Abstract
Currently, there is no FDA-approved vaccine against Yersinia pestis, the causative agent of bubonic and pneumonic plague. Since both humoral immunity and cell-mediated immunity are essential in providing the host with protection against plague, we developed a live-attenuated vaccine strain by deleting the Braun lipoprotein (lpp) and plasminogen-activating protease (pla) genes from Y. pestis CO92. The Δlpp Δpla double isogenic mutant was highly attenuated in evoking both bubonic and pneumonic plague in a mouse model. Further, animals immunized with the mutant by either the intranasal or the subcutaneous route were significantly protected from developing subsequent pneumonic plague. In mice, the mutant poorly disseminated to peripheral organs and the production of proinflammatory cytokines concurrently decreased. Histopathologically, reduced damage to the lungs and livers of mice infected with the Δlpp Δpla double mutant compared to the level of damage in wild-type (WT) CO92-challenged animals was observed. The Δlpp Δpla mutant-immunized mice elicited a humoral immune response to the WT bacterium, as well as to CO92-specific antigens. Moreover, T cells from mutant-immunized animals exhibited significantly higher proliferative responses, when stimulated ex vivo with heat-killed WT CO92 antigens, than mice immunized with the same sublethal dose of WT CO92. Likewise, T cells from the mutant-immunized mice produced more gamma interferon (IFN-γ) and interleukin-4. These animals had an increasing number of tumor necrosis factor alpha (TNF-α)-producing CD4+ and CD8+ T cells than WT CO92-infected mice. These data emphasize the role of TNF-α and IFN-γ in protecting mice against pneumonic plague. Overall, our studies provide evidence that deletion of the lpp and pla genes acts synergistically in protecting animals against pneumonic plague, and we have demonstrated an immunological basis for this protection.
INTRODUCTION
Yersinia pestis, a Gram-negative bacterium of the Enterobacteriaceae family, is the causative agent of bubonic, septicemic, and pneumonic plague. Pneumonic plague is the deadliest form in humans, with a 100% case fatality rate (CFR) if left untreated and a 70% CFR with treatment (1). Plague was once thought to be a disease of the past, when over 200 million deaths were attributed to three pandemics, during which the plague microbe was spread by trade routes to nearly every continent (1–6). However, with the expansion of international trade routes and global climate change, Y. pestis has been classified by the World Health Organization as a reemerging human pathogen (7). In addition, the plague bacterium has gained notoriety as a biothreat agent and is now categorized as a tier 1 select agent by the Centers for Disease Control and Prevention (CDC) (8–10).
The plague bacterium is spread by the infected fleas of rodents, which can pass the infection to humans, which are accidental hosts, through a flea bite (11). The organism is endemic in a wide variety of rodents and their fleas, thus making eradication impractical (11). Y. pestis has also been known to naturally reestablish itself (possibly due to a third life cycle), which enables the bacterium to persist in a dormant state in dead hosts (5, 12). For example, outbreaks occurred in Algeria (2003) after 48 years of silence and in India (1994) after 28 years of silence, and each outbreak had an extremely high number of plague-associated deaths, as the public health sector was unprepared for an outbreak (5, 12). The availability of a vaccine as a prophylaxis would negate possible plague threats, either natural or intentional. Thus, human vaccination is highly desirable in regions of endemicity where plague is prevalent and in the case of a possible act of terrorism, as was observed during the 2001 anthrax attack through the U.S. Postal Service and the recent use of ricin in letters sent to government officials (April 2013) (9).
There is no Food and Drug Administration (FDA)-licensed vaccine against plague. Although levofloxacin was recently approved by the FDA for adults and children solely on the basis of studies of efficacy against all forms of plague in animals (13), the antimicrobials must be administered within 20 to 24 h after exposure for adequate protection (9, 14). Promising recombinant subunit plague vaccines, which are under clinical investigation, consist of a low-calcium-response V (LcrV [V]) antigen, a component of the type 3 secretion system (T3SS), as well as an effector and the capsular antigen F1. These vaccines elicit high antibody titers in rodents; however, their potential as efficacious vaccines has been debated because of varied responses in nonhuman primates (NHPs) (12–16). Specifically, African green monkeys (AGMs), in which the symptoms of plague mimic those in humans and represent an ideal model with which to study Y. pestis infection (17–21), exhibit highly varied protective responses to pneumonic plague (despite similar antibody titers). These findings suggest that antibody titers to F1 and LcrV may not correlate with protection, and, more importantly, these antigens are poorly immunogenic in humans (22).
In addition, F1-minus strains of Y. pestis that occur naturally are as virulent as the encapsulated organism; moreover, different strains of the plague bacterium possess LcrV antigens with highly divergent amino acid sequences (2, 4). Consequently, F1-LcrV (F1-V)-based vaccines may not be effective against all Y. pestis strains that exist in nature (2, 4, 5). Recent studies also indicated that a cell-mediated immune response, i.e., a response requiring CD4+, CD8+, and Th17 cells, is crucial in host protection against pneumonic plague (15, 17–19), underscoring the need for developing a live-attenuated plague vaccine. A naturally occurring Y. pestis EV76 vaccine strain lacking the pigmentation locus is currently used for immunizing people in the states of the former Soviet Union (5, 20). However, this vaccine is not approved by the FDA because of its high reactogenicity due to the presence of lipopolysaccharide (LPS) and the lack of characterization of this vaccine strain (13, 19, 20). Therefore, the goal of this study was to develop a viable live-attenuated vaccine candidate which would be able to protect mice against both pneumonic and bubonic plague by triggering humoral and cell-mediated immune responses. This candidate strain might serve as a starting point from which other virulence genes could be deleted to develop a safe and efficacious vaccine for human use. We chose to focus on the genes encoding Braun lipoprotein (lpp) and plasminogen-activating protease (pla). These two genes are located on different parts of the genome (the chromosome and the plasmid, respectively), and deletion of these genes leads to the development of a stable mutant with a minimal probability of reversion to the wild-type (WT) phenotype.
Lpp represents one of the components of the cell wall, and one copy of the gene for this protein is encoded on the 4.65-Mb chromosome of Y. pestis CO92 (4). Lpp links the peptidoglycan layer to the outer bacterial membrane, and our earlier studies have shown that its absence decreases the ability of Y. pestis to survive in macrophages (23, 24). Further, Lpp triggers Toll-like receptor 2 (TLR2), leading to an inflammatory response in the host cells (23, 25). Specifically, Lpp and LPS purified from Yersinia enterocolitica synergize to induce the production of proinflammatory cytokines both in vitro and in vivo, leading to septic shock, one of the hallmarks of a severe infection with Y. pestis (23, 25).
The pla gene is encoded on the 9.5-kb pPCP-1 plasmid at approximately 180 copies per bacterial cell (26). Two other functional proteins, namely, Pst (pesticin activity protein) and Pim (pesticin immunity protein), are also carried by pPCP-1 and provide a selective growth advantage to virulent Y. pestis bacteria (26, 27). Pla is a surface protease of the omptin family which functions by cleaving plasminogen to plasmin and by degrading α2-antiplasmin, a plasmin inhibitor (26–28). This function aids in the dissolution of fibrin clots, allowing deep tissue dissemination of the bacteria during bubonic plague (29, 30). Prevention of dissolution of fibrin deposits represents an important first step in combating Y. pestis infections by preventing bacterial dissemination and killing of the microbes through the recruitment of neutrophils and, potentially, Th17 cells via production of interleukin-6 (IL-6) by thrombin (18, 31, 32). Pla also plays a role in pneumonic plague, as the Δpla mutant fails to colonize lung tissue in high numbers (31–34).
In an earlier study, we showed that the Δlpp single mutant was attenuated in mouse models of both bubonic and pneumonic plague (23). We also observed that curing of the pPCP-1 plasmid from the Δlpp isogenic mutant resulted in a highly attenuated disease phenotype for pneumonic plague in a mouse model (35). These studies led us to construct a double isogenic mutant, the Δlpp Δpla mutant, to directly discern the extent of bacterial attenuation by targeting two genes without affecting the products of other genes carried by the pPCP-1 plasmid. Consistent with our hypothesis, deletion of both the lpp and pla genes led to synergistic attenuation of the virulence of the double mutant in evoking pneumonic plague, and the double mutant triggered protective humoral and cell-mediated immunity in mice, characteristics which represent the hallmarks of an effective vaccine.
MATERIALS AND METHODS
Bacterial strains and plasmids.
All of the bacterial strains and plasmids used in this study are listed in Table 1. Y. pestis was grown in heart infusion broth (HIB; Difco, Voigt Global Distribution Inc., Lawrence, KS) at 26 to 28°C with constant agitation (180 rpm). For growth on a solid surface, Y. pestis was grown on either HIB agar or 5% sheep blood agar (SBA) plates (Teknova, Hollister, CA). Luria-Bertani (LB) medium was used for growing recombinant Escherichia coli at 37°C with agitation. All of our studies were performed in a tier 1 select agent biosafety level 2 laboratory located in the Galveston National Laboratory.
TABLE 1.
Bacterial strains and plasmids used in this study
| Strain or plasmid | Description and source | Reference or source |
|---|---|---|
| Strains | ||
| Y. pestis | ||
| CO92 | Virulent WT Y. pestis biovar Orientalis strain isolated in 1992 from a fatal pneumonic plague case and naturally resistant to polymyxin B | 36, 37 |
| Δlpp CO92 | lpp gene deletion mutant of Y. pestis CO92 | 23 |
| Δpla CO92 | pla gene in-frame deletion mutant of Y. pestis CO92 | This study |
| Δlpp Δpla CO92 | lpp and pla gene double deletion mutant of Y. pestis CO92 | This study |
| CO92(pBR322) | WT Y. pestis transformed with pBR322 (Tcs) | 35 |
| CO92 Δlpp(pBR322) | CO92 Δlpp mutant transformed with pBR322 (Tcs) | 35 |
| CO92 Δpla(pBR322) | CO92 Δpla mutant transformed with pBR322 (Tcs) | This study |
| CO92 Δlpp Δpla(pBR322) | CO92 Δlpp Δpla double mutant transformed with pBR322 (Tcs) | This study |
| CO92 Δpla (pBR322Ypla) | Y. pestis pla deletion mutant complemented via plasmid pBR322Ypla (Tcs) | This study |
| Δlpp Δpla (pBR322Ypla) | Y. pestis lpp and pla double deletion mutant complemented via plasmid pBR322Ypla (Tcs) | This study |
| E. coli SM10 | Strain containing the λpir gene (lysogenized with λpir phage) designed for cloning and propagation of a plasmid with the R6K origin of replication | 38 |
| Plasmids | ||
| pBR322 | Cloning vector for complementation (Tcr Apr) | GE Healthcare |
| pKD13 | Template plasmid for PCR amplification of the Kmr gene cassette flanked by FLP recombinase recombination target sites | 39 |
| pFlp2 | Vector that produces the FLP recombinase to remove the Kmr gene cassette from the mutant | 40 |
| pDMS197 | Suicide vector with a conditional R6K origin of replication (ori) and a levansucrase gene (sacB) from Bacillus subtilis used for homologous recombination | 41 |
| pBR322Ypla | Recombinant plasmid containing the pla gene-coding region and its putative promoter in vector pBR322 used to complement the Δpla mutant of Y. pestis (Tcs) | This study |
| pDMS197plaUDKm | Suicide vector pDMS197-based recombinant plasmid containing the Y. pestis CO92 pla gene up- and downstream flanking DNA fragments with the Kmr cassette used for homologous recombination | This study |
Restriction endonucleases and T4 DNA ligase were obtained from Promega (Madison, WI). Advantage cDNA PCR kits were purchased from Clontech (Palo Alto, CA). All digested plasmid DNA or DNA fragments from agarose gels were purified by using QIAquick kits (Qiagen, Inc., Valencia, CA).
Construction of Δpla single and Δlpp Δpla double in-frame deletion mutants of Y. pestis CO92.
The Δpla single and Δlpp Δpla double in-frame deletion mutants were generated by homologous recombination (23). On the basis of the genome sequence of WT CO92 (GenBank accession number NC_003143), the up- and downstream DNA sequences flanking the pla gene were PCR amplified using the primer sets Plaup5-Plaup3 and Pladn5-Pladn3, respectively (Table 2). A kanamycin resistance (Kmr) gene cassette with flippase (FLP) recombinase recognition target sites at both ends was PCR amplified from plasmid pKD13 using a specific primer set, Km5-Km3 (Tables 1 and 2). The above-mentioned DNA fragments were ligated together through their compatible restriction enzyme sites (Table 2). The resulting DNA fragment containing the pla upstream flanking region, the Kmr gene cassette, and the pla downstream flanking region was subsequently cloned into the pDMS197 suicide vector at the appropriate restriction enzyme sites (39) using E. coli SM10 (Table 1). The recombinant plasmid pDMS197plaUDKm (Table 1) was then transformed by electroporation (Genepulser Xcell; Bio-Rad, Hercules, CA) (23) into WT CO92 or the Δlpp single mutant of CO92, generating the Δpla single mutant and the Δlpp Δpla double mutant, respectively. The transformants were plated onto HIB agar plates containing 5% sucrose and 100 μg/ml kanamycin. The Kmr colonies were PCR screened using primer sets Pla5-Pla3 and Up5-Dn3 (Table 2). The colonies showing genomic replacement of the pla gene with the Kmr gene cassette (intermediate form) were transformed with the plasmid pFlp2, which expresses the gene encoding FLP recombinase, to remove the Kmr gene cassette. The plasmid pFlp2 was then cured with 5% sucrose; the final Δpla mutants were sensitive to kanamycin (Kms) and free of plasmid pFlp2. An in-frame deletion of the pla gene was further confirmed by genomic sequencing with the primer Spla (Table 2).
TABLE 2.
Sequences of primers used in this study
| Primer(s) | Primer sequence(s) (5′–3′)a | Purpose |
|---|---|---|
| Plaup5-Plaup3 | AATGAGCTCCGGCCAGGCAGATCCACATAATG (SacI), ATCGGATCCTCATTAGACACCCTTAATC (BamHI) | PCR amplification of the upstream flanking fragment of the pla gene of Y. pestis CO92 |
| Pladn5-Pladn3 | ATCGAATTCTGAAAAATACAGATCATATC (EcoRI), TTCGGTACCTATAACTCGTAGGTTATATTG (KpnI) | PCR amplification of the downstream flanking fragment of the pla gene of Y. pestis CO92 |
| Km5-Km3 | ATTCCGGGGATCCGTCGACC (BamHI), CTTGAATTCTGTAGGCTGGAGCTGCTT (EcoRI) | PCR amplification of the Kmr gene cassette with FLP recombinase recognition target sites at both ends from plasmid pKD13 |
| Pla5-Pla3 | TTACAGTTGCAGCCTCCACC, ATTCTTATCAATGGTCTGAG | PCR amplification of the coding region of the pla gene of Y. pestis CO92 |
| Up5-Dn3 | TCCATCTCCGTATCAATCGG, TTGCCGTGATCGCGCTGAAC | Generation of the pla mutants of Y. pestis CO92; the pla mutant verification primers were located on the bacterial chromosome outside the flanking DNA sequences |
| Spla | CCACCGTTTCTTATGTGAGC | Confirmation of the in-frame deletion of the pla gene by chromosomal DNA sequencing; the primers were located upstream of the pla gene |
| Cplaup-Cpladn | ATGCATGCGGCTCAACGCTCGTTGTCG (SphI) ACGTCGACTCAGAAGCGATATTGCAGAC (SalI) | Amplification of the pla gene and its promoter region for the complementation studies |
Underlining indicates the restriction enzyme sites in the primers, and the restriction enzymes are indicated in parentheses.
Complementation of Δpla mutant strains of Y. pestis CO92.
The coding region of the pla gene, along with its promoter, was PCR amplified using primers Cplaup and Cpladn (Table 2), and the amplified DNA fragment was cloned into the pBR322 plasmid vector, thus generating the recombinant plasmid pBR322Ypla. The pBR322Ypla recombinant plasmid was then transformed into Y. pestis Δpla single mutant and Δlpp Δpla double mutant strains via electroporation (Table 1) (23, 35). The complemented Y. pestis Δpla(pBR322Ypla) and Δlpp Δpla(pBR322Ypla) strains were sensitive to tetracycline due to inactivation of the tetracycline resistance (Tcr) gene on the plasmid. As appropriate controls, a tetracycline-susceptible (Tcs) variant of the pBR322 vector (35) was also electroporated into WT CO92 and the Δpla single mutant and Δlpp Δpla double mutant of Y. pestis (Table 1).
In vitro characterization of Y. pestis CO92 Δlpp Δpla double mutant. (i) Functionality of the T3SS.
The low calcium response (LCR) is a distinctive trait of the Yersinia T3SS in which effectors designated Yersinia outer membrane proteins (Yops), such as YopE and YopH, are secreted in response to a low calcium signal. To demonstrate the functionality of the T3SS, the secretion of Yops from Y. pestis cultures (WT CO92 as well as Δlpp, Δpla, and Δlpp Δpla mutants of CO92) was induced by the addition of EGTA (Sigma-Aldrich, St. Louis, MO), as we previously described (23, 35). Briefly, aliquots (500 μl) from different cultures were removed after 5 min of EGTA addition, followed by separation of bacterial cells from the supernatants. The presence of Yops in cell pellets and supernatants was analyzed by immunoblotting using antibodies to YopE (Santa Cruz Biotechnology, Santa Cruz, CA) and YopH (Agrisera, Stockholm, Sweden) (23, 35).
(ii) Serum resistance and membrane blebbing.
WT CO92 and its Δlpp Δpla double mutant were incubated with serum pooled from 5 naive mice. Heat-inactivated serum and phosphate-buffered saline (PBS) served as controls. After 1 h of incubation at 37°C, the number of surviving bacteria (number of CFU) in each sample was determined by serial dilution and plating on SBA plates, as we previously described (23, 35).
To evaluate membrane integrity, both WT CO92 and the Δlpp Δpla double mutant were grown to exponential phase at 28°C (optical density at 600 nm [OD600], 0.8). The cells were washed, pelleted, fixed, and subjected to transmission electron microscopy (42).
(iii) Measurement of gentamicin MIC.
The MICs of gentamicin for WT Y. pestis CO92 and its Δlpp Δpla double mutant were determined by using the Etest (bioMérieux Inc., Durham, NC). Briefly, the overnight cultures were diluted (1:4) with fresh HIB and continued to grow at 28°C for 2 h (OD600, 0.6). The bacterial cultures were then spread evenly onto SBA plates, and the Etest strips with predefined gentamicin concentrations (range, 0.016 to 256 μg/ml) were placed in the center of the plates, which were then incubated for 48 h at 28°C or 37°C, and the MICs were recorded.
Survival of WT Y. pestis CO92 and its mutant strains in murine macrophages.
RAW 264.7 cells were infected with WT CO92 and its mutant strains (the Δlpp, Δpla, and Δlpp Δpla mutants) at a multiplicity of infection (MOI) of 1. The infected macrophages were incubated at 37°C with 5% CO2 for 30 min, followed by 1 h of treatment with 100 μg/ml gentamicin to kill extracellular bacteria. The surviving bacteria inside the macrophages were enumerated immediately after the gentamicin treatment (0-h time point) and 4 h later by serial dilution and plating, as we previously described (35, 43).
Animal studies.
All of the mouse studies were performed in an animal biosafety level 3 facility under a protocol approved by the University of Texas Medical Branch (UTMB) Institutional Animal Care and Use Committee. Six- to 8-week-old female Swiss Webster mice were purchased from Taconic Laboratories (Germantown, NY) and challenged with WT Y. pestis CO92 and the Δlpp, Δpla, or Δlpp Δpla mutant strain by either the subcutaneous (s.c.) or intranasal (i.n.) route to induce bubonic and pneumonic plague, respectively, as we previously described (23). The inoculation of the bacterial suspension into the nares leads to animal inhalation of bacterial droplets, resulting in the development of pneumonic plague. To generate survival curves, mice were assessed for mortality over a period of 30 days. For histopathology, cytokine/chemokine analysis, enzyme-linked immunosorbent assay (ELISA) for antibody isotyping, and bacterial dissemination, the sera and organs of the animals were harvested at the time points indicated below.
Histopathology and bacterial dissemination.
Mice infected with 5 × 105 CFU (representing 1,000 50% lethal doses [LD50s] of WT CO92, where 1 LD50 is equal to 500 CFU) of WT CO92, the Δlpp and Δpla single mutants, and the Δlpp Δpla double mutant strain by the i.n. route were euthanized at 2, 6, 8, and 14 days postinfection (p.i.). Portions of the lungs, liver, and spleen from 3 representative animals were removed and immersion fixed in 10% neutral buffered formalin (23, 35). The tissues were sectioned at 5 μm, mounted on glass slides, stained with hematoxylin-eosin (H&E), and evaluated by light microscopy in a blinded fashion. Tissue lesions were scored on the basis of a severity scale, which correlated with estimates of lesion distribution and the extent of tissue involvement (minimal, 2 to 10%; mild, >10 to 20%; moderate, >20 to 50%; severe, >50%), as previously described (23, 35). Bacteria consistent with Y. pestis infection were present in some sections, although bacterium-specific staining was not performed.
At the indicated time points, various tissues (lungs, liver, spleen) and blood were evaluated for the dissemination of bacteria (23). The bacterial colonies were counted to determine the numbers of CFU per organ or per ml (for blood).
Measurement of antibodies and cytokines/chemokines in sera.
Concurrently with the collection of tissues for histopathology and determination of bacterial dissemination from infected mice, blood samples were drawn on days 2, 4, 8, and 16 from mice injected with the bacteria by the s.c. route and on days 2, 4, 6, and 14 from those inoculated by the i.n. route. Uninfected naive mice served as the control group. The sera were extracted and filtered using Costar 0.22-μm-pore-size centrifuge tube filters from Corning Inc. (Corning, NY). The cytokine/chemokine levels in the serum samples were analyzed as we previously described (35, 43).
Specific antibody responses (IgG and various isotypes) to WT CO92 (whole bacteria) as well as to the F1-LcrV (F1-V) antigens of CO92 were measured by ELISA. Briefly, ELISA plates were coated with either F1-V (1 ng/ml; BEI Resources, Manassas, VA) or the whole plague bacterium overnight at 4°C. For preparing the latter, the WT CO92 culture was grown overnight at 28°C in HIB. The culture was diluted, and the growth temperature was shifted to 37°C until an OD600 of 0.8 was reached. This shift in the temperature allowed F1 production and T3SS induction (23). The culture was then resuspended to a concentration of 5 × 109 CFU/ml and used to coat plates treated with poly-l-lysine (10 μg/ml). A serial dilution (1:5) of serum was made to evaluate antibody titers, and a positive antibody titer was defined as the inverse of the highest serum dilution giving an absorbance reading of ≥0.2. Antibody classes and IgG isotypes were also examined by using specific isotype secondary antibodies, as we previously described (44).
T cell responses.
A total of 60 mice were challenged by the i.n. route with 250 CFU of WT CO92 or its Δlpp Δpla double mutant (30 mice per group). At 14, 21, and 60 days p.i., spleens were harvested from 5 mice in each infected group, and T cells were isolated from each animal by using a CD3ε MicroBead kit for magnetically assisted cell separation (Miltenyi Biotec GmbH, Bergisch Gladbach, Germany). T cells isolated from uninfected mice were used as controls at each time point. All isolated T cells were incubated ex vivo with γ-irradiated antigen-presenting cells (APCs) from naive mice that either were pulsed with heat-killed WT CO92 or remained unpulsed. The proliferation of T cells was measured by their ability to incorporate [3H]thymidine, as we previously described (43). The culture supernatants were collected at 48 h and subjected to a multiplex assay with a Milliplex assay kit (Millipore), which detected 6 cytokines/chemokines.
The T cell subsets producing gamma interferon (IFN-γ) and tumor necrosis factor alpha (TNF-α) were measured by flow cytometry. Briefly, T cells from animals infected with WT CO92 or the Δlpp Δpla double mutant or uninfected mice were cultured as described above with pulsed APCs in 24-well plates at 37°C for 5 days. Cells were treated with ionomycin (1 μg/ml) and phorbol 12-myristate 13-acetate (PMA; 10 μg/ml) and 2 h later were incubated with brefeldin A (1 μg/ml) for 3 h to accumulate intracellular cytokines. The T cells were then surface stained with monoclonal anti-mouse CD4-Pacific Blue (BioLegend, San Diego, CA), viable dye allophycocyanin-Cy7 (Molecular Probes, Eugene, OR), and anti-mouse CD8-phycoerythrin (PE) (BioLegend) for 30 min in the dark at 4°C. Subsequently, the T cells were permeabilized with a staining buffer set (eBioscience, San Diego, CA) and stained with IFN-γ–fluorescein isothiocyanate (BioLegend) and TNF-α–PE–Cy7 (BioLegend) for 30 min. The cells were acquired on a flow cytometer (LSR II Fortessa; UTMB Core) and analyzed by using fluorescence-activated cell sorting (FACS) Diva software.
Statistical analyses.
Whenever appropriate, analysis of variance (ANOVA) with the Bonferroni correction or Tukey's post hoc test with one-way ANOVA was employed for data analysis. We used Kaplan-Meier survival estimates for animal studies, and P values of ≤0.05 were considered significant.
RESULTS
In vitro characterization of Δlpp and Δpla single mutants and Δlpp Δpla double mutants of Y. pestis CO92.
An in-frame deletion of the pla gene from WT bacteria and the Δlpp mutant of CO92 resulting in the Δpla single mutant and the Δlpp Δpla double mutant, respectively, was ascertained by DNA sequencing of the flanking regions of the target gene. The growth rate of the mutants compared to that of WT CO92 did not show any defects (data not shown). The deletion of the pla gene from multiple copies of the pPCP-1 plasmid as well as that of the lpp gene from the chromosome of the mutants was confirmed by PCR and Western blot analysis (data not shown).
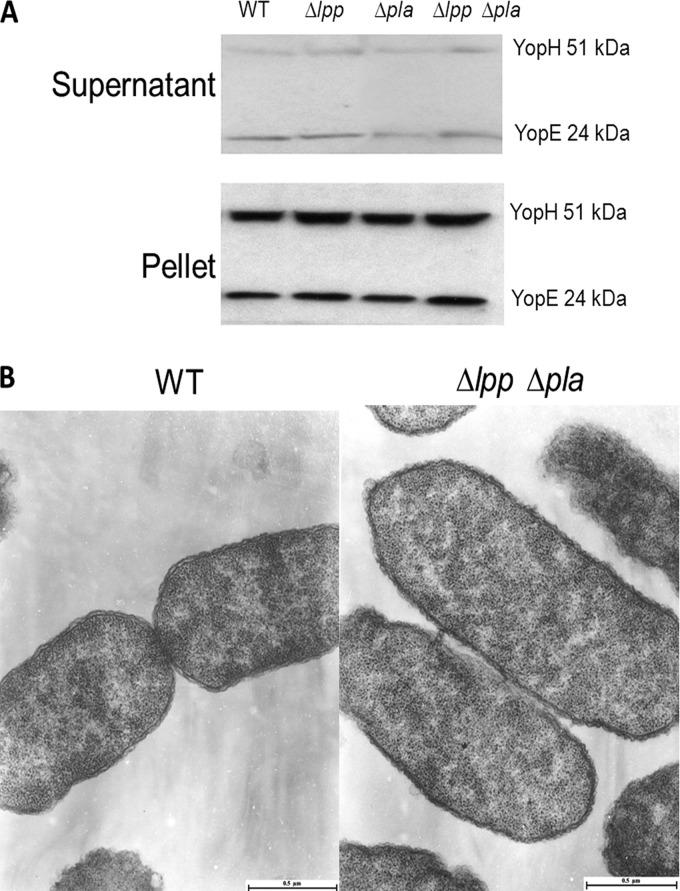
The secretion and translocation of Yops through the T3SS represent a key virulence mechanism of Y. pestis, which is tightly regulated. Under a high-calcium environment (e.g., HIB medium), the secretion and translocation of Yops are restricted but triggered rapidly when bacteria come in contact with the eukaryotic cells or when calcium is chelated by the addition of EGTA (43, 45, 46). To determine whether deletion of the above-mentioned genes affected any other phenotype(s) which could compromise the virulence of the mutant, we specifically evaluated the functionality of the T3SS by measuring the secretion of T3SS effectors (YopE and YopH) via Western blot analysis. As shown in Fig. 1A, similar levels of these effectors were noted in the bacterial pellet and the supernatant across all tested strains upon addition of EGTA. We also examined cell membrane integrity by performing transmission electron microscopy and found no indication of membrane blebbing when comparing WT CO92 with its Δlpp Δpla double mutant. However, in some bacterial mutant cells, the outer membrane appeared to be vesiculated along the surface (Fig. 1B). Likewise, it was noted that, in comparison with WT CO92 cells, some Δlpp Δpla double mutant cells had a tighter periplasmic space which seemed to be filled with electron-dense material.
FIG 1.
T3SS function and transmission electron microscopy. WT CO92 and the Δlpp, Δpla, and Δlpp Δpla mutants were grown overnight and then diluted 1:20 with fresh HIB. The cultures were grown for an additional 3 h at 28°C and then shifted to 37°C for 2 h. The secretion of YopE and YopH was induced by the addition of 5 mM EGTA. Culture supernatants and pellets were collected 5 min after EGTA addition. (A) The presence of YopE and YopH in the samples was analyzed by the use of antibodies to YopE and YopH. To evaluate membrane integrity, both WT CO92 and the Δlpp Δpla double mutant were grown to exponential phase at 28°C (OD600, 0.8). The cells were washed, pelleted, fixed, and subjected to transmission electron microscopy (B).
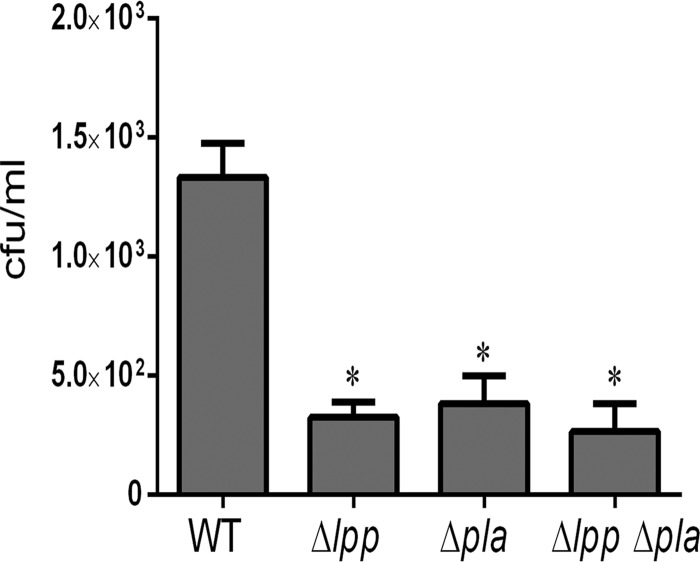
To examine the survivability of the Y. pestis CO92 mutants in macrophages, RAW 264.7 cells were used. As depicted in Fig. 2, WT CO92 could survive in macrophages to 4 h p.i. in a gentamicin protection assay, but the single (Δlpp and Δpla) and the double (Δlpp Δpla) mutants could not efficiently resist the hostile environment of the macrophages. Similar survival data were noted at later time points of 8 and 24 h (data not shown). These effects were not related to the differential sensitivity to gentamicin, as the MIC of this antimicrobial for both WT CO92 and the Δlpp Δpla double mutant was 0.5 μg/ml at 37°C and 0.75 μg/ml at 28°C.
FIG 2.
Intracellular survival of WT Y. pestis CO92 and its mutant strains in murine macrophages. RAW 264.7 macrophages were infected with the WT and its tested mutants at an MOI of 1 for 30 min. Monolayers were treated with 100 μg/ml gentamicin for 1 h to kill extracellular bacteria. At 4 h (after gentamicin treatment), macrophages were lysed and cultured on SBA plates. Three independent experiments were performed. The data were analyzed using one-way ANOVA with the Bonferroni correction, and a P value of ≤0.05 was considered significant. Asterisks, significant difference by comparison of the results for the mutants with those for WT CO92.
Attenuation of Y. pestis CO92 Δlpp Δpla double mutant in a mouse model of bubonic plague and generation of a protective immune response.
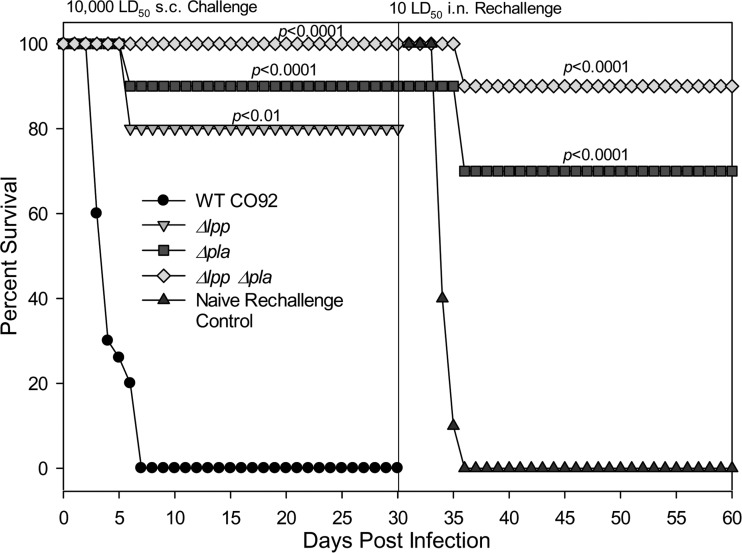
The virulence potential of the Δlpp Δpla double mutant in a mouse model of bubonic plague was determined by infecting animals via the s.c. route with 5 × 105 CFU dose (representing 10,000 LD50s, where 1 LD50 is equal to 50 CFU of WT CO92) (25). As depicted in Fig. 3, mice started dying between days 4 and 6 p.i., and all of the animals infected with WT CO92 succumbed to infection by day 6. However, increased survival rates of 80%, 90%, and 100% were observed for the Δlpp and Δpla single mutant-infected and the Δlpp Δpla double mutant-infected animals, respectively. Importantly, no signs of discomfort were observed in surviving mice infected with either Δlpp Δpla double mutant and extremely mild signs of discomfort were observed in surviving mice infected with the Δlpp or Δpla single mutant. In contrast, mice infected with WT CO92 exhibited ruffled fur, hunched back, lethargy, buboes, and an inability to groom. Although the temperature of the infected animals was not monitored, no significant difference regarding food consumption and body weight was observed in the mutant-infected groups. By using telemetry (47), we will be able to measure the physiological functions of the animals (e.g., respiration rate, cardiac function) in our future studies.
FIG 3.
Survival analysis of mice infected with WT Y. pestis CO92 and its mutant strains by the route causing bubonic plague. Mice were challenged by the s.c. route with 5 × 105 CFU (representing 10,000 LD50s of WT CO92) of WT Y. pestis CO92 and its various mutants at day 0 and observed for mortality. At 30 days p.i., mice that had survived the initial infection were challenged with 10 LD50s of WT CO92 by the i.n. route. We found a 90% survival rate for the Δlpp Δpla double mutant-immunized animals and a 77% survival rate for the Δpla single mutant-immunized mice following challenge with WT CO92. The data were analyzed by using Kaplan-Meier survival estimates, and P values of ≤0.05 were considered significant.
To evaluate specific immunity that could have developed in mice after infection with the WT CO92 mutants, we challenged survivors of the Δpla single mutant-immunized and Δlpp Δpla double mutant-immunized groups with 10 LD50s (1 LD50 = 500 CFU) of WT CO92 via the i.n. route 30 days following the initial infection. The i.n. route was chosen, as it results in the highest CFR in humans. In Fig. 3, 90% of mice that were initially infected with the Δlpp Δpla double mutant survived i.n. challenge with WT CO92. All of the age-matched naive animals infected with WT CO92 died by day 5 p.i.
The highly attenuated phenotype of the Δlpp Δpla double mutant in mice prompted us to evaluate the mutant's resistance to serum killing. Our data showed that both WT CO92 and its Δlpp Δpla double mutant had a 100% survival rate either in untreated or heat-inactivated serum or in PBS at 37°C. These data indicate that deletion of the lpp and pla genes does not affect bacterial resistance to serum (23, 32).
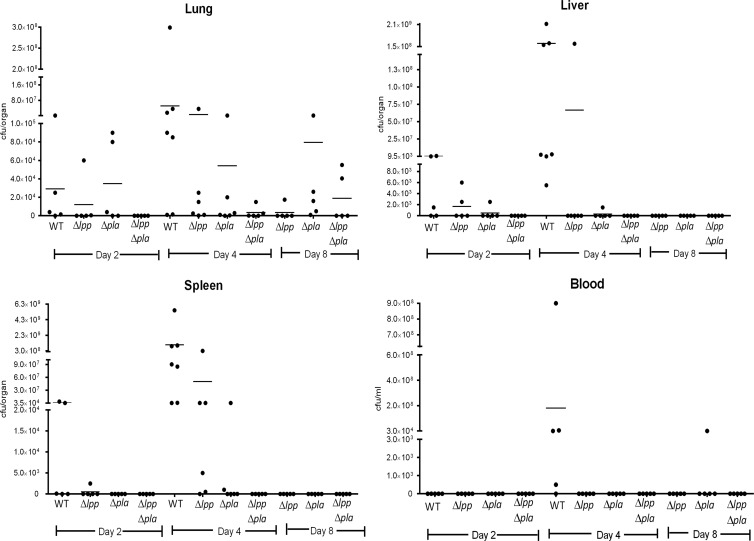
Dissemination of Y. pestis CO92 mutants to peripheral organs in a mouse model of bubonic plague.
We challenged 20 to 25 mice per group by the s.c. route with 5 × 105 CFU of WT CO92 or the Δlpp, Δpla, or Δlpp Δpla mutant. Five to seven mice were sacrificed per time point (2, 4, 8, and 16 days), and the numbers of CFU per organ or ml were determined. As depicted in Fig. 4, WT CO92 could be detected in the lungs of some mice 2 days after infection, reaching an average number of ∼8 × 107 CFU/organ (5/7 mice were positive) by day 4 prior to death. Likewise, an increase in the number of CFU of the Δlpp and Δpla single mutants in the lungs of some mice (3/6 and 2/6, respectively) was noted over a period of 4 days, albeit these bacterial numbers were lower than those from animals infected with WT CO92 at the corresponding time point of 4 days. Importantly, the count of the Δlpp Δpla double mutant was below the limit of detection in the lungs of mice (4/5) until day 4. On day 8, while the Δlpp single mutant was minimally detected (1/5 mice), the average numbers of the Δpla single mutant and the Δlpp Δpla double mutant in the lungs of animals were ∼8 × 104 (4/5 mice were positive) and 2 × 104 (2/5 mice were positive) CFU/organ, respectively. By day 16, no Δlpp, Δpla, or Δlpp Δpla mutant bacteria were detected in the lungs (data not shown).
FIG 4.
Dissemination of WT Y. pestis CO92 and its mutant strains to the peripheral organs of mice infected by the route causing bubonic plague. Mice (20 to 25 per group) were challenged by the s.c. route with 5 × 105 CFU of WT Y. pestis CO92 and its various mutants at day 0. On days 2, 4, 8, and 16, five to seven animals per group were sacrificed and the spleen, liver, lungs, and blood were collected. Each organ (except for blood) was homogenized and plated to determine the bacterial load. The data were analyzed by one-way ANOVA and Tukey's post hoc test, and a P value of ≤0.05 was considered significant. Because of the terminal nature of some animals, blood could not be drawn from them.
A similar bacterial dissemination pattern for WT CO92 and the Δlpp and Δpla single mutants emerged in the spleen and liver of mice up to day 4. By day 8, all mutants were cleared from the spleen (Fig. 4). The Δlpp Δpla double mutant was not cultivated from the spleen at any time point between 2 and 16 days p.i. While we could detect WT CO92 (7/7 mice were positive) and its Δlpp single mutant (1/5 mice were positive) in the liver on day 4, both the Δpla and the Δlpp Δpla mutants either were observed at much decreased levels or were undetectable between 2 and 16 days p.i. Finally, only WT CO92 was detectable in the blood of mice on day 4 (4/5 mice were positive), and the Δpla single mutant was detected in the blood of one mouse on day 8. Neither the Δlpp single mutant nor the Δlpp Δpla double mutant was cultivated from blood at any time point between days 2 and 16 (Fig. 4; day 16 data are not shown).
Cytokine/chemokine levels in sera of mice infected with WT Y. pestis CO92 and its Δlpp Δpla double mutant in a bubonic plague model.
There was a general decrease in the cytokine/chemokine levels in the sera of mice infected with the Δlpp Δpla double mutant compared to the levels in WT CO92-infected animals (Table 3). We have shown data for day 4, as animals infected with WT CO92 were terminal at this time point. Of the 31 cytokines/chemokines, the levels of granulocyte colony-stimulating factor (G-CSF), IL-1β, IL-6, IP-10, monocyte chemoattractant protein (MCP-1), and RANTES were significantly reduced in the sera of mice infected with the Δlpp Δpla double mutant compared to the levels in the sera of animals infected with WT CO92. This general trend of a lower cytokine/chemokine response in the mutant-infected mice correlated with the observation that there was a rapid clearance of the Δlpp Δpla double mutant from mouse organs and blood (Fig. 4).
TABLE 3.
Changes in cytokine and chemokine levels in serum of mice infected with WT CO92 and the Δlpp Δpla double mutant
| Day (route of administration) and strain | Concna (pg/ml) |
||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TNF-α | IFN-γ | G-CSF | GM-CSF | M-CSF | IL-1α | IL-1β | IL-2 | IL-3 | IL-4 | IL-5 | IL-6 | IL-7 | IL-9 | IL-10 | IL-12(p40) 12(p40) | IL-12 (p70) | IL-13 | IL-15 | IL-17 | IP-10 | Eotaxin | KC | LIF | LIX | MCP-1 | MIG | MIP-1α | MIP-2 | RANTES | VEGF | |
| Day 4 (s.c.) | |||||||||||||||||||||||||||||||
| WT (pg/ml) | 310 ± 507 | 2,260 ± 4,330 | 10,918 ± 5,975 | 248 ± 159 | 62 ± 38 | 321 ± 113 | 103 ± 23 | 21 ± 25 | 307 ± 480 | 90 ± 173 | ND | 3,858 ± 3,587 | 33 ± 40 | 46 ± 104 | 77 ± 67 | ND | 62 ± 89 | 1,190 ± 1,837 | 124 ± 204 | 230 ± 516 | 1,740 ± 828 | 1,469 ± 1,020 | 3,528 ± 5,069 | 70 ± 123 | 7,822 ± 2,819 | 3,411 ± 4,627 | 7,403 ± 3,517 | 515 ± 276 | 874 ± 1,272 | 78 ± 57 | 11 ± 7 |
| Δlpp Δpla mutant | ND | ND | 1,708 ± 987*** | ND | 20 ± 20 | 279 ± 179 | 23 ± 26* | 9 ± 5 | ND | 11 ± 2 | 9 ± 20 | 309 ± 248** | ND | ND | 22 ± 22 | ND | ND | ND | ND | ND | 348 ± 97*** | 1,070 ± 199 | 213 ± 114 | ND | 8,111 ± 4,454 | 102 ± 39* | 798 ± 363 | 271 ± 79 | 201 ± 128 | 22 ± 6*** | 5 ± 1 |
| Day 2 (i.n.) | |||||||||||||||||||||||||||||||
| WT (pg/ml) | 69 ± 45 | 274 ± 217 | 26,495 ± 12,979 | 274 ± 79 | 89 ± 51 | 876 ± 177 | 148 ± 98 | 11 ± 7 | 28 ± 7 | 1 ± 3 | 56 ± 43 | 7,458 ± 3,643 | 23 ± 7 | 1,054 ± 165 | 139 ± 78 | 24 ± 10 | 290 ± 166 | 265 ± 100 | 77 ± 22 | 376 ± 366 | 1,654 ± 742 | 2,024 ± 413 | 5,588 ± 4,282 | 98 ± 46 | 15,891 ± 508 | 2,323 ± 2,376 | 52,532 ± 10,237 | 316 ± 122 | 385 ± 109 | 81 ± 40 | 33 ± 34 |
| Δlpp Δpla mutant | 37 ± 12* | 380 ± 417 | 14,299 ± 8,604 | 185 ± 71 | 47 ± 9 | 808 ± 184 | 54 ± 41 | 4 ± 4 | 16 ± 12 | ND | 19 ± 13 | 5,465 ± 4,315 | 14 ± 5 | 1,054 ± 153 | 62 ± 27* | 25 ± 18 | 213 ± 144 | 240 ± 112 | 55 ± 34 | 101 ± 116*** | 1,643 ± 429 | 1,289 ± 342*** | 814 ± 401*** | 42 ± 40 | 8,389 ± 2,100 | 94 ± 38 | 8,079 ± 4,499 | 316 ± 232 | 262 ± 42 | 27 ± 10 | 16 ± 7 |
Abbreviations and symbols: GM-CSF, granulocyte-macrophage colony-stimulating factor; M-CSF, macrophage colony-stimulating factor; LIF, leukemia inhibitory factor; LIX, lipopolysaccharide-induced CXC chemokine; MIG, monokine induced by gamma interferon; MIP-1α, macrophage inflammatory protein 1α; VEGF, vascular endothelial growth factor; ND, not detected; *, P < 0.05; **, P < 0.01; ***, P < 0.001.
Antibodies specific to Y. pestis WT CO92 and its antigens (F1-V) were detected in mice challenged with the Δpla single mutant and Δlpp Δpla double mutant in the bubonic plague model.
Surviving mice challenged with 5 × 105 CFU of the Δpla single mutant or Δlpp Δpla double mutant by the s.c. route (Fig. 3) were bled on day 16 to perform ELISA. Animals challenged with WT CO92 did not survive this 2-week time frame. As noted in Fig. 5A, animals infected with either the Δpla single mutant or the Δlpp Δpla double mutant exhibited significantly increased titers of total IgG to whole CO92 cells compared to the titers in naive mice. Likewise, when the ELISA plates were coated with the F1-V antigens, significantly increased IgG antibody titers were detected in the sera of both groups of mutant-infected mice compared to the titers in naive mouse serum (Fig. 5B). However, the Δpla single mutant seemed to generate better IgG1 (Fig. 5C) and IgG2a (Fig. 5D) antibody responses than the Δlpp Δpla double mutant. These data indicate a trend toward a Th2-based immune response in a mouse model of bubonic plague.
FIG 5.
Antibody responses of mice challenged with the mutant strains of Y. pestis CO92 by the route causing bubonic plague. Mice were challenged by the s.c. route with 5 × 105 CFU of the Δpla single mutant or the Δlpp Δpla double mutant at day 0, and survivors were bled 16 days later to determine antibody titers. (A) To observe the general antibody responses (IgG) to Y. pestis, we grew WT Y. pestis CO92 at 28°C overnight and then shifted the temperature to 37°C for 4 h and used the bacteria to coat the plates for ELISA. An ELISA was also performed on plates coated with the F1-V antigens to measure the overall antigen-specific IgG response (B) and the response to the IgG1(C), IgG2a (D), and IgG2b (E) isotypes. The geometric mean of each sample (n = 5) was used for data plotting. The data were analyzed statistically by one-way ANOVA with Tukey's post hoc test, and P values of ≤0.05 were considered significant.
Attenuation of the Δlpp Δpla double mutant of Y. pestis CO92 in a mouse model of pneumonic plague and generation of a protective immune response.
The virulence potential of the Δlpp Δpla double mutant in comparison to that of WT CO92 and its Δlpp and Δpla single mutants in a mouse model of pneumonic plague was determined by infecting animals by the i.n. route with 5 × 105 CFU (representing 1,000 LD50s of WT CO92, where 1 LD50 is equal to 500 CFU). As shown in Fig. 6, mice started dying between days 3 and 5 p.i., and an increased survival rate for animals infected with the Δpla and Δlpp Δpla mutants was observed. Mice infected with WT CO92 and its Δlpp single mutant died by day 5, with a slight increase in the mean time to death for mice infected with the latter organism compared to that for the WT-challenged animals, while only 40% of the mice infected with the Δpla single mutant survived. It was expected that animals infected with the Δlpp single mutant at such a high challenge dose would not survive (23, 24, 35, 43). On the contrary, the Δlpp Δpla double mutant-infected mice showed 100% survival. Similar to the bubonic plague model, the Δlpp Δpla double mutant-infected animals were clinically healthy, while mice infected with WT CO92 as well as with the Δlpp or Δpla single mutant exhibited marked clinical signs. These data indicate that although individual mutations alone were not sufficient to protect animals from high bacterial challenge doses, deletion of both the lpp and pla genes led to synergistic attenuation of the double mutant in a mouse model of pneumonic plague.
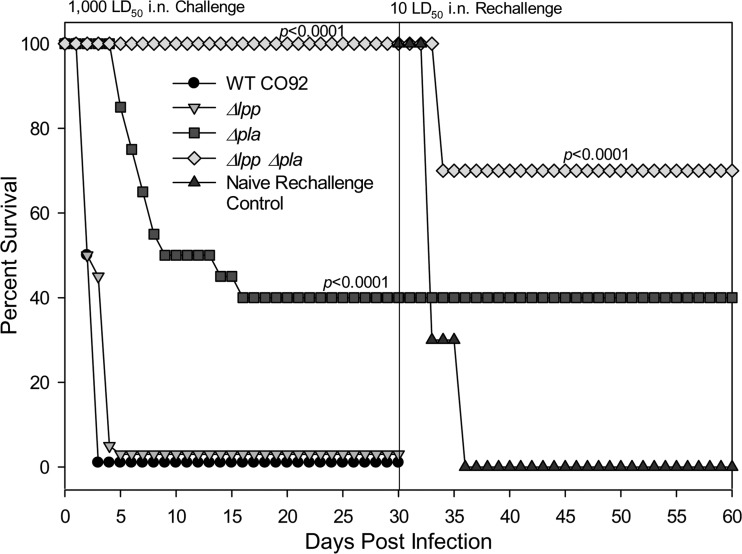
FIG 6.
Survival analysis of mice infected with WT Y. pestis CO92 and its mutant strains by the route causing pneumonic plague. Mice (20 to 30 per group) were challenged by the i.n. route with 5 × 105 CFU (representing 1,000 LD50s of WT CO92) of WT Y. pestis CO92 and its various mutants at day 0 and observed for mortality. At 30 days p.i., survivors were rechallenged with 10 LD50s of the WT CO92 strain by the i.n. route and observed for mortality. The data were statistically analyzed by using Kaplan-Meier's survival estimates, and a P value of ≤0.05 was considered significant.
To evaluate whether Y. pestis-specific immunity developed in the surviving mice, they were challenged with 10 LD50s of WT CO92 (5,000 CFU) via the i.n. route 30 days following the initial infection. As shown in Fig. 6, 70% of the animals that were initially infected with the Δlpp Δpla double mutant survived challenge with the WT CO92 strain. Although 100% of the mice initially infected with the Δpla single mutant survived rechallenge, there was a significant mortality rate (60%) during the initial phase of infection. Mice that were age and sex matched served as controls and succumbed to infection. Overall, our results indicate that the double mutant was not lethal to mice but provided animals with significant protection from subsequent WT CO92 infection, irrespective of the route of initial challenge, s.c. or i.n. (Fig. 3 and 6).
Dissemination of Y. pestis CO92 mutants to peripheral organs in a mouse model of pneumonic plague.
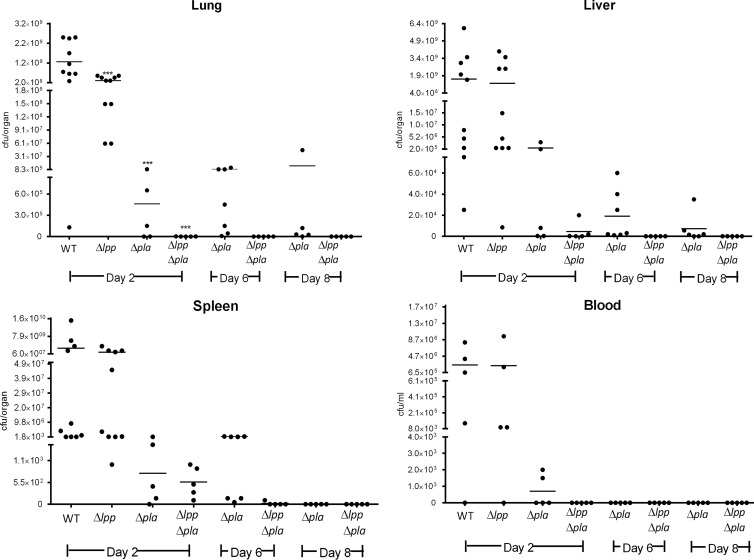
First, 20 to 30 mice per group were challenged by the i.n. route with 5 × 105 CFU of WT CO92 or the Δlpp, Δpla, or Δlpp Δpla mutant. Then, 5 to 10 mice per time point (2, 6, 8, and 14 days) were sacrificed and the numbers of CFU in various organs were determined. By day 2, significant multiplication of WT CO92 (10/10 mice) and its Δlpp single mutant (10/10 mice) was seen in the lungs, liver, and spleen (Fig. 7). The blood of 4/5 animals infected with either WT CO92 or its Δlpp single mutant had high bacterial counts, while the blood of 2/5 mice was positive for the Δpla mutant, although at low numbers. The Δpla single mutant was generally detected in lower numbers (close to the challenge dose) in all of these organs on day 2 (Fig. 7), and the Δlpp Δpla double mutant was found at low to undetectable numbers in the peripheral organs. All of the mutants were present in the lungs at a statistically significantly lower level than WT CO92. By day 6, all of the animals infected with WT CO92 and its Δlpp single mutant died, and, hence, there were no data for those groups. Although the Δpla single mutant was detectable in the lungs up to day 8 (2/5 mice were positive), the spleen was negative on day 8 (Fig. 7). The double mutant was only minimally detected, if at all, in all of the organs between days 6 and 14 (day 14 data are not shown). The Δlpp Δpla double mutant was undetectable in the blood at all time points.
FIG 7.
Dissemination of WT Y. pestis CO92 and its mutants to peripheral organs of mice infected by the route causing pneumonic plague. Mice were challenged by the i.n. route with 5 × 105 CFU of WT Y. pestis CO92 and its various mutants at day 0. On days 2, 6, 8, and 14, 5 to 10 animals per group were sacrificed and the spleen, liver, lungs, and blood were collected. Each organ (except for blood) was homogenized and plated to determine the bacterial load. The data were analyzed by one-way ANOVA and Tukey's post hoc test. Statistically significant values are indicated (***, P < 0.001), and these data were compared to those for animals infected with WT CO92. By day 2, all of the WT bacterium- and Δlpp mutant-infected mice had died. Because of the terminal nature of some animals, blood could not be drawn from them.
Cytokine/chemokine levels in sera of mice infected with WT Y. pestis CO92 and its Δlpp Δpla double mutant in a pneumonic plague model.
As noted above for the mouse model of bubonic plague, there was a general decrease in the cytokine/chemokine levels in the sera of mice infected with the Δlpp Δpla double mutant compared to the sera of WT CO92-infected animals (Table 3). Specifically, at 2 days after infection, the levels of TNF-α, IL-10, IL-17, and keratinocyte-derived chemokine (KC) were significantly downregulated in mice infected with the Δlpp Δpla double mutant compared to their levels in mice infected with the WT. This general trend of a lower cytokine/chemokine response in the mutant-infected mice correlated with the rapid clearance of the Δlpp Δpla double mutant from organs and blood (Fig. 7).
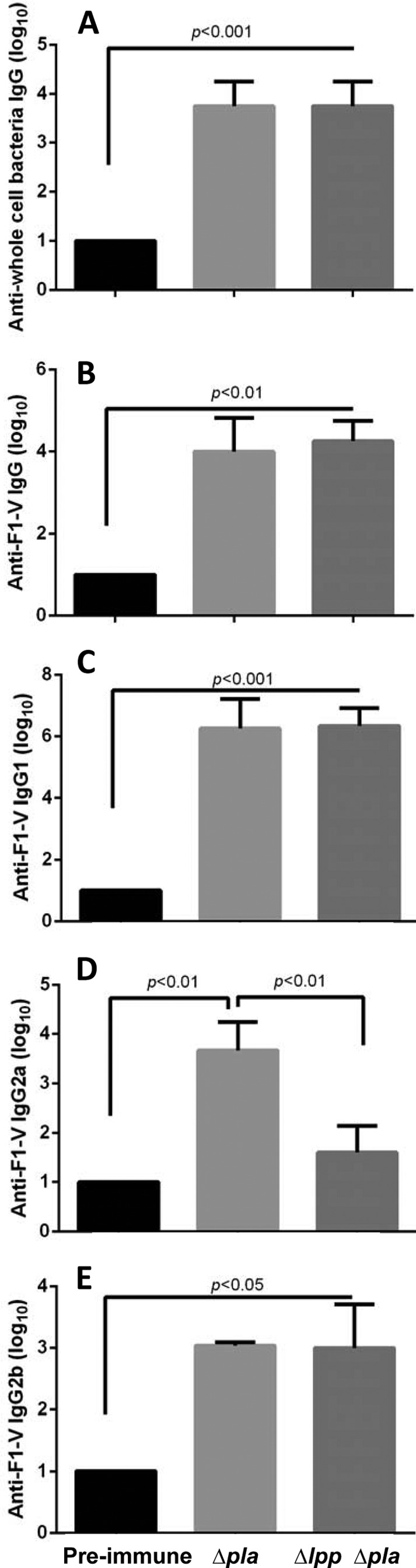
Antibodies specific to WT Y. pestis CO92 and its F1-V antigens were detected in mice challenged with the Δpla single mutant and Δlpp Δpla double mutant in the pneumonic plague model.
Mice challenged by the i.n. route with the Δpla single mutant and the Δlpp Δpla double mutant exhibited total IgG titers (1:10,000) significantly higher than those in preimmune sera when ELISA plates were coated with WT CO92 on day 14 (Fig. 8). Likewise, high IgG titers of 1:3,125 for both the mutants were observed when ELISA plates were coated with F1-V. Titers of 1:3,125 were noted for IgG1 and IgG2a, indicating that a balanced Th1 and Th2 response was generated by both the Δpla single mutant-challenged and Δlpp Δpla double mutant-challenged mice (Fig. 8). Our data indicate that the Th1 response generated by the double mutant might be stronger than that generated by the Δpla single mutant (see the IgG2a antibody titers in Fig. 8). The IgG2b titers against the F1 and LcrV antigens were similar for both the single mutant and the double mutant (Fig. 8). The relative ratio of IgG1/IgG2a was 1:1 for both the Δpla single mutant and the Δlpp Δpla double mutant, thereby indicating a trend toward a balanced Th1-Th2 immune response.
FIG 8.
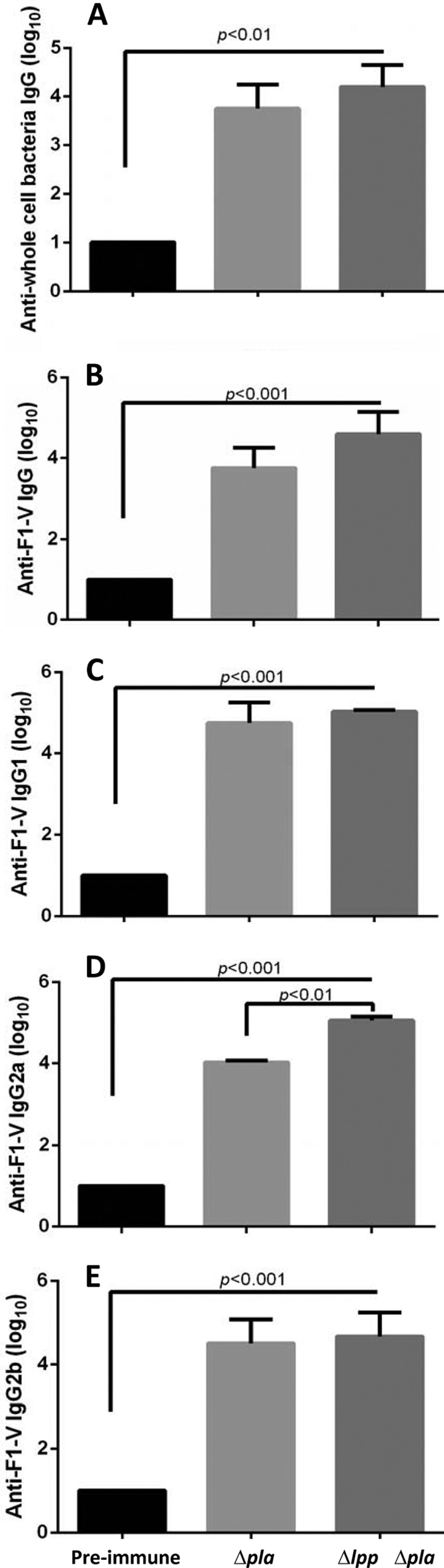
Antibody responses of mice challenged with the mutant strains of Y. pestis CO92 by the route causing pneumonic plague. Mice (n = 10) were challenged by the i.n. route with 5 × 105 CFU of the Δpla single mutant or the Δlpp Δpla double mutant on day 0 and bled 14 days later to determine the antibody titers in serum. (A) WT Y. pestis CO92 was grown to coat the plates for ELISA to observe the total IgG antibody response to Y. pestis. An ELISA was also performed to examine the total antigen-specific IgG (B), IgG1 (C), IgG2a (D), and IgG2b (E) responses when the plates were coated with the F1-V antigens of Y. pestis. The geometric mean of each sample (n = 5) was used for plotting of the data. The data were analyzed statistically by one-way ANOVA with Tukey's post hoc test, and P values of ≤0.05 were considered significant.
Complementation of the Δpla single mutant and Δlpp Δpla double mutant of Y. pestis CO92 in a mouse model of pneumonic plague.
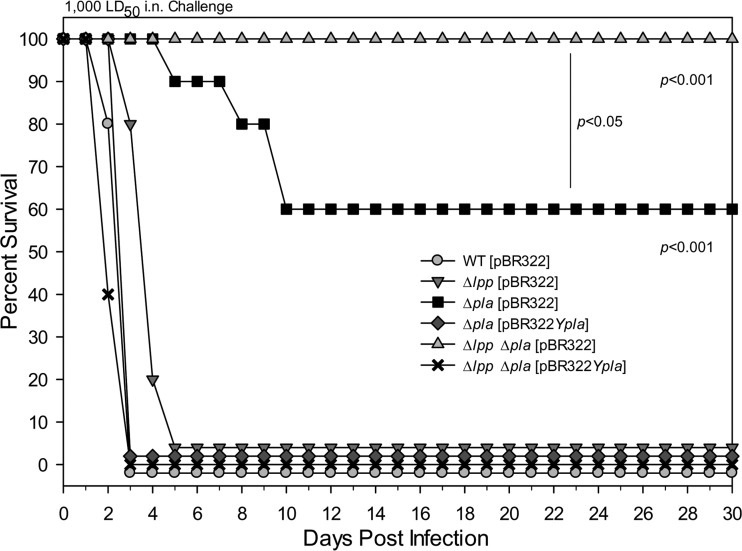
To test whether we could demonstrate the restoration of the virulence of the Δpla single mutant and the Δlpp Δpla double mutant, we complemented them with the pla gene in trans and tested the mutants in a mouse model of pneumonic plague (Fig. 9). All of the animals infected with WT CO92(pBR322) (Table 1) by the i.n. route at a dose of 1,000 LD50s died by day 3. Likewise, all of the animals infected with the Δlpp(pBR322) single mutant died at the WT CO92 dose equivalent of 1,000 LD50s by day 5. However, an attenuation of the virulence of this Δlpp mutant was observed, as the mean time to death of the mice was increased compared to that of the WT CO92-infected animals (day 3 versus day 5). While the virulence of both the Δpla(pBR322) single mutant (60% survival) and the Δlpp Δpla(pBR322) double mutant (100% survival) was attenuated at the same challenge dose of WT CO92, the death rates of the mice increased to 100% (0% survival by day 3) when the above-mentioned mutants were complemented with the pla gene. We also observed a statistically significant increase in survival when comparing the Δpla(pBR322) single mutant and the Δlpp Δpla(pBR322) double mutant.
FIG 9.
Survival analysis of mice infected with WT Y. pestis CO92 and its complemented mutant strains by the route causing pneumonic plague. Mice (10 per group) were challenged by the i.n. route with 5 × 105 CFU (representing 1,000 LD50s of WT CO92) of WT Y. pestis CO92, its various mutants, and the complemented Δpla single mutant or the Δlpp Δpla double mutant (at day 0) and observed for mortality. The data were analyzed by using Kaplan-Meier survival estimates, and a P value of ≤0.05 was considered significant. The data between WT CO92 and its various mutants as well as between the Δpla single mutant and the Δlpp Δpla double mutant were compared.
Histopathology.
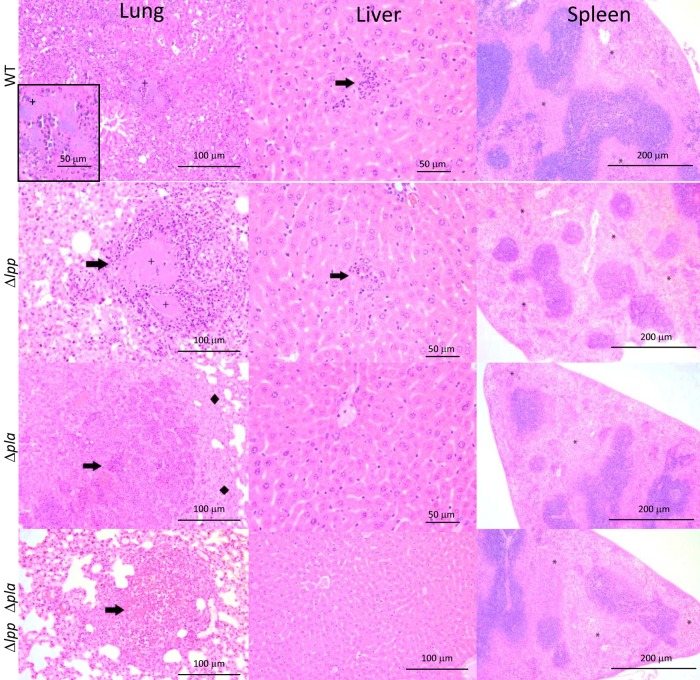
Portions of the mouse tissues were stained with H&E to assess the level of tissue damage after infection (pneumonic plague) with WT CO92 and its Δlpp and Δpla single mutants and Δlpp Δpla double mutant at a dose of 5 × 105 CFU. Uninfected control mice exhibited no significant lesions, and tissues appeared normal (data not shown). All of the mice infected with the WT and the Δlpp, Δpla, and Δlpp Δpla mutants had lung lesions at 2 days p.i., but the severity and prevalence of the lesions were notably decreased in the Δlpp Δpla double mutant-challenged animals (Fig. 10). At 2 days p.i., mild to moderate tissue lesions (20 to 50% tissue involvement) were noted in the lungs of animals infected with WT CO92 and the Δlpp and Δpla single mutants. Lung lesions included edema, hemorrhage, fibrinous infiltrates, acute inflammation, and leukocytosis. Additionally, bacteria were observed in WT- and Δlpp mutant-challenged mice. In Fig. 10, the enlarged inset in the image of the lungs of WT CO92 shows the presence of bacteria.
FIG 10.
Histopathology of mouse tissues following infection with WT Y. pestis CO92 and mutant strains. Mice were challenged by the i.n. route with 5 × 105 CFU of either WT CO92 or its mutants. At 2 days p.i., a portion of the lungs, liver, and spleen was stained with H&E and evaluated. Organs from 3 animals were examined, and representative data are shown here. Arrows in lung and liver images, inflammation; plus signs in lung images, observable bacterial presence; diamonds, edematous areas; asterisks in spleen images, areas of decreased cellularity in the red pulp and marginal zones of the white pulp.
Further, in the lungs of mice infected with WT CO92 and the Δlpp and Δpla single mutants, there was a noticeable collapse in the structure of the alveoli accompanied by congestion and disintegration of the alveolar sacs and an increase in neutrophil recruitment, which led to an acute inflammatory response. The Δlpp Δpla double mutant-infected mice, on the other hand, exhibited only mild lesions (10 to 20% tissue involvement) in their lungs, indicative of a decrease in tissue damage and consistent with a decline in the virulence of this mutant (Fig. 6). Although some inflammation was noted in the lungs of mice infected with the Δlpp Δpla double mutant (Fig. 10), recruitment of neutrophils was at a much reduced level, which also correlated with the decrease in proinflammatory cytokine levels that we observed in the sera of mice at 2 days p.i. (Table 3).
In the liver, WT CO92-infected mice exhibited mild, acute inflammation (3/3 mice) and the presence of bacteria (1/3 mice). Two of 3 Δlpp mutant-infected mice, 3 of 3 Δpla mutant-infected mice, and 3 of 3 Δlpp Δpla mutant-infected mice had no liver lesions, and no mutant-infected animals had bacteria in the liver, indicative of a decreased ability of the mutants to disseminate (Fig. 7). All WT CO92-infected animals had splenic lesions, which included acute inflammation, myeloid hyperplasia, and decreased cellularity in the red pulp and mild to moderate (20 to 50% tissue involvement) depletion in the marginal zones of the white pulp.
All Δlpp and Δpla mutant-infected mice and 2 of 3 Δlpp Δpla mutant-infected mice had splenic lesions that were similar to those seen in mice infected with WT CO92, which was expected, as we observed a cell-based immune response. All mice tended to show some alterations in the red pulp, indicative of antigen processing from the lymph and bloodstream, in addition to the recruitment of lymphocytes from the spleen (Fig. 10). Subsequently, at days 6 and 8 p.i., a general trend toward clearing and containment of the infection was observed in mice infected with the mutants; notably, the Δlpp Δpla double mutant-infected mice never showed bacteria in any of the examined organs, and the level of inflammatory tissue involvement did not exceed 20% (data not shown).
T cell activation by the Δlpp Δpla double mutant of Y. pestis CO92 in a mouse model of pneumonic plague.
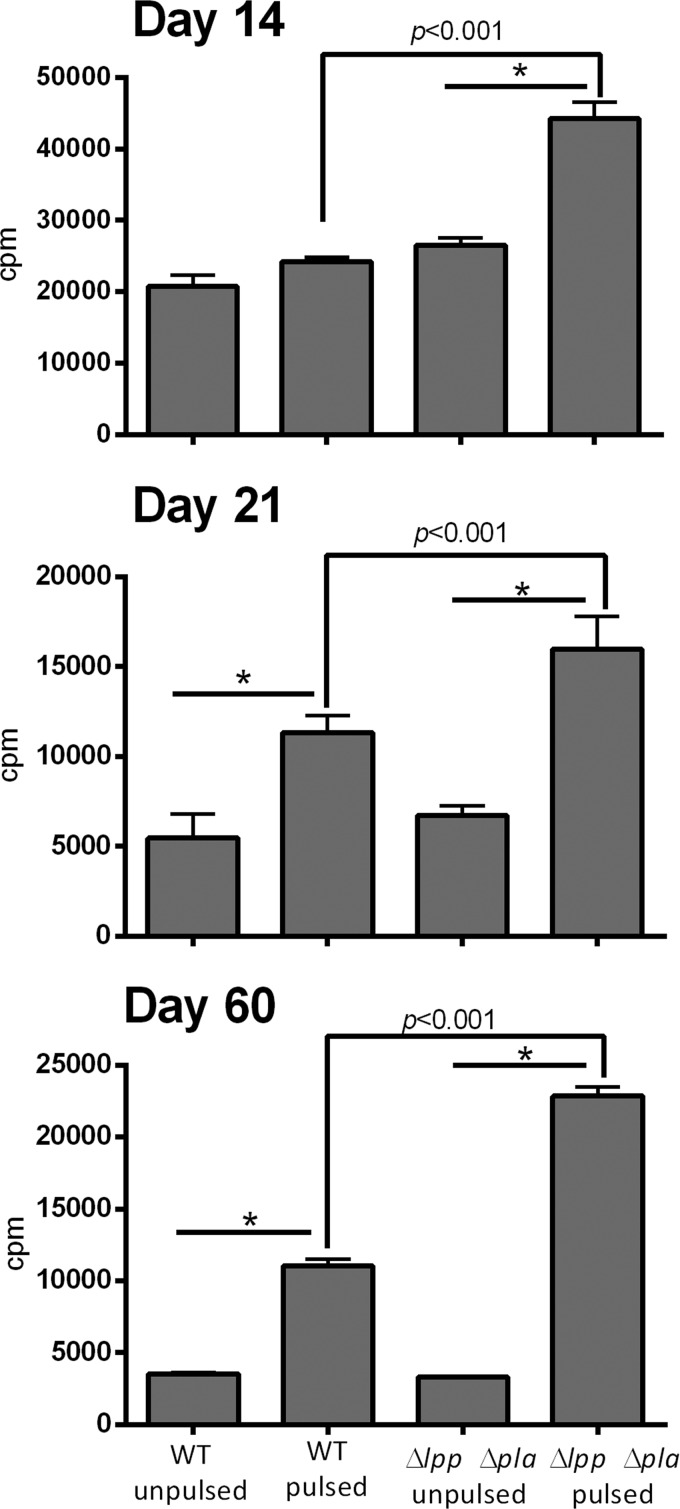
To investigate the specific T cell responses in mice infected with the Δlpp Δpla double mutant, T cells were isolated from the spleens of animals challenged with a sublethal dose of either WT CO92 or its Δlpp Δpla mutant at three time points: 14, 21, and 60 days. Although some mice infected with WT CO92 died during the course of infection, we had enough survivors (at least n = 5) for each time point to obtain statistically significant data. We chose these time points to examine early and recall (memory) immune responses. The isolated T cells were then stimulated for 3 days with APCs that had been incubated with heat-killed WT CO92 and then γ-irradiated. As shown in Fig. 11, T cells from both WT CO92-infected mice and Δlpp Δpla mutant-infected mice proliferated strongly, specifically, on days 21 and 60. Importantly, T cells from the mutant-infected mice proliferated more than T cells from the WT CO92-infected animals at all 3 time points tested (Fig. 11). Together, these data indicate that the Δlpp Δpla mutant-immunized mice had a better recall response to WT CO92 antigens than the WT bacterium-immunized animals.
FIG 11.
Proliferation of T cells isolated from WT Y. pestis CO92- and Δlpp Δpla mutant-infected mice. A total of 60 mice were i.n. challenged with a sublethal dose (250 CFU) of WT CO92 or the Δlpp Δpla double mutant (30 mice per group). At 14, 21, and 60 days p.i., T cells were isolated separately from the spleens of 5 mice in each infected group and stimulated for 3 days with APCs that had been pulsed with heat-killed WT CO92 and then γ-irradiated. Data were analyzed by using the Bonferroni correction with a one-way ANOVA, and a P value of ≤0.05 was considered significant. *, statistical significance in comparing unpulsed to pulsed T cells (P < 0.001) for both WT- and mutant-infected mice. The results represent averages from 2 independent experiments.
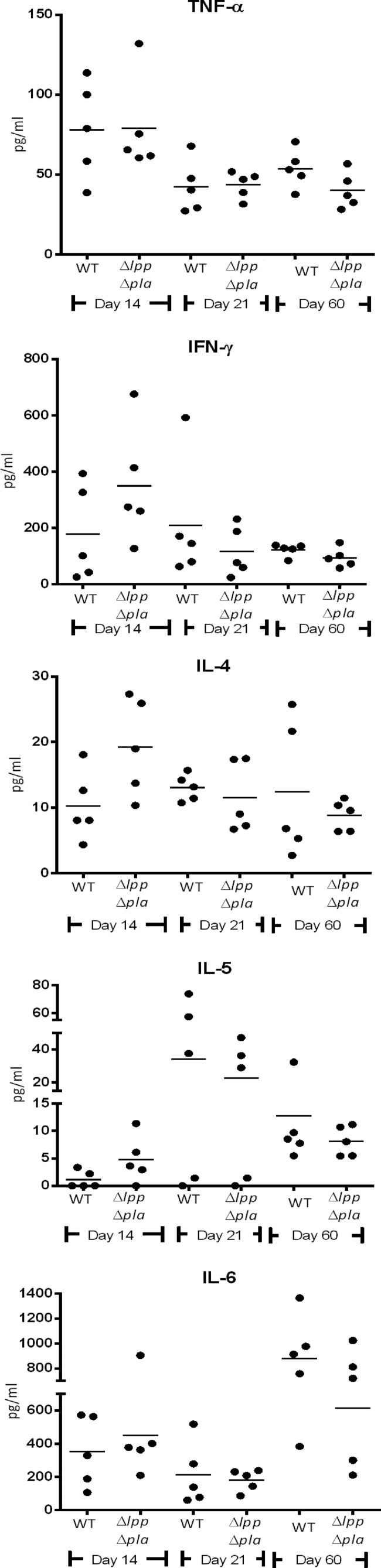
The supernatants from APC-stimulated T cells from WT CO92-challenged and Δlpp Δpla double mutant-challenged mice were harvested at 48 h for multiplex analysis of 6 cytokines/chemokines. We found that T cells from animals immunized with the Δlpp Δpla double mutant had higher levels of IFN-γ and IL-4 on day 14; although the data did not reach statistical significance (Fig. 12). The levels of other cytokines (TNF-α, IL-5, and IL-6) were similar across the three time points in the Δlpp Δpla double mutant-immunized and the WT bacterium-immunized mice (Fig. 12). The presence of both TNF-α and IFN-γ indicated a Th1-based response, which is critical in clearing an intracellular infection. Overall, our data provided evidence that the Δlpp Δpla double mutant is capable of stimulating a protective, cell-based immune response, while it is highly attenuated in causing an infection in animals. We did not observe any IL-17 response from the T cells of WT- or double mutant-immunized mice (data not shown). These cytokine data also indicated a balanced Th1/Th2 immune response generated by the Δlpp Δpla double mutant.
FIG 12.
Cytokine production by T cells isolated from WT Y. pestis CO92- and CO92 mutant-immunized mice after ex vivo pulsing with plague bacterium antigens. A total of 60 mice were i.n. challenged with a sublethal dose (250 CFU) of the WT or the Δlpp Δpla mutant (30 mice per group). At 14, 21, and 60 days p.i., spleens from 5 mice in each infected group (at each time point) were harvested, and T cells were isolated from each animal separately (including uninfected controls) and incubated with pulsed or unpulsed APCs. After 48 h of incubation, supernatants were harvested for analysis by use of a Milliplex kit. Data were analyzed by use of the Bonferroni correction with one-way ANOVA, and a P value of ≤0.05 was considered significant.
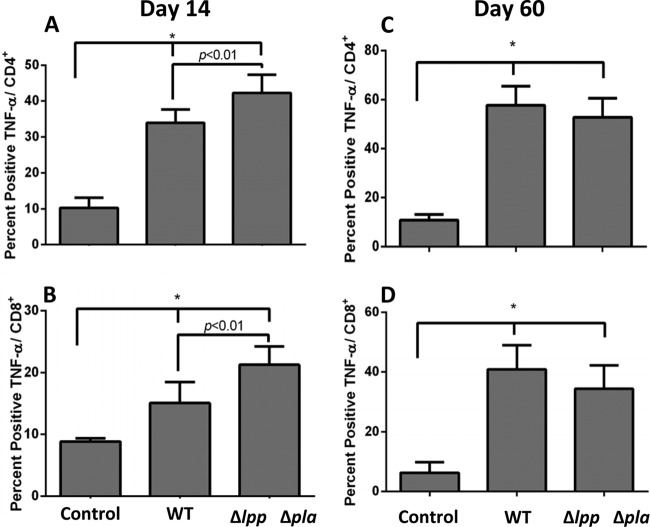
Activation of T cell subsets by the Δlpp Δpla double mutant of Y. pestis CO92 in a mouse model of pneumonic plague.
T cells from animals infected with WT CO92 or the Δlpp Δpla double mutant or uninfected mice were cultured with pulsed APCs for 5 days. As shown in Fig. 13, on day 14 we noted a significant increase in the levels of CD4+ TNF-α-secreting T cells in the Δlpp Δpla mutant-immunized mice compared to those in WT bacterium-infected animals (Fig. 13A). On day 60, however, similar percentages of CD4+ TNF-α-producing T cells from WT CO92- and Δlpp Δpla double mutant-immunized animals were observed (Fig. 13B). Likewise, on day 14 the percentage of CD8+ T cells producing TNF-α also increased in the mutant-immunized mice (Fig. 13C), while on day 60 both WT- and mutant-immunized animals had similar percentages of CD8+ T cells producing this cytokine (Fig. 13D). These data indicate that the Δlpp Δpla double mutant is capable of inducing CD4+ and CD8+ T cell-specific responses in terms of TNF-α production at least as good as or better than those in the WT bacterium-immunized mice. Such a cellular immune response is important in protecting mice against pneumonic plague.
FIG 13.
Flow cytometry of T cells isolated from WT Y. pestis CO92- and CO92 mutant-immunized mice after ex vivo pulsing with plague bacterium antigens. T cells from animals infected with WT CO92 or the Δlpp Δpla double mutant or uninfected mice (see the legend to Fig. 12) were cultured with pulsed APCs for 5 days. Cells were then stained and read on a flow cytometer (LSR II Fortessa), and the data were analyzed by using FACS Diva software. T cells were stained on days 14 (CD4+0 cells [A] and CD8+ cells [C]) and 60 (CD4+ cells [B] and CD8+ cells [D]). These data represent averages from two independent experiments. Data were analyzed by Tukey's post hoc test with one-way ANOVA, and a P value of ≤0.05 was considered significant. *, statistical significance (P < 0.05) between control mice and WT CO92-infected or Δlpp Δpla double mutant-infected mice.
DISCUSSION
Our study has developed a platform that could potentially lead to the development of a legitimate and well-defined live-attenuated plague vaccine, as the Δlpp Δpla double isogenic mutant generated was highly attenuated and effective at establishing long-term immunity against plague in the host. Although the subunit plague vaccines composed of F1 and LcrV antigens are currently in clinical trials, these vaccines evoke only a strong humoral immune response, which may not be adequate in protecting humans (15, 22, 48, 49). The lack of an FDA-approved vaccine and the need for both humoral and cell-mediated immune responses to effectively combat plague infections warrant a continued search for new live-attenuated plague vaccine candidates. The Δlpp Δpla double mutant could possibly provide the background strain, which, after some additional manipulations to reduce reactogenicity, might become an excellent vaccine candidate.
In an earlier study, we demonstrated that when the pPCP-1 plasmid harboring the pla gene was cured from the Δlpp single mutant, the resulting strain was highly attenuated in a mouse model of pneumonic plague (35). However, since the pPCP-1 plasmid encodes the pst and pim genes, among others, it was essential to create an isogenic Δpla mutant for vaccine development purposes.
On the basis of both in vitro and in vivo characterization (35, 50), it was apparent that there were no pleiotropic effects associated with the deletion of two genes, lpp and pla, from WT CO92 (Fig. 1, 3, 6, and 9). To be an attractive live-attenuated vaccine strain, it should be quickly cleared from the host after triggering both arms of the immune response. Therefore, we examined the survivability of the Δlpp Δpla double mutant in macrophages, the primary cell type that is affected during pneumonic plague. Indeed, we noted that the Δlpp Δpla double mutant was unable to survive in macrophages beyond 4 h in vitro (Fig. 2) and that it was largely cleared from all organs of mice by day 2 in mouse models of bubonic and pneumonic plague (Fig. 4 and 7).
In our earlier study, we have shown that the Δlpp single mutant was also unable to survive within macrophages due to the downregulation of a gene encoding the global stress response protein A (GsrA) (35, 51). However, it is unclear how Pla directly or indirectly contributes to bacterial survival in the host cell, but the literature indicates that Pla can enhance bacterial invasion of epithelial cells and mediate the delivery of T3SS effectors into the host (34).
We were intrigued by our results that the Δpla single mutant was unable to survive in macrophages (Fig. 2). These data are in contrast to those from our earlier study in which we demonstrated that WT CO92 cured of the pPCP-1 plasmid was initially (4 to 8 h) sensitive to the macrophage environment but recovered and had a survived rate similar to that of WT CO92 by 24 h (35). Therefore, it is tempting to speculate that other genes present on the pPCP-1 plasmid (e.g., pst and pim) might modulate the survival of the plasmid-cured CO92 strain in macrophages compared to that for the Δpla single mutant, and this possibility needs further investigation. Finally, although we used murine RAW 264.7 macrophages, we have shown that macrophages derived from human HL-60 cells behaved very similarly (43).
Our data corroborate earlier findings that the ability of the Δpla single mutant to disseminate to peripheral organs is impeded in a mouse model of bubonic plague (29, 30). However, in a mouse model of pneumonic plague, our data indicated that the Δpla single mutant retained its capability to disseminate to the liver and spleen up to day 6 p.i., although the number of bacteria and animals that were positive for infection was greatly reduced compared to that for WT CO92-infected mice (Fig. 7). Importantly, on day 2 p.i., there was a statistically significant decrease in the count of the Δpla single mutant at the initial infection site (lungs) compared to that of WT CO92 (Fig. 7). These data indicate the failure of the Δpla mutant to colonize lung tissue, as reported earlier by Lathem et al. (32). The difference in the pattern of Δpla mutant dissemination in mouse models of bubonic and pneumonic plague could be related to the highly vascularized nature of the lungs, allowing the escape of some bacteria through alveolar capillaries and, thus, initiating systemic infection (33).
Pla facilitates digestion of fibrin matrices at peripheral sites of infection, thereby disrupting physical barriers that impede bacterial dissemination (34). The inability of the Δlpp Δpla double mutant to dissolve fibrin deposits due to the absence of Pla would enable innate and adaptive host effector cells to quarantine and destroy the invading bacteria. A recent study has also implicated the role of fibrin in innate and T cell-mediated protection of mice against pneumonic plague (33), as fibrin-dependent signals provide a cue for neutrophils to combat Y. pestis infection. However, in the above-mentioned study (33), it was also noted that the fibrinogen-deficient mice which had antibodies to F1 and LcrV were protected from developing pneumonic plague. These data suggest that fibrinogen does not contribute to antibody-mediated protection of animals. Taken together, the Δlpp Δpla double mutant would avoid mitigation of the innate and cell-mediated signals associated with fibrin deposits.
In a mouse model of pneumonic plague, the levels of four cytokines/chemokines showed statistically significant decreases compared to their levels in the WT CO92-infected animals (Table 3). One of them was KC, which attracts neutrophils to the site of an infection, and this may contribute to the impaired neutrophil infiltration observed in the tissues of mice infected with the Δlpp Δpla double mutant compared to that observed in mice infected with WT CO92 (Fig. 10).
The levels of IL-17 and TNF-α were also significantly reduced in the Δlpp Δpla double mutant-infected mice. IL-17 is known to increase chemokine production in tissues to recruit neutrophils and monocytes to the inflammation site and, in conjunction with IL-23, is responsible for severe tissue damage (18). In addition, IL-17 synergizes with TNF-α to produce damaging effects in the host (18). Finally, the double mutant-infected animals produced significantly less anti-inflammatory cytokine IL-10 (Table 3) than the WT-infected animals. This could possibly be related in part to deletion of the lpp gene from the double mutant, as the absence of Lpp would result in a more greatly reduced activation of TLR2, the latter of which LcrV also uses to promote the production of IL-10 (25). Our future study will investigate this possibility in detail.
The production of both IgG1 and IgG2a antibodies in a mouse model of pneumonic plague infected with the Δlpp Δpla double mutant indicated a balanced Th1/Th2 CD4+-based immune response (Fig. 8). The IgG1 isotype corresponds to an increased stimulation of the Th2 CD4+ T cell subset, principally producing IL-4 and thereby stimulating an antibody-mediated immune response. Indeed, T cells from our double mutant-immunized mice had higher IL-4 levels than T cells from animals infected with WT CO92 at the sublethal dose (Fig. 12). The IgG2a isotype, on the other hand, corresponds to an increase in the Th1 CD4+ T cell subset, which mainly secretes TNF-α and IFN-γ, which are required for combating an intracellular infection with activated cytotoxic lymphocytes (52). T cells from the Δlpp Δpla double mutant-immunized mice similarly had higher levels of IFN-γ and TNF-α than T cells from WT CO92-infected animals (Fig. 12 and 13). The current notion in the plague field is that cellular immunity augments antibody-mediated defense (15, 17). In other words, antibodies alone provide unreliable protection, while a cellular immune response, such as the one elicited by a live-attenuated vaccine, provides dependable protection. Consistent with this hypothesis, our data depicted that both cell-based immunity (Fig. 11 to 13) and humoral immunity (Fig. 8) were elicited by the Δlpp Δpla double mutant, providing comprehensive protection against pneumonic plague.
The route of infection seems to play a role in dictating which type of antibodies are elicited by the Δlpp Δpla double mutant during plague. For example, in the bubonic plague model, the Δpla single mutant elicited both IgG1 and IgG2a, while the Δlpp Δpla double mutant predominately elicited IgG1 (Fig. 5). However, animals infected with the above-mentioned single or double mutant in a pneumonic plague model produced similar levels of IgG1 and IgG2a (Fig. 8). An earlier study also indicated a predominant Th2 response in mice by immunization with F1-V by the s.c. route and a balanced Th1/Th2 response when mice were immunized by the i.n. route (53).
No detectable IgA was measured in the sera of mice infected with the Δpla single mutant or the Δlpp Δpla double mutant by any route (data not shown). However, IgA antibodies are rarely seen in serum during pneumonic plague, as the hallmark of disease is not the colonization of the lungs by the bacteria but, rather, rapid dissemination from the lungs. Thus, the lack of an IgA response may not be a necessity to contain Y. pestis infection (54).
The T cell proliferative responses specific to Y. pestis antigens were significantly more robust in the Δlpp Δpla double mutant-immunized mice than in animals infected with WT CO92 (Fig. 11). Live-attenuated vaccine strains tend to elicit reduced T cell responses compared to those elicited by WT bacteria due to overattenuation (15, 19, 20), thus making our findings significant. In our early study in which mice were infected with another double mutant, a Δlpp ΔmsbB mutant of Y. pestis, we showed T cell proliferative responses comparable to those seen in the WT CO92-infected animals (43). Here, we have provided evidence that a majority of the T cells that were proliferating after immunization of mice with either the Δlpp Δpla double mutant or WT CO92 were TNF-α-producing CD4+ and CD8+ cells (Fig. 13).
We preferred to measure cytokine responses both in the T cell supernatants by a multiplex assay and in the CD4+ and CD8+ subsets of T cells by flow cytometry in WT- and double mutant-immunized mice. Our rationale was not to miss their detection due to low levels or degradation. Indeed, we could detect IFN-γ production in the T cell supernatants by multiplex assay but not in T cell subsets. Conversely, TNF-α was seen both in T cell subsets and in the supernatants of T cells. These data could be explained by the fact that the detection of cytokines in the supernatant (such as in the multiplex assay) is dependent on the total number of T cells used and their ability to produce these mediators. Further, some discrepancy in the levels of cytokines detected could also be related to the sensitivity of the two methods used. Mechanistically, both TNF-α and IFN-γ combat Y. pestis infection by upregulating the production of inducible nitric oxide synthase 2 (iNOS) in macrophages (55). In addition, both of these cytokines have the potential to augment oxidative mechanisms in neutrophils (55).
The protective role of these two cytokines during plague has further been established, as neutralizing antibodies against these cytokines negatively impact antibody (to F1 and LcrV)-mediated protection against pneumonic plague (15, 17). Conversely, endogenous TNF-α and IFN-γ could protect mice against Y. pestis infection without any protective antibodies to F1 and LcrV (15).
Taken together, our data tend to suggest that the TNF-α and IFN-γ produced by T cells during the immunization of mice with the Δlpp Δpla double mutant would activate macrophages to kill intracellular plague bacteria during secondary infection (Fig. 6), while the neutrophils activated by the same cytokines would kill extracellular Y. pestis bacteria, possibly in a fibrin-dependent manner (31, 33). Finally, the IL-17 produced by T cells has been implicated to play a role in protection of the host against pneumonic plague (18), although how it contributes to protection is unclear, as it is not related to rapid bacterial clearance or neutrophil recruitment (18, 56–58). In our study, we were unable to detect IL-17 from T cells in WT CO92- or double mutant-immunized mice. However, because the Δlpp Δpla double mutant rapidly clears from the host and the production of TNF-α and IFN-γ by T cells would activate neutrophils, IL-17 might not be absolutely required for protection, and this needs further investigation. In summary, our data indicate that the Δlpp Δpla double mutant stimulates WT bacterium-like or better protective humoral and cellular immune responses in mice without lethality.
The dose of the Δlpp Δpla double mutant which was used to induce pneumonic plague in this study (5 × 105 CFU) was lower than that of the EV76 strain (5.8 × 106 CFU) used as a live-attenuated vaccine strain in the former Soviet Union (48). Since the Δlpp Δpla double mutant still possesses an intact LPS, it would have issues related to reactogenicity. Consequently, introduction of additional mutations in the current Δlpp Δpla double mutant, e.g., mutations that reduce the biological potency of LPS, or deletion of other virulence genes may present a logical step in the future. In our earlier study, we modified the LPS of Y. pestis CO92 by deleting the msbB gene, which encodes an acyltransferase that is responsible for the addition of lauric acid to the lipid A moiety of LPS (43). We have shown that the Δlpp ΔmsbB mutant was more attenuated than the single mutants (i.e., the Δlpp or ΔmsbB mutant) alone in a mouse model of pneumonic plague and that it generated cell-mediated immune responses (43). On the other hand, studies have also implicated opsonic antibodies to the antigenically variable LPS O antigens as primary immune effectors against Pseudomonas aeruginosa-associated acute lung infection (59, 60). Therefore, fine-tuning of attenuation and the immunogenicity is a key to the development of a successful live-attenuated vaccine.
Most importantly, vaccines like the one described in this study could possibly represent attractive options for immunocompetent individuals (military personnel and others who have been exposed to the pathogen); the suitability of vaccines in immunocompromised people is always a concern. For example, cancer patients undergoing treatment and transplant and autoimmune patients treated with immunosuppressive agents represent a growing segment of the population. Consequently, the Δlpp Δpla double mutant could serve as a starting point or an excellent platform from which other virulence genes could be deleted to develop a safe and efficacious new-generation vaccine for mass immunization.
ACKNOWLEDGMENTS
This research was supported by NIH/NIAID grants AI064389 and NO1-AI-30065 awarded to A.K.C. We also acknowledge a UC7 grant (AI070083), which facilitated our research in the Galveston National Laboratory, Galveston, TX. C. J. van Lier was supported in part by a T32 Biodefense Training Grant (AI060549).
We thank members of the Electron Microscopy Core Laboratory for their assistance with performing electron microscopy studies.
Footnotes
Published ahead of print 31 March 2014
REFERENCES
- 1.Prentice MB, Rahalison L. 2007. Plague. Lancet 369:1196–1207. 10.1016/S0140-6736(07)60566-2 [DOI] [PubMed] [Google Scholar]
- 2.Huang XZ, Nikolich MP, Lindler LE. 2006. Current trends in plague research: from genomics to virulence. Clin. Med. Res. 4:189–199. 10.3121/cmr.4.3.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ligon BL. 2006. Plague: a review of its history and potential as a biological weapon. Semin. Pediatr. Infect. Dis. 17:161–170. 10.1053/j.spid.2006.07.002 [DOI] [PubMed] [Google Scholar]
- 4.Perry RD, Fetherston JD. 1997. Yersinia pestis—etiologic agent of plague. Clin. Microbiol. Rev. 10:35–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. 2006. Interregional meeting on prevention and control of plague, Antanarivo, Madagascar, 1 to 11 April. World Health Organization, Geneva, Switzerland: http://www.who.int/csr/resources/publications/WHO_HSE_EPR_2008_3w.pdf [Google Scholar]
- 6.Wagner DM, Klunk J, Harbeck M, Devault A, Waglechner N, Sahl JW, Enk J, Birdsell DN, Kuch M, Lumibao C, Poinar D, Pearson T, Fourment M, Golding B, Riehm JM, Earn DJ, Dewitte S, Rouillard JM, Grupe G, Wiechmann I, Bliska JB, Keim PS, Scholz HC, Holmes EC, Poinar H. 2014. Yersinia pestis and the Plague of Justinian 541-543 AD: a genomic analysis. Lancet Infect. Dis. 14:319–326. 10.1016/S1473-3099(13)70323-2 [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization Media Center. 6 August 2009, posting date Plague: questions and answers about plague. World Health Organization, Geneva, Switzerland: http://www.who.int/ith/diseases/plague/en/ [Google Scholar]
- 8.Pearson GS, Woollett GR, Chevrier MI, Tucker JB, Smithson AE. 1998. Biological weapons proliferation: reasons for concern, courses of action, p 18 Henry L. Stimson Center, Washington, DC [Google Scholar]
- 9.Centers for Disease Control and Prevention. 17 November 2008, posting date Protecting the American public by ensuring the safe and secure possession, use, and transfer of select agents and toxins that pose a threat to public health. CDC Select Agent Program, Centers for Disease Control and Prevention, Atlanta, GA: www.cdc.gov/phpr/documents/DSAT_brochure_July2011.pdf [Google Scholar]
- 10.Inglesby TV, Dennis DT, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Koerner JF, Layton M, McDade J, Osterholm MT, O'Toole T, Parker G, Perl TM, Russell PK, Schoch-Spana M, Tonat K. 2000. Plague as a biological weapon. JAMA 283:2281–2290. 10.1001/jama.283.17.2281 [DOI] [PubMed] [Google Scholar]
- 11.Keeling MJ, Gilligan CA. 2000. Metapopulation dynamics of bubonic plague. Nature 407:903–906. 10.1038/35038073 [DOI] [PubMed] [Google Scholar]
- 12.Easterday WR, Kausrud KL, Star B, Heier L, Haley BJ, Ageyev V, Colwell RR, Stenseth NC. 2012. An additional step in the transmission of Yersinia pestis? ISME J. 6:231–236. 10.1038/ismej.2011.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.FDA. 2012. African green monkey (Chlorocebus aethiops) animal model development to evaluate treatment of pneumonic plague. Briefing package. FDA, Bethesda, MD: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/Anti-InfectiveDrugsAdvisoryCommittee/UCM297180.pdf [Google Scholar]
- 14.Quenee LE, Ciletti NA, Elli D, Hermanas TM, Schneewind O. 2011. Prevention of pneumonic plague in mice, rats, guinea pigs and non-human primates with clinical grade rV10, rV10–2 or F1-V vaccines. Vaccine 29:6572–6583. 10.1016/j.vaccine.2011.06.119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smiley ST. 2008. Current challenges in the development of vaccines for pneumonic plague. Expert Rev. Vaccines 7:209–221. 10.1586/14760584.7.2.209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williamson ED, Packer PJ, Waters EL, Simpson AJ, Dyer D, Hartings J, Twenhafel N, Pitt MLM. 2011. Recombinant (F1+V) vaccine protects cynomolgus macaques against pneumonic plague. Vaccine 29:4771–4777. 10.1016/j.vaccine.2011.04.084 [DOI] [PubMed] [Google Scholar]
- 17.Smiley ST. 2008. Immune defense against pneumonic plague. Immunol. Rev. 225:256–271. 10.1111/j.1600-065X.2008.00674.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lin JS, Kummer LW, Szaba FM, Smiley ST. 2011. IL-17 contributes to cell-mediated defense against pulmonary Yersinia pestis infection. J. Immunol. 186:1675–1684. 10.4049/jimmunol.1003303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenzweig JA, Jejelowo O, Sha J, Erova TE, Brackman SM, Kirtley ML, van Lier CJ, Chopra AK. 2011. Progress on plague vaccine development. Appl. Microbiol. Biotechnol. 91:265–286. 10.1007/s00253-011-3380-6 [DOI] [PubMed] [Google Scholar]
- 20.Feodorova VA, Motin VL. 2012. Plague vaccines: current developments and future perspectives. Emerg. Microbes Infect. 1:e36. 10.1038/emi.2012.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meyer KF. 1970. Effectiveness of live or killed plague vaccines in man. Bull. World Health Organ. 42:653–666 [PMC free article] [PubMed] [Google Scholar]
- 22.Williamson ED, Flick-Smith HC, LeButt C, Rowland CA, Jones SM, Waters EL, Gwyther RJ, Miller J, Packer PJ, Irving M. 2005. Human immune response to a plague vaccine comprising recombinant F1 and V antigens. Infect. Immun. 73:3598–3608. 10.1128/IAI.73.6.3598-3608.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sha J, Agar SL, Baze WB, Olano JP, Fadl AA, Erova TE, Wang S, Foltz SM, Suarez G, Motin VL, Chauhan S, Klimpel GR, Peterson JW, Chopra AK. 2008. Braun lipoprotein (Lpp) contributes to virulence of yersiniae: potential role of Lpp in inducing bubonic and pneumonic plague. Infect. Immun. 76:1390–1409. 10.1128/IAI.01529-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu T, Agar SL, Sha J, Chopra AK. 2010. Deletion of Braun lipoprotein gene (lpp) attenuates Yersinia pestis KIM/D27 strain: role of Lpp in modulating host immune response, NF-κβ activation and cell death. Microb. Pathog. 48:42–52. 10.1016/j.micpath.2009.09.002 [DOI] [PubMed] [Google Scholar]
- 25.Aliprantis AO, Yang RB, Mark MR, Suggett S, Devaux B, Radolf JD, Klimpel GR, Godowski P, Zychlinsky A. 1999. Cell activation and apoptosis by bacterial lipoproteins through Toll-like receptor-2. Science 285:736–739. 10.1126/science.285.5428.736 [DOI] [PubMed] [Google Scholar]
- 26.Sodeinde OA, Goguen JD. 1988. Genetic analysis of the 9.5-kilobase virulence plasmid of Yersinia pestis. Infect. Immun. 56:2743–2748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lähteenmäki K, Virkola R, Sarén A, Emödy L, Korhonen TK. 1998. Expression of plasminogen activator Pla of Yersinia pestis enhances bacterial attachment to the mammalian extracellular matrix. Infect. Immun. 66:5755–5762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perry R, Fetherston J, Suomalainen M, Haiko J, Kukkonen M, Korhonen T, Lähteenmäki K, Virkola Westerlund-Wikström B, Lobo L, Ramu P. 2007. Using every trick in the book: the Pla surface protease of Yersinia pestis, p 268–278 In The genus Yersinia, vol 603 Springer, New York, NY: [DOI] [PubMed] [Google Scholar]
- 29.Sodeinde OA, Subrahmanyam YV, Stark K, Quan T, Bao Y, Goguen JD. 1992. A surface protease and the invasive character of plague. Science 258:1004–1007. 10.1126/science.1439793 [DOI] [PubMed] [Google Scholar]
- 30.Sebbane F, Jarrett CO, Gardner D, Long D, Hinnebusch BJ. 2006. Role of Yersinia pestis plasminogen activator in the incidence of distinct septicemic and bubonic forms of flea-borne plague. Proc. Natl. Acad. Sci. U. S. A. 102:5526–5530. 10.1073/pnas.0509544103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Szaba FM, Smiley ST. 2002. Roles for thrombin and fibrin(ogen) in cytokine/chemokine production and macrophage adhesion in vivo. Blood 99:1053–1059. 10.1182/blood.V99.3.1053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lathem W, Price P, Miller V, Goldman W. 2007. A plasminogen-activating protease specifically controls the development of primary pneumonic plague. Science 315:509–513. 10.1126/science.1137195 [DOI] [PubMed] [Google Scholar]
- 33.Luo D, Lin JS, Parent MA, Mullarky-Kanevsky I, Szaba FM, Kummer LW, Duso DK, Tighe M, Hill J, Gruber A, Mackman N, Gailani D, Smiley ST. 2013. Fibrin facilitates both innate and T cell-mediated defense against Yersinia pestis. J. Immunol. 190:4149–4161. 10.4049/jimmunol.1203253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Caulfield AJ, Lathem WW. 2012. Substrates of the plasminogen activator protease of Yersinia pestis. Adv. Exp. Med. Biol. 954:253–260. 10.1007/978-1-4614-3561-7_32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Agar SL, Sha J, Baze WB, Erova TE, Foltz SM, Suarez G, Wang S, Chopra AK. 2009. Deletion of Braun lipoprotein gene (lpp) and curing of plasmid pPCP1 dramatically alter the virulence of Yersinia pestis CO92 in a mouse model of pneumonic plague. Microbiology 155:3247–3259. 10.1099/mic.0.029124-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Doll JM, Zeitz PS, Ettestad P, Bucholtz AL, Davis T, Gage K. 1994. Cat-transmitted fatal pneumonic plague in a person who traveled from Colorado to Arizona. Am. J. Trop. Med. Hyg. 51:109–114 [DOI] [PubMed] [Google Scholar]
- 37.Parkhill J, Wren BW, Thomson NR, Titball RW, Holden MT, Prentice MB, Sebaihia M, James KD, Churcher C, Mungall KL, Baker S, Basham D, Bentley SD, Brooks K, Cerdeño-Tárraga AM, Chillingworth T, Cronin A, Davies RM, Davis P, Dougan G, Feltwell T, Hamlin N, Holroyd S, Jagels K, Karlyshev AV, Leather S, Moule S, Oyston PC, Quail M, Rutherford K, Simmonds M, Skelton J, Stevens K, Whitehead S, Barrell BG. 2001. Genome sequence of Yersinia pestis, the causative agent of plague. Nature 413:523–527. 10.1038/35097083 [DOI] [PubMed] [Google Scholar]
- 38.Miller VL, Mekalanos JJ. 1988. A novel suicide vector and its use in construction of insertion mutations: osmoregulation of outer membrane proteins and virulence determinants in Vibrio cholerae requires toxR. J. Bacteriol. 170:2575–2583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Datsenko KA, Wanner BL. 2000. One-step inactivation of chromosomal genes in Escherichia coli K-12 using PCR products. Proc. Natl. Acad. Sci. U. S. A. 97:6640–6645. 10.1073/pnas.120163297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Choi KH, Schweizer H. 2005. An improved method for rapid generation of unmarked Pseudomonas aeruginosa deletion mutants. BMC Microbiol. 5:30. 10.1186/1471-2180-5-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Edwards RA, Keller LH, Schifferli DM. 1998. Improved allelic exchange vectors and their use to analyze 987P fimbria gene expression. Gene 207:149–157. 10.1016/S0378-1119(97)00619-7 [DOI] [PubMed] [Google Scholar]
- 42.Sha J, Fadl AA, Klimpel GR, Niesel DW, Popov VL, Chopra AK. 2004. The two murein lipoproteins of Salmonella enterica serovar Typhimurium contribute to the virulence of the organism. Infect. Immun. 72:3987–4003. 10.1128/IAI.72.7.3987-4003.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sha J, Kirtley ML, van Lier CJ, Wang S, Erova TE, Kozlova EV, Cao A, Cong Y, Fitts EC, Rosenzweig JA, Chopra AK. 2013. Deletion of the Braun lipoprotein-encoding gene and altering the function of lipopolysaccharide attenuate the plague bacterium. Infect. Immun. 81:815–828. 10.1128/IAI.01067-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tao P, Mahalingam M, Kirtley ML, van Lier CJ, Sha J, Yeager LA, Chopra AK, Rao VB. 2013. Mutated and bacteriophage T4 nanoparticle arrayed F1-V immunogens from Yersinia pestis as next generation plague vaccines. PLoS Pathog. 9:e1003495. 10.1371/journal.ppat.1003495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lawal A, Kirtley ML, van Lier CJ, Erova TE, Kozlova EV, Sha J, Chopra AK, Rosenzweig JA. 2013. The effects of modeled microgravity on growth kinetics, antibiotic susceptibility, cold growth, and the virulence potential of a Yersinia pestis ymoA-deficient mutant and its isogenic parental strain. Astrobiology 13:821–832. 10.1089/ast.2013.0968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rosenzweig JA, Weltman G, Plano GV, Schesser K. 2005. Modulation of yersinia type three secretion system by the S1 domain of polynucleotide phosphorylase. J. Biol. Chem. 280:156–163. 10.1074/jbc.M405662200 [DOI] [PubMed] [Google Scholar]
- 47.Lawrence WS, Hardcastle JM, Brining DL, Weaver LE, Ponce C, Whorton EB, Peterson JW. 2009. The physiologic responses of Dutch belted rabbits infected with inhalational anthrax. Comp. Med. 59:257–265 [PMC free article] [PubMed] [Google Scholar]
- 48.Titball RW, Williamson ED. 2001. Vaccination against bubonic and pneumonic plague. Vaccine 19:4175–4184. 10.1016/S0264-410X(01)00163-3 [DOI] [PubMed] [Google Scholar]
- 49.Kummer LW, Szaba FM, Parent MA, Adamovicz JJ, Hill J, Johnson LL, Smiley ST. 2008. Antibodies and cytokines independently protect against pneumonic plague. Vaccine 26:6901–6907. 10.1016/j.vaccine.2008.09.063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bartra SS, Styer KL, O'Bryant DM, Nilles ML, Hinnebusch BJ, Aballay A, Plano GV. 2008. Resistance of Yersinia pestis to complement-dependent killing is mediated by the Ail outer membrane protein. Infect. Immun. 76:612–622. 10.1128/IAI.01125-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Galindo CL, Sha J, Moen ST, Agar SL, Kirtley ML, Foltz SM, McIver LJ, Kozlova EV, Garner HR, Chopra AK. 2010. Comparative global gene expression profiles of wild-type Yersinia pestis CO92 and its Braun lipoprotein mutant at flea and human body temperatures. Comp. Funct. Genomics 2010:342168. 10.1155/2010/342168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kuby J, Kindt TJ, Goldsby RA, Osborne BA. 2007. Kuby immunology, p 396 WH Freeman & Co, San Francisco, CA [Google Scholar]
- 53.DuBois AB, Freytag LC, Clements JD. 2007. Evaluation of combinatorial vaccines against anthrax and plague in a murine model. Vaccine 25:4747–4754. 10.1016/j.vaccine.2007.03.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Anderson GW, Jr, Worsham PL, Bolt CR, Andrews GP, Welkos SL, Friedlander AM, Burans JP. 1997. Protection of mice from fatal bubonic and pneumonic plague by passive immunization with monoclonal antibodies against the F1 protein of Yersinia pestis. Am. J. Trop. Med. Hyg. 56:471–473 [DOI] [PubMed] [Google Scholar]
- 55.Lukaszewski RA, Kenny DJ, Taylor R, Rees DGC, Hartley MG, Oyston PCF. 2005. Pathogenesis of Yersinia pestis infection in BALB/c mice: effects on host macrophages and neutrophils. Infect. Immun. 73:7142–7150. 10.1128/IAI.73.11.7142-7150.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Miossec P, Korn T, Kuchroo VK. 2009. Interleukin-17 and type 17 helper T cells. N. Engl. J. Med. 361:888–898. 10.1056/NEJMra0707449 [DOI] [PubMed] [Google Scholar]
- 57.Wilke CM, Bishop K, Fox D, Zou W. 2011. Deciphering the role of Th17 cells in human disease. Trends Immunol. 32:603–611. 10.1016/j.it.2011.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ali R, Kumar S, Naqvi RA, Sheikh IA, Rao DN. 2013. Multiple antigen peptide consisting of B- and T-cell epitopes of F1 antigen of Y. pestis showed enhanced humoral and mucosal immune response in different strains of mice. Int. Immunopharmacol. 15:97–105. 10.1016/j.intimp.2012.10.029 [DOI] [PubMed] [Google Scholar]
- 59.Kamei A, Coutinho-Sledge YS, Goldberg JB, Priebe GP, Pier GB. 2011. Mucosal vaccination with a multivalent, live-attenuated vaccine induces multifactorial immunity against Pseudomonas aeruginosa acute lung infection. Infect. Immun. 79:1289–1299. 10.1128/IAI.01139-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pier GB, Meluleni G, Goldberg JB. 1995. Clearance of Pseudomonas aeruginosa from the murine gastrointestinal tract is effectively mediated by O-antigen-specific circulating antibodies. Infect. Immun. 63:2818–2825 [DOI] [PMC free article] [PubMed] [Google Scholar]