Abstract
Although nonalcoholic steatohepatitis (NASH) is typically associated with obesity, it has also been reported to occur in lean individuals exposed to industrial chemicals. Occupational exposure to vinyl chloride (VC) is a well-documented risk factor for hemangiosarcoma, but has not previously been associated with steatohepatitis. Here, we evaluate liver biopsies from 25 non-obese, highly-exposed, VC workers for steatohepatitis. Next, we evaluate associated metabolic and cytokine abnormalities in affected workers controlled by 26 chemical workers with no to minimal VC exposures, and 11 unexposed, healthy volunteers. Among highly-exposed VC workers, the prevalence of steatohepatitis was 80%. Of these, 55% had fibrosis and four had hemangiosarcoma. We have coined the term, toxicant-associated steatohepatitis (TASH), to describe this condition which was not explained by obesity or alcohol. Although mean serum transaminases were normal in TASH, total cytokeratin18, but not the caspase-cleaved fragment, was elevated. Despite the absence of obesity, workers with TASH had insulin resistance with reduced adiponectin levels. TASH was also associated with markedly elevated serum tumor necrosis factor alpha and interleukins 1β, 6, and 8. Serum antioxidant activity was reduced in TASH.
Conclusion
TASH occurred frequently in these non-obese VC workers with high cumulative exposures and normal liver enzymes. Elevated total cytokeratin 18 suggested the presence of necrotic cell death in TASH and may be a useful serologic biomarker. TASH was further characterized by insulin resistance, elevated pro-inflammatory cytokines, and impaired antioxidant defenses. The threshold VC exposure and the role of other chemical agents in TASH are as yet unknown.
Keywords: nonalcoholic fatty liver disease, polyvinyl chloride, hemangiosarcoma, alcoholic hepatitis, NASH
Nonalcoholic fatty liver disease (NAFLD) is the most common chronic liver disease in the United States, and its prevalence is rising (1). By histology, NAFLD resembles alcoholic liver disease, although affected individuals, by definition, do not drink. NAFLD encompasses a spectrum of liver pathology beginning with fat accumulation (steatosis), which may trigger an inflammatory and fibrotic response (steatohepatitis or NASH) and progress to cirrhosis and hepatocellular carcinoma. NAFLD is generally believed to be the hepatic manifestation of obesity and the metabolic syndrome. However, recent reports document NASH in lean petrochemical workers as well as cancer patients treated with chemotherapy (2, 3). A “two hit” model has been proposed to explain why some, but not all, NAFLD patients develop progressive disease (4). Multiple “second hits” including pro-inflammatory cytokines, and metabolic abnormalities such as insulin resistance and oxidative stress have been described. It is unknown why these associated abnormalities do not affect all NAFLD patients, but differential exposures to occupational and environmental toxicants could potentially play a role (1).
Monomeric vinyl chloride (VC) is a relevant chemical toxicant. VC production was recently estimated at 27 million metric tons annually, valued at US $19 billion (5). VC is most often polymerized into the ubiquitous plastic, polyvinyl chloride (PVC). To date, more than 80,000 American chemical workers have been exposed to VC (6). Furthermore, VC has been identified as a degradation product of chlorinated solvents, and it is present in landfill leachate where it potentially places surrounding populations at risk (6). VC is a classic mediator of both malignant and benign liver diseases. Initial concern regarding VC exposure related to hepatic hemangiosarcoma (7). However, hepatocellular carcinoma has become a more recent issue (7–10). The benign liver lesions historically associated with VC exposure include focal hepatocytic hyperplasia (FHH), focal mixed hyperplasia (FMH), sinusoidal dilation, and portal fibrosis (11). Importantly, most histopathologic research in benign VC-induced liver disease was done prior to the initial description of NASH by Ludwig et al. in 1980, and certainly prior to the recognition of NASH as a significant clinical entity (12). Notably, in his final publication regarding VC-related benign liver disease, the late Hans Popper noted that FHH and FMH were often obscured by “fatty infiltration and/or chronic disease (hepatitis/granuloma)” (11). More recently, NASH was reported in lean petrochemical workers from Brazil exposed to 18 chemicals including vinyl chloride (3). Furthermore, four ultrasound studies published within the last decade have noted a high incidence of hepatomegaly, steatosis, and fibrosis in VC workers (13–16). Unfortunately, these studies were uncontrolled and histological confirmation was not provided. However, older limited pathologic data describe non-specific fatty changes in VC workers (10, 11, 17). Biopsy proven NASH has never been documented in American plastics workers, and the associated metabolic and cytokine abnormalities have never been investigated in chemical workers with steatohepatitis. Here, we describe a high prevalence of a unique form of steatohepatitis which we have termed toxicant-associated steatohepatitis (TASH) occurring in non-obese, non-drinking VC workers with high cumulative exposures. Selected associated metabolic and cytokine abnormalities are examined and compared to other chemical workers with no to minimal VC exposures as well as unexposed healthy volunteers.
Patients and Methods
Subjects
In 1974, Creech and Johnson reported the occurrence of the unusual liver tumor, hemangiosarcoma, in three chemical workers at a single PVC production facility (18). Subsequently, approximately 1200 workers exposed to over 30 industrial chemicals were enrolled in a medical surveillance program initiated by the manufacturer in collaboration with the National Cancer Institute and University of Louisville, which created a large database and specimen bank (19). The most intensive surveillance was targeted to a much smaller group of approximately 100 chemical operators and helpers who frequently entered and manually cleaned PVC batch reactor vessels. These workers encountered exceptionally high VC exposures often exceeding 1000 parts-per-million (ppm) during the manual scraping and chipping of resins from the reactor walls from the onset of plant operations in 1942 until the implementation of the modern time-weighted VC exposure limit of 1 ppm in 1975 (20). All 25 cases of hepatic hemangiosarcoma to date from the Louisville plant have occurred in this group of highly-exposed VC workers. As part of the cancer surveillance program, high-risk workers underwent serial physical examinations with laboratory testing. Baseline percutaneous liver biopsies were obtained from 1974–1977, and serum was archived at −80° C at the University. In some cases, surgical wedge liver biopsies were obtained during abdominal operations for hemangiosarcoma. The original slides from 25 of these high-risk workers were obtained from our specimen bank and were over-read by a single, modern-day, expert hepato-pathologist, who examined the slides for steatohepatitis. Henceforth, in this manuscript, this group of chemical workers will be referred to as the Biopsied VC Worker Group. The subgroup of the biopsied VC worker group with steatohepatitis will be referred to as the TASH Group.
Two groups of healthy (negative) controls were selected for serologic evaluation of the metabolic and cytokine abnormalities thought to contribute to steatohepatitis. The Healthy Chemical Worker Control Group consisted of 26 healthy, non-drinking, chemical workers who had normal liver enzymes and no history of liver disease or other significant medical problems either at the time of serum sample collection or at any point during the cancer surveillance project. They were age, sex, and body mass index (BMI) matched as closely as possible to the TASH group. They were employed in the plastics or catalyst industries and had minimal to no VC exposures. Serum samples were archived at −80° C for a similar length of time as the samples from the TASH group. The Healthy Unexposed Control Group consisted of 11 modern-day subjects who did not work in the chemical industry and had normal liver enzymes and no history of liver disease, significant ethanol consumption, or obesity. Serum samples from this last group were stored at −80° C for less than 1 year. All research subjects gave informed consent and institutional IRB approval was obtained prior to the initiation of this project in accordance with the 1975 Declaration of Helsinki.
Exposure Indices
VC exposures were characterized in several ways based on employment records. First, the duration of employment, which approximates the duration of VC exposure, through the time of liver biopsy was determined. Then, occupational VC exposure during the month of the liver biopsy was determined. Next, an index of cumulative exposure, the cumulative exposure rank month (CERM), was determined for each employee at the time of liver biopsy as described previously (21). Briefly, all jobs in the plant were assigned a rank from 0–6 based on the level of VC exposure. Workers who were absent from the plant for a month were assigned a score of zero for that month, while workers with intimate skin contact or high inhalational exposures were assigned a score of six. Ranks were summed yearly (maximum yearly score 72), and the CERM was calculated. These highly-exposed employees typically worked jobs with monthly exposure indices of six, with daily exposures in excess of 1000 PPM. By estimating that a CERM of 72 was equivalent to 1000 parts-per-million-year (ppm-yr), the cumulative exposures at the time of liver biopsy were determined in ppm-yr.
Histological Evaluation of Liver Biopsies
Routine hematoxylin and eosin as well as trichrome stained slides from liver biopsies of the 25 highly-exposed VC workers were obtained from our specimen bank. They were then graded and staged by a single expert hepato-pathologist using the Brunt criteria (22). The NAFLD activity score (NAS) was determined (22, 23).
Serum Analysis
Serum cytokines and adipokines were determined by multi-analyte chemiluminescent detection using LINCOplex Human Adipokine Panel A and B kits (Millipore, Billerica, MA) on the Luminex®100™ IS System (Austin, TX). Specifically, tumor necrosis factor α (TNFα), interleukin-1β (IL-1β), interleukin-6 (IL-6), interleukin-8 (IL-8), macrophage chemoattractant protein-1 (MCP-1), adiponectin, leptin, and insulin were measured. Serum cytokeratin 18 (CK-18) whole (M65®) and caspase-cleaved fragments (M30 Apoptosense®) were measured by ELISA (diaPharma, Columbus, OH). Serum total antioxidant activity was measured by the Antioxidant Assay Kit (Cayman Chemical, Ann Arbor, MI) which evaluates the ability of antioxidants in the sample to inhibit the oxidation of 2,2′-azino-di-[3-ethylbenzthiazoline sulphonate] by metmyoglobin. Results are reported as mean ± standard deviation.
Statistical Analysis
Intergroup comparisons were performed by one-way ANOVA with Tukey’s post-test using GraphPad Prism version 5.00 for Windows (San Diego, California). Potential gender differences between groups were evaluated by Fisher’s exact test. A p value less than 0.05 was considered statistically significant.
Results
Demographic Information
Demographic data for the biopsied VC worker group and control groups are given as Table 1. All 25 VC workers were white males which was reflective of plant hiring practices at that time. The mean age at the time of liver biopsy was 45.0±7.4 years (standard deviation). The mean body mass index was 25.7±3.8 kg/m2. The mean duration of employment at the time of liver biopsy was 19.0±7.0 years, and the mean CERM was 820±482, corresponding to an estimated mean cumulative VC exposure of 11,391±6699 ppm-yr at the time of biopsy. Workers were also exposed to lower levels of a multiple of additional industrial chemicals (Table 2). While four subjects reported alcohol consumption, only one subject consumed more than 1 drink per day. Two reported a past medical history of diabetes, while seven subjects had a history of hypertension. Although the healthy unexposed control group contained more females than both the biopsied VC worker group and the healthy chemical worker control group, no significant differences in mean age or BMI were present. No significant differences in age, sex, or BMI were observed between the biopsied VC workers and the healthy chemical worker controls.
Table 1.
Demographic Information
| Demographic Variable | Healthy Unexposed Controls | Healthy Chemical Worker Controls | Biopsied VC Workers |
|---|---|---|---|
| Number | 11 | 26 | 25 |
| Age | 44.3 (11.4) | 48.4 (8.0) | 45.0 (7.4) |
| Gender (% male) | 64% | 96%a | 100%a |
| BMI (kg/m2) | 24.9 (4.9) | 27.1 (3.9) | 25.7 (3.8) |
p<0.05 vs. Healthy Unexposed Controls.
Table 2.
Chemical Exposures Reported at the PVC Plant
| Acetylene |
| Acrylamides: Acrylamide, Methyl, N-Octyl |
| Acrylates: n-Butyl, Ethyl, 2 Ethyl Hexyl, Hydroxyethyl, Methyl, Dimethyl, Methoxyethyl |
| Acrylonitrile |
| Acrylic Acid |
| Bisphenol A |
| Butadiene |
| Caprylyl Chloride |
| Chlorinated Solvents: Carbon Tetrachloride, Chloroform, Trichloroethylene |
| Chloro Ethyl Vinyl Ether |
| Diethyl Maleate |
| Ethylene Glycol |
| Hexane |
| Methacrylic Acid |
| Methanol |
| Mercuric Chloride |
| Phenol |
| Polyvinyl Chloride Dust |
| Styrene |
| Toluene |
| Vinyl Acetate |
| Vinylidene Chloride |
Liver Biopsy Results
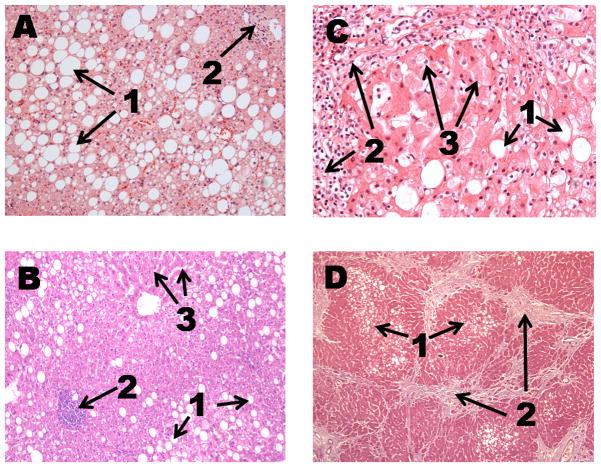
Liver chemistries obtained at the time of liver biopsy were normal and are given as Table 3. Although mean liver enzymes were normal, all 25 liver biopsies were abnormal. An extremely high prevalence of fatty liver disease (84%, 21/25) and steatohepatitis (80%, 20/25) was observed. The liver biopsies demonstrated typical morphologic features of steatohepatitis including small and large droplet macrovesicular steatosis, Mallory-Denk bodies, balloon degeneration, inflammatory infiltrate, and lipogranulomas. Grade 2 or higher activity was present in 30% (6 of 20) of the cases of steatohepatitis. The mean NAS score was 4.5±2.3. Fibrosis was present in 55% (11 of 20) of steatohepatitis cases. Of these, 8 subjects had stage 2 or higher fibrosis and one had fatty cirrhosis. Sinusoidal dilation, an atypical finding for NAFLD, was noted in 76% (16 of 21) of cases and was usually mild. Representative photomicrographs demonstrating some of these findings are shown as Figure 1. Because affected workers generally did not suffer from obesity or alcoholism, we have coined the term toxicant-associated steatohepatitis (TASH) to describe this unique form of steatohepatitis.
Table 3.
Liver Chemistries of the Biopsied VC Workers
| Liver Chemistry Test | Mean Value (s.d.) |
|---|---|
| ALT (0–55 U/L) | 26.3 (43.2) |
| AST (0–50 U/L) | 31.4 (29.4) |
| Alkaline Phosphatase (25–140 U/L) | 94.2 (54.6) |
| Total Bilirubin (0.2–1.2 mg/dL) | 0.8 (0.6) |
| Albumin (3.5–5.5 g/dL) | 4.0 (0.5) |
Laboratory reference ranges are given in parentheses.
Figure 1.
The one individual reporting significant alcohol consumption (21 drinks per week) had mild steatohepatitis without fibrosis and normal liver enzymes (AST 11 U/L, ALT 8 U/L). Therefore, while ethanol may have contributed to this case of steatohepatitis, the serum transaminase pattern was more consistent with TASH.
Four subjects with steatohepatitis also had concomitant hepatic hemangiosarcoma, and a fifth subsequently developed this tumor 7 years later. Three subjects with steatohepatitis had repeat liver biopsies at 1–6 years. Two of the 3 showed progressive liver injury and fibrosis despite removal from the workplace. 76% (16/21) of subjects with fatty liver have died to date. Of these, 38% (6/16) died from liver related causes such as hemangiosarcoma or cirrhosis. Other causes of death included non-hepatic solid organ tumors, chronic obstructive pulmonary disease, and congestive heart failure.
Of the 4 subjects without hepatic steatosis on biopsy, 3 of 4 had inflammatory changes suggestive of chronic hepatitis, and 3 of 4 had fibrosis (stage 1–2). One biopsy revealed prominent granulomas resembling sarcoid while another demonstrated prominent Mallory-Denk bodies in the absence of steatosis. All four had mild sinusoidal dilation.
Serum Transaminase and Cytokeratin 18 Levels
Next, archived serum from the time of liver biopsy was obtained from 16 subjects with TASH who did not have hemangiosarcoma and was compared to the 26 member healthy chemical worker control group, and the 11 member healthy unexposed control group. The mean age of the 16 member TASH group was 45.7±7.6 years which was not statistically different from the other groups. The mean BMI of this TASH group was 26.2±3.9 kg/m2 and was similar to the control groups. The healthy unexposed control group contained a significantly greater percentage of female subjects than both the TASH and the healthy chemical worker control groups. At the time of liver biopsy, the mean duration of employment in the TASH group was 18.9±7.5 years, and the mean CERM was 858±466, corresponding to an estimated mean cumulative VC exposure of 11,913±6480 ppm-yr. Based on employment records, all sixteen subjects with TASH had high-level occupational VC exposures during the month in which their liver biopsies were performed.
Mean serum transaminases and cytokeratin 18 values are given as table 4. Notably, both AST (19.9±8.0 U/L) and ALT (29.0±48.3 U/L) were normal in TASH. CK-18 M65® was elevated in TASH (583.4±319.2 U/L) compared to both the healthy unexposed control group (215.8 ±98.6 U/L) and healthy chemical worker control group (272.7±71.3 U/L). The CK-18 caspase-cleaved fragment (M30®) was numerically, but not statistically higher in TASH than in either control group (Table 4).
Table 4.
Serum Transaminase and Cytokeratin 18 Levels
| Laboratory Variable | Healthy Unexposed Controls | Healthy Chemical Worker Controls | TASH |
|---|---|---|---|
| ALT (U/L) | 14.0 (8.6) | 28.4 (11.3) | 29.0 (48.3) |
| AST (U/L) | 20.8 (3.3) | 21.5 (7.3) | 19.9 (8.0) |
| CK-18 M30® (U/L) | 164.1 (26.3) | 150.9 (74.6) | 183.7 (88.6) |
| CK-18 M65® (U/L) | 215.8 (98.6) | 272.7 (71.3) | 583.4 (319.2)a,b |
p<0.001 vs. Healthy Unexposed Controls;
p<0.001 vs. Healthy Chemical Worker Controls.
Serum Glucose, Triglycerides, Insulin, and Adipokine Levels
Mean serum glucose, triglycerides, insulin, adiponectin, and leptin are given as Table 5. The mean fasting glucose was higher in TASH (112.0±26.3 mg/dL) than in both the healthy unexposed control group (89.3±16.8 mg/dL) and the healthy chemical worker control group (89.4±11.9 mg/dL). Mean serum insulin levels were higher in TASH (1155.8±1500.4 pg/ml) than in the healthy chemical worker control group (327.3±372.6 pg/ml). Although two subjects with TASH reported a history of diabetes, only one had a fasting blood glucose ≥ 126 mg/dL, and neither was taking any diabetes medications. Of the remaining fourteen subjects, twelve had impaired fasting glucose defined as serum glucose ranging between 100–125 mg/dL (24). Some, but not all, TASH subjects with impaired fasting glucose also had hyperinsulinemia. However, all subjects with insulin levels exceeding 700 pg/ml also had impaired fasting glucose. Fasting serum triglycerides were normal in TASH and were similar to controls (Table 5). Mean serum adiponectin was significantly reduced in TASH (14.4±8.3 μg/ml) compared to the healthy unexposed controls (54.9±50.4 μg/ml). The mean serum leptin level was not increased in TASH, nor was it significantly different from controls (Table 5).
Table 5.
Serum Glucose, Triglycerides, Insulin, and Adipokine Levels
| Laboratory Variable | Healthy Unexposed Controls | Healthy Chemical Worker Controls | TASH |
|---|---|---|---|
| Glucose (mg/dL) | 89.3 (16.8) | 89.4 (11.9) | 112.0 (26.3)a,b |
| Triglycerides (mg/dL) | 123.0 (71.2) | 145.4 (101.6) | 128.8 (47.2) |
| Insulin (pg/ml) | 517.8 (440.5) | 327.3 (372.6) | 1155.8 (1500.4)c |
| Adiponectin (μg/ml) | 54.9 (50.4) | 29.5 (17.6)a | 14.4 (8.3)d |
| Leptin (ng/ml) | 11.8 (9.6) | 10.4 (12.9) | 7.2 (4.8) |
p<0.05 vs. Healthy Unexposed Controls;
p<0.01 vs. Healthy Chemical Worker Controls;
p<0.05 vs. Healthy Chemical Worker Controls;
p<0.001 vs. Healthy Unexposed Controls.
Serum Pro-inflammatory Cytokine Levels
Mean serum levels of TNFα, IL-1β, IL-6, IL-8, and MCP-1 are displayed as table 6. TASH was associated with a significantly increased mean serum TNFα (11.2±18.0 pg/ml) compared to the healthy chemical worker control group (3.0±1.2 pg/ml). TASH was associated with significantly increased serum IL-1β (9.1±11.9 pg/ml) compared to both the healthy unexposed (0.1±0.1 pg/ml) and the healthy chemical worker (0.4±0.6 pg/ml) control groups. Likewise, mean serum IL-6 was significantly elevated in TASH (10.9±10.6 pg/ml) compared to both the healthy unexposed (1.4±1.6 pg/ml) and the healthy chemical worker (3.5±3.0 pg/ml) control groups; and IL-8 was also significantly increased in TASH (12.0±12.9 pg/ml) compared to both the healthy unexposed (2.7±1.9 pg/ml) and the healthy chemical worker control (3.7± 1.6 pg/ml) groups. No significant differences were seen in mean serum MCP-1 levels between any groups (Table 6).
Table 6.
Serum Pro-inflammatory Cytokine and Antioxidant Activity Levels
| Laboratory Variable | Healthy Unexposed Controls | Healthy Chemical Worker Controls | TASH |
|---|---|---|---|
| TNFα (pg/ml) | 4.1 (1.5) | 3.0 (1.2) | 11.2 (18.0)a |
| IL-1β (pg/ml) | 0.1 (0.1) | 0.4 (0.6) | 9.1 (11.9)b,c |
| IL-6 (pg/ml) | 1.4 (1.6) | 3.5 (3.0) | 10.9 (10.6)b,d |
| IL-8 (pg/ml) | 2.7 (1.9) | 3.7 (1.6) | 12.0 (12.9)b,d |
| MCP-1 (pg/ml) | 276.5 (121.5) | 329.4 (137.9) | 302.3 (148.0) |
| Antioxidant Activity (mM) | 4.1 (0.3) | 3.5 (0.8) | 2.6 (0.3)c,e |
p<0.05 vs. Healthy Chemical Worker Controls;
p<0.01 vs. Healthy Unexposed Controls;
p<0.001 vs. Healthy Chemical Worker Controls;
p<0.01 vs. Healthy Chemical Worker Controls;
p<0.001 vs. Healthy Unexposed Controls.
Serum Antioxidant Activity
Mean total serum antioxidant activity is provided in Table 6. TASH was associated with reduced antioxidant activity (2.6±0.3 mmol/l) compared to both the healthy unexposed control group (4.1±0.3 mmol/l) and the healthy chemical worker control group (3.5±0.8 mmol/l).
Discussion
Our work demonstrates that steatohepatitis was exceptionally common in this group of highly-exposed vinyl chloride workers. In fact, 80% of biopsied VC workers had steatohepatitis, and to our knowledge, this is the highest incidence of steatohepatitis ever reported in any single group. In comparison, steatohepatitis has been reported to occur in 10%–35% of heavy drinkers and 25%–55% of bariatric surgery patients (25, 26). In our study, the affected VC workers were not obese, and except in potentially one case, their steatohepatitis could not be explained by ethanol. Therefore, as a group, they had no identifiable risk factor for steatohepatitis other than their industrial chemical exposures. Although exposures were far greater for VC than for the other chemicals in the plant, we cannot exclude a contribution from these other chemicals to the development of either TASH or hemangiosarcoma. This study provides the most comprehensive and mechanistic description of steatohepatitis in chemical workers to date. However, our report is strengthened by multiple previously published studies documenting abnormal liver enzymes, ultrasonographic evidence of hepatomegaly or steatosis, and even biopsy proven NASH in chemical workers exposed to a multitude of industrial chemicals (3, 13, 16, 27–29). We believe that there is now sufficient evidence to create a new category of steatohepatitis to be applied to these workers, and we propose to call it toxicant-associated steatohepatitis or TASH.
The workers in our study were exposed to much higher cumulative exposures than permitted under the Occupational Safety and Health Administration’s Vinyl Chloride Standard (29 CFR 1910.1017), which mandates that VC exposures average less than 1 ppm over an 8 hour work day. Therefore, the risk, if any, for VC workers hired subsequent to the implementation of this standard in 1975 cannot be estimated from our work. We must caution, however, that in our study, TASH was associated with normal liver enzymes. Therefore, the practice of liver enzyme surveillance in chemical workers could potentially be insensitive for the diagnosis of TASH. A recent ultrasound study of 347 asymptomatic polyvinyl chloride workers reported a 38.9% prevalence of fatty liver in spite of a normal mean BMI (13). These data suggest that TASH could also be a problem for modern-day VC workers with much more moderate cumulative exposures. Other studies suggest that TASH could be a problem which is not limited to the plastics industry (3). Although serial liver biopsies were not available in all workers, 3 subjects had repeat liver biopsies following removal from the workplace. Of these, 2 had progressive liver injury and fibrosis suggesting that TASH may not always be reversible even after the exposure is withdrawn. Similar results were noted in a prior study documenting the reversibility of steatohepatitis in only 10 of 20 chemical workers removed from a petrochemical plant (27). The potential additive effects of ethanol, obesity, and chemical exposure on the pathogenesis and progression of steatohepatitis are not well known. However, it was recently demonstrated that ethanol consumption and VC exposure acted synergistically in the development of both cirrhosis and hepatocellular carcinoma (8). Combined, these data call for more studies of TASH utilizing new serologic biomarkers such as cytokeratin 18, imaging, and liver biopsy in selected chemical workers exposed to a wide range of industrial chemicals across BMI’s and differing patterns of ethanol consumption throughout their careers.
In addition to the rigorous histopathologic examination of TASH, serum was also evaluated for associated abnormalities. Multiple potentially important mechanistic changes were identified. The pattern of serum CK-18 elevation suggested that TASH was associated predominantly with necrosis rather than the apoptosis frequently reported in NASH and alcoholic hepatitis (30). Insulin resistance and adiponectin reduction were noted in TASH. However, hypertriglyceridemia and hyperleptinemia, frequently observed in NASH, were not present. Serum antioxidants and levels of pro-inflammatory cytokines were elevated in TASH as classically described in alcoholic hepatitis.
Vinyl chloride is metabolized in a strikingly similar fashion to ethanol and this could potentially account for the observed similarities between TASH and alcoholic hepatitis. While initial studies suggested that at low substrate concentrations (below 100 ppm) VC is metabolized by a pathway involving alcohol dehydrogenase, most studies have concentrated on the role of CYP2E1 as the initial catalyst of vinyl chloride metabolism (31). At concentrations up to approximately 220 ppm, VC is metabolized by CYP2E1 forming the highly reactive genotoxic epoxide, chloroethylene oxide. Chloroethylene oxide either spontaneously or enzymatically is converted to chloroacetaldehyde (32). In either pathway, chloroacetaldehyde is formed. While chloroethylene oxide and chloroacetaldehyde are both genotoxic, chloroethylene oxide was found to be approximately 450 times more potent (33). Consistent with this view, there is a good correlation between vinyl chloride-DNA adduct formation and the ability of CYP2E1 to metabolize vinyl chloride (34). In some rodent species other CYPs also metabolize vinyl chloride at very high VC concentrations. However the relevance of those isoenzymes in human exposure effects is questionable. CYP2E1 polymorphisms were associated with fibrosis in VC workers from Taiwan and possibly hemangiosarcoma at the Louisville plant (35, 36). However, due to the very high prevalence of TASH in the present study, it is unlikely that the CYP2E1 polymorphism played a critical role in the development of steatohepatitis. In a manner parallel to ethanol metabolism, chloroacetaldehyde is detoxified via an aldehyde dehydrogenase dependent pathway. In addition, both chloroacetaldehyde and chloroacetic acid appear to be substrates for glutathione S-transferases, with mercapturic acids and thiodiglycolic acid being the major excretion products. Thus, in both ethanol and vinyl chloride metabolism, reactive carbonyl intermediates are formed that may be critical for the formation of steatohepatitis. We believe that chloroacetaldehyde and chloracetic acid could be important mediators of TASH, just as acetaldehyde and acetate are important in the pathogenesis of alcoholic liver disease (37).
The classically described liver disease occurring in VC workers is hemangiosarcoma (18). In the present study, four subjects with TASH had concomitant hemangiosarcoma, and a fifth subsequently developed this tumor 7 years later. Therefore, all five subjects who either had or went on to develop hepatic hemangiosarcoma had TASH on their index liver biopsy. The carcinogenic mode of action for VC has historically been attributed to its genotoxicity (38). However, the potential contribution of the inflammatory lesion, TASH, on the development of VC-related hepatic hemangiosarcoma and hepatocellular carcinoma warrants further study.
There are several weaknesses inherent to this study. First, as in all steatohepatitis studies, it is reasonable to question if subjects truthfully reported their ethanol consumption. Because this study was a component of a larger employer-initiated liver cancer screening and surveillance project, a degree of under-reporting of alcohol use might be anticipated. However, even if all the subjects were heavy drinkers, the observed 80% prevalence of steatohepatitis is much higher would otherwise be expected. Furthermore, mean serum AST activity was normal in TASH, which is inconsistent with alcoholic hepatitis. Different serum cold storage times and the lack of liver biopsy in control subjects could influence the results of our serologic analysis. However, it must be noted that the healthy chemical worker control samples which are from the same era as the TASH samples have similar values to the modern day healthy unexposed controls for most analytes tested. This suggests that different cold storage times did not significantly influence our results. Furthermore, control subjects had normal mean serum CK-18 levels suggesting that they were, in fact, free from liver disease. Hepatitis B and C serologies were not performed due to limited sample volumes. However, neither the subjects’ medical histories nor their clinical/pathological data were consistent with viral hepatitis.
Toxicant-associated steatohepatitis is a unique clinically entity which appears to occur in specific groups of chemical workers where it is probably under-recognized as affected individuals may have normal liver enzymes. Future studies should be performed to more precisely determine the prevalence and natural history of TASH. The potential relationship between TASH and liver cancer, including both hemangiosarcoma and hepatocellular carcinoma, should be investigated.
Acknowledgments
Financial Support: This research was supported in part by the Sheila Sherlock Clinical and Translational Research Award in Liver Diseases from the American Association for the Study of Liver Diseases (M.C.), the National Institutes of Health Grant P30ES014443-01A1 (pilot project, M.C., C.M.), the National Institutes of Health Loan Repayment Program (M.C.), the University of Louisville Alcohol Research Center (1P01AA017103-01) (M.C., C.M.), and the Department of Veterans Affairs (M.C., C.M.).
The authors would like to acknowledge the Bioinformatics, Biostatistics & Computational Biology (BBCB) Facility Core of the University of Louisville Center for Environmental Genomics and Integrative Biology (CEGIB) and Lark Reynolds, manager of the U of L occupational hepatology database and specimen bank, for their assistance with statistical analysis and data/specimen acquisition respectively.
Abbreviations
- NAFLD
nonalcoholic fatty liver disease
- NASH
nonalcoholic steatohepatitis
- VC
vinyl chloride
- PVC
polyvinyl chloride
- FHH
focal hepatocytic hyperplasia
- FMH
focal mixed hyperplasia
- TASH
toxicant-associated steatohepatitis
- ppm
parts-per-million
- CERM
cumulative exposure rank month
- ppm-yr
parts-per-million-year
- BMI
body mass index
- NAS
NAFLD activity score
- TNFα
tumor necrosis factor α
- IL-1β
interleukin-1β
- IL-6
interleukin-6
- IL-8
interleukin-8
- MCP-1
macrophage chemoattractant protein-1
- CK-18
cytokeratin 18
References
- 1.Cave M, Deaciuc I, Mendez C, Song Z, Joshi-Barve S, Barve S, McClain C. Nonalcoholic fatty liver disease: predisposing factors and the role of nutrition. J Nutr Biochem. 2007;18:184–195. doi: 10.1016/j.jnutbio.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 2.Vauthey JN, Pawlik TM, Ribero D, Wu TT, Zorzi D, Hoff PM, Xiong HQ, et al. Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol. 2006;24:2065–2072. doi: 10.1200/JCO.2005.05.3074. [DOI] [PubMed] [Google Scholar]
- 3.Cotrim HP, De Freitas LA, Freitas C, Braga L, Sousa R, Carvalho F, Parana R, et al. Clinical and histopathological features of NASH in workers exposed to chemicals with or without associated metabolic conditions. Liver Int. 2004;24:131–135. doi: 10.1111/j.1478-3231.2004.0897.x. [DOI] [PubMed] [Google Scholar]
- 4.Day CP, James OF. Steatohepatitis: a tale of two “hits”? Gastroenterology. 1998;114:842–845. doi: 10.1016/s0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 5.Sass JB, Castleman B, Wallinga D. Vinyl chloride: a case study of data suppression and misrepresentation. Environ Health Perspect. 2005;113:809–812. doi: 10.1289/ehp.7716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kielhorn J, Melber C, Wahnschaffe U, Aitio A, Mangelsdorf I. Vinyl chloride: still a cause for concern. Environ Health Perspect. 2000;108:579–588. doi: 10.1289/ehp.00108579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Falk H, Creech JL, Jr, Heath CW, Jr, Johnson MN, Key MM. Hepatic disease among workers at a vinyl chloride polymerization plant. Jama. 1974;230:59–63. [PubMed] [Google Scholar]
- 8.Mastrangelo G, Fedeli U, Fadda E, Valentini F, Agnesi R, Magarotto G, Marchi T, et al. Increased risk of hepatocellular carcinoma and liver cirrhosis in vinyl chloride workers: synergistic effect of occupational exposure with alcohol intake. Environ Health Perspect. 2004;112:1188–1192. doi: 10.1289/ehp.6972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong RH, Chen PC, Du CL, Wang JD, Cheng TJ. An increased standardised mortality ratio for liver cancer among polyvinyl chloride workers in Taiwan. Occup Environ Med. 2002;59:405–409. doi: 10.1136/oem.59.6.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saurin JC, Taniere P, Mion F, Jacob P, Partensky C, Paliard P, Berger F. Primary hepatocellular carcinoma in workers exposed to vinyl chloride: a report of two cases. Cancer. 1997;79:1671–1677. doi: 10.1002/(sici)1097-0142(19970501)79:9<1671::aid-cncr6>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 11.Tamburro CH, Makk L, Popper H. Early hepatic histologic alterations among chemical (vinyl monomer) workers. Hepatology. 1984;4:413–418. doi: 10.1002/hep.1840040310. [DOI] [PubMed] [Google Scholar]
- 12.Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55:434–438. [PubMed] [Google Scholar]
- 13.Hsiao TJ, Wang JD, Yang PM, Yang PC, Cheng TJ. Liver fibrosis in asymptomatic polyvinyl chloride workers. J Occup Environ Med. 2004;46:962–966. doi: 10.1097/01.jom.0000137722.66767.38. [DOI] [PubMed] [Google Scholar]
- 14.Maroni M, Fanetti AC. Liver function assessment in workers exposed to vinyl chloride. Int Arch Occup Environ Health. 2006;79:57–65. doi: 10.1007/s00420-005-0018-y. [DOI] [PubMed] [Google Scholar]
- 15.Maroni M, Mocci F, Visentin S, Preti G, Fanetti AC. Periportal fibrosis and other liver ultrasonography findings in vinyl chloride workers. Occup Environ Med. 2003;60:60–65. doi: 10.1136/oem.60.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saad AA, el-Sewedy SM, Bader GA, Mousa SM, Mahdy MM. Biochemical effects of vinyl chloride monomer on the liver of occupationally exposed workers. East Mediterr Health J. 2000;6:979–986. [PubMed] [Google Scholar]
- 17.Ho SF, Phoon WH, Gan SL, Chan YK. Persistent liver dysfunction among workers at a vinyl chloride monomer polymerization plant. J Soc Occup Med. 1991;41:10–16. doi: 10.1093/occmed/41.1.10. [DOI] [PubMed] [Google Scholar]
- 18.Creech JL, Jr, Johnson MN. Angiosarcoma of liver in the manufacture of polyvinyl chloride. J Occup Med. 1974;16:150–151. [PubMed] [Google Scholar]
- 19.Dannaher CL, Tamburro CH, Yam LT. Occupational carcinogenesis: the Louisville experience with vinyl chloride-associated hepatic angiosarcoma. Am J Med. 1981;70:279–287. doi: 10.1016/0002-9343(81)90763-4. [DOI] [PubMed] [Google Scholar]
- 20.Lewis R. Vinyl Chloride and Polyvinyl Chloride. In: Lewis R, editor. Occupational Medicine: State of the Art Reviews, Health Issues in the Plastics and Rubber Industries. 4. Vol. 14. Philadelphia: Hanley & Belfus, Inc; 1999. pp. 719–742. [PubMed] [Google Scholar]
- 21.Greenberg RA, Tamburro CH. Exposure indices for epidemiological surveillance of carcinogenic agents in an industrial chemical environment. J Occup Med. 1981;23:353–358. [PubMed] [Google Scholar]
- 22.Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999;94:2467–2474. doi: 10.1111/j.1572-0241.1999.01377.x. [DOI] [PubMed] [Google Scholar]
- 23.Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, Ferrell LD, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321. doi: 10.1002/hep.20701. [DOI] [PubMed] [Google Scholar]
- 24.Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, Kitzmiller J, et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26:3160–3167. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- 25.Carithers RI, McClain CJ. Alcoholic Liver Disease. In: Feldman M, Freidman LS, Brant LJ, editors. Sleisenger & Fordtran’s Gastrointestinal and Liver Disease. Vol. 2. Philadelphia: Elsevier; 2006. pp. 1771–1792. [Google Scholar]
- 26.Clark JM. The epidemiology of nonalcoholic fatty liver disease in adults. J Clin Gastroenterol. 2006;40 (Suppl 1):S5–10. doi: 10.1097/01.mcg.0000168638.84840.ff. [DOI] [PubMed] [Google Scholar]
- 27.Cotrim HP, Andrade ZA, Parana R, Portugal M, Lyra LG, Freitas LA. Nonalcoholic steatohepatitis: a toxic liver disease in industrial workers. Liver. 1999;19:299–304. doi: 10.1111/j.1478-3231.1999.tb00053.x. [DOI] [PubMed] [Google Scholar]
- 28.Michailova A, Kuneva T, Popov T. A comparative assessment of liver function in workers in the petroleum industry. Int Arch Occup Environ Health. 1998;71 (Suppl):S46–49. [PubMed] [Google Scholar]
- 29.Perez CA, Bosia JD, Cantore MS, Chiera A, Cocozzella DR, Adrover RE, Borzi S, et al. Liver damage in workers exposed to hydrocarbons. Gastroenterol Hepatol. 2006;29:334–337. doi: 10.1157/13089716. [DOI] [PubMed] [Google Scholar]
- 30.Wieckowska A, Zein NN, Yerian LM, Lopez AR, McCullough AJ, Feldstein AE. In vivo assessment of liver cell apoptosis as a novel biomarker of disease severity in nonalcoholic fatty liver disease. Hepatology. 2006;44:27–33. doi: 10.1002/hep.21223. [DOI] [PubMed] [Google Scholar]
- 31.Hefner RE, Jr, Watanabe PG, Gehring PJ. Preliminary studies on the fate of inhaled vinyl chloride monomer (VCM) in rats. Environ Health Perspect. 1975;11:85–95. doi: 10.1289/ehp.751185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bolt HM. Vinyl chloride-a classical industrial toxicant of new interest. Crit Rev Toxicol. 2005;35:307–323. doi: 10.1080/10408440490915975. [DOI] [PubMed] [Google Scholar]
- 33.Rannug U, Gothe R, Wachtmeister CA. The mutagenicity of chloroethylene oxide, chloroacetaldehyde, 2-chloroethanol and chloroacetic acid, conceivable metabolites of vinyl chloride. Chem Biol Interact. 1976;12:251–263. doi: 10.1016/0009-2797(76)90041-7. [DOI] [PubMed] [Google Scholar]
- 34.Guengerich FP, Kim DH, Iwasaki M. Role of human cytochrome P-450 IIE1 in the oxidation of many low molecular weight cancer suspects. Chem Res Toxicol. 1991;4:168–179. doi: 10.1021/tx00020a008. [DOI] [PubMed] [Google Scholar]
- 35.Hsieh HI, Chen PC, Wong RH, Wang JD, Yang PM, Cheng TJ. Effect of the CYP2E1 genotype on vinyl chloride monomer-induced liver fibrosis among polyvinyl chloride workers. Toxicology. 2007;239:34–44. doi: 10.1016/j.tox.2007.06.089. [DOI] [PubMed] [Google Scholar]
- 36.Antonino-Green D, Linder MW, Fortwengler P, Looney S, Geoghegan TE, Valdes RJ. Cytochrome P4502E1 polymorphism and glutathione S-transferase genotypes are linked to vinyl chloride-induced angiosarcoma [abstract] Proc Am Assoc Canc Res. 2000:41. [Google Scholar]
- 37.Mello T, Ceni E, Surrenti C, Galli A. Alcohol induced hepatic fibrosis: role of acetaldehyde. Mol Aspects Med. 2008;29:17–21. doi: 10.1016/j.mam.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 38.Dogliotti E. Molecular mechanisms of carcinogenesis by vinyl chloride. Ann Ist Super Sanita. 2006;42:163–169. [PubMed] [Google Scholar]