholar]
- Neumeister A, Turner EH, Matthews JR, Postolache TT, Barnett RL, Rauh M, Vetticad RG, Kasper S, Rosenthal NE. Effects of tryptophan depletion vs catecholamine depletion in patients with seasonal affective disorder in remission with light therapy. Archives of General Psychiatry. 1998;55:524–530. doi: 10.1001/archpsyc.55.6.524. [DOI] [PubMed] [Google Scholar]
- Mond J, Hay P, Rodgers B, Owen C, Crosby R, Mitchell J. Use of extreme weight control behaviors with and without binge eating in a community sample: Implications for the classification of bulimic-type eating disorders. International Journal of Eating Disorders. 2006;39:294–302. doi: 10.1002/eat.20265. [DOI] [PubMed] [Google Scholar]
- Neigo S, Pratt EM, Agras WS. Subjective or objective binge: Is the distinction valid? International Journal of Eating Disorders. 1997;22:291–298. doi: 10.1002/(sici)1098-108x(199711)22:3<291::aid-eat8>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Praschak-Rieder N, Willeit M, Wilson AA, Houle S, Meyer JH. Seasonal variation in human brain serotonin transporter binding. Archives of General Psychiatry. 2008;65:1072–1078. doi: 10.1001/archpsyc.65.9.1072. [DOI] [PubMed] [Google Scholar]
- Pratt EM, Neigo SH, Agras WS. Does the size of a binge matter? International Journal of Eating Disorders. 1998;24:307–312. doi: 10.1002/(sici)1098-108x(199811)24:3<307::aid-eat8>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Rohan KJ, Lindsey KT, Roecklein KA, Lacy TJ. Cognitive-behavioral therapy, light therapy, and their combination in treating seasonal affective disorder. Journal of Affective Disorders. 2004;80:273–283. doi: 10.1016/S0165-0327(03)00098-3. [DOI] [PubMed] [Google Scholar]
- Rohan KJ, Roecklein KA, Lindsey KT, Johnson LG, Lippy RD. A randomized controlled trial of cognitive behavioral therapy, light therapy, and their combination for seasonal affective disorder. Journal of Consulting and Clinical Psychology. 2007;75:489–500. doi: 10.1037/0022-006X.75.3.489. [DOI] [PubMed] [Google Scholar]
- Rohan KJ, Sigmon ST. Seasonal mood patterns in a Northeastern college sample. Journal of Affective Disorders. 2000;59:85–96. doi: 10.1016/s0165-0327(99)00137-8. [DOI] [PubMed] [Google Scholar]
- Rosen JC, Leitenberg H, Fisher C, Khazam C. Binge eating episodes in bulimia nervosa: the amount and type of food consumed. International Journal of Eating Disorders. 1986;5:255–267. [Google Scholar]
- Rosen LN, Targum SD, Terman M, Bryant MJ, Hoffman H, Kasper SF, Hamovit JR, Docherty JP, Welch B, Rosenthal NE. Prevalence of seasonal affective disorder at four latitudes. Psychiatry Research. 1990;31:131–144. doi: 10.1016/0165-1781(90)90116-m. [DOI] [PubMed] [Google Scholar]
- Rosenthal NE, Bradt GH, Wehr TA. Seasonal Pattern Assessment Questionnaire. Bethesda: National Institute of Mental Health; 1984. [Google Scholar]
- Rosenthal NE, Genhart M, Jacobsen FM, Skwerer RG, Wehr TA. Disturbances of appetite and weight regulation in seasonal affective disorder. Annals of the New York Academy of Sciences. 1987;499:216–230. doi: 10.1111/j.1749-6632.1987.tb36213.x. [DOI] [PubMed] [Google Scholar]
- Rosenthal N, Sack D, Gillin C, Lewy A, Goodwin F, Davenport Y, Mueller PS, Newsome DA, Wehr TA. Seasonal affective disorder: A description of the syndrome and preliminary findings with light therapy. Archives of General Psychiatry. 1984;41:72–80. doi: 10.1001/archpsyc.1984.01790120076010. [DOI] [PubMed] [Google Scholar]
- Shapiro JR, Berkman ND, Brownley KA, Sedway JA, Lohr KN, Bulik CM. Bulimia nervosa treatment: A systematic review of randomized controlled trials. International Journal of Eating Disorders. 2007;10:321–336. doi: 10.1002/eat.20372. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Yanovski S, Marcus MD. The questionnaire on eating and weight patterns-revised (QEWP-R) New York: New York State Psychiatric Institute; 1993. [Google Scholar]
- Srivastava S, Donaldson LF, Rai D, Melichar JK, Potokar J. Single bright light exposure decreases sweet taste threshold in healthy volunteers. Journal of Psychopharmacology. 2013;27:921–929. doi: 10.1177/0269881113499206. [DOI] [PubMed] [Google Scholar]
- Terman M, Terman JS, Rafferty B. Experimental design and measures of success in the treatment of winter depression by bright light. Psychopharmacology Bulletin. 1990;26:505–510. [PubMed] [Google Scholar]
- Wildes JE, Marcus MD, Fagiolini A. Prevalence and correlates of eating disorder co-morbidity in patients with bipolar disorder. Psychiatry Research. 2008;161:51–58. doi: 10.1016/j.psychres.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JBW, Link MJ, Rosenthal NE, Amira L, Terman M. Structured Interview Guide for the Hamilton Rating Scale – Seasonal affective disorder version (SIGH-SAD) New York: New York State Psychiatric Institute; 1992. [Google Scholar]
- Yanovski SZ, Leet M, Yanovski JA. Food selection and intake of obese women with binge eating disorder. American Journal of Clinical Nutrition. 1992;56:975–980. doi: 10.1093/ajcn/56.6.975. [DOI] [PubMed] [Google Scholar]