Abstract
Context
Children at end of life often lack access to hospice care at home or in a dedicated facility. The factors that may influence whether or not hospices provide pediatric care are relatively unknown.
Objectives
The purpose of this study was to understand the institutional and resource factors associated with provision of pediatric hospice care.
Methods
This study used a retrospective, longitudinal design. The main data source was the 2002 to 2008 California State Hospice Utilization Data Files. The sample size was 311 hospices or 1368 hospice observations over seven years. Drawing on institutional and resource dependence theory, this study used generalized estimating equations to examine the institutional and resource factors associated with provision of pediatric hospice care. Interaction terms were included to assess the moderating effect of resource factors on the relationship between institutional factors and provision of care.
Results
Membership in professional groups increased the probability (19%) of offering hospice services for children. Small- (−22%) and medium-sized (−11%) hospices were less likely to provide care for children. The probability of providing pediatric hospice care diminished (−23%) when competition increased in the prior year. Additionally, small size attenuated the accreditation-provision relationship and medium size magnified the membership-provision relationship.
Conclusion
Professional membership may promote conformity to industry standards of pediatric care and remove the unknowns of providing hospice care for children. Hospices, especially medium-sized hospices, interested in developing or expanding care for children may benefit by identifying a pediatric champion to join a professional group.
Keywords: Children, hospice care, hospice organizations, GEE, end of life
Introduction
The national debate about health care reform and the Patient Protection and Affordable Care Act of 2010 sparked a surge of interest in how our society and health care systems provide care for the terminally ill (1). Although the debate has focused on the elderly (e.g., fictitious “death panels”), terminally ill children also face a real and immediate problem accessing appropriate care at the end of life (2). Recent studies have demonstrated that hospice care provides physical and psychosocial benefits for children and their families (3–4). Despite the potential value of hospice care for children, it is estimated that approximately 90% of children who may benefit from hospice services never receive it, and as few as 40% of community-based hospices provide care to children (5–6).
A number of factors are related to whether or not terminally ill children receive hospice care, including family acceptance of the child’s limited life expectancy, clinician referrals to hospice, and state and federal health reimbursement policies (7–8). Obtaining hospice care may also depend on whether or not hospices provide care for children. However, we are just beginning to understand what influences hospices to provide pediatric hospice care (9). In particular, hospices are influenced by the institutional nature of the hospice industry. For example, hospices are often pressured to conform to the rules, regulations, norms, and beliefs about providing end-of-life care by key stakeholders such as the Centers for Medicare and Medicaid Services (10–12). At the same time, hospices face resource constraints that influence their ability to provide hospice care. For example, hospices commonly rely on private donations to subsidize care for high-cost patient populations, particularly children (13). Without these funding sources, hospices may not have the resources to provide pediatric hospice care. In addition, hospices that lack sufficient resources may respond differently to institutional pressures (14). This dynamic tension between institutional and resource pressures may be critical in whether or not hospice care is ultimately provided for children. In the current economic recession, as an example, many hospices are reacting to the changing economy and modifying service provision as a means to maintain and enhance resource flows, often contrary to institutional pressures (15). Understanding the relationships between institutional and resource influences and provision of pediatric hospice care is important, if providing hospice care for children is to expand. Therefore, the purpose of this study was to examine the associations among institutional and resource factors and the provision of pediatric hospice care.
Conceptual Framework
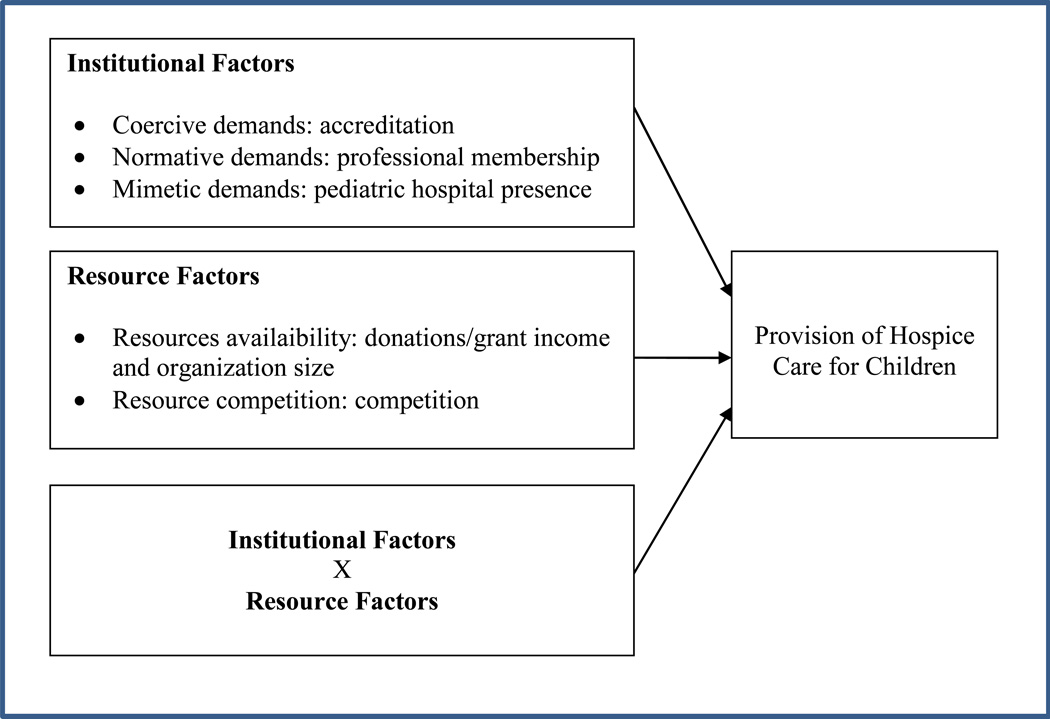
This study was guided by institutional and resource dependence theories (Fig. 1). The main assumption of institutional theory is that organizations operate in an institutional environment that is composed of rules, laws, professional standards, beliefs, and values (16). Organizations must conform to this environment in order to gain legitimacy and survive. There are three types of institutional demands that hospices face: coercive, normative, and mimetic pressures (17). Coercive demands are pressures exerted by key regulatory stakeholders that require organizations to comply with rules and regulations of the industry (e.g., accreditation). Normative demands are pressures to comply with professional standards and are enforced through a sense of social obligation (e.g., membership in a professional group). Mimetic demands are pressures to imitate the behavior of other organizations. In an environment with increasing uncertainty, copying provision of care practices provides organizations with a reference for modeling what works elsewhere (e.g., pediatric hospital).
Figure 1.
Conceptual framework for institutional and resources factors associated with the provision of hospice care services for children.
Resource dependence theory emphasizes that organizations do not have all the internal resources and capabilities necessary for survival, so they must develop exchange relationships with other entities (18). Organizations actively strive to minimize their dependence on resource holders and gain control of resources for their survival. An organization's ability to lessen its dependence is influenced by resource availability and competition (18). For example, the availability of financial resources from donations and grants may allow hospices to generate a financial buffer in case of resource constraints. Additionally, competition plays an important role. The more competitive the environment is, the greater the strains on the shared pool of resources; survival depends on how organizations outcompete competitors (18).
Finally, the literature suggests that resource factors may moderate the relationship between institutional factors and provision of care (14). Resource constraints may diminish the influence of rules, regulations, norms, and values imposed on hospices to provide hospice care to children. Conversely, a lack of resources may intensify the relationship between institutional factors and provision of hospice care for children because hospices would need to creatively respond to the demands of institutional stakeholder to provide pediatric care. As a result, hospices' response to conflicting institutional and resource demands may affect whether or not care is provided for children.
Methods
Study Design and Sample
This study used a longitudinal, retrospective design to assess relationships among institutional and resource factors and the provision of hospice care for children. The sample was drawn from hospices in California from 2002 to 2008. After inclusion (i.e., an active hospice program licensure) and exclusion (i.e., unknown business entity status, duplicate entry, or lack of patient or financial data) criteria were applied, the sample size was 1368 hospice/year observations over seven years.
Data Sources
The data for this study were derived from multiple sources. The main source was the 2002 to 2008 California Office of Statewide Health Planning and Development’s (CA OSHPD) State Utilization Data File of Home Health Agencies and Hospice Facilities. The data files contained information on hospice agency demographics and financial performance. Participation in the annual CA OSHPD survey is mandatory for licensed hospice and home health agencies. The study also used the Children’s Hospice and Palliative Care Coalition’s (CHPCC) membership list, the National Association of Children's Hospitals and Related Institutions’ (NACHRI) Hospital Directory, the California Department of Finance’s California Income Data reports, the California Employment Development Department’s Monthly Labor Forces Data for Counties, and the California Department of Public Health’s Death Statistical Data Files.
Measures
Dependent Variable
Provision of care for children was defined as providing community-based hospice care. This variable, derived from the CA OSHPD data set, was measured as whether a hospice provided care for children less than one year old to 20 years old in a 12-month period.
Independent Variables
A group of independent variables was composed of institutional factors drawn from the constructs of institutional theory. As a measure of coercive demands, accreditation was defined as whether or not a hospice was accredited by the Accreditation Commission for Health Care (ACHC), the Community Health Accreditation Program (CHAP), the Joint Commission, and/or other accrediting agencies. Professional membership in a coalition was used to capture normative demands. A binary measure of whether or not a hospice was a member of the CHPCC was created. This variable was constructed by manually reviewing the CHPCC membership list and matching the membership list with the CA OSHPD list of hospices. Mimetic demands were characterized by a pediatric hospital presence in the community, which was considered a source from which hospices could copy pediatric care practices. It was defined as whether or not a hospice had a pediatric hospital in their county and was measured using the hospital addresses from the NACHRI directory and matching them with the hospices’ county locations in the CA OSHPD database.
A second group of independent variables was composed of resource pressures drawn from the major constructs of resource dependence theory. Donation/grant income was used as a variable to represent the availability of external resources. The variable was defined as whether or not the hospice organization had any donation, grant, unrelated business, or other income in a 12-month period. The availability of internal resources was captured by organization size. Using a hospice industry formula (20), hospices were categorized as small (≤ 25 patients/day), medium (26 to 100 patients/day), and large (≥ 101 patients/day). To measure competition, we constructed the Herfindahl-Hirshman Index (HHI), operationalized as distribution of market share among hospices in a county (dividing the total number of all patient days for each hospice by the total number of hospice patients days in each county, and then summing up the square of the proportion for each hospice in the county). The HHI indicates the degree of concentration in the market, so we reversed it (i.e., 1 - HHI) to measure the degree of competition in the hospice market.
To control for other factors likely related to the provision of hospice care for children, organizational factors (i.e., service area, agency type, ownership, and organizational age) and market factors (i.e., per capita income, unemployment, and child mortality) also were included in the analysis.
Data Analysis
Standard descriptive statistics for all study variables were calculated to identify anomalies in the data and to ensure that the assumptions of all analyses were met. The means, percentiles, minimums, maximums, and standard deviations were used to describe sample characteristics.
Multivariate logistic generalized estimating equations (GEEs) were used to model the direct and moderating effects of repeated observations on hospice organizations over seven years (19). The model specifications included a binomial variance function, logit link function, and unstructured working correlation structure. The results are reported as average marginal effects and odds ratios. To reduce endogeneity, all independent and control variables were lagged by one year (20). As a result of the lag, there was a reduction in the sample size used in the GEE analysis (N = 1036 vs. N = 1368). To examine the moderating effect of resource factors on the relationship between institutional factors and provision of pediatric hospice care, we interacted resource and institutional factors. Using a series of steps, blocks of variables were entered into the moderating model as recommended by Baron and Kenny (21). The first step was to enter the control variables (control model), followed by the predictor variables (main effect model), and then the interaction terms (moderation model). Results were reported as odds ratios and average marginal effects. The discussion refers to results from the main effect and moderation models, unless otherwise indicated. If a significant interaction existed, the interpretation of the moderating effect was facilitated by plotting the regression lines in this nonlinear model (22). All analyses were conducted using Stata 11.0 software (Statacorp LP, College Station, TX).
Results
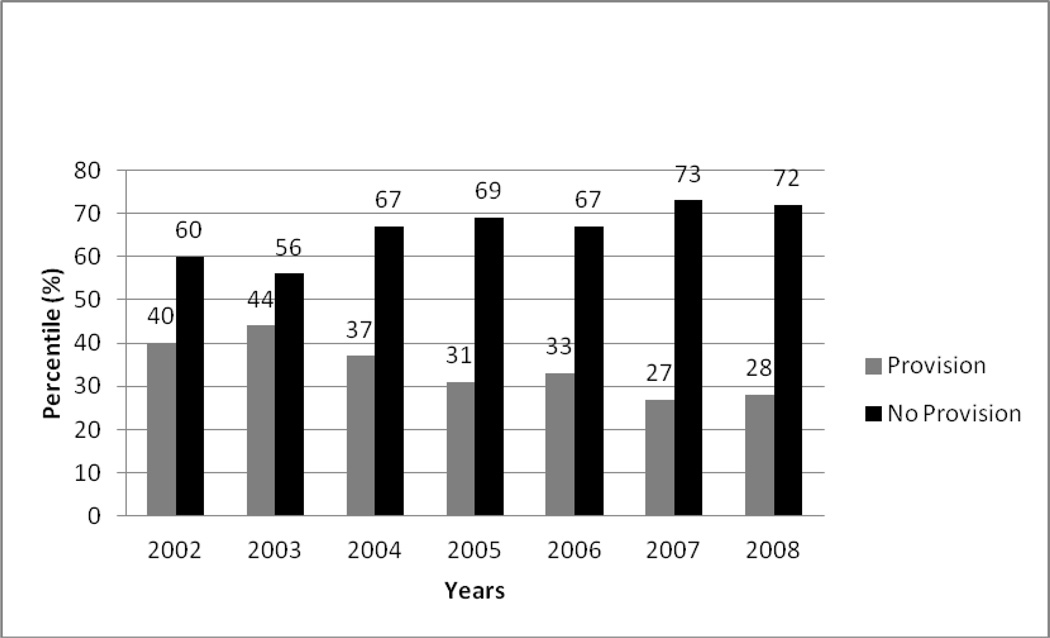
The characteristics of the sample are presented in Table 1. Slightly more than a third of the sample provided pediatric hospice care during the study time frame. The percentage of hospices providing care for children declined from 40% in 2002 to 28% in 2008 (Fig. 2). Less than half of the hospices (46.5%) were accredited by the ACHC, CHAP, Joint Commission, or other accrediting agencies. Additionally, few hospices (17.3%) were members of a professional pediatric end-of-life coalition. A majority of hospices (58.2%) had a pediatric hospital in their community. More than half of the organizations did not have access to other income in the form of grants, donations, or unrelated business revenue. Most hospices were medium sized with 26 to 100 patients/days. The level of competition, as determined by the HHI, was 0.72, indicating a relatively competitive market (range = 0 [monopoly] to 1.0 [extremely competitive]).
Table 1.
Characteristics of the Sample (N = 1368)
| Variable | Percentage/ Mean |
Standard Deviation |
Minimum | Maximum |
|---|---|---|---|---|
| Dependent Variable | ||||
| Provision of hospice care for children | 33.6% | --- | 0.00 | 1.00 |
| Independent Variables | ||||
| Institutional Factors | ||||
| Accreditation | 46.5% | --- | 0.00 | 1.00 |
| Professional membership | 17.3% | --- | 0.00 | 1.00 |
| Pediatric hospital presence | 58.2% | --- | 0.00 | 1.00 |
| Resource Factors | ||||
| No donation/grant income | 56.1% | --- | 0.00 | 1.00 |
| Organization size | ||||
| Small | 34.7% | --- | 0.00 | 1.00 |
| Medium | 47.7% | --- | 0.00 | 1.00 |
| Large | 17.6% | --- | 0.00 | 1.00 |
| Competition | 0.72 | 0.28 | 0.00 | 0.96 |
| Control Variables | ||||
| Organizational Factors | ||||
| Service Area | ||||
| Urban service area | 60.3% | --- | 0.00 | 1.00 |
| Rural service area | 8.9% | --- | 0.00 | 1.00 |
| Mixed service area | 30.8% | --- | 0.00 | 1.00 |
| Agency type | ||||
| Freestanding | 64.4% | --- | 0.00 | 1.00 |
| Hospital-based | 15.0% | --- | 0.00 | 1.00 |
| Home health-based | 17.5% | --- | 0.00 | 1.00 |
| Long -term care-based | 3.1% | --- | 0.00 | 1.00 |
| Ownership | ||||
| For profit | 52.2% | --- | 0.00 | 1.00 |
| Government | 5.3% | --- | 0.00 | 1.00 |
| Nonprofit | 42.5% | --- | 0.00 | 1.00 |
| Organizational age | 9.22 | 8.12 | 1.00 | 42.00 |
| Market Factors | ||||
| Per capita income ($000) | 36.1 | 9.6 | 18.80 | 86.10 |
| Unemployment | 0.06 | 0.02 | 3.00 | 22.00 |
| Child mortality | 0.02 | 0.01 | 0.00 | 11.00 |
Figure 2.
Provision of hospice care for children from 2002 to 2008.
Most hospices provided services in urban communities (60.3%). Freestanding hospices were the most common (64.4%), and over half of the hospices were for-profit (52.2%). On average, hospices were nine years old, with a range from one year for hospices that had just started operations to 42 years for long-standing hospices. Hospices operated in counties with an average per capita income of $36,141, and the average annual unemployment rate was 6%. Although the average child mortality rate in the counties was 2%, some counties experienced no mortalities, and the rate in some counties was as high as 11%.
The results of the multivariate GEE analysis are presented in Table 2. Among the institutional factors (main effect model), professional membership was significantly related to provision of pediatric hospice care. Relative to non-members, members of a professional group had an increased probability (19%) of providing hospice services for children. Accreditation and pediatric hospital presence had no significant association with the provision of pediatric hospice care.
Table 2.
The Effects of Institutional and Resource Factors on the Provision of Hospice Care for Children (N = 1036)
| Step 1 (Control Model) |
Step 2 (Main Effect Model) |
Step 3 (Moderation Model) |
||||
|---|---|---|---|---|---|---|
| OR (SE) | AME | OR(SE) | AME | OR(SE) | AME | |
| Control Variables | ||||||
| Organizational Factors | ||||||
| Service Area | ||||||
| Urban service area | (ref) | (ref) | (ref) | (ref) | (ref) | (ref) |
| Rural service area | 0.71 (0.21) | −0.07 | 0.53 (0.20) | −0.11 | 0.50 (0.20) | −0.12 |
| Mixed service area | 1.16 (0.28) | 0.03 | 1.02 (0.26) | 0.01 | 1.02 (0.27) | 0.01 |
| Agency Type | ||||||
| Freestanding | (ref) | (ref) | (ref) | (ref) | (ref) | (ref) |
| Hospital-based | 0.52 (0.14) | −0.13a | 0.63 (0.17) | −0.08 | 0.61 (0.18) | −0.08 |
| Home health-based | 0.71 (0.19) | −0.07 | 0.81 (0.24) | −0.04 | 0.78 (0.23) | −0.04 |
| Long-term care-based | 0.51 (0.18) | −0.13 | 0.33 (0.21) | −0.19 | 0.24 (0.19) | −0.24 |
| Ownership | ||||||
| For profit | (ref) | (ref) | (ref) | (ref) | (ref) | (ref) |
| Government | 1.05 (0.44) | 0.01 | 1.23 (0.53) | 0.04 | 1.09 (0.46) | 0.02 |
| Nonprofit | 1. 96 (0.54) | 0.13 a | 1.81 (0.52) | 0.10 a | 1.91 (0.60) | 0.11 a |
| Organizational Age | 1.80 (0.26) | 0.12 b | 1.42 (0.21) | 0.06 a | 1.28 (0.20) | 0.04 |
| Market Factors | ||||||
| Per capita income | 0.99 (0.02) | −0.01 | 0.98 (0.02) | −0.01 | 0.98 (0.02) | −0.01 |
| Unemployment | 1.08 (0.07) | 0.01 | 1.05 (0.07) | 0.01 | 1.05 (0.07) | 0.01 |
| Child mortality | 0.93 (0.11) | −0.01 | 0.96 (0.09) | −0.01 | 0.95 (0.10) | −0.01 |
| Year 2003 | 0.61 (0.11) | −0.10 c | 0.58 (0.12) | −0.10 c | 0.58 (0.12) | −0.09 c |
| Year 2004 | 0.50 (0.10) | −0.14 b | 0.45 (0.10) | −0.14b | 0.44 (0.11) | −0.14 b |
| Year 2005 | 0.61 (0.12) | −0.10 a | 0.55 (0.11) | −0.11 c | 0.56 (0.13) | −0.10 a |
| Year 2006 | 0.56 (0.13) | −0.12a | 0.52 (0.13) | −0.12 c | 0.53 (0.14) | −0.11 a |
| Year 2007 | 0.54 (0.12) | −0.12 c | 0.52 (0.13) | −0.12 c | 0.53 (0.13) | −0.11 a |
| Independent Variables | ||||||
| Institutional Factors | ||||||
| Accreditation | 0.85 (0.15) | −0.03 | 0.22 (0.16) | −0.04 a | ||
| Professional membership | 2.63 (0.72) | 0.19 b | 1.03 (1.20) | 0.18 | ||
| Pediatric hospital presence | 0.89 (0.27) | −0.02 | 2.28 (3.50) | −0.04 | ||
| Resource Factors | ||||||
| No donation/grant income | 0.80 (0.14) | −0.04 | 0.78 (0.26) | −0.04 | ||
| Organization size | ||||||
| Large | (ref) | (ref) | (ref) | (ref) | ||
| Small | 0.27 (0.09) | −0.22 b | 0.10 (0.06) | −0.22 b | ||
| Medium | 0.53 (0.14) | −0.11 a | 0.33 (0.15) | −0.12 a | ||
| Competition | 0.28 (0.16) | −0.23 a | 0.23 (0.22) | −0.25 | ||
| Interactions | ||||||
| No other income × accreditation | 1.08 (0.33) | |||||
| No other income × membership | 0.76 (0.28) | |||||
| No other income × pediatric hospital | 1.07 (0.35) | |||||
| Small size × accreditation | 6.76 (3.50) b | |||||
| Medium size × accreditation | 1.29 (0.52) | |||||
| Small size × membership | 2.20 (2.30) | |||||
| Medium size × membership | 2.83 (1.50) a | |||||
| Small size × pediatric hospital | 0.59 (0.38) | |||||
| Medium size × organization leader | 1.05 (0.48) | |||||
| Competition × accreditation | 2.96 (2.40) | |||||
| Competition × membership | 1.67 (2.20) | |||||
| Competition × pediatric hospital | 0.24 (0.43) | |||||
OR = odds ratio; SE = standard error; AME = average marginal effect.
P<0.05.
P<0.001.
P<0.01.
The analysis of the resource factors (main effect model) revealed that organizational size and competition were significantly associated with the provision of pediatric care. Compared to large hospices, small-sized (−22%) and medium-sized (−11%) hospices were less likely to provide hospice for children. Additionally, the probability of providing pediatric hospice care diminished (−23%) when competition increased in the prior year. A lack of donation/grant income did not significantly predict the provision of hospice care for children.
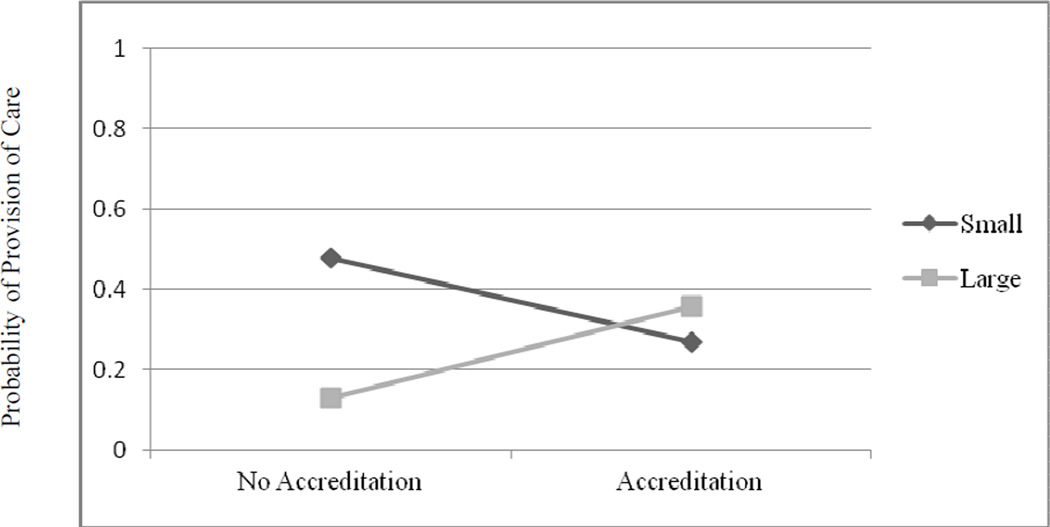
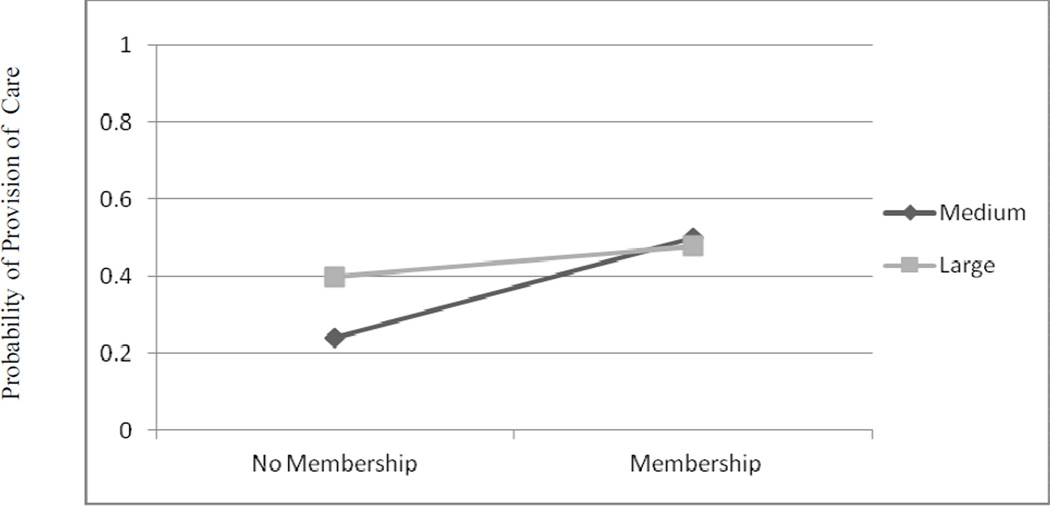
Table 2 also illustrates the influence of resource and institutional interactions (moderation model) on the provision of pediatric hospice care. Although some of the coefficients on the interaction terms were statistically significant (i.e., accreditation and small size, professional membership and medium size), interpretation of the statistical significance and sign of the interaction terms in nonlinear models is difficult because they are not necessarily indicative of an interaction. As a result, the accreditation-small size and professional membership-medium size relationships were examined graphically (22). Figure 3 shows that small organizational size did attenuate the relationship between accreditation and the provision of hospice care for children. Figure 4 demonstrates that instead of attenuating the provision of hospice care for children, professional membership promoted it among medium-sized hospices.
Figure 3.
Plot of the interaction between accreditation and small-sized organizations on the provision of hospice care for children.
Figure 4.
Plot of the interaction between organizational membership and medium-sized hospices on the provision of care for children.
Discussion
Our analysis suggests that the percentage of hospices that provided pediatric care in California significantly declined from 2002 to 2008 and that several institutional and resource factors are associated with whether or not hospices provide pediatric hospice services. From the perspective of institutional theory, we found that membership in a professional group was associated with the provision of pediatric hospice care. Several studies (10, 23–24) have suggested that the training, networking opportunities, and policy updates offered to members of a professional group may encourage organizations to provide care for special populations such as children. There is also a possibility that hospices caring for children may seek out professional membership to support them in their effort. Through membership, organizations also may develop an understanding of what is valued and expected in providing hospice care for children. As a result, membership in a professional group may remove the unknowns of providing hospice care for children and promote conformity to professional standards and available guidelines for pediatric hospice care. Our finding suggest that although coercive and mimetic institutional pressures have little influence on providing pediatric hospice care, the normative power of the professional membership may motivate hospices to comply with professional standards and guidelines that recommend providing care for children.
There were other interesting findings from our analysis regarding resource factors. Similar to other hospice studies, we found that whether or not hospices provided pediatric hospice care depended on organizational size (25–26). Small- and medium-sized hospices may not have all the internal resources and capabilities necessary to provide care for children. These organizations also may lack the financial or physical assets (e.g., property, facilities, and equipment), human capital, technology, or other organizational resources needed to offer pediatric medication, equipment, supplies, and trained nursing care (27–28). To explore this further, we conducted a post-hoc analyses comparing the average medication, equipment, and medical supply expenses of small, medium, and large hospices and found that small- and medium-sized hospices had fewer resource expenses than large hospices. Thus, small- and medium-sized hospices may be influenced in their provision of pediatric care by the type and intensity of resources required.
This study also revealed that operating in competitive environments affected whether or not a hospice provided pediatric services. The negative influence of competition on the provision of care for children may be because providing expensive hospice care to children draws critical financial and human resources from the main focus of the hospices’ business (29). Hospice care for the elderly represents an important revenue stream because of Medicare funding and the potential for extended lengths of stay in hospice (13). Hospices generally compete among themselves for these admissions. In highly competitive markets, hospices may allocate financial and human resources to marketing for and providing additional services (e.g., Meals-on-Wheels) aimed at attracting elderly patients (13). Services that do not contribute to the business’s main focus, such as providing hospice care for children, may be perceived by hospice administrators as a drain on resources that creates a competitive disadvantage. These findings suggest that increased competition may draw critical resources away from providing hospice care for children.
Several of the findings about the moderating role of resource factors are also worth noting. We found that small organizational size did attenuate the relationship between accreditation and the provision of hospice care for children. This finding was congruent with other researchers (14), suggesting that small organizations experiencing resource constraints may be less likely to provide services even in the presence of institutional standards (14). An explanation for this stems from the nature of accreditation in the health care field. Accreditation requires hospices to have established and prescribed infrastructures, policies, procedures, and requirements for the provision of care, treatment, and services (30–31); however, accrediting agencies can only remove accreditation if a hospice does not meet its standards. There are no legal or financial sanctions for noncompliance such as fines or fees. Furthermore, most hospices already meet the Medicare and Medicaid hospice certification guidelines and often question the value of accreditation (13, 32). Therefore, the lack of meaningful sanctions related to accreditation may make it easier for administrators in small hospices to decide not to provide care for children.
Contrary to expectations, the association between professional membership and the provision of hospice care for children increased in medium-sized organizations. Membership in a pediatric end-of-life professional group may provide these medium-sized hospices with an opportunity to network and obtain knowledge about pediatric end of life (33). Medium-sized hospices may be able to respond faster and with more flexibility to information from such professional groups than smaller or larger hospices (13, 34). Our finding suggests that membership in those groups may not act as a normative pressure on hospices to provide care for children but rather as a social network of critical support and guidance on issues of caring for children at the ends of their lives. Future research design should explore and clarify the role of professional membership in hospice decision making.
This study had several limitations. The first limitation relates to omitted variable bias. The study did not control for every institutional, resource, organizational, or market factor that may have affected the provision of hospice care for children. For example, staff caseload could be a critical factor in whether or not hospices provide care for children, because children often require additional staff resources during their hospice admissions (8). However, efforts were made to capture as much information about practice and environmental influences as possible within the constraints of available secondary databases. Another limitation is that our findings are generalizable only to community-based hospices in the state of California during the study time frame. However, California has historically been a leader in hospice care and has health care policies and patterns that are influential in the national arena (25, 35). In addition, California often implements new and emerging health care services before they are adopted in other states.
Despite its drawback, the findings of this study have implications for hospice professionals and policy makers interested in developing or expanding pediatric hospice care services. Hospices may benefit from identifying a pediatric hospice champion in the organization who will connect with a professional group. The role of a champion is generally to shape organizational change by protecting those involved in the implementation of change, building organizational support for the change, facilitating the use of organizational resources, and encouraging the growth of an organizational network that supports the implementation of change (36). The importance of a champion is well documented in the quality improvement literature (37). However, there is emerging evidence that champions also may be effective in fostering change in health care practices such as providing care for children (38–39). In fact, recent studies have found that although a champion may be effective in implementing smaller changes like adopting new technology, more than one champion is often needed for changes in organizational behavior (40–41). Therefore, hospices may benefit from identifying multiple pediatric champions within their organizations. Future research might explore the relationship between champions who join a professional group and the provision of hospice care for children.
Additionally, the finding that accreditation was not related to the provision of pediatric hospice care underscores the need to incorporate pediatric hospice standards of care as part of the accreditation process. This study raises concern that pediatric hospice care is not evaluated by accrediting agencies. In fact, during the study time frame, there were no industry standards for pediatric hospice care (42). They only recently have been introduced by the National Hospice and Palliative Care Organization and are now available for voluntary adoption. Although hospice associations are often instrumental in suggesting industry standards to accrediting agencies (13), pediatric standards have not been adopted by accrediting agencies. Therefore, drawing upon the long-standing collaboration between hospice associations and accrediting agencies and based on the findings of this study, hospice associations may play an important role and be a driving force that advocates for pediatric standards to be adopted by accrediting agencies.
Conclusion
The goal of this study was to understand the institutional and resource factors that influence hospices to provide pediatric care. This is one of the first studies to provide evidence that over a relatively short period of time (2002–2008), terminally ill children and their families encountered substantial changes in the availability of hospice care. The number of hospices grew during the study time frame, but the proportion of hospices providing care for children significantly diminished. The findings from this study beg the larger question of whether or not hospices should provide care for children in light of their resource challenges. If hospices choose not to provide care to children, they risk violating the hospice mission and damaging the reputation of hospices as a place where end-of-life care is delivered to all in need regardless of age, race, gender, and illness type. Once community-based hospices decide not to provide care for children, what category of patients will be next? Indeed, this slippery slope has the potential to contribute to the disparities already present in end-of-life care (2). However, should hospices choose to provide care or expand services for children, institutional and resource factors might be modifiable at the organizational level (e.g., identifying a champion) and at the policy level (e.g., introducing pediatric standards into the accreditation process). Additionally, by engaging in care for children, hospices become an integral part of the pediatric health care system and contribute in a meaningful way to the care continuum as children transition through their disease trajectory (13). Additional studies that develop our understanding of the role of hospices in the provision of care for children are clearly warranted, and as the science progresses, further inquiries into interventions aimed at improving the provision of hospice care for children are needed, if access to and the quality of end-of-life care for terminally ill children and their families are to improve.
Acknowledgements
This research was supported by grants from the National Institute of Nursing Research (T32NR008856), Agency for Healthcare Research and Quality (1R36HS020164-01), and the Alpha Alpha Chapter of Sigma Theta Tau. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research, National Institutes of Health, or Agency for Healthcare Research and Quality.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
A portion of this article was presented as a poster at the 2011 National Institute of Nursing Research Science of Compassion: Future Directions in End of Life and Palliative Care Conference, Bethesda, Maryland, August 21, 2011.
Disclosures
The authors declare no conflicts of interest.
References
- 1.The White House. The White House: President Barack Obama. [Accessed December 30, 2009];2009 Available from http://www.whitehouse.gov.libproxy.lib.unc.edu/.
- 2.Institute of Medicine. When children die. Washington, DC: National Academies Press; 2003. [Google Scholar]
- 3.Davies B, Steele R, Collins JB, Cook K, Smith S. The impact on families of respite care in a children's hospice program. J Palliat Care. 2004;20:277–286. [PubMed] [Google Scholar]
- 4.Dickens DS. Comparing pediatric deaths with and without hospice support. Pediatr Blood Cancer. 2010;54:746–750. doi: 10.1002/pbc.22413. [DOI] [PubMed] [Google Scholar]
- 5.ChiPPS. A call for change: Recommendations to improve the care of children living with life-threatening conditions. Alexandria, VA: National Hospice and Palliative Care Organization; 2001. [Google Scholar]
- 6.Sanchez-Varela A, Deal A, Hanson L, et al. Barriers to hospice for children as perceived by hospice organizations in North Carolina. Am J Hosp Palliat Care. 2012;29(3):171–176. doi: 10.1177/1049909111412580. [DOI] [PubMed] [Google Scholar]
- 7.Dabbs D, Butterworth L, Hall E. Tender mercies: increasing access to hospice services for children with life-threatening conditions. Am J Mat Child Nurs. 2007;32:311–319. doi: 10.1097/01.NMC.0000288003.10500.00. [DOI] [PubMed] [Google Scholar]
- 8.Davies B, Sehring SA, Partridge J, et al. Barriers to palliative care for children: perceptions of pediatric health care providers. Pediatrics. 2008;121:282–288. doi: 10.1542/peds.2006-3153. [DOI] [PubMed] [Google Scholar]
- 9.Lindley LC, Mark B, Lee SD. Providing hospice care to children and young adults: a descriptive study of end-of-life organizations. J Hosp Palliat Nurse. 2009;11:315–323. doi: 10.1097/NJH.0b013e3181bcfd62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ginn G, Moseley C. Community health orientation, community-based quality improvement, and health promotion services in hospitals. J Healthc Manag. 2004;49:293–306. [PubMed] [Google Scholar]
- 11.Pollack H, D'Aunno T. HIV testing and counseling in the nation's outpatient substance abuse treatment system, 1995–2005. J Subst Abuse Treat. 2010;38:307–316. doi: 10.1016/j.jsat.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Wells R, Lemark C, D'Aunno T. Insights from a national survey into why substance abuse treatment units add prevention and outreach services. Subst Abuse Treat Prev Policy. 2006;1:21. doi: 10.1186/1747-597X-1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Connor SR. Hospice and palliative care. New York: Routledge; 2009. [Google Scholar]
- 14.Goodrick E, Salancik G. Organizational discretion in responding to institutional practices: hospitals and cesarean births. Adm Sci Q. 1996;41:1–28. [Google Scholar]
- 15.Bardhan A, Walker R. California, pivot of the great recession. Berkley, CA: Institute for Research on Labor and Employment; 2010. Working paper No. 203-10. [Google Scholar]
- 16.Scott WR. Institutions and organizations. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 17.DiMaggio PJ, Powell WW. The iron cage revisited: institutional isomorphism and collective rationality in organizational fields. Am Sociol Rev. 1983;48:147–160. [Google Scholar]
- 18.Pfeffer J, Salancik G. The external control of organizations: A resource dependence perspective. New York: Harper and Row; 1978. [Google Scholar]
- 19.Liang K, Zeger S. Longitudinal data analysis using generalized linear models. Biometrics. 1986;73:13–22. [Google Scholar]
- 20.McCue M. Association of market, organizational and financial factors with the number and types of capital expenditures. Health Care Manage Rev. 2011;36:67–77. doi: 10.1097/HMR.0b013e3181edd97f. [DOI] [PubMed] [Google Scholar]
- 21.Baron R, Kenny D. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 22.Aiken LS, West S. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- 23.Olden P, Clement D. The prevalence of hospital health promotion and disease prevention services: good news, bad news, and policy implications. Milbank Q. 2000;78:115–146. doi: 10.1111/1468-0009.00163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Proenca E, Rosko M, Zinn J. Correlates of hospital provision of prevention and health promotion services. Med Care Res Rev. 2003;60:58–78. doi: 10.1177/1077558702250244. [DOI] [PubMed] [Google Scholar]
- 25.Lorenz K, Asch S, Rosenfeld K, Liu H, Ettner S. Hospice admission practices: where does hospice fit in the continuum of care? J Am Geriatric Soc. 2004;52:725–730. doi: 10.1111/j.1532-5415.2004.52209.x. [DOI] [PubMed] [Google Scholar]
- 26.White KR, Cochran CE, Patel UB. Hospital provision of end-of-life services: who, what, and where? Med Care. 2002;40:17–25. doi: 10.1097/00005650-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Himelstein B. Palliative care for infants, children, adolescents, and their families. J Palliat Med. 2006;9:163–181. doi: 10.1089/jpm.2006.9.163. [DOI] [PubMed] [Google Scholar]
- 28.Orloff S. Incorporating children in an adult hospice program. In: Armstrong-Dailey A, Zarbock S, editors. Hospice care for children. Oxford: Oxford University Press; 2001. pp. 353–377. [Google Scholar]
- 29.Thorpe K, Phelps C. The social role of not-for-profits organizations: hospital provision of charity care. Econ Inquiry. 2001;29:472–484. [Google Scholar]
- 30.Au M, Taylor E, Gold M. Improving access to language services in health care: A look at national and state efforts. Washington, DC: Mathematica Policy Research; 2009. [Google Scholar]
- 31.Connor SR. Development of hospice and palliative care in the United States. Omega. 2007;56:89–99. doi: 10.2190/om.56.1.h. [DOI] [PubMed] [Google Scholar]
- 32.Abel E. The hospice movement: Institutionalizing innovation. Int J Health Serv. 1986;16:71–85. doi: 10.2190/RQBV-J2PG-VFNM-1H97. [DOI] [PubMed] [Google Scholar]
- 33.Mata H, Latham TP, Ransome Y. Benefits of professional organization membership and participation in national conferences: considerations for students and new professionals. Health Promot Pract. 2010;11:450–453. doi: 10.1177/1524839910370427. [DOI] [PubMed] [Google Scholar]
- 34.Daft R. Organization theory and design. Mason, OH: Thomson South-Western; 2004. [Google Scholar]
- 35.Hospice Association of America. Hospice facts & statistics. [Accessed December, 30, 2009];2008 Available from http://www.nahc.org/facts/HospiceStats08.pdf. [Google Scholar]
- 36.Greenhalgh T, Robert G, Macfarlane F, et al. Diffusion of innovations in service organizations: Systematic review and recommendations. Milbank Q. 2004;82:581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shortell S, Marsteller J, Lin M, et al. The role of perceived team effectiveness in improving chronic illness care. Med Care. 2004;42:1040–1048. doi: 10.1097/00005650-200411000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Acolet D, Allen E, Houston R, et al. Improvement in neonatal intensive care unit care: a cluster randomized controlled trial of active dissemination of information. Arch Dis Child Fetal Neonatal Ed. 2011;96(6):F434–F439. doi: 10.1136/adc.2010.207522. [DOI] [PubMed] [Google Scholar]
- 39.Doumit G, Gattellari M, Grimshaw J, O'Brien M. Local opinion leaders: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2007;24(1) doi: 10.1002/14651858.CD000125.pub3. CD000125. [DOI] [PubMed] [Google Scholar]
- 40.Damschroder L, Banaszak-Holl J, Kowalski C, et al. The role of the champion in infection prevention: Results from a multisite qualitative study. Qual Saf Health Care. 2009;18:434–440. doi: 10.1136/qshc.2009.034199. [DOI] [PubMed] [Google Scholar]
- 41.Gallagher K, Nutting P, Nease D, et al. It takes two: using coleaders to champion improvements in small primary care practices. J Am Board Fam Med. 2010;23:632–639. doi: 10.3122/jabfm.2010.05.090198. [DOI] [PubMed] [Google Scholar]
- 42.Friebert S, Huff S. NHPCO's pediatric standards: a key step in advancing care for American's children. [Accessed September 12, 2011];NewsLine. 2009 :9–12. Available from: http://www.nhpco.org/files/public/chipps/Peds-Standards_article_NL-0209.pdf. [Google Scholar]