Abstract
INTRODUCTION
Peripheral neuropathy is the most common neurological complication of HIV but is widely under-diagnosed in resource-limited settings. We investigated the utility of screening tools administered by non-physician health care workers (HCW) and quantitative sensory testing (QST) administered by trained individuals for identification of moderate/severe neuropathy.
METHODS
We enrolled 240 HIV-infected outpatients using two-stage cluster randomized sampling. HCWs administered the several screening tools. Trained study staff performed QST. Tools were validated against a clinical diagnosis of neuropathy.
RESULTS
Participants were 65% women, mean age 36.4 years, median CD4 324 cells/μL. 65% were taking antiretrovirals, and 18% had moderate/severe neuropathy. The screening tests were 76% sensitive in diagnosing moderate/severe neuropathy with negative predictive values of 84–92%. QST was less sensitive but more specific.
DISCUSSION
Screening tests administered by HCW have excellent negative predictive values and are promising tools for scale-up in resource-limited settings. QST shows promise for research use.
Keywords: sensitivity and specificity, HIV, peripheral nervous system diseases, developing countries, screening tools
INTRODUCTION
Peripheral neuropathy is the most common neurologic complication of HIV infection with an estimated 35% prevalence in AIDS patients from high-income countries.1–3 Very few studies of the prevalence of HIV-associated peripheral neuropathy in HIV outpatient care settings using standardized assessments have been performed in resource-limited regions, though these report prevalence rates of 49–76%.4,5 Basic neuropathy treatments are available in resource-limited settings, including symptomatic treatment with amitriptyline, discontinuing neurotoxic medications, and vitamin B6 and B12 supplementation. Thus, accurate and timely diagnosis is critical to prevent serious morbidity.6 However, in high-income countries, diagnosis typically requires evaluation by a specialist and sophisticated technology, such as nerve conduction studies.7 In resource-limited settings without access to specialized equipment and few neurologists, diagnosis is challenging, and, thus, peripheral neuropathy remains widely under-recognized and under-treated.
Task-shifting, or the delegation of healthcare tasks to less specialized healthcare workers, is advocated by the World Health Organization (WHO) and is common in many resource-limited locations to enable scale-up of antiretroviral programs.8 A simple, low-cost, and low-technology diagnostic tool for HIV-associated peripheral neuropathy that can be administered by non-physician healthcare workers (HCW) may improve diagnosis and treatment of this condition.
Several screening tools to identify individuals with HIV-associated peripheral neuropathy have been developed, including the Brief Peripheral Neuropathy Screen, the Subjective Peripheral Neuropathy Screen (Subjective-PNS), and the Single Question Neuropathy Screen.7,9–11 Simple quantitative sensory testing (QST) methods which require minimal training for administration, including the monofilament, Rydel-Seiffer graduated tuning fork, and two-point discriminator, have also been used in the evaluation of peripheral neuropathies caused by etiologies other than HIV.12–15 These tools have demonstrated high diagnostic utility when administered by specialized physicians in high-income countries.
Our objectives were to investigate the diagnostic accuracy of: (1) neuropathy screening tools administered by HCW and (2) QST administered by trained individuals for identification of moderate/severe neuropathy in a resource-limited setting. We also sought to estimate the prevalence and describe the risk factors for peripheral neuropathy in an HIV outpatient care setting in sub-Saharan Africa.
MATERIALS AND METHODS
The Kenya Medical Research Institute National Ethical Review Committee and University of California San Francisco Committee on Human Research approved this study. Written informed consent was obtained from all participants.
SUBJECT SELECTION
Between February and July 2010, we enrolled 240 HIV infected adults over age 18 who were obtaining care at 16 outpatient clinics supported by Family AIDS Care and Education Services (FACES) in Nyanza Province, Kenya. Exclusion criteria included: active neurological infection, tumor, or other evolving process; physical deficit or severe medical illness that would impair ability to participate in the evaluation; active intoxication with alcohol or other substances; and inability to speak English, Kiswahili, or Dholuo (the predominant local languages) well enough to complete study procedures.
Participants were selected using two-stage cluster sampling. Population-proportionate sampling of clinics with replacement was used at the first stage to identify 30 clusters (16 clinics represented). At the second stage, random number tables were used to select 8 participants per cluster based on their order of arrival at the facility. Theoretically, this method approximates a random sample of clinic visits without requiring weights.16
DIAGNOSTIC TOOL
We developed a novel diagnostic tool—the Neuropathy Severity Score (NSS)—which was created by combining the Subjective Peripheral Neuropathy Screen with a functional status assessment derived from the physical function scale from the Medical Outcomes Study Core Survey Instrument.10,17 This was done to create a diagnostic tool which corresponded to definitions of neuropathy in the Kenya National Guidelines and because we hypothesized that assessing functional impairment would allow better differentiation between mild neuropathy and moderate/severe disease.18 In addition, several items were added so that scores from the following existing screening tools could be calculated: the Brief Peripheral Neuropathy Screen, Subjective Peripheral Neuropathy Screen, and Single Question Neuropathy Screen (Appendix 1, supplemental material, Figure 1).7,9,10,17 The Single Question Neuropathy Screen is “Tingling, burning or numbness in feet or hands?”9
STUDY PROCEDURES
HCW providing routine clinical care to study participants at each study site administered the diagnostic tool. Before administering the tool, each HCW received an approximately 15 minute one-to-one or small group training on tool administration (including ankle reflexes) from a study staff member. In nearly all cases, administration of the diagnostic tool occurred before any other study procedures. Both study staff and HCW were blinded to each other’s assessments.
QST was typically performed after the neurological examination and by the study staff who administered the gold standard examination. QST included monofilament, graduated tuning fork, and two-point discrimination testing. Protocols and normative data were adapted from prior research (Appendix 2, supplemental material). The order of test administration was determined using a random number table. The examiner then rated each test subjectively as reliable, questionable, or invalid at the conclusion of QST.
The diagnostic tool and QST were compared to a “gold standard” standardized clinical assessment including a complete history and neurological exam which was performed by study staff including: a neurologist (ACM) who evaluated n=103, a 3rd year neurology resident who evaluated n=13, an internal medicine physician (JK) who evaluated n=29, or a 4th year medical student (DC) who evaluated n=95. The neurologist conducted a half day training on the neurological examination for JK and DC, observed each individual conducting neurological examinations, and together they reviewed 30 individuals who participated in a pilot study conducted by the same group.19 The senior neurology resident was observed by the neurologist conducting neurological examinations but did not undergo additional clinical training. She did however receive several hours of training on study procedures and standardized approaches to grading neuropathy. Due to financial constraints and the remote nature of many of our study sites, we were not able to have more than 1 study staff conduct a neurological examination, and thus we were unable to measure inter-observer variability between the individuals conducting the gold standard examination. As a proxy, we compared the prevalence of moderate-severe neuropathy as diagnosed by each of these individuals.
The diagnosis and grading of neuropathy was based on this assessment. Peripheral neuropathy was defined as the presence of at least 1 sign of neuropathy, either reduced sensation to pinprick, reduced vibratory sensation, or reduced or absent ankle reflexes, according to the AIDS Clinical Trials Group (ACTG) criteria.4,20
We performed a sensitivity analysis using a second definition for neuropathy based on case definitions proposed by the American Academy of Neurology, American Association of Electrodiagnostic Medicine, and the American Academy of Physical Medicine and Rehabilitation (AAN/AAEM/AAPMR).21 These criteria suggest that diagnosis of distal symmetric polyneuropathy for field or epidemiologic studies conducted without nerve conduction studies should include the following criteria: (1) neuropathic symptoms; (2) decreased or absent ankle reflexes; (3) decreased distal sensation; and (4) presence or absence of distal muscle weakness or atrophy. In our assessment we asked about the following neuropathic symptoms: paresthesias, numbness, pain, or allodynia. We called ankle reflexes decreased or absent if both ankle reflexes were graded as 1 or 0. We tested the following sensory modalities: light touch, pinprick, temperature, vibration, and proprioception. If abnormalities were observed in at least 1 modality, we graded sensation as reduced.
Neuropathy was further classified as mild, moderate, or severe as follows: (1) mild neuropathy: pinprick diminished in the toes or vibration perception 5–10 seconds at the hallux; (2) moderate neuropathy: pinprick reduced to the ankles or vibration <5 seconds at the hallux; (3) severe neuropathy: pinprick diminished above the ankles or vibration perception absent at the hallux. Each participant also underwent a sociodemographic survey and chart audit.
STATISTICAL ANALYSIS
The sample was dichotomized into those with no or mild peripheral neuropathy versus moderate or severe neuropathy. T-tests and Fisher exact tests were used to compare key clinical and demographic characteristics known to affect the development of peripheral neuropathy between the 2 groups. Variables included: age; height; immune status (current and nadir CD4, WHO stage); nutritional status (body mass index, food insecurity, mean corpuscular volume as a proxy for vitamin B12 deficiency); exposure to neurotoxic medications (stavudine and isoniazid); and other clinical co-morbidities which can lead to neuropathy (alcohol use, liver or renal failure, syphilis infection).
Diagnostic utilities of each test were determined using the clinician’s assessment of neuropathy as the reference test. QST results rated as ‘invalid’ were excluded from the analysis. Sensitivity, specificity, predictive values, likelihood ratios, and accuracy were calculated for each test. A kappa statistic was calculated to compare agreement between ankle reflexes assessed by HCW administering the diagnostic tool and study staff conducting the gold standard clinical assessment. Pearson correlation coefficients were calculated to assess the relationship between each component of the diagnostic tool and the diagnosis of moderate/severe neuropathy. Statistical analyses were performed using Stata 10.0 (StataCorp, College Station, Texas).
RESULTS
Study participants were young and predominantly female. Almost half the participants were WHO disease stage 3 or 4, two-thirds had ever taken antiretroviral therapy, and median CD4+ T-cell count was 324 cells/μL (Table 1). Based on the gold standard assessment, using ACTG criteria 71% (171/240) of participants had peripheral neuropathy, with 54% (129) mild, 13% (31) moderate, and 5% (11) severe neuropathy. Using AAN/AAEM/AAPMR criteria, 29% (70/240) of participants had peripheral neuropathy, with 12% mild (29), 13% (30) moderate, and 5% (11) severe neuropathy. In general, the AAN/AAEM/AAPMR criteria were more stringent. As compared to AAN/AAEM/AAPMR criteria, the ACTG criteria identified 1 additional individual with severe neuropathy, 6 additional individuals with moderate neuropathy, and 110 additional individuals with mild neuropathy.
TABLE 1.
Summary of clinical characteristics and neuropathy risk factors of the study population and comparison by neuropathy as diagnosed using ACTG criteria.
| Overall (n = 240) | None/Mild (n = 198) | Moderate/Severe (n = 42) | p | |
|---|---|---|---|---|
| Age (years) [mean (SD)] | 36.4 (10.5) | 35.2 (10.2) | 42 (10.2) | < 0.001 |
| Female [% (n)] | 65% (157) | 68% (135) | 52% (22) | 0.05 |
| Height (cm) [mean (SD)] | 165 (17) | 164 (19) | 168 (8) | 0.15 |
|
| ||||
| IMMUNE STATUS | ||||
|
| ||||
| Most Recent CD4 [mean (SD)] | 363 (243) | 362 (254) | 368 (189) | 0.46 |
| Nadir CD4 [mean (SD)] | 252 (212) | 261 (224) | 209 (133) | 0.35 |
| WHO Stage 3/4 [% (n)] | 46% (110) | 42% (83) | 66% (27) | 0.006 |
| Months since HIV diagnosis [mean (SD)] | 21 (18) | 19 (17) | 30 (19) | <0.001 |
|
| ||||
| NUTRITIONAL STATUS | ||||
|
| ||||
| Body Mass Index (BMI) [mean (SD)] | 21.1 (3.1) | 21.1 (3.2) | 21.5 (2.5) | 0.34 |
| Food Insecurity* [% (n)] | 8% (18) | 6% (12) | 14% (6) | 0.07 |
| MCV† ever > 100 fL [% (n)] | 17% (40) | 15% (29) | 26% (11) | 0.07 |
|
| ||||
| EXPOSURE TO NEUROTOXIC MEDICATIONS | ||||
|
| ||||
| History of Isoniazid Use [% (n)] | 16% (38) | 17% (33) | 12% (5) | 0.48 |
| Current stavudine use [% (n)] | 39% (94) | 36% (72) | 52% (22) | 0.05 |
| Ever on stavudine [% (n)] | 48% (116) | 41% (82) | 81% (34) | <0.001 |
| Stavudine stopped due to neuropathy [% (n)] | 7% (16) | 4% (7) | 21% (9) | 0.02 |
Food insecurity defined as eating an average of 1 meal per day or having gone ≥ 1 day without eating in the past one week.
MCV – Mean Corpuscular Volume.
When compared to those with no/mild neuropathy, participants with moderate/severe neuropathy by ACTG criteria were significantly older, had been diagnosed with HIV for a longer period of time, were more likely to be WHO stage 3 or 4, and were more likely to have ever used or to have discontinued stavudine due to peripheral neuropathy (Table 1). Alcohol use, elevated alanine aminotransferase and elevated creatinine were not significantly different between the 2 groups (data not shown). Sensitivity analysis using AAN/AAEM/AAPMR criteria demonstrated similar relationships (Appendix 3, supplemental material).
The NSS-Total score, Subjective Peripheral Neuropathy Screen-Total and Maximum scores, and Single Question Neuropathy Screen all had good sensitivity, and fair specificity in diagnosing moderate/severe peripheral neuropathy with excellent negative predictive values (Table 2). The Brief Peripheral Neuropathy Screen had the lowest sensitivity, but agreement between ankle reflexes assessed by the HCW and those assessed by study staff was poor (K=0.09). Typically, HCW rated ankle reflexes as normal when study staff rated them as reduced or absent.
TABLE 2.
Diagnostic utility of neuropathy screening tools and quantitative sensory tests for diagnosing mild/moderate neuropathy and for diagnosing severe neuropathy (vs. no/mild/moderate neuropathy) as diagnosed using ACTG criteria.
| Test | n | Sens | Spec | PPV | NPV | Acc | LR+ | LR− | AUC | Cutoff |
|---|---|---|---|---|---|---|---|---|---|---|
| Moderate/Severe Neuropathy vs. No/Mild Neuropathy | ||||||||||
|
| ||||||||||
| NSS – Total | 240 | 76% | 57% | 27% | 92% | 60% | 1.77 | 0.42 | 0.696 | ≥ 2 |
| NSS – Maximum | 240 | 62% | 69% | 30% | 89% | 68% | 1.98 | 0.55 | 0.688 | ≥ 2 |
| Subjective Peripheral Neuropathy Screen – Total | 240 | 76% | 61% | 29% | 92% | 63% | 1.93 | 0.39 | 0.716 | ≥ 2 |
| Subjective Peripheral Neuropathy Screen – Maximum | 240 | 76% | 56% | 27% | 92% | 59% | 1.71 | 0.43 | 0.698 | ≥ 1 |
| Single Question Neuropathy Screen | 240 | 76% | 56% | 27% | 92% | 59% | 1.71 | 0.43 | 0.659 | ---- |
| Brief Peripheral Neuropathy Screen | 240 | 17% | 94% | 37% | 84% | 80% | 2.75 | 0.89 | 0.553 | ---- |
| Monofilament | 236 | 68% | 93% | 68% | 93% | 89% | 10.18 | 0.35 | 0.813 | ≥ 2 |
| Graduated Tuning Fork | 238 | 56% | 81% | 38% | 90% | 76% | 2.91 | 0.54 | 0.684 | --- |
| Two-Point Discrimination | 207 | 75% | 53% | 23% | 94% | 57% | 1.6 | 0.47 | 0.714 | ≥ 4 |
|
| ||||||||||
| Severe Neuropathy vs. No/Mild/Moderate Neuropathy | ||||||||||
|
| ||||||||||
| NSS – Total | 240 | 91% | 78% | 17% | 99% | 79% | 4.16 | 0.12 | 0.862 | ≥ 12 |
| NSS – Maximum | 240 | 91% | 81% | 19% | 99% | 82% | 4.84 | 0.11 | 0.863 | ≥ 5 |
| Subjective Peripheral Neuropathy Screen – Total | 240 | 100% | 74% | 16% | 100% | 75% | 3.88 | 0 | 0.863 | ≥ 6 |
| Subjective Peripheral Neuropathy Screen – Maximum | 240 | 82% | 73% | 13% | 99% | 78% | 3.26 | 0.35 | 0.839 | ≥ 2 |
| Single Question Neuropathy Screen | 240 | 100% | 52% | 9% | 100% | 55% | 2.1 | 0 | 0.762 | ---- |
| Brief Peripheral Neuropathy Screen | 240 | 18% | 93% | 10% | 96% | 89% | 2.45 | 0.88 | 0.554 | ---- |
| Monofilament | 236 | 100% | 87% | 28% | 100% | 88% | 7.76 | 0 | 0.967 | ≥ 2 |
| Graduated Tuning Fork | 238 | 100% | 78% | 18% | 100% | 79% | 4.54 | 0 | 0.9 | ---- |
| Two-Point Discrimination | 207 | 100% | 73% | 15% | 100% | 75% | 3.76 | 0 | 0.876 | ≥ 5 |
Abbreviations: Acc: Accuracy; AUC: Area Under Curve; LR: Likelihood Ratio; NSS – Neuropathy Severity Score; Sens: Sensitivity; Spec: Specificity.
Monofilament examination had the highest diagnostic utility for moderate/severe neuropathy of any modality tested with excellent specificity and positive likelihood ratio (Table 2). Graduated tuning fork examination also had good utility, though the utility of two-point discrimination was limited. The diagnostic utility of each test improved significantly when the sample was dichotomized into no/mild/moderate neuropathy versus severe neuropathy (Table 2). All 3 QST tests, the Subjective Peripheral Neuropathy Screen total score, and the Single Question Neuropathy Screen exhibited 100% sensitivity for severe neuropathy. Monofilament additionally had high specificity and accuracy. Positive predictive values for all tests were much lower due to the lower prevalence of severe neuropathy. Sensitivity analysis using the AAN/AAEM/AAPMR criteria for moderate/severe neuropathy and severe neuropathy did not demonstrate dramatic differences (Appendix 3).
DISCUSSION
Our study demonstrates that the Single Question Neuropathy Screen is an excellent screening tool for the diagnosis of moderate/severe peripheral neuropathy when administered by HCW. It has a negative predictive value of over 90%, suggesting that it could be useful in a clinical setting to identify patients who should be more carefully evaluated for more definitive diagnosis, withdrawal of neurotoxic medications, or possible nutritional supplementation. Because the Single Question Neuropathy Screen requires virtually no training and less than a minute to administer, it is feasible to implement in resource-constrained clinical settings that have high patient volume and staff turnover. One caution is that in our study, the Single Question Neuropathy Screen was actually administered as 3 separate questions (Figure 1). Therefore, its performance may vary slightly when administered as a single question. In addition, monofilament testing demonstrated high negative predictive values and may hold promise for clinical settings with additional resources or for research purposes.
FIGURE 1.
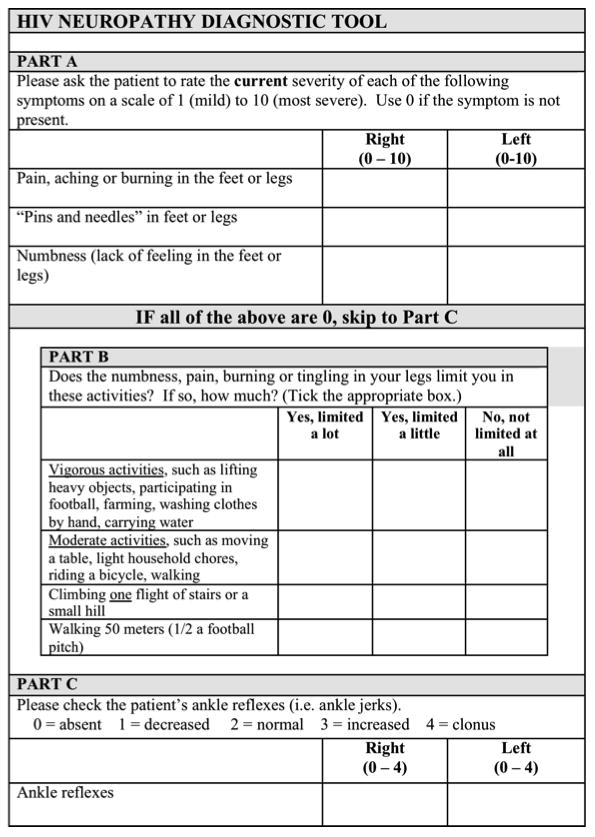
Diagnostic tool administered to study participants by non-physician healthcare workers.
Despite its simplicity, the diagnostic utility of the Single Question Neuropathy Screen in the hands of an HCW is comparable to more complex screening tools in our population and has demonstrated utility (96% sensitivity and 80% specificity) in another HIV-infected population from Zambia.9 The higher sensitivity and specificity in Zambia could be due to several factors. First, the difference between the 2 studies may be due to the choice of gold standards; the Zambian study used the Brief Peripheral Neuropathy Screen which includes neuropathic symptoms in the definition of peripheral neuropathy, whereas our study used the ACTG criteria for peripheral neuropathy which does not include neuropathic symptoms. However, sensitivity analysis using the AAN/AAEM/AAPMR criteria, which includes neuropathic symptoms, did not demonstrate substantial differences in utility. Second, in the Zambian study the individual performing the Brief Peripheral Neuropathy Screen was not blinded to the results of the Single Question Neuropathy Screen which may have led to bias. Finally, the Single Question Neuropathy Screen is a subset of the items of the Brief Peripheral Neuropathy Screen. Thus, these assessments are not completely independent and may have led to incorporation bias.22,23
More complex screening tools did not result in marked improvements in utility. While Subjective Peripheral Neuropathy Screen demonstrated slightly higher specificity than the Single Question Neuropathy Screen, it takes longer to administer and requires more training. The addition of a functional status assessment to our novel diagnostic tool – the NSS – did not significantly improve the diagnostic utility over the Subjective Peripheral Neuropathy Screen. This may be because very few participants, including those with moderate/severe neuropathy, reported functional status limitations. Our population may have reported low levels of functional impairment because: i) they had few limitations; ii) the questions did not adequately measure these limitations; or iii) cultural customs may have led to individuals minimizing their limitations. This deserves further exploration.
The Brief Peripheral Neuropathy Screen is used commonly in large studies such as those run by the AIDS Clinical Trial Groups.7,24 It has also been used successfully by HCW in a similar cohort in eastern Kenya after extensive practical training from a specialist.25 However, in our sample the Brief Peripheral Neuropathy Screen had the lowest sensitivity. Several factors may have contributed to this disparity. First, a modified version of the Brief Peripheral Neuropathy Screen was administered in this study. Vibratory testing was omitted, because tuning forks are not commonly available in primary healthcare centers in Kenya and thus would not be feasible for scale-up across our clinical setting. However, omission of vibratory testing likely does not fully account for the low sensitivity as, in the initial validation of the Brief Peripheral Neuropathy Screen, ankle jerks had much stronger associations with neuropathy than vibration sense.7
Second, despite additional training in ankle reflex assessment and the provision of reflex hammers if needed, there was poor agreement on ankle reflexes between HCW and study staff. These results are in contrast to a study from eastern Kenya.25 In that study, HCW received extensive one-on-one training in testing ankle reflexes by a specialist, were provided additional time to practice ankle reflex testing on colleagues, and still reported that assessing ankle reflexes was the most difficult portion of the Brief Peripheral Neuropathy Screen. In our prior research, nurses and clinical officers who provide HIV outpatient care in Kenya report discomfort diagnosing neurological conditions.26 Anecdotally, this is because they receive little training in Neurology during their education due to scarce resources for neurological care and teaching in Kenya, and there are only 10 neurologists in the entire country.27 Thus, the training need for HCW to reliably use screening tools is an important consideration when choosing a screening tool for widespread implementation in resource-limited settings.
Monofilament examination demonstrated the highest overall diagnostic utility and can be performed in approximately 3 minutes. Although not previously tested in HIV-infected populations, monofilament examinations have demonstrated diagnostic efficacy in diabetic neuropathy to predict foot ulceration15,28 and in leprosy to predict nerve involvement.29 In addition, nurses have successfully administered the monofilament examination to assess diabetic neuropathy in a similar setting in Tanzania.30 Furthermore, a review of 4 studies comparing monofilament to nerve conduction studies found that sensitivities ranged from 57–93% and specificities from 75–100%.31 These findings suggest that the monofilament may be useful in resource-constrained settings where a high level of diagnostic precision is required.
Graduated tuning fork examination also performed well. In other studies, graduated tuning fork examination has demonstrated good predictive values for foot ulceration in diabetes32 and could distinguish individuals with electrophysiologically confirmed polyneuropathy due to diabetes or Waldenström macroglobulinemia.12,33 However, we anticipate that reliable administration of the graduated tuning fork examination would likely require significant training to be administered correctly by HCW. It may be useful in research settings, as it provides graded assessments of neuropathy, though prior to use in longitudinal studies further testing of inter- and intra- rater reliability would be necessary.
Although two-point discrimination examination also performed well, 33 participants were excluded from the analysis because of invalid results. Anecdotally, this test was difficult to administer, and many participants had difficulty understanding and following directions for this test. It was also the most time-consuming of all the methods tested, taking 5–7 minutes to complete. Finally, prior research has also documented other limitations such as lower sensitivity and poor reliability of repeated testing in the lower extremities. 34–39
The overall prevalence of moderate and severe neuropathy was considerable regardless of the diagnostic criteria used (ACTG vs AAN/AAEM/AAPMR). However, the prevalence of mild neuropathy was substantially higher using the ACTG criteria. The primary difference between the 2 criteria is that the AAN/AAEM/AAPMR requires neuropathic symptoms (numbness, paresthesias, pain) as well as 2 neurological signs, while the ACTG criteria requires only 1 sign. The clinical significance of neurological signs of neuropathy in the absence of symptoms is not clear.40 Further longitudinal research and correlation with nerve conduction studies will be important to determine which of these diagnostic criteria is more clinically relevant for peripheral neuropathy in the setting of HIV in resource-limited settings.
Nonetheless, these estimates of the prevalence of peripheral neuropathy were generally comparable to previous studies from similar settings where prevalence ranged from 49% to 76%.4,5 The high prevalence of peripheral neuropathy may be in part because a high proportion of participants were currently taking or had previously taken stavudine and/or isoniazid, which have well-known neurotoxic effects.41,42 A South African cohort of individuals who had taken stavudine for more that 6 months demonstrated a peripheral neuropathy prevalence rate of 57%.43 Many participants in our study had an elevated mean corpuscular volume, which was used as a proxy for vitamin B12 deficiency. However, these results may be difficult to interpret, as stavudine and zidovudine, 2 of the first-line antiretroviral medications in Kenya, have both been shown to induce macrocytosis, and 59% of participants with neuropathy in this study were currently on stavudine and/or zidovudine.44
Many established neuropathy risk factors were also found to be significantly associated with moderate/severe neuropathy in this population, including age, WHO stage, and history of stavudine use.43,45 In contrast to a recent Zambian study, poor nutrition, as measured by food insecurity and BMI, did not appear to be a risk factor.5 However, a recent study from Thailand found no significant association between BMI and neuropathy.46 Similarly, alcohol use did not appear to be a risk factor in our cohort. This may be explained by under-reporting; in our population, self-reported alcohol use was very low among study participants, though prior research suggests that 28% of men and 7% of women presenting to primary healthcare centers in Kenya have alcohol dependence.47
This study has several limitations. First, it was not possible to definitively identify other etiologies of neuropathy due to resource limitations; instead we used a chart audit and survey. Second, we were not able to use an objective gold standard like epidermal nerve fiber density or neurophysiological studies due to resource limitations.48 Although imperfect, a standardized clinical assessment of neuropathy has been used widely in other studies as a reference test.4,20,48 Third, the experience and tool-specific training of the HCW administering the diagnostic tool at each site varied. While each HCW received a brief one-to-one or small group training by study staff on the day the tool was administered, some HCW also attended a half day training session on the neurological exam given a few months before study initiation.26 Regardless, these short training sessions were not enough to enable reliable testing of the ankle reflexes, suggesting that screening tools which rely on neurological examination are not likely the best choices for widespread implementation in HIV outpatient care settings.
In general, the screening tools and QST that we tested in this study did not perform as well as in our pilot study.19 However, because our pilot study was so small (n=30) the confidence intervals around the estimates of sensitivity and specificity, in most cases, overlap the estimates presented here (data not shown). However, in the pilot study a neurologist confirmed all the gold standard examinations, while in this study a variety of individuals with different levels of training performed the gold standard examinations. We were unable to calculate inter-observer agreement between our gold standard examinations because of resource limitations and the fact that many of our study sites were quite remote. However, there was no significant difference between prevalence estimates for moderate-severe peripheral neuropathy as diagnosed by each of our examiners (χ2=3.79; P=0.29).
Finally, the administration of QST had limitations. The individual administering QST was not blinded to and typically performed the clinical assessment and diagnosis of neuropathy, which may have resulted in bias. To minimize bias, diagnoses and QST scoring were based on objective findings and explicit protocols. Finally, QST was nearly always performed after the neurological examination and frequently at the end of the study protocol, so participant fatigue could have resulted in additional variability in QST results.
In conclusion, neuropathy is a prevalent condition in resource-limited settings. Because neuropathy can often be treated with symptom management, nutritional supplementation, or modification of offending medication regimens, identification of individuals with neuropathy is essential to improve long-term health outcomes for individuals living with HIV-infection. Our results indicate that the Single Question Neuropathy Screen has excellent sensitivity and negative predictive value for neuropathy when administered by HCW in resource-constrained HIV outpatient clinical settings. Since it requires virtually no training and less than a minute to administer, it could easily be implemented across sub-Saharan Africa. Monofilament testing also shows promise for identifying peripheral neuropathy in clinical settings with more resources or for research purposes. Accurate and early diagnosis of neuropathy with these tools could prevent significant morbidity and lead to improved quality of life of HIV-infected persons in resource-limited settings.
Supplementary Material
Acknowledgments
This study was supported by the Fulbright African Regional Research Program (Meyer), American Academy of Neurology Practice Research Training Fellowship (Meyer), Doris Duke International Clinical Research Fellowship (Cettomai), and American Medical Association Foundation Seed Grant (Cettomai). In addition, this study was supported by the Fogarty International Clinical Research Fellowship (Meyer, Kwasa) (5 R24 TW00798; 3 R24 TW00798-02S1) from the National Institutes of Health, Fogarty International Center through Vanderbilt University, the National Cancer Institute (NCI), the National Institute on Drug Abuse (NIDA), Office of the Director, National Institutes of Health and the National Institute of Mental Health (NIMH).
We would like to thank the medical officers, clinical officers, nurses, staff and patients at FACES for their participation. In addition, we would like to thank Justin McArthur, MBBS, MPH, Edwin Lwanya, Elizabeth Opiyo, and John Onyuo for their contributions to our work. This paper is published with the permission of the Director of KEMRI.
Dr. Deanna Cettomai has received research support from the Doris Duke Charitable Foundation and an NIH/Johns Hopkins Pre-Doctoral Clinical Research Training Program T32 grant.
Dr. Judith Kwasa has received research support from the NIH Fogarty International Clinical Research Scholarship.
Dr. Gretchen Birbeck has received NIH research support, including travel and meeting attendance related to R01, R21 and K23 awards, as well as research support from the Doris Duke Charitable Fund.
Dr. Richard Price has received support from NIH/NIMH research grants, an investigator-initiated research grant from Merck and a lecture honorarium from Abbott.
Dr. Craig Cohen has received funds from Osel, Inc. to conduct a Phase 2a clinical trial of LACTIN-V, a vaginal probiotic to prevent recurrent bacterial vaginosis.
Dr. Elizabeth Bukusi has received funding from NIH, CDC, the Bill and Melinda Gates Foundation, and the International Partnership for Microbicides.
Dr. Ana-Claire Meyer has received research support from the Fulbright African Regional Research Program, NIH Fogarty International Clinical Research Fellowship (5 R24 TW00798; 3 R24 TW00798-02S1). She is currently the recipient of a K01 and R21 from NIH.
List of Abbreviations
- AAEM
American Association of Electrodiagnostic Medicine
- AAN
American Academy of Neurology
- AAPMR
American Academy of Physical Medicine and Rehabilitation
- ACTG
AIDS Clinical Trials Group
- AIDS
Acquired Immunodeficiency Syndrome
- BMI
body mass index
- FACES
Family AIDS Care and Education Services
- HCW
health care workers
- HIV
Human Immunodeficiency Virus
- MCV
mean corpuscular volume
- NSS
Neuropathy Severity Score
- QST
quantitative sensory testing
- RPR
rapid plasma reagin
- WHO
World Health Organization
Footnotes
Ms. Caroline Kendi has nothing to disclose.
References
- 1.McArthur J. HIV dementia: an evolving disease. J Neuroimmunology. 2004;157:3–10. doi: 10.1016/j.jneuroim.2004.08.042. [DOI] [PubMed] [Google Scholar]
- 2.Ellis R, Rosario D, Clifford DB, McArthur JC, Simpson DM, Alexander T, Gelman B, Vaida F, Collier A, Marra C, Ances B, Atkinson J, Dworkin R, Morgello S, Grant I for the CHARTER study group. Continued high prevalence and adverse clinical impact of human immunodeficiency virus-assocated sensory neuropathy in the era of combination antiretroviral therapy: the CHARTER study. Arch Neurol. 2010;67:552–558. doi: 10.1001/archneurol.2010.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghosh S, Chandran A, Jansen J. Epidemiology of HIV-Related Neuropathy: A Systematic Literature Review. AIDS Research and Human Retroviruses. 2012;28:36–48. doi: 10.1089/AID.2011.0116. [DOI] [PubMed] [Google Scholar]
- 4.Maritz J, Benatar M, Dave JA, Harrison TB, Badri M, Levitt NS, Heckmann JM. HIV neuropathy in South Africans: frequency, characteristics, and risk factors. Muscle Nerve. 2010;41:599–606. doi: 10.1002/mus.21535. [DOI] [PubMed] [Google Scholar]
- 5.Birbeck GL, Kvalsund MP, Byers PA, Bradbury R, Mang’ombe C, Organek N, Kaile T, Sinyama AM, Sinyangwe SS, Malama K, Malama C. Neuropsychiatric and socioeconomic Status Impact Antiretroviral Adherence and Mortality in Rural Zambia. Am J Trop Med Hyg. 2011;85:782–789. doi: 10.4269/ajtmh.2011.11-0187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Price R. Neurological complications of HIV infection. Lancet. 1996;348:445–452. doi: 10.1016/S0140-6736(95)11035-6. [DOI] [PubMed] [Google Scholar]
- 7.Cherry C, Wesselingh S, Lal L, McArthur J. Evaluation of a clinical screening tool for HIV-associated sensory neuropathies. Neurology. 2005;65:1778–1781. doi: 10.1212/01.wnl.0000187119.33075.41. [DOI] [PubMed] [Google Scholar]
- 8.Shumbusho F, van Griensven J, Lowrance D, Turate I, Weaver MA, Price J, Binagwaho A. Task shifting for scale-up of HIV care: evaluation of nurse-centered antiretroviral treatment at rural health centers in Rwanda. PLoS Med. 2009;6:e1000163. doi: 10.1371/journal.pmed.1000163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kandiah PA, Atadzhanov M, Kvalsund MP, Birbeck GL. Evaluating the diagnostic capacity of a single-question neuropathy screen (SQNS) in HIV positive Zambian adults. J Neurol Neurosurg Psychiatry. 2010;81:1380–1381. doi: 10.1136/jnnp.2009.183210. [DOI] [PubMed] [Google Scholar]
- 10.Venkataramana AB, Skolasky RL, Creighton JA, McArthur JC. Diagnostic utility of the subjective peripheral neuropathy screen in HIV-infected persons with peripheral sensory polyneuropathy. AIDS Read. 2005;15:341–344. 348–349, 354. [PubMed] [Google Scholar]
- 11.McArthur JH. The reliability and validity of the subjective peripheral neuropathy screen. J Assoc Nurses AIDS Care. 1998;9:84–94. doi: 10.1016/S1055-3290(98)80048-4. [DOI] [PubMed] [Google Scholar]
- 12.Martina IS, van Koningsveld R, Schmitz PI, van der Meche FG, van Doorn PA. Measuring vibration threshold with a graduated tuning fork in normal aging and in patients with polyneuropathy. European Inflammatory Neuropathy Cause and Treatment (INCAT) group. J Neurol Neurosurg Psychiatry. 1998;65:743–747. doi: 10.1136/jnnp.65.5.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Merkies IS, Schmitz PI, van der Meche FG, van Doorn PA. Reliability and responsiveness of a graduated tuning fork in immune mediated polyneuropathies. The Inflammatory Neuropathy Cause and Treatment (INCAT) Group. J Neurol Neurosurg Psychiatry. 2000;68:669–671. doi: 10.1136/jnnp.68.5.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Periyasamy R, Manivannan M, Narayanamurthy VB. Changes in Two Point Discrimination and the law of mobility in Diabetes Mellitus patients. J Brachial Plex Peripher Nerve Inj. 2008;3:3. doi: 10.1186/1749-7221-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mayfield JA, Sugarman JR. The use of the Semmes-Weinstein monofilament and other threshold tests for preventing foot ulceration and amputation in persons with diabetes. J Fam Pract. 2000;49:S17–29. [PubMed] [Google Scholar]
- 16.Frerichs R. Simple Analytic Procedures for Rapid Microcomputer-Assisted Cluster Surveys in Developing Countries. Public Health Reports. 1989;104:24–35. [PMC free article] [PubMed] [Google Scholar]
- 17.Medical Outcomes Study Core Survey Instrument. RAND Health. 2008 [Google Scholar]
- 18.National AIDS and STI Control Program; Health Mo, editor. Guidelines for Antiretroviral Drug Therapy in Kenya. 3. Nairobi; 2006. [Google Scholar]
- 19.Cettomai D, Kwasa J, Kendi C, Birbeck GL, Price R, Bukusi E, Cohen C, Meyer A. Utility of Quantitative Sensory Testing and Screening Tools in Identifying HIV-Associated Peripheral Neuropathy in Western Kenya: Pilot Testing. PLoS One. 2011;5:e14256. doi: 10.1371/journal.pone.0014256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cherry CL, Affandi JS, Imran D, Yunihastuti E, Smyth K, Vanar S, Kamarulzaman A, Price P. Age and height predict neuropathy risk in patients with HIV prescribed stavudine. Neurology. 2009;73:315–320. doi: 10.1212/WNL.0b013e3181af7a22. [DOI] [PubMed] [Google Scholar]
- 21.England J, Gronseth G, Franklin G, Miller R, Asbury A, Carter G, Cohen J, Fisher M, Howard J, Kinsella L, Latov N, Lewis R, Low P, Sumner A. Distal symmetric polyneuropathy: A definition for clinical research. Report of the American Academy of Neurology, the American Association of Electrodiagnostic Medicine, and the American Academy of Physical Medicine and Rehabilitation. Neurology. 2005;64:199–207. doi: 10.1212/01.WNL.0000149522.32823.EA. [DOI] [PubMed] [Google Scholar]
- 22.Furukawa T, Guyatt G. Sources of bias in diagnostic accuracy studies and the diagnostic process. CMAJ. 2006:174. doi: 10.1503/cmaj.060014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rutjes A, Reitsma J, Di Nisio M, Smidt N, van Rijn J, Bossuyt P. Evidence of bias and variation in diagnostic accuracy studies. CMAJ. 2006:174. doi: 10.1503/cmaj.050090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simpson DM, Katzenstein DA, Hughes MD, Hammer SM, Williamson DL, Jiang Q, Pi JT. Neuromuscular function in HIV infection: analysis of a placebo-controlled combination antiretroviral trial. AIDS Clinical Group 175/801 Study Team. AIDS. 1998;12:2425–2432. doi: 10.1097/00002030-199818000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Mehta SA, Ahmed A, Kariuki BW, Said S, Omasete F, Mendillo M, Laverty M, Holzman R, Valentine F, Sivapalasingam S. Implementation of a validated peripheral neuropathy screening tool in patients receiving antiretroviral therapy in Mombasa, Kenya. Am J Trop Med Hyg. 2010;83:565–570. doi: 10.4269/ajtmh.2010.09-0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cettomai D, Kwasa J, Birbeck GL, Price R, Bukusi E, Meyer A. Training needs and evaluationof a neuro-HIV training module for non-physician healthcare workers in Western Kenya. Journal of the Neurological Sciences. 2011;307:92–96. doi: 10.1016/j.jns.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jowi J. Provision of care to people with epilepsy in Kenya. East Afr Med J. 2007;84:97–99. [PubMed] [Google Scholar]
- 28.Armstrong D, Lavery L, Vela S, Quebedeaux T, Fleischli J. Choosing a Practical Screening Instrument to Identify Patients at Risk for Diabetic Foot Ulceration. Arch Intern Med. 1998;158:289–292. doi: 10.1001/archinte.158.3.289. [DOI] [PubMed] [Google Scholar]
- 29.van Brakel W, Nicholls P, Wilder-Smith E, Das L, Barkataki P, Lockwood D on behalf of the INFIR Study Group. Early Diagnosis of Neuropathy in Leprosy-Comparing Diagnostic Tests in a Large Prospective Study (the INFIR Cohort Study) PLOS Neglected Tropical Diseases. 2008;2:e212. doi: 10.1371/journal.pntd.0000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smide B. Outcome of foot examinations in Tanzanian and Swedish diabetic patients, a comparative study. J Clin Nurs. 2009;18:391–398. doi: 10.1111/j.1365-2702.2008.02492.x. [DOI] [PubMed] [Google Scholar]
- 31.Feng Y, Schlosser F, Sumpio B. The Semmes Weinstein monofilament examination as a screening tool for diabetic peripheral neuropathy. J Vasc Surg. 2009;50:675–682. doi: 10.1016/j.jvs.2009.05.017. [DOI] [PubMed] [Google Scholar]
- 32.Sosenko J, Kato M, Soto R, Bild D. Comparison of Quantitative Sensory Threshold Measures for Their Association with Foot Ulceration in Diabetic Patients. Diabetes Care. 1990;13:1057–1061. doi: 10.2337/diacare.13.10.1057. [DOI] [PubMed] [Google Scholar]
- 33.Pestronk A, Florence J, Levine T, Al-Lozi M, Lopate G, Miller T, Ramneantu I, Waheed W, Stambuk M. Sensory exam with a quantitative tuning fork: Rapid, sensitive and predictive of SNAP amplitude. Neurology. 2004:62. doi: 10.1212/01.wnl.0000106939.41855.36. [DOI] [PubMed] [Google Scholar]
- 34.Spindler HA, Dellon AL. Nerve conduction studies and sensibility testing in carpal tunnel syndrome. J Hand Surg Am. 1982;7:260–263. doi: 10.1016/s0363-5023(82)80176-7. [DOI] [PubMed] [Google Scholar]
- 35.Marlowe ES, Bonner FJ, Jr, Berkowitz AR. Correlation between two-point discrimination and median nerve sensory response. Muscle Nerve. 1999;22:1196–1200. doi: 10.1002/(sici)1097-4598(199909)22:9<1196::aid-mus5>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 36.Aszmann OC, Dellon AL. Relationship between cutaneous pressure threshold and two-point discrimination. J Reconstr Microsurg. 1998;14:417–421. doi: 10.1055/s-2007-1000202. [DOI] [PubMed] [Google Scholar]
- 37.Braddom RL, Hollis JB, Castell DO. Diabetic peripheral neuropathy: a correlation of nerve conduction studies and clinical findings. Arch Phys Med Rehabil. 1977;58:308–313. [PubMed] [Google Scholar]
- 38.Gelberman RH, Szabo RM, Williamson RV, Dimick MP. Sensibility testing in peripheral-nerve compression syndromes. An experimental study in humans. J Bone Joint Surg Am. 1983;65:632–638. [PubMed] [Google Scholar]
- 39.Nakazumi Y, Hamasaki M. Electrophysiological studies and physical examinations in entrapment neuropathy: sensory and motor functions compensation for the central nervous system in cases with peripheral nerve damage. Electromyogr Clin Neurophysiol. 2001;41:345–348. [PubMed] [Google Scholar]
- 40.Kamerman P, Wadley A, Cherry C. HIV-Associated Sensory Neuropathy: Risk Factors and Genetics. Curr Pain Headache Rep. 2012:16. doi: 10.1007/s11916-012-0257-z. [DOI] [PubMed] [Google Scholar]
- 41.Sacktor N, Nakasujja N, Skolasky RL, Robertson K, Musisi S, Ronald A, Katabira E, Clifford DB. Benefits and risks of stavudine therapy for HIV-associated neurologic complications in Uganda. Neurology. 2009;72:165–170. doi: 10.1212/01.wnl.0000339042.96109.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marks DJ, Dheda K, Dawson R, Ainslie G, Miller RF. Adverse events to antituberculosis therapy: influence of HIV and antiretroviral drugs. Int J STD AIDS. 2009;20:339–345. doi: 10.1258/ijsa.2008.008361. [DOI] [PubMed] [Google Scholar]
- 43.Wadley AL, Cherry CL, Price P, Kamerman PR. HIV Neuropathy Risk Factors and Symptom Characterization in Stavudine-Exposed South Africans. J Pain Symptom Manage. 2011;41:700–706. doi: 10.1016/j.jpainsymman.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 44.Geene D, Sudre P, Anwar D, Goehring C, Saaidia A, Hirschel B. Causes of macrocytosis in HIV-infected patients not treated with zidovudine. Swiss HIV Cohort Study. J Infect. 2000;40:160–163. doi: 10.1053/jinf.1999.0628. [DOI] [PubMed] [Google Scholar]
- 45.Cherry CL, Skolasky RL, Lal L, Creighton J, Hauer P, Raman SP, Moore R, Carter K, Thomas D, Ebenezer GJ, Wesselingh SL, McArthur JC. Antiretroviral use and other risks for HIV-associated neuropathies in an international cohort. Neurology. 2006;66:867–873. doi: 10.1212/01.wnl.0000203336.12114.09. [DOI] [PubMed] [Google Scholar]
- 46.Konchalard K, Wangphonpattanasiri K. Clinical and electrophysiologic evaluation of peripheral neuropathy in a group of HIV-infected patients in Thailand. J Med Assoc Thai. 2007;90:774–781. [PubMed] [Google Scholar]
- 47.World Health Organization. Global Status Report on Alcohol 2004. Geneva: World Health Organization; 2004. [Google Scholar]
- 48.McArthur JC, Stocks EA, Hauer P, Cornblath DR, Griffin JW. Epidermal nerve fiber density: normative reference range and diagnostic efficiency. Arch Neurol. 1998;55:1513–1520. doi: 10.1001/archneur.55.12.1513. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


