SUMMARY
Background
Sitting time is associated with adverse health outcomes including chronic disease and premature mortality. However, it is not known if the association of sitting time with cardiometabolic risk factors varies across socio-demographic or health factors.
Methods
The sample included 4560 adults (≥ 20 years) who participated in the cross-sectional 2007–2010 U.S. NHANES. Participants self-reported typical daily sitting time. Weight, height, blood pressure, and fasting triglycerides, HDL-cholesterol (HDL-C), glucose, and insulin were measured. Insulin resistance (HOMA-IR) and beta cell function (HOMA-%B) were calculated. A sub-sample of 3727 participants underwent an oral glucose tolerance test to obtain 2-h post-load glucose levels. Population-weighted linear regression analysis was used to examine the association between sitting time and each cardiometabolic risk factor, stratified by sex, race, socio-economic status, and activity level. Analyses were controlled for demographics, socio-economic status, survey cycle, personal and family medical history, diet, and physical activity.
Results
Sitting time was significantly associated with adverse levels of waist circumference, body mass index, triglycerides, HDL-C, insulin, HOMA-IR, HOMA-%B, and 2-h post-load glucose, but not with blood pressure or glucose level. In stratified analyses, sitting time was most consistently related to cardiometabolic risk factors among low and middle socio-economic groups and for those who reported no weekly physical activity, but there were few differences between sex or race groups.
Conclusions
Self-reported sitting time was associated with adverse cardiometabolic risk factors consistently across sex and race groups in a representative U.S. sample, independent of other risk factors. Excessive sitting warrants public health concern.
Keywords: sitting time, sedentary behavior, cardiovascular disease, cardiometabolic risk factors
Sitting time is associated with deleterious health outcomes including weight gain,(1) cardiovascular disease (CVD)(2) and all-cause and CVD mortality.(3,4) Given the high global prevalence of sitting,(5) these adverse health consequences have serious public health implications. However, it is not known if the association of sitting time with cardiometabolic risk factors varies by sociodemographic factors or activity level.
Evidence is mixed on whether there are sex differences in the association between sitting time and cardiometabolic risk factors. One study found consistent associations between Australian men and women.(6) In contrast, an examination of British adults found a significant interaction between self-reported sitting time and systolic blood pressure, with a significant association in women but not in men, but no other differences by sex for other cardiometabolic risk factors.(7) A hospital-based case-control study of Indian adults found no association between sitting time at work and risk of acute myocardial infarction, but analyses were not stratified by sex.(8) Finally, an analysis of Chilean adults found significant associations between sitting time and cardiometabolic risk factors when controlled for sex, but it is not known if these associations differed by sex.(9)
One study of a nationally representative U.S. sample, derived from the U.S. NHANES 2003–2006, found little meaningful difference across sex or race groups in the association of accelerometer-derived sitting time and cardiometabolic risk factors.(10) However, to our knowledge there has been no examination of the association between self-reported sitting time and cardiometabolic risk in a nationally representative sample of U.S. adults. Furthermore, it is unknown of these associations differ by socio-economic status or physical activity level. The present study investigated the relationship between self-reported sitting time and cardiometabolic risk factors among a nationally representative sample of U.S. adults, stratified by sex, race, socio-economic status, and physical activity level.
METHODS
Design and participants
The sample consisted of participants in the 2007/2008 and 2009/2010 National Health and Nutrition Examination Survey (NHANES), a cross-sectional examination of 20,686 participants selected using a complex, multistage probability design to represent the non-institutionalized civilian U.S. population. Participants completed an in-home questionnaire interview and a randomly selected sub-sample attended a Mobile Examination Center for a physical examination. Full protocols, which were approved by the National Center for Health Statistics Ethics Board, are available at http://www.cdc.gov/nchs/nhanes.htm.
There were 5133 participants aged ≥ 20 years who participated in the morning fasting laboratory examination. For the present analysis, exclusion criteria included failure to report sitting time (n = 14) or missing data on primary analysis variables (n = 533). Those with a zero value for sample weight (n = 26) were also excluded, which occurred due to merging data elements from multiple NHANES waves. The final sample consisted of 4560 participants.
Self-reported sitting time
To assess sitting time, participants reported the amount of time spent sitting or reclining (in 2007–2008) or sitting only (2009–2010) in a typical day. Participants were asked to consider time spent sitting at work and at home, during transportation, sitting with friends, reading, playing cards, watching television or using a computer, but to exclude time spent sleeping. In the 2007–2008 cycle, participants were asked: “How much time do you usually spend sitting or reclining on a typical day?” In the 2009–2010 cycle, participants were asked: “How much time do you usually spend sitting on a typical day?” The International Physical Activity Questionnaire (IPAQ) contains a similar question on sitting time (“During the last 7 days, how much time did you usually spend sitting on a weekday/weekend day?”), with acceptable reliability and validity.(11, 12)
Cardiometabolic risk factors
Weight was measured to the nearest 0.1 kg using a digital scale, with participants clothed in a standard examination gown. Height was measured to the nearest 0.1 cm using a stadiometer. Body mass index (BMI) was calculated as weight divided by height squared (kg/m2). Waist circumference was measured to the nearest 0.1 cm at the superior border of the iliac crest. Systolic and diastolic blood pressures were measured with a mercury sphygmomanometer and are reported as averages of three to four measurements. Fasting measures of triglycerides, HDL-cholesterol (HDL-C), glucose, and insulin were obtained by venipuncture on the arm. The Homeostatic Model Assessment was calculated to determine measurements of insulin resistance (HOMA-IR) and beta cell function (HOMA-%B). A sub-sample of 3727 individuals underwent an oral glucose tolerance test (OGTT) to obtain 2-h post-load glucose levels. Documentation of the laboratory methodologies, including instruments used to assay the blood measures in each NHANES survey cycle, is available at http://www.cdc.gov/nchs/nhanes.htm.
Covariates
Participants self-reported their age and sex at the screening interview. During the in-home questionnaire interview, participants self-reported medication use for the control of cholesterol, hypertension, insulin, or diabetes; diagnosis of diabetes, CVD, or cancer; and family medical history (close relative) of diabetes or myocardial infarction. Self-reported race/ethnicity was categorized as non-Hispanic white, non-Hispanic black, Mexican American, or Other. Education status was categorized as less than 9th grade, 9th to 11th grade, high school diploma, some college or associate’s degree, or college graduate or above. Marital status was categorized as married, widowed, divorced, separated, never married, or living with partner. Socio-economic status was defined using the poverty income ratio, which is family income divided by a poverty threshold specific to family size. Participants reported the minutes per day and days per week of moderate and vigorous physical activity (MVPA) during sports, fitness or recreational activities. A weighted MVPA/week score counted vigorous minutes as twice that of moderate activity, to comply with current physical activity guidelines that recommend 75 min/week of vigorous activity or 150 min/week of moderate activity.(13)
Dietary intake was self-reported using two 24 h dietary recalls. The U.S. Department of Agriculture food composition database was used to determine intakes for total energy, saturated fat as a percentage of total energy intake, sodium, potassium, fiber, caffeine, and calcium.(14) Average daily intake was computed by averaging the two dietary recalls. Alcohol status was categorized based on the U.S. dietary guidelines as non-drinker, light drinker (men < 28 g/d; women < 14 g/d), moderate drinker (men 28 to < 56 g/d; women 14 to <28 g/d), or heavy drinker (men ≥56 g/d; women ≥ 28 g/d).(15) Participants were classified by smoking status based on serum cotinine levels assessed during the physical examination as non-(<10 ng/dL), light (10 to <100 ng/dL), moderate (100 to <300 ng/dL), or heavy (≥300 ng/dL) smoker.
Statistical analysis
Participants were categorized into sitting groups using tertiles, representing low (≤ 3 hours/day), moderate (> 3 to ≤ 6 hr/day), or high (> 6 hr/day) sitting time/day. Analyses were conducted using SAS Version 9.3 (SAS Institute Inc., Cary, NC, USA) and were population-weighted using the average of the two year fasting subsample weights from the 2007–2008 and 2009–2010 cycles.(16) Analysis of 2-h post-load glucose level was performed on the OGTT sub-sample only, and the average of the two year OGTT weights from the 2007–2008 and 2009–2010 cycles was used for the OGTT analyses.
Population-weighted descriptive characteristics were calculated using proc surveyfreq and proc surveymeans, stratified by sitting group. Skewed continuous variables were transformed using the natural logarithm for analysis and then back-transformed to the geometric mean for presentation of the results. Population-weighted linear regression analysis using proc surveyreg was used to examine the association between sitting time and each cardiometabolic risk factor in the overall sample and stratified by sex; race (White, African American, or Mexican American); socio-economic status (tertile); and MVPA level (0 minutes/week, > 0 and < 150 minutes/week, 150 to < 300 minutes/week, and ≥ 300 minutes/week). Covariates were selected based on their previously demonstrated association with sitting time(17) and their inclusion in prior studies on the relationship between sitting time and cardiometabolic risk.(6, 10) Covariates included age, age squared, sex, race/ethnicity, survey cycle (2007–2008 or 2009–2010), socio-economic status, educational attainment, marital status, medication use, medical history, family medical history, MVPA/week, smoking status, energy intake, saturated fat (as a percentage of daily energy intake), sodium intake, and alcohol status. Analyses of blood pressure also included potassium, fiber, caffeine, and calcium intake as covariates. When stratified, models excluded the variable of interest (i.e. sex, race, socio-economic status, or MVPA level). Beta coefficients were back-transformed to the geometric mean and converted to percent difference in the dependent variable per 1 hr/day higher sitting time. Multivariable-adjusted means of cardiometabolic risk factors within each sitting group in the overall sample are reported in figures. Analysis of covariance, adjusted for all covariates, was used to determine the p for trend across sitting time groups for each cardiometabolic risk factor. Statistical significance was accepted at p < 0.05.
RESULTS
Participants were on average 46.6 (interquartile range, IQR: 45.8 to 47.5) years old, with a weighted distribution of 52.2% women and 69.4% white, 10.7% African American, 8.5% Mexican American, and 11.4% other race/ethnicity. The population-weighted average sitting time was 5.7 (IQR: 5.5 to 5.8) hr/day. Population-weighted descriptive characteristics stratified by sitting time are reported in Table 1.
Table 1.
Population-weighted descriptive characteristics of U.S. adults ≥ 20 years (NHANES 2007–2010), stratified by sitting time.
| Sitting Time | |||
|---|---|---|---|
| Low | Moderate | High | |
| N | 1670 | 1554 | 1336 |
| Age, ± SE | 45.3 ± 0.6 | 47.9 ± 0.6 | 46.6 ± 0.7 |
| Male, % ± SE | 48.0 ± 1.4 | 47.5 ± 1.4 | 50.8 ± 1.7 |
| Race/Ethnicity, % ± SE | |||
| White | 60.7 ± 3.5 | 71.7 ± 2.4 | 75.0 ± 2.1 |
| African American | 11.6 ± 1.4 | 10.8 ± 1.2 | 9.8 ± 1.3 |
| Mexican American | 14.1 ± 2.1 | 7.2 ± 1.3 | 4.7 ± 0.8 |
| Other | 13.5 ± 2.0 | 10.2 ± 1.3 | 10.6 ± 1.2 |
| Waist Circumference, cm a | 94.6 (84.5, 105.2) | 97.8 (88.4, 108.0) | 97.5 (86.9, 109.1) |
| Body Mass Index, kg/m2 a | 27.2 (23.5, 31.1) | 28.1 (24.1, 32.3) | 28.1 (24.0, 32.1) |
| Systolic blood pressure, mm Hg a | 118.2 (106.8, 126.7) | 118.9 (109.0, 128.1) | 117.2 (106.6, 125.9) |
| Diastolic blood pressure, mm Hg a | 67.9 (60.9, 75.2) | 67.5 (60.8, 75.5) | 68.6 (61.8, 76.0) |
| Triglycerides, mmol/L a | 1.2 (0.9, 1.7) | 1.3 (0.9, 1.8) | 1.3 (0.9, 1.7) |
| HDL-C, mmol/L a | 1.4 (1.1, 1.7) | 1.3 (1.1, 1.6) | 1.3 (1.1, 1.6) |
| Fasting plasma glucose, mmol/L a | 5.7 (5.0, 5.9) | 5.7 (5.1, 6.0) | 5.6 (5.1, 5.9) |
| Fasting insulin, mmol/L a | 54.1 (33.1, 87.0) | 60.9 (37.8, 97.6) | 62.2 (39.3, 97.8) |
| HOMA-IR a | 2.3 (1.3, 3.8) | 2.6 (1.5, 4.3) | 2.6 (1.6, 4.3) |
| HOMA-%B a | 87.5 (57.8, 135.2) | 96.1 (63.0, 150.0) | 101.2 (68.6, 151.5) |
| 2 h post-load plasma glucose, mmol/L a, b | 5.9 (4.6, 7.2) | 6.1 (4.8, 7.5) | 6.1 (4.8, 7.5) |
Parentheses indicate interquartile range. Low is self-reported sitting time ≤ 3 hours/day, moderate is > 3 and ≤ 6 hours/day, and high is > 6 hours/day.
Back-transformed from the natural logarithm.
Sub-sample analysis, n = 1374 for low sitting time, n = 1251 for moderate sitting time, and n = 1102 for high sitting time.
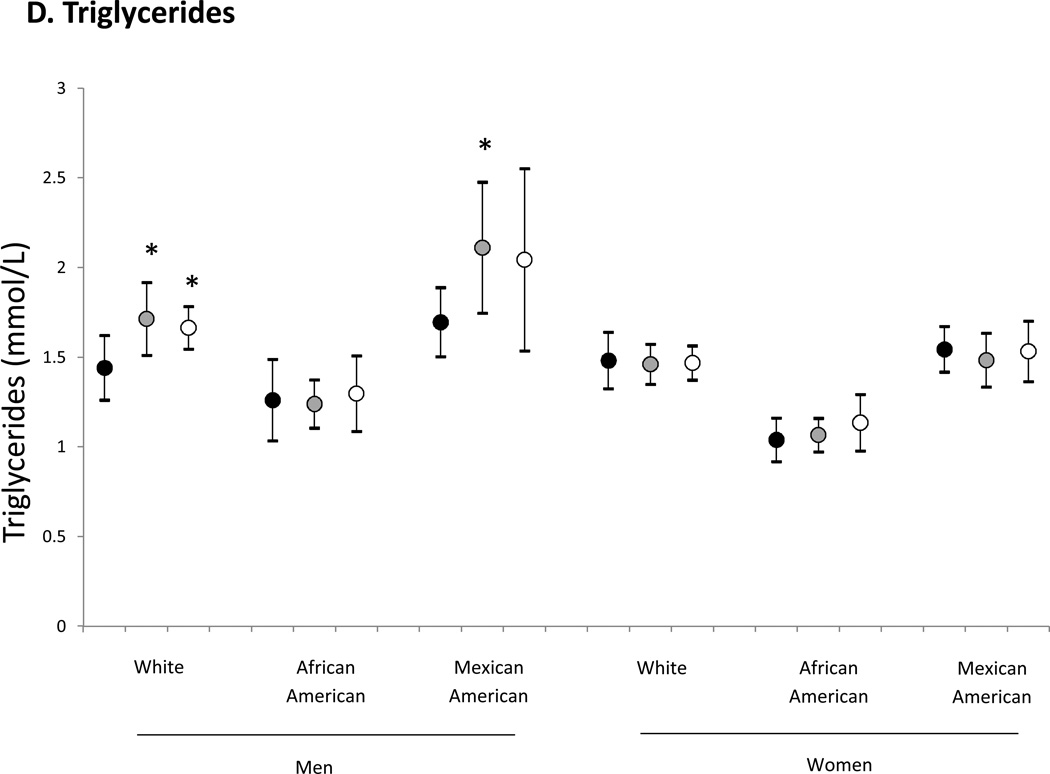
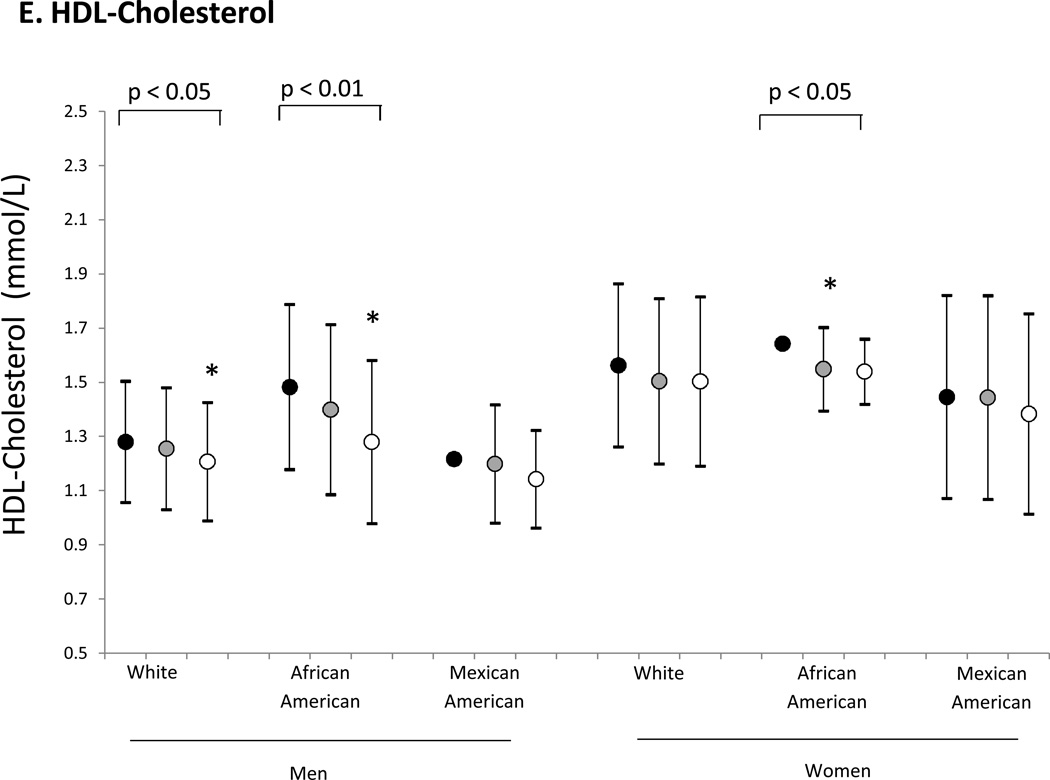
Multivariable linear regression analyses demonstrated a significant relationship between sitting time and levels of waist circumference, BMI, triglycerides, HDL-C, insulin, HOMA-IR, HOMA-%B, and 2-h post-load plasma glucose (Table 2). There was no significant association between sitting time and blood pressure or glucose level. For both men and women, there was a significant relationship between sitting time and waist circumference, HDL-C, insulin, HOMA-IR, and HOMA-%B. Sitting time was significantly related to BMI in women only and to triglycerides and 2-h post-load plasma glucose in men only. For all three race groups, sitting time was related to waist circumference, insulin, HOMA-IR, and HOMA-%B, and for two race groups sitting time was associated with BMI, HDL-C, and 2-h post-load plasma glucose.
Table 2.
Population-weighted percent difference in cardiometabolic risk factor given 1 hr/day higher sitting time in U.S. adults ≥ 20 years (NHANES 2007–2010).
| All | Sex | Race | Socio-Economic Status | MVPA Level (min/week) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | White | AA | MA | Low | Middle | High | 0 | <150 | 150 to 300 |
>300 | ||
| WC | 0.30** | 0.19*** | 0.35* | 0.24* | 0.39* | 0.90*** | 0.61*** | 0.50** | 0.06 | 0.59*** | 0.14 | 0.13 | 0.01 |
| BMI | 0.37* | 0.06 | 0.62** | 0.34* | 0.56 | 1.13*** | 0.64*** | 0.78*** | −0.01 | 0.73** | 0.18 | 0.19 | −0.07 |
| SBP | −0.11 | −0.13 | −0.10 | −0.08 | −0.24 | 0.22 | −0.27* | −0.03 | −0.09 | −0.13 | −0.11 | −0.15 | 0.07 |
| DBP | 0.05 | 0.18 | −0.10 | −0.01 | −0.06 | 0.72** | −0.08 | 0.22 | 0.02 | 0.10 | 0.18 | 0.20 | 0.07 |
| TG | 1.03*** | 1.52*** | 0.50 | 1.06** | 0.80 | 1.23 | 1.20* | 2.00*** | 0.49 | 1.08** | 1.19 | −0.16 | 2.22** |
| HDL-C | −0.82*** | −0.97*** | −0.60* | −0.75** | −1.17*** | −0.67 | −1.17*** | −1.18*** | 0.50 | −0.84*** | −0.38 | −0.86* | −1.13** |
| Glucose | −0.04 | −0.13 | 0.02 | 0.02 | −0.22 | −0.02 | −0.06 | 0.15 | −0.22 | 0.03 | 0.01 | 0.03 | −0.17 |
| Insulin | 2.41*** | 2.18*** | 2.58*** | 2.36*** | 2.18** | 2.56** | 2.37*** | 2.73*** | 1.99*** | 2.77*** | 2.80** | 1.20 | 2.36** |
| HOMA-IR | 2.37*** | 2.01** | 2.58*** | 2.41*** | 1.98* | 2.50** | 2.30*** | 2.89*** | 1.77** | 2.81*** | 2.82* | 1.23 | 2.18* |
| HOMA-%B | 2.40*** | 2.27*** | 2.54*** | 2.31*** | 2.60*** | 2.54*** | 2.63*** | 2.30*** | 2.29*** | 2.65*** | 2.55* | 1.20 | 2.54*** |
| 2-h Glucose a | 0.65** | 0.72* | 0.48 | 0.82** | 0.67* | 0.72 | 0.47 | 1.29*** | 0.23 | 0.72** | 1.34* | 0.12 | 0.46 |
Note.
p < .001,
p < .01,
p < .05.
2-h Glucose = 2-h post-load plasma glucose, BMI = body mass index, DBP = diastolic blood pressure, HDL-C = high density lipoprotein cholesterol, HOMA-IR = homeostatic model of insulin resistance, HOMA-%B = homeostatic model of percentage beta-cell function, MVPA = moderate to vigorous physical activity, SBP = systolic blood pressure, TG = triglycerides, WC = waist circumference. Beta coefficients were back-transformed to the geometric mean and converted to percent difference in the dependent variable per 1 hr/day higher sitting time. Each model includes the covariates age, age squared, sex, race/ethnicity, survey cycle, socio-economic status, educational attainment, marital status, medication use, medical history, family medical history, MVPA min/week, smoking status, energy intake, saturated fat (as a percentage of daily energy intake), sodium intake, and alcohol status. For blood pressure, the model also includes potassium, fiber, caffeine, and calcium. When stratified, models exclude the variable of interest (i.e. sex, race, socio-economic status, or MVPA level).
Sub-sample analysis (n = 3175).
Across socio-economic groups, sitting time was most consistently related to cardiometabolic risk factors in the low and middle tertiles of socio-economic status, though each of the insulin measures (insulin, HOMA-IR, and HOMA-%B) were related to sitting time for every socio-economic class. Across MVPA levels, sitting time was most consistently related to cardiometabolic risk factors in the group that reported 0 minutes/week of MVPA. Waist circumference, HDL-C, insulin, HOMA-IR, and HOMA-%B were most consistently related to sitting time across each of the stratified analyses, compared to the other cardiometabolic risk factors.
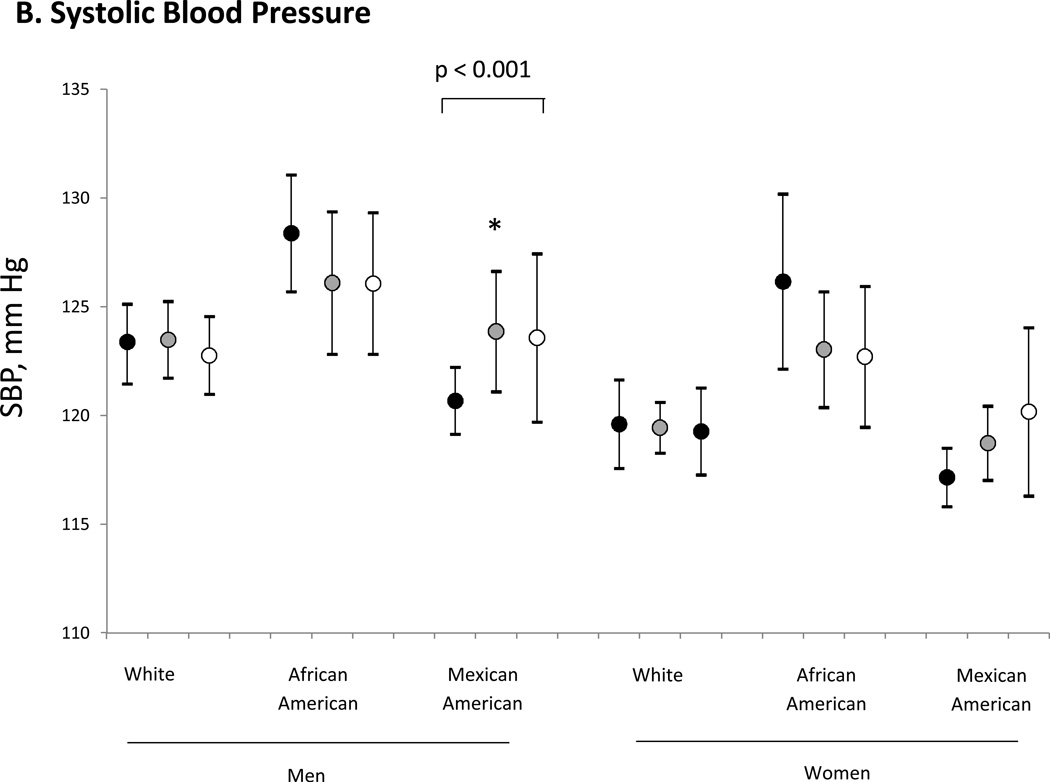
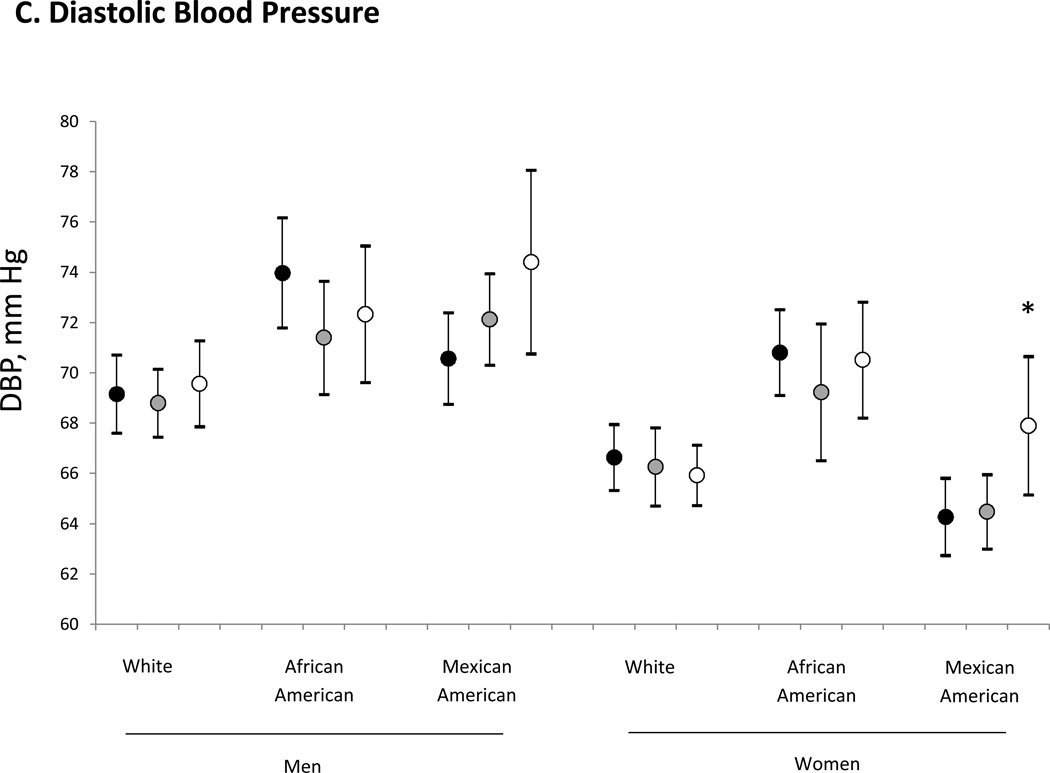
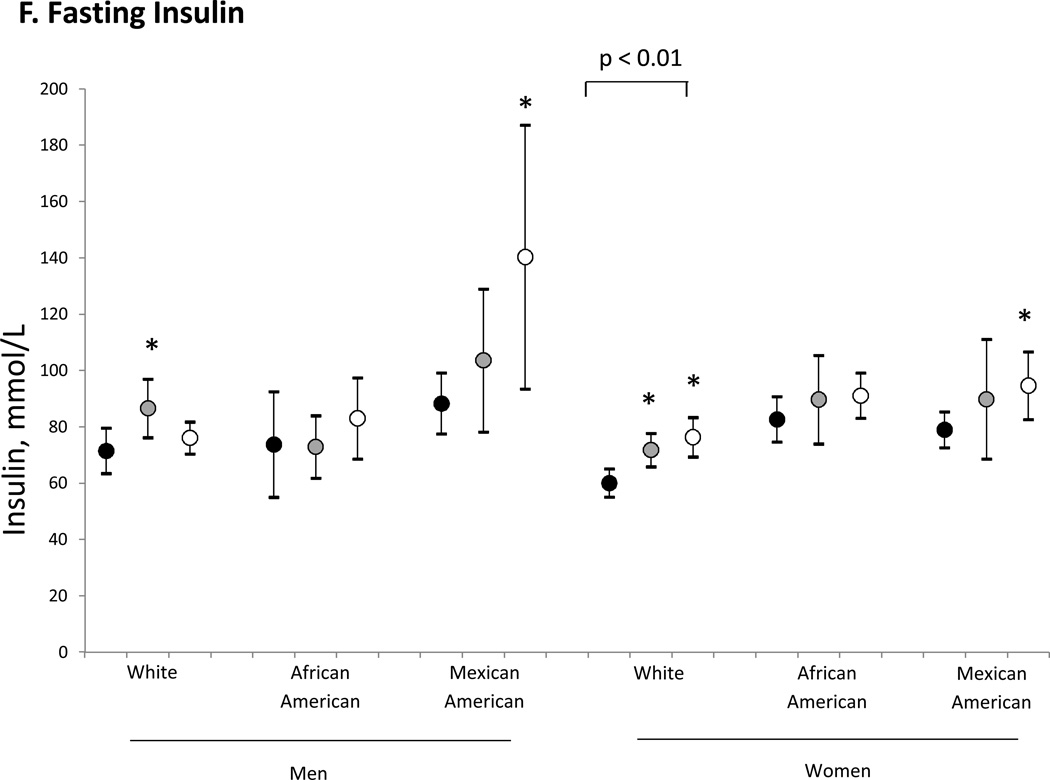
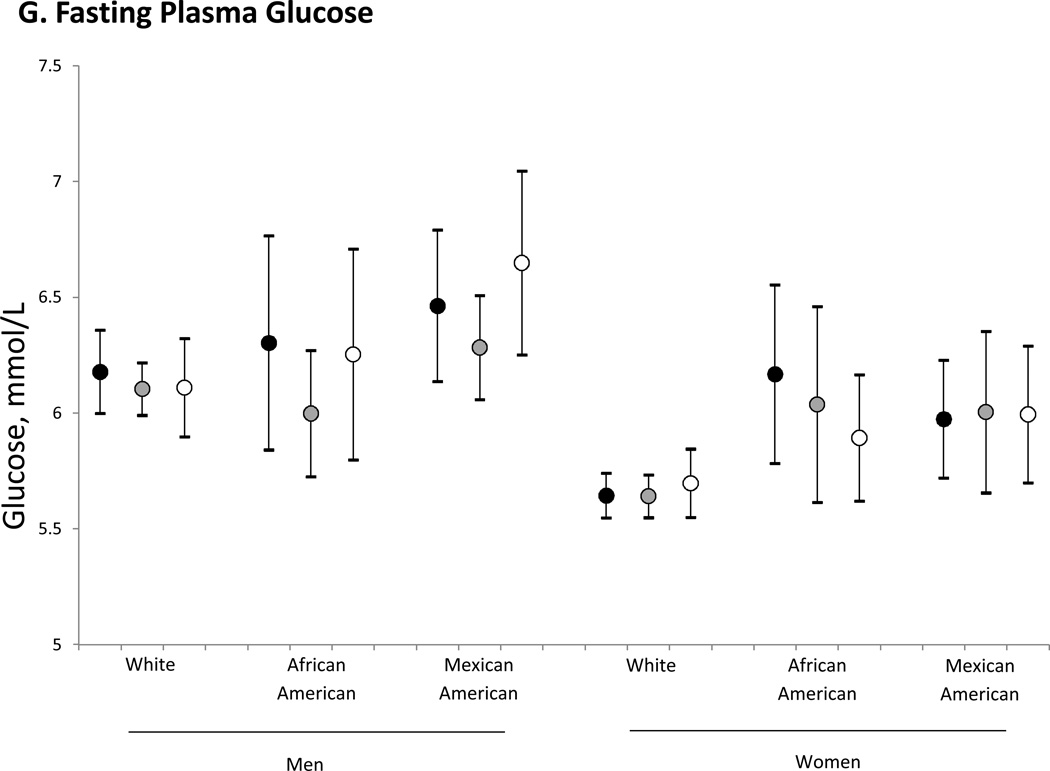
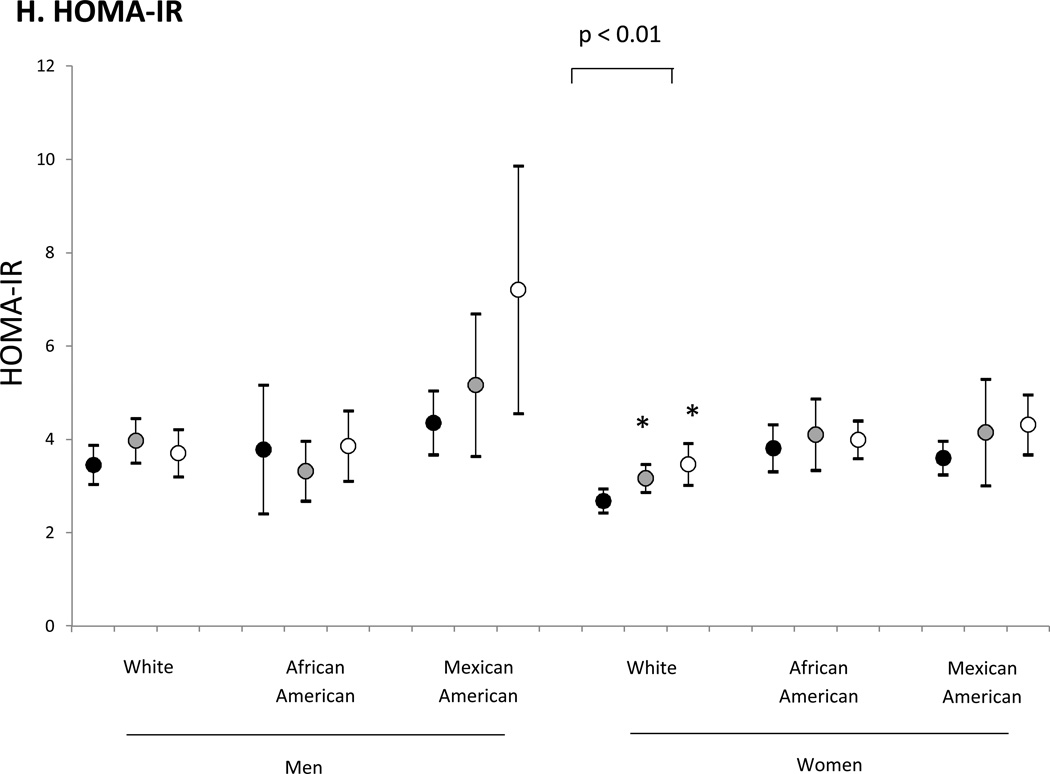
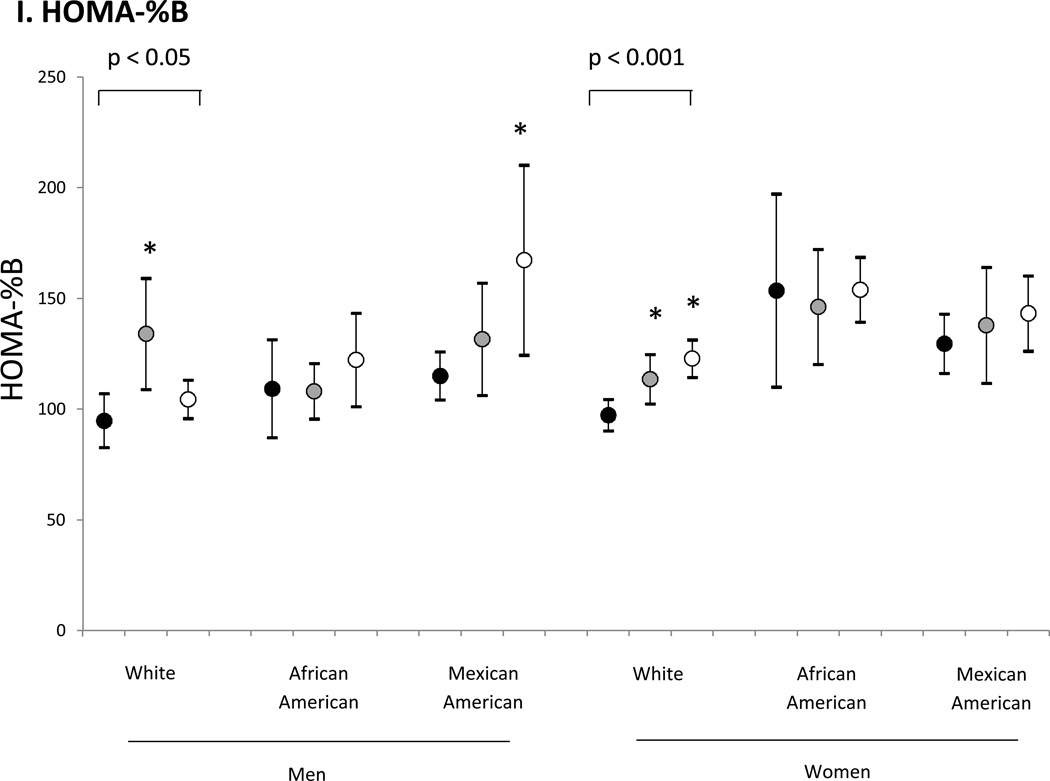
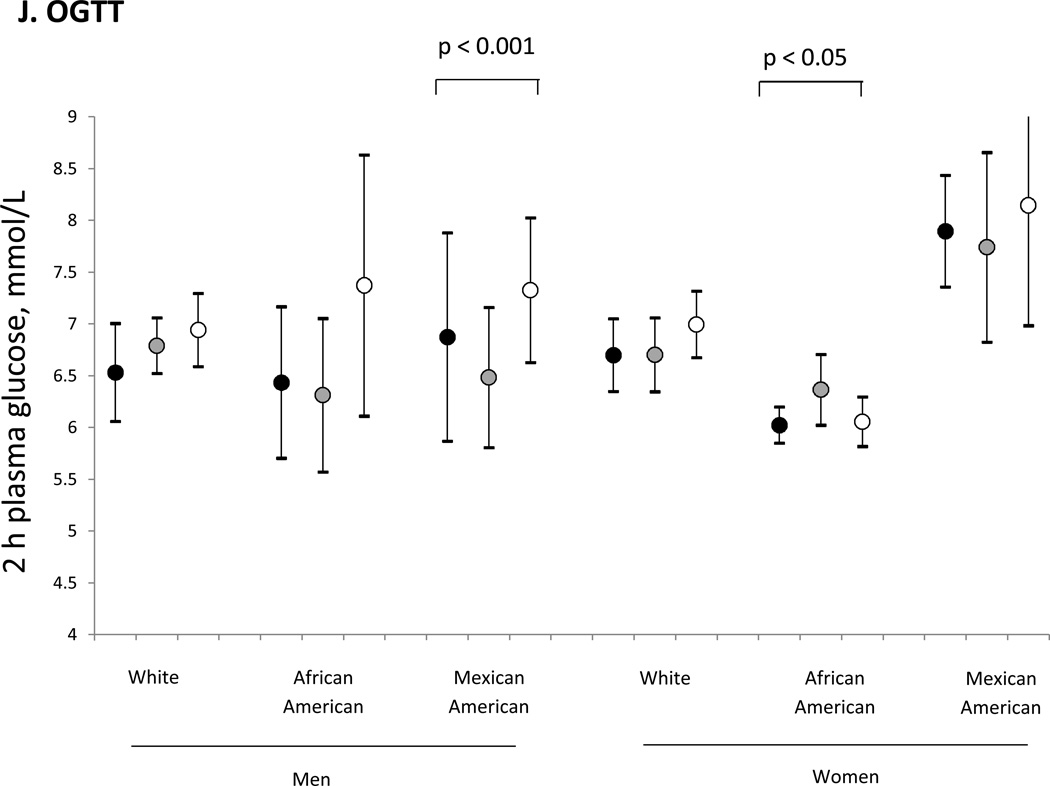
Across sitting time groups, there was a significant p for trend for waist circumference, triglycerides, HDL-C, insulin, HOMA-IR, HOMA-%B, and 2-h post-load plasma glucose (all p < 0.05) but not for blood pressure. Compared to the low sitting time group, the moderate and high sitting time groups had significantly higher waist circumference, triglycerides, insulin, HOMA-IR, and HOMA-%B, and significantly lower HDL-C (all p < 0.05). Additionally, the high sitting time group had significantly higher 2-h post-load plasma glucose, compared to the low sitting time group (p < 0.05). Figure 1a–j displays multivariable-adjusted means of cardiometabolic risk factors within each sitting time group, stratified by sex and race. There was no pattern of consistent sex or race differences in the associations.
Figure 1.
a–j. Association of total sitting time with a) waist circumference, b) systolic blood pressure, c) diastolic blood pressure, d) triglycerides, e) HDL-cholesterol, f) fasting insulin, g) fasting plasma glucose, h) insulin resistance (HOMA-IR), i) beta cell function (HOMA-%B), and j) 2 h post-load glucose, in US adults ≥ 20 years, stratified by sex and race (NHANES 2007–2010).
Note. * Indicates significant difference from < 3 hours/day of sitting time. Error bar indicates 95% confidence interval. Black circles indicate the low sitting group (< 3 hours/day), gray circles indicate the moderate sitting group (> 3 and ≤ 6 hours/day), and white circles indicate the high sitting group (> 6 hours/day). Models controlled for age, survey cycle, MVPA/week, socio-economic status, educational attainment, medication use, medical history, family medical history, age squared, marital status, smoking status, energy intake, saturated fat intake (as percentage energy daily intake), sodium intake, alcohol status. Analysis of blood pressure also controlled for potassium, fiber, caffeine, and calcium intake.
DISCUSSION
Sitting time, as assessed by self-report in NHANES 2007–2010, was significantly related to several cardiometabolic risk factors, including waist circumference, BMI, triglycerides, HDL-C, insulin, HOMA-IR, HOMA-%B, and 2-h post-load glucose. Adults reporting moderate to high amounts of sitting time had significantly worse cardiometabolic risk factors compared to those adults in the lowest category of sitting time. The relationship between time spent sitting and adverse risk factors persisted even in models adjusted for demographics, socio-economic status, medication use, medical history, family medical history, and health behaviors, including diet. These findings suggest that time spent sitting may exert an adverse influence on cardiometabolic health above and beyond the traditional risk factors such as age, sex, race, smoking status, and energy intake. Importantly, even controlling for amount of MVPA did not attenuate the relationship between sitting time and adverse cardiometabolic health, indicating that the adverse association of sitting time with health risk is distinct from MVPA.
A unique contribution of these findings to the literature on sitting time and cardiometabolic risk is the stratification by sex, race, socio-economic status, and MVPA level. Men and women demonstrated similar associations between sitting time and cardiometabolic risk, although triglycerides and 2-h post-load glucose were only associated with sitting time in men. Significant associations were also found for both men and women the Australian Diabetes, Obesity and Lifestyle (AusDiab) study in models that used similar covariates, though triglycerides and 2-h post-load glucose were also associated with sitting among women.(6) Additionally, self-reported sitting was associated with a continuous metabolic syndrome risk score in both men and women in a Flemish cohort.(18) In contrast, other studies have demonstrated stronger associations between sitting and health risk among women compared to men. One study of 505 British adults who self-reported sitting found an association between sitting and fasting insulin among women, but not men.(19) Stronger associations were found for women versus men in a study that used accelerometer-determined sitting time.(20) Future research should clarify whether or not there are sex differences in the association between sitting and health risk, and if so, explore potential physiological or lifestyle mechanisms.
In the race-stratified analyses, Whites, African Americans, and Mexican Americans each had significant associations between sitting time and waist circumference, fasting insulin, HOMA-IR, and HOMA-%B. As indicated in a recent meta-analysis, no known studies have examined ethnic differences between general sitting and health risk.(21) The present findings are the first known comparisons of the association between sitting time and cardiometabolic risk across race groups in the U.S. and demonstrate no appreciable race differences.
In analyses stratified by income, associations between sitting time and cardiometabolic risk were strongest in the low and middle socio-economic groups. In fact, in the high socio-economic group, only the insulin measures (fasting insulin, HOMA-IR, and HOMA-%B) were significantly associated with sitting time. Similar to the present findings, a differing association between sitting time and health risk across neighborhood socio-economic status was demonstrated in a study of 1048 working Australian adults.(21) Leisure-time sitting mediated the relationship between educational attainment and overweight/obesity, indicating that the higher rate of obesity among less educated adults was partly attributable to higher amounts of leisure-time sitting. Higher socio-economic groups may have better access to healthcare and healthy lifestyle options, potentially protecting them from the negative health consequences of sitting.
Across MVPA levels, the strongest associations with sitting time emerged for those reporting no engagement in MVPA. However, groups reporting higher levels of MVPA still showed associations between sitting time and triglycerides, HDL-C, and the insulin measures. Although significant relationships between sitting time and heath variables have been presented herein, even when adjusting for MVPA, it seems as though engagement in a certain level of MVPA may negate or reduce the potentially harmful health consequences of high amounts of sitting. This hypothesis warrants further study.
The present findings support results of a study of Australian adults, in which self-reported sitting time was related to adverse levels of waist circumference, BMI, triglycerides, HDL-C, 2-h plasma glucose, and fasting insulin, but not to fasting plasma glucose.(6) However, there was also a significant relationship with systolic blood pressure in the Australian adults and with diastolic blood pressure in Australian women, which was not found in the present study. An association between self-reported sitting and incident hypertension was also demonstrated in a longitudinal study of Spanish university graduates followed for 40 months, though associations were significant only for sitting while driving and using the computer, not television viewing or sleeping.(22) The cardiometabolic risk associated with sitting time supports a potential pathway for the association between sitting and the development of type 2 diabetes.(23)
Healy et al. (2011) found similar associations between sedentary behavior, measured by accelerometry, and cardiometabolic risk factors, based on a nationally representative sample in NHANES 2003–2006.(10) Like the present findings for sitting time, accelerometer-measured sedentary behavior was significantly associated with insulin resistance (HOMA-IR) and beta cell function (HOMA-%B). The present study found that adults who sat more also had higher glucose levels following an oral glucose tolerance test compared to those who sat less. The important distinction is that the present study used sitting time assessed by self-report, whereas Healy et al. (2011) quantified sedentary behavior with the Actigraph accelerometer, with sedentary time defined as < 100 counts per minute. Although self-report is subject to participant bias, the use of accelerometry can also be biased due to incomplete data and measurement error.(24) Given the association with cardiometabolic risk, self-reported sitting time could be useful in a clinical setting and in epidemiological field studies, whereas accelerometry can incur extra cost, time, and participant and clinician/researcher burden. In population-based research, incorporating both self-report and device-based measurement of sedentary behavior may be ideal.(25)
Determining the number of hours per day of sitting that is associated with adverse cardiometabolic health is important for potential clinical and public health recommendations. The present study found significant cardiometabolic health differences with self-reported sitting more than 3 hr/day compared to sitting less than 3 hr/day. These cutoff values are similar to findings of increased mortality in adults self-reporting ≥ 6 hr/day of sitting versus < 3 hr/day in both women and men, regardless of MVPA level.(26) Yet these sitting time levels are lower than other studies that have studied clinical outcomes. For instance, in a study of middle-aged and elderly women, risk of cardiovascular events was only higher for women reporting ≥ 12 hr/day of sitting (including laying down) compared to those reporting < 4 hr/day sitting, with no difference among other durations of sitting.(27) Risk of cardiovascular disease was significantly higher among postmenopausal women reporting ≥ 16 hr/day sitting versus those who spent < 4 hr/day sitting, but no differences were shown among other durations of sitting.(2) Future research should investigate whether certain self-report and objectively measured sitting time amounts are particularly associated with adverse health risk and health outcomes, in order to determine what is considered excessive sitting.
The potential mechanisms explaining the association between sitting time and cardiometabolic risk are unclear. Sitting may deprive the body of muscular contraction needed to interrupt unhealthy molecular signals that are associated with metabolic disease.(28) Studies of rodents have demonstrated that forced sedentary behavior decreased skeletal muscle activity that, in turn, compromised HDL-C production.(29) This theory is supported by the present finding in which sitting was associated with reduced levels of HDL-C in the overall sample and across most stratified groups. Sitting time may displace light-intensity activity, as demonstrated by the highly inverse association between sitting time and light-intensity activity in Australian adults, compared to a weak association between MVPA and sitting time or light-intensity activity.(30) Importantly, light-intensity activity is independently associated with reduced cardiometabolic risk for elevated glucose, type 2 diabetes, and elevated blood lipids.(28) An additional potential mechanism is increased energy intake during sitting time,(31, 32) though additional studies are needed.
A major strength of this study was the use of a nationally representative sample of U.S. adults, which allowed for stratification by sociodemographic and health factors. Several potential confounding variables were controlled in the analysis between sitting time and cardiometabolic risk factors, though additional confounders may be present. Sitting time was assessed as self-reported sitting in a typical day. This question is similar but not identical to that used in the AusDiab study, which asked for typical weekday and weekend day sitting time which was then extrapolated to total weekly minutes.(6) The use of a self-report sitting time question is distinct from an analysis of NHANES 2003–2006 which used sedentary time derived from accelerometry.(10) However, the present and prior findings (6, 10) each indicate associations between sitting time and deleterious risk factors, in spite of differing methods to operationalize sitting. This was a cross-sectional examination, so causal inferences between sitting time and cardiometabolic risk cannot be made. Given the insufficient longitudinal evidence,(23) future research should investigate whether there is a longitudinal relationship between sitting and the development of cardiometabolic risk to determine if sitting is a causal factor of adverse health consequences.
In conclusion, self-reported sitting time was associated with adverse cardiometabolic risk factors consistently across sex and race groups and more so in low and middle socio-economic status groups and for those who reported no physical activity. These associations were independent of other traditional risk factors including demographics, diet, physical activity, and personal and family medical history. Excessive sitting warrants public health concern.
What are the new findings.
Self-reported sitting was associated with elevated waist circumference, body mass index, triglycerides, insulin resistance, and 2-h post-load plasma glucose, and with lower HDL-C, in a nationally representative U.S. sample
The association between sitting time and health risk factors persisted across sex and race groups and when controlling for other traditional risk factors including demographics, diet, physical activity, and personal and family medical history
Associations between sitting time and cardiometabolic risk factors were particularly strong among adults in low and middle socio-economic groups and for adults who reported no engagement in moderate to vigorous physical activity
How might it impact on clinical practice in the near future
Self-reported sitting time may indicate patients at elevated cardiometabolic health risk
Physicians may query patients’ sitting time as part of health behavior risk assessment
Sedentary behavior counseling may be incorporated into primary care settings to encourage the reduction in daily time spent sitting
Public health recommendations may incorporate the need to reduce sitting time, as a distinct public health message from the need for moderate to vigorous physical activity
Acknowledgments
Funding: A.E.S. is funded by an NIH NIDDK National Research Service Award, T32DK064584-06. P.T.K. is supported, in part, by the Louisiana Public Facilities Authority Endowed Chair in Nutrition.
Footnotes
Contributorship Statement: Staiano, Harrington, Barreira, and Katzmarzyk contributed to the analysis and interpretation of the data; Staiano drafted the article and Harrington, Barreira, and Katzmarzyk revised it critically for important intellectual content; and all four authors gave final approval of the version to be published.
Competing interest: The authors have no conflicts of interest to declare.
REFERENCES
- 1.Brown WJ, Williams L, Ford JH, et al. Identifying the energy gap: magnitude and determinants of 5-year weight gain in midage women. Obes Res. 2005;13:1431–1441. doi: 10.1038/oby.2005.173. [DOI] [PubMed] [Google Scholar]
- 2.Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716–725. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 3.Katzmarzyk PT, Church TS, Craig CL, et al. Sitting Time and Mortality from All Causes, Cardiovascular Disease, and Cancer. Medicine & Science in Sports & Exercise. 2009;41(5):998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- 4.Matthews CE, George SM, Moore SC, et al. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012;95:437–445. doi: 10.3945/ajcn.111.019620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bauman A, Ainsworth BE, Sallis JF, et al. The descriptive epidemiology of sitting. A 20-country comparison using the International Physical Activity Questionnaire (IPAQ) Am J Prev Med. 2011;41:228–235. doi: 10.1016/j.amepre.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Thorp AA, Healy GN, Owen N, et al. Deleterious associations of sitting time and television viewing time with cardiometabolic risk biomarkers: Australian Diabetes, Obesity and Lifestyle (AusDiab) study 2004–2005. Diabetes Care. 2010;33:327–334. doi: 10.2337/dc09-0493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stamatakis E, Hamer M, Tilling K, et al. Sedentary time in relation to cardio-metabolic risk factors: differential associations for self-report vs accelerometry in working age adults. International Journal of Epidemiology. 2012;41:1328–1337. doi: 10.1093/ije/dys077. [DOI] [PubMed] [Google Scholar]
- 8.Rastogi T, Vaz M, Spiegelman D, et al. Physical activity and risk of coronary heart disease in India. Int J Epidemiol. 2004;33:759–767. doi: 10.1093/ije/dyh042. [DOI] [PubMed] [Google Scholar]
- 9.Celis-Morales CA, Perez-Bravo F, Ibanez L, et al. Objective vs. self-reported physical activity and sedentary time: effects of measurement method on relationships with risk biomarkers. PLoS One. 2012;7:e36345. doi: 10.1371/journal.pone.0036345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Healy GN, Matthews CE, Dunstan DW, et al. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32:590–597. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 12.Rosenberg DE, Bull FC, Marshall AL, et al. Assessment of sedentary behavior with the International Physical Activity Questionnaire. J Phys Act Health. 2008;5(Suppl 1):S30–S44. doi: 10.1123/jpah.5.s1.s30. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Department of Health and Human Services. Washington, DC: US Government Printing Office; 2008. 2008 Physical Activity Guidelines for Americans. [Google Scholar]
- 14.U.S. Department of Agriculture Agricultural Research Services. USDA National Nutrient Database for Standard Reference, Release 24. 2011. [Accessed June 15, 2012]; at http://ndb.nal.usda.gov/.
- 15.U.S. Department of Agriculture. Dietary Guidelines for Americans, 2010. [Accessed June 15, 2012]; at http://health.gov/dietaryguidelines/.
- 16.National Center for Health Statistics. Specifying weighting parameters. [Accessed January 18, 2013];2011 at http://www.cdc.gov/nchs/tutorials/nhanes/surveydesign/Weighting/intro_i.htm.
- 17.Rhodes RE, Mark RS, Temmel CP. Adult sedentary behavior: a systematic review. Am J Prev Med. 2012;42:e3–e28. doi: 10.1016/j.amepre.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 18.Wijndaele K, Duvigneaud N, Matton L, et al. Sedentary behaviour, physical activity and a continuous metabolic syndrome risk score in adults. Eur J Clin Nutr. 2009;63:421–429. doi: 10.1038/sj.ejcn.1602944. [DOI] [PubMed] [Google Scholar]
- 19.Yates T, Khunti K, Wilmot EG, et al. Self-reported sitting time and markers of inflammation, insulin resistance, and adiposity. Am J Prev Med. 2012;42:1–7. doi: 10.1016/j.amepre.2011.09.022. [DOI] [PubMed] [Google Scholar]
- 20.Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31:661–666. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- 21.Proper KI, Cerin E, Brown WJ, et al. Sitting time and socio-economic differences in overweight and obesity. Int J Obes (Lond) 2007;31:169–176. doi: 10.1038/sj.ijo.0803357. [DOI] [PubMed] [Google Scholar]
- 22.Beunza JJ, Martinez-Gonzalez MA, Ebrahim S, et al. Sedentary behaviors and the risk of incident hypertension: the SUN Cohort. Am J Hypertens. 2007;20:1156–1162. doi: 10.1016/j.amjhyper.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Thorp AA, Owen N, Neuhaus M, et al. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am J Prev Med. 2011;41:207–215. doi: 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 24.Westerterp KR. Assessment of physical activity: a critical appraisal. Eur J Appl Physiol. 2009 Apr;105(6):823–828. doi: 10.1007/s00421-009-1000-2. [DOI] [PubMed] [Google Scholar]
- 25.Healy GN, Clark BK, Winkler EA, et al. Measurement of adults' sedentary time in population-based studies. Am J Prev Med. 2011;41:216–227. doi: 10.1016/j.amepre.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patel AV, Bernstein L, Deka A, et al. Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. American Journal of Epidemiology. 2010;172:419–429. doi: 10.1093/aje/kwq155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ekelund U, Griffin SJ, Wareham NJ. Physical activity and metabolic risk in individuals with a family history of type 2 diabetes. Diabetes Care. 2007;30:337–342. doi: 10.2337/dc06-1883. [DOI] [PubMed] [Google Scholar]
- 28.Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56:2655–2667. doi: 10.2337/db07-0882. [DOI] [PubMed] [Google Scholar]
- 29.Hamilton MT, Healy GN, Dunstan DW, et al. Too little exercise and too much sitting: Inactivity physiology and the need for new recommendations on sedentary behavior. Current Cardiovascular Risk Reports. 2008;2:292–298. doi: 10.1007/s12170-008-0054-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31:369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 31.Bowman SA. Television-viewing characteristics of adults: correlations to eating practices and overweight and health status. Prev Chronic Dis. 2006;3:A38. [PMC free article] [PubMed] [Google Scholar]
- 32.Gore SA, Foster JA, DiLillo VG, et al. Television viewing and snacking. Eat Behav. 2003;4:399–405. doi: 10.1016/S1471-0153(03)00053-9. [DOI] [PubMed] [Google Scholar]