The prevalence of type 2 diabetes is increasing exponentially in Asia and globally1. Of even greater concern is the fact that the incidence of type 2 diabetes has increased rapidly over a very short period of time in Asian countries2. There are many causes for this; chief among them are the decline of β‐cell function in Asians, and increased obesity resulting from rapid lifestyle changes with increased abdominal obesity and a reduction in muscle mass being issues of particular concern1. These changes have triggered rapid growth in type 2 diabetes prevalence, even among younger people1. At the same time, achievement of glucose target rates for the successful management of diabetes mellitus is far from satisfactory both globally and in Asian countries. Therefore, this requires urgent improvement. There is also a serious economic aspect to this problem; the use of antidiabetic medications and expensive oral agents aggravates the economic burden for most countries experiencing an explosive increase in the number of diabetes patients. The use of insulin also increases medical expenses. Given that the most effective and basic method of diabetes management is a well‐balanced lifestyle, there is an urgent need for the development of new treatment models aimed at lifestyle monitoring for diabetes management.
Rapid developments in information technology (IT) have led to the adoption of several interactive communication systems to treat diabetes patients (Figure 1). With these interactive IT‐based systems, patients can upload glucose data that they have measured with a glucometer using high‐speed internet lines or cell phones. Medical teams can then review the uploaded data and send feedback to patients. With this feedback, patients can control their diabetes more efficiently by managing their lifestyle and/or treatment medication. This system has been introduced not only in Korea, but also in the USA and UK, and is a rising star in the effective management of diabetes mellitus.
Figure 1.
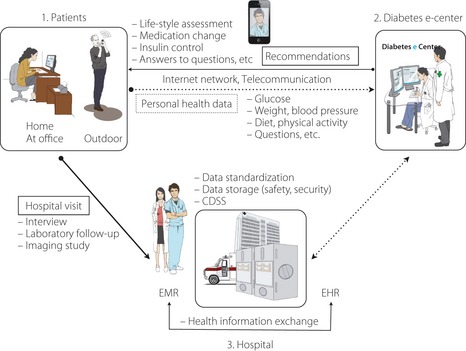
Patients can upload their data, such as glucose levels, bodyweight, blood pressure and so on measured at home or outdoors with some devices through a high‐speed internet line or telecommunication network. Physicians can review the uploaded data by the patients and send some recommendations, such as lifestyle assessment, medication change or answers to questions to the patients. The uploaded health data also can be transferred to an electronic healthcare system (EHR) in hospital, and the data can be stored with a standardized form and be exchanged with an electronic medical record system in hospital. The data in the electronic medical record (EMR) and EHR system can be analyzed with the clinical decision support system (CDSS) and a new meaning can be found, and then it can also be sent to the patients to help them control diabetes more efficiently.
According to a 2006 study by Cho et al., an internet‐based glucose management system helped patients with type 2 diabetes to lower their blood glucose level and maintain this level within the target range for approximately 3 years3. In another study, a cell phone‐based diabetes management system that allowed patients to check their glucose level with their cell phones and transmit that data directly also showed promising results4. This encouraging clinical evidence prompted the development and launch of a large‐scale national project named SMART Care in Korea 2 years ago. SMART Care is a new management system for type 2 diabetes, which uses a new communications device; results from the clinical trials currently underway seem to suggest the wait is worthwhile.
However, despite many positive clinical results and evidence of positive long‐term effects, much work is required before such diabetes management systems can be widely adopted. Legal and systematic issues in individual countries can also present hurdles. First, there are concerns about patient privacy. For example, there are limitations in terms of sending patient information outside the hospital. In addition, administering medical treatment over the internet can give rise to legal issues. The most important factor, however, is cost effectiveness. Questions remain as to who would be responsible for building the IT infrastructure, such as high‐speed internet networks, that is necessary for such systems to operate effectively. There is also the issue of payment of maintenance costs incurred by medical staff to run such interactive systems. A longer‐term view would suggest that the use of these new IT‐based glucose management systems could reduce medical welfare spending by lowering the rate of diabetes‐related complications and leading to better management of diabetes patients. However, because these systems require high initial set‐up and maintenance costs, their simple large‐scale deployment appears unlikely. Nonetheless, with the development of home healthcare devices and IT‐based communication technology, the development of new diabetes management system using IT is accelerating. Glucometers have been widely used for many years at home, and recent progress in biotechnology and nanotechnology is expediting the development of new home medical devices that can measure various human biosignals. Devices that can assess total cholesterol or triglyceride levels are already available, while a device that will allow measurement of liver enzymes, such as aspartate aminotransferase and alanine transaminase, will be available soon. These devices could play a crucial role in monitoring hyperlipemia, alcoholic hepatitis or viral hepatitis. Furthermore, clinical trials of a system that can wirelessly transfer continuously‐monitored patients' pulse, electrocardiography and/or activity rate to the medical team are currently undergoing clinical trials. Closer monitoring of lifestyle for patients with type 2 diabetes could be possible using the aforementioned devices, and lifestyle could be standardized and categorized for real application in diabetes management.
The aforementioned systems could be even more beneficial in countries that have a rapidly increasing rate of patients with type 2 diabetes, but that do not have well‐developed medical infrastructure. Although such systems can require good IT infrastructure, such as high‐speed Internet networks, the expansion of cellular phone networks in many countries without widely available high‐speed internet networks could still signify benefits from IT‐based diabetes management systems. In addition, the growing popularity of smart phones could be very useful in the application of IT‐based diabetes management systems. Recently, for example, there has been strong interest in the clinical decision supporting system (CDSS) software program that allows feedback to be provided automatically to patients after analysis of clinical data; this is a more effective and economical way to provide care to patients. Although still in the development stage, CDSS is expected to handle even more complex data in the future, as well as having a better logic system that yields optimal answers for patients. We expect this software to open up new horizons in diabetes treatment. Its use should also reduce the burden on medical staff and maximize cost effectiveness for healthcare systems.
Another study by Cho et al. noted that this new software can automatically feed suggestions to patients or provide certain data to physicians after analyzing glucose data that patients have provided over the internet. Thus, there are positive clinical effects, and the medical workload is reduced as well5.
Advances in smart phone technology have made it possible for patients to send data, including glucose levels, personal information, questionnaires, events and image‐based information, to medical staff. These medical staff can now also transmit feedback and various forms of data, including graphs, images and movie clips. This allows for more intimate communication and information exchange between patients and medical staff. It also makes it possible to gather more diverse patient data, and analysis of this data should pave the way for more in‐depth patient care software. For example, when patients transmit bodyweight data and information on the amount of exercise carried out alongside simple glucose level data, medical professionals are able to carefully examine the causes of changes in glucose levels. This means they can make on‐the‐spot diagnoses, thus helping patients manage their glucose levels. Furthermore, when visible diabetic complications, such as diabetic foot ulcers, are noticed by patients, they can send images to physicians at an early stage; this will, in turn, help doctors to treat the complications more effectively. For those patients who live in remote areas and have limited immediate access to hospitals, this form of glucose management will even be more effective.
As aforementioned, many Asian countries are experiencing exponential growth in the number of patients with type 2 diabetes, and this is believed to be the result of increasing obesity. Abdominal obesity and accelerating muscle mass reduction as a result of a lack of exercise are a particular problem. To make matters worse, unlike in Western countries, Asian countries are seeing increasing numbers of patients in their early 30s with type 2 diabetes1. Given this, the use of the IT‐based glucose and lifestyle management system will not only help control glucose levels, but will also bring about fundamental changes in bodyweight management. It will also promote more exercise among patients with type 2 diabetes. Furthermore, with the younger generation being more familiar with IT‐based systems, results could be more effective.
More effective glycemic control for diabetes mellitus patients is now vital. However, advances in in‐home health devices and communication technology are about to usher in a new era in diabetes management. New IT‐based diabetes management systems might curb the exponential growth of diabetes and diabetes‐related complications in many Asian countries.
References
- 1.Yoon KH, Lee JH, Kim JW, et al Epidemic obesity and type 2 diabetes in Asia. Lancet 2006; 368: 1681–1688 [DOI] [PubMed] [Google Scholar]
- 2.Chan JC, Malik V, Jia W, et al Diabetes in Asia: epidemiology, risk factors and pathophysiology. JAMA 2009; 301: 2129–2140 [DOI] [PubMed] [Google Scholar]
- 3.Cho JH, Chang SA, Kwon HS, et al Long‐term effect of the Internet‐based glucose monitoring system on HbA1c reduction and glucose stability: a 30‐month follow‐up study for diabetes management with a ubiquitous medical care system. Diabetes Care 2006; 29: 2625–2631 [DOI] [PubMed] [Google Scholar]
- 4.Cho JH, Lee HC, Lim DJ, et al Mobile communication using a mobile phone with a glucometer for glucose control in Type 2 patients with diabetes: as effective as an Internet‐based glucose monitoring system. J Telemed Telecare 2009; 15: 77–82 [DOI] [PubMed] [Google Scholar]
- 5.Cho JH, Choi YH, Kim HS, et al Effectiveness and safety of a glucose data‐filtering system with automatic response software to reduce the physician workload in managing type 2 diabetes. J Telemed Telecare 2011; 17: 257–262 [DOI] [PubMed] [Google Scholar]


