Abstract
Radiofrequency inferior turbinate reduction (RFITR) of inferior turbinate hypertrophy (ITH) is an effective way to treat patients with intractable nasal mucosal obstruction. The objective of this study was to assess smell ability, nasal symptoms, inferior turbinate grading (ITG), peak nasal inspiratory flow (PNIF) of patients with chronic rhinitis (CR), and ITH before and after RFITR. Patients with CR and ITH, aged 18–60 years, who underwent RFITR, were prospectively recruited. Smell ability (measured by smell detection threshold [SDT]), visual analog scale (VAS) of nasal symptoms, ITG, and PNIF before and 6–10 weeks after RFITR were compared. Forty-eight subjects were included. All nasal symptoms were significantly decreased after RFITR. After surgery, SDT (tested by phenyl ethyl alcohol) was worsened in 7 patients (14.6%), improved in 8 patients (16.7%), and did not change in 33 patients (68.7%). SDT after RFITR of six patients in the worsened SDT group were still within normal range (> −6.5). There was only one patient whose SDT changed from normosmia to mild hyposmia (−7.25 to −5.38). In the improved SDT group, two of eight patients had obviously better SDT after RFITR, which changed from moderate hyposmia to normosmia (−3.65 to −10; −3.73 to −10), whereas six of eight patients had little better SDT after RFITR. RFITR also significantly reduced ITG and improved PNIF. In conclusion, the treatment of patients with CR and ITH with RFITR significantly improved PNIF, ITG, and nasal symptoms assessed by VAS, although SDT after RFITR could be the same or improved or worsened.
Keywords: Chronic rhinitis, inferior turbinate hypertrophy, peak nasal inspiratory flow, radiofrequency inferior turbinate reduction, smell detection threshold
Chronic rhinitis (CR) is a common chronic disease caused by inflammation of the nasal mucosa. The most common presenting symptom of CR is nasal obstruction from mucosal hypertrophy.1 Treatment of CR consists of irritant avoidance, pharmacotherapy, and surgical treatment such as radiofrequency inferior turbinate reduction (RFITR).2
Olfactory sensation is one of the most important sensory perceptions in humans because it detects dangerous substances (e.g., gas leak) and facilitates flavor and taste sensation.3 Smell dysfunction can worsen patients' quality of life and can lead to depression in some patients.4–7 Twenty-two percent of patients with CR were found to have smell dysfunction caused by obstruction of airflow to the olfactory cleft.8–10
Today, RFITR has been used popularly in the treatment of inferior turbinate hypertrophy (ITH). The principle is the use of radiofrequency, which was changed to heat, resulting in coagulation necrosis and volumetric tissue reduction.11 These leads to decreased nasal obstruction and improved sense of smell.
Banhiran and colleagues12 compared visual analog scale (VAS) of 28 patients with CR who failed medical treatment before and after RFITR. VAS of the sense of smell, severity, and frequency of nasal obstruction improved 50, 89.3, and 85.7%, respectively. Rhee and colleagues13 studied smell ability (measured by butanol threshold test) of 28 patients with nasal obstruction caused by ITH before and after RFITR. Fifty-six percent of patients with hyposmia improved in their smell ability after RFITR. In contrast, Black and colleagues14 found that there were no significant differences in smell ability of 20 patients with CR and ITH after RFITR.
Recently, Garzaro and colleagues15 studied smell ability of 40 patients with nasal obstruction caused by ITH before and after RFITR. Anosmia, hyposmia, and normosmia were observed in 2, 33, and 5 patients, respectively, before surgery in contrast with 1, 5, and 34 patients, respectively, after surgery. This prospective before and after study was aimed to assess smell ability, nasal symptoms, inferior turbinate grading (ITG), peak nasal inspiratory flow (PNIF) of patients with CR, and ITH after RFITR.
MATERIALS AND METHODS
Patients aged 18–60 years with persistent CR and ITH who underwent RFITR were recruited from October 2011 to November 2012 after approval from the Siriraj Institutional Review Board (Si 362/2010). To date, there is no universal consensus on the definition of CR. However, the consensus of rhinologists from seven medical schools in Thailand defines CR as the presence of nasal obstruction, rhinorrhea, sneezing, and itching for >1 month.16 The term “persistent” is defined by the presence of the aforementioned symptoms >4 days/wk for >4 weeks.17 All patients had grades II–III (Friedman grading system11) ITH and failed conservative treatment, which consisted of avoidance, environmental control, and medication (antihistamine, oral decongestants, intranasal corticosteroids, saline irrigation, or steam inhalation) for at least 4 weeks. Patients were excluded if they had history or physical examination that indicated other causes of nasal obstruction, e.g., nasal polyp, nasal tumor, and/or sensorineural olfactory disorder, e.g., post–head trauma, dementia, Alzheimer's disease, multiple sclerosis, or congenital disorders. Patients who underwent other sinonasal surgery or had abnormal sense of smell from upper airway infection, e.g., viral rhinitis or sinusitis, were also excluded. Informed consent was obtained before enrolling into the study.
Smell ability (measured by smell detection threshold [SDT]), VAS of nasal obstruction and sense of smell, ITG, and PNIF before and 6–10 weeks after RFITR were compared.
Subjective Evaluation of Nasal Symptoms
All patients were asked to fill in the questionnaires using standard VASs or VAS (0–10) to assess the severity of nasal symptoms including nasal obstruction, anterior nasal discharge, nasal itching, sneezing, and sense of smell before and after treatment with radiofrequency. We defined a score of 0 as no symptom and a score of 10 as maximal symptom severity.
Nasal Endoscopy
A 4-mm telescope (KARL STORZ GmbH & Co. KG, Tuttlingen, Germany) was used to detect any abnormalities in nasal cavity that could rule in or rule out patients according to inclusion and exclusion criteria, respectively.
Inferior Turbinate Grading
ITG was graded by anterior rhinoscopy and nasal endoscopy according to the Friedman grading system (Table 1).11
Table 1.
Friedman grading system of inferior turbinate hypertrophy
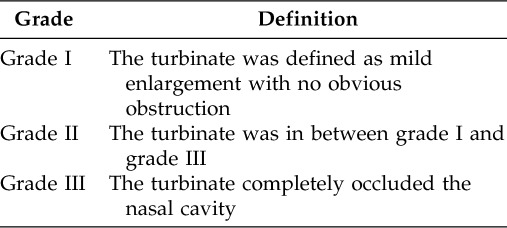
Source: Ref. 11.
Peak Nasal Inspiratory Flow
The severity of nasal obstruction was recorded by measuring the volume of nasal airflow (L/min) using the In-Check nasal peak flowmeter (Celki Thai Co., Ltd., Bangkok, Thailand). Patients were asked to exhale and then inhale through the nose three times and the maximum value among three values was chosen as the PNIF.
Phenyl Ethyl Alcohol (PEA) Test
Smell threshold was measured by asking the patients to sniff PEA (S.M. Chemical, Bangkok, Thailand), which had rose-like smell. The PEA was prepared in clear bottles in different concentrations to identify the lowest concentration that could be detected by the patients (SDT). The details of the test have been described previously.18 The SDT was then differentiated into normosmia, hyposmia, and anosmia as followed18:
SDT > −2 = anosmia
SDT −2 to −3.49 = severe hyposmia
SDT −3.5 to −4.49 = moderate hyposmia
SDT −4.5 to −6.49 = mild hyposmia
SDT ≤ −6.5 = normosmia
Radiofrequency Inferior Turbinate Reduction
We used a temperature-controlled (somnoplasty model S2; Somnus Medical Technologies, Sunnyvale, CA) and nontemperature-controlled (Sutter; Sutter Medizintechnik GmbH, Freiburg, Germany) machine to perform RFITR. The selection of instruments depended on the preference of the surgeon. The procedure is already described elsewhere.12
Statistical Analysis
Because the data were not normally distributed, nonparametric statistics were used. Data analysis was performed by comparing outcome variables (nasal obstruction, rhinorrhea, sense of smell, nasal itching measured by VAS, SDT, ITG, and PNIF) before and after RFITR. This was performed by Wilcoxon signed-rank test. The correlation between SDT and VAS (nasal obstruction and sense of smell) before and after RFITR was performed using Spearman's rank order correlation. Significant level was accepted at p < 0.05 in two-tailed tests. The computer program used for calculation in this study was the IBM SPSS Version 13.0 (SPSS, Inc., Chicago, IL).
RESULTS
Forty-eight subjects (36 men and 12 women; mean age ± SD, 44 ± 10.8 years; age range, 18–60 years) were included in this study. All nasal symptoms (evaluated by using VAS) were significantly decreased after RFITR (p < 0.05; Table 2). The mean scores of SDT were −9.47 before surgery and −9.76 after surgery (p = 0.39).
Table 2.
The comparison of outcome variables before and after surgery

Data are presented in the median (25th–75th percentiles).
*Wilcoxon signed-rank test.
VAS = visual analog scale; ITG = inferior turbinate grading; PNIG = peak nasal inspiratory flow.
After surgery, SDT was worsened in 7 patients (14.6%), improved in 8 patients (16.7%), and did not change in 33 patients (68.7%; Table 3). SDT after RFITR of six patients in the worsened SDT group were still within normal range (> −6.5). There was only one patient whose SDT changed from normosmia to mild hyposmia (−7.25 to −5.38). In the improved SDT group, two of eight patients had obviously better SDT after RFITR, which changed from moderate hyposmia to normosmia (−3.65 to −10 and −3.73 to −10), whereas six of eight patients had little better SDT after RFITR but their SDT after RFITR was still within normal range. RFITR significantly reduced the size of the inferior turbinate and improved PNIF (p < 0.05; Table 2). The significant correlation between SDT and either VAS of nasal congestion or VAS of the sense of smell before and after surgery was not found (Table 4). No patient experienced postoperative complications, e.g., bleeding, infection, mucosal ulceration, or crusting.
Table 3.
The change of smell ability (SDT) measured by PEA before and after surgery

SDT = smell detection threshold; PEA = phenyl ethyl alcohol.
Table 4.
The correlation between outcome variables
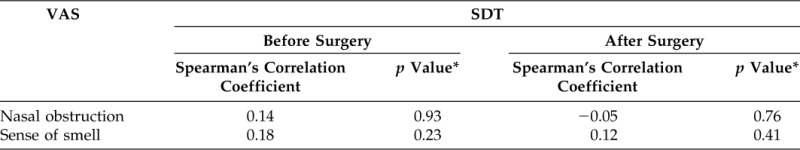
*Spearman's rank order correlation.
SDT = smell detection threshold; VAS = visual analog scale.
DISCUSSION
Twenty-two percent of patients with CR were found to have smell dysfunction caused by obstruction of airflow to olfactory cleft.8–10 We found smell dysfunction in 4.2% of our patients, which was lower than those observed in previous studies.8–10 This difference is because of the fact that previous studies included patients with chronic rhinosinusitis with nasal polyps, in whom smell dysfunction was the leading complaint, or because of the reliability of the olfactory test. RFITR is one of the treatments of resistant nasal obstruction in patients with CR and ITH. It is quite simple with minimal complication.13,14 The decreased nasal obstruction should lead to better smell ability. We studied the effect of RFITR on subjective, semiobjective, and objective parameters 6–10 weeks postoperatively. Subjective parameters included VAS of nasal obstruction, rhinorrhea, sense of smell, nasal itching, and sneezing. RFITR significantly decreased all VASs of nasal symptoms consistent with previous studies.12,13 In addition to improved nasal obstruction, other symptoms such as rhinorrhea, sense of smell, nasal itching, and sneezing of patients with CR were also improved after RFITR, indicating that RFITR also affected neural and secretory elements of nasal mucosa.12–14 Another subjective parameter is ITG, which was classified by the Friedman grading system.11 RFITR significantly decreased ITG compared with its preoperative values, in agreement with decreased VAS of nasal obstruction.
The semiobjective parameter was SDT, which was measured using PEA. RFITR led to better smell ability (16.7%), same smell ability (68.7%), and worse smell ability (14.6%). Previous studies showed that RFITR could improve smell function12,13,15 or did not change smell function.14,15 For example, Back and colleagues14 did not find any change of smell ability before and after RFITR, whereas Garzaro and colleagues15 showed that RFITR could improve smell function and did not change smell function.
The possible explanation why RFITR did not improve SDT in all patients was, first, the preoperative SDT of the majority of patients (n = 46 or 95.8%) was classified as normosmia and the SDT of the majority of patients (n = 33 or 68.7%) did not change postoperatively. This might explain why we did not see many patients who had improved SDT after surgery. Furthermore, the preoperative SDT of only two patients (4.2%) was classified as moderate hyposmia, which their postoperative SDTs were classified as normosmia.
Second, for the majority of patients (six of seven) who had worse SDT and the majority of patients (six of eight) who had better SDT after RFITR, their postoperative SDTs were still classified as normosmia. These could be caused by intraindividual variation of the PEA test, which was a forced-choice procedure because their preoperative SDTs were classified as normosmia as well.
Third, we did not find any possible etiology why one patient had worse SDT after RFITR (preoperative SDT was −7.25 [normosmia] and postoperative SDT was −5.38 [mild hyposmia]). However, after 3-month follow-up, this patient's smell ability returned to normosmia.
PNIF was the objective parameter. RFITR significantly improved PNIF, which was in agreement with improved ITG and VAS of nasal obstruction postoperatively. In addition, there was no complication after RFITR.
We also investigated the relationship between SDT and VAS (nasal obstruction and sense of smell) before and after RFITR. We found no significant relationship among those parameters, indicating that subjective, semiobjective, and objective parameters did not go in the same direction, which could occur in any study. The reason for such discrepancies may be related to different factors that could affect smell perception. Nasal obstruction might not be the only cause that contributed to smell function. Smell ability is a special sensation that depends on age, sex, and individual experience.3 Therefore, the individual perception of severity of smell dysfunction is different. Patients might not be able to perceive smell dysfunction although they had abnormal SDT.18 Furthermore, self-evaluation of smell ability has been shown to be unreliable in normosmic patients,19,20 which were the majority of our patients, (n = 46 or 95.8%) in contrast with hyposmic patients, which were the minority of our patients (n = 2 or 4.2%).20 Normosmic patients might pay limited attention to their sense of smell, resulting in unreliable rating of olfactory function.19 In the assessment of smell function, because subjective evaluation by patients (measured by VAS) may not be related to semiobjective evaluation using SDT, clinical evaluation of smell function needs both subjective and semiobjective, if possible objective, appraisal.
CONCLUSION
The treatment of nasal obstruction in patients with CR and ITH by RFITR significantly improved PNIF, ITG, nasal obstruction, nasal itching, sneezing, rhinorrhea, and sense of smell as assessed by VAS although SDT after RFITR could be the same or improved or worsened.
ACKNOWLEDGMENTS
The authors thank Suthipol Udompunturak, their consulting statistician, and Jeerapa Kerdnoppakhun, their research assistant, for their kind contributions. They also thank all staffs of the Rhinology and Allergy Division as well as all patients who participated in this study.
Footnotes
Funded by Siriraj Research Development Fund, Faculty of Medicine Siriraj Hospital, Mahidol University
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Eriksson J, Ekerljung L, Sundblad BM, et al. Cigarette smoking is associated with high prevalence of chronic rhinitis and low prevalence of allergic rhinitis in men. Allergy 68:347–354, 2013 [DOI] [PubMed] [Google Scholar]
- 2. Moore JR, Bicknell PG. A comparison of cryosurgery and submucous diathermy in vasomotor rhinitis. J Laryngol Otol 94:1411–1413, 1980 [DOI] [PubMed] [Google Scholar]
- 3. Snow JB., Jr Importance of the chemical senses. In Taste and Smell Disorders. Seiden AM. (Ed). New York, NY: Thieme Medical Publishers, 1–3, 1997 [Google Scholar]
- 4. Deems DA, Doty RL, Settle RG, et al. Smell and taste disorders, a study of 750 patients from the University of Pennsylvania Smell and Taste Center. Arch Otolaryngol Head Neck Surg 117:519–528, 1991 [DOI] [PubMed] [Google Scholar]
- 5. Hummel T, Nordin S. Olfactory disorders and their consequences for quality of life. Acta Otolaryngol 125:116–121, 2005 [DOI] [PubMed] [Google Scholar]
- 6. Santos DV, Reiter ER, DiNardo LJ, Costanzo RM. Hazardous events associated with impaired olfactory function. Arch Otolaryngol Head Neck Surg 130:317–319, 2004 [DOI] [PubMed] [Google Scholar]
- 7. Miwa T, Furukawa M, Tsukatani T, et al. Impact of olfactory impairment on quality of life and disability. Arch Otolaryngol Head Neck Surg 127:497–503, 2001 [DOI] [PubMed] [Google Scholar]
- 8. Apter AJ, Mott AE, Frank ME, Clive JM. Allergic rhinitis and olfactory loss. Ann Allergy Asthma Immunol 75:311–316, 1995 [PubMed] [Google Scholar]
- 9. Doty RL, Mishra A. Olfaction and its alteration by nasal obstruction, rhinitis, and rhinosinusitis. Laryngoscope 111:409–423, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Simola M, Malmberg H. Sense of smell in allergic and nonallergic rhinitis. Allergy 53:190–194, 1998 [DOI] [PubMed] [Google Scholar]
- 11. Friedman M, Tanyeri H, Lim J, et al. A safe, alternative technique for inferior turbinate reduction. Laryngoscope 109:1834–1837, 1999 [DOI] [PubMed] [Google Scholar]
- 12. Banhiran W, Tantilipikorn P, Metheetrairut C, et al. Quality of life in patients with chronic rhinitis after radiofrequency inferior turbinate reduction. J Med Assoc Thai 93:950–960, 2010 [PubMed] [Google Scholar]
- 13. Rhee CS, Kim DY, Won TB, et al. Changes of nasal function after temperature-controlled radiofrequency tissue volume reduction for the turbinate. Laryngoscope 111:153–158, 2001 [DOI] [PubMed] [Google Scholar]
- 14. Bäck LJ, Hytönen ML, Malmberg HO, Ylikoski JS. Submucosal bipolar radiofrequency thermal ablation of inferior turbinates: A long-term follow-up with subjective and objective assessment. Laryngoscope 112:1806–1812, 2002 [DOI] [PubMed] [Google Scholar]
- 15. Garzaro M, Pezzoli M, Pecorari G, et al. Radiofrequency inferior turbinate reduction: An evaluation of olfactory and respiratory function. Otolaryngol Head Neck Surg 143:348–352, 2010 [DOI] [PubMed] [Google Scholar]
- 16. Assanasen P, Bunnag C, Tunsuriyawong P, et al. Rhinosinusitis registry in Thailand. Siriraj Med J 57(suppl 1):105–106, 2005 [Google Scholar]
- 17. Bousquet J, Khaltaev N, Cruz AA, et al. ; World Health Organization; GA(2)LEN; AllerGen. Allergic Rhinitis and Its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy 63(suppl 86):8–160, 2008 [DOI] [PubMed] [Google Scholar]
- 18. Assanasen P, Tunsuriyawong P, Pholpornphisit W, et al. Smell detection threshold in Thai adults. J Med Assoc Thai 92:813–816, 2009 [PubMed] [Google Scholar]
- 19. Landis BN, Hummel T, Hugentobler M, et al. Ratings of overall olfactory function. Chem Senses 28:691–694, 2003 [DOI] [PubMed] [Google Scholar]
- 20. Nguyen DT, Nguyen-Thi PL, Jankowski R. How does measured olfactory function correlate with self-ratings of the sense of smell in patients with nasal polyposis? Laryngoscope 122:947–952, 2012 [DOI] [PubMed] [Google Scholar]


