Excellent progress has been made in improving patient survival after burn injury over the last five decades. Since the first study in 19491, the likelihood of survival has improved substantially with the last major analysis in 19982 showing that the major determinants for mortality for all ages are age >60 years, burn size >40% Total Body Surface Area (TBSA), and presence of direct injury to the lung (e.g. inhalation injury). The extraordinary increase in likelihood of survival of all ages, but particularly in children, has largely resulted from early surgical excision of the burn with immediate closure of the wound with the patient’s own skin or other biological materials. Improvements in modern critical care and anesthesia management have further supported these advances in both children and adults.
From the NIH-sponsored large-scale collaborative program “Inflammation and the Host Response to Injury”, standard operating procedures (SOPs) have been published to more consistently help manage burn patients.3 Multitudes of nutritional, metabolic, physiologic, and immunological alterations are addressed with supportive protocols for resuscitation, hyperglycemia, perioperative antibiotic prophylaxis, among others. In the accompanying paper4 in The Lancet, clinicians followed these SOPs and demonstrated that half of the children with burn injuries even involving 90% TBSA survived their injuries. Children with TBSA <62% can be treated successfully with the SOPs, but for those children with injuries >62% TBSA, SOPs with additional measures become necessary for survival. These additional measures include novel surgical management of wounds, more advanced monitoring, and pharmaceutical treatment options and regimens as described in The Lancet paper.
Furthermore, advances in neonatal and pediatric intensive care have now compensated for the physiological and anatomical features of children under two; therefore, they should be expected to survive injuries with comparable burn sizes and presence of inhalation injury as well as older children5 as was also shown in the accompanying paper. In other words, there are only two determinants for likelihood of survival in children – burn size and presence of inhalation injury.
In adults, improvements in survival have been less dramatic, but nonetheless, meaningful. When survival by age is examined as an outcome from a burn center, there should be no age-related, statistically significant differences in survival from birth to age 60. And, in fact, this survival outcome from the burn center would be consistent with a center of excellence. When patients more than 60 years old are considered, co-morbidities and reduced organ function present at the time of the injury begin to exponentially contribute to a reduced likelihood of survival as shown in many other life-threatening human diseases.
It is true that in many developing countries, these survival outcomes may not be readily achievable. However, the failure to achieve these results is less a knowledge deficit on the part of national burn leadership than it is a system issue affected by patient referral patterns, limited availability of versus tremendous need for resources, district hospital physician or surgeon training in burn care, reimbursement practices for both the hospital and clinicians, together with political awareness of the issues and the legislative commitment and political willpower to invoke change.
In developed countries, however, survival is expected as shown in the accompanying paper. With this fact, it is time to think beyond survival to the quality of life of those who survive. Clinicians have traditionally assigned their own values to the quality of a burn patient’s survival. It is now time to allow the patient and family to weigh in with their views of how this injury has impacted their lives. Recent articles6–8 have validated burn-specific outcomes instruments to measure the quality of life after burn injury from the patient and family perspectives. Going forward, broader use of such post-burn injury questionnaires should be taken to drive future strategies not only to ensure survival, but also to enhance the quality of life for those who do survive.
In addition to the survival data, The Lancet article includes data on cytokines, acute phase reactant molecules, and hypermetabolic response measurements and other biomarkers that might distinguish those children with an expectedly good outcome from those whose injury exceeds 62% TBSA, who have a significantly higher risk of clinical complications (multi-organ failure and sepsis) and death, thereby requiring extraordinary efforts. Use of such data may someday help clinicians to distinguish, even predict these two different clinical trajectories in individual patients.
Burn injury presents with a reproducible hypermetabolic syndrome9 that shares many molecular features seen in the chronic immune-inflammatory syndrome coined “immunometabolism”10. These features, at least in part, are driven by statistically significant up-regulation or down-regulation of 80% of the patient’s circulating leukocyte genes in direct response to the burn injury.11 Many outcomes described in The Lancet article may result from this transcriptomic response. Clinical medicine currently focuses to treat these immunometabolic effects individually (e.g. insulin therapy to reduce the insulin-resistant hyperglycemia), whereas, there is a bright future in which interventions might well be more effective when directed at the transcriptomic response to burn injury itself.
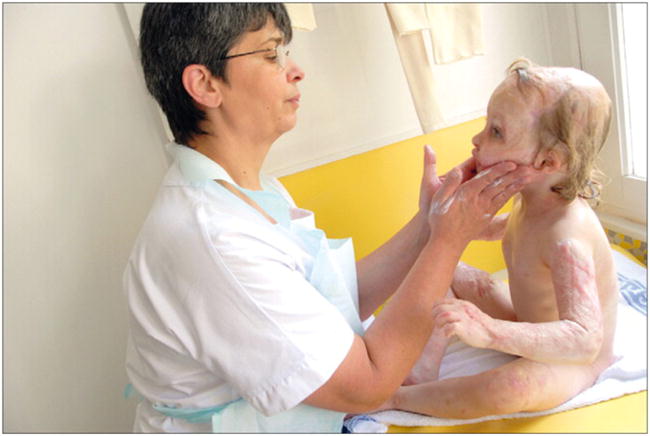
Figure 1.
Footnotes
I declare that I have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bull JP, Squire JR. A study of mortality in a burns unit: Standards for the evaluation of alternative methods of treatment. Ann Surg. 1949;130:160–73. doi: 10.1097/00000658-194908000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ryan CM, Schoenfeld DA, Thorpe WP, et al. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998;338:362–6. doi: 10.1056/NEJM199802053380604. [DOI] [PubMed] [Google Scholar]
- 3.Silver GM, Klein MB, Herndon DN, et al. Standard operating procedures for the clinical management of patients enrolled in a prospective study of Inflammation and the Host Response to Injury. J Burn Care Res. 2007;28:222–30. doi: 10.1097/BCR.0B013E318031AA44. [DOI] [PubMed] [Google Scholar]
- 4.Kraft R, Herndon DN, Al-Mousawi AM, et al. Burn size and survival probability in pediatric patients in modern burn care. Lancet. 2010 doi: 10.1016/S0140-6736(11)61345-7. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheridan RL, Weber JM, Schnitzer JJ, et al. Young age is not a predictor of mortality in burns. Pediatr Crit Care Med. 2001;2:223–4. doi: 10.1097/00130478-200107000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Sheridan RL, Hinson MI, Liang MH, et al. Long-term outcome of children surviving massive burns. JAMA. 2000;283:69–73. doi: 10.1001/jama.283.1.69. [DOI] [PubMed] [Google Scholar]
- 7.Daltroy LH, Liang MH, Phillips CB, et al. American Burn Association/Shriners Hospitals for Children burn outcomes questionnaire: Construction and psychometric properties. J Burn Care Res. 2000;21:29–39. doi: 10.1097/00004630-200021010-00007. [DOI] [PubMed] [Google Scholar]
- 8.Kazis LE, Liang MH, Lee A, et al. The development, validation, and testing of a health outcomes burn questionnaire for infants and children 5 years of age and younger. J Burn Care Res. 2002;23:196–207. doi: 10.1097/00004630-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Herndon DN, Tompkins RG. Support of the metabolic response to burn injury. The Lancet. 2004;363:1895–902. doi: 10.1016/S0140-6736(04)16360-5. [DOI] [PubMed] [Google Scholar]
- 10.Mathis D, Shoelson SE. Immunometabolism: an emerging frontier. Nat Rev Immunol. 2011;11:81–3. doi: 10.1038/nri2922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xiao WZ, Mindrinos MN, Seok JH, et al. A genomic storm in critically injured humans. J Exp Med. doi: 10.1084/jem.20111354. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]


