Abstract
A prediction model was developed in the Framingham Heart Study (FHS) to evaluate short-term risk of hypertension. Our goal was to determine the predictive ability of the FHS hypertension model in a cohort of young adults advancing into middle age and compare it with the predictive ability of prehypertension, and individual components of the FHS model. We studied 4,388 participants, age 18-30 years without hypertension at baseline, enrolled in the Coronary Artery Risk Development in Young Adults (CARDIA) Study who participated in 2 consecutive exams occurring 5 years apart between the baseline (1985-1986) and Year 25 examination (2010-2011). Weibull regression was used to assess the association of the FHS model overall, individual components of the FHS model, and prehypertension with incident hypertension. Over the 25 year follow-up period, 1179 participants developed incident hypertension. The FHS hypertension model (c-index=0.84, 95% CI=0.83, 0.85) performed well in discriminating those who did and did not develop hypertension and was better than prehypertension alone (c-index=0.71, 95% CI=0.70, 0.73). The predicted risk from the FHS hypertension model was systematically lower than the observed hypertension incidence initially (χ2= 249.4; p<0.001), but demonstrated a good fit after recalibration (χ2= 14.6; p=0.067). In summary, the FHS model performed better than prehypertension and may be a useful tool for identifying young adults with a high risk for developing hypertension.
Keywords: hypertension, prehypertension, epidemiology, risk
INTRODUCTION
Hypertension affects nearly 1 in 3 adults in the US,1 with the lifetime risk of hypertension approaching 90% for middle-aged, normotensive adults.2, 3 Because the sequelae of hypertension include cardiovascular morbidity and mortality, effective prevention strategies are essential for reducing the public health burden of hypertension. Lifestyle modification and pharmacologic therapy have been shown to lower blood pressure and reduce the risk of developing hypertension4-6 and may be important components of early interventions among high-risk individuals. The precursors of cardiovascular risk factors manifest early in life, so identifying young adults at high risk for hypertension has important implications for the development and implementation of prevention strategies.
To better identify high-risk individuals who should be targeted for early interventions, the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7)7 added prehypertension, defined as systolic blood pressure (SBP) between 120 and 139 mmHg and/or diastolic blood pressure (DBP) between 80 and 89 mmHg among individuals not meeting hypertension criteria, as an official blood pressure classification in 2003. Several studies have reported that individuals with prehypertension are more likely to progress to hypertension compared with individuals with normal SBP and DBP.8-10 However, with 28% of adults in the US having prehypertension,1 additional approaches may be needed to better identify individuals at high risk for hypertension.
Framingham Heart Study (FHS) investigators developed a hypertension risk prediction model that included age, sex, SBP, DBP, body mass index, cigarette smoking, and parental history of hypertension.11 The prognostic value of this FHS model has been validated in at least two external cohorts.12, 13 However, it has also been reported that SBP alone predicted incident hypertension just as well as the FHS model in a multi-ethnic cohort of middle-aged and older adults in the US.13
The performance of the FHS model among young adults has not been evaluated. The incidence of hypertension increases with age,1 so young adults are a key demographic for identifying those at high risk for hypertension. The purpose of this study was to evaluate the predictive ability of the FHS model for the incidence of hypertension and compare its performance with prehypertension alone, and individual components of the FHS model among African-American and white adults from the Coronary Artery Risk Development in Young Adults (CARDIA) Study.
METHODS
Study Design and Population
CARDIA is a prospective, community-based cohort study of young adults designed to investigate trends and determinants of cardiovascular disease in the US. A detailed overview of the study design, recruitment, and objectives has been previously published.14
Briefly, the baseline examination (1985-1986) included 5,115 African-American and white men and women aged 18-30 years from 4 urban areas: Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA. In-person follow-up examinations were conducted at 2 (1987-1988), 5 (1990-1991), 7 (1992-1993), 10 (1995-1996), 15 (2000-2001), 20 (2005-2006), and 25 (2010-2011) years following the baseline examination. Participant retention rates for each of the follow-up examinations were high, with 72% (n=3,499) of surviving participants completing the year 25 examination. Each in-person examination included interviewer-administered questionnaires, physical examination, and specimen collection. Centralized training and certification, standardized methods, and quality control measures were implemented to ensure high data quality for all examinations. The Institutional Review Board at each participating site approved each study examination and participants provided written informed consent.
Participants with hypertension at baseline (n=146), missing covariates (n=50), and did not attend 2 consecutive examinations occurring 5 years apart during the study period (n=504) were excluded. Additionally, participants with diabetes at baseline (n=27) were excluded to correspond with the FHS exclusion criteria, resulting in a sample size of 4,388 participants eligible for these analyses.
Blood Pressure Measurement
SBP and DBP were measured at each CARDIA examination following standardized protocols.15 After resting for 5 minutes in the seated position, blood pressure was measured three times at one-minute intervals using an appropriate sized cuff, with the average of the second and third measurements used to determine SBP and DBP. SBP and DBP were measured using a random zero sphygmomanometer at baseline and years 5, 10, and 15 and a standard automated BP measurement monitor (Omron® model HEM907XL) at years 20 and 25. The BP measurements at years 20 and 25 were calibrated to random zero sphygmomanometer values based on dual readings on a subset of CARDIA participants to ensure comparability (please see http://hyper.ahajournals.org).16 Data on antihypertensive medication use was collected at each examination via self-report and data abstraction of medication bottles brought to the examination. Incident hypertension was defined as the first study examination at which the participant had SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg and/or initiated treatment with antihypertensive medications. Prehypertension was defined as 120≤SBP≤139 mmHg or 80≤SBP≤89 mmHg among those not meeting hypertension criteria.7
Ascertainment of Covariates
Information on age, sex, race, smoking status, and parental history of hypertension was collected using standardized questionnaires. Height and weight were measured by certified technicians with participants wearing light clothing and no shoes and were used to calculate body mass index (BMI) in kg/m2.15 Participants fasted for 8 hours prior to each CARDIA examination for the collection of fasting blood samples. Diabetes was defined as fasting glucose ≥ 7.0 mmol/l (126 mg/dL) or use of antihyperglycemic therapy.
FHS Risk Prediction Model
The FHS risk prediction model11 consists of the following components: age, sex, BMI, smoking, parental history of hypertension, SBP, and DBP. The model also contains an interaction term between age and DBP. Age, BMI, SBP, and DBP were evaluated as continuous variables. Sex (women vs. men), smoking (current vs. former or never smoker), and parental history of hypertension (both, one, or no parental history) were evaluated as categorical variables. The predicted risk of hypertension was calculated for each participant using the FHS equation below:
where X = time in years between examinations and Y = 22.9495 – 0.1564*age – 0.2029*women – 0.0593*SBP – 0.1285*DBP – 0.1907*smoking – 0.1661*parental hypertension – 0.0339*BMI + 0.001624*age*DBP.
Statistical Analyses
The total follow-up period was 25 years, with the median time interval between examinations being 5 years. Data from the years 2 and 7 examinations were not included in this analysis to allow equally spaced time intervals for the assessment of incident hypertension. The time interval between 2 CARDIA examinations comprised a single time period and participants could contribute up to 5 time periods at risk for hypertension: (1) baseline to year 5 exam; (2) year 5 exam to year 10 exam; (3) year 10 exam to year 15 exam; (4) year 15 exam to year 20 exam; and (5) year 20 exam to year 25 exam. The 4,388 participants contributed 15,166 time periods at risk, with FHS components updated at the beginning of each time interval. If a participant developed hypertension, they were no longer at risk for hypertension and were not included in subsequent time periods. If a participant did not develop hypertension, they were still considered at risk and included in subsequent time periods if they attended those examinations. Weibull regression for interval-censored data was used to evaluate the association of the FHS model, prehypertension model, and individual components of the FHS model with incident hypertension.17, 18
Discrimination was evaluated using the c-index to assess how the model performed in identifying those who did and did not develop hypertension in CARDIA. C-indexes were calculated for the FHS model, prehypertension, and individual FHS model components. Because the data were interval-censored and the exact date participants developed hypertension was unknown, uniform resampling of event times was used for calculating the c-index and its 95% confidence interval based on 200 resamples. Bayes information criterion (BIC) was used to compare the performance of the models, with a lower BIC indicating better model fit. Using the FHS model, the predicted risk for hypertension was calculated for each participant for each time period at risk. Participants were grouped into deciles based on their predicted risk for hypertension and calibration was evaluated using the modified Hosmer-Lemeshow goodness of fit chi-square statistic to compare predicted risk to observed risk for hypertension across deciles.19 Additionally, a recalibrated model was generated by replacing the FHS hypertension incidence with the observed CARDIA hypertension incidence20 and a best fit model was generated using the variables from the FHS model applied in the CARDIA study. All statistical analyses were conducted using SAS version 9.2 (SAS Institute, Cary, NC).
RESULTS
Participant characteristics at baseline are presented overall in Table 1. The mean age of participants was 24.9 years, 55.5% of the participants were women, and 49.3% were African-American. Most participants had SBP < 120 mmHg and DBP < 80 mmHg, although 22.1% had prehypertension at baseline.
Table 1.
Baseline characteristics of participants: the Coronary Artery Risk Development in Young Adults (CARDIA) Study
| Participant characteristics | Overall N = 4388 |
|---|---|
| Age (mean, SD) | 24.9 (3.6) |
| Sex | |
| Men, n (%) | 1951 (44.5) |
| Women, n (%) | 2437 (55.5) |
| Race | |
| African-American | 2163 (49.3) |
| White | 2225 (50.7) |
| Education | |
| High school graduate or less | 1659 (37.8) |
| Some college | 2292 (52.2) |
| Graduate/professional school | 437 (10.0) |
| Smoking status | |
| Not current smoker, n (%) | 3098 (70.6) |
| Current smoker, n (%) | 1290 (29.4) |
| Body mass index, kg/m2 | |
| Normal (<25), n (%) | 2899 (66.1) |
| Overweight (25-29.9), n (%) | 1005 (22.9) |
| Obese (≥30.0), n (%) | 484 (11.0) |
| Parental history of hypertension | |
| Neither had HTN, n (%) | 2210 (50.4) |
| One had HTN, n (%) | 1741 (39.7) |
| Both had HTN, n (%) | 437 (9.9) |
| Systolic blood pressure, mm Hg | |
| < 110, n (%) | 2395 (54.6) |
| 110-114, n (%) | 577 (13.2) |
| 115-119, n (%) | 631 (14.4) |
| 120-124, n (%) | 462 (10.5) |
| 125-129, n (%) | 184 (4.2) |
| 130-134, n (%) | 106 (2.4) |
| 135-139, n (%) | 33 (0.8) |
| Diastolic blood pressure, mm Hg | |
| <70, n (%) | 2664 (60.7) |
| 70-74, n (%) | 683 (15.6) |
| 75-79, n (%) | 595 (13.6) |
| 80-84, n (%) | 320 (7.3) |
| 85-89, n (%) | 126 (2.9) |
| Prehypertension* | |
| No, n (%) | 3417 (77.9) |
| Yes, n (%) | 971 (22.1) |
Prehypertension defined as systolic blood pressure 120-139 mm Hg or diastolic blood pressure 80-89 mm Hg.
Between the baseline and year 25 examinations, 1179 incident hypertension events occurred, with a higher incidence noted among those who were obese, had higher SBP and DBP levels, and had prehypertension (Table 2). In a multivariable adjusted model, each of the individual components of the FHS model was associated with incident hypertension during follow-up (please see http://hyper.ahajournals.org). Additionally, prehypertension was associated with incident hypertension in an unadjusted model (hazard ratio (HR) = 6.81, 95% confidence interval (CI) = 6.06, 7.66).
Table 2.
5-year cumulative incidence for hypertension: the Coronary Artery Risk Development in Young Adults (CARDIA) Study
| Participant characteristics | No. of Events | Time Periods at Risk* | Percentage Developing Hypertension over 5 years |
|---|---|---|---|
| Overall | 1179 | 15166 | 7.8 |
| Age | |||
| <25 years | 53 | 2159 | 2.5 |
| 25 years and older | 1126 | 13007 | 8.7 |
| Sex | |||
| Men | 549 | 6548 | 8.4 |
| Women | 630 | 8618 | 7.3 |
| Race | |||
| African-American | 758 | 6670 | 11.4 |
| White | 421 | 8496 | 5.0 |
| Smoking status | |||
| Not current smoker | 861 | 11513 | 7.5 |
| Current smoker | 318 | 3653 | 8.7 |
| Body mass index, kg/m2 | |||
| Normal (<25) | 272 | 7557 | 3.6 |
| Overweight (25-29.9) | 402 | 4548 | 8.8 |
| Obese (≥30.0) | 505 | 3061 | 16.5 |
| Parental history of hypertension | |||
| Neither had HTN | 458 | 7859 | 5.8 |
| One had HTN | 541 | 5905 | 9.2 |
| Both had HTN | 180 | 1402 | 12.8 |
| Systolic blood pressure, mm Hg | |||
| < 110 | 187 | 8391 | 2.2 |
| 110-114 | 194 | 2524 | 7.7 |
| 115-119 | 247 | 1987 | 12.4 |
| 120-124 | 210 | 1230 | 17.1 |
| 125-129 | 169 | 582 | 29.0 |
| 130-134 | 113 | 329 | 34.3 |
| 135-139 | 59 | 123 | 48.0 |
| Diastolic blood pressure, mm Hg | |||
| <70 | 171 | 7761 | 2.2 |
| 70-74 | 180 | 3185 | 5.7 |
| 75-79 | 305 | 2364 | 12.9 |
| 80-84 | 314 | 1295 | 24.2 |
| 85-89 | 209 | 561 | 37.3 |
| Prehypertension† | |||
| No | 457 | 12044 | 3.8 |
| Yes | 722 | 3122 | 23.1 |
Participants could contribute up to 5 time periods at risk.
Prehypertension defined as systolic blood pressure 120-139 mm Hg or diastolic blood pressure 80-89 mm Hg.
The FHS model performed well in discriminating between those who did and did not develop hypertension (c-index=0.84, 95% CI=0.83, 0.85). This model demonstrated better performance than a model that included prehypertension only (c-index=0.71, 95% CI=0.70, 0.73). The FHS model also demonstrated better performance when compared with the individual components of the FHS model (Table 3). Overall, current smoking and sex discriminated poorly, whereas the interaction of age and DBP had the highest discrimination (c-index=0.81, 95% CI=0.79, 0.82) among the individual FHS model components. The FHS model had a lower BIC (BIC=6322.49), indicating good model fit, than prehypertension (BIC=7291.02) and each of the individual components of the FHS model. When analyses were stratified by race, the discrimination performance for each of the models was similar for African-American and white participants and the FHS model had the lowest BIC for African-American and white participants.
Table 3.
C-indexes (95% CI) for incident hypertension, the Coronary Artery Risk Development in Young Adults (CARDIA) Study
| Models | Overall | African-Americans | Whites |
|---|---|---|---|
| Framingham Model | 0.84 (0.83, 0.85) | 0.81 (0.79, 0.82) | 0.87 (0.86, 0.89) |
| Individual Components of Framingham Model | |||
| Age | 0.66 (0.65, 0.68) | 0.68 (0.66, 0.69) | 0.70 (0.68, 0.73) |
| Sex | 0.52 (0.50, 0.53) | 0.51 (0.50, 0.52) | 0.55 (0.53, 0.58) |
| Current smoking | 0.52 (0.50, 0.53) | 0.51 (0.50, 0.52) | 0.51 (0.50, 0.52) |
| Body mass index | 0.69 (0.68, 0.71) | 0.65 (0.63, 0.67) | 0.72 (0.70, 0.74) |
| Parental history of hypertension | 0.58 (0.56, 0.59) | 0.56 (0.54, 0.58) | 0.56 (0.54, 0.58) |
| Systolic blood pressure | 0.78 (0.77, 0.80) | 0.74 (0.73, 0.76) | 0.81 (0.80, 0.83) |
| Diastolic blood pressure | 0.78 (0.77, 0.80) | 0.75 (0.73, 0.77) | 0.81 (0.79, 0.83) |
| Age, diastolic blood pressure, and interaction | 0.81 (0.79, 0.82) | 0.78 (0.77, 0.80) | 0.85 (0.83, 0.86) |
| Prehypertension Only Model* | 0.71 (0.70, 0.73) | 0.69 (0.67, 0.71) | 0.73 (0.71, 0.75) |
Prehypertension defined as systolic blood pressure 120-139 mm Hg or diastolic blood pressure 80-89 mm Hg.
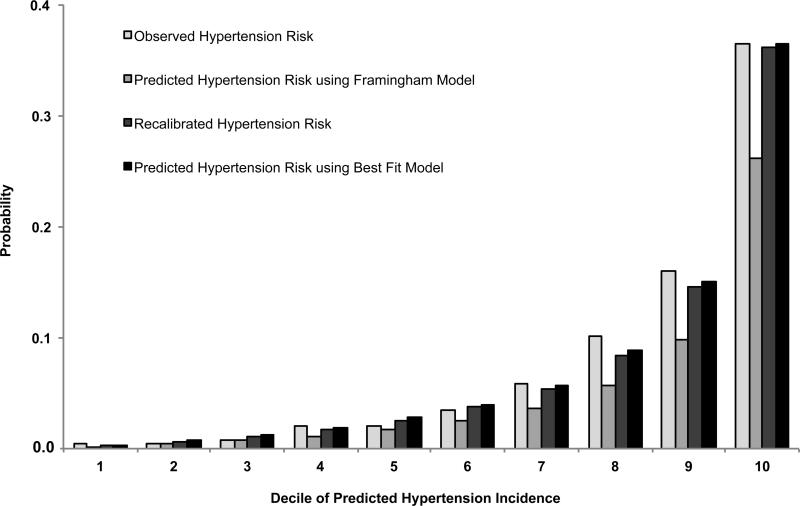
Within each decile of predicted hypertension risk, the FHS model underestimated the mean observed hypertension risk (χ2 = 249.4, p<0.001). Using the hypertension incidence from CARDIA to recalibrate the model, a good model fit was obtained (χ2 = 14.6, p=0.067) which was comparable to the best fit model (χ2 = 12.9, p=0.116) (Figure 1).
Figure 1.
Observed, predicted, recalibrated, and best fit mean hypertension risks by deciles of predicted risk obtained from the Framingham hypertension model. Observed represents actual hypertension incidence in the CARDIA Study. Predicted represents hypertension incidence obtained from the original Framingham model. Recalibrated represents mean hypertension incidence obtained using the actual hypertension incidence from the CARDIA Study and Framingham model coefficients. Best fit represents mean hypertension incidence obtained using the variables in the Framingham model but allowing coefficients to vary.
DISCUSSION
In this cohort study of young adults, the FHS model provided very good discrimination for identifying those who did and did not develop incident hypertension during 5 year follow-up periods and performed better than prehypertension. The prehypertension classification is meant to be used to identify individuals at high risk for hypertension,7 but the current results suggest the use of additional demographic and clinical parameters in the FHS model may better identify high-risk individuals. The FHS model systematically underestimated hypertension risk initially, but this was corrected by recalibrating the model using the hypertension incidence rates from our population.
Previous studies have reported that prehypertension alone may not be the most useful metric for discriminating between those who will and will not develop hypertension.12, 13 In the Multi-Ethnic Study of Atherosclerosis, a model with SBP alone performed better than a model with prehypertension alone and just as well as the FHS model.13 Also, a predicted risk >20% from the FHS hypertension risk score was a better predictor of incident hypertension compared with prehypertension alone in the Whitehall II study.12 Both of the previous studies evaluated middle-aged and older adults, while the current study assessed a cohort of young adults just upon entry into middle-age and also found that the FHS model was a better predictor of incident hypertension than prehypertension. It is important to identify predictors of hypertension among young adults because 78.8% of young adults have ideal blood pressure levels,21 thus highlighting the importance of promoting and sustaining ideal blood pressure levels in this age demographic for the prevention of hypertension later in life.
Individuals with prehypertension are more likely to have elevated levels of cardiovascular risk factors,22 but the prehypertension classification alone does not take into account these risk factors. Prehypertension is a simple classification that has been advocated for use clinically, but it is infrequently conveyed to patients23 and may not be the best risk stratification tool with 28% of adults meeting prehypertension criteria.1 It has been reported that individuals in the upper range of prehypertension (i.e., SBP of 130-139 mmHg and/or DBP of 85-89 mmHg) have an increased risk of hypertension compared with individuals in the lower range of prehypertension (i.e., SBP of 120-129 mmHg and/or DBP of 80-84 mmHg).8-10 However, when the predictive ability of the upper range of the prehypertension classification was evaluated in this study, the discrimination for incident hypertension was poorer than the overall prehypertension classification and the FHS model. Given the unsettled issue regarding whether pharmacologic therapy should be prescribed for individuals who meet prehypertension criteria,24, 25 the findings from the current study suggest better characterization of individuals at risk for hypertension based on the assessment of multiple factors is needed to develop appropriate prevention and treatment strategies.
DBP increases during young adulthood but decreases after middle-age26 and DBP is more strongly associated with an increased risk of coronary heart disease than SBP at younger ages.27 This suggests that DBP may play a key role in hypertension risk prediction among young adults. DBP and the age and DBP models demonstrated very good discrimination in the current study compared with the other individual components and were comparable to the overall FHS model for predicting incident hypertension.
In our community-based study of young adults transitioning into middle-age, the predicted hypertension risk estimates obtained from the FHS model overestimated the observed hypertension risk. Applying the FHS model to external populations is likely to result in a systematic overestimation or underestimation of predicted hypertension risk for a particular population when differences in incidence rates and mean levels of risk factors occur. The overestimation observed in our study was corrected after recalibrating the model for our population, but these observed differences highlight the importance of properly adjusting prediction models for use in external populations to prevent an overestimation or underestimation of risk.
This study has several potential limitations. The FHS model used parental medical records and clinic assessments to obtain a validated measure of parental history of hypertension while only self-reported parental history of hypertension was available in the current study. A previous study indicated that children's self-reported parental history of hypertension had a high positive predictive value but a low negative predictive value,28 suggesting that more participants may classify their parents as normotensive when their parents were actually hypertensive. However, self-reported measures of parental history of hypertension are the most feasible if the FHS model is used in clinical settings and self-reported parental history of medical conditions is routinely collected at clinic visits. Additionally, parental history of hypertension was assessed at baseline and years 5 and 10 so this variable could not be updated for each time interval evaluated. While we used appropriate sized cuffs, calibrated instruments, and standardized protocols to assess blood pressure, these measures may not be universally implemented in clinical settings. This could affect the accuracy and validity of blood pressures obtained for use in hypertension risk prediction models. Lastly, hypertension status was determined based on mean blood pressure at a single clinic visit. JNC 7 guidelines recommend using blood pressure from 2 or more clinic visits,7 but this was not available in the current study.
PERSPECTIVES
While the prehypertension classification is simple to use for identifying young adults with an increased risk of hypertension, it did not discriminate as well in this study when compared with the FHS model that contains demographic and clinical predictors that are routinely collected in clinical practice. The FHS model was able to identify those who did and did not develop hypertension, but the prediction model had to be recalibrated to obtain better fitting risk estimates for this population. Risk prediction models that go beyond the prehypertension classification may be used to better identify young adults with an increased risk of hypertension who may benefit from the adoption of preventive measures early in life. The ability to identify young adults at high risk for hypertension will provide the opportunity to efficiently apply risk reduction interventions in addition to population-based approaches for the prevention of hypertension.
Novelty and Significance.
What is New?
■ Prehypertension alone did not perform as well as the Framingham hypertension model for identifying individuals who developed incident hypertension over a 5-year period. The Framingham hypertension model includes standard demographic and clinical parameters and was able to better characterize young adults entering into middle age who had a higher risk of hypertension.
What is Relevant?
■ The prevalence and incidence of hypertension increases with age, so the maintenance of ideal blood pressure levels early in life is important for the prevention of hypertension. The ability to identify individuals with a higher risk of hypertension who may benefit from population-based and targeted prevention efforts is needed.
Summary
■ The prehypertension classification was developed to identify individuals at high risk for hypertension, but the current results suggest the use of additional demographic and clinical parameters is better for risk stratification. The Framingham hypertension model may be used to better identify high-risk individuals among young adults entering into middle age, with the understanding that model adjustments may be needed when the Framingham hypertension model is applied to other populations.
Acknowledgments
SOURCES OF FUNDING
This research was supported by contracts N01-HC-48047 through N01-HC-48050 and N01-HC-95095 from the National Heart, Lung, and Blood Institute.
Footnotes
CONFLICT OF INTEREST/DISCLOSURE STATEMENT
None.
REFERENCES
- 1.Ostchega Y, Yoon SS, Hughes J, Louis T. Hypertension awareness, treatment, and control--continued disparities in adults: United States, 2005-2006. NCHS Data Brief. 2008:1–8. [PubMed] [Google Scholar]
- 2.Carson AP, Howard G, Burke GL, Shea S, Levitan EB, Muntner P. Ethnic differences in hypertension incidence among middle-aged and older adults: The Multi-Ethnic Study of Atherosclerosis. Hypertension. 2011;57:1101–1107. doi: 10.1161/HYPERTENSIONAHA.110.168005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vasan RS, Beiser A, Seshadri S, Larson MG, Kannel WB, D'Agostino RB, Levy D. Residual lifetime risk for developing hypertension in middle-aged women and men. JAMA. 2002;287:1003–1010. doi: 10.1001/jama.287.8.1003. [DOI] [PubMed] [Google Scholar]
- 4.Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension: A scientific statement from the American Heart Association. Hypertension. 2006;47:296–308. doi: 10.1161/01.HYP.0000202568.01167.B6. [DOI] [PubMed] [Google Scholar]
- 5.Julius S, Nesbitt SD, Egan BM, Weber MA, Michelson EL, Kaciroti N, Black HR, Grimm RH, Jr., Messerli FH, Oparil S, Schork MA. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med. 2006;354:1685–1697. doi: 10.1056/NEJMoa060838. [DOI] [PubMed] [Google Scholar]
- 6.Luders S, Schrader J, Berger J, Unger T, Zidek W, Bohm M, Middeke M, Motz W, Lubcke C, Gansz A, Brokamp L, Schmieder RE, Trenkwalder P, Haller H, Dominiak P. The PHARAO study: Prevention of hypertension with the angiotensin-converting enzyme inhibitor ramipril in patients with high-normal blood pressure: A prospective, randomized, controlled prevention trial of the German hypertension league. J Hypertens. 2008;26:1487–1496. doi: 10.1097/HJH.0b013e3282ff8864. [DOI] [PubMed] [Google Scholar]
- 7.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., Jones DW, Materson BJ, Oparil S, Wright JT, Jr., Roccella EJ. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 8.Jimenez-Corona A, Lopez-Ridaura R, Stern MP, Gonzalez-Villalpando C. Risk of progression to hypertension in a low-income Mexican population with prehypertension and normal blood pressure. Am J Hypertens. 2007;20:929–936. doi: 10.1016/j.amjhyper.2007.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: A cohort study. Lancet. 2001;358:1682–1686. doi: 10.1016/S0140-6736(01)06710-1. [DOI] [PubMed] [Google Scholar]
- 10.Winegarden CR. From “prehypertension” to hypertension? Additional evidence. Ann Epidemiol. 2005;15:720–725. doi: 10.1016/j.annepidem.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 11.Parikh NI, Pencina MJ, Wang TJ, Benjamin EJ, Lanier KJ, Levy D, D'Agostino RB, Sr., Kannel WB, Vasan RS. A risk score for predicting near-term incidence of hypertension: The Framingham Heart Study. Ann Intern Med. 2008;148:102–110. doi: 10.7326/0003-4819-148-2-200801150-00005. [DOI] [PubMed] [Google Scholar]
- 12.Kivimaki M, Batty GD, Singh-Manoux A, Ferrie JE, Tabak AG, Jokela M, Marmot MG, Smith GD, Shipley MJ. Validating the Framingham hypertension risk score: Results from the Whitehall II Study. Hypertension. 2009;54:496–501. doi: 10.1161/HYPERTENSIONAHA.109.132373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muntner P, Woodward M, Mann DM, Shimbo D, Michos ED, Blumenthal RS, Carson AP, Chen H, Arnett DK. Comparison of the Framingham Heart Study hypertension model with blood pressure alone in the prediction of risk of hypertension: The Multi-Ethnic Study of Atherosclerosis. Hypertension. 2010;55:1339–1345. doi: 10.1161/HYPERTENSIONAHA.109.149609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR, Jr, Liu K, Savage PJ. CARDIA: Study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 15.National Heart Lung and Blood Institute [April 2, 2013];Coronary Artery Risk Development in Young Adults (CARDIA) study manuals of operation. 1985 Available at: http://www.cardia.dopm.uab.edu/exam-materials2/manual-of-operations.
- 16.Hozawa A, Jacobs DRJ, Steffes MW, Gross MD, Steffen LM, Lee D-H. Circulating carotenoid concentrations and incident hypertension: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. J Hypertens. 2009;27:237–242. doi: 10.1097/HJH.0b013e32832258c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allison PD. Survival analysis using SAS: A practical guide. SAS Publishing; Cary, NC: 2010. [Google Scholar]
- 18.Collett D. Modelling survival data in medical research. Chapman & Hall; London, UK: 1994. [Google Scholar]
- 19.Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S. A comparison of goodness-of-fit tests for the logistic regression model. Stat Med. 1997;16:965–980. doi: 10.1002/(sici)1097-0258(19970515)16:9<965::aid-sim509>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 20.D'Agostino RB, Sr., Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: Results of a multiple ethnic groups investigation. JAMA. 2001;286:180–187. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 21.Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, Daviglus ML, Lloyd-Jones DM. Status of cardiovascular health in US adults. Circulation. 2012;125:45–56. doi: 10.1161/CIRCULATIONAHA.111.035733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Greenlund KJ, Croft JB, Mensah GA. Prevalence of heart disease and stroke risk factors in persons with prehypertension in the United States, 1999-2000. Arch Intern Med. 2004;164:2113–2118. doi: 10.1001/archinte.164.19.2113. [DOI] [PubMed] [Google Scholar]
- 23.Viera AJ, Bangura F, Mitchell CM, Cerna A, Sloane P. Do clinicians tell patients they have prehypertension? J Am Board Fam Med. 2011;24:117–118. doi: 10.3122/jabfm.2011.01.100206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chobanian AV. Prehypertension revisited. Hypertension. 2006;48:812–814. doi: 10.1161/01.HYP.0000241684.29799.14. [DOI] [PubMed] [Google Scholar]
- 25.Egan B, Julius S. Prehypertension: Risk stratification and management considerations. Curr Hypertens Rep. 2008;10:359–366. doi: 10.1007/s11906-008-0068-0. [DOI] [PubMed] [Google Scholar]
- 26.Franklin SS, Gustin W, Wong ND, Larson MG, Weber MA, Kannel WB, Levy D. Hemodynamic patterns of age-related changes in blood pressure : The Framingham Heart Study. Circulation. 1997;96:308–315. doi: 10.1161/01.cir.96.1.308. [DOI] [PubMed] [Google Scholar]
- 27.Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, Levy D. Does the relation of blood pressure to coronary heart disease risk change with aging? : The Framingham Heart Study. Circulation. 2001;103:1245–1249. doi: 10.1161/01.cir.103.9.1245. [DOI] [PubMed] [Google Scholar]
- 28.Murabito JM, Nam B-H, D'Agostino RB, Lloyd-Jones DM, O'Donnell CJ, Wilson PWF. Accuracy of offspring reports of parental cardiovascular disease history: The Framingham Offspring Study. Ann Intern Med. 2004;140:434–440. doi: 10.7326/0003-4819-140-6-200403160-00010. [DOI] [PubMed] [Google Scholar]