Abstract
Hypertensive heart disease is the target organ response to arterial hypertension. Left ventricular hypertrophy represents an important predictor for cardiovascular events. Myocardial fibrosis, a common end point in hypertensive heart disease, has been linked to the development of left ventricular hypertrophy and diastolic dysfunction. Echocardiography is clinically useful in the detection of left ventricular hypertrophy and the assessment of diastolic function. Although echocardiography is more widely available, cardiac magnetic resonance has been demonstrated to be more reproducible for the estimation of left ventricular mass. Future developments in cardiac magnetic resonance techniques may facilitate the quantification of diffuse fibrosis that occurs in hypertensive heart disease. Thus, advances in cardiac imaging provide comprehensive, noninvasive tools for imaging left ventricular hypertrophy, diastolic dysfunction, myocardial fibrosis and ischemia observed in hypertensive heart disease. The objective of this article is to summarize the state-of-the-art and the future of multimodality imaging of hypertensive heart disease.
Keywords: cardiac magnetic resonance, diastolic function, echocardiography, hypertension, hypertensive heart disease, left ventricular hypertrophy, left ventricular mass, myocardial fibrosis
Hypertensive heart disease (HHD) is the target organ response to systemic arterial hyper-tension. Patients with longstanding hypertension are at increased risk for developing left ventricular hypertrophy (LVH) and diastolic dysfunction [1]. Arterial hypertension represents one of the most common risk factors for the development of heart failure, conferring approximately a twofold increased risk in men and a threefold risk in women relative to normotensive subjects [2]. This article summarizes the state-of-the-art and the future of multi-modality noninvasive imaging in HHD with a focus on imaging LVH, diastolic dysfunction, myocardial fibrosis and ischemia secondary to hypertension.
Why is HHD important?
Left ventricular hypertrophy develops as an initially adaptive response of the normal heart to an increased afterload from a variety of reasons, systemic hypertension being the most common. Data from the Framingham Heart Study has established LVH as a risk factor for cardiovascular morbidity and mortality, independent of other cardiovascular risk factors, including blood pressure (BP) itself [4,5]. LVH regression during treatment [6] has translated to improvement in cardiovascular outcomes [7,8]. It is therefore important to identify patients with LVH, both for prognosis and for tighter BP control. Ventricular arrhythmias occur more frequently in hypertensive patients [9], with QT dispersion increasing directly with left ventricular mass (LVM) [10]. There is also a link between HHD and atrial fibrillation, whose likelihood increases by 40–50% in the presence of hypertension [11]. Increased susceptibility to ischemic heart disease rounds out the cardiovascular sequelae of HHD, with a sixfold higher risk of myocardial infarction in hypertensive patients than in normotensive individuals [2].
Imaging hypertensive LVH
LV mass
The identification of LVH in the hypertensive patient is important from a prognostic standpoint. It identifies the patient with hypertension who may require more aggressive BP control. In patients with essential hypertension and baseline LVH on ECG, lower LVM during antihypertensive treatment is associated with lower rates of clinical end points, independently of the effects of BP lowering and treatment modality [12].
The calculation of LVM on echo is based on a mathematical formula:
as modified by Devereux et al. using the American Society of Echocardiography convention [13], where LVIDD is left ventricle internal dimension in diastole, PWTD is posterior wall thickness in diastole and IVSD is intraventricular septal thickness in diastole. This modified formula was validated on necropsy findings in 52 subjects [13]. Table 1 shows previously published cut-off values for LVH and LVM evaluated by echocardiography and cardiac magnetic resonance (CMR).
Table 1.
Accepted criteria and cut-off values for left ventricular hypertrophy and left ventricular mass by currently available imaging techniques.
| Imaging technique | Male g/m2 | Female g/m2 |
|---|---|---|
| Echocardiography | ||
| M-mode LVM indexed BSA | >125 | >110 |
| 2D echo LVM indexed BSA | >102 | >88 |
| Cardiac magnetic resonance | ||
| TGE LVM indexed BSA | >96 | >77 |
| SSFP indexed BSA | >83 | >67 |
BSA: Body surface area; LVH: Left ventricular hypertrophy; LVM: Left ventricular mass; SSFP: Steady-state free precession; TGE: Turbo gradient echo.
Modified from [25].
Relative wall thickness
Relative wall thickness (RWT) is measured in clinical studies as:
The reference cut-off value for increased RWT derived from upper limits of normal samples is usually 0.45 [14]. RWT provides information regarding LV geometry independent of other calculations [15], precluding the requirement of most corrections. LV geometry as evaluated by RWT may provide an independent stratification of LV systolic and diastolic functions in essential hypertension [15]. Measurements of LV mass and RWT are prognostically important in the hypertensive patients without LVH. In the Losartan Intervention For Endpoint Reduction in Hypertension (LIFE) study, patients with inappropriately high but nonhypertrophic LV mass had a higher RWT and BMI. It was observed that inappropriately high LV mass was associated with relevant, often preclinical, manifestations of cardiac disease in the absence of traditionally defined echocardiographic LV hypertrophy and concentric geometry [16].
Geometric patterns of LV remodeling in hypertension
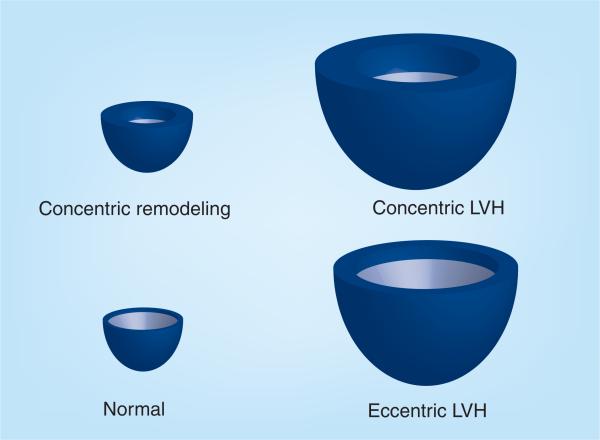
Different geometric forms of LVH have been adopted to classify the maladaptive responses of the LV in hypertension [14,17]. LV geometry is classified into four exclusive groups (Figure 1; [18]) on the basis of LVM and RWT: concentric LVH (increased mass and increased RWT), eccentric LVH (increased mass and normal RWT), concentric remodeling (normal mass and increased RWT) and normal geometry (normal mass and normal RWT). Concentric hypertrophy carries the highest risk and eccentric hypertrophy an intermediate risk, whereas concentric remodeling is associated with a smaller, albeit important risk [19,20].
Figure 1. Classification of left ventricular geometry on the basis of left ventricular mass and relative wall thickness.
LVH: Left ventricular hypertrophy.
Adapted with permission from [18].
Echocardiography to assess LVH in HHD
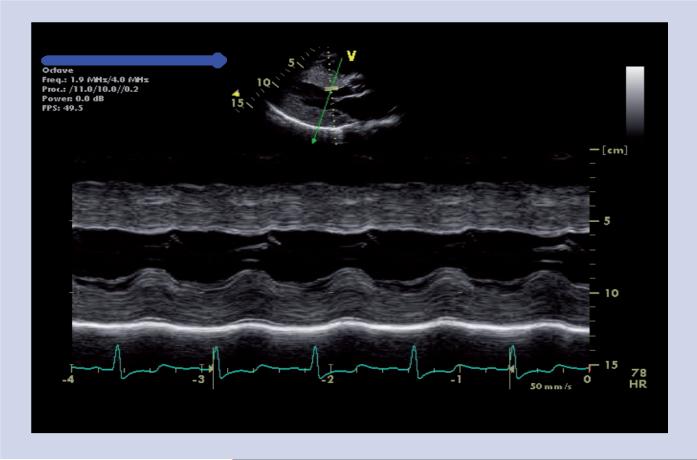
The prevalence of LVH on echocardiography in hypertensive patients has been reported to be approximately 40% [21,22]. Both M-mode (Figure 2) and 2D echocardiography are used in the measurement of LVM. M-mode echocardio graphy has the advantage of superior endocardial definition, as the high frame rate improves the spatial resolution. M-mode echocardio graphy was the first echo method to be validated and it is relatively simple and quick. The M-mode method measures the left ventricle (LV) in one dimension and assumes a prolate ellipsoid shape for the LV with a ratio of long:short axis lengths of 2:1. The M-mode method will detect all but the mildest degrees of LVH.
Figure 2.
Marked left ventricular hypertrophy noted on 2D-guided M-mode echo.
However, the accuracy and reproducibility of M-mode echocardio graphy at measuring LVM has been debated. There is a potential for variations in measured wall thickness, depending on the ultrasound beam angle to the LV wall and the assumption that the wall thickness is uniform throughout the LV. In addition, the assumed prolate ellipsoid shape of the LV is no longer valid in patients with LVH [23]. Furthermore, LVM as measured by M-mode echocardio graphy relies on linear measurements of wall thickness [12], which, when cubed, increase the standard deviation (SD) by a factor of 2–3. As elevated LVM is defined as mean +2 SD, M-mode echocardiography has the potential to underestimate the prevalence of LVH in hypertensive cohorts (Table 1) [24,25].
Two dimensional echocardiography (Figure 3) is thought to be more accurate and reproducible than the M-mode method [26], and is now more commonly used for LVM measurements. 2D echocardiography relies on mathematical formulae to estimate the LVM but there is no cube function in these formulae and hence measurement errors are not magnified. However, it still assumes a prolate ellipsoid shape of the LV and a uniform LV wall thickness.
Figure 3. Left ventricular hypertrophy on 2D echo.
(A) Parasternal long-axis view. (B) Parasternal short-axis view.
3D echocardiography for LVH assessment
3D echocardiography has improved the intra- and inter-observer variability of the LVM measurements compared with M-mode and 2D echocardiography [27], with its accuracy reported to be close to that of CMR [28]. Quantification of LVM using real-time 3D echocardiography is highly reproducible and correlates well with CMR [29]. In contrast to M-mode and 2D echocardiography, 3D echocardiography does not rely on geometrical assumptions for calculating LVM [29]. The second-generation real-time 3D technology that offers second-generation matrix array probes with 3000 simultaneously active ultrasound elements has solved the acquisition difficulties, while advances in computer technology and ana lysis software have shortened the duration of postprocessing [30]. However, superior-quality 3D images are still dependent on optimal echo windows and up to a third of patients have suboptimal echo windows for this purpose.
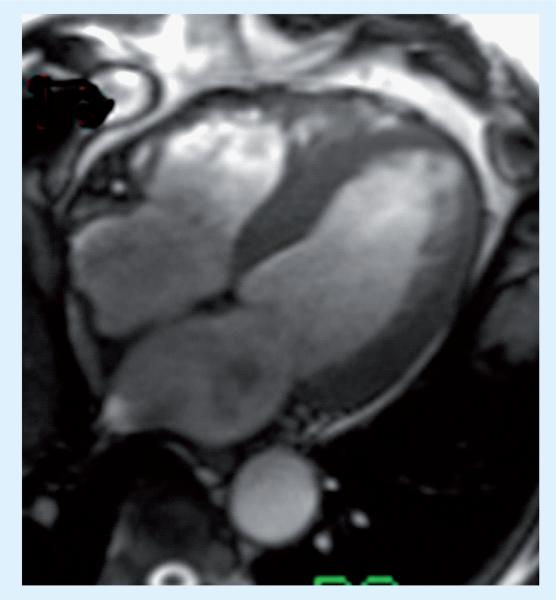
CMR for LVH assessment
As discussed previously, the cubing of the measurements for LV wall thickness when using M-mode echocardiography amplifies any errors of such measurements, resulting in a significant variation of LVM estimates compared with direct measurement using techniques such as CMR [31,32]. CMR has been demon strated to be more reproducible than either M-mode or 2D echocardiography measurements [32–34] for the estimation of LVM [35,36]. It provides a spatially defined 3D dataset at multiple levels throughout the heart, and hence the measurement of LVM does not require geometric assumptions about the shape of the LV. CMR has been validated in animal studies [37–39] and the excellent contrast between blood, and myocardial tissue and the high spatial resolution means that the endocardial and epicardial contours are easily defined. Presently, the methodology of choice for measuring LVM by CMR is steady-state free precession (SSFP) cine imaging (Figure 4). The absolute values of LVM measured by CMR tend to be lower than those for echocardiography (Table 1) because SSFP cine imaging allows the visualization of myocardial trabeculae and thus includes trabeculae in the LV volume measurement excluding it from the mass. Echocardiography, however, generally includes trabeculation in the measurement of LV mass. Although CMR has excellent reproducibility for measuring LVM and is widely perceived as the gold standard, its accuracy has not been validated against necropsy LV weight in humans.
Figure 4.
Four-chamber long-axis view on an end-diastolic frame from a steady-state free precession cine image set demonstrating left ventricular hypertrophy by cardiac magnetic resonance.
Implications for clinical trials
Echocardiography has been successfully used in large clinical trials and has provided a wealth of knowledge in patients with hypertensive LVH [12,40]. Although 2D echocardiographic determination of LVM is useful in identifying patients with severe LVH, its high measurement variability impairs its value in the subgroup of hypertensive patients with milder concentric and/or eccentric LVH, and in those with concentric remodeling. Demonstration of LVM regression using M-mode or 2D echocardiographic methods requires relatively large cohorts of patients because of the relatively high observer and interstudy variability [41]. CMR or 3D echocardiography should be the techniques of choice in clinical trials investigating LVM regression where the accuracy of LVM measurements will allow for the accurate detection of small degrees of change in LVM in smaller cohorts of patients, particularly when recruitment of large numbers of patients is not possible.
Cardiac magnetic resonance can also demonstrate parallel reductions in LV mass and chamber volume with normalization of LV ejection fraction during a relatively brief period of improved BP control with multiple agents that interrupt the hypertrophic stimuli from the RAAS. Particularly notable is the short duration of treatment required to detect such changes using a highly reproducible method such as CMR [42,43]. Echocardiographic studies of LVH regression have typically required longer treatment periods to demonstrate LVH regression as well as larger sample sizes. Table 2 lists the advantages and disadvantages of the various methods currently available to assess LVH.
Table 2.
Advantages and disadvantages of the various methods currently available to assess left ventricular hypertrophy.
| Measure | ECG | M-Mode | 2D echo | 3D echo | CMR |
|---|---|---|---|---|---|
| Cost | + | ++ | ++ | ++ | +++ |
| Sensitivity | + | ++ | ++ | +++ | +++ |
| Specificity | +++ | +++ | +++ | +++ | +++ |
| Availability | +++ | +++ | +++ | + | + |
| Complexity | + | + | ++ | ++ | ++ |
+: Low; ++: Moderate; +++: High; CMR: Cardiac magnetic resonance.
Modified from [25].
Assessment of intramyocardial function in HHD
Intramyocardial strain is a complex marker of the effect of hyper-trophy on myocardial mechanics. In hypertrophy, changes in gene expression, contractile protein kinetics, calcium handling and metabolism all occur and might contribute to reduced myocardial deformation, which initially may be adaptive. However, over the longer term it may affect global myocardial performance and prognosis. LV midwall shortening (MWS), an indirect measure of myocardial performance assessed by transthoracic echocardiography, is decreased in a subset of patients with hypertensive LVH [44]. These patients are at increased risk for cardiovascular events despite normal endocardial fractional shortening [45].
Echocardiographic calculation of MWS is a geometry-based index derived from linear measurements of the posterior and the septal walls, and consequently cannot distinguish between septal versus posterior wall function. Thus, whether depressed MWS represents global or regional intrinsic depression of LV myocardial function in pressure-overload hypertrophy is unknown. Previous experiments demonstrated that increased LV pressure could have dissimilar effects on regional LV wall stress because of different radii of curvature, resulting in regional mechanical heterogeneity caused by dissimilar afterload [46].
Cardiac magnetic resonance tissue tagging allows intramyo cardial displacement and strain to be measured noninvasively by monitoring motion of identifiable material points distributed throughout the myocardium [47–49]. MWS is depressed in hypertensive LVH as demonstrated by CMR myocardial tagging [50]. The advent of Harmonic Phase imaging [51] has enabled the use of this technique in large epidemiologic studies such as the Multi-Ethnic Study of Atherosclerosis (MESA). In this cohort study designed to investigate the nature of atherosclerosis in asymptomatic individuals, a total of 1184 participants (aged 45–84 years) underwent tagged CMR. Regional LV function was quantified by analyzing peak systolic circumferential strain (Ecc). Higher diastolic BP (DBP) was associated with lower Ecc (p ≤ 0.002). The study concluded that higher DBP and smoking are associated with decreased regional LV function in asymptomatic individuals [52]. The association between reduced regional LV function and higher DBP was substantially attenuated after controlling for LV mass, underscoring the importance of LVH in the development of regional LV dysfunction.
Diastolic dysfunction in HHD
Diastolic dysfunction is one of the earliest manifestations of HHD. It refers to abnormalities in the mechanical properties of the heart, such as decreased diastolic distensibility, slowed filling or relaxation of the LV – regardless of whether the LVEF is normal or abnormal, and whether the patient is symptomatic or asymptomatic [53,54]. Diastolic dysfunction is estimated to affect approximately 50% of hypertensive patients in the community [55] and correlates with the development of LVH [56,57]. Patients with longstanding hypertension are at increased risk for developing LVH-associated abnormalities of myocardial relaxation, which contribute to abnormal LV filling in diastole and elevated intracardiac filling pressures [57].
As discussed previously, the prediction of cardiovascular morbidity and mortality in hypertensive individuals may be independent of BP itself [58]. The abnormal compliance of the LV with increased filling pressures for a given volume and higher incidence of subendocardial ischemia with associated diastolic dysfunction are a few of the many postulated mechanisms for the deleterious effects of LVH.
Importance of imaging diastolic function in HHD
Adequate control of arterial pressure in hypertensive patients should favorably alter loading conditions in the short term, while, in the long term promote regression of hypertrophy. Diastolic dysfunction in HHD improves as LVH regresses [59]. Interestingly, abnormalities of diastolic function can also be detected by sensitive imaging techniques in the absence of LVH, thus suggesting that these abnormalities could precede or develop independently of LVH. The benefits of LVH regression in hypertensive individuals appear to be independent of and additive to the effects of BP lowering [12], suggesting that the improvement in diastolic dysfunction with LVH regression may play a role.
Echocardiography for diastolic dysfunction
Generally, in early hypertension there is delayed relaxation of the myocardium because of hypertrophy and mild degrees of stiffening, affecting the peak early filling (E-wave) and late diastolic filling (A-wave) velocities of the mitral valve inflow, manifested as a reduced E/A ratio. In severe, long-standing hypertension, the LV can develop systolic dysfunction as well. At this point, there may be evidence of more advanced diastolic dysfunction with a normal or high E/A ratio, representing pseudo-normal filling or a restrictive physiology.
Until recently, the most widely accepted and utilized method to assess LV diastolic function noninvasively has been assessment of transmitral inflow or pulmonary venous flows utilizing Doppler echocardiography [60,61]. Neither of these techniques evaluate LV relaxation directly. Instead, they measure the impact of altered LV diastolic properties by assessing diastolic flow velocities that result from pressure gradient changes at the mitral orifice, and systolic and diastolic flow velocities in the pulmonary veins, respectively. These conventional Doppler assessments are very much load-dependent, and as such can change dramatically due to small alterations in heart rate or ventricular preload [62,63].
Tissue Doppler imaging (TDI) is a relatively new technique that allows direct quantification of mitral annular velocities. TDI can measure early diastolic mitral annular velocity (Ea), and a late (atrial contraction) diastolic mitral annular velocity (Am) (Figure 5) [64]. Nagueh et al. and others have reported that, although transmitral Doppler E-wave velocity is altered by changes in preload or left atrial pressures [65], Ea at the lateral left ventricular base does not change significantly, and effects of preload can be corrected by a ratio of E/Ea [66].
Figure 5.
Tissue Doppler imaging in a patient with hypertension demonstrating reduced early diastolic mitral annular velocity (Ea), suggestive of diastolic dysfunction.
Strain & strain rate
These measures provide a more detailed characterization of myocardial mechanics and may reveal subclinical abnormalities earlier in HHD than is apparent by the detection of LVH or overt DD. It should be emphasized that reduced strain and strain rate, which is a sensitive marker for preclinical HHD, are nonspecific and have also been reported in preclinical infiltrative and hypertrophic cardiomyopathy, and are likely to be present in a broad range of other disease states as well. Thus, strain and strain rate data must be put in context of the clinical situation.
2D-speckle imaging
Newer methods, such as 2D-speckle imaging, appear to provide a direct angle- and geometry-independent measure of circumferential strain (ε) [67]. A principal advantage of speckle tracking imaging is that it offers measurements of strain that, unlike tissue Doppler, are not dependent on insonation angle. Amundsen et al. showed a good correlation between longitudinal 2D strain values and those obtained by CMR tagging [68]. This method permits measurement of the three principal systolic strains: circumferential, longitudinal and radial. Narayanan et al. noted that HHD with normal ejection fraction is associated with reduced myocardial velocities and reduced regional function but normal global systolic strain (ε) [69]. Velocity abnormalities occur early in hypertension and may be an appropriate target for preventive strategies because they occur before abnormalities in global ε [69]. These data suggest that velocity abnormalities occur relatively early in hypertensive subjects, are associated with (or even responsible for) diastolic filling abnormalities, and thus may be a target for preventive strategies [70].
CMR for diastolic dysfunction
There is homology between CMR and transthoracic echo-cardiography for the assessment of diastolic inflow, with excellent agreement of quantitative velocity measurements [71]. Diastolic blood flow assessment by CMR can be performed in a single scan, either in a single breath-hold or averaged over approximately 3 min. This can be part of a routine CMR examinations, either as an adjunctive test when evaluating systolic function or even as a primary test when echocardiographic data cannot be obtained. Thus, CMR has a demonstrated potential to define diastolic function and quantify its properties in terms of active and passive stages, and its relaxation and compliance characteristics. CMR is also useful for assessing inflow and myocardial velocities, and revealing properties of the chamber and myocardium [72], thus providing insights not fully available with other invasive and noninvasive strategies.
Myocardial fibrosis
A common end point of many cellular and noncellular pathologic processes in HHD is myocardial fibrosis. Fibrosis quantification in endomyocardial samples obtained via transjugular biopsy showed a significantly greater collagen volume fraction in patients with hyper-tension than in normotensive controls [73]. Myocardial fibrosis in animals is associated with worsening ventricular systolic function, abnormal cardiac remodeling and increased ventricular stiffness [74]. The link between collagen turnover and myo cardial fibrosis is not fully understood, but it is thought to play an important role in the development of diastolic dysfunction [75,76].
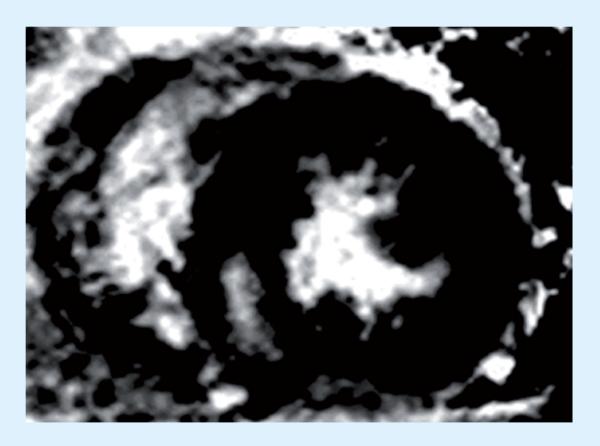
Imaging myocardial fibrosis
Various imaging techniques have emerged to quantify myocar-dial fibrosis noninvasively. Echocardiography with integrated backscatter show good correlation with collagen volume fraction, recognizing that slightly less than half of patients may have suitable backscatter signal for ana lysis [77]. A more robust approach for visualization of myocardial fibrosis is late gadolinium enhancement (LGE)-CMR (Figure 6) [78].
Figure 6.
Late gadolinium enhancement–cardiac magnetic resonance in a patient with hypertensive left ventricular hypertrophy demonstrating a mid-wall region of late gadolinium enhancement in the inferoseptum.
This technique shows enhancement in regions of fibrosis with appropriate T1-weighted techniques 10–15 min after intravenous administration of gadolinium-based contrast because of:
Expanded extravascular volume in fibrotic myocardium that is occupied by this extracellular contrast agent;
Impaired efflux of gadolinium-based contrast due to vascular changes in fibrotic myocardium.
A recent study showed that approximately half of patients with LV hyper trophy due to arterial hypertension manifested patchy enhancement on LGE imaging [79]; this pattern is clearly distinguishable from the subendocardial enhancement of infarcted myocardium. Raman et al. have shown that severity of diastolic dysfunction increases with extent of fibrosis by LGE [80].
Visibly enhanced myocardial regions by LGE-CMR may be absent in HHD even in the presence of diffuse interstitial fibrosis. A critical drawback to the technique of LGE-CMR in the detection of more diffuse myocardial fibrosis is that it is qualitative, not quantitative, and it relies on the difference in signal intensity between scarred and normal adjacent myocardium to generate image contrast. Because collagen deposition in LVH is commonly diffuse, the technique of delayed contrast enhancement often shows no regional scarring.
This has prompted the development of the technique of T1 mapping by which quantification of global T1 time can help to quantify diffuse myocardial fibrosis. These studies are in the early phases of technique development and application. T1 mapping may be applied to the entire myocardium allowing quantification of differences in T1 relaxation, an intrinsic property of spins or protons in fibrotic versus normal myocardium. These differences are further exaggerated after gadolinium administration, which showed good correlation with collagen volume fraction in a small study of post-orthotopic heart transplant patients by Iles et al. [81]. Their data demonstrated profound differences in myocardial contrast accumulation between normal and heart failure subjects utilizing post-contrast T1 mapping, with histologic data supporting their assertion that these changes reflect diffuse fibrosis. The differences also correlated with echocardiographic measurements of diastolic function, indicating shortening of T1 time may reflect altered diastolic function as a functional consequence of myocardial fibrosis. T1 mapping has the potential to be an end point in future therapeutic trials targeting fibrosis in HHD, eliminating the need for serial invasive endomyocardial biopsies [82].
Ischemia in HHD
In hypertensive patients, coronary arterial insufficiency may occur as a consequence of increased coronary arterial resistance, including diminished coronary flow and flow reserve, and altered blood rheology. These changes in the coronary circulation are independent of occlusive atherosclerotic epicardial arterial disease. Diminished coronary flow and flow reserve, increased coronary vascular resistance and blood viscosity in hypertension, and the increased myocardial oxygen demand engendered by the elevated arterial pressure and increased cardiac mass all play a major part in the high prevalence of sudden death and silent ischemia associated with hypertension. Abnormalities in the coronary micro circulation that accompany cardiac hypertrophy play a significant role in the pathogenesis of the complications associated with LVH [83].
Imaging for ischemia in HHD
Myocardial perfusion scintigraphy may be valuable and could have a potential role in the detection of diminished coronary flow and flow reserve in HHD. However, there are issues with the technique in this patient population. Since myocardial thallium uptake is dependent on regional Na+–K+ pump function, and technetium uptake is dependent on myocardial blood flow, any myocardial pathology may produce an abnormal image. It may thus be postulated that hypertensive patients, especially those with LVH, may have perfusion abnormalities unrelated to epicar-dial coronary artery disease that serve to alter the kinetics of radio-isotope tracer agent and result in abnormal images interpreted as representing ischemia or infarction [84]. In HHD, Picano et al. have shown that ST segment depression and/or myocardial perfusion abnormalities are frequently found with angiographically normal coronary arteries associated with LVH and/or microvascular disease [85]. Although stress echocardiography tends to have a higher specificity in HHD for angiographically proven epicardial CAD [85], the sensitivity of wall motion abnormalities for detection of ischemia is markedly reduced in the presence of LVH.
Microvascular disease as a cause of endothelial dysfunction has been proposed as one of the etiologies of chest pain and myocardial ischemia in patients with hypertension and/or diabetes and normal coronary arteries on angiography [86]. Patients with positive stress testing for coronary ischemia and exclusion of significant coronary stenosis invasively were found to have subendocardial perfusion deficits on stress perfusion CMR [87]. Stress perfusion CMR allows noninvasive differentiation between patients with significant stenosis and patients with micro vascular disease caused by hypertension and/or diabetes based on the temporal and spatial extent of perfusion deficits. Patients with microvascular disease more often have diffuse perfusion deficits with shorter persistence than patients with significant epicardial coronary artery disease [88].
Clinical applications of imaging HHD
In clinical practice the ECG is usually the first test performed to assess for the presence of LVH. Although LVH on ECG has the potential to identify the subgroup of patients with the highest LVM and the highest risk [89,90], false positives are very common in the young and in patients of African–American origin. In addition, a normal ECG does not exclude the presence of LVH [91], and these patients should be evaluated further with imaging.
Echocardiography is the preferred initial imaging strategy since it can confirm the presence of LVH as well as provide additional information such as LV systolic/diastolic function and the presence or absence of other potential causes of LVH. CMR can provide useful information in patients with suboptimal echo windows. It must be noted that at the present time, there is limited data available on CMR techniques such as T1 mapping and LGE in hypertensive LVH. The relative expense of CMR precludes its routine use in patients with hypertensive LVH, but for clinical trials of LVH and LV mass reduction with antihypertensive therapy, CMR or 3D echocardiography should be the imaging modality of choice.
Expert commentary
In spite of advances in therapies, the hypertensive patient's risk of heart failure has changed little since its recognition by large population-based studies over the past decades. Hypertensive LVH is an established predictor of cardiovascular events in hypertension. Since a normal ECG does not exclude the presence of LVH, imaging is important for diagnosis and prognostication in HHD. 2D echocardiography still remains the imaging technique of choice for the initial assessment of HHD. However, advanced echocardiographic tools (including 3D echocardio graphy) and CMR techniques offer a more comprehensive assessment of HHD, although they are limited by inadequate acoustic windows in a third of patients and cost, respectively. The newer real-time 3D echocardiographic technology now offers second-generation matrix array probes, solving the acquisition difficulties, while advances in computer technology and ana lysis software have shortened the duration of postprocessing. CMR is a reliable means of evaluating cardiac morphology, and therefore well suited for identifying and characterizing hypertensive patients with LVH and accurately measuring LV mass. Such precise measurements of LV mass using CMR or 3D echocardiography allows a smaller sample size to detect changes in clinical trials of LVH regression on hypertensive therapy.
Five-year view
Advances in imaging have provided tools for comprehensive noninvasive imaging of LVH, diastolic dysfunction, myocardial fibrosis and ischemia observed in HHD. The currently available echocardiographic techniques such as TDI, strain, strain rate and speckled tracking will continue to evolve and become more routine and user friendly in the years ahead. 2D-speckle imaging appears to provides a direct angle- and geometry-independent measure of circumferential strain. Advances in understanding myocardial mechanics in hypertension, coupled with targeted therapies, suggest that routine clinical application of these advanced echocardiographic methods could benefit patients in the detection of subclinical disease, quantification of myocardial tissue dynamics, and tracking changes in disease progression or in response to hypertensive therapies. Since diastolic dysfunction often precedes the development of LVH, these techniques will help early detection of diastolic dysfunction in the absence of LVH.
Cardiac magnetic resonance has demonstrated great potential to define diastolic function in terms of active and passive stages, and its relaxation and compliance characteristics. In the future, CMR is likely to utilized more often in HHD to assess inflow and myocardial velocities, and revealing properties of the LV, thus providing insights not fully available via other invasive and noninvasive strategies. Imaging fibrosis may improve the understanding of the pathophysiology of HHD. Novel CMR methods, such as T1 mapping, could become established as a tool for non invasive quantification of diffuse myocardial fibrosis in LVH, which could be used to evaluate newer therapies aimed at reducing myocardial fibrosis.
Key issues.
Hypertensive left ventricular hypertrophy (LVH) represents a powerful predictor for cardiovascular morbidity and mortality, independent of other cardiovascular risk factors, even blood pressure itself.
A normal ECG does not exclude the presence of LVH, and therefore patients should be evaluated further with imaging.
Echocardiography is clinically useful in the detection of LVH and the assessment of diastolic function.
Cardiac magnetic resonance (CMR) has been demonstrated to be more accurate and reproducible for the estimation of left ventricular (LV) mass.
Precise measurement of LV mass using CMR or 3D echocardiography allows a smaller sample size to detect changes in clinical trials.
Myocardial fibrosis, a common end point in hypertensive heart disease (HHD), has been linked to the development of LVH and diastolic dysfunction.
Recent developments in CMR techniques, such as T1 mapping, can help us quantify diffuse fibrosis that occurs in HHD.
Noninvasive quantification of diffuse myocardial fibrosis in LVH is highly desirable in evaluating newer therapies aimed at reducing myocardial fibrosis.
Acknowledgments
Christopher M Kramer receives research equipment support from Siemens Healthcare.
Footnotes
Financial & competing interests disclosure
The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
• of interest
•• of considerable interest
- 1•.Janardhanan R, Desai AS, Solomon SD. Therapeutic approaches to diastolic dysfunction. Curr. Hypertens. Rep. 2009;11(4):283–291. doi: 10.1007/s11906-009-0048-z. [Progressive abnormalities of passive stiffness or active relaxation of the myocardium that impair ventricular filling during diastole may be an important contributor to the development of heart failure in patients with preserved ejection fraction. In this review, the epidemiology and pathophysiology of diastolic dysfunction and heart failure with preserved ejection fraction are discussed.] [DOI] [PubMed] [Google Scholar]
- 2.Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA. 1996;275(20):1557–1562. [PubMed] [Google Scholar]
- 3.Kannel WB, Gordon T, Castelli WP, Margolis JR. Electrocardiographic left ventricular hypertrophy and risk of coronary heart disease. The Framingham study. Ann. Intern. Med. 1970;72(6):813–822. doi: 10.7326/0003-4819-72-6-813. [DOI] [PubMed] [Google Scholar]
- 4.Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N. Engl. J. Med. 1990;322(22):1561–1566. doi: 10.1056/NEJM199005313222203. [DOI] [PubMed] [Google Scholar]
- 5.Verdecchia P, Schillaci G, Borgioni C, et al. Prognostic value of left ventricular mass and geometry in systemic hypertension with left ventricular hypertrophy. Am. J. Cardiol. 1996;78(2):197–202. doi: 10.1016/s0002-9149(96)90395-1. [DOI] [PubMed] [Google Scholar]
- 6.Wachtell K, Bella JN, Rokkedal J, et al. Change in diastolic left ventricular filling after one year of antihypertensive treatment: the Losartan Intervention For Endpoint Reduction in Hypertension (LIFE) Study. Circulation. 2002;105(9):1071–1076. doi: 10.1161/hc0902.104599. [DOI] [PubMed] [Google Scholar]
- 7.Okin PM, Devereux RB, Jern S, et al. Regression of electrocardiographic left ventricular hypertrophy during antihypertensive treatment and the prediction of major cardiovascular events. JAMA. 2004;292(19):2343–2349. doi: 10.1001/jama.292.19.2343. [DOI] [PubMed] [Google Scholar]
- 8.Verdecchia P, Schillaci G, Borgioni C, et al. Prognostic significance of serial changes in left ventricular mass in essential hypertension. Circulation. 1998;97(1):48–54. doi: 10.1161/01.cir.97.1.48. [DOI] [PubMed] [Google Scholar]
- 9.McLenachan JM, Henderson E, Morris KI, Dargie HJ. Ventricular arrhythmias in patients with hypertensive left ventricular hypertrophy. N. Engl. J. Med. 1987;317(13):787–792. doi: 10.1056/NEJM198709243171302. [DOI] [PubMed] [Google Scholar]
- 10.Dimopoulos S, Nicosia F, Donati P, et al. QT dispersion and left ventricular hypertrophy in elderly hypertensive and normotensive patients. Angiology. 2008;59(5):605–612. doi: 10.1177/0003319707310276. [DOI] [PubMed] [Google Scholar]
- 11.Kannel WB, Wolf PA, Benjamin EJ, Levy D. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am. J. Cardiol. 1998;82(8A):2N–9N. doi: 10.1016/s0002-9149(98)00583-9. [DOI] [PubMed] [Google Scholar]
- 12.Devereux RB, Wachtell K, Gerdts E, et al. Prognostic significance of left ventricular mass change during treatment of hypertension. JAMA. 2004;292(19):2350–2356. doi: 10.1001/jama.292.19.2350. [DOI] [PubMed] [Google Scholar]
- 13.Devereux RB, Alonso DR, Lutas EM, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am. J. Cardiol. 1986;57(6):450–458. doi: 10.1016/0002-9149(86)90771-x. [DOI] [PubMed] [Google Scholar]
- 14.Savage DD, Garrison RJ, Kannel WB, et al. The spectrum of left-ventricular hypertrophy in a general-population sample – the Framingham-Study. Circulation. 1987;75(1):26–33. [PubMed] [Google Scholar]
- 15.Li L, Shigematsu Y, Hamada M, Hiwada K. Relative wall thickness is an independent predictor of left ventricular systolic and diastolic dysfunctions in essential hypertension. Hypertens. Res. 2001;24(5):493–499. doi: 10.1291/hypres.24.493. [DOI] [PubMed] [Google Scholar]
- 16.Palmieri V, Wachtell K, Bella JN, et al. Usefulness of the assessment of the appropriateness of left ventricular mass to detect left ventricular systolic and diastolic abnormalities in absence of echocardiographic left ventricular hypertrophy: the LIFE study. J. Hum. Hypertens. 2004;18(6):423–430. doi: 10.1038/sj.jhh.1001719. [DOI] [PubMed] [Google Scholar]
- 17.Ganau A, Devereux RB, Roman MJ, et al. Patterns of left-ventricular hypertrophy and geometric remodeling in essential- hypertension. J. Am. Coll. Cardiol. 1992;19(7):1550–1558. doi: 10.1016/0735-1097(92)90617-v. [DOI] [PubMed] [Google Scholar]
- 18••.Foppa M, Duncan BB, Rohde LE. Echocardiography-based left ventricular mass estimation. How should we define hypertrophy? Cardiovasc. Ultrasound. 2005;3:17. doi: 10.1186/1476-7120-3-17. [Reviews the most common measures that have been employed in left ventricular hypertrophy evaluation, and emphasizes that echocardiography will remain a relatively inexpensive and accurate diagnostic tool.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verdecchia P, Schillaci G, Borgioni C, et al. Adverse prognostic significance of concentric remodeling of the left ventricle in hypertensive patients with normal left ventricular mass. J. Am. Coll. Cardiol. 1995;25(4):871–878. doi: 10.1016/0735-1097(94)00424-O. [DOI] [PubMed] [Google Scholar]
- 20.Koren MJ, Devereux RB, Casale PN, Savage DD, Laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann. Intern. Med. 1991;114(5):345–352. doi: 10.7326/0003-4819-114-5-345. [DOI] [PubMed] [Google Scholar]
- 21.Savage DD, Drayer JI, Henry WL, et al. Echocardiographic assessment of cardiac anatomy and function in hypertensive subjects. Circulation. 1979;59(4):623–632. doi: 10.1161/01.cir.59.4.623. [DOI] [PubMed] [Google Scholar]
- 22.Devereux RB, Savage DD, Drayer JI, Laragh JH. Left ventricular hypertrophy and function in high, normal, and low-renin forms of essential hypertension. Hypertension. 1982;4(4):524–531. doi: 10.1161/01.hyp.4.4.524. [DOI] [PubMed] [Google Scholar]
- 23.Salcedo EE, Gockowski K, Tarazi RC. Left ventricular mass and wall thickness in hypertension. Comparison of M mode and two dimensional echocardiography in two experimental models. Am. J. Cardiol. 1979;44(5):936–940. doi: 10.1016/0002-9149(79)90225-x. [DOI] [PubMed] [Google Scholar]
- 24.Korner PI, Jennings GL. Assessment of prevalence of left ventricular hypertrophy in hypertension. J. Hypertens. 1998;16(6):715–723. doi: 10.1097/00004872-199816060-00001. [DOI] [PubMed] [Google Scholar]
- 25••.Alfakih K, Reid S, Hall A, Sivananthan MU. The assessment of left ventricular hypertrophy in hypertension. J. Hypertens. 2006;24(7):1223–1230. doi: 10.1097/01.hjh.0000234097.47379.fd. [Comprehensive review on the evaluation of hypertensive left ventricular hypertrophy.] [DOI] [PubMed] [Google Scholar]
- 26.Agabiti-Rosei E, Muiesan ML, Salvetti M. Evaluation of subclinical target organ damage for risk assessment and treatment in the hypertensive patients: left ventricular hypertrophy. J. Am. Soc. Nephrol. 2006;17(4 Suppl. 2):S104–S108. doi: 10.1681/ASN.2005121336. [DOI] [PubMed] [Google Scholar]
- 27.Buck T, Hunold P, Wentz KU, Tkalec W, Nesser HJ, Erbel R. Tomographic three-dimensional echocardiographic determination of chamber size and systolic function in patients with left ventricular aneurysm: comparison to magnetic resonance imaging, cineventriculography, and two-dimensional echocardiography. Circulation. 1997;96(12):4286–4297. doi: 10.1161/01.cir.96.12.4286. [DOI] [PubMed] [Google Scholar]
- 28.Gutberlet M, Abdul-Khaliq H, Grothoff M, et al. [Evaluation of left ventricular volumes in patients with congenital heart disease and abnormal left ventricular geometry. Comparison of MRI and transthoracic 3-dimensional echocardiography]. Rofo. 2003;175(7):942–951. doi: 10.1055/s-2003-40435. [DOI] [PubMed] [Google Scholar]
- 29.Kuhl HP, Schreckenberg M, Rulands D, et al. High-resolution transthoracic real-time three-dimensional echocardiography: quantitation of cardiac volumes and function using semi-automatic border detection and comparison with cardiac magnetic resonance imaging. J. Am. Coll. Cardiol. 2004;43(11):2083–2090. doi: 10.1016/j.jacc.2004.01.037. [DOI] [PubMed] [Google Scholar]
- 30.von Bardeleben RS, Kuhl HP, Mohr-Kahaly S, Franke A. Second-generation real-time three-dimensional echocardiography. Finally on its way into clinical cardiology? Z. Kardiol. 2004;93(Suppl. 4):IV56–IV64. doi: 10.1007/s00392-004-1409-x. [DOI] [PubMed] [Google Scholar]
- 31.Missouris CG, Forbat SM, Singer DR, Markandu ND, Underwood R, MacGregor GA. Echocardiography overestimates left ventricular mass: a comparative study with magnetic resonance imaging in patients with hypertension. J. Hypertens. 1996;14(8):1005–1010. [PubMed] [Google Scholar]
- 32••.Myerson SG, Montgomery HE, World MJ, Pennell DJ. Left ventricular mass: reliability of M-mode and 2-dimensional echocardiographic formulas. Hypertension. 2002;40(5):673–678. doi: 10.1161/01.hyp.0000036401.99908.db. [Cardiovascular magnetic resonance is a suitable tool for this purpose, and this review assesses the technique in comparison with others and examines the clinical and research implications of the improved reproducibility.] [DOI] [PubMed] [Google Scholar]
- 33.Bottini PB, Carr AA, Prisant LM, Flickinger FW, Allison JD, Gottdiener JS. Magnetic resonance imaging compared to echocardiography to assess left ventricular mass in the hypertensive patient. Am. J. Hypertens. 1995;8(3):221–228. doi: 10.1016/0895-7061(94)00178-E. [DOI] [PubMed] [Google Scholar]
- 34.Papavassiliu T, Kuhl HP, van Dockum W, et al. Accuracy of one- and two-dimensional algorithms with optimal image plane position for the estimation of left ventricular mass: a comparative study using magnetic resonance imaging. J. Cardiovasc. Magn. Reson. 2004;6(4):845–854. doi: 10.1081/jcmr-200036157. [DOI] [PubMed] [Google Scholar]
- 35.Sakuma H, Fujita N, Foo TK, et al. Evaluation of left ventricular volume and mass with breath-hold cine MR imaging. Radiology. 1993;188(2):377–380. doi: 10.1148/radiology.188.2.8327681. [DOI] [PubMed] [Google Scholar]
- 36.Pattynama PM, Lamb HJ, van der Velde EA, van der Wall EE, de Roos A. Left ventricular measurements with cine and spin-echo MR imaging: a study of reproducibility with variance component analysis. Radiology. 1993;187(1):261–268. doi: 10.1148/radiology.187.1.8451425. [DOI] [PubMed] [Google Scholar]
- 37.Katz J, Milliken MC, Stray-Gundersen J, et al. Estimation of human myocardial mass with MR imaging. Radiology. 1988;169(2):495–498. doi: 10.1148/radiology.169.2.2971985. [DOI] [PubMed] [Google Scholar]
- 38.Florentine MS, Grosskreutz CL, Chang W, et al. Measurement of left ventricular mass in vivo using gated nuclear magnetic resonance imaging. J. Am. Coll. Cardiol. 1986;8(1):107–112. doi: 10.1016/s0735-1097(86)80099-7. [DOI] [PubMed] [Google Scholar]
- 39.Keller AM, Peshock RM, Malloy CR, et al. In vivo measurement of myocardial mass using nuclear magnetic resonance imaging. J. Am. Coll. Cardiol. 1986;8(1):113–117. doi: 10.1016/s0735-1097(86)80100-0. [DOI] [PubMed] [Google Scholar]
- 40.Devereux RB, Dahlof B, Gerdts E, et al. Regression of hypertensive left ventricular hypertrophy by losartan compared with atenolol: the Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial. Circulation. 2004;110(11):1456–1462. doi: 10.1161/01.CIR.0000141573.44737.5A. [DOI] [PubMed] [Google Scholar]
- 41.Grothues F, Smith GC, Moon JC, et al. Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. Am. J. Cardiol. 2002;90(1):29–34. doi: 10.1016/s0002-9149(02)02381-0. [DOI] [PubMed] [Google Scholar]
- 42.Reichek N, Devereux RB, Rocha RA, et al. Magnetic resonance imaging left ventricular mass reduction with fixed-dose angiotensin-converting enzyme inhibitor-based regimens in patients with high-risk hypertension. Hypertension. 2009;54(4):731–737. doi: 10.1161/HYPERTENSIONAHA.109.130641. [DOI] [PubMed] [Google Scholar]
- 43.Pitt B, Reichek N, Willenbrock R, et al. Effects of eplerenone, enalapril, and eplerenone/enalapril in patients with essential hypertension and left ventricular hypertrophy: the 4E-left ventricular hypertrophy study. Circulation. 2003;108(15):1831–1838. doi: 10.1161/01.CIR.0000091405.00772.6E. [DOI] [PubMed] [Google Scholar]
- 44.Shimizu G, Hirota Y, Kita Y, Kawamura K, Saito T, Gaasch WH. Left ventricular midwall mechanics in systemic arterial hypertension. Myocardial function is depressed in pressure-overload hypertrophy. Circulation. 1991;83(5):1676–1684. doi: 10.1161/01.cir.83.5.1676. [DOI] [PubMed] [Google Scholar]
- 45.de Simone G, Devereux RB, Koren MJ, Mensah GA, Casale PN, Laragh JH. Midwall left ventricular mechanics. An independent predictor of cardiovascular risk in arterial hypertension. Circulation. 1996;93(2):259–265. doi: 10.1161/01.cir.93.2.259. [DOI] [PubMed] [Google Scholar]
- 46.Lew WY, LeWinter MM. Regional comparison of midwall segment and area shortening in the canine left ventricle. Circ. Res. 1986;58(5):678–691. doi: 10.1161/01.res.58.5.678. [DOI] [PubMed] [Google Scholar]
- 47.Axel L, Dougherty L. MR imaging of motion with spatial modulation of magnetization. Radiology. 1989;171(3):841–845. doi: 10.1148/radiology.171.3.2717762. [DOI] [PubMed] [Google Scholar]
- 48.Young AA, Imai H, Chang CN, Axel L. Two-dimensional left ventricular deformation during systole using magnetic resonance imaging with spatial modulation of magnetization. Circulation. 1994;89(2):740–752. doi: 10.1161/01.cir.89.2.740. [DOI] [PubMed] [Google Scholar]
- 49.Clark NR, Reichek N, Bergey P, et al. Circumferential myocardial shortening in the normal human left ventricle. Assessment by magnetic resonance imaging using spatial modulation of magnetization. Circulation. 1991;84(1):67–74. doi: 10.1161/01.cir.84.1.67. [DOI] [PubMed] [Google Scholar]
- 50.Palmon LC, Reichek N, Yeon SB, et al. Intramural myocardial shortening in hypertensive left ventricular hypertrophy with normal pump function. Circulation. 1994;89(1):122–131. doi: 10.1161/01.cir.89.1.122. [DOI] [PubMed] [Google Scholar]
- 51.Osman NF, Prince JL. Visualizing myocardial function using HARP MRI. Physics Med. Biol. 2000;45(6):1665–1682. doi: 10.1088/0031-9155/45/6/318. [DOI] [PubMed] [Google Scholar]
- 52.Rosen BD, Saad MF, Shea S, et al. Hypertension and smoking are associated with reduced regional left ventricular function in asymptomatic: individuals the Multi-Ethnic Study of Atherosclerosis. J. Am. Coll. Cardiol. 2006;47(6):1150–1158. doi: 10.1016/j.jacc.2005.08.078. [DOI] [PubMed] [Google Scholar]
- 53.Gaasch WH, Zile MR. Left ventricular diastolic dysfunction and diastolic heart failure. Annu. Rev. Med. 2004;55:373–394. doi: 10.1146/annurev.med.55.091902.104417. [DOI] [PubMed] [Google Scholar]
- 54.Aurigemma GP, Gaasch WH. Diastolic heart failure. N. Engl. J. Med. 2004;351(11):1097–1105. doi: 10.1056/NEJMcp022709. [DOI] [PubMed] [Google Scholar]
- 55.Redfield MM, Jacobsen SJ, Burnett JC, Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289(2):194–202. doi: 10.1001/jama.289.2.194. [DOI] [PubMed] [Google Scholar]
- 56.Wachtell K, Smith G, Gerdts E, et al. Left ventricular filling patterns in patients with systemic hypertension and left ventricular hypertrophy (the LIFE study). Losartan Intervention For Endpoint. Am. J. Cardiol. 2000;85(4):466–472. doi: 10.1016/s0002-9149(99)00773-0. [DOI] [PubMed] [Google Scholar]
- 57.Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and diastolic heart failure: Part I: diagnosis, prognosis, and measurements of diastolic function. Circulation. 2002;105(11):1387–1393. doi: 10.1161/hc1102.105289. [DOI] [PubMed] [Google Scholar]
- 58.Kannel WB, Levy D, Cupples LA. Left ventricular hypertrophy and risk of cardiac failure: insights from the Framingham Study. J. Cardiovasc. Pharmacol. 1987;10(Suppl. 6):S135–S140. [PubMed] [Google Scholar]
- 59.Smith VE, White WB, Meeran MK, Karimeddini MK. Improved left ventricular filling accompanies reduced left ventricular mass during therapy of essential hypertension. J. Am. Coll. Cardiol. 1986;8(6):1449–1454. doi: 10.1016/s0735-1097(86)80322-9. [DOI] [PubMed] [Google Scholar]
- 60.Nishimura RA, Tajik AJ. Evaluation of diastolic filling of left ventricle in health and disease: Doppler echocardiography is the clinician's Rosetta Stone. J. Am. Coll. Cardiol. 1997;30(1):8–18. doi: 10.1016/s0735-1097(97)00144-7. [DOI] [PubMed] [Google Scholar]
- 61.Schillaci G, Pasqualini L, Verdecchia P, et al. Prognostic significance of left ventricular diastolic dysfunction in essential hypertension. J. Am. Coll. Cardiol. 2002;39(12):2005–2011. doi: 10.1016/s0735-1097(02)01896-x. [DOI] [PubMed] [Google Scholar]
- 62.Ishida Y, Meisner JS, Tsujioka K, et al. Left ventricular filling dynamics: influence of left ventricular relaxation and left atrial pressure. Circulation. 1986;74(1):187–196. doi: 10.1161/01.cir.74.1.187. [DOI] [PubMed] [Google Scholar]
- 63.Choong CY, Herrmann HC, Weyman AE, Fifer MA. Preload dependence of Doppler-derived indexes of left ventricular diastolic function in humans. J. Am. Coll. Cardiol. 1987;10(4):800–808. doi: 10.1016/s0735-1097(87)80273-5. [DOI] [PubMed] [Google Scholar]
- 64.Waggoner AD, Bierig SM. Tissue Doppler imaging: a useful echocardiographic method for the cardiac sonographer to assess systolic and diastolic ventricular function. J. Am. Soc. Echocardiogr. 2001;14(12):1143–1152. doi: 10.1067/mje.2001.115391. [DOI] [PubMed] [Google Scholar]
- 65••.Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J. Am. Coll. Cardiol. 1997;30(6):1527–1533. doi: 10.1016/s0735-1097(97)00344-6. [Seminal paper that demonstrated that mitral E velocity, corrected for the influence of relaxation (i.e., the E/Ea ratio), relates well to mean pulmonary capillary wedge pressure and may be used to estimate left ventricular filling pressures.] [DOI] [PubMed] [Google Scholar]
- 66.Sohn DW, Chai IH, Lee DJ, et al. Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J. Am. Coll. Cardiol. 1997;30(2):474–480. doi: 10.1016/s0735-1097(97)88335-0. [DOI] [PubMed] [Google Scholar]
- 67.Hurlburt HM, Aurigemma GP, Hill JC, et al. Direct ultrasound measurement of longitudinal, circumferential, and radial strain using 2-dimensional strain imaging in normal adults. Echocardiography. 2007;24(7):723–731. doi: 10.1111/j.1540-8175.2007.00460.x. [DOI] [PubMed] [Google Scholar]
- 68.Amundsen BH, Helle-Valle T, Edvardsen T, et al. Noninvasive myocardial strain measurement by speckle tracking echocardiography: validation against sonomicrometry and tagged magnetic resonance imaging. J. Am. Coll. Cardiol. 2006;47(4):789–793. doi: 10.1016/j.jacc.2005.10.040. [DOI] [PubMed] [Google Scholar]
- 69.Narayanan A, Aurigemma GP, Chinali M, Hill JC, Meyer TE, Tighe DA. Cardiac mechanics in mild hypertensive heart disease: a speckle-strain imaging study. Circ. Cardiovasc. Imaging. 2009;2(5):382–390. doi: 10.1161/CIRCIMAGING.108.811620. [DOI] [PubMed] [Google Scholar]
- 70.Solomon SD, Janardhanan R, Verma A, et al. Effect of angiotensin receptor blockade and antihypertensive drugs on diastolic function in patients with hypertension and diastolic dysfunction: a randomised trial. Lancet. 2007;369(9579):2079–2087. doi: 10.1016/S0140-6736(07)60980-5. [DOI] [PubMed] [Google Scholar]
- 71.Rathi VK, Doyle M, Yamrozik J, et al. Routine evaluation of left ventricular diastolic function by cardiovascular magnetic resonance: a practical approach. J. Cardiovasc. Magn. Reson. 2008;10:36. doi: 10.1186/1532-429X-10-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rathi VK, Biederman RW. Expanding role of cardiovascular magnetic resonance in left and right ventricular diastolic function. Heart Fail. Clin. 2009;5(3):421–435. vii. doi: 10.1016/j.hfc.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 73.Querejeta R, Varo N, Lopez B, et al. Serum carboxy-terminal propeptide of procollagen type I is a marker of myocardial fibrosis in hypertensive heart disease. Circulation. 2000;101(14):1729–1735. doi: 10.1161/01.cir.101.14.1729. [DOI] [PubMed] [Google Scholar]
- 74.Conrad CH, Brooks WW, Hayes JA, Sen S, Robinson KG, Bing OH. Myocardial fibrosis and stiffness with hypertrophy and heart failure in the spontaneously hypertensive rat. Circulation. 1995;91(1):161–170. doi: 10.1161/01.cir.91.1.161. [DOI] [PubMed] [Google Scholar]
- 75.Kass DA, Bronzwaer JG, Paulus WJ. What mechanisms underlie diastolic dysfunction in heart failure? Circ. Res. 2004;94(12):1533–1542. doi: 10.1161/01.RES.0000129254.25507.d6. [DOI] [PubMed] [Google Scholar]
- 76.Martos R, Baugh J, Ledwidge M, et al. Diastolic heart failure: evidence of increased myocardial collagen turnover linked to diastolic dysfunction. Circulation. 2007;115(7):888–895. doi: 10.1161/CIRCULATIONAHA.106.638569. [DOI] [PubMed] [Google Scholar]
- 77.Mizuno R, Fujimoto S, Saito Y, Nakamura S. Non-invasive quantitation of myocardial fibrosis using combined tissue harmonic imaging and integrated backscatter analysis in dilated cardiomyopathy. Cardiology. 2007;108(1):11–17. doi: 10.1159/000095595. [DOI] [PubMed] [Google Scholar]
- 78••.Raman SV. The hypertensive heart. An integrated understanding informed by imaging. J. Am. Coll. Cardiol. 2010;55(2):91–96. doi: 10.1016/j.jacc.2009.07.059. [Current imaging techniques offer noninvasive approaches to detecting myocardial fibrosis, ischemia, hypertrophy and disordered metabolism that form the substrate for hypertensive heart disease. This article emphasizes the need to recognize aortopathy and atrial myopathy as contributors to myocardial disease warranting incorporation of aortic and atrial functional measurements into a comprehensive understanding of the hypertensive heart.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rudolph A, Abdel-Aty H, Bohl S, et al. Noninvasive detection of fibrosis applying contrast-enhanced cardiac magnetic resonance in different forms of left ventricular hypertrophy relation to remodeling. J. Am. Coll. Cardiol. 2009;53(3):284–291. doi: 10.1016/j.jacc.2008.08.064. [DOI] [PubMed] [Google Scholar]
- 80.Moreo A, Ambrosio G, De Chiara B, et al. Influence of myocardial fibrosis on left ventricular diastolic function: noninvasive assessment by cardiac magnetic resonance and echo. Circ. Cardiovasc. Imaging. 2009;2(6):437–443. doi: 10.1161/CIRCIMAGING.108.838367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81•.Iles L, Pfluger H, Phrommintikul A, et al. Evaluation of diffuse myocardial fibrosis in heart failure with cardiac magnetic resonance contrast-enhanced T1 mapping. J. Am. Coll. Cardiol. 2008;52(19):1574–1580. doi: 10.1016/j.jacc.2008.06.049. [Contrast-enhanced cardiac MRI T1 mapping identifies changes in myocardial T1 times in heart failure, which appear to reflect diffuse fibrosis.] [DOI] [PubMed] [Google Scholar]
- 82.Brilla CG, Funck RC, Rupp H. Lisinopril-mediated regression of myocardial fibrosis in patients with hypertensive heart disease. Circulation. 2000;102(12):1388–1393. doi: 10.1161/01.cir.102.12.1388. [DOI] [PubMed] [Google Scholar]
- 83.Marcus ML, Koyanagi S, Harrison DG, Doty DB, Hiratzka LF, Eastham CL. Abnormalities in the coronary circulation that occur as a consequence of cardiac hypertrophy. Am. J. Med. 1983;75(3A):62–66. doi: 10.1016/0002-9343(83)90120-1. [DOI] [PubMed] [Google Scholar]
- 84.Poe ND, Eber LM, Norman AS, Selin CE, Terao EN. Myocardial images in nonacute coronary and noncoronary heart diseases. J. Nucl. Med. 1977;18(1):18–23. [PubMed] [Google Scholar]
- 85.Picano E, Palinkas A, Amyot R. Diagnosis of myocardial ischemia in hypertensive patients. J. Hypertens. 2001;19(7):1177–1183. doi: 10.1097/00004872-200107000-00001. [DOI] [PubMed] [Google Scholar]
- 86.Cannon RO, 3rd, Watson RM, Rosing DR, Epstein SE. Angina caused by reduced vasodilator reserve of the small coronary arteries. J. Am. Coll. Cardiol. 1983;1(6):1359–1373. doi: 10.1016/s0735-1097(83)80037-0. [DOI] [PubMed] [Google Scholar]
- 87.Panting JR, Gatehouse PD, Yang GZ, et al. Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging. N. Engl. J. Med. 2002;346(25):1948–1953. doi: 10.1056/NEJMoa012369. [DOI] [PubMed] [Google Scholar]
- 88.Bernhardt P, Levenson B, Albrecht A, Engels T, Strohm O. Detection of cardiac small vessel disease by adenosine-stress magnetic resonance. Int. J. Cardiol. 2007;121(3):261–266. doi: 10.1016/j.ijcard.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 89.Alfakih K, Walters K, Jones T, Ridgway J, Hall AS, Sivananthan M. New gender-specific partition values for ECG criteria of left ventricular hypertrophy: recalibration against cardiac MRI. Hypertension. 2004;44(2):175–179. doi: 10.1161/01.HYP.0000135249.66192.30. [DOI] [PubMed] [Google Scholar]
- 90.Schillaci G, Verdecchia P, Porcellati C, Cuccurullo O, Cosco C, Perticone F. Continuous relation between left ventricular mass and cardiovascular risk in essential hypertension. Hypertension. 2000;35(2):580–586. doi: 10.1161/01.hyp.35.2.580. [DOI] [PubMed] [Google Scholar]
- 91.Levy D, Labib SB, Anderson KM, Christiansen JC, Kannel WB, Castelli WP. Determinants of sensitivity and specificity of electrocardiographic criteria for left ventricular hypertrophy. Circulation. 1990;81(3):815–820. doi: 10.1161/01.cir.81.3.815. [DOI] [PubMed] [Google Scholar]