Summary
Urban Health Plan, Inc. (UHP) implemented a comprehensive asthma management program that has resulted in sustained improvements in patient outcomes for UHP’s primarily Latino and Black populations in the South Bronx. UHP is now engaged in a community-academic partnership to build community research capacity from its strength in quality improvement.
Keywords: asthma, Latino, Black, community health center, quality improvement, electronic health record, community-academic partnership
The South Bronx is one of the poorest congressional districts in the nation and has some of the highest asthma prevalence rates 1 in the nation (see Table 1). This report describes the development of UHP’s comprehensive asthma management program, Asthma Relief Street, which has resulted in sustained, improved asthma outcomes for nearly 8,000 asthmatic patients. The report also describes a community-academic partnership funded by the National Institute on Minority Health and Health Disparities with goals for strengthening UHP’s quality improvement program and moving the partnership into the realm of community-based research, as a model for dissemination.
Table 1.
Comparison of asthma prevalence for pediatric and adult patients
| Asthma Prevalence Rate | ||
|---|---|---|
| Pediatric | Adult | |
| United States (2009) | 9.6%14 | 8.4%17 |
| New York State (2009) | 11.0%15 | 9.8%17 |
| New York City (2009) | 11.2%15 | 4.0%18 |
| Bronx (2009) | 26.9%16 | 6.6%18 |
| South Bronx (2009) | 28.5%16 | 6.5%18 |
| Urban Health Plan, Inc. (2011) | 26.4%* | 13.4%** |
UHP patients ages 0–17 seen for primary care from 1/1/2011 to 12/31/2011, n = 16,388, of which 26.5% (4,322) had a diagnosis of asthma.
UHP patients ages ≥18 seen for primary care from 1/1/2011 to 12/31/2011, n = 29,291, of 13.5% (3,940) had a diagnosis of asthma.
UHP, founded in 1974, is an unaffiliated network of federally qualified community health centers based in the South Bronx and Queens, whose mission is to improve the health status of underserved communities. In Table 2, the demographics of those being seen for primary care, as well as those patients who have a diagnosis of asthma, are described. Its patients are primarily Latino and Black. In 2011, UHP served 48,000 patients through 248,000 patient visits at all of its sites.
Table 2.
2011 Demographic characteristics of patients receiving primary care at UHP
| Demographic | Children, 0 – <18 years old (n=16,985) | Adults 18 years and older (n=30,807) |
|---|---|---|
| Gender | ||
| Male | 8,444 (49.7%) | 10,962 (35.6%) |
| Female | 8,541 (50.3%) | 19,845 (64.4%) |
| Race/ethnicity | ||
| Black | 2,087 (12.3%) | 2,967 (9.6%) |
| Hispanic | 13,818 (81.4%) | 25,490 (82.7%) |
| White | 28 (0.2%) | 217 (0.7%) |
| Other or mixed | 1,052 (6.2%) | 2,133 (6.9%) |
| Clinical | ||
| Asthma diagnosis | 4,322 (25.4%) | 3,940 (12.8%) |
| No asthma diagnosis | 12,663 (74.6%) | 26,867 (87.2%) |
Background
In 2001, UHP began participation in a health disparities performance improvement collaborative sponsored by the Health Resources and Services Administration Bureau of Primary Health Care. The purpose of the collaborative was for community health centers throughout the country to improve asthma health outcomes. Participating health centers were instructed, through sponsored group meetings, on the use of evidence-based quality improvement methods to support an evidence-based intervention. The quality improvement approach was supported via:
The Institute for Healthcare Improvement Breakthrough Series2
The Model for Improvement3
The Chronic Care Model4
Using these methods, UHP assembled an interdisciplinary performance improvement team to initially test changes and seek improvement focused on pediatric asthma care. The UHP Executive and Board of Directors established a performance improvement initiative as part of an UHP strategic plan, and allocated resources to these activities. The asthma team included members of the executive and senior administration, as well as section heads and directors of pediatrics and school health, and other clinical associates.
Intervention
Pilot-work began within the pediatrics department at the main community health center site and the team focused on the incorporation of evidence-based guidelines5 into clinical practice, and the creation of a registry for tracking pediatric asthma clinical measures, such as symptom-free days and controller medications for persistent asthmatics. Prior to the team’s intervention, evidence-based guidelines were not widely disseminated to providers, and therefore, clinical measures were not tracked or shared with providers. As a result, there was little knowledge of, or accountability for pediatric asthma health outcomes.
The team developed an asthma patient chart form based on national guidelines6 to collect data and track all measures to populate the registry; this tracking was crucial to the project’s success. This form was followed by a template in UHP’s electronic health record (EHR) in 2006. The team now tracks performance by reviewing electronically monthly-generated data graphs. Regularly sharing this information with providers was identified as key in building an effective asthma program.
To improve asthma outcomes for the pediatric patient population, the team recognized that the current delivery system was inadequate to meet the educational needs of patients,7 so asthma health educators (AHE), trained by the Director of Pediatrics, were incorporated into the program design. Equally important, the team worked on utilizing community resources to assist patients and their parents/guardians with asthma care. Visiting nurses, a state-funded pest control management program, and durable medical equipment vendors for products such as nebulizers and aerochambers were instrumental in establishing a comprehensive asthma program.
Delivery system
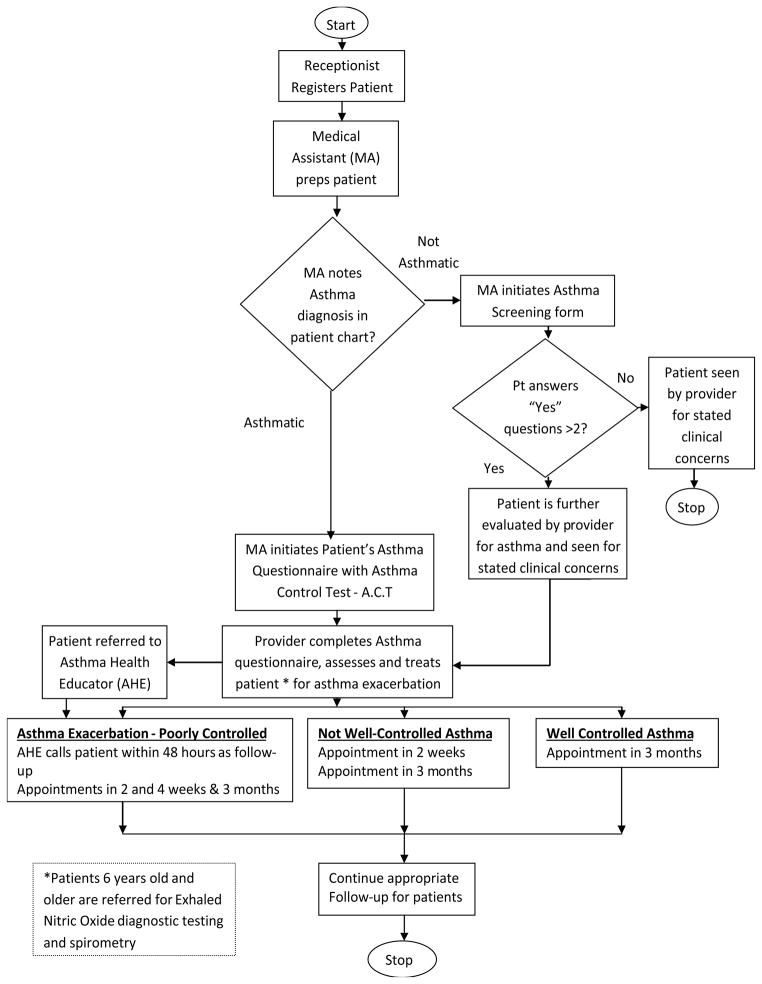
We adopted a workflow algorithm for the identification and tracking of patients using the EHR and for optimizing appropriate treatment (Figure 1.). Staff roles were delineated to ensure efficiency. All patients were initially screened for asthma risk factors by the medical assistant (MA) and the responses were documented in the EHR. Patients diagnosed with asthma were screened for symptoms at every scheduled and walk-in visit. The MA asked questions about days with asthma-related symptoms, as well as symptom-free days, emergency room visits, and hospitalizations. Patients were also screened with the evidence-based Asthma Control Test (ACT),6 which is a scored self-assessment of asthma control. When the patient saw the provider, asthma control and medication use were reviewed and the asthma action plan was updated. The provider also addressed any other asthma concerns with the patient/family.
Figure 1.
As part of the asthma management program, patients were encouraged to set self-management goals collaboratively with the AHE, with a goal of empowering patients and families in asthma self-management. The AHE used UHP’s asthma curriculum to educate patients and families to maintain asthma control over time. The five lessons were developed by UHP clinicians based on observed patient needs and included: definition of asthma; signs/symptoms of exacerbations; recommendations on remediation in the home to address environmental triggers; differences between “controller” and “rescue” medications;8 and understanding of spirometry and exhaled nitric oxide. These lessons were incorporated into every asthma counseling session, as needed. Patients six years of age and older were tested for exhaled nitric oxide to measure airway inflammation, to identify risk of acute exacerbations, and to evaluate adherence to use of “controller” medications.9 Patients also received biannual spirometry to assist in severity classification.
Each individualized asthma action plan included treatment guidance to help the patient achieve and maintain asthma control. The Asthma Relief Street program (Figure 1) followed patients as determined by asthma severity and control.10 Patients with well-controlled, persistent asthma, were scheduled for follow-up every 3 months. Patients who were not well-controlled or had poorly-controlled, persistent asthma were seen every two to three weeks, until their asthma was well controlled.11 Patients with an acute exacerbation were seen within 48–72 hours.
Sustainability
This type of program cannot succeed without full support from senior leaders. At UHP, these leaders attended every implementation team meeting and served as an integral part of the project team. Building consensus for change for improvement among staff and providers by highlighting the gap between current care and best practices is necessary. Provider champions can be effective in conveying this message to their peers. This program required senior leaders and staff to carefully assess the current care process and be open to radically changing the way services are provided.
The quality and comprehensiveness of care can be increased by use of a team approach. For example, dividing responsibilities for the standardized asthma screening between MAs and providers helps to facilitate comprehensive care without placing an undue burden on doctors.
Institutional changes endure only when integrated into an organization’s formal policies and procedures. For example, the use of EHRs to standardize and update screening and treatment guidelines and forms allows UHP staff to easily keep abreast of and incorporate new scientific evidence into the everyday practice of medicine.
In 2003, this performance improvement initiative was spread to include adults diagnosed with asthma. The system was modified as appropriate to include adult asthmatics and used the same criteria to manage, treat, educate, and assess improvement.
Performance improvement results
For a decade, UHP has provided standardized, evidence-based asthma care at all UHP sites, for approximately 5,000 pediatric and 3,000 adult asthmatics whose health outcomes are tracked and reported monthly through UHP’s Clinical Quality Council. UHP’s asthma outcomes: 95.8% of asthma patients have an asthma severity assessment; 95.4% of persistent asthmatics are on anti-inflammatory medication per clinical guidelines; 68.2% of asthma patients have a documented asthma self-management goal; and only 5.2% of asthma patients have a self-reported visit to the emergency room in the six months preceding their most recent visit. See Table 3 for comparison of outcomes for 2001 (pediatrics), 2003 (adults) and 2011 (combined), and program goals.
Table 3.
UHP Pre and post adult and pediatric asthma program goals
| Adult and Pediatric Asthmatic Patients | ||||
|---|---|---|---|---|
| Measure | Pre-Asthma Program Implementation | Post Asthma Program Implementation | Asthma Program Goal | |
| Pediatrics | Adult | Pediatrics and Adults | ||
| August, 2001 | August, 2003 | December, 2011 | ||
| N | 40* | 50* | 8262 | |
| Average number of symptom-free days (out of the last 14 days) | n/a | n/a | 10.9 | 10 |
| Percent of persistent asthma patients on anti-inflammatory meds | n/a | 60% | 95.4% | 100% |
| Percent of asthma patients with severity assessment | 45% | 25% | 95.8% | 90% |
| Percent of asthma patients with current self-management | 40% | 0% | 68.2% | 70% |
| Percent of asthma patients with visit to ED/urgent care for asthma in last six months | 45% | 16% | 5.2% | 5% |
| Average number of lost Days work/school in a month | n/a | n/a | 0.2 | 1 |
| Percentage of asthma patients with influenza immunization** | 47% | 0% | 40.1% | 90% |
Review of randomly selected patients’ charts.
Performance measure added in January 2004.
n/a = not available
Creating a business case for quality
In 2008, UHP was asked to engage in a project to assess the cost of the UHP asthma program, using the Quality Assurance Reporting Requirements (QARR),12 New York State’s version of the federal government’s Healthcare Effectiveness Data and Information Set (HEDIS).13 UHP joined one of the state’s largest Medicaid managed care insurance plans, designated for this report as Health Insurance Plan,” and participated in a review of costs, based on the performance initiative. The QARR tool continues to be used by all Medicaid Managed Care state plans and incorporates both HEDIS and NY state specific measures.
Quality health care can be defined as the extent to which patients get the care they need in a manner that most effectively protects or restores their health. This means having timely access to care, getting treatment that medical evidence has found to be effective, and getting appropriate preventive care.12 The QARR measures are related to the desired outcomes for asthma care and include: improved asthma control; reduction in hospitalizations and unnecessary health care encounters; improved patient awareness; and appropriate use of medications.
An UHP Executive Committee reviewed records of asthmatic patients (n=235 visits) who have been concurrently enrolled with the Health Insurance Plan and had been treated at UHP for the past two years (2006–2007), and who have had at least one of the following in each of these two years: emergency department visit with asthma as the principal diagnosis; or acute inpatient discharge with asthma as the principal diagnosis; or four outpatient asthma visits with asthma as one of the listed diagnosis and at least two asthma medications dispensing events; or four asthma medication dispensing events.
UHP aggregated the CPT codes for a subset of these 235 visits of 50 unduplicated patients, and translated these codes into relative value units in order to determine UHP’s cost, compared to the revenue generated. The Health Insurance Plan provided the costs associated with the care of these patients. The Health Insurance Plan conducted a financial comparative analysis, to determine the economic value of services to these patients between those serviced by UHP, non-UHP Bronx providers and their entire provider network.
Business case for quality study conclusion
UHP generated revenue not only covered the costs of the care provided to the Health Insurance Plan’s asthmatic patients, but also was more cost effective than all other Health Insurance Plan’s network of providers for the care of asthmatic patients during 2006–2007 (See Table 4). Specifically, the costs were 22% less for the adult asthmatic population and 39% less for the pediatric population; these data were documented in a corporate communication from the Health Insurance Plan in 2008.
Table 4.
UHP and “Health Insurance Plan” cost comparison
| Adult per Member/Per Month Comparative COST Data – 2006 to 2007 | |||
|---|---|---|---|
| OTHER Health Insurance Plan Network Providers | UHP Health Insurance Plan Network Providers | % Difference | |
| Health Insurance Plan’s Network within Bronx County | $239.24 | $219.96 | −8% |
| Health Insurance Plan’s Network within New York City | $246.93 | $219.96 | −11% |
| Health Insurance Plan’s Entire Network | $280.62 | $219.96 | −22% |
| Pediatric per Member/Per Month Comparative Data – 2006 to 2007 | |||
| OTHER Health Insurance Plan Network Providers | UHP Health Insurance Plan Network Providers | % Difference | |
| Health Insurance Plan’s Network within Bronx County | $77.03 | $49.18 | −36% |
| Health Insurance Plan’s Network within New York City | $78.22 | $49.18 | −37% |
| Health Insurance Plan’s Entire Network | $81.11 | $49.18 | −39% |
The Health Insurance Plan and UHP, corporate communication, 2008
Organizational learning
Since implementing the Asthma team in 2001, UHP has initiated other performance-improvement teams. The results of which is the establishment of a quality improvement program supported by UHP’s Institute for the Advancement of Community Health, established in 2005. Though challenging, the performance-improvement framework has proven beneficial in creating innovative approaches to addressing health disparities in the community.
Community-academic partnership
The implementation of an EHR provides for the continuity of patient care. It also permits a review of data that can support quality improvement initiatives. In addition, data review from the EHR offers the opportunity for retrospective analysis and this can lead to clinical questions that the community, and its providers, can formulate. The EHR can also be used as a prospective tool for collecting clinical data. Realizing this potential, in July 2010, UHP and Albert Einstein College of Medicine (Einstein) received a three-year National Institute for Minority Health and Health Disparities grant (1RC4MD-005783-02) to develop a collaborative model to build capacity for community-based research. This partnership combines UHP’s success in performance-improvement, such as its asthma program, with Einstein’s expertise in clinical and community-based research. The partnership developed a vision statement (See Box 1) as a guide toward meeting our shared goals. Among our priorities are: developing research infrastructure at UHP, clinical research training, jointly developing research proposals and publishing scientific reports.
Box 1. Shared vision to build community-based research capacity.
Bronx Community Collaborative Opportunities for Research & Education (Bronx C2ORE)
Shared Vision
Bronx C2ORE will:
…be guided by shared values of respect and understanding of each others’ skills, knowledge and perspectives regarding research and community health; a willingness to consider new ways of doing things; and mutual recognition of the work we can do together.
…create a sustainable community-based partnership between an academic research institution and a community health center that integrates and enhances the research culture in both institutions.
…successfully implement the community-based partnership by:
Training UHP staff on research methods
Building the required infrastructure at each institution
Co-developing at least 3 research proposals between the partner organizations
Publishing in peer-reviewed journals
Impacting policy and enhancing community health
…communicate our community-based research partnership model within our institutions, and with other community health centers, academic institutions, government agencies, policy making institutions, and beyond.
Conclusion
UHP has developed, and sustained, a cost effective asthma management program for over a decade. Performance improvement activities have been incorporated at UHP and supported at all levels. The EHR tracks the data and with the addition of the community-academic partnership, UHP’s asthma program can benefit from the asthma researchers at Einstein. The Einstein researchers also greatly benefit from learning real-world issues in asthma management, health disparities, and successes in quality improvement.
Contributor Information
Deborah Lester, Director of the Institute for the Advancement of Community Health at Urban Health Plan, Inc.
Acklema Mohammad, Section Director of Pediatrics at Urban Health Plan, Inc.
Eileen E. Leach, Chief of Staff at Urban Health Plan, Inc.
Paloma I. Hernandez, President and Chief Executive Officer at Urban Health Plan, Inc.
Elizabeth A. Walker, Professor of Medicine at the Albert Einstein College of Medicine.
References
- 1.Whu R, Cirilo G, Wong J, et al. Risk factors for pediatric asthma in the South Bronx. J Asthma. 2007;44(10):855–9. doi: 10.1080/02770900701752516. [DOI] [PubMed] [Google Scholar]
- 2.Nembhard IM. Learning and improving in quality improvement collaboratives: which collaborative features do participants value most? Health Serv Res. 2009;44 (2 Pt 1):359–78. doi: 10.1111/j.1475-6773.2008.00923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Langley J, Nolan K, Nolan T, Norman C, Provost L. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. San Francisco: Jossey-Bass; 1996. [Google Scholar]
- 4.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288 (14):1775–9. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 5.National Asthma Education and Prevention Program. Guidelines for the Diagnosis and Management of Asthma (EPR-3) Bethesda, MD: National Heart Lung and Blood Institute; 2007. Available at: http://www.nhlbi.nih.gov/guidelines/asthma/ [Google Scholar]
- 6.National Heart, Lung and Blood Institute. Expert panel report 2: guidelines for the diagnosis and management of asthma. Bethesda, MD: National Institutes of Health; 1997. NIH publication 97-4051. [Google Scholar]
- 7.Acevedo-Nieves RM. Exposing barriers to asthma care in Hispanic children. Nurse Pract. 2008;33 (4):37–42. doi: 10.1097/01.NPR.0000314756.03293.ca. [DOI] [PubMed] [Google Scholar]
- 8.Ortega AN, Gergen PJ, Paltiel AD, et al. Impact of site of care, race, and Hispanic ethnicity on medication use for childhood asthma. Pediatrics. 2002;109(1):E1. doi: 10.1542/peds.109.1.e1. [DOI] [PubMed] [Google Scholar]
- 9.Chan M, Sitaraman S, Dosanjh A. Asthma control test and peak expiratory flow rate: independent pediatric asthma management tools. J Asthma. 2009;46 (10):1042–4. doi: 10.3109/02770900903331101. [DOI] [PubMed] [Google Scholar]
- 10.Naqvi M, Thyne S, Choudhry S, et al. Ethnic-specific differences in bronchodilator responsiveness among Blacks, Puerto Ricans, and Mexicans with asthma. J Asthma. 2007;44(8):639–48. doi: 10.1080/02770900701554441. [DOI] [PubMed] [Google Scholar]
- 11.New York State Consensus Asthma Guideline Expert Panel. Clinical Guideline for the Diagnosis, Evaluation and Management of Adults and Children with Asthma. Albany, NY: New York State Department of Health; 2011. Available at http://www.health.ny.gov/publications/4750.pdf. [Google Scholar]
- 12.New York State Department of Health. About eQARR 2008. Albany, NY: Division of Quality & Evaluation; 2008. Available at http://www.health.ny.gov/health_care/managed_care/reports/eqarr/2008/about.htm. [Google Scholar]
- 13.Healthcare Effectiveness Data and Information Set. What is HEDIS? Washington, DC: National Committee for Quality Assurance; 2011. Available at: http://www.ncqa.org/tabid/59/Default.aspx. [Google Scholar]
- 14.Akinbami LJ, Moorman JE, Liu X. National health statistics reports. 32. Hyattsville, MD: National Center for Health Statistics; 2011. Asthma prevalence, health care use, and mortality: United States, 2005–2009. [PubMed] [Google Scholar]
- 15.Public Health Information Group. Current Asthma Prevalence in Children, 2006–2008. New York State Asthma Surveillance Summary Report. Albany. New York: Center for Community Health. New York State Department of Health; 2009. Available at: http://www.health.ny.gov/statistics/ny_asthma/pdf/2009_asthma_surveillance_summary_report.pdf. [Google Scholar]
- 16.New York City Department of Health and Mental Hygiene. Youth Risk Behavior Survey. 2009 Available at: https://a816-healthpsi.nyc.gov/epiquery/EpiQuery/YRBS/index.html.
- 17.Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System Survey Data. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2009. [Google Scholar]
- 18.New York City Department of Health and Mental Hygiene. Community Health Survey. 2009 Available at: https://a816-healthpsi.nyc.gov/epiquery/EpiQuery/CHS/index2009.html.