Abstract
College matriculation begins a period of transition that is marked by new freedoms and responsibilities by and increases in a variety of risky behaviors, including smoking. Trauma and post-traumatic stress disorder (PTSD) are well-established risk factors for smoking outcomes, and thus may be a point of intervention for college smoking. Yet, no studies have examined associations among trauma, PTSD, and smoking in college students. The present study provides such an examination. Matriculating student smokers (N=346) completed surveys in September (T1) and at five subsequent time points (T2-T6) over their first year of college. With latent growth analysis, we modeled smoking trajectories conditioned on PTSD symptom status (i.e., No PTSD Symptoms vs. Partial PTSD vs. Full PTSD). Results showed that, although smoking tended to decline during the first semester for all groups, significant risk for escalation in smoking during the second semester was conferred specifically by the presence of PTSD at matriculation. Interventions that offer support and resources to students entering college with PTSD may help to prevent smoking behaviors from escalating, and may ultimately prevent the adoption of daily smoking in later adulthood.
Keywords: College, Smoking, Trajectories
Introduction
Though once studied only as a sample of convenience, the current literature emphasizes the college population as one with distinctive mental health needs (Arnett, 2000). The college years are a time of increased autonomy, decreased adult supervision, and new social opportunities and relationships (Arnett, 2000; 2005). Together these can contribute to experimentation with or even permanent adoption of high-risk health behaviors, including smoking (Fromme, Corbin, & Kruse, 2008; Rigotti et al., 2000). Though smoking initiation typically occurs during adolescence (Substance Abuse and Mental Health Services Administration, 2006), those who already smoke may shift into heavier smoking patterns during the college years (Patterson, Lerman, Kaufman, Neuner, & Audrain-McGovern, 2004; Wechsler et al.,1998). Moreover, in contrast to drinking, which tends to drop off substantially post-graduation (Donovan, Jessor, & Jessor, 1983), college smoking is more likely to continue into later adulthood (Everett et al., 1999). Importantly, patterns of smoking behavior during college tend to be complex and typically do not follow a simple linear trajectory (Colder et al., 2008), and there are individual differences among student smokers with respect to smoking patterns over time. Thus, research examining factors that predict smoking trajectories is needed in order to help identify students at risk for long-term cigarette involvement and to aid in the understanding of and intervention for this behavior.
An important contributor to cigarette use is psychological distress, including distress resulting from traumatic experiences. As many as 2/3 of college students report lifetime trauma exposure (Marx & Sloan, 2003; Read, Ouimette, Colder, White, & Farrow, 2011; Scarpa et al., 2002), and many go on to experience significant post-traumatic stress (PTSD) symptoms. The DSM-IV TR defines PTSD as an anxiety disorder which follows trauma exposure (Criterion A), and which is characterized by re-experiencing of the trauma, avoidance of trauma stimuli, and hyper-arousal (Criteria B, C, and D). A large body of research has implicated trauma and PTSD in the etiology and maintenance of smoking (see Feldner, Babson, & Zvolensky, 2007a and Fu et al., 2007 for reviews). For example, individuals with PTSD have greater lifetime and current smoking rates (Acierno, Kilpatrick, Resnick, Saunders, & Best, 1996; Lasser et al., 2000), smoke more heavily (Beckham et al., 1995; Feldner et al., 2007a), have more difficulty quitting smoking (Hapke et al., 2005; Lasser et al., 2000), and are more likely to relapse to smoking after a quit attempt (Zvolensky et al., 2007) than those without this diagnosis.
Though college students are at risk for trauma exposure and associated distress (Amir & Sol, 1999; Bernat, Ronfeldt, Calhoun, & Arias, 1998; Smyth, Hockmeyer, Heron, Wonderlich, & Pennebacker, 2008), no studies have examined trauma and PTSD as risk factors for smoking in college samples. This is an important area for inquiry, as trauma and PTSD have shown prospective relations with alcohol and other substance behavior in college (Read et al., in press).
Trauma, Traumatic Stress, and Smoking
Smoking to cope with, or to self-medicate, distress or other negative emotions has been forwarded as one mechanism that might explain the PTSD-smoking link (Khantzian, 2003; Saladin, Brady, Dansky, & Kilpatrick, 1995). Recent research supports such a pathway; individuals with PTSD expect smoking to reduce negative affect and are motivated to smoke to regulate negative mood (Feldner et al., 2007b; Marshall et al., 2008) and anxiety levels (Zvolensky et al., 2004), and thus may use cigarettes as a means of coping with PTSD symptoms (Jacobsen, Southwick, & Kosten, 2001).
Though they did not examine PTSD symptoms per se, several college-based studies have identified a link between negative affect more broadly and cigarette use (e.g., McCormack et al., 1993; Morrell, Cohen, & McChargue, 2010; O’Hare & Sherrer, 2000). Two recent studies in particular point to an affect management pathway for these young adults. In 2007, Nichter, Nichter, and Carkoglu reported smoking to alleviate distress to be a common motivation for college smokers. More recently still, Magid et al. (2009) found negative affect to be among the strongest prospective predictors of smoking in college students. Together, these findings show that college students smoke to alleviate distress, and suggest that college students with PTSD could be at risk for smoking for this purpose.
Stability and Change in Smoking Behaviors: The Importance of Transitions
Work by Parra et al. (2007) and others (e.g., Bartholow, Sher, & Krull, 2003; Jackson, Sher, Gotham & Wood, 2001; Schulenberg et al., 2002) has emphasized the importance of transitional periods in emerging adulthood with respect to substance use. Matriculation into college is one important developmental transition, yet there are others that occur even within that first college year. Indeed, in just their first year of college, students enter a new social environment, occupy it for a period of time, leave it mid-year for a sustained (winter) break, and then re-transition back into the college environment when the break is over. Even those students not living on campus or away from home will experience such fluctuation, albeit to a lesser extent. These fluctuations have been linked to substance use behaviors (Del Boca et al., 2004; Lee et al., 2009; Maggs, Williams, & Lee, 2011), and may have implications for PTSD and smoking. During these periods of transition, students with PTSD may turn to behaviors such as smoking in an effort to manage the many changes and challenges that they face as more familiar resources are absent or less available.
Summary and Present Study
The first year of college represents a major step into “emerging adulthood” and is a time of increased autonomy, social change, and experimentation with risk behaviors. As such, this is an important time during which to examine smoking. Though an abundant literature has identified a link between PTSD and smoking in older adult populations, the extent to which PTSD may confer risk for smoking has not been examined in college students. Moreover, prospective investigations of relations between PTSD and smoking have been few.
Accordingly, the objective of the present study was to provide what is to our knowledge the first examination of the prospective relationship between post-traumatic stress and smoking in students at their transition into and over the course of the first college year. We hypothesized that significant PTSD symptoms at college matriculation (T1) would be associated with elevated risk for smoking over the first year of college. We posited that this would be reflected in higher initial levels of cigarette use at matriculation, and greater escalation of smoking across the freshman year. As prior research has shown the first year of college to be one of variability in smoking (e.g., Colder et al., 2008), we expected escalation to follow a complex, not necessarily linear, trajectory.
It has been widely noted that anxiety disorders such as PTSD share nonspecific general negative affectivity (Simms, Watson, & Doebbelling, 2002, Watson & Clark, 1998) – a feature that also has been implicated in smoking (Ameringer & Leventhal, 2010; Kahler et al., 2010; Kassle, Stroud, & Paronis, 2003). Thus, we included trait negative affectivity in our models in order to isolate the unique influence of PTSD, above and beyond the more general influence of negative affectivity.
Method
Participants
Participants were enrolled in an ongoing longitudinal study of PTSD and substance use behavior in college. All students who reported smoking at some point during the first year of college were included in the present analyses. The sample for the present study was comprised of 346 (66% female) participants. At T1, the average age was 18.10 (SD=0.44). Seventy-nine percent self-identified as Non-Hispanic Caucasian (n = 273), 8% as Asian (n =29), 5% as Black (n =18), 4% as Hispanic/Latino (n = 12), less than 1% as Hawaiian/Pacific Islander (n=1), and 3% as multi-racial (n =11). Two participants did not report ethnicity. Roughly equal numbers of participants reported living on (n = 170) and off campus (n =174). Of those living off-campus, most (89%, n=155) reported living at home with family. Eligibility, recruitment, and sample selection procedures are described below.
Procedure
Initial recruitment screen
Details of this procedure are published elsewhere (Read et al., 2011; Read et al., in press). Participants were incoming freshmen at two mid-size public universities in the northeastern and southeastern United States. In the summer prior to matriculation, an initial screening procedure was implemented to identify those eligible for our longitudinal study. After data cleaning and deletion of cases with significant missing data, the final screened sample consisted of 3,014 students.
Longitudinal sample selection
Next, students were selected for participation in the longitudinal study using demographic, trauma exposure and PTSD symptom data from the eligibility screen. To ensure sufficient representation of students with significant traumatic stress, we invited for participation all those who endorsed (1) at least one Criterion A (components A1 and A2, see below) trauma and (2) at least one symptom from each of the three PTSD symptom clusters (i.e., B, C, and D). Across sites, a total of 649 participants met these criteria. Another 585 students who did not meet trauma criteria were selected randomly from the screened sample and invited for longitudinal follow-up.
E-mails were sent to this selected sample (N = 1,234) inviting participation in the longitudinal study, and including a link to the study website that contained the baseline (September; T1) survey. Participants received a $20 gift card for completion of the baseline survey. Eighty-one percent (N=1,002) of those invited to participate in the study completed the baseline survey in September of their freshmen year. This constituted the final longitudinal sample. Among these, those who entered college (T1) with either full or partial PTSD (see below) smoked more (based on quantity-frequency index, see below) than did those without significant PTSD symptoms, F(2, 955) =6.02, p<.01.
This longitudinal sample was then assessed three more times (October [T2], November [T3], December [T4]) in the first semester and twice (February [T5], April [T6]) during the second semester. Data from T1-T6 were used in the present study. Across cohorts, the 1- year retention rate was 91.3%. Because we were interested in smoking trajectories in the first year of college, analyses for this study were conducted only for participants who reported having smoked in the year prior to matriculation, or who reported smoking at least once over the six assessment points (N = 346). Students meeting these criteria did not differ from the larger prospective sample with respect to sex, age, or ethnicity.
Measures
Cigarette Use
At each assessment, participants were asked to indicate how often they had smoked in the past month. Response options included: 0=never in the past month; 1=about once in the past month; 2=2-3 times in the past month; 3=once or twice a week; 4=3-4 times a week; 5=nearly every day; and 6=everyday. Participants also reported on typical quantity of cigarettes smoked in the past month. Response options for this item included: 0=didn’t smoke in the past month; 1=1-5 cigarettes per day; 2=6-10 cigarettes per day; 3=11-15 cigarettes per day; 4=16-20 cigarettes per day; and 5=more than 20 cigarettes per day. At baseline (T1) only, participants also were asked to report on the frequency and quantity of smoking over the past year.
The best way to assess the kind of low-level and/or infrequent smoking that is commonly observed in adolescents and college students has been the topic of some debate (Colby, Tiffany, Shiffman, & Niaura, 2000; Harris et al., 2009; Mermelstein et al., 2002). Data suggest that quantity-frequency indices show strong associations with gold-standard interview assessments, and yield reasonable estimations of smoking behavior in low-level smokers (Harris et al., 2009). Thus, in this college sample we modeled smoking behaviors with an index of smoking quantity X frequency based on our ordinal categorical scales (see above) at each time point. This index allowed for estimation of typical smoking behavior while reducing skew that could compromise model estimation (see Duncan et al., 2006).1 Quantity and Frequency items were highly correlated (.81) with one another across the six time points. This suggests that students who smoked more frequently also smoked more cigarettes, and supports the choice to combine these indicators. The possible range for this variable was 0 – 30.
Big Five Inventory
To isolate the unique influences of PTSD, we controlled for trait negative affectivity in all of our models. We assessed this construct with the 8-item Neuroticism subscale of the Big Five Inventory (BFI; John & Srivastava, 1999), a self report measure that assesses five personality dimensions: Openness, Conscientiousness, Extraversion, Agreeableness, and Neuroticism. Items are short phrases based on adjectives describing prototypical personality dimension features and are scored using a 5-point Likert scale that ranges from disagree strongly to agree strongly. Representative items from the neuroticism subscale include “is sad, depressed” and “worries a lot.” Internal reliability for this scale was good (alpha = .85). This measure was administered at baseline (T1).
Trauma Exposure
The DSM-IV-TR defines trauma as exposure to a traumatic event (A.1), accompanied by fear, helplessness, or horror (A.2). The Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000©) is a 22-item self-report questionnaire that assesses a range of traumatic experiences consistent with the DSM- IV-TR definition, including the subjective responses that comprise Criterion A.2. This measure has demonstrated good psychometric properties, and has been used in a range of populations, including college students (Kubany et al., 2000). The TLEQ was used to assess trauma exposure at baseline.
Traumatic Stress Symptoms
Baseline traumatic stress symptoms were assessed using the PTSD Checklist-Civilian Version (PCL-C; Weathers, Huska, & Keane, 1991; Weathers, Litz, Herman, Huska, & Keane, 1993). This 17-item measure assesses Criteria B (re-experiencing), C (avoidance/numbing), and D (arousal) of the PTSD construct consistent with the DSM-IV-TR. It has been used in a variety of populations, including college students, and corresponds strongly to gold-standard interview measures of PTSD (Andrykowski, Cordova, Studts, & Miller, 1998; Lang, Laffaye, Satz, Dresselhaus, & Stein, 2003). Participants rated how much they had been bothered by each symptom in the past month on a 5-point scale. A computer-based prompt reminded them of the specific Criterion A trauma(s) they had endorsed, embedding these Criterion A traumas in the PCL instructions on each web page. Thus, PTSD symptoms were queried specifically in response to their own Criterion A stressors. Internal reliability in this sample was strong (total PCL score: .93). As the PCL was designed to assess the full multi-dimensional PTSD construct all items from the Re-experiencing (Repeated, disturbing memories, thoughts, or images of the stressful experience(s); Suddenly acting or feeling as if the stressful experience(s) were happening again) Avoidance/Numbing (e.g., “Avoiding activities or situations because they reminded you of the stressful experience(s)”, “Feeling emotionally numb or being unable to have loving feelings for those close to you”), and Hyperarousal (e.g., Being “super-alert” or watchful or on guard”; “Feeling jumpy or easily startled”) symptom clusters were assessed. Internal reliability within each cluster also was strong (Re-Experiencing: .86, Avoidance/Numbing: .83, Hyperarousal: .83).
Many trauma-exposed individuals experience significant distress that falls below the threshold of full PTSD, but that still is associated with significant impairment and deleterious outcomes (Mylle & Maes, 2004; Mendlowicz & Stein, 2000; Schnurr et al., 2000; Schnurr, Friedman, & Vernardy, 2002; Zlotnick, Franklin, & Zimmerman, 2002). Accordingly, in the present study we modeled the influence of subsyndromal PTSD on smoking outcomes by creating a “Partial PTSD” group. Partial PTSD has been operationalized in different ways, but usually consists of a criterion A event and a criterion B symptom, and some combination of criterion C and D symptoms (Franklin et al., 2002; Schnurr et al., 2000). Based on this, our “Partial PTSD” group was comprised of students who reported Criterion A trauma exposure and at least one above threshold symptom in each of the three symptom clusters (minimum total of four symptoms). Those below threshold for Full or Partial PTSD were classified in the “No PTSD” group.
Scores for PTSD group designation were calculated with Blanchard et al.’s (1996) empirically derived cut-scores in which PCL items were rated as either above or below severity threshold. Items rated as 3 or 4 (depending on the item) or higher were scored as a “1”. All other ratings were scored as a “0”. Thus, each of the 17 items was dichotomously scored as “present” or “absent”. Symptoms were summed within each cluster. Consistent with the DSM-IV-TR, participants were classified in the Full PTSD group if they reported at least one Criterion A trauma (A.1. exposure and A.2. fear/helplessness/ horror) and one or more B (Re-experiencing) symptoms, three or more C (Avoidance/Numbing) symptoms, and two or more D (Arousal) symptoms, for a minimum total of seven symptoms.
Finally, to capture PTSD symptom severity, we also created a continuous variable representing the number of PTSD symptoms endorsed by summing across the 17 dichotomously scored PCL items. Participants with no criterion A event received a score of zero on this index. This variable was entered into a secondary analysis in order to test the effects of PTSD on smoking trajectories based on categorical and continuous representations of PTSD.
Data Analytic Plan
We began by examining patterns of missing data. With the exception of 32 participants who were missing data on the past month smoking index at baseline (T1), all participants had complete data on all other Time 1 variables. Sixty-seven percent (n = 230) of the participants completed all six assessments, 86 % (n=296) completed at least 5 of the 6 assessments, and only 1% (n = 4) completed two assessments or less. To examine the potential influence of missing data from other time points, we compared those with complete smoking data at all six time points (n=230; 66.5%) and those who were missing at least one time point of smoking data (n=116; 33.5%) on baseline variables. These comparisons revealed no significant differences between those with complete smoking data and those who were missing one or more time points on T1 smoking, trauma status, site, sex, or neuroticism (all ps > .05). Those with missing data were more likely to be smokers at baseline (past month or past year), χ2 (1)=7.54, p = .006. To reduce bias that can result from missing data, we used full-information maximum likelihood with robust estimation, rather than casewise deletion.
After data cleaning, we examined frequencies of trauma, PTSD, and cigarette use, as well as descriptive characteristics of our participants based on their PTSD status. Our central question was whether baseline PTSD symptom status (Trauma and PTSD Group) predicted change in smoking across the first year of college. We used latent growth models to test our question of interest as they provide an analytic framework to describe sample average trajectories as well as individual differences in growth and predictors of individual differences in growth (Curran & Muthen, 1999). We first tested a series of unconditional growth models to determine the overall shape of the smoking trajectory (Step 1), and then conditional growth models with trauma and PTSD status as predictors of growth (Step 2).
Unconditional growth models of smoking
Latent growth models were estimated in Mplus version 5.2 (Muthen & Muthen, 2008). As is typical of smoking data in college populations, the observed smoking variables were skewed (all skewness indices > 2.50) and thus robust maximum likelihood estimation was used to correct model fit indices and standard errors for the effects of non-normality. To test competing trajectory models, nested model tests were performed using robust maximum likelihood chi-square difference tests. We also report the Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), and Root Mean Square Approximation (RMSEA). According to Hu and Bentler (1999), CFI >.95, TLI > .95, and RMSEA < .05 indicate that a model fits the data well.
Conditional growth models of smoking by PTSD symptom status
Next, we modeled trajectories of smoking based on PTSD symptom categories. For this, participants were categorized into one of three PTSD groups based on their responses to the TLEQ and PCL: (1) a No PTSD group with no significant PTSD symptoms; (2) a Partial PTSD group, including those with a criterion A trauma and at least 1 symptom from each cluster, but below threshold for a full PTSD diagnosis; and (3) a Full PTSD group (those with criterion A trauma and at least 1 B, 3 C, and 2 D symptoms).
Using these three PTSD groups, we created two dummy coded variables with No PTSD as the referent group. Comparison across these dummy coded variables allowed us to examine the relative contribution of Partial and Full PTSD symptoms to smoking behavior when compared with No PTSD. To control for the possible contribution of general negative affectivity, the conditional growth model included baseline trait negative affect with BFI neuroticism subscale. Site and gender also were included as covariates. Additionally, we controlled for initial smoking status as students who do not have a history of regular smoking may have different smoking trajectories than students with recent prior smoking experience. We did this by grouping participants into two categories: those who endorsed past month or past year smoking at baseline (coded 1) and those who did not endorse smoking at baseline (coded 0). This variable was modeled as a covariate.
Finally, we conducted a secondary analysis to examine the effects of PTSD symptom severity on smoking trajectories. For this analysis, the dummy coded PTSD variables were replaced by the continuous variable representing PTSD symptom count. This allowed us to examine the effects of PTSD on smoking trajectories across categorical versus continuous representations of PTSD.
Results
Rates of Trauma, PTSD, and Smoking Involvement
Eighty-one percent of the sample (n=281) had experienced at least one Criterion A trauma. Among these, the average number of traumas was 3.46 (SD=2.29). Trauma types were diverse and included, but were not limited to, interpersonal traumas (e.g., unwanted sexual attention, n = 46, 16%; physical assault by partner, (n = 40, 14%), natural disasters (e.g., hurricane, flood, tornado, etc., n = 38, 14%), sudden/unexpected death of someone close (n = 187, 67%), life-threatening illness or injury of other (n = 131, 47%) or self (n = 21, 8%), and motor vehicle accidents (n = 45, 16%). Sixty-one percent of the sample (n=211) either had no trauma history (n=65), or reported minimal symptomatology (n = 146) despite having had a traumatic event. Nearly 19% (n= 64) met criteria for partial PTSD. Another 21% percent (n=71) met Full PTSD criteria. The mean number of PTSD symptoms endorsed was 4.19 (SD = 4.15).
At baseline (T1) participants reported average smoking of less than once per week in the past month, and smoked zero to five cigarettes per smoking day. The mean for the smoking quantity-frequency index varied across the year, with the highest smoking level observed at baseline (M = 2.98, SD = 4.90), and the lowest observed during the fourth assessment period (M = 2.08, SD = 4.17), which began in December and continued over winter break. Eighty-four percent of the sample (n=292) reported past year smoking at baseline, with the remaining 15% (n=53) not reporting smoking until a subsequent assessment point during the freshman year. Of these participants who did not report prior smoking at baseline, the majority (n=33; 62%) first reported smoking during the first semester. See Table 1 for smoking characteristics by PTSD group.
Table 1.
Comparison of Baseline Demographics and Self-Report Measures Based on PTSD Group Status
| No PTSD (n=211) |
Partial PTSD (n=64) |
Full PTSD (n=71) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | χ 2 | df | p | |
| Sex | |||||||||
| Female | 126 | 59.7 | 49 | 76.6 | 54 | 76.1 | 10.12 | 2 | .006 |
| Ethnicity | |||||||||
| Caucasian | 171 | 81.0 | 46 | 71.9 | 56 | 80.0 | 2.45 | 2 | .289 |
| Other | 40 | 19.0 | 18 | 28.1 | 15 | 20.0 | |||
| M | SD | M | SD | M | SD | F | df | p | |
| Age | 18.11 | .45 | 18.03 | .25 | 18.11 | .52 | 0.91 | (2, 343) | .403 |
| # Criterion A Events (TLEQ) | 1.99 | 2.07 | 3.64 | 2.12 | 4.49 | 2.76 | 38.66 | (2, 343) | .000 |
| PTSD Symptom Count (PCL - Blanchard cutoffs) |
1.52 | 1.93 | 5.95 | 1.98 | 10.54 | 2.27 | 561.37 | (2, 343) | .000 |
| Neuroticism (BFI) | 2.94 | 0.83 | 3.32 | 0.91 | 3.57 | 0.72 | 16.92 | (2, 343) | .000 |
| T1 Smoking (QF) (past month) | 2.66 | 4.91 | 3.16 | 5.28 | 3.72 | 4.49 | 1.18 | (2,311) | .301 |
| T1 Smoking Freq. (past month) | 1.74 | 2.04 | 1.93 | 2.05 | 2.71 | 2.31 | 5.12 | (2,311) | .007 |
| T1 Smoking Quant. (past month) | 0.75 | 0.86 | 0.85 | 0.91 | 0.86 | 0.79 | 0.59 | (2,311) | .555 |
Note. The No PTSD Group is comprised of those with No Criterion A (n=65) and Criterion A Only (n=146).
Smoking Over the First Year of College
Unconditional growth model
Visual inspection of means for the smoking across the 6 time points revealed a complex trajectory that did not appear to conform to a simple linear or polynomial function. In addition, the data pointed to a natural transition point at T4 (i.e., transition into and out of winter break) where there was a dramatic shift in the slope of smoking trajectories (see Figure 1). Accordingly, following recommendations by Bollen and Curran (2006), we proceeded to fit a piecewise LGCM. We chose T4 as our “knot” (i.e., transition point connecting two distinct growth factors; Flora, 2008). Piece one of the trajectory represented a growth factor capturing change in smoking from T1 to T4 (1st semester) and piece two of the trajectory represented change in smoking from T4 to T6 (2nd semester). This approach allowed us to model trajectories separately before and after this natural transition point. In our models, observations of smoking at each wave were specified as indicators of the latent growth factors with fixed factor loadings. An intercept factor was specified by setting manifest variable loadings to 1.0. Slope factor loadings were set such that the intercept represented baseline levels of smoking. Because the first piece of the model included four points of data, we were able to model both linear and quadratic growth factors. As the second piece included only three data points, only a linear growth factor was identified.
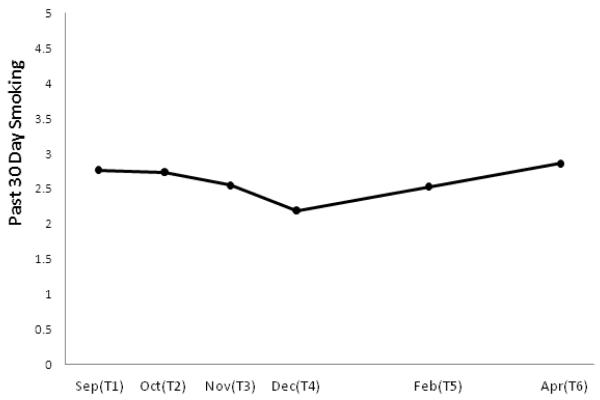
Figure 1.
Model-implied means for past 30 day smoking (quantity × frequency) for the six assessment points (T1-T6) during the first year of college. Unconditional growth model is shown.
In our first model we specified only an intercept. We then added linear growth factors in two pieces (semester 1 and semester 2), and finally added a quadratic growth factor to the first semester trajectory. Relative to the intercept only model, the addition of the linear growth factors for the first (T1-T4) and second (T4-T6) semesters resulted in significant improvement in model fit, Δχ2 (7) =36.47, p < .001. The addition of the quadratic growth factor to the first semester (T1-T4) also lead to significant model fit improvement, Δχ2 (5)=26.80, p < .001.
We examined means and variances in the growth factors. Significant means for growth factors suggest that the average within-person growth in smoking is different from zero, whereas significant variances suggest that there is between person variability in this change. In the final model with a quadratic trend for the first semester and a linear trend for the second semester, the variances for the intercept, first semester linear growth factor, and first semester quadratic growth factor were significant (ps < .05), whereas the variance for the second semester linear growth factor was not significant (p =.20). Only the means of the intercept (M=2.77, p < .001, 95% CI [2.27, 3.28]) and second linear growth factor (M=0.17, p=.002, 95% CI [0.06, 0.27]) were significantly different from zero. The means for the first semester linear (M=0.05, p = .795, 95% CI [−0.31, 0.41]) and quadratic (M = −0.08, p =.141, 95% CI [−0.19, 0.03]) growth factors were not statistically significant. However, visual inspection of mean smoking patterns suggested that smoking declined more rapidly towards the end of the first semester, and having specified the intercept as the first assessment likely resulted in a zero linear trend in the first semester. For descriptive purposes only, we re-ran the model with the intercepts for the growth factors set at T3 (November assessment), and results suggested a significant linear decline in smoking (M = −0.28, p =.001, 95% CI [−0.44, −0.11]). The linear increase in smoking over the second semester also remained significant (M= 0.17, p =.002, 95% CI [0.06, 0.27]). The mean for the first semester quadratic growth factor was not significant (M= −0.08, p = 0.141, 95% CI [−0.19, 0.03]), but the variance was significant (p < .01), and this factor contributed substantially to improvement in model fit. Accordingly, we retained the quadratic growth factor in our model.
Having established that smoking declined over the first semester, we once again set the intercepts for the growth factors at T1 for interpretability purposes. Thus, the final unconditional piecewise growth model consisted of a quadratic decline in smoking during the first semester (T1- T4) and then a linear increase in smoking in the second semester (T4 -T6). This model fit the data very well, χ2 (7)=2.32, p = .940, CFI = 1.00, TLI =1.04, RMSEA < .001, and accounted for 78%-98% of the variances in the observed smoking variables. This model is presented in Figure 1.
Conditional growth model Smoking as a function of post-traumatic stress
Next we estimated conditional models with the intercept specified at T1 and growth factors regressed on dummy coded PTSD group variables and covariates (site, gender, negative emotionality, and initial smoking status). The conditional model fit the data well, χ2 (23) =9.61, p = .993 CFI = 1.00, TLI =1.04, RMSEA < .001. The variance in each growth factor accounted for by the set of predictors was 9.6% for the intercept, 1.8% for the first semester linear growth factor, 10.0% for the second semester linear growth factor, and 1.3% for the first semester quadratic factor.
Covariate effects
Three of the four covariates had at least marginally significant effects on the intercept factor (ps < .10). The nature of these effects were such that greater levels of smoking at matriculation (T1) were reported by men (B = 1.07, SE = 0.56, p = .058, 95% CI [−0.04, 2.17]), students higher on neuroticism (B = 0.49, SE = 0.26, p = .059, 95% CI [−0.02, 1.01]), and as expected, students who endorsed smoking in the year prior to matriculation (B = 3.22, SE = 0.30, p < .001, 95% CI [2.63, 3.82]). There were no intercept differences by site. Initial smoking status was the only covariate associated with the first semester linear trajectory (B = −0.75, SE = 0.26, p = .004, 95% CI [−1.26, −0.24]), and site was the only covariate significantly related to the second semester linear trajectory (B = 0.15, SE = 0.06, p = .011, 95% CI [0.03, 0.26]).
PTSD effects
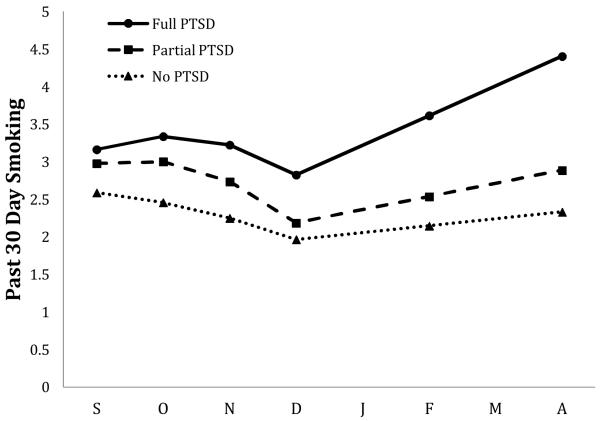
We also did not observe intercept differences in smoking based on PTSD status upon entry into college (ps > .30), and PTSD group did not predict first semester linear or quadratic growth factors (ps > .40). Thus, PTSD status did not impact smoking trajectories in the first semester of college; across PTSD groups, the typical trajectory over this period was characterized by a modest decline in smoking.
PTSD status was, however, a significant predictor of a linear increase in smoking in the second semester. Though there was no significant difference between the No PTSD and Partial PTSD groups (B = 0.08, SE = 0.13, p = .520, 95% CI [−0.17, 0.34]), the No PTSD group and Full PTSD groups had significantly different linear smoking trajectories in the second semester (B = 0.30, SE = 0.15, p = .039, 95% CI [0.02, 0.59]). PTSD status explained 3.1% of the variance in the second semester linear growth factor, above and beyond variance accounted for by the covariates.
We re-ran the model with each PTSD group as the referent group in order to examine whether the predicted mean of the second semester linear trend was significantly different from zero within each group. Results showed that the linear smoking trend for the second semester was significant and positive only for the Full PTSD group (predicted M = 0.40, SE = 0.14, p = .005, 95% CI [0.12, 0.67]). That is, participants with Full PTSD at matriculation tended to increase their smoking over the second semester, whereas smoking did not change significantly for the two groups lower in PTSD symptom severity. 2 These trajectories are depicted in Figure 2.
Figure 2.
Model-implied means for past 30 day smoking (quantity × frequency) for the six assessment points (T1-T6) during the first year of college. Growth model is conditioned on PTSD group. No PTSD was the referent group for these comparisons. Model controlled for site, negative affectivity, gender, and initial smoking status.
The results of our secondary analysis, with a continuous measure of PTSD symptom severity replacing the PTSD grouping variables were consistent with the findings above. The model fit the data well, χ2 (21) =11.83, p = .944, CFI = 1.00, TLI =1.03, RMSEA < .001. PTSD symptom severity was not a significant predictor of the intercept factor, or of linear or quadratic growth factors in the first semester (ps > .20), but did significantly predict the second semester linear smoking trajectory (B = 0.03, SE = 0.02, p = .035, 95% CI [0.002, 0.07]). Students who endorsed a more PTSD symptoms at baseline reported greater increases in smoking during the second semester of freshman year.
Discussion
The present study offers a first test of the prospective influence of PTSD on smoking trajectories in a sample of emerging adults in their first year of college. Consistent with a self-medication conceptualization, results of our latent growth models showed that entering college with PTSD places students at risk for escalation in smoking as the academic year progresses. As we controlled for general negative affectivity in our models, findings speak to the distinct relationship between PTSD and smoking.
When smoking trajectories were examined independent of PTSD status, the overall pattern of change in our sample suggested that smoking levels were highest at matriculation, then declined during the fall semester and then began to rebound slightly during the spring semester. The early escalation and then slow decline over the first semester is consistent with other examinations of first year college smoking trajectories (e.g., Colder et al., 2006). Yet individual variability in these patterns has been noted, especially as smoking is observed over the later part of the first academic year (Colder et al., 2008). Factors which may contribute to such variability are not well understood. Our study may help to shed light on these processes.
Our study diverges from others that have examined smoking trajectories in the first year of college in that we modeled the influence of PTSD on these patterns. In doing so, we found that the influence of PTSD appears to unfold over the academic year, against the backdrop of the college environment. Consistent with findings of first year college smoking when PTSD is not modeled (Colder et al., 2006), students in our sample without full PTSD tended to decrease smoking over the first semester and to maintain these declines for the rest of the academic year. Yet smoking patterns among those with PTSD show a different trajectory as the academic year progressed; those in the Full PTSD group showed more rapid escalation in smoking during the spring semester.
The emergence of PTSD effects on smoking trajectories over time is consistent with contemporary theories of substance use development, many of which emphasize social influences in the etiology of smoking acquisition. According to these models, as smoking behavior progresses, the weight of the etiological influence shifts away from conviviality, and toward more internal processes (e.g., negative emotion), and on the pharmacological factors that maintain dependence (Dierker & Mermelstein, 2010). With this in mind, we interpret our findings in a social-developmental context. At the beginning of the school year, patterns of smoking among students with PTSD is indistinct from those of students without PTSD, and indeed may reflect the same process as it does for other students who are beginning college – social experimentation. Yet as the year progresses and there are other natural transition points (winter break), students who began college with PTSD may come to rely increasingly on smoking to cope, evidenced in our data by an eventual re-escalation in smoking. Taken together, this suggests that it may be how those with PTSD manage the challenges of the college environment over time that is relevant for smoking behavior.
Though smoking rates in this college sample – as in other college samples (c.f. Dierker et al., 2006; Rigotti et al., 2000; Thompson et al., 2007) are relatively low, it is important to bear in mind that low-level smoking is not synonymous with unimportant smoking. Indeed, low level smoking carries with it significant health risks (NCI, 1998). Moreover, it is low level smoking that is on the rise among adults in the U.S. (King et al., 2011).
At least some research suggests that psychological responses to trauma are spectral in nature, with more severe symptoms falling further along the spectrum (Broman-Fulks et al., 2006; Ruscio, Ruscio, & Keane, 2002). In this study we modeled PTSD continuously (i.e., number of PTSD symptoms) in addition to categorically in order to examine whether conceptualizing PTSD as a continuous variable would lead to different results. It did not. Instead, these analyses replicated what we found in our main analyses; students who endorsed a greater number of PTSD symptoms at baseline showed greater increases in smoking during the second semester of freshman year. It is perhaps worth noting that the purely continuous characterization of PTSD symptoms that is represented by the symptom severity scores from the PCL does not by itself adequately capture the essence of the PTSD construct. Since its inception in 1980 (DSM III), PTSD has been shown, both conceptually and empirically, to consist not just of a hierarchy of symptoms, but of unique symptom clusters. Though the specific dimensions of these symptom clusters has been the subject of debate (King, Leskin, King & Weathers, 1998; Miller et al., 2010; Simms et al., 2002), the conceptualization of PTSD as a multidimensional construct and not simply a unidimensional scale remains consistent. As such, data presented here allow for understanding of both the influence of general severity of symptoms as well as the PTSD diagnosis itself.
Findings here for smoking are consistent with other work from our group showing both full and sub-threshold PTSD syndromes to be associated with risk for other substance use (alcohol, illicit drugs; Read et al., 2011). Though in the present study the Partial PTSD group did not differ significantly in their smoking trajectory from the No PTSD group, we did observe some modest evidence for a “stepped” pattern across the PTSD groups at least in absolute levels of cigarette use. Those in the Full PTSD group showed the highest rates of smoking, followed by those with Partial PTSD, and then by those in the No PTSD group. Still, the magnitude of difference between the Partial PTSD and the No PTSD groups was not large enough to reach statistical significance.
Limitations and Future Directions
This study had a number of strengths, including a sample drawn from two universities in different regions of the U.S., a high retention rate, measures with strong psychometric properties, and a prospective design with frequent assessments over the first year of college. There also were some limitations and several directions for future investigation. These are discussed below.
As our objective was to examine patterns of smoking as a function of PTSD, we included in our sample only those for whom we could reasonably identify such patterns – students who reported smoking during the first-year assessment period. We did not examine smoking initiation. Data show that most students who smoke have initiated smoking well before beginning college (Substance Abuse and Mental Health Services Administration, 2006; Wechsler et al., 1998). This was evident in our data; only fifteen percent (n =53) of the students who smoked in their freshman year reported no past year smoking at baseline (i.e., they “initiated” during freshman year). Indeed, we included initial smoking status (in-college initiators) as a model covariate to determine whether smoking initiation during the first college year influenced trajectories, and found that it did not yield much in the way of prediction.
Given our aim of examining the effects of PTSD symptom status at matriculation on smoking over the first year of college, we did not model the effects of new traumas or repeated victimization, nor did we consider changes in PTSD symptoms over time. Exploration of how dynamic changes in these phenomena affect smoking trajectories will be an interesting avenue of future inquiry. Examination of other dynamic associations between PTSD and smoking in college samples could also be fruitful. For example, recent data from Cougle, Zvolensky, Fitch, and Sach-Ericsson (2010) show that individuals with PTSD and other co-occurring distress are at greater risk for deleterious smoking outcomes than are those with a single disorder alone. In the present study we modeled negative affectivity to isolate the unique influence of PTSD above and beyond trait affective vulnerability. However, we did not look at the aggregate effects of PTSD and negative affectivity, or other co-occurring distress. Extending the present work to address how other trait factors or co-occurring psychopathology may operate synergistically with PTSD will yield additional important information about the PTSD-smoking link.
The objective of our study was to examine the influence of trauma and PTSD in a population in whom these associations seldom have been tested, college students. Yet it is important to bear in mind that in many ways, U.S. college students differ from the general U.S. population (Heinrich et al., 2010). Indeed, though recent data show that college students report rates of trauma and PTSD comparable to the general community (see Read, Ouimette, White, Colder, & Farrow, 2011; Smyth et al., 2008), and the types of traumas reported in our college sample are strikingly similar to community and even to veteran samples (Breslau et al., 1998; Fikretoglu, Brunet, Schmitz, Guay, & Pedlar, 2006), there likely are features of the college student population that are unique to this group. For example, it could be argued that college students may have greater social support and coping resources than others with PTSD. As such, findings from this study may not generalize to other, non-college populations or to college populations outside the U.S. Further, even within college populations, replication with more diverse college samples (e.g., 2 year colleges, community colleges) will build on the present findings.
Finally, some studies have noted ethnic differences for both trauma and PTSD (Hoyt & Yeater, 2010; McGruder-Johnson, Davidson, Gleaves, Stock, & Finch, 2000; Read et al., 2011) and for smoking (e.g., Meyers, Doran, Trinidad, Klonoff, & Wall, 2010; Morrell, Cohen, Bacci, & West, 2005). Accordingly, the relative ethnic homogeneity of this sample may limit the generalizability of our findings.
Summary and Conclusions
Findings from this work suggest that students experiencing PTSD symptoms as they matriculate into college are at greater risk for progression of smoking—risk that emerges over the academic year. These findings have intervention implications. Identifiable risk for smoking progression is present as early as matriculation. Accordingly, early identification and intervention with those with significant PTSD symptoms may deter the development of smoking patterns over the first college year, and thus may help to prevent smoking behaviors from developing in later adulthood.
Acknowledgements
This work was supported by a grant from the National Institute on Drug Abuse (R01DA018993) to Dr. Jennifer P. Read.
We would like to thank Rachel Bachrach and Melissa Griffin for their helpful comments on earlier drafts of this manuscript, and Sherry Farrow, Ashlyn Swartout, and Jen Merrill for their myriad contributions to this project. We also thank the members of the UB Alcohol Research Lab for their many efforts to support data collection for this study, and the participants for sharing their experiences.
The TLEQ was used with permission from WPS. Copyright © 2004 by Western Psychological Services. WPS, 12031 Wilshire Boulevard, Los Angeles, California 90025, U.S.A, Format adapted by J. Read, SUNY at Buffalo.
Notes
To examine how findings may have been affected by our scoring of the smoking indices, we also examined another method that has been used in smoking research to create composite quantity-frequency indices for smoking (see Hu et al., 2008). We transformed the smoking variables from ordinal metrics into metrics reflecting monthly frequency of smoking and typical number of cigarettes smoked. We did this by choosing the numerical mid-point of ranges of the categorical response options for both quantity and frequency, and for frequency this midpoint was rescaled to represent monthly frequency (e.g., the mid-point of the frequency option “once or twice per week” is 1.5. This number is multiplied by 4 (number of weeks in a month) to obtain a monthly smoking frequency of 6 times). We formed a new Q × F index based on these values. This measure correlated between .83 and .90 across the time points (all ps <.0001) with the Q-F measure used in the study, suggesting that it was strongly related to the Quantity-Frequency that we used in our models. Given the comparability of the two q-f indices, and the advantage of our ordinally based index which reduced skew, we opted to retain this index for our substantive analyses. More data and syntax for this analysis are available from the first author.
Given that alcohol use is highly prevalent among college students, and has been linked to smoking in college (Dierker et al., 2006; Jackson et al., 2010) we attempted to examine whether alcohol involvement may have confounded the associations we observed between PTSD and smoking. To do so, we re-ran the models with alcohol use (quantity × frequency index analogous to the smoking index) included as a time-varying covariate, which involves regressing each observed smoking variable on the observed alcohol use variable for the corresponding time point. These covariate adjusted smoking variables were then analyzed using identical latent growth modeling procedures. Results of these models were consistent with the models that did not account for alcohol use, with the exception that the effect of PTSD group on the second semester linear smoking trajectory was slightly less reliable (β = .19, SE = .10, p = .069). Follow up analyses were consistent with those that did not include alcohol: there was a significant linear increase in smoking during the second semester for the Full PTSD group only (p=.024).These findings suggest that, although alcohol use may play a small role in the association between PTSD and smoking in our data, there is a unique effect of PTSD on smoking that cannot be fully accounted for by drinking.
References
- Acierno R, Kilpatrick DG, Resnick HS, Saunders BE, Best CL. Violent assault, posttraumatic stress disorder, and depression: Risk factors for cigarette use among adult women. Behavior Modification. 1996;20:363–384. doi: 10.1177/01454455960204001. [DOI] [PubMed] [Google Scholar]
- Ameringer KJ, Leventhal AM. Applying the tripartite model of anxiety and depression to cigarette smoking: An integrative review. Nicotine & Tobacco Research. 2010;12:1183–1194. doi: 10.1093/ntr/ntq174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir M, Sol O. Psychological impact and prevalence of traumatic events in a student sample in Israel: The effect of multiple traumatic events and physical injury. Journal of Traumatic Stress. 1999;12:139–154. doi: 10.1023/A:1024754618063. [DOI] [PubMed] [Google Scholar]
- Andrykowski M, Cordova M, Studts J, Miller T. Posttraumatic Stress Disorder after treatment for breast cancer: Prevalence of diagnosis and use of the PTSD Checklist—civilian version (PCL-C) as a screening instrument. Journal of Consulting and Clinical Psychology. 1998;66:586–590. doi: 10.1037//0022-006x.66.3.586. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist. 2000;55:469–480. [PubMed] [Google Scholar]
- Arnett JJ. The developmental context of substance use in emerging adulthood. Journal of Drug Issues. 2005;42:235–253. [Google Scholar]
- Bartholow BD, Sher KJ, Krull JL. Changes in heavy drinking over the third decade of life as a function of collegiate fraternity and sorority involvement: A prospective, multilevel analysis. Health Psychology. 2003;22:616–626. doi: 10.1037/0278-6133.22.6.616. [DOI] [PubMed] [Google Scholar]
- Beckham JC, Roodman AA, Shipley RH, Hertzberg MA, Cunha GH, Kudler HS, et al. Smoking in Vietnam combat veterans with post-traumatic stress disorder. Journal of Traumatic Stress. 1995;8:461–472. doi: 10.1007/BF02102970. [DOI] [PubMed] [Google Scholar]
- Bernat JA, Ronfeldt HM, Calhoun KS, Arias I. Prevalence of traumatic events and peritraumatic predictors of post-traumatic stress symptoms in a nonclinical sample of college students. Journal of Traumatic Stress. 1998;11:645–664. doi: 10.1023/A:1024485130934. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behavior Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. John Wiley & Sons; New York, NY: 1989. [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation perspective. Wiley; Hoboken, NJ: 2006. [Google Scholar]
- Brandon TH. Negative affect as motivation to smoke. Current Directions in Psychological Science. 1994;3:33–37. [Google Scholar]
- Breslau N, Davis GC, Schultz LR. Post-traumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Archives of General Psychiatry. 2003;60:289–294. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- Broman-Fulks JJ, Ruggiero KJ, Green BA, Kilpatrick DG, Danielson CK, Resnick HS, Saunders BE. Taxometric investigation of PTSD: Data from two nationally representative samples. Behavior Therapy. 2006;37:364–380. doi: 10.1016/j.beth.2006.02.006. [DOI] [PubMed] [Google Scholar]
- Clark LA. Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology. 2005;114:505–521. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- Colby SM, Tiffany ST, Shiffman S, Niaura RS. Are adolescent smokers dependent on nicotine? A review of the evidence. Drug and Alcohol Dependence. 2000;59(Suppl. 1):S83–S95. doi: 10.1016/s0376-8716(99)00166-0. [DOI] [PubMed] [Google Scholar]
- Colder CR, Flay BR, Segawa E, Hedeker D, Tobacco Etiology Research Network (TERN) Trajectories of smoking among freshmen college students with prior smoking history and risk for future smoking: Data from the University Project Tobacco Etiology Research Network (UpTERN) study. Addiction. 2008;103:1534–1543. doi: 10.1111/j.1360-0443.2008.02280.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colder CR, Lloyd-Richardson EE, Flaherty BP, Hedeker D, Segawa E, Flay BR, The Tobacco Etiology Research Network The natural history of college smoking: Trajectories of daily smoking during the freshman year. Addictive Behaviors. 2006;31:2212–2222. doi: 10.1016/j.addbeh.2006.02.011. [DOI] [PubMed] [Google Scholar]
- Cougle JR, Zvolensky MJ, Fitch KE, Sachs-Ericsson N. The role of comorbidity in explaining the associations between anxiety disorders and smoking. Nicotine & Tobacco Research. 2010;12:355–364. doi: 10.1093/ntr/ntq006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ. A latent curve framework for the study of developmental trajectories in adolescent substance use. In: Rose JS, Chassin L, Presson CC, Sherman SJ, editors. Multivariate applications in substance use research. Erlbaum; New Jersey: 2000. pp. 1–33. [Google Scholar]
- Curran PJ, Muthen BO. The application of latent curve analysis to testing developmental theories in intervention research. American Journal of Community Psychology. 27:567–590. doi: 10.1023/A:1022137429115. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Another look at heavy episodic drinking and alcohol use disorders among college and non-college youth. Journal of Studies on Alcohol. 2004;65:477–488. doi: 10.15288/jsa.2004.65.477. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Darkes J, Greenbaum PE, Goldman MS. Up close and personal: Temporal variability in the drinking of individual college students during their first year. Journal of Consulting and Clinical Psychology. 2004;72:155–164. doi: 10.1037/0022-006X.72.2.155. [DOI] [PubMed] [Google Scholar]
- Dierker L, Lloyd-Richardson E, Stolar M, Flay B, Tiffany S, Collins L, Clayton R. The proximal association between smoking and alcohol use among first year college students. Drug and Alcohol Dependence. 2006;81:1–9. doi: 10.1016/j.drugalcdep.2005.05.012. [DOI] [PubMed] [Google Scholar]
- Dierker L, Mermelstein R. Early emerging nicotine-dependence symptoms: A signal of propensity for chronic smoking behavior in adolescents. The Journal of Pediatrics. 2010;56:818–822. doi: 10.1016/j.jpeds.2009.11.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan JE, Jessor R, Jessor L. Problem drinking in adolescence and young adulthood: A follow-up study. Journal of Studies on Alcohol. 1983;44:109–137. doi: 10.15288/jsa.1983.44.109. [DOI] [PubMed] [Google Scholar]
- Everett SA, Husten CG, Kann L, Warren CW, Sharp D, Crossett L. Smoking initiation and smoking patterns among US college students. Journal of American College Health. 1999;48:55–60. doi: 10.1080/07448489909595674. [DOI] [PubMed] [Google Scholar]
- Feldner MT, Babson KA, Zvolensky MJ. Smoking, traumatic event exposure, and post-traumatic stress: A critical review of the empirical literature. Clinical Psychology Review. 2007a;27:14–45. doi: 10.1016/j.cpr.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldner MT, Babson KA, Zvolensky M, Vujanovic AA, Lewis SF, Gibson LE, Monson CM, Bernstein A. Post-traumatic stress symptoms and smoking to reduce negative affect: An investigation of trauma-exposed daily smokers. Addictive Behaviors. 2007b;32:214–227. doi: 10.1016/j.addbeh.2006.03.032. [DOI] [PubMed] [Google Scholar]
- Flora DB. Specifying piecewise latent trajectory models for longitudinal data. Structural Equation Modeling. 2008;15:513–533. [Google Scholar]
- Fromme K, Corbin WR, Kruse MI. Behavioral risks during the transition from high school to college. Developmental Psychology. 2008;44:1497–1504. doi: 10.1037/a0012614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu SS, McFall M, Saxon AJ, Beckham JC, Carmody TP, Baker TP, Dewleen G, Joseph AM. Post-traumatic stress disorder and smoking: A systematic review. Nicotine & Tobacco Research. 2007;9:1071–1084. doi: 10.1080/14622200701488418. [DOI] [PubMed] [Google Scholar]
- Gotham HJ, Sher KJ, Wood PK. Alcohol involvement and developmental task completion during young adulthood. Journal of Studies on Alcohol. 2003;64:32–34. doi: 10.15288/jsa.2003.64.32. [DOI] [PubMed] [Google Scholar]
- Hapke U, Schumann A, Rumpf H, John U, Konerding U, Meyer C. Association of smoking and nicotine dependence with trauma and post-traumatic stress disorder in a general population sample. The Journal of Nervous and Mental Disease. 2005;193:843–846. doi: 10.1097/01.nmd.0000188964.83476.e0. [DOI] [PubMed] [Google Scholar]
- Halperin AC, Smith SS, Heiligenstein E, Brown D, Fleming MF. Cigarette smoking and associated health risks among students at five universities. Nicotine & Tobacco Research. 2010;12:96–104. doi: 10.1093/ntr/ntp182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KJ, Golbeck AL, Cronk NJ, Catley D, Conway K, Williams KB. Timeline Follow-Back Versus Global Self-Reports of Tobacco Smoking: A Comparison of Findings With Nondaily Smokers. Psychology of Addictive Behaviors. 2009;23:368–372. doi: 10.1037/a0015270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinrich J, Hein SJ, Norenzayan A. The weirdest people in the world? Behavioral and Brain Sciences. 2010;33:61–135. doi: 10.1017/S0140525X0999152X. [DOI] [PubMed] [Google Scholar]
- Hoyt T, Yeater EA. Comparison of posttraumatic stress disorder symptom structure models in Hispanic and White college students. Psychological Trauma: Theory, Research, Practice, and Policy. 2010;2:19–30. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jackson KM, Colby SM, Sher KJ. Daily patterns of conjoint smoking and drinking in college student smokers. Psychology of Addictive Behaviors. 2010;24:424–435. doi: 10.1037/a0019793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ, Gotham HJ, Wood PK. Transitioning into and out of large effect drinking in young adulthood. Journal of Abnormal Psychology. 2001;110:378–391. doi: 10.1037//0021-843x.110.3.378. [DOI] [PubMed] [Google Scholar]
- Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with post-traumatic stress disorder: A review of the literature. American Journal of Psychiatry. 2001;158:1184–1190. doi: 10.1176/appi.ajp.158.8.1184. [DOI] [PubMed] [Google Scholar]
- John OP, Srivastava S. The Big Five trait taxonomy: History, measurement, and theoretical perspectives. In: Pervin LA, John OP, editors. Handbook of personality. 2nd ed Guilford; New York: 1999. pp. 102–138. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG. Monitoring the Future national survey results on drug use, 1975-2000. Volume II: College students and adults ages 19-40. 2001 (NIH Publication No. 01-4935. [Google Scholar]
- Kahler CW, Leventhal AM, Daughters SB, Clark MA, Colby SM, Ramsey SE, Boergers J, Abrams DB, Niaura R, Buka, Stephen L. Relationships of personality and psychiatric disorders to multiple domains of smoking motives and dependence in middle-aged adults. Nicotine & Tobacco Research. 2010;12:381–389. doi: 10.1093/ntr/ntq014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassel JD, Stroud LR, Paronis CA. Smoking, stress and negative affect: Correlation, causation, and context across stages of smoking. Psychological Bulletin. 2003;129:270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis revisited: The dually diagnosed patient. Primary Psychiatry. 2003;10:47–48. [Google Scholar]
- King B, Dube S, Kaufmann R, Shaw L, Pechacek T. Vital Signs: Current Cigarette Smoking Among Adults Aged 18 Years —United States, 2005–2010. Morbidity and Mortality Weekly Report. 2011;60(35):1207–1212. [PubMed] [Google Scholar]
- King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the Clinician-Administered PTSD Scale: evidence for the dimensionality of posttraumatic stress disorder. Psychological Assessment. 1998;10:90–96. [Google Scholar]
- Kubany ES, Haynes SY, Leisen MB, Owens JA, Kaplan AS, Watson SB, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Lang A, Laffaye C, Satz L, Dresselhaus T, Stein M. Sensitivity and specificity of the PTSD Checklist in detecting PTSD in female veterans in primary care. Journal of Traumatic Stress. 2003;16:257–264. doi: 10.1023/A:1023796007788. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Turner AP, Mallet KA, Geisner IM. Predicting drinking behavior and alcohol-related problems among fraternity and sorority members: Examining the role of descriptive and injunctive norms. Psychology of Addictive Behaviors. 2004;18:203–212. doi: 10.1037/0893-164X.18.3.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population based prevalence study. JAMA: Journal of the American Medical Association. 2000;284:2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Lee CM, Lewis MA, Neighbors C. Preliminary Examination of Spring Break Alcohol Use and Related Consequences. Psychology of Addictive Behaviors. 2009;23:689–694. doi: 10.1037/a0016482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, Neighbors C, Oster-Aaland L, Kirkeby BS, Larimer ME. Indicated prevention for incoming freshmen: Personalized normative feedback and high-risk drinking. Addictive Behaviors. 2007;32:2495–2508. doi: 10.1016/j.addbeh.2007.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maggs JL, Williams LR, Lee CM. Ups and downs of alcohol use among first-year college students: Number of drinks, heavy drinking, and stumble and pass out drinking days. Addictive Behaviors. 2011;36:197–202. doi: 10.1016/j.addbeh.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magid V, Colder CR, Stroud LR, Nichter M, Nichter M. Negative affect, stress, and smoking in college students: Unique associations independent of alcohol and marijuana use. TERN Members; Addictive Behaviors. 2009;34:973–975. doi: 10.1016/j.addbeh.2009.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall EC, Zvolensky MJ, Vujanovic AA, Gibson LE, Gregor K, Bernstein A. Evaluation of smoking characteristics among community-recruited daily smokers with and without posttraumatic stress disorder and panic psychopathology. Journal of Anxiety Disorders. 2008;22:1214–1226. doi: 10.1016/j.janxdis.2008.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marx BP, Sloan DM. The role of emotion in the psychological functioning of adult survivors of childhood sexual abuse. Behavior Therapy. 2003;33:563–577. [Google Scholar]
- McCabe SE, West BT, Wechsler H. Trends and college-level characteristics associated with the non-medical use of prescription drugs among U.S. college students from 1993-2001. Addiction. 2007;102:455–465. doi: 10.1111/j.1360-0443.2006.01733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack AS, Laybold AM, Dickerman NJ, Budd CF. Stress and substance use: Student attitudes toward alcohol, marijuana, and cocaine. College Student Journal. 1993;27:215–222. [Google Scholar]
- McGruder-Johnson AK, Davidson ES, Gleaves DH, Stock W, Finch JF. Interpersonal violence and posttraumatic symptomatology: The effects of ethnicity, gender, and exposure to violent events. Journal of Interpersonal Violence. 2000;15:205–221. [Google Scholar]
- Mendlowicz MV, Stein MB. Quality of life in individuals with anxiety disorders. American Journal of Psychiatry. 2000;157:669–682. doi: 10.1176/appi.ajp.157.5.669. [DOI] [PubMed] [Google Scholar]
- Mermelstein R, Colby SM, Patten C, Prokhorov A, Brown R, Myers M, Adelman W, Hudmon K, McDonald P. Methodological issues in measuring treatment outcome in adolescent smoking cessation studies. Nicotine and Tobacco Research. 2002;4:395–403. doi: 10.1080/1462220021000018470. [DOI] [PubMed] [Google Scholar]
- Miller MW, Wolf EJ, Harrington KM, Brown TA, Kaloupek DG, Keane TM. An evaluation of competing models for the structure of PTSD symptoms using external measures of comorbidity. Journal of Traumatic Stress. 2010;23:631–638. doi: 10.1002/jts.20559. [DOI] [PubMed] [Google Scholar]
- Myers MG, Doran NM, Trinidad DR, Klonoff EA, Wall TL. A prospective study of cigarette smoking initiation during college: Chinese and Korean American students. Health Psychology. 2009;28:448–456. doi: 10.1037/a0014466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrell HR, Cohen LM, Bacchi D, West J. Predictors of smoking and smokeless tobacco use in college students: A preliminary study using web-based survey methodology. Journal of American College Health. 2005;54(2):108–115. doi: 10.3200/JACH.54.2.108-115. [DOI] [PubMed] [Google Scholar]
- Morrell HR, Song AV, Halpern-Felsher BL. Predicting adolescent perceptions of the risks and benefits of cigarette smoking: A longitudinal investigation. Health Psychology. 2010;29:610–617. doi: 10.1037/a0021237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus: The comprehensive modeling program for applied researchers. version 5.2 Los Angeles, CA: 2008. [Google Scholar]
- Mylle J, Maes M. Partial post-traumatic stress disorder revisited. Journal of Affective Disorders. 2004;78:37–48. doi: 10.1016/s0165-0327(02)00218-5. [DOI] [PubMed] [Google Scholar]
- Neighbors CL, Geisner IM, Lee CM. Perceived marijuana norms and social expectancies among entering college student marijuana users. Psychology of Addictive Behaviors. 2008;22:433–438. doi: 10.1037/0893-164X.22.3.433. [DOI] [PubMed] [Google Scholar]
- Nichter M, Nichter M, Carkoglu A, TERN members Reconsidering stress and smoking: A qualitative study among college students. Tobacco Control: An International Journal. 2007;16:211–214. doi: 10.1136/tc.2007.019869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hare T, Sherrer MV. Co-occurring stress and substance abuse in college first offenders. Journal of Human Behavior in the Social Environment. 2000;3:29–44. [Google Scholar]
- Parra GR, Krull JL, Sher K.j., Jackson KM. Frequency of heavy drinking and perceived peer alcohol involvement: Comparison of influence and selection mechanisms from a developmental perspective. Addictive Behaviors. 2007;32:2211–2225. doi: 10.1016/j.addbeh.2007.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson F, Lerman C, Kaufmann V, Neuner G, Audrain-McGovern J. Cigarette Smoking Practices Among American College Students: Review and Future Directions. Journal of American College Health. 2004;52:203–210. doi: 10.3200/JACH.52.5.203-212. [DOI] [PubMed] [Google Scholar]
- Read JP, Colder CR, Merrill JE, Ouimette P, White J, Swartout A. Trauma and Posttraumatic Stress Symptoms Influence Alcohol and Other Drug Problem Trajectories in the First Year of College. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0028210. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Farrow SM, Jaanimagi U, Ouimette PC. Assessing Trauma and Traumatic Stress via the Internet: Measurement Equivalence and Participant Reactions. Traumatology. 2009;15:94–102. [Google Scholar]
- Read JP, Ouimette P, White J, Colder C, Farrow S. Rates of DSM IV-TR trauma exposure and post-traumatic stress disorder among newly matriculated college students. Trauma: Theory, Research, and Practice. 2011;3:148–156. doi: 10.1037/a0021260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigotti NA, Lee JE, Wechsler H. US college students’ use of tobacco products: Results of a national survey. JAMA. 2000;284:699–705. doi: 10.1001/jama.284.6.699. [DOI] [PubMed] [Google Scholar]
- Rimsza ME, Moses KS. Substance abuse on the college campus. Pediatric Clinics of North America. 2005;2005:52–307. doi: 10.1016/j.pcl.2004.10.008. [DOI] [PubMed] [Google Scholar]
- Ruggiero KJ, Del Ben K, Scotti JR, Rabalais AE. Psychometric properties of the PTSD Checklist—Civilian Version. Journal of Traumatic Stress. 2003;16:495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- Saladin ME, Brady KT, Dansky BS, Kilpatrick DG. Understanding comorbidity between PTSD and substance use disorders: Two preliminary investigations. Addictive Behaviors. 1995;20:643–655. doi: 10.1016/0306-4603(95)00024-7. [DOI] [PubMed] [Google Scholar]
- Scarpa A, Fikretoglu D, Bowser F, Hurley JD, Pappert CA, Romero N, Van Voorhees E. Community violence exposure in university students: A replication and extension. Journal of Interpersonal Violence. 2002;17:253–272. [Google Scholar]
- Schnurr PP, Ford JD, Friedman MJ, Green BL, Dain BJ, Sengupta A. Predictors and outcomes of post-traumatic stress disorder in World War II veterans exposed to mustard gas. Journal of Consulting and Clinical Psychology. 2000;68:258–268. [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Vernardy NC. Research on post-traumatic stress disorder: Epidemiology, pathophysiology, and assessment. Psychotherapy in Practice. 2002;58:877–889. doi: 10.1002/jclp.10064. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Maggs JL. A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. Journal of Studies on Alcohol. 2002;114:54–70. doi: 10.15288/jsas.2002.s14.54. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Rutledge PC. Heavy drinking across the transition to college: Predicting first-semester heavy drinking from pre-college variables. Addictive Behaviors. 2007;32:819–835. doi: 10.1016/j.addbeh.2006.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simms LJ, Watson D, Doebbelling BN. Confirmatory factor analyses of posttraumatic stress symptoms in deployed and non-deployed veterans of the Gulf War. Journal of Abnormal Psychology. 2002;111:637–647. doi: 10.1037//0021-843x.111.4.637. [DOI] [PubMed] [Google Scholar]
- Smyth JM, Hockemeyer JR, Heron KE, Wonderlich SA, Pennebaker JW. Prevalence, type, disclosure, and severity of adverse life events in college students. Journal of American College Health. 2008;57:69–76. doi: 10.3200/JACH.57.1.69-76. [DOI] [PubMed] [Google Scholar]
- Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial post-traumatic stress disorder: Findings from a community survey. American Journal of Psychiatry. 1997;154:1114–1119. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration [Retrieved July 23, 2010];Results from the 2005 National Survey on Drug Use and Health: National findings (Office of Applied Studies, NSDUH Series H-30, DHHS Publication No. SMA 06-4194) 2006 from http://www.oas.samhsa.gov/NSDUH/2k5nsduh/tabs/2k5Tabs.pdf.
- Thompson B, Coronado G, Chen L, Thompson LA, Halperin A, Jaffe R, Zbikowski SM. Prevalence and characteristics of smokers at 30 Pacific Northwest colleges and universities. Nicotine & Tobacco Research. 2007;9:429–438. doi: 10.1080/14622200701188844. [DOI] [PubMed] [Google Scholar]
- Ullman J, Filipas HH. Gender differences in social reactions to abuse disclosures, post-abuse coping, and PTSD of child sexual abuse survivors. Child Abuse and Neglect. 2005;29:767–782. doi: 10.1016/j.chiabu.2005.01.005. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Rigotti NA, Gledhill-Hoyt J, Lee H. Increased levels of cigarette use among college students: A cause for national concern. JAMA: Journal of the American Medical Association. 1998;280:1673–1678. doi: 10.1001/jama.280.19.1673. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Huska JA, Keane TM. The PTSD Checklist- Civilian Version (PCL-C) F.W. Weathers, National Center for PTSD, Boston VAMC, 150 S. Huntington Ave.; Boston, MA: 1991. p. 02130. Available from. [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the meeting of the International Society for Traumatic Stress Studies; San Antonio, TX. Oct, 1993. [Google Scholar]
- Wetter DW, Kenford S, L., Welsch SK, Smith SS, Fouladi RT, Fiore MC, Baker TB. Prevalence and Predictors of Transitions in Smoking Behavior Among College Students. Health Psychology. 2004;23:168–177. doi: 10.1037/0278-6133.23.2.168. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Franklin CL, Zimmerman M. Does “subthreshold” post-traumatic stress disorder have any clinical relevance? Comprehensive Psychiatry. 2002;43:413–419. doi: 10.1053/comp.2002.35900. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Cardenas SJ, Colotla VA, Marshall EC, Feldner MT. Anxiety sensitivity and early relapse to smoking: A test among Mexican daily, low-level smokers. Nicotine & Tobacco Research. 2007;9:483–491. doi: 10.1080/14622200701239621. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Feldner MT, Leen-Feldner E, Bonn-Miller MO, McLeish AC, Gregor K. Evaluating the role of anxiety sensitivity in smoking outcome expectancies among regular smokers. Cognitive Therapy and Research. 2004;28:473–486. [Google Scholar]