Abstract
BACKGROUND CONTEXT
Postoperative malalignment of the cervical spine may alter cervical spine mechanics, and put patients at risk for clinical adjacent segment pathology requiring surgery.
PURPOSE
To investigate whether a relationship exists between cervical spine sagittal alignment and clinical adjacent segment pathology requiring surgery (CASP-S) following anterior cervical fusion (ACF).
STUDY DESIGN
Retrospective matched study.
PATIENT SAMPLE
One hundred twenty two patients undergoing ACF from 1996 to 2008 were identified, with a minimum of 2 year follow-up.
OUTCOME MEASURES
Radiographs were reviewed to measure the sagittal alignment using C2 and C7 sagittal plumb lines, distance from the fusion mass plumb line to the C2 and C7 plumb lines, the alignment of the fusion mass, caudally adjacent disc angle, the sagittal slope angle of the superior endplate of the vertebra caudally adjacent to the fusion mass, T1 sagittal angle, overall cervical sagittal alignment, and curve patterns by Katsuura classification.
METHODS
One hundred twenty two patients undergoing ACF from 1996 to 2008 were identified, with a minimum of 1 year follow-up. Patients were divided into groups according to the development of CASP requiring surgery (Control / CASP-S) and by number/location of levels fused. Radiographs were reviewed to measure the sagittal alignment using C2 and C7 sagittal plumb lines, distance from the fusion mass plumb line to the C2 and C7 plumb lines, the alignment of the fusion mass, caudally adjacent disc angle, the sagittal slope angle of the superior endplate of the vertebra caudally adjacent to the fusion mass, T1 sagittal angle, overall cervical sagittal alignment, and curve patterns by Katsuura classification. Appropriate statistical tests were performed to calculate relationships between the variables and the development of CASP-S. No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
RESULTS
The groups were similar with regard to demographic and surgical variables. Lordosis was preserved in 82% (50/61) of the control group but in only 66% (40/61) of the CASP-S group (p = 0.033). More patients with a straight curve pattern developed CASP-S. The distance from the C2 to the C7 plumb line and T1 sagittal slope angle were lower in the CASP-S group with C5/6 fusions compared to control group. Also, the distance from C5/6 fusion mass to C7 plumb line and C7 sagittal slope angle were lower in the CASP-S group with C5/6 fusions.
CONCLUSIONS
Our results suggest that malalignment of the cervical spine following an ACF at C5/6 has an effect on the development of clinical adjacent segment pathology requiring surgery.
Keywords: Plumb line, Clinical adjacent segment pathology, Anterior cervical fusion
Introduction
Clinical adjacent segment pathology may affect more than one-fourth of all patients within ten years after an anterior cervical arthrodesis [1, 2]. The risk factors for clinical adjacent segment pathology include preexisting degeneration at the adjacent levels [1], previous cervical fusion [1] and sagittal cervical malalignment [3, 4]. Malalignment of the cervical spine in the sagittal plane has been shown to increase adjacent segment disc pressures in cadaver models [5].
The sagittal alignment measured by C2–C7 Cobb’s angle does not describe where C2 lies, relative to C7 [6]. The position of C2, relative to C7, in the sagittal plane is closely maintained [6–8]. The cervical plumb lines from the C2 in the long-standing radiographs were distributed in a narrow range (16.1 ± 11.6 mm) anterior to the center of C7 in a study with all 52 adult patients visiting for lumbar spine problem [6] and in a range (16.8 ± 11.2 mm) in a study with 100 asymptomatic volunteers [7]. The distance between cervical sagittal plumb lines from C2 and C7 may be another important element for cervical sagittal alignment. However, to our knowledge there is no report about the relationship between the cervical sagittal alignment measured by the cervical sagittal plumb lines and clinical adjacent segment pathology in anterior cervical arthrodesis. The purpose of this study is to determine whether postoperative cervical sagittal alignment measured by the cervical sagittal plumb lines from C2 and C7 can be related to clinical adjacent segment pathology requiring surgery following anterior cervical arthrodesis.
Materials and Methods
Institutional review board approved this study. The surgical records of the senior author were queried, to identify adult patients undergoing anterior cervical discectomy or corpectomy and fusion between 1996 and 2008. Those patients undergoing surgery for non-degenerative disease (trauma, infection, tumor, deformity, inflammation) were excluded.
Clinical adjacent segment pathology is defined as degeneration at a segment adjacent to a fusion, causing symptoms. The cohort identified was divided into patients undergoing clinical adjacent segment pathology surgery (CASP-S) and those who did not (Control). The CASP-S group was composed of patients who underwent secondary adjacent segment surgery because of symptoms concordant with adjacent segment pathology. Demographic data included age at surgery, gender, comorbidities including diabetes mellitus, smoking history, Body Mass Index (BMI), and diagnosis. Follow-up was defined as the period after surgery in the control group, and the time from index surgery to reoperation in the CASP-S group.
Surgical data collected included levels of surgery, number of fusion levels and type of bone graft (autograft vs. allograft).
Radiographs at the final follow-up or before an additional surgery were assessed in each group to determine the distance between the C2 and the C7 sagittal plumb lines, distance from the plumb line of the fusion mass to C2 and C7 plumb lines, the sagittal slope angle of the superior endplate of the vertebra caudally adjacent to the fusion mass, T1 sagittal angle, caudally adjacent disc angle, alignment of the fusion mass, overall cervical sagittal alignment, and curve patterns, including kyphotic, straight, lordotic, sigmoid.
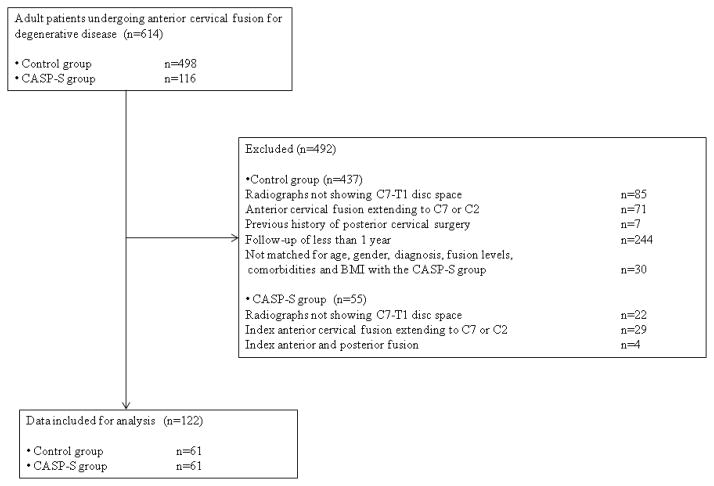
Routine lateral radiographs were obtained using standard techniques. The patient stands upright, his head facing forward. The X-ray tube is positioned 72 inches from the patient. The C2 sagittal plumb line was drawn with a lateral gravity plumb line from the center of C2 (Figure 1). The center of C2 was noted by the intersection of crossing diagonals of vertebral body of C2 on the lateral radiograph. The C7 sagittal plumb line was drawn with a lateral gravity plumb line from the center of C7 (Figure 1). The plumb line of fusion mass was drawn with a lateral gravity plumb line from the center of fusion mass (Figure 1). The center of C7 or fusion mass was noted by the intersection of crossing diagonals on the lateral radiograph. The distance between the plumb lines was measured as the shortest perpendicular distance between the two lines (Figure 1). The caudally adjacent disc angle was measured as the angle between the caudal and cranial endplates of the disc just caudal to the fusion mass (Figure 2). The sagittal slope angle of the superior endplate of the vertebra caudally adjacent to the fusion mass was measured as the angle between a horizontal line and the cranial endplate of the vertebra caudally adjacent to the fusion mass (Figure 2). T1 sagittal angle was measured as the angle between a horizontal line and the cranial endplate of T1 (Figure 2). The alignment of the fusion mass was measured as the Cobb angle between cranial and caudal endplates of the fusion mass (Figure 3). The overall cervical sagittal alignment was measured as the Cobb angle between cranial endplate of C2 and caudal endplates of C7 (Figure 3).
Figure 1.

Radiographs were assessed for the distance from C2 to C7 sagittal plumb line (C–A), distance from the plumb line of the fusion mass to each plumb line (C–B or B–A).
Figure 2.
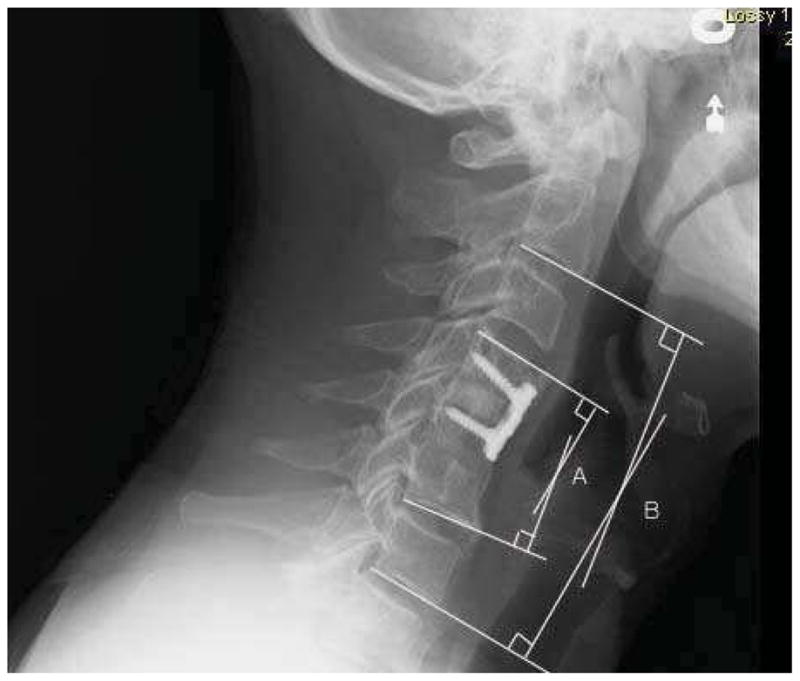
Radiographs were assessed for caudally adjacent disc angle (A), sagittal slope angle of superior endplate of vertebrae caudally adjacent to fusion mass (B) and T1 sagittal slope angle (C).
Figure 3.
Radiographs were assessed for alignment of the fusion mass (Cobb’s angle between cranial and caudal endplates of fusion mass, A) and overall cervical sagittal alignment (C2–C7 Cobb’s angle, B).
The curve pattern of the cervical spine was classified by Katsuura [3] as lordotic, straight, kyphotic or sigmoid based on the shape and the angle formed by tangent lines to the posterior cortex of C2 and C7.
Comparisons of categorical variables were made using Fisher’s exact tests. Comparisons of continuous and ordinal variables were made using t-test or Wilcoxon-Mann-Whitney test due to the non-normal distribution. Tests were two-tailed and p < 0.05 was considered significant. Logistic regression was used to estimate odds ratios (OR) and 95% confidence intervals (CI) for variables with significant associations with clinical adjacent segment pathology requiring surgery. The area under ROC curve (AUC) is the concordant index (c-index), which was used to identify which radiographic measurements could be most effective at predicting clinical adjacent segment pathology requiring surgery. Cox regression analysis was also used to estimate variables with significant associations with clinical adjacent segment pathology requiring surgery. SAS version 9.2 (SAS Institute, Cary, NC) was used for analysis.
Results
614 Patients were identified as having undergone anterior cervical fusion for degenerative disease (Figure 4). For the CASP-S group 116 patients were identified. For the control group 498 patients were identified. We removed the patients in the CASP-S group who had radiographic studies which did not show the C7-T1 disc space, those with the index anterior cervical fusion extending to C7 or C2, or those with index anterior and posterior fusion. In the control group, we excluded patients who had radiographic studies which did not show C7-T1, anterior cervical fusion to C7 or C2, previous history of posterior cervical surgery or a follow-up of less than 1 year. In addition, we excluded those that did not match for age, gender, diagnosis, the fusion level, comorbidities and BMI with the CASP-S group. This left sixty-one patients who underwent further surgery for clinical adjacent segment pathology and 61 control patients. The control group has three subgroups: one level fusion (C4/5=4, C5/6=28), two level fusion (C3/4/5=4, C4/5/6=20) and three level fusion (C3/4/5/6=5) (Table 1). The CASP-S group also has three subgroups: one level fusion (C4/5=6, C5/6=26), two level fusion (C3/4/5=4, C4/5/6=19) and three level fusion (C3/4/5/6=6) (Table 1).
Figure 4.
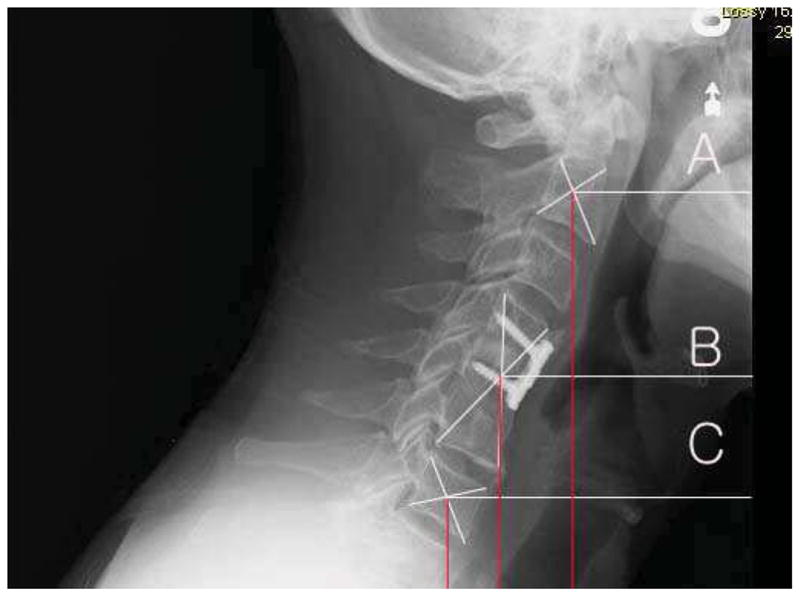
Inclusion-exclusion flow diagram
Table 1.
Composition of the Subgroups According to the Development of Clinical Adjacent Segment Pathology requiring Surgery and by Number and Location of Levels Fused
| Control group | CASP-S group | |||||||
|---|---|---|---|---|---|---|---|---|
| Fusion level | One | C4/5 | 4 | 32 | 61 | 6 | 32 | 61 |
|
|
|
|||||||
| C5/6 | 28 | 26 | ||||||
|
|
|
|||||||
| Two | C3/4/5 | 4 | 24 | 4 | 23 | |||
|
|
|
|||||||
| C4/5/6 | 20 | 19 | ||||||
|
|
|
|||||||
| Three | C3/4/5/6 | 5 | 6 | |||||
The mean age at surgery, gender, diagnosis for surgery, comorbidities including diabetes mellitus, smoking history, BMI, type of bone graft, and follow-up period were similar (Table 2).
Table 2.
Demographic and Surgical Data between Control and CASP-S Group
| Control group (n=61) | CASP-S group (n=61) | |||
|---|---|---|---|---|
| Age | 49.4 ± 11.1 | 49.2 ± 9.8 | p=0.911 | |
| Sex | M : F | 28 : 33 | 20 : 41 | p=0.352 |
| Diagnosis | Myelopathy | 2 | 2 | p=1.000 |
| Myeloradiculopathy | 11 | 11 | ||
| Radiculopathy | 48 | 48 | ||
| Diabetes mellitus | 4 | 1 | p=0.365 | |
| Smoking | 18 | 23 | p=0.251 | |
| BMI | 27.6 ± 4.3 | 27.5 ± 5.4 | p=0.920 | |
| Bone graft | Allograft | 56 | 50 | p=0.179 |
| Autograft | 5 | 10 | ||
| Follow-up period (months) | 44.0 ± 24.2 (12–110) | 53.3 ± 36.4 (9–156) | p=0.350* | |
Note : t-test was used due to the normal distribution.
Wilcoxon-Mann-Whitney test was used if variables are not normal distributed.
The curve pattern by Katsuura’s classification was lordotic in 90 cases, straight in 28 cases, sigmoid in 3 cases and kyphotic in 1 case (Table 3). Physiologic lordosis was preserved in 82% (50/61) of the control group, but in only 66% (40/61) of the CASP-S group (p=0.033, Fisher’s exact test). There were more patients with a straight curve pattern in the CASP-S group.
Table 3.
Association of Classifications by Katsuura with Clinical Adjacent Segment Pathology requiring Surgery
| Control group (n=61) | CASP-S group (n=61) | |||
|---|---|---|---|---|
| Classification by Katsuura | Kyphosis (n=1) | 1 (1.6%) | 0 | p=0.033 |
| Lordosis (n=90) | 50 (82.0%) | 40 (65.6%) | ||
| Sigmoidosis (n=3) | 0 | 3 (4.9%) | ||
| Straight (n=28) | 10 (16.4%) | 18 (29.5%) | ||
Note: Fisher’s exact test was used.
The following radiographic findings did not differ significantly between the two groups with one, two and three level fusions: the distance from C2 to C7 sagittal plumb lines, distance from the fusion mass to each plumb line, the sagittal slope angle of the superior endplate of the vertebrae distally adjacent to the fusion mass, the T1 sagittal slope angle, caudally adjacent disc angle, alignment of the fusion mass, overall cervical sagittal alignment (Table 4). Also, if we compare the CASP-S subgroup of the 32 patients who underwent fusion at one level versus the control subgroup, the only significant difference was the distance from C2 to C7 sagittal plumb line (Table 4).
Table 4.
Comparisons of Radiographs Measurements Between Control and CASP-S Group
| Control group / CASP-S group | ||||||
|---|---|---|---|---|---|---|
| One, two, three level (n=61) Median (interquartile) |
One level subgroup (n=32) Median (interquartile) |
C5/6 fusion sub-subgroup (n=28) Median (interquartile) |
||||
| Distance from fusion mass to C2 plumb line | 10(5–14) / 7(3–13) | p=0.233* | 10(6.5–14.5) / 7.5(3–13) | p=0.092* | 11(8–16) / 8.5(5–14) | p=0.086* |
| Distance from fusion mass to C7 plumb line | 11(8–15) / 9(6–13) | p=0.095* | 11(8–14) / 9(6–11) | p=0.053* | 11(7–13) / 8(6–9) | p=0.021* |
| Distance from C2 to C7 sagittal plumb line | 20(16–28) / 17(10–27) | p=0.117* | 20(18–27) / 17(10–23) | p=0.044* | 20(18–28) / 17(11–22) | p=0.032* |
| Sagittal slope angle of superior endplate of vertebrae caudally adjacent to fusion mass | 28(24–34) / 26(21–32) | p=0.112 | 28(24–34) / 24(21–32) | p=0.058 | 29(24–34) / 24(21–31) | p=0.034 |
| T1 sagittal slope angle | 30(26–35) / 28(23–33) | p=0.100 | 30(26–34) / 26(22–33) | p=0.075 | 30(27–34) / 25(22–33) | p=0.049 |
| Caudally adjacent disc angle | −4(−6, −1) / −3(−7, −1) | p=0.496* | −4(−6, −2) / −3(−8, −1) | p=0.808* | −4(−5, −2) / −3(−7, −1) | p=0.664* |
| Alignment of the fusion mass | −1(−6,1) / 0(−8,5) | p=0.564 | 0(−3,3) / 0(−7,7) | p=0.808 | 0(−2,4) / 0(−5,8) | p=0.856 |
| Overall cervical sagittal alignment | 22(−28, −13) / −18(−24, −9) | p=0.101 | −21(−25, −10) / −15(−23, −7) | p=0.424 | −21(−25, −10) / −14(−22, −5) | p=0.328 |
Note : t-test was used due to the normal distribution.
Wilcoxon-Mann-Whitney test was used if variables are not normal distributed.
If we compare the CASP-S sub-subgroup of the 28 patients who underwent fusion at the C5/6 level versus the control sub-subgroup, there was a significant difference between the control and CASP sub-subgroups for the following: the distance from C2 to C7 sagittal plumb lines, distance from the fusion mass to the C7 plumb line, the sagittal slope angle of the superior endplate of the vertebra distally adjacent to the fusion mass (C7 sagittal slope angle) and T1 sagittal slope angle (Table 4). The distance from C2 to C7 sagittal plumb line and from the fusion mass to the C7 plumb line decreased in the CASP-S sub-subgroup with C5/6 level fusion compared to the control sub-subgroup with C5/6 level fusion. Also, C7 sagittal slope angle and T1 sagittal slope angle decreased in the CASP-S sub-subgroup with C5/6 level fusion compared to the control sub-subgroup with C5/6 level fusion.
The distance from the fusion mass to the C7 plumb line and the C7 sagittal slope angle were found to be potential risk factors for predicting clinical adjacent segment pathology requiring surgery using logistic regression analysis for the patients with the C5/6 disc level fused (Table 5). The distance from the fusion mass to the C7 plumb line was found to be a potential risk factor for predicting clinical adjacent segment pathology requiring surgery using Cox regression analysis for the patients with the C5/6 disc level fused (Table 6).
Table 5.
Univariate Risk Factors for Predicting Clinical Adjacent Segment Pathology requiring Surgery in Patients with C5/6 Level Fusion (n=54)
| Risk Factor | OR (95% CI) unit=5 | p value | c-index |
|---|---|---|---|
| Distance from fusion mass to C2 plumb line | 1.312 (0.894, 1.925) | 0.166 | 0.637 |
| Distance from fusion mass to C7 plumb line | 2.463 (1.143, 5.304) | 0.021 | 0.683 |
| Distance from C2 to C7 sagittal plumb line | 1.345 (0.993, 1.821) | 0.055 | 0.670 |
| C7 sagittal slope angle | 1.481 (1.016, 2.157) | 0.041 | 0.669 |
| T1 sagittal slope angle | 1.469 (0.993, 2.173) | 0.055 | 0.661 |
| Caudally adjacent disc angle | 0.901 (0.433, 1.875) | 0.781 | 0.535 |
| Alignment of the fusion mass | 0.963(0.649, 1.428) | 0.850 | 0.519 |
| Overall cervical sagittal alignment | 0.884 (0.692, 1.129) | 0.322 | 0.587 |
| Straight vs. Lordosis | 2.190 (0.657, 7.285) | 0.202 | 0.581 |
Note: c-index, usually 0.90–1 = excellent, 0.80–0.90 = good, 0.70–0.80 = fair, 0.60–0.70 = poor, 0.50–0.60 = fail
Table 6.
Cox regression analysis for Predicting Clinical Adjacent Segment Pathology requiring Surgery in Patients with C5/6 Level Fusion (n=54)
| Risk Factor | Hazard ratio (95% CI) | p value |
|---|---|---|
| Distance from fusion mass to C7 plumb line | 0.828 (0.714, 0.959) | 0.012 |
Discussion
The prevalence of clinical adjacent segment pathology requiring surgery after anterior cervical decompression and arthrodesis has been reported to be 9% at five years [1], 12% at six years [9] and 19.2 % at ten years [1]. The incidence of surgery for clinical adjacent segment pathology has been reported to be between 1.5% and 4% annually following anterior cervical arthrodeses [1, 10]. Several risk factors for the development of clinical adjacent segment pathology have been reported, including cervical malalignment [3, 4]. The standing sagittal plumb lines from C2 and C7 are closely maintained in a tight range of variation in the normal cervical spine [6–8]. Therefore, if the usually close distance between these sagittal plumb lines is perturbed by surgical intervention, one could theorize that the altered cervical sagittal alignment might result in increased risk for adjacent segment pathology. However, to our knowledge there is no report examining this topic. We therefore determined whether postoperative cervical sagittal alignment, measured by the sagittal plumb lines from C2 and C7 may be associated with clinical adjacent segment pathology requiring surgery following anterior cervical arthrodesis.
We measured the distance between C2 and C7 plumb lines in the sagittal plane. This gives an alternative method for assessing overall cervical alignment. For instance, two patients can have the same degree of cervical lordosis but if one of them has severe thoracic kyphosis such that their head projects well in front of their sternum, that patient will have a larger distance between the two plumb lines than one who has normal thoracic alignment. Kuntz et al. [8] reviewed 12 articles regarding sagittal alignment in asymptomatic adults. They found that the C2-S1 sagittal vertical axis and C7-S1 sagittal vertical axis were maintained in a narrow range for alignment of the spine over the pelvis and femoral heads [8]. The cervical plumb lines from C2 in the long-standing radiographs were distributed in a narrow range (16.1 ± 11.6 mm) anterior to the center of C7 in 52 adult patients presenting with lumbar spine problems [6]. The range was equally narrow (16.8 ± 11.2 mm) in a study with 100 asymptomatic volunteers [7]. Such plumb lines have been shown to be useful in predicting adjacent level degeneration following lumbar fusion. A lower incidence of adjacent-level change was demonstrated in patients with a normal C7 plumb line alignment following lumbar spinal fusion [11]. We felt that a similar finding might be found in the cervical spine by assessing sagittal balance with C2 and C7 plumb lines. However, to our knowledge, no investigator had ever utilized C2 and C7 plumb lines to assess the adverse effect of cervical malalignment on clinical adjacent segment pathology.
Our study showed that the distance from the C2 to C7 sagittal plumb lines and the distance from the fusion mass to the C7 plumb line was significantly less in the patients fused at C5/6 with clinical adjacent segment pathology requiring surgery compared to the patients fused at C5/6 without clinical adjacent segment pathology requiring surgery. Also, in the patients fused at the C5/6 level, the C7 and T1 sagittal slope angles were lower (i.e., the endplate was more horizontal) for those with clinical adjacent segment pathology requiring surgery compared with those without. The T1 sagittal slope angle is related to the distance from C2 to C7 sagittal plumb lines. The T1 sagittal angle correlated with a positive sagittal balance of the C2 plumb line in asymptomatic volunteers [6]. A 10cm positive sagittal balance of the C2 plumb line (C2 line 10cm in front of C7) was associated with greater than 25 degrees of T1 sagittal angle and negative sagittal balance of the C2 plumb line is seen in patients with less than 13 degree of T1 sagittal angle [6]. In addition, the distance from the fusion mass to the C7 plumb line and the C7 sagittal slope angle were found to be potential risk factors for predicting clinical adjacent segment pathology requiring surgery in the patients with C5/6 fusions. In contrast to our results using plumb lines and sagittal slope angles, our study showed that clinical adjacent segment pathology requiring surgery had no relationship with the alignment of the fused segment or the overall cervical sagittal alignment. Faldini et al. [4] found that malalignment after cervical arthrodesis promotes degenerative changes at levels adjacent to the fused segment (radiographical adjacent segment pathology). They retrospectively studied 107 patients with one-level anterior cervical discectomy and fusion [4]. The degree of adjacent-level degeneration was assessed using the formation of osteophytes, periarticular ossicles, cartilage narrowing with subchondral bone sclerosis, pseudocystic areas and altered bone shape on the X-ray as evidence of degeneration [12]. Adjacent segment degeneration was found in 27% of cases fused in lordosis and 60% of cases with fused in kyphosis [4]. But, they found no relationship between the overall cervical spine alignment and adjacent segment degeneration [4].
Katsuura et al. [3] evaluated forty-two patients who underwent anterior cervical interbody fusion surgery with lateral standard radiographs of the cervical spine. They diagnosed radiographical adjacent segment pathology when radiographic findings were consistent with the patient’s symptoms and signs and when at least one of following criteria was met: (a) evident intervertebral disc space narrowing; (b) newly developed instability more than 3 mm on flexion and extension radiographs; (c) posterior vertebral spur formation [3]. They found that the alignment of the fusion mass and the overall cervical sagittal alignment in the postoperative radiographs were more kyphotic in the patients with the radiographic adjacent-level degeneration [3].
While both of the above studies showed that kyphosis was associated with radiographic degeneration at adjacent levels, they investigated radiographical adjacent segment pathology, not clinical adjacent segmental pathology requiring secondary surgery (CASP-S). Radiographic degeneration is not always related to clinical symptoms [13]. Therefore, we divided the cohort into two groups based upon the need for additional operation for adjacent segment pathology. Contrary to both of the previous studies which only looked at radiographic degeneration at the adjacent segment, our study shows that reoperation at the adjacent segment had no relationship with either the alignment of the fusion mass or the overall cervical sagittal alignment.
As with any study, the present investigation may have several potential problems. First, it is a retrospective study. Therefore, we did not have a protocol for standardizing all radiographs. Patients were asked to hold their neck in a neutral position. However, this may have been affected by neck pain. Secondly, we do not have radiographs before the primary operation. Since we were mainly interested in knowing the effect of postoperative cervical alignment on the incidence of CASP-S, pre-operative radiographs are non-contributory. Third, the major indication for the adjacent segment operation was pain, but other problems could be potential indications for adjacent segment operations. Fourth, the degree of radiographical adjacent segment pathology was not evaluated in the current study. We only checked the relationship between the postoperative cervical sagittal alignment and clinical adjacent segment pathology requiring surgery following anterior cervical arthrodesis. Our analysis allows for a better understanding of the relationship between alignment and clinical adjacent segment pathology requiring surgery. Fifth, some patients in the control group are highly likely to require surgery sometime in the future. Although our follow-up period was an average of 44 months for the control and 53 months for surgical groups, that may not have been long enough to detect the effect of follow-up on CASP. Finally, ours is an observational study which points out a correlation but cannot explain why such a correlation occurs. It is beyond the scope of a non-biomechanical study to elucidate the exact patho-mechanism by which such a correlation occurs.
Our results showed that the alignment of the post-operative cervical spine has an effect on the development of symptomatic adjacent level pathology requiring surgery. Further investigation may help to explain the mechanism by which such a correlation occurs.
Footnotes
The First and Corresponding author of a manuscript had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis as well as the decision to submit for publication
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81:519–28. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Riew KD, Norvell DC, Chapman JR, Skelly AC, Dettori JR. Introduction/Summary statement: adjacent segment pathology. Spine (Phila Pa 1976) 2012;37(22 Suppl):S1–7. doi: 10.1097/BRS.0b013e31826cef01. [DOI] [PubMed] [Google Scholar]
- 3.Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001;10:320–4. doi: 10.1007/s005860000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Faldini C, Pagkrati S, Leonetti D, Miscione MT, Giannini S. Sagittal Segmental Alignment as Predictor of Adjacent-Level Degeneration After a Cloward Procedure. Clin Orthop Relat Res. 2011;469:674–81. doi: 10.1007/s11999-010-1614-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park DH, Ramakrishnan P, Cho TH, et al. Effect of lower two-level anterior cervical fusion on the superior adjacent level. J Neurosurg Spine. 2007;7:336–40. doi: 10.3171/SPI-07/09/336. [DOI] [PubMed] [Google Scholar]
- 6.Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010;10:994–8. doi: 10.1016/j.spinee.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 7.Hardacker JW, Shuford RF, Capicotto PN, Pryor PW. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine (Phila Pa 1976) 1997;22:1472–80. doi: 10.1097/00007632-199707010-00009. discussion 80. [DOI] [PubMed] [Google Scholar]
- 8.Kuntz Ct, Levin LS, Ondra SL, Shaffrey CI, Morgan CJ. Neutral upright sagittal spinal alignment from the occiput to the pelvis in asymptomatic adults: a review and resynthesis of the literature. J Neurosurg Spine. 2007;6:104–12. doi: 10.3171/spi.2007.6.2.104. [DOI] [PubMed] [Google Scholar]
- 9.Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75:1298–307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004;4:190S–4S. doi: 10.1016/j.spinee.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 2001;10:314–9. doi: 10.1007/s005860000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Borenstein DG, O’Mara JW, Jr, Boden SD, et al. The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects : a seven-year follow-up study. J Bone Joint Surg Am. 2001;83:1306–11. doi: 10.2106/00004623-200109000-00002. [DOI] [PubMed] [Google Scholar]