Abstract
The inner city Emergency Department (ED) provides a window of opportunity for screening for alcohol and other drug misuse and substance use disorders (SUDs), in order to facilitate linkage for individuals who are in need of services targeting such issues. The majority of prior work in this area has focused on alcohol use. This study used latent class analyses to characterize substance use/SUDs among adults presenting to the ED for medical complaints or injuries. Participants (n=14,557; 77% participation; 45% male; 54% African-American) completed a computerized survey assessing demographics, health functioning, and substance use/SUDs. Although injured patients were significantly more likely to use tobacco, alcohol, and marijuana, and were more likely to have an alcohol use disorder, presenting complaint was not related to other drug use/diagnoses. Five latent classes were identified: (1) non users/SUDs (65.9%) (2) binge drinkers (24.3%), (3) marijuana users/SUD (3.5%), (4) cocaine users/SUD (2.9%), and (5) poly-drug users (3.3%). Compared to class 1, participants in the other classes were younger, male, without health insurance, with poor mental health functioning, tobacco users, and had prior substance use treatment. African-Americans were most likely to be in classes 3 or 4 and employed participants were most likely to be in class 2. In comparison to class 1, classes 2 and 3 reported better physical health; class 2 was more likely to present for injury whereas class 5 was more likely to present for a medical complaint. ED-based screening and interventions approaches need to address the co-occurrence of alcohol, illicit drug, and psychoactive prescription drug use.
Keywords: Keywords: Emergency, Alcohol, Drug, Substance Use Disorder, Prescription, African-American
1. Introduction
Nationally, the prevalence of substance use disorders is high. In 2005, the National Survey on Drug Use and Health indicated 22.2 million individuals over the age of 12 met DSM-IV criteria (American Psychiatric Association, 1994) for substance abuse or dependence in the past year. Males were approximately two times more likely than females to have a substance use disorder (12.0% vs. 6.4%, respectively) (Substance Abuse and Mental Health Services Administration, 2006). Approximately 22.7 percent of the general U.S. population engaged in binge drinking (five more drinks on the same occasion) and 8.1 percent of the U.S. population over the age of 12 had used an illicit drug in the preceding month (Substance Abuse and Mental Health Services Administration, 2006). Regrettably, multiple epidemiologic studies have shown that, at best, only about 10% of those who need substance use treatment actually do receive it (Cohen, Feinn, Arias, & Kranzler, 2007; Compton, Thomas, Stinson, & Grant, 2007; Substance Abuse and Mental Health Services Administration, 2004, 2006). Data from the National Survey on Drug Use and Health finds that among patients in substance use treatment, 11.7% were referred to treatment by their general practitioner while 10.2% received services after a visit to an emergency department (ED) visit (Substance Abuse and Mental Health Services Administration, 2006).
Numerous studies show that ED patients, both injured and medical, have higher rates of alcohol use than the general population, with injured patients being particularly at risk for alcohol misuse (Cherpitel, 1992, 1993). For example, up to 47% of trauma patients presenting for injury-related conditions have positive blood alcohol concentrations (Cherpitel, 1997, 1998; Soderstrom, Trifillis, Shankar, Clark, & Cowley, 1988)while as many as 50% of severely injured trauma patients requiring hospitalization have positive alcohol screens (Cornwell, et al., 1998; D'Onofrio & Degutis, 2004). Rates of alcohol problems range from 8–11% for abuse and from 10–16% for dependence in ED settings (Cherpitel, 1998).
Compared to alcohol users, far less is known about illicit drug users presenting to the ED. Overall, the rates of self-reported drug use in the ED are estimated to range from 1–5%; however, among patients whom biological markers are obtained, the prevalence of illicit drug use ranges from 35–40% (Vitale & Van de Mheen, 2006). Prior research has shown that individuals who use drugs are more likely to seek ED care than non-users (Cherpitel, 2003; El-Guebaly, Armstrong, & Hodgins, 1998; Vitale & Van de Mheen, 2006). In addition, many patients who use drugs do not seek primary care services (due to lack of insurance, lack of availability, etc) or are inconsistent users of those services and remain unrecognized until legal or employment consequences emerge. The inner-city ED is a crucial location for interventions with drug-using individuals, given that patients who use inner-city EDs often do not have a primary care physician, do not routinely receive medical care other than in the ED setting, are minority patients, and/or are patients of lower socioeconomic status, and are therefore more likely to utilize the ED for their sole source of care (D. Baker, Stevens, & Brook, 1991; Bindman, Grumbach, Keane, Rauch, & Luce, 1991; Grumbach, Keane, & Bindman, 1993; McCaig & Burt, 2003; Pane, Farner, & Salness, 1991).
In 2005 data, the Drug Abuse Warning Network (DAWN) reported that approximately 800,000 visits to participating EDs involved illicit drug use; cocaine use is the most frequent drug mentioned, followed by marijuana, heroin, and stimulants (methamphetamine and amphetamines) (Substance Abuse and Mental Health Services Administration, 2006). Cocaine use has been implicated in approximately 20% of chest pain patients presenting to an inner-city ED (Booth, et al., 2005). Survey data regarding the prevalence of illicit drug use disorders is generally lacking in the ED literature. A notable exception found that 14.7% of patients met criteria for a substance use disorder (Rockett, Putnam, Jia, & Smith, 2003). However, this prior ED study did not examine the prevalence of alcohol and drug use, and substance use disorders (SUDs) separately for alcohol and various illicit drugs.
This study included a comprehensive, systematic evaluation of adult ED patients (injured and medical) between ages 19 and 60 presenting for care in a large, inner city hospital in Flint, Michigan. This study expands the work of prior ED studies to examine the co-occurrence of substance use (alcohol, illicit drug, and psychoactive prescription drug use) and SUDs using latent class analyses. Further, the demographic and health related markers of membership in the latent classes were examined. Because the ED setting is an important venue for providing interventions with patients who have alcohol and/or illicit drug use/disorders, comprehensive understanding of the substance use patterns could inform future intervention research in this setting.
2. Methods
2.1. Study Design
The study site was the Hurley Medical Center ED in Flint, Michigan, an urban, university-affiliated Level 1 trauma center. All study-eligible adult patients presenting to the ED were recruited to complete a health screen seven days per week from November, 2005 through January, 2009. Recruitment staff covered shifts in the ED from 9am –11:30pm, seven days a week. Based on the investigators’ previous work in the ED on refusal rates by shift, the midnight shift was excluded (Blow, et al., 2006). A computerized screening instrument was administered after written consent was obtained from eligible patients. Participants completing the 10-minute computerized survey received a $1.00 gift (e.g., puzzle books, pens). The study was approved by the University of Michigan and the Hurley Medical Center Institutional Review Boards and Certificates of Confidentiality were obtained from NIAAA and NIDA.
2.2 Participants
Patients between the ages of 19–60 were approached by research staff to participate. Patients were excluded from the study if they were pregnant, had unstable vital signs, were unable to provide informed consent (e.g. unconscious), were acutely suicidal, or presented for a sexual assault, or psychiatric evaluation. Participants that were acutely intoxicated were only approached after they were deemed clinically clear to provide consent. Patients who refused to participate in the study were asked if they would provide information on gender and race as well as reasons for refusing to participate.
2.3 Measures
Participating patients completed the screening instrument on programmed web tablets. The screener asked whether participants were being seen for an injury or medical complaint. Questions about alcohol and drug use were embedded in an overall brief health and lifestyle screening instrument to maximize the accuracy of responses and to put substance use questions in the broader context of health behaviors and health screening (Saunders, Aasland, Babor, Fuente, & Grant, 1993). The Medical Outcome Study Short-Form (SF-12) was administered to assess physical and mental health functioning (Ware, 1976; Ware & Sherbourne, 1992). These indicators of health status have been widely studied and are generally accepted outcomes for screening and intervention studies (Fleming, Barry, Manwell, Johnson, & London, 1997; Wallace, Cutler, & Haines, 1988).
Measures of substance use and DSM-IV substance use disorders were taken from the Substance Abuse Outcomes Module (SAOM; (Smith, et al., 2006). The SAOM measures past 30-day alcohol use frequency, number of drinking days, average consumption and frequency of binge drinking, drug use frequency, along with questions to ascertain past year DSM-IV diagnoses for alcohol and drug abuse/dependence. Past month drug use frequency was obtained for tobacco use, binge drinking, cocaine and marijuana use, other illicit drugs (e.g., heroin, hallucinogens, inhalants, club drugs) and psychoactive prescription drugs (e.g., depressants, opiates/analgesics, sedatives, stimulants), which could have been obtained illegally or with a prescription. The DSM-IV delineates abuse from dependence, with dependence considered the more serious of the two. In order to meet criteria for substance dependence, an individual must evidence physiological (e.g., tolerance, withdrawal) and/or behavioral (e.g., inability to stay with self-imposed limits on use) impairments whereas substance abuse is diagnosed based upon an individual’s experience of repeated social consequences (e.g., work or school absenteeism, involvement with the legal system) related to his/her substance use. The SAOM was modified for this study to separately elicit DSM-IV diagnoses for cocaine and cannabis abuse and dependence. In the most recent evaluation, the SAOM was shown to be reliable (internal reliability, coefficient ∀0.58–0.90, test-retest reliability 0.56–0.99) and valid (concurrent validity generally 0.5–0.8, predictive validity 0.5–0.9) (Smith, et al., 2006).
2.4 Data Analyses
Data were analyzed using SAS 9.2 (SAS). Descriptive statistics were computed for basic socio-demographic variables, alcohol and illegal drug use, physical and mental health functioning, and DSM-IV diagnoses of any substance abuse or dependence and (separately) alcohol, cocaine, and marijuana abuse or dependence. Bivariate analyses were computed to contrast injured and non-injured medical patients on demographics, health, and substance use variables. Specifically, chi-square tests were used for categorical variables. The tests conducted for continuous variables were either two-sample t-tests or general linear model F-tests for three groups. Because of the large sample size (> 5,600) and multiple testing, the level of significance for tests was set at p < 0.01 to reduce the chance of a Type I Error.
Next, classes of participants sharing common substance use behaviors and substance use disorders were identified with latent class analysis (LCA). Latent class analysis (LCA) is a multivariate technique which can be applied for cluster, factor, or regression analytic purposes. Latent constructs are created from indicator variables and then used to construct clusters, factors, or to predict dependents in regression mode. LCA is commonly used to classify cases into a set of latent classes, based on categorical indicator variables such as survey items. The analyses were carried out in an exploratory fashion using Mplus (version 4.2). Specifically, rather than testing a previously specified, a priori solution, we examined the fit of a series of different LCA models. First, a single group model was examined; then, additional groups were added to the model until no significant empirical and conceptual improvements were observed. The model’s empirical fit was based on the Bayesian Information Criterion (BIC), with lower values reflecting an improved fit. In addition, entropy was examined, which shows how well the indicators predict subgroup membership, with a value closer to 1.0 indicating better prediction. The conceptual fit of each model was examined by a visual representation of subgroups. Next, bivariate analysis was conducted to assess the associations of classes of substance use groups based on: demographic (gender, age, race, marital status, education, employment, insurance), health (physical heath composite <=25th percentile, SF-12 mental health composite <= 25th percentile, injury), and other substance use variables (tobacco use, prior substance use treatment). Lastly, multinomial logistic regression was used to predict these substance use groups, using simultaneous forced entry, based on the demographic and health variables.
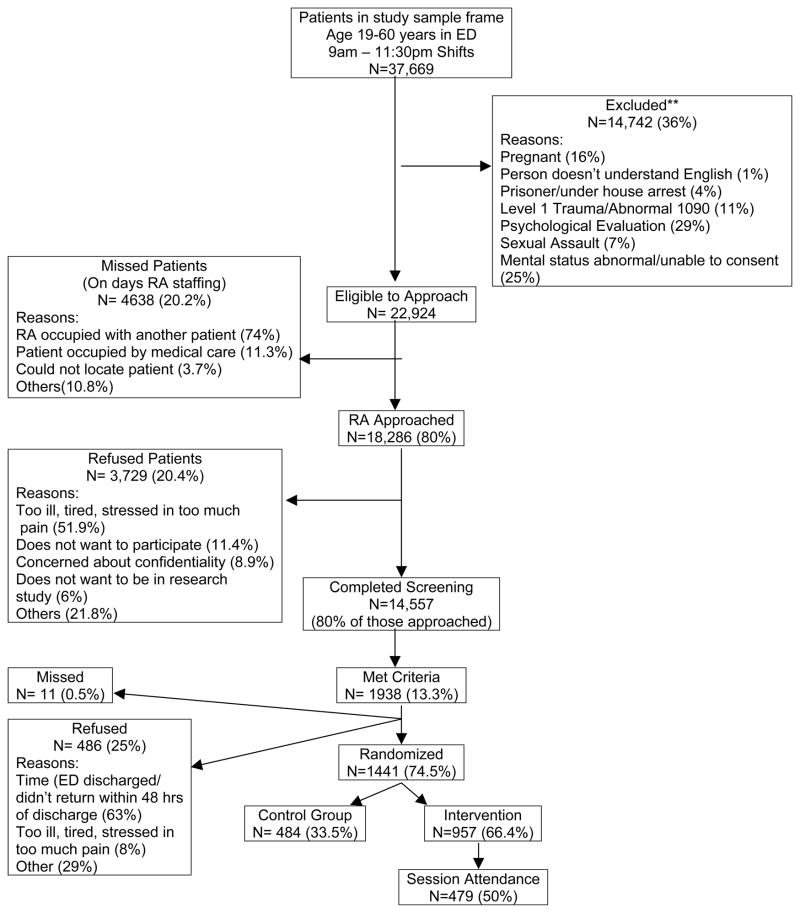
3. Results
Among the 22,924 potentially eligible patients who presented during the recruitment period, 80% (n=18,286) were approached. Reasons for missed patients (n=4638) included: research staff occupied with another patient (74%), patient occupied by medical care (11.3%), could not locate patient (3.7%), and other (10.8%). Overall, 80% of the approached patients (n=14,557) consented to complete the screening survey (Figure 1). Among the refusals, 52% were too ill, tired or weak, or in too much pain to participate, 17% did not want to participate, about 9% were concerned about confidentiality, and 22% refused to participate due to various reasons (e.g., survey was too long, family refused access, too stressed to participate (5%). Of the refusals, 46% were male and 53% were African-American. The race and gender of those who refused was similar to the study group.
Figure 1. Study Flowchart.
Some patients had multiple ED visits and were screened more than once (N= 2,168). The first screen was used in data analysis. Multiple visits by individuals patients are not reflected in the N of the overall sample frame.
**Excluded: Tallied for 12 months of study and tripled to estimate 36 months of recruitment.
On average, the study participants were relatively young (mean age=36.2 years, SD=11.6), female (55.2%), African-American (54.3%), had a high school degree or less (62.7%), had some health insurance including Medicaid and Medicare (71.1%), had income less than 20K per year (64.8%), and were unemployed (53.7%) (see Table 1). On average, their self-rated physical and mental health scores on the physical and mental components of the SF-12 were 45.96 and 46.95, respectively, compared to mean scores for a community sample of 50.12 and 50.04, respectively (Ware, 1976; Ware & Sherbourne, 1992). Only about one-quarter (32.5%) presented to the ED with injuries; thus most patients presented for medical reasons. Sixteen percent of the sample met DSM-IV criteria for either abuse or dependence of alcohol or illicit drugs, including 12.9% with alcohol abuse/dependence, 5.9% marijuana abuse/dependence, and 3.7% cocaine abuse/dependence.
Table 1.
Background Characteristics, Health Status, and Substance Use by Chief Complaint.
| Variable | Injury (n=4,734) M (SD)/% |
Medical (n=9,823) M (SD)/% |
Total (n=14,557) M (SD)/% |
|---|---|---|---|
| Background Characteristics | |||
| Age1 | 35.5 (11.2) | 36.5 (11.7) | 36.2 (11.6) |
| Male1 | 56.0 | 39.5 | 44.8 |
| Black or African-American1 | 46.4 | 58.1 | 54.3 |
| Married or Living Together | 31.0 | 31.1 | 31.1 |
| Any College | 37.8 | 37.1 | 37.3 |
| With Health Insurance1/a | 73.7 | 78.8 | 77.1 |
| Annual Income: < $20,0001a | 61.4 | 66.6 | 64.8 |
| Employed1/a | 51.9 | 43.6 | 46.3 |
| Health | |||
| Physical (≤ 25th Percentile)1 | 20.2 | 27.3 | 25.0 |
| Mental (≤ 25th Percentile)1 | 21.7 | 26.6 | 25.0 |
| Inject Drugs | 0.7 | 0.5 | 0.5 |
| Substance Use | |||
| Used Tobacco (past 30 Days)1 | 58.4 | 53.5 | 55.1 |
| Alcohol Use (past 30 Days)1 | 53.6 | 45.1 | 47.9 |
| Binge Drinking (any)1a | 26.7 | 19.9 | 22.1 |
| Marijuana Use (past 30 Days)3 | 22.6 | 20.4 | 21.1 |
| Cocaine Use (past 30 Days) | 4.3 | 4.1 | 4.1 |
| Heroin/Hallun./Inhal./Club (past 30 | 0.9 | 0.6 | 0.7 |
| Prescription Opiate Use Days) | 11.7 | 12.0 | 11.9 |
| Prescription Depressant/Sedative Use | 5.1 | 4.8 | 4.9 |
| Prescription Stimulant Use | 0.2 | 0.2 | 0.2 |
| Substance Use Disorders | |||
| Substance Use Treatment (past 3 months) | 4.7 | 4.3 | 4.5 |
| Alcohol Abuse or Dependence1 | 14.8 | 12.0 | 12.9 |
| Marijuana Abuse or Dependence | 6.2 | 5.8 | 5.9 |
| Cocaine Abuse or Dependence | 3.5 | 3.7 | 3.7 |
| Any Substance Abuse or Dependence1 (Alcohol/Marijuana/Cocaine) | 18.0 | 15.5 | 16.3 |
Notes: Percentages are column percentages; M=mean; SD=Standard deviation
Some subjects did not respond or skipped this question.
3.1. Non-Injured Medical Patients vs. Injured Patients
3.1.1. Demographics
As compared to the injured patients, medical patients were significantly more likely to be older age, female, African-American, have health insurance; medical patients reported less income and employment than injured patients (see Table 1). There were no significant differences between these populations in marital status or education.
3.1.2. Health
The medical patients were more likely to report poor health status on either the physical or mental components of the SF-12 than injured patients (e.g., in the lowest 25th percentile, Table 1).
3.1.3. Substance Use
The medical patients had less use of tobacco, alcohol, binge drinking, and marijuana in the past 30 days (Table 1). Use of other illicit drugs (e.g., cocaine) and prescription drugs did not differ based on presenting complaint (medical vs. injury). Although injured patients were significantly more likely than medical patients to meet criteria for alcohol abuse/dependence and substance abuse/dependence, marijuana and cocaine abuse/dependence did not differ based on presenting complaint. Further, the absolute number of patients with substance abuse/dependence presenting to the ED for medical reasons (n=1523) far exceeded the number of patients with substance abuse/dependence presenting for injury (n=852).
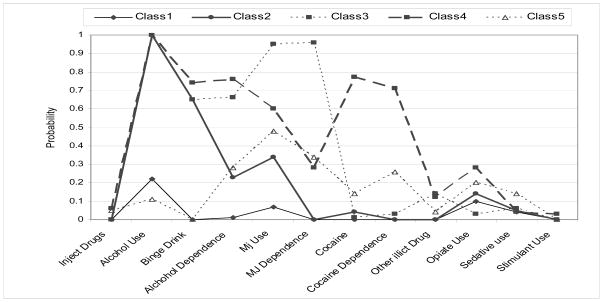
3.2. Latent Class Analyses of Substance Use and Substance Use Disorders
A total of six LCA models were examined, ranging from one to six classes. The one-class solution exhibited a poor fit with the data relative to the other models. The empirical fit of the five-class solution best fit the data (BIC = 82095; entropy = 0.86), as compared to the two-class (BIC = 85774; entropy = 0.823), three-class (BIC = 83558; entropy = 0.813), and four-class (BIC = 82716; entropy = 0.805) solutions. The improvement from five-class solution to six-class solution was very small (BIC=81828); however, entropy decreased with the 6-class solution (0.841). Thus, the five-class solution was retained in subsequent analyses (Figure 2).
Figure 2. Five-class solution of substance use/disorder groups among ED patients.
The probability of endorsing each substance use characteristics is shown in Table 2. Participants in Class 1, consisting of 65.9% of the sample, had near zero probabilities of use most substances. Although 22% of participants in this class reported alcohol use, they did not report any binge drinking. Participants in Class 2, consisting of 24.3% of the sample, had relatively high probability of binge drinking but relatively modest probability of meeting criteria for an alcohol use disorder; although these participants reported some marijuana use, they did not meet criteria for a marijuana use disorder. Other illicit drug use was low in this group although some prescription opiate use was reported. Participants in Class 3, consisting of 3.5% of the sample, had the greatest probability of using marijuana and meeting criteria for a marijuana use disorder. These participants were also likely to report binge drinking and meet criteria for an alcohol use disorder. The probability of reporting other illicit drug use was most common in this group; the probability of reporting prescription drug use was low in this group. Participants in Class 4, comprising 2.9% of the sample, had the highest probably of using cocaine and meeting criteria for a cocaine use disorder. These participants were also likely to report alcohol use/disorders and to a less extent, marijuana use/disorders and other illicit drug use. This group had the greatest probability of prescription opiate use. Participants in Class 5 (3.3% of the sample) had zero probability of binge drinking but relatively modest probability of reporting an alcohol use disorder; these participants appeared to report moderate probabilities of marijuana use/disorder and cocaine use/disorder. This group had the greatest probability of prescription sedative use and the second highest probability of prescription opiate use. Note that Class 4 and Class 5 reported the greatest probability of injecting drugs.
Table 2.
Conditional probabilities of variables clustered by substance use/disorder groups.
| Items | Class1 (Non-User/SUD) n=9597 (65.9%) | Class2 (Binge Drinkers) n=3541 (24.3%) | Class3 (Marijuana Use/SUD)n=508 (3.5%) | Class4 (Cocaine Use/SUD)n=429 (2.9%) | Cass5 (Poly-drug Users) n=482 (3.3%) |
|---|---|---|---|---|---|
| Inject Drugs | 0.00 | 0.00 | 0.00 | 0.06 | 0.05 |
| Alcohol Use (past 30 Days)1 | 0.22 | 1.00 | 1.00 | 1.00 | 0.11 |
| Binge Drinking (any)1a | 0.00 | 0.65 | 0.65 | 0.74 | 0.00 |
| Alcohol Abuse or Dependence1 | 0.01 | 0.23 | 0.66 | 0.76 | 0.28 |
| Marijuana Use (past 30 Days)3 | 0.07 | 0.34 | 0.95 | 0.60 | 0.48 |
| Marijuana Abuse or Dependence | 0.00 | 0.00 | 0.96 | 0.28 | 0.34 |
| Cocaine Use (past 30 Days) | 0.00 | 0.04 | 0.01 | 0.77 | 0.14 |
| Cocaine Abuse or Dependence | 0.00 | 0.00 | 0.03 | 0.71 | 0.26 |
| Other Illicit Drug (past 30 Days) | 0.00 | 0.00 | 0.14 | 0.12 | 0.04 |
| Prescription Opiate Use | 0.10 | 0.14 | 0.03 | 0.28 | 0.20 |
| Prescription Sedative Use | 0.04 | 0.05 | 0.06 | 0.04 | 0.14 |
| Prescription Stimulant Use | 0.00 | 0.00 | 0.00 | 0.03 | 0.00 |
3.3 Characteristics of Latent Classes of Substance Use Groups
The multinomial regression model was completed to estimate the association of substance use groups with individual factors. The overall model was significant (Wald test χ2 = 2975.25, p<0.0001). Compared to the non-use/SUD group, the other groups were younger, male, without health insurance, with poor mental health functioning, tobacco users, and had a prior history of substance use treatment. Unique relationships among the substance use groups were found for race, employment, physical health functioning and injury. African-Americans were most likely to be in Classes 3 or 4, the marijuana use/SUD disorder group and the cocaine use/SUD group. Relative to the non use/SUD group, participants in Class 2 (the binge drinkers) were most likely to be employed whereas the other substance use groups were less likely to be employed. Relative to the non-use/SUD group, participants in Classes 2 and 3 (binge drinkers and marijuana use/SUD, respectively) reported better physical health. Finally, in comparison to the non-use/SUD group, participants in Class 2 (binge drinkers) were more likely to present for injury whereas participants in Class 5 (poly-drug users) were more likely to present for a medical complaint.
4. Discussion
Many studies have documented the presence of alcohol use and, to a lesser extent, other drug use, among patients in emergency settings, particularly among injured patients (Academic ED SBIRT Research Collaborative, 2007; Cherpitel, 1993; Rockett, et al., 2003; Soderstrom, Dischinger, Kerns, & Trifillis, 1995; Vitale & Van de Mheen, 2006). This study expands the knowledge in the field by examining the prevalence and unique correlates of the pattern of substance use and SUD’s among a diverse sample of patients seeking care at an inner city ED, over half of whom were African-American. More specifically, this study is the first ED-based study to use latent class analyses to identify the co-occurrence of substance use and SUDs.
Overall, 16% (approximately one in six patients) met criteria for a DSM-IV substance use disorder (SUD), with alcohol being the most frequent substance use disorder (13%). These rates of alcohol and overall SUDs are similar to prior research (Cherpitel, 1993; Rockett, et al., 2003); however, our findings are novel, determining that 4–6% of patients that were surveyed met criteria for either a cocaine or marijuana use disorder. Rates of illicit drug use among inner city ED patients exceeded prior ED studies (Vitale & Van de Mheen, 2006): 21% reported marijuana use and 4% reported cocaine use. Further, 12% of ED patients reported prescription opiate use and 5% reported prescription depressant/sedative use. Finally, a novel finding from this study is that substance use patterns co-varied with psychoactive prescription drug use (i.e., opiates, depressants/sedatives). Thus, SBIRT models for addressing substance abuse among ED patients should include psychoactive prescription drug use.
Similar to findings from NESARC data (Agrawal, Lynskey, Madden, Bucholz, & Heath, 2007), findings from LCA analyses provides evidence for both the severity (as indicated by parallel lines of varying degrees) and heterogeneity (as indicated by intersecting lines) of substance use classes. Classes 1 (non-user/SUD) and 2 (binge drinkers) were clearly less severe than the other classes. Regarding heterogeneity in the pattern of substance use, two-thirds of inner-city ED patients (Class 1) did not binge drink or use illicit drugs, although they reported some psychoactive prescription drug use. One-quarter of ED patients (Class 2) reported binge drinking and marijuana use, most of whom did not meet criteria for a SUD. Three other fairly equally proportioned groups of ED patients were identified with more significant substance use/SUDs: marijuana use/SUD, cocaine use/SUD, and poly-drug use. Patients in the marijuana use/SUD group (3.5%) were also likely to meet criteria for an alcohol use disorder and use other illicit drugs; this group was unlikely to report prescription drug use. Patients in the cocaine use/SUD group (3%) were also likely to report alcohol use/disorders but reported less marijuana use/disorders and other illicit drug use; these patients were most likely to report prescription opiate use. Finally, patients in the poly-drug use group (3%) did not report binge drinking/alcohol use disorders, but reported relatively moderate marijuana and cocaine use/SUD, and prescription opiate and sedative use. In terms of risk for HIV infection, participants in the cocaine use/SUD and poly-drug use groups reported the greatest probability of injecting drugs.
Key findings regarding markers of the substance use groups were that compared to the non-use group, the other substance use groups were younger, male, without health insurance, with poor mental health functioning, tobacco users, and had prior substance use treatment. Further, unique findings were that African-Americans were most likely to be in the marijuana use/SUD disorder and cocaine use/SUD groups (Classes 3 or 4). In addition, the binge drinkers/no SUD group (Class 2) was most likely to be employed whereas the other substance use groups were less likely to be employed relative to the non use/SUD group. Studies are needed to address health disparities among African-Americans both in use of illicit drugs and access to substance use treatment. The inner city ED may be an ideal location to access minorities and/or patients with lower socio-economic status; these patients often do not have a primary care physician and are more likely to utilize the ED for their sole source of care (D. Baker, et al., 1991; Bindman, et al., 1991; Grumbach, et al., 1993; McCaig & Burt, 2003; Pane, et al., 1991). Further, these findings are consistent with the literature from non-ED settings showing that drug users often have co-occurring mental health problems (Barry, et al., 2006; Grant, 1995; Johnson, Brems, & Burke, 2002; Kandel, Huang, & Davies, 2001; Vincent, Schoobridge, Ask, Allsop, & Ali, 1998) and poor physical health (Adrian & Barry, 2003; Chen, Scheier, & Kandel, 1996; Garrity, et al., 2007; Marzuk, et al., 1995; Vincent, et al., 1998).
In comparison to injured patients, medical patients were more likely to be older, female, and African-American, have lower socioeconomic resources (less income and employment), and poorer health status (physical and mental). In contrast, injured patients reported greater use of tobacco, alcohol, marijuana than did medical patients. Further, the binge drinker group was most likely to present for injury whereas the poly-drug user group was more likely to present for a medical complaint. Thus, it is clear that injured patients are generally relatively healthy but would benefit from screening and interventions for smoking, alcohol, and drug use, particularly for binge drinking. Data also suggest that medical patients would benefit from ED-based substance use screening and intervention, when needed, for several reasons. Women and African-Americans, the groups most likely to present with medical complaints, are more likely to have health disparities in obtaining substance use treatment (Cohen, et al., 2007). Rates of “hard” drugs (e.g., cocaine) and associated disorders (i.e., marijuana and cocaine) did not differ by presenting complaint which is consistent with a recent review (Vitale & Van de Mheen, 2006). Further, psychoactive prescription drugs did not differ based on presenting complaint. Although rates of alcohol abuse/dependence and SUDs were lower among medical patients than among injured patients, the number of medical patients presenting to the ED with SUDs greatly exceeded the number of injured patients with SUDs. Therefore, universal screening for substance use/SUD is recommended for inner city EDs.
The increased likelihood of ED visits among substance users has raised a call for effective and efficient methods of screening and intervention for alcohol and drug-related problems in emergency settings (Academic ED SBIRT Research Collaborative, 2007; Edward Bernstein & Bernstein, 2008). Of particular concern are those individuals who meet criteria for SUDs because they may have more frequent visits to the ED, higher costs, and poor health care outcomes. Although studies from primary care settings generally support the impact of BI’s on alcohol misuse (for meta-analysis see Kaner, et al., 2007), findings for the efficacy of BI’s on ED patients with alcohol misuse ((Bazargan-Hejazi, et al., 2005; Blow, et al., 2006; D'Onofrio, et al., 2008; Havard, Shakeshaft, & Sanson-Fisher, 2008; Mello, et al., 2005; Monti, et al., 2007; Neumann, et al., 2006; Soderstrom, et al., 2007) or with alcohol use disorders (Blow, et al., 2009; Guth, et al., 2008; Moyer, Finney, Swearingen, & Vergun, 2002; Vasilaki, Hosier, & Cox, 2006) are mixed. It is possible that focus on a single substance, such as alcohol, without examination of substance use more broadly, could explain discrepancies in findings. For example, data from this study suggests substantial overlap among binge drinking and marijuana use. Further, although studies from mostly non-ED settings support BI’s for illicit drug use (Baker, et al., 2005; Bernstein, et al., 2007; Bernstein, Bernstein, & Levenson, 1997; Stotts, Schmitz, Rhoades, & Grabowski, 2001; Tait, Hulse, Robertson, & Sprivulis, 2005), it is unclear if BI’s are effective for ED patients with poly-drug use and/or disorders. Given the heterogeneity in drug use classes, studies examining SBIRT approaches for drug use will need to tailor these approaches to illicit and psychoactive prescription drug use patterns. For example, the marijuana user/SUD class would necessitate different intervention content than the cocaine use/SUD; although both groups use alcohol and illicit drug use, prescription opiate use and injection drug use would also need to be addressed in the cocaine use group.
Limitations of this study include the possibility that the rates of alcohol and drug problems may have been underestimated because this study chose to omit the midnight shift from screening. Findings may not generalize to suburban or rural ED settings. Although it is possible that patients may have underreported their substance use, methods to increase validity of self-report were used including using standardized measures and assuring confidentiality. Replication of the latent classes identified in this sample is required with additional attention to other risk behaviors and other potential covariates. For example, prior research has suggested that substance use patterns vary by psychiatric co-morbidity (Agrawal, et al., 2007; Lynskey, et al., 2006).
5. Conclusions
An ED visit for care related to either injuries or a medical complaint may provide an ideal opportunity to target screening, BI, and linkage to treatment for individuals with substance use and SUDs. Given findings regarding rates of illicit and psychoactive prescription drug use and rates of drug use disorders among the inner city ED patients, and health disparities in access to substance use treatment among such patients, research is needed to develop and test interventions aimed at reducing poly-substance use and increasing substance use treatment entry among this vulnerable population.
Table 3.
Association of substance use group and socio-demographic and health variables.
| Variable | Class1 (Non-User/SUD) n=9597 (65.9%) | Class2 (Binge Drinkers) n=3541 (24.3%) | Class3 (Marijuana Use/SUD) n=508 (3.5%) | Class4 (Cocaine Use/SUD) n=429 (2.9%) | Class5 (Poly-drug Users) n=482 (3.3%) |
|---|---|---|---|---|---|
| Age | 37.3 (11.9) | 34.9 (11.1) | 34.2 (10.7) | 37.5 (10.2) | 28.3 (7.9) |
| Male | 37.31% | 60.58% | 57.36% | 62.47% | 70.08% |
| Black or African-American | 55.72% | 51.45% | 49.08% | 55.71% | 66.14% |
| Married or Living Together | 33.21% | 23.03% | 28.27% | 21.68% | 26.57% |
| Any college | 59.33% | 73.86% | 67.33% | 74.59% | 73.43% |
| With Health Insurance | 82.01% | 76.46% | 67.54% | 65.73% | 62.01% |
| Employed | 47.31% | 25.73% | 49.69% | 30.54% | 35.83% |
| Physical (≤ 25th Percentile) | 26.73% | 29.46% | 20.70% | 29.14% | 14.76% |
| Mental (≤ 25th Percentile) | 22.19% | 43.98% | 25.44% | 53.38% | 32.87% |
| Injury | 30.59% | 26.81% | 38.81% | 36.36% | 34.06% |
| Tobacco | 43.85% | 78.22% | 74.30% | 90.68% | 81.89% |
| Treatment Program | 2.02% | 31.12% | 4.32% | 23.08% | 10.43% |
Table 4.
Socio-demographic and health correlates of substance use/disorder groups.
| Variable | Class2 (Binge Drinkers)n=3541 (24.3%) | Class3 (Marijuana Use/SUD)n=508 (3.5%) | Class4 (Cocaine Use/SUD)n=429 (2.9%) | Class5 (Poly-drug Users)n=482 (3.3%) |
|---|---|---|---|---|
| Age | 0.98 (0.97– 0.98)* | 0.92 (0.91– 0.93)* | 0.99 (0.98–1.01) | 0.97 (0.97–0.98)* |
| Male | 2.02 (1.85– 2.20)* | 4.13 (3.34–5.10) * | 2.61 (2.10–3.25)* | 2.61 (2.12–3.21)** |
| Black or African- American | 0.94 (0.87–1.03) | 2.01 (1.64– 2.46)** | 1.24 (1.01–1.53)* | 0.88 (0.73–1.08) |
| Married or Living Together | 0.85 (0.78–0.93) | 1.02 (0.82–1.26) | 0.74 (0.58–0.95) | 0.83 (0.66–1.04) |
| Any College | 0.98 (0.90–1.09) | 1.07 (0.86–1.33) | 0.84 (0.67–1.07) | 0.87 (0.70–1.09) |
| With Health Insurance | 0.65 (0.59– 0.72)* | 0.57 (0.46– 0.69)** | 0.51 (0.41–0.64)* | 0.90 (0.71–1.13) |
| Employed | 1.15 (1.05– 1.26)* | 0.72 (0.59– 0.88)* | 0.78 (0.62–0.99)* | 0.57 (0.45–0.71)* |
| Physical (≤25th Percentile) | 0.87 (0.78– 0.96)* | 0.75 (0.57– 0.98)* | 0.93 (0.73–1.18) | 1.05 (0.84–1.32) |
| Mental (≤25th Percentile) | 1.32 (1.20– 1.46)* | 2.20 (1.78– 2.70)* | 3.93 (3.18–4.86)* | 2.54 (2.07–3.11)* |
| Injury | 1.13 (1.03– 1.23)* | 0.93 (0.76–1.14) | 1.15 (0.93–1.43) | 0.72 (0.58–.90)** |
| Tobacco | 3.33 (3.05– 3.65)* | 5.29 (4.16– 6.73)* | 8.35 (5.98–11.67)* | 2.98 (2.36–3.76)* |
| Treatment Program | 1.46 (1.16– 1.83)* | 3.20 (2.27– 4.50)** | 7.57 (5.70– 10.04)*** | 12.38(9.60– 15.96)*** |
Note: Class 1 (Non-use) is the reference group for the regression. AOR (Adjusted odds ratio and 95% confidence interval)
Acknowledgments
We would like to thank the project staff for their work on the project and Peter De Chavez for assistance with data analyses. Finally, special thanks are owed to the patients and medical staff at Hurley Medical Center for their support of this project.
References
- Academic ED SBIRT Research Collaborative. The impact of screening, brief intervention, and referral for treatment on emergency department patients' alcohol use. Ann Emerg Med. 2007;50(6):699–710. doi: 10.1016/j.annemergmed.2007.06.486. [DOI] [PubMed] [Google Scholar]
- Adrian M, Barry S. Physical and mental health problems associated with the use of alcohol and drugs. Subst Use Misuse. 2003;38(11–13):1575–1614. doi: 10.1081/ja-120024230. [DOI] [PubMed] [Google Scholar]
- Agrawal A, Lynskey M, Madden P, Bucholz K, Heath A. A latent class analysis of illicit drug abuse/dependence: results from the National Epidemiological Survey on Alcohol and Related Conditions. Addiction. 2007;102(1):94–104. doi: 10.1111/j.1360-0443.2006.01630.x. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: APA; 1994. [Google Scholar]
- Baker A, Lee N, Claire M, Lewin T, Grant T, Pohlman S, et al. Brief cognitive behavioural interventions for regular amphetamine users: a step in the right direction. Addiction. 2005;100(3):367–378. doi: 10.1111/j.1360-0443.2005.01002.x. [DOI] [PubMed] [Google Scholar]
- Baker D, Stevens C, Brook R. Patients who leave a public hospital emergency department without being seen by a physician. Causes and consequences. JAMA. 1991;266(8):1085–1090. [PubMed] [Google Scholar]
- Barry K, Milner K, Blow F, Impens A, Welsh D, Amash J. Screening psychiatric emergency department patients with major mental illnesses for at-risk drinking. Psychiatr Serv. 2006;57(7):1039–1042. doi: 10.1176/ps.2006.57.7.1039. [DOI] [PubMed] [Google Scholar]
- Bazargan-Hejazi S, Bing E, Bazargan M, Der-Martirosian C, Hardin E, Bernstein J, et al. Evaluation of a brief intervention in an inner-city emergency department. Ann Emerg Med. 2005;46(1):67–76. doi: 10.1016/j.annemergmed.2004.10.014. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Bernstein J. Effectiveness of alcohol screening and brief motivational intervention in the emergency department setting. Ann Emerg Med. 2008;51(6):751–754. doi: 10.1016/j.annemergmed.2008.01.325. [DOI] [PubMed] [Google Scholar]
- Bernstein E, Bernstein J, Feldman J, Fernandez W, Hagan M, Mitchell P, et al. An evidence based alcohol screening, brief intervention and referral to treatment (SBIRT) curriculum for emergency department (ED) providers improves skills and utilization. Subst Abus. 2007;28(4):79–92. doi: 10.1300/J465v28n04_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein E, Bernstein J, Levenson S. Project ASSERT: an ED-based intervention to increase access to primary care, preventive services, and the substance abuse treatment system. Ann Emerg Med. 1997;30(2):181–189. doi: 10.1016/s0196-0644(97)70140-9. [DOI] [PubMed] [Google Scholar]
- Bindman A, Grumbach K, Keane D, Rauch L, Luce J. Consequences of queuing for care at a public hospital emergency department. JAMA. 1991;266(8):1091–1096. [PubMed] [Google Scholar]
- Blow F, Barry K, Walton M, Maio R, Chermack S, Bingham C, et al. The efficacy of two brief intervention strategies among injured, at-risk drinkers in the emergency department: Impact of tailored messaging and brief advice. J Stud Alcohol. 2006;67(4):568–578. doi: 10.15288/jsa.2006.67.568. [DOI] [PubMed] [Google Scholar]
- Blow F, Ilgen M, Walton M, Czyz E, McCammon R, Chermack S, et al. Severity of baseline alcohol use as a moderator of brief interventions in the emergency department. Alcohol Alcohol. 2009;44(5):486–490. doi: 10.1093/alcalc/agp031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth B, Weber J, Walton M, Cunningham R, Massey L, Thrush C, et al. Characteristics of cocaine users presenting to an emergency department chest pain observation unit. Acad Emerg Med. 2005;12(4):329–337. doi: 10.1197/j.aem.2004.11.021. [DOI] [PubMed] [Google Scholar]
- Chen K, Scheier L, Kandel D. Effects of chronic cocaine use on physical health: a prospective study in a general population sample. Drug Alcohol Depend. 1996;43(1–2):23–37. doi: 10.1016/s0376-8716(96)01285-9. [DOI] [PubMed] [Google Scholar]
- Cherpitel C. Drinking patterns and problems: a comparison of ER patients in an HMO and in the general population. Alcohol Clin Exp Res. 1992;16(6):1104–1109. doi: 10.1111/j.1530-0277.1992.tb00705.x. [DOI] [PubMed] [Google Scholar]
- Cherpitel C. Alcohol and violence-related injuries: an emergency room study. Addiction. 1993;88(1):79–88. doi: 10.1111/j.1360-0443.1993.tb02765.x. [DOI] [PubMed] [Google Scholar]
- Cherpitel C. Alcohol and violence-related injuries in the emergency room. Recent Dev Alcohol. 1997;13:105–123. doi: 10.1007/0-306-47141-8_6. [DOI] [PubMed] [Google Scholar]
- Cherpitel C. Differences in performance of screening instruments for problem drinking among blacks, whites and Hispanics in an emergency room population. J Stud Alcohol. 1998;59(4):420–426. doi: 10.15288/jsa.1998.59.420. [DOI] [PubMed] [Google Scholar]
- Cherpitel C. Changes in substance use associated with emergency room and primary care services utilization in the United States general population: 1995–2000. Am J Drug Alcohol Abuse. 2003;29(4):789–802. doi: 10.1081/ada-120026261. [DOI] [PubMed] [Google Scholar]
- Cohen E, Feinn R, Arias A, Kranzler H. Alcohol treatment utilization: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;86(2–3):214–221. doi: 10.1016/j.drugalcdep.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Compton W, Thomas Y, Stinson F, Grant B. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007;64(5):566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Cornwell E, Belzberg H, Velmahos G, Chan L, Demetriades D, Stewart B, et al. The prevalence and effect of alcohol and drug abuse on cohort-matched critically injured patients. Am Surg. 1998;64(5):461–465. [PubMed] [Google Scholar]
- D'Onofrio G, Degutis L. Screening and brief intervention in the emergency department. Alcohol Res Health. 2004;28(2):63–72. [PMC free article] [PubMed] [Google Scholar]
- D'Onofrio G, Pantalon M, Degutis L, Fiellin D, Busch S, Chawarski M, et al. Brief intervention for hazardous and harmful drinkers in the emergency department. Ann Emerg Med. 2008;51(6):742–750. doi: 10.1016/j.annemergmed.2007.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Guebaly N, Armstrong S, Hodgins D. Substance abuse and the emergency room: programmatic implications. J Addict Dis. 1998;17(2):21–40. doi: 10.1300/J069v17n02_03. [DOI] [PubMed] [Google Scholar]
- Fleming M, Barry K, Manwell L, Johnson K, London R. Brief physician advice for problem alcohol drinkers. A randomized controlled trial in community-based primary care practices. JAMA. 1997;277(13):1039–1045. [PubMed] [Google Scholar]
- Garrity T, Leukefeld C, Carlson R, Falck R, Wang J, Booth B. Physical health, illicit drug use, and demographic characteristics in rural stimulant users. J Rural Health. 2007;23(2):99–107. doi: 10.1111/j.1748-0361.2007.00076.x. [DOI] [PubMed] [Google Scholar]
- Grant B. Comorbidity between DSM-IV drug use disorders and major depression: results of a national survey of adults. J Subst Abuse. 1995;7(4):481–497. doi: 10.1016/0899-3289(95)90017-9. [DOI] [PubMed] [Google Scholar]
- Grumbach K, Keane D, Bindman A. Primary care and public emergency department overcrowding. Am J Public Health. 1993;83(3):372–378. doi: 10.2105/ajph.83.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guth S, Lindberg S, Badger G, Thomas C, Rose G, Helzer J. Brief intervention in alcohol-dependent versus nondependent individuals. J Stud Alcohol. 2008;69(2):243–250. doi: 10.15288/jsad.2008.69.243. [DOI] [PubMed] [Google Scholar]
- Havard A, Shakeshaft A, Sanson-Fisher R. Systematic review and meta-analyses of strategies targeting alcohol problems in emergency departments: interventions reduce alcohol-related injuries. Addiction. 2008;103(3):368–376. doi: 10.1111/j.1360-0443.2007.02072.x. [DOI] [PubMed] [Google Scholar]
- Johnson M, Brems C, Burke S. Recognizing comorbidity among drug users in treatment. Am J Drug Alcohol Abuse. 2002;28(2):243–261. doi: 10.1081/ada-120002973. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Huang FY, Davies M. Comorbidity between patterns of substance use dependence and psychiatric syndromes. Drug Alcohol Depend. 2001;64(2):233–241. doi: 10.1016/s0376-8716(01)00126-0. [DOI] [PubMed] [Google Scholar]
- Kaner E, Beyer F, Dickinson H, Pienaar E, Campbell F, Schlesinger C, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2007;(2):CD004148. doi: 10.1002/14651858.CD004148.pub3. [DOI] [PubMed] [Google Scholar]
- Lynskey M, Agrawal A, Bucholz K, Nelson E, Madden P, Todorov A, et al. Subtypes of illicit drug users: a latent class analysis of data from an Australian twin sample. Twin Res Hum Genet. 2006;9(4):523–530. doi: 10.1375/183242706778024964. [DOI] [PubMed] [Google Scholar]
- Marzuk P, Tardiff K, Leon A, Hirsch C, Stajic M, Portera L, et al. Fatal injuries after cocaine use as a leading cause of death among young adults in New York City. N Engl J Med. 1995;332(26):1753–1757. doi: 10.1056/NEJM199506293322606. [DOI] [PubMed] [Google Scholar]
- McCaig L, Burt C. National Hospital Ambulatory Medical Care Survey: 2001 emergency department summary. Adv Data. 2003;(335):1. [PubMed] [Google Scholar]
- Mello M, Nirenberg T, Longabaugh R, Woolard R, Minugh A, Becker B, et al. Emergency department brief motivational interventions for alcohol with motor vehicle crash patients. Ann Emerg Med. 2005;45(6):620–625. doi: 10.1016/j.annemergmed.2005.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monti P, Barnett N, Colby S, Gwaltney C, Spirito A, Rohsenow D, et al. Motivational interviewing versus feedback only in emergency care for young adult problem drinking. Addiction. 2007;102(8):1234–1243. doi: 10.1111/j.1360-0443.2007.01878.x. [DOI] [PubMed] [Google Scholar]
- Moyer A, Finney J, Swearingen C, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97(3):279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- Neumann T, Neuner B, Weiss-Gerlach E, Psych D, Tønnesen H, Gentilello L, et al. The effect of computerized tailored brief advice on at-risk drinking in subcritically injured trauma patients. J Trauma. 2006;61(4):805–814. doi: 10.1097/01.ta.0000196399.29893.52. [DOI] [PubMed] [Google Scholar]
- Pane G, Farner M, Salness K. Health care access problems of medically indigent emergency department walk-in patients. Ann Emerg Med. 1991;20(7):730–733. doi: 10.1016/s0196-0644(05)80832-7. [DOI] [PubMed] [Google Scholar]
- Rockett I, Putnam S, Jia H, Smith G. Assessing substance abuse treatment need: a statewide hospital emergency department study. Ann Emerg Med. 2003;41(6):802–813. doi: 10.1067/mem.2003.189. [DOI] [PubMed] [Google Scholar]
- SAS (Version 9.2) Cary, NC: SAS Institute; [Google Scholar]
- Saunders J, Aasland O, Babor T, Fuente J, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Smith G, Burnam M, Mosley C, Hollenberg J, Mancino M, Grimes W. Reliability and validity of the substance abuse outcomes module. Psychiatr Serv. 2006;57(10):1452–1460. doi: 10.1176/ps.2006.57.10.1452. [DOI] [PubMed] [Google Scholar]
- Soderstrom C, DiClemente C, Dischinger P, Hebel J, McDuff D, Auman K, et al. A controlled trial of brief intervention versus brief advice for at-risk drinking trauma center patients. J Trauma. 2007;62(5):1102–1112. doi: 10.1097/TA.0b013e31804bdb26. [DOI] [PubMed] [Google Scholar]
- Soderstrom C, Dischinger P, Kerns T, Trifillis A. Marijuana and other drug use among automobile and motorcycle drivers treated at a trauma center. Accid Anal Prev. 1995;27(1):131–135. doi: 10.1016/0001-4575(94)00043-l. [DOI] [PubMed] [Google Scholar]
- Soderstrom C, Trifillis A, Shankar B, Clark W, Cowley R. Marijuana and alcohol use among 1023 trauma patients. A prospective study. Arch Surg. 1988;123(6):733–737. doi: 10.1001/archsurg.1988.01400300079013. [DOI] [PubMed] [Google Scholar]
- Stotts A, Schmitz J, Rhoades H, Grabowski J. Motivational interviewing with cocaine-dependent patients: A pilot study. J Consult Clin Psychol. 2001;69(5):858–862. doi: 10.1037//0022-006x.69.5.858. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. NSDUH Series H-25, DHHS Publication No SMA 04-3964. Office of Applied Studies; Rockville, MD: 2004. Results from the 2003 National Survey on Drug Use and Health: National findings. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. NSDUH Series H-30, DHHS Publication No SMA 06-4194. Office of Applied Studies; Rockville, MD: 2006. Results from the 2005 National Survey on Drug Use and Health: National findings. [Google Scholar]
- Tait R, Hulse G, Robertson S, Sprivulis P. Emergency department-based intervention with adolescent substance users: 12-month outcomes. Drug Alcohol Depend. 2005;79(3):359–363. doi: 10.1016/j.drugalcdep.2005.03.015. [DOI] [PubMed] [Google Scholar]
- Vasilaki E, Hosier S, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: a meta-analytic review. Alcohol Alcohol. 2006;41(3):328–335. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- Vincent N, Schoobridge J, Ask A, Allsop S, Ali R. Physical and mental health problems in amphetamine users from metropolitan Adelaide, Australia. Drug Alcohol Rev. 1998;17(2):187–195. doi: 10.1080/09595239800186991. [DOI] [PubMed] [Google Scholar]
- Vitale S, Van de Mheen H. Illicit drug use and injuries: A review of emergency room studies. Drug Alcohol Depend. 2006;82(1):1–9. doi: 10.1016/j.drugalcdep.2005.08.017. [DOI] [PubMed] [Google Scholar]
- Wallace P, Cutler S, Haines A. Randomised controlled trial of general practitioner intervention in patients with excessive alcohol consumption. Br Med J. 1988;297(6649):663–668. doi: 10.1136/bmj.297.6649.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE., Jr Scales for measuring general health perceptions. Health Serv Res. 1976;11(4):396–415. [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Jr, Sherbourne C. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992:473–483. [PubMed] [Google Scholar]