Abstract
A 40-year old woman, gravida 4, para 4, presented with sudden lower abdominal pain and severe vaginal bleeding at 17 weeks of gestation. Clinical symptoms and ultrasonographic finding revealed placental abruption. The volume of bleeding was heavy and led to disseminated intravascular coagulation and hypovolemic shock. We performed blood transfusion and therapy to treat the critical condition. However, the mother’s condition continued to worsen. Therefore, we performed a hysterotomy and aborted the pregnancy to save the mother. Since heavy bleeding caused by placental abruption leading to a life-threatening condition for a mother before the 20 weeks of gestation is very rare, the present case is an important case study.
Key words: placental abruption, disseminated intravascular coagulopathy, second trimester
Introduction
Placental abruption occurs when the placenta partially or completely detaches from the uterine wall during the pregnancy or during parturition before the delivery of the fetus; it occurs in 0.5-1.5% of all pregnancies.1,2 Clinical presentation varies depending on the degree of placental detachment. However, blood flow through the placenta to the fetus can be partially or completely blocked, increasing fetal mortality. Morbidities affecting the mother also increase, because disseminated intravascular coagulation (DIC) can cause severe blood loss. Placental abruption is most frequently observed during the 24th to 26th weeks of pregnancy, decreasing in frequency thereafter. Onset before the 20 weeks of pregnancy is very rare.2 Here, we report a case of placental abruption with severe blood loss at the 17 weeks of gestation.
Case Report
The patient was a 40-year old woman with four prior normal vaginal deliveries. She had no abnormal medical or family history. She smoked 20 cigarettes per day. She also denied the occurrence of any trauma.
She presented with sudden severe lower abdominal pain at 17 weeks gestation, accompanied by severe vaginal bleeding. She was immediately transferred from another hospital. Until this point, the pregnancy had been proceeding normally without bleeding or abdominal pain.
Clinical findings: She was pale, blood pressure was 80/50 mmHg, and pulse rate was 120 per minute. Heavy vaginal bleeding with blood clots was confirmed. The uterus was contracting continuously, leading to severe lower abdominal pain.
Abdominal ultrasound: It showed a single live fetus with a normal heart rate. Additionally, the placenta was attached to the anterior uterine wall, but a well-defined 5×3 cm high-intensity region and a 1×2-cm lowintensity region were noted within the placenta suggestive of intra-placental hemorrhage (Figure 1).
Figure 1.

Placenta attached to the anterior uterine wall. A well-defined 5×3-cm highintensity region and a 1×2-cm low-intensity region were confirmed within the placenta (↑).
Initial laboratory findings: blood parameters were as follows: hemoglobin, 7.9 g/dL; platelet count, 82,000/L; prothrombin time, 320 seconds (control, 11.4 seconds); partial prothrombin time, >400 seconds (control, 11.4 seconds); serum fibrinogen, 17 mg/dL (reference range: 270-471 mg/dL). The results confirmed the presence of anemia and consumptive coagulopathy. Protein S activation was not measured.
A diagnosis of placental abruption at 17 weeks of gestation was made by clinical symptoms and ultrasonographic finding. She was hospitalized to treat the DIC, and hemorrhagic hypovolemic shock secondary to placental abruption.
Progression after hospitalization
A total of 16 units frozen plasma and 10 units packed red cells were transfused to treat the DIC and hemorrhagic shock. However, hematological parameters 2 h post-transfusion worsened: hemoglobin, 5.0 g/dL; platelet count, 42,000/L; blood pressure, 70/40 mmHg; pulse rate, 120 per minute. Vaginal bleeding continued, with a total blood loss of 2200 mL after hospitalization. Fetal heartbeat was confirmed by ultrasound.
She had been in a serious condition due to the DIC and hemorrhagic shock. We determined that the delivery of the fetus was necessary to save her. However, since the dilation of the uterine cervix was only 2 cm, rapid delivery could not be expected. Therefore, we decided to perform a hysterotomy and terminate the pregnancy for life-threatening maternal hemorrhage.
Intraoperative findings
Blood infiltration was evident in the uterine muscle layer (i.e., Couvelaire uterus) (Figure 2). A hematoma covering 60% of the posterior wall of the placenta was observed when the uterus was excised and the fetus and placenta were removed (Figure 2). Intravenous infusion of oxytocin was initiated after the placenta was removed. Satisfactory uterine contraction and natural reduction in bleeding from the uterus were confirmed; therefore, any other medication and gauze packing was unnecessary.
Figure 2.
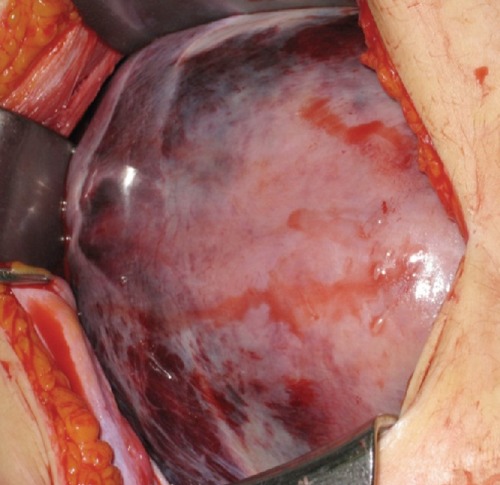
Uterus during operation. There is clear evidence of blood infiltration in the uterine muscle (i.e., Couvelaire uterus).
Postoperative findings
A total of 20 units frozen plasma and 12 units packed red cells were transfused during the operation. Uterine bleeding decreased, and the volume of blood loss was 380 mL 4 h after the operation. Twenty-four-hour postoperative hemoglobin was 9.9 g/dL, platelet count was 102,000/L, prothrombin time was 10.4 seconds (control, 11.4 seconds), partial prothrombin time was 25.8 seconds (control, 29.4 seconds), and serum fibrinogen was 296 mg/dL (reference range: 270-471 mg/dL). The DIC improved, and vaginal bleeding became minimal; therefore, treatment was halted, and the patient was discharged 6 days after the operation.
Histopathological studies revealed a blood clot attached to the deciduous placenta and infiltration of blood into the surrounding intervillous space, confirming ischemic changes. These placental pathological findings are concordant with those observed in placental abruption.
Discussion and Conclusions
Placental abruption is one of the serious complications of pregnancy, because it leads to both poor maternal and fetal/neonatal outcome. In cases involving severe blood loss, incurring a risk of the maternal mortality, improvement from the life-threatening condition should be prioritized. However, since placental abruption with severe blood loss causing a life-threatening situation for the mother is rare for pregnancies before the 20 week of gestaion, the present case is an important case study.
The diagnosis of placental abruption usually depends on the clinical manifestations, and confirmed the placental detachment after delivery. Clinical symptoms include vaginal bleeding, uterine pain, and continuous uterine stiffening.2 The usefulness of ultrasonography have been reported as the adjunctive diagnosis, and it is widely used for this purpose. Ultrasound findings include retroplacental hematoma, placental thickness.3 In the present case, the patient presented with sudden and severe vaginal bleeding accompanied by lower abdominal pain. In addition, uterine stiffness was observed and intra-placental hematoma was confirmed by ultrasound. On the basis of these observations, we diagnosed the patient with placental abruption even though the pregnancy was only in the 17 weeks of gestation. Hypostasis of the uterus, i.e., Couvelaire uterus, was confirmed during the operation. The histology of the placenta showed retroplacental blood clot as well as bleeding and ischemic changes in the intervillous space. These findings demonstrate that placental abruption can occur and is diagnosable at the 17 weeks’ gestation. Placental abruption most frequently occurs during the 26 weeks’ gestation and rarely before the 20 weeks.2 Our patient had severe DIC during the second trimester following separation of the placenta. Placental abruption at this stage of pregnancy is very uncommon, but the associated DIC can be life threatening. Similar case reports and short communications were published in the literature in the late 1980s.4-7 It is interesting to note that only 1 case was sufficiently severe to warrant dilation and evacuation,8 whereas the other obstetrics cases were followed with cautious conservative treatment as long as the fetus was alive, and the pregnancies were completed with fetal survival. In addition, although severe DIC developed rapidly, the coagulopathy was completely resolved. However, it is important to distinguish placental abruption as one of the causes of bleeding during the early phase of the second trimester.
Next, the delivery method for fetuses before the 24 weeks gestation must be considered for severe placental abruption. Oyelese and Ananth proposed an algorithm that calls for the delivery of premature fetuses before the 24 weeks regardless of the certainty of its survival, if there is danger to the mother; however, they do not discuss the method of delivery.2 On the basis of the present patient’s four prior normal pregnancies and stiff uterine contractions, we surmised the condition would naturally progress to vaginal delivery. However, dilation of the uterine cervix did not advance. On the other hand, bleeding continued, the mother’s anemia worsened, blood pressure decreased, tachycardia was observed, and her general condition worsened. Therefore, we opted to terminate the pregnancy through surgical intervention involving hysterotomy. Termination led to rapid improvement of the mother’s condition, suggesting that the surgical intervention was effective.
Hematological findings at the time of hospitalization already revealed reduction of blood fibrinogen and platelets as well as continuous massive vaginal bleeding. Hence, we surmised that the placental abruption led to secondary DIC, causing life-threatening blood loss for the mother. Therefore, we transfused fresh frozen plasma to correct the DIC; we simultaneously performed rapid transfusions to reduce circulating blood volumes. DIC is most common in patients with comparatively large ablated areas of the placenta or those with prior in utero fetal deaths.7 However, in this case, the fetus was alive, and the mother still presented with DIC, which differs from previously reported cases. Similar cases of DIC with live fetuses accompanying placental abruption report that DIC is more prevalent because there is more movement of tissue factors during the second trimester than the third.5 In such cases, even a small ablation could lead to DIC.5 DIC can occur with placental abruption early in the pregnancy without adversely affecting the fetal heart rate; however, it may be a distinct characteristic of placental abruption occurring early in pregnancy. There is a report that pregnancy can be maintained even after anti-DIC therapy for placental abruption of normally implanted placenta, which led to improvement.9
Seckin reported that progression from placental abruption to DIC is rare during the second trimester; if it does occur, the presence of factors for thromboembolic formation must be investigated.10 However, unfortunately, protein S, C for inherited thrombophilic conditions were untested in the presented case.
The present patient was a 40-year-old woman who smoked. The risk factors leading to the onset of placental abruption include smoking (odds ratio: 1.5-2.5) and age over 35 (odds ratio: 1.3-2.6).1 Furthermore, history of previous placental abruption has a high recurrence rate (odds ratio: 3.2-25.8).1 Therefore, she should avoid next pregnancy.
This case illustrate that if there is a life-threatening obstetrical hemorrhage secondary to placental abruption, even early in the second trimester, pregnancy terminated promptly.
References
- 1.Tikkanen M. Placental abruption: epidemiology, risk factors and consequences. Acta Obstet Gynecol Scand 2011;90:140-9 [DOI] [PubMed] [Google Scholar]
- 2.Oyelese Y, Ananth CV. Placental abruption. Obstet Gynecol 2006;108:1005-16 [DOI] [PubMed] [Google Scholar]
- 3.Glantz C, Purnell L. Clinical utility of sonography in the diagnosis and treatment of placental abruption. J Ultrasound Med 2002;21:837-40 [DOI] [PubMed] [Google Scholar]
- 4.Monteiro AA, Inocencio AC, Jorge CS. Placental abruption with disseminated intravascular coagulopathy in the second trimester of pregnancy with fetal survival. Case report. Br J Obstet Gynaecol 1987;94: 811-2 [DOI] [PubMed] [Google Scholar]
- 5.Panayotidis C, Willett M, Kiwanuka A. Hysterotomy for maternal life-threatening hemorrhage secondary to placental abruption at 24 weeks gestation. Obstet J Gynaecol 2003;23:310-11 [DOI] [PubMed] [Google Scholar]
- 6.Hodgson DT, Lotfipour S, Fox JC. Vaginal bleeding before 20 weeks gestation due to placental abruption leading to disseminated intravascular coagulation and fetal loss after appearing to satisfy criteria for routine threatened abortion: a case report and brief review of the literature. J Emerg Med 2007;32:387-92 [DOI] [PubMed] [Google Scholar]
- 7.Cunningham GF, MacDonald PC, Gant NF. Obstetrical hemorrhage. In: Williams Obstetrics, 23rd ed. New York: McGraw-Hill; 2010. pp 761-9 [Google Scholar]
- 8.Oláh KS, Gee H, Needham PG. The management of severe disseminated intravascular coagulopathy complicating placental abruption in the second trimester of pregnancy. Br J Obstet Gynaecol 1988;95:419-20 [DOI] [PubMed] [Google Scholar]
- 9.Barton DP, Turner MJ, Stronge JM. Fetal survival following coagulopathy at 17 weeks’ gestation. Obstet Gynecol 1989;74: 468-69 [PubMed] [Google Scholar]
- 10.Seckin NC, Inegöl I, Turhan NO, et al. A life-threatening second trimester disseminated intravascular coagulopathy with protein S deficiency. Clin Appl Thromb Hemost 2004;10:289-91 [DOI] [PubMed] [Google Scholar]


