Abstract
Aims/Introduction
Recently, the prevalence of lifestyle‐related disease has increased, and its associated medical costs have become considerable. Although walking is thought to prevent lifestyle‐related disease, few studies have evaluated its effect on medical costs in Japanese subjects. We aimed at evaluating the effect of walking on medical costs by simulation mainly focusing on diabetes in the Japanese population.
Materials and Methods
A Markov model focusing on diabetes was constructed. As complications of diabetes, ‘dialysis’, ‘ischemic heart disease’ and ‘stroke’ were included. The model has four states: ‘non‐diabetes’, ‘diabetes’, ‘dialysis’ and ‘dead’, and ‘ischemic heart disease’ and ‘stroke’ were included as events that occurred in each state. The effect of walking was included as changing the rate of transition and incident rates of events.
Results
After 10 years, the numbers of subjects with diabetes were 4.3 and 7.3% lower for daily increase of 3,000 and 5,000 steps, respectively. The numbers of cases of ischemic heart disease and stroke also decreased. Lower medical costs were also seen according to the daily increase in steps. In 10 years, the total medical costs were 5.2 and 8.4% lower for 3,000 and 5,000 steps increase, respectively. The cost reduction associated with a daily increase of 3,000 steps walked was calculated as ¥0.00146 for each step.
Conclusions
Walking is one of the most common and accessible forms of exercises. The present results suggested that walking reduced the medical costs associated with lifestyle‐related disease, which will have a large impact on health policy.
Keywords: Diabetes, Medical costs, Simulation
Introduction
Recently, the prevalence of lifestyle‐related disease, especially diabetes, has increased and the associated medical costs have become a considerable part of the overall medical financial burden1. In Japan, the medical cost associated with diabetes, ischemic heart disease and stroke was estimated to be approximately ¥4.9 trillion; that is, approximately 15% of the total medical cost in 20042.
Physical inactivity is thought to play a part in the recent increase in lifestyle‐related disease, and regular exercise is recommended for health maintenance and disease prevention3. Walking is one of the most common, popular and accessible exercises, and is believed to prevent some diseases, especially those associated with lifestyle. In fact, there is some epidemiological evidence that walking decreases the risk of diabetes, ischemic heart disease and stroke6. Therefore, it is expected that the medical costs associated with lifestyle‐related disease can be reduced by walking. However, few quantitative studies have been carried out, and the effect of walking on medical cost is unclear in the Japanese population.
The purpose of the present study was to evaluate the effect of walking on medical costs using a simulation model mainly focusing on diabetes in the Japanese population.
Materials and Methods
Model
We constructed a Markov model focusing on diabetes to estimate the change in the medical cost of diabetes and related diseases by walking (Figure 1). The following three states, ‘normal’, ‘border’ and ‘diabetes’ were selected to represent the diabetes status. The ‘border’ represents people with borderline diabetes. The ‘border’ was combined with ‘normal’, because subjects with borderline diabetes are generally untreated and do not incur any diabetes‐related medical costs. This combined group was termed ‘non‐diabetes’. As complications of diabetes, we included ‘dialysis’, ‘ischemic heart disease’ and ‘stroke’ in the model, because these complications are thought to account for a considerable part of diabetes‐related medical costs. Dialysis was included in the model as a state. Ischemic heart disease and stroke were included in the model as events, because most of the costs of these diseases were thought to be associated with the acute phase. We assumed that these events can occur in each state of the model except dialysis, because dialysis itself accounted for most of the medical costs associated with dialysis patients in Japan. The directions of transition between states are shown in Figure 1 as arrows. We assumed that the transition from ‘diabetes’ to ‘non‐diabetes’ did not occur. The rate of transition between states and the incident rates of events were determined based as much as possible on papers and statistical data published in Japan. The effect of walking was included in the model as changing the rate of transition between states and the incident rates of events. The target of our simulation was middle‐aged people, and the probabilities of this age group were used as much as possible.
Figure 1.
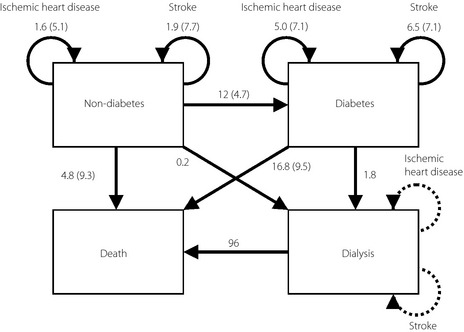
Simulation model. The arrows represent the directions of transition. The numbers associated with the arrows represent transition probabilities (per 1,000 person‐years) and the numbers in the parentheses represent the risk reduction (per 1,000 steps walking). The dashed arrows attached to the ‘dialysis’ means that the costs of the ‘ischemic heart disease’ and ‘stroke’ of dialysis patients were assumed to be included in the cost of dialysis.
Transition Probabilities
The transition probabilities were estimated using literature about Japanese subjects or statistical data published in Japan9.
The transition rate from ‘non‐diabetes’ to ‘diabetes’ was calculated as follows: for example, in a study of Japanese people, 15 and 29 incident cases of diabetes were observed in 5 years from 592 normal subjects and 140 borderline subjects, respectively9. Therefore, the incident rate of diabetes from ‘non‐diabetes’ per 1,000 person‐years was: (15 + 29)/(592 + 140)/5 ×1,000 = 12.0.
The incident rates of ischemic heart disease and stroke were taken from a Japanese large prospective study12. The rate of dialysis was estimated from statistical data as follows: in a National Health and Nutrition Survey in 2007, the number of cases of diabetes was estimated as 8,900,000 (total Japanese population was 104,000,000). The number of patients who started dialysis in the year 2008 was 37,355, of which 16,126 started dialysis because of diabetic nephropathy11. The incident rate of dialysis of non‐diabetic people per 1,000 person‐years was then estimated as (37,355 − 16,126)/(104,000 − 8,900) = 0.2, and the incident rate of dialysis in diabetics per 1,000 person‐years was estimated as 16,126/8,900 = 1.8. The transition probabilities and the references are listed in Table 1.
Table 1. Transition probabilities.
| Incidence ratea | References | |
|---|---|---|
| Non‐diabetes → diabetes | 12.0 | Shibasaki et al.9 |
| 11.4 | The Funagata Study: Daimon et al.10 | |
| Non‐diabetes → dialysis | 0.2 | An Overview of Regular Dialysis Treatment in Japan as of Dec. 31, 200811 |
| Stroke (non‐diabetes) | 1.9 | The Hisayama Study: Fujishima et al.12 |
| Myocardial infarction (non‐diabetes) | 1.6 | The Hisayama Study: Fujishima et al.12 |
| Non‐diabetes → death | 4.8 | Vital Statistics in Japan (2007) |
| Diabetes → dialysis | 1.8 | An Overview of Regular Dialysis Treatment in Japan as of Dec. 31, 200811 |
| Stroke (diabetes) | 6.5 | The Hisayama Study: Fujishima et al.12 |
| Myocardial infarction (diabetes) | 5.0 | The Hisayama Study: Fujishima et al.12 |
| Diabetes → death | 16.8 | The Funagata Study: Tominaga et al.13 |
| Dialysis → death | 96.0 | An Overview of Regular Dialysis Treatment in Japan as of Dec. 31, 200811 |
Incidence rate per 1,000 person‐years.
Risk Reduction by Walking
The quantitative risk reduction by walking could not be found in the Japanese literature, and was therefore estimated using literature from overseas14. For example, it was reported that the relative risk of diabetes with 15.7 metabolic equivalent tasks (METs) of exercise per week was 0.7714. A MET is equivalent to 20 min walking at a speed of 67 m/min26, therefore 15.7 METs per week is equivalent to walking 3 km per day, and if we assume that the length of a step is 70 cm, that is equivalent to 4,293 steps per day. Therefore the relative risk associated with one step per day was 0.77^(1/4,293) = 0.999939 (where ^ represents exponentiation) and risk reduction with 1,000 steps per day was 1 − 0.999939^1,000 = 0.059.
The relative risk of death in non‐diabetics by walking is reported to be 0.71 with 898 kcal walking per week23. In the study, one block (12 blocks = 1.6 km) was regarded to be equivalent to 8.3 kcal. Therefore 898 kcal per week is equivalent to 2.1 km per day, and if the length of a step is 70 cm, that is equivalent to 2,944 steps per day. Therefore the relative risk associated with one step per day was 0.71^(1/2,944) = 0.99988 and the risk reduction with 1,000 steps per day was 1 − 0.99988^1,000 = 0.1098. The risk reduction per 1,000 steps walked and the references are listed in Table 2.
Table 2. Risk reduction by walking (per 1,000 steps).
| Risk reductiona | References | |
|---|---|---|
| Non‐diabetes → diabetes | 5.9 | The Nurses' Health Study: Hu et al.14 |
| 3.5 | The Women's Health Study: Weinstein et al.15 | |
| Non‐diabetes → dialysis | NA | |
| Stroke (non‐diabetes) | 7.3 | The Nurses' Health Study: Hu et al.16 |
| 8.0 | The Harvard Alumni Health Study: Lee et al.17 | |
| Myocardial infarction (non‐diabetes) | 7.6 | The Nurses' Health Study: Manson et al.18 |
| 4.0 | The Harvard Alumni Health Study: Sesso et al.19 | |
| 2.6 | The Health Professionals' Follow‐up Study: Tanasescu et al.20 | |
| Non diabetes → death | 7.7 | The Harvard Alumni Health Study: Paffenbarger et al.21 |
| 8.1 | The Harvard Alumni Health Study: Paffenbarger et al.22 | |
| 11.0 | The Study of Osteoporotic Fractures: Gregg et al.23 | |
| Diabetes → dialysis | NA | |
| Stroke (diabetes) | 7.1 | The Nurses' Health Study: Hu et al.24 |
| Myocardial infarction (diabetes) | 7.1 | The Nurses' Health Study: Hu et al.24 |
| Diabetes → death | 9.5 | The National Health Interview Survey (NHIS): Gregg et al.25 |
| Dialysis → death | NA |
Risk reduction per 1,000 steps (%). NA, not available.
The values of transition rate and risk reduction used in the calculation were determined from these values and are shown in Figure 1.
Estimation of Medical Costs
The medical costs associated with each status and events were estimated from public statistical data in Japan. The details of the method of estimation have been reported elsewhere27. For example, in the Survey of Medical Care Activities in Public Health Insurance in 2008, the medical costs associated with diabetes were reported as ¥11,246,310,840 for 30,737 cases of hospitalization and ¥35,413,890,370 for 2,088,768 cases of outpatients (1 month). Therefore, the medical costs associated with diabetes per month were estimated as:(11,246,310,840 + 35,413,890,370)/(30,737 + 2,088,768) = 22 014.7.
Therefore, the medical costs per year (in thousands of yen) were estimated as 264.2 for diabetes. Other medical costs per year (in thousands of yen) were estimated as 4,781.2 for dialysis, 820.3 for myocardial infarction and 1,379.0 for stroke.
The medical costs in the present study are represented in ‘yen’. To convert yen to US dollars, multiply by 0.0126 (as of 13 November 2012).
Simulation
As aforementioned, the target of our simulation was middle‐aged Japanese people. In this simulation, the medical cost in 1,000 hypothetical subjects was calculated during 10 years according to their walking status, namely no increase, and a daily increase of 3,000 and 5,000 steps. The cycle was 1 year, and the costs and others were calculated per cycle and added up for 10 years.
In the National Health and Nutrition Survey in 2007, the prevalence of diabetes was 8.0% and therefore, 80 of the 1,000 subjects were assumed to be diabetes in the initial state. The medical cost of non‐diabetic subjects was assumed to be zero in the simulation. The same survey reported that 55.5% of the diabetic patients received medical care, and therefore this percentage of the total medical costs of diabetes patients was included.
As the central part of this model was ‘diabetes’, the (one‐way) sensitivity analyses were carried out by changing the parameters related to diabetes; that is, the transition rate from non‐diabetes to diabetes, and the risk reduction of the rate by walking.
Results
The number of patients after 10 years and the total number of events during 10 years are shown in Table 3. The numbers of cases of diabetes and death became lower according to the daily increase in steps walked. After 10 years, the numbers of cases with diabetes and death were 4.3 and 7.3%, and 25.3 and 38.5% lower for 3,000 and 5,000 steps, respectively. The numbers of cases of ischemic heart disease and stroke also decreased according to the daily increase in steps. During 10 years, the numbers of cases of ischemic heart disease and stroke were 16.2% (25.5%) and 21.0% (32.5%) lower for 3,000 (5,000) steps, respectively.
Table 3. Number of patients after 10 years and total number of events during 10 years.
| Diabetes* | Dialysis* | Death* | Ischemic heart disease† | Stroke† | |
|---|---|---|---|---|---|
| 0 | 157 | 2.64 | 59 | 20 | 24 |
| +3,000 steps | 150 (−4.3%) | 2.61 (−1.2%) | 44 (−25.3%) | 16 (−16.2%) | 19 (−21.0%) |
| +5,000 steps | 146 (−7.3%) | 2.59 (−2.1%) | 36 (−38.4%) | 15 (−25.5%) | 16 (−32.5%) |
The numbers in parenthesis are the relative reduction compared with the case of ‘0’. *Number of patients after 10 years. †Total number of events during 10 years.
The medical costs during 10 years are shown in Table 4, and were also lower according to the daily increase in steps. In 10 years, the total medical costs were ¥15.6 million and ¥25.0 million lower for 3,000 and 5,000 steps, respectively. That is an approximate 5.2 and 8.4% of the total medical cost during 10 years. Taking into account death, the cost reduction was calculated as ¥0.00146 for each step when there was a daily increase of 3,000 steps walked.
Table 4. Medical costs during 10 years (millions of yen) and relative reduction.
| Total | Diabetes | Ischemic heart disease | Stroke | Dialysis | |
|---|---|---|---|---|---|
| 0 | 297.5 | 180.2 | 14.5 | 31.1 | 71.8 |
| +3,000 steps | 281.9 (−5.2%) | 173.9 (−3.4%) | 12.3 (−15.5%) | 24.6 (−20.9%) | 71.1 (−0.9%) |
| +5,000 steps | 272.5 (−8.4%) | 169.9 (−5.7%) | 35.5 (−24.5%) | 21.0 (−32.4%) | 70.7 (−1.5%) |
The numbers in parenthesis are the relative reduction compared with the case of ‘0’.
The results were relatively insensitive to the changes of parameters about diabetes. According to the 10% change of the transition rate from non‐diabetes to diabetes, the cost reduction changed by approximately 6.3%, and according to the 10% change of the risk reduction of the rate from non‐diabetes to diabetes by walking, the cost reduction changed by approximately 6.8%.
Discussion
We have developed a simulation model focusing on diabetes in the Japanese population and calculated the medical costs associated with walking. We found that medical costs can be reduced by walking, and the reductions were 5.2 and 8.4% for a respective daily increase of 3,000 and 5,000 steps. A large part of the reduction in medical costs came from the reduced medical costs associated with diabetes and stroke. Diabetes accounted for approximately 60% of the total medical cost in this simulation, and the contribution to the reduction of the medical cost was large despite the small reduction in the number of diabetes patients (4.3%). It should be noted that the potential medical cost reduction for diabetes was approximately twice as much as the estimated value, because the estimated value was calculated from the medical cost of diabetes patients receiving medical care (55.5% of the diabetes patients). In contrast, stroke accounted for approximately 10% of the total medical cost in this simulation, the contribution to the reduction of the medical cost was large. Unlike Western countries, stroke is reportedly more common than ischemic heart disease in the Japanese population12. In fact, the medical cost associated with stroke was approximately 2.3‐fold as much as the medical cost associated with ischemic heart disease in the 2004 statistics2. Furthermore, it has been suggested that the risk reduction by walking was greater for stroke, especially for ischemic stroke, than for coronary heart disease7. These facts and the present results could suggest that the medical cost reduction by walking is more effective in the Japanese population than in others.
Many studies have examined the medical costs associated with physical inactivity by simulation29 or direct estimation31; however, most of them were from overseas and the results cannot be applied to the Japanese because of the differences in the incidence of disease and the healthcare systems. In our model, the parameters used in the simulation were taken as much as possible from studies with Japanese subjects, and the medical costs were also estimated from Japanese statistical reports. A direct estimation of the reduction of medical costs associated with walking has been reported from Japan36. In that study, compared with subjects walking less than 0.5 h/day, the reductions in medical costs per month were ¥700 and ¥2,600 for subjects walking 0.5–1 h/day and more than 1 h/day, respectively. If we assume that the speed of walking is 67 m/min and the length of a step is 70 cm, the reduction of medical cost was estimated as ¥0.0054 per step. If we take into account that our estimate might be low due to the simplicity of the model (see below), our estimate (¥0.00146 per step) did not contradict the results of the reported study.
As with many simulation studies, the present study had several limitations mainly coming from the simplification of the real world. First, our model was focused on diabetes, and other medical conditions were ignored. As suggested by many reports in the literature, physical activity has beneficial effects on many medical conditions37, and including these conditions might increase the medical cost reduction by walking. Second, the structure within health statuses (‘non‐diabetes’ or ‘diabetes’) was ignored. In the model, the transition probabilities and medical costs were assumed to be equal for all subjects within a status. In reality, however, there were subjects with different sex, age and severity in each status, and the transition probabilities or event rates would be different according to the characteristics of the subjects. Furthermore, the medical cost of diabetes would also be different according to the characteristics (severity) of the subjects. If the severity of diabetes is decreased by walking, the medical cost is also expected to decrease and, as a consequence, the reduction in medical cost by walking becomes larger. This effect was also not included in our model.
Despite the limitations, to the best of our knowledge, the present study was the first simulation study that focused on diabetes in the Japanese population, and gave a consistent result with a direct estimation. The medical costs associated with lifestyle‐related diseases, especially diabetes, are increasing rapidly. In Japan, the medical cost associated with diabetes, ischemic heart disease and stroke was estimated to be approximately ¥4.9 trillion in 2004. Applying our estimate of a cost reduction of 5.5% associated with a daily increase of 3,000 steps walked, it would save approximately ¥255 billion. Walking is one of the most common, popular and accessible exercises available to most people, and if the medical costs associated with lifestyle‐related diseases can be reduced by walking, it will have a large impact on health policy. Although the beneficial health effects associated with walking have been advocated, to date very few quantitative discussions, especially in terms of medical cost, have been published. We hope that our present study will become the starting point of such discussions.
Acknowledgement
This work was supported by a Health Science Research Grant (Research on Diabetes H18‐002) from the Ministry of Health, Labour and Welfare of Japan. No competing interests declared.
(J Diabetes Invest, doi: 10.1111/jdi.12114, 2013)
References
- 1.van Dieren S, Beulens JW, van der Schouw YT, et al The global burden of diabetes and its complications: an emerging pandemic. Eur J Cardiovasc Prev Rehabil 2010; 17(Suppl. 1): S3–S8 [DOI] [PubMed] [Google Scholar]
- 2.Ministry of Health Labour and Welfare . Annual Health, Labour and Welfare Report 2007–2008.
- 3.Ministry of Health Labour and Welfare of Japan . Exercise and Physical Activity Guide for Health Promotion 2006.
- 4.Haskell WL, Lee IM, Pate RR, et al Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007; 116: 1081–1093 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization . Global Recommendations on Physical Activity for Health. 2010 [PubMed]
- 6.Jeon CY, Lokken RP, Hu FB, et al Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care 2007; 30: 744–752 [DOI] [PubMed] [Google Scholar]
- 7.Boone‐Heinonen J, Evenson KR, Taber DR, et al Walking for prevention of cardiovascular disease in men and women: a systematic review of observational studies. Obes Rev 2009; 10: 204–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murtagh EM, Murphy MH, Boone‐Heinonen J. Walking: the first steps in cardiovascular disease prevention. Curr Opin Cardiol 2010; 25: 490–496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shibazaki S, Tanaka T, Nagai M. Study of factors related to change in glucose intolerance in individuals. J Jpn Diabetes Soc 2001; 44: 387–392 (Japanese). [Google Scholar]
- 10.Daimon M, Oizumi T, Saitoh T, et al Decreased serum levels of adiponectin are a risk factor for the progression to type 2 diabetes in the Japanese Population: the Funagata study. Diabetes Care 2003; 26: 2015–2020 [DOI] [PubMed] [Google Scholar]
- 11.Patient Registration Committee . Japanese Society for Dialysis Therapy, An Overview of Regular Dialysis Treatment in Japan as of Dec. 31, 2008. Japanese Society for Dialysis Therapy, Tokyo, 2009. (Japanese). [Google Scholar]
- 12.Fujishima M, Kiyohara Y, Kato I, et al Diabetes and cardiovascular disease in a prospective population survey in Japan: the Hisayama Study. Diabetes 1996; 45(Suppl. 3): S14–S16 [DOI] [PubMed] [Google Scholar]
- 13.Tominaga M, Eguchi H, Manaka H, et al Impaired glucose tolerance is a risk factor for cardiovascular disease, but not impaired fasting glucose. The Funagata Diabetes Study. Diabetes Care 1999; 22: 920–924 [DOI] [PubMed] [Google Scholar]
- 14.Hu FB, Sigal RJ, Rich‐Edwards JW, et al Walking compared with vigorous physical activity and risk of type 2 diabetes in women: a prospective study. JAMA 1999; 282: 1433–1439 [DOI] [PubMed] [Google Scholar]
- 15.Weinstein AR, Sesso HD, Lee IM, et al Relationship of physical activity vs body mass index with type 2 diabetes in women. JAMA 2004; 292: 1188–1194 [DOI] [PubMed] [Google Scholar]
- 16.Hu FB, Stampfer MJ, Colditz GA, et al Physical activity and risk of stroke in women. JAMA 2000; 283: 2961–2967 [DOI] [PubMed] [Google Scholar]
- 17.Lee IM, Paffenbarger RS Jr. Physical activity and stroke incidence: the Harvard Alumni Health Study. Stroke 1998; 29: 2049–2054 [DOI] [PubMed] [Google Scholar]
- 18.Manson JE, Hu FB, Rich‐Edwards JW, et al A prospective study of walking as compared with vigorous exercise in the prevention of coronary heart disease in women. N Engl J Med 1999; 341: 650–658 [DOI] [PubMed] [Google Scholar]
- 19.Sesso HD, Paffenbarger RS Jr, Lee IM. Physical activity and coronary heart disease in men: the Harvard Alumni Health Study. Circulation 2000; 102: 975–980 [DOI] [PubMed] [Google Scholar]
- 20.Tanasescu M, Leitzmann MF, Rimm EB, et al Exercise type and intensity in relation to coronary heart disease in men. JAMA 2002; 288: 1994–2000 [DOI] [PubMed] [Google Scholar]
- 21.Paffenbarger RS Jr, Hyde RT, Wing AL, et al Physical activity, all‐cause mortality, and longevity of college alumni. N Engl J Med 1986; 314: 605–613 [DOI] [PubMed] [Google Scholar]
- 22.Paffenbarger RS Jr, Hyde RT, Wing AL, et al The association of changes in physical‐activity level and other lifestyle characteristics with mortality among men. N Engl J Med 1993; 328: 538–545 [DOI] [PubMed] [Google Scholar]
- 23.Gregg EW, Cauley JA, Stone K, et al Relationship of changes in physical activity and mortality among older women. JAMA 2003; 289: 2379–2386 [DOI] [PubMed] [Google Scholar]
- 24.Hu FB, Stampfer MJ, Solomon C, et al Physical activity and risk for cardiovascular events in diabetic women. Ann Intern Med 2001; 134: 96–105 [DOI] [PubMed] [Google Scholar]
- 25.Gregg EW, Gerzoff RB, Caspersen CJ, et al Relationship of walking to mortality among US adults with diabetes. Arch Intern Med 2003; 163: 1440–1447 [DOI] [PubMed] [Google Scholar]
- 26.Ainsworth BE, Haskell WL, Whitt MC, et al Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 2000; 32: S498–S504 [DOI] [PubMed] [Google Scholar]
- 27.Kato M, Goto A, Tanaka T, et al Health effects of walking – an attempt at quantitative evaluaiton by simulation focusing on diabetes. Obes Diab (himan to tonyobyo) 2010; 9(Suppl. 9): S39–S47 (Japanese). [Google Scholar]
- 28.Japan Arteriosclerosis Longitudinal Study (JALS) Group . Japan Arteriosclerosis Longitudinal Study‐Existing Cohorts Combine (JALS‐ECC): rationale, design, and population characteristics. Circ J 2008; 72: 1563–1568 [DOI] [PubMed] [Google Scholar]
- 29.Hatziandreu EI, Koplan JP, Weinstein MC, et al A cost‐effectiveness analysis of exercise as a health promotion activity. Am J Public Health 1988; 78: 1417–1421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jones TF, Eaton CB. Cost‐benefit analysis of walking to prevent coronary heart disease. Arch Fam Med 1994; 3: 703–710 [DOI] [PubMed] [Google Scholar]
- 31.Pratt M, Macera CA, Wang G. Higher direct medical costs associated with physical inactivity. Phys Sportsmed 2000; 28: 63–70 [DOI] [PubMed] [Google Scholar]
- 32.Katzmarzyk PT, Gledhill N, Shephard RJ. The economic burden of physical inactivity in Canada. CMAJ 2000; 163: 1435–1440 [PMC free article] [PubMed] [Google Scholar]
- 33.Wang G, Pratt M, Macera CA, et al Physical activity, cardiovascular disease, and medical expenditures in U.S. adults. Ann Behav Med 2004; 28: 88–94 [DOI] [PubMed] [Google Scholar]
- 34.Oldridge NB. Economic burden of physical inactivity: healthcare costs associated with cardiovascular disease. Eur J Cardiovasc Prev Rehabil 2008; 15: 130–139 [DOI] [PubMed] [Google Scholar]
- 35.Janssen I. Health care costs of physical inactivity in Canadian adults. Appl Physiol Nutr Metab 2012; 37: 803–806 [DOI] [PubMed] [Google Scholar]
- 36.Tsuji I, Takahashi K, Nishino Y, et al Impact of walking upon medical care expenditure in Japan: the Ohsaki Cohort Study. Int J Epidemiol 2003; 32: 809–814 [DOI] [PubMed] [Google Scholar]
- 37.Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ 2006; 174: 801–809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kruk J. Physical activity in the prevention of the most frequent chronic diseases: an analysis of the recent evidence. Asian Pac J Cancer Prev 2007; 8: 325–338 [PubMed] [Google Scholar]


