Abstract
Objective
To describe factors associated with multimorbidity in community-dwelling older adults; to determine if a simple measure of multimorbidity predicts death over 5 years; and to assess if any effect of multimorbidity on mortality is independent of key covariates.
Design
Analysis of an existing population-based cohort study. Cox proportional hazards models were constructed for time to death.
Setting
Manitoba.
Participants
A total of 1751 community-dwelling adults aged 65 and older were interviewed and followed for 5 years.
Main outcome measures
Age, sex, marital status, living arrangement, education, Mini-Mental State Examination (MMSE) score, Center for Epidemiologic Studies Depression Scale score, and the Older Americans Resource and Services Multidimensional Functional Assessment Questionnaire score were recorded for each participant. Multimorbidity was defined based on a simple list of common health complaints and diseases, followed by an open-ended question about other problems. These were summed and the scores ranged from 0 to 16. Death and time of death were determined during the 5-year interval by death certificate, administrative data, or proxy report.
Results
Multimorbidity was more prevalent in women; older age groups; and those with lower educational levels, lower MMSE scores, more depressive symptoms, and higher levels of disability. Multimorbidity was a predictor of mortality in unadjusted models (hazard ratio 1.09, 95% CI 1.05 to 1.12). In models adjusting for age, sex, education, marital status, living arrangement, and Center for Epidemiologic Studies Depression Scale and MMSE scores, this effect persisted (hazard ratio 1.04, 95% CI 1.00 to 1.08). However, after adjusting for functional status, the effect of multimorbidity was no longer significant.
Conclusion
Multimorbidity predicts 5-year mortality but the effect might be mediated by disability.
Résumé
Objectif
Déterminer les facteurs associés à la multi-morbidité chez les personnes âgées qui vivent dans la communauté; vérifier si une simple mesure de multi-morbidité permet de prédire la mort sur une période de 5 ans; et établir si un éventuel effet de la multi-morbidité sur la mortalité est indépendant de certaines covariables clés.
Type d’étude
Analyse d’une étude déjà en cours sur une cohorte de nature démographique. Des modèles à risque proportionnel de Cox ont été utilisés pour établir le moment de la mort.
Contexte
Le Manitoba.
Participants
Un total de 1751 personnes de 65 ans et plus vivant dans la communauté ont été interviewés et suivis pendant 5 ans.
Principaux paramètres à l’étude
Pour chaque participant, on a noté l’âge, le sexe, l’état matrimonial, les conditions de logement, la scolarité et les scores au mini-examen de l’état mental (MMSE), à l’échelle de dépression du centre d’études épidémiologiques et à l’Older Americans Resource and Services Multidimensional Functional Assessment Questionnaire. Pour définir la multi-morbidité, on s’est basé sur une simple liste des plaintes et des maladies des participants, suivie d’une question ouverte portant sur d’autres problèmes. On a fait la somme des problèmes de santé et attribué des scores allant de 0 à 16. La mort et le moment du décès au cours des 5 années du suivi ont été établis grâce aux certificats de décès, aux données administratives et à des rapports substitutifs.
Résultats
La prévalence de la multi-morbidité était plus élevée chez les femmes, dans les groupes plus âgés et chez les moins scolarisés, et chez ceux qui avaient un score plus bas au MMSE, plus de symptômes de dépression et un plus haut niveau d’incapacité. La multi-morbidité était un prédicteur de mortalité dans les modèles non ajustés (rapport de risque 1,09, IC à 95 % 1,05 à 1,12). On observait le même effet dans les modèles ajustés pour l’âge, le sexe, la scolarité, l’état matrimonial, et les conditions de vie, et pour les scores à l’échelle de dépression du centre d’études épidémiologiques et au MMSE (rapport de risque 1,04, IC à 95 % 1,00 à 1,08). Toutefois, après ajustement pour l’état fonctionnel, l’effet de la multi-morbidité n’était plus significatif.
Conclusion
La multi-morbidité est prédictive de la mortalité de 5 ans, mais cet effet pourrait être dû à une incapacité.
Diseases often cluster together,1–3 sharing common risk factors and antecedents. Multimorbidity is important, as the cumulative effect of diseases might be more substantial than the effect of any one disease. Moreover, it might complicate the care of people with multiple comorbid conditions. Treating all existing diseases could result in a substantial burden of care and polypharmacy if guidelines for treating each individual condition are followed.4 As well, the prognosis of people with multimorbidities might be poor, particularly in older populations.
Multiple comorbidities are common,5–9 especially in older adults.10,11 Reported prevalence varies, depending on sampling frame and measurement of multimorbidities,12 and there are relatively few prospective studies of multimorbidities.13,14 The importance of multimorbidity has long been recognized in clinical care15,16 and in epidemiologic studies.17 However, it has received much less attention than the epidemiology of single-system diseases.18 More recently, primary care research has begun to investigate the epidemiology of multimorbidities. Definitions and approaches to measurement have been reviewed19–21 and scales have been developed and proposed for different settings.22–25 The effect of multimorbidities on health outcomes has received increased attention: multimorbidities predict mortality and hospitalization,26,27 lower health-related quality of life,28 psychological distress,29 depression,30 and disability.31–33 Increasingly, studies are conducted in populations with specific diseases; for example, multimorbidity predicts death in persons with colon cancer33 and cardiovascular disease.34
Disability is also common late in life, and is often related to multimorbidity.35,36 Commonly, it is the accumulation of clinical and subclinical diseases that predicts disability. These diseases might interact and have aggregate effects on functional capacity that are greater than the effect of any single disease. Disability predicts death and institutionalization in community-dwelling and hospitalized older adults. Yet, disability might not be considered in risk scores, clinical predication rules, or case-mix adjustment.37
In spite of this long-standing recognition, treatment guidelines rarely consider the co-occurrence of disease or disability. Moreover, the current organ-based specialization model in medicine might not be the ideal model of care for those with multimorbidities and disability. Some have therefore advocated for changes to the health care system that would recognize the complexity of the medical status of those with multimorbidities, and the long duration of the disease trajectories.7,38–43 There is also a need for research into the care of those with multimorbidities, as there is currently little study into interventions in these groups.44,45
Measurement of multimorbidity is difficult. Diseases might need to be weighted differently, as their effect on mortality, disability, and health service use might differ. Disease severity is also important, with varying degrees of organ failure having markedly different expected outcomes. The effect of some diseases might be modified by the existence of other diseases and deficits. Interactions between diseases and other factors such as sex, age, and disability might also be important. Finally, the measurement of multimorbidity might be limited by the availability of data. Administrative, biomedical, and self-reported data all differ in availability and accuracy. In spite of problems in defining and measuring multimorbidity, the notion of a complex, cumulative effect of health problems remains critical to the care of many people. Most previous studies have been conducted in clinical samples or using administrative data. There are few population-based studies and few studies using self-reported data or simple, easily gathered data. There are also few population-based studies that consider potential confounding or mediating factors such as depression, cognition, and disability. We have therefore conducted an analysis of an existing population-based cohort study of aging and cognition, with the following objectives26:
to describe factors associated with multimorbidity in community-dwelling older adults;
to determine if a simple measure of multimorbidity consisting of self-reported health problems predicts death over 5 years in community-dwelling older adults; and
to determine if any effect of multimorbidity on mortality is independent of the effects of age, sex, education, cognition, functional status, and depressive symptoms.
METHODS
Population
Analyses were based on secondary data from the Manitoba Study of Health and Aging (MSHA), a population-based study conducted in Manitoba in conjunction with the Canadian Study of Health and Aging.26 The original aims of this study were to determine prevalence and risk factors for dementia in Manitoba, and to examine social correlates of aging. In 1991 to 1992, community-dwelling adults aged 65 and older were interviewed (this is referred to as time 1). The original sampling frame was from a list provided by Manitoba Health, and was comprehensive and representative. Older age groups (older than 85 years) were oversampled, and sampling was stratified by region, with representation from the entire province. Persons residing in institutions (nursing homes and chronic care hospitals) did not undergo the screening interview and were not included in these analyses. Initially, 2890 persons were selected, of whom 1751 were enrolled. These participants underwent follow-up clinical assessments 5 years later (referred to as time 2). Informed consent was obtained from participants or appropriate proxies. The research was approved by the Research Ethics Committee of the Faculty of Medicine at the University of Manitoba, and adhered to the Declaration of Helsinki.
Measures
Participants were interviewed in their homes by trained interviewers. Data gathered included age, sex, education level (years of education), living arrangement (alone vs not alone), and marital status, which we categorized as never married, married, separated or divorced, and widowed. The Center for Epidemiologic Studies Depression Scale (CES-D)27 was used to measure depressive symptoms. This is a valid, reliable measure of depressive symptoms. We considered the score as a continuous factor scored from 0 to 60, as in this data set the CES-D predicts death across the entire scale.46 The Modified Mini-Mental State Examination (3MS)47 was used as the screening test for cognitive impairment and dementia. The 3MS is an expanded version of the Mini-Mental State Examination (MMSE); Teng et al added items on date and place of birth, animal naming, similarities, and a second recall task and expanded scoring of each question from 30 points to 100 points.47 The 3MS was conducted in a manner that allowed calculation of the MMSE. We considered the MMSE score as a continuous factor. In looking for interactions, we dichotomized the MMSE score at a cut point of 24, with scores of 24 or greater indicating cognitive impairment.
Functional status was measured by asking participants about their ability to perform basic activities of daily living (ADL) (eating, dressing, grooming, getting in and out of bed, taking a bath or shower, and using the bathroom), instrumental activities of daily living (using the telephone, getting to places farther than walking distance, going shopping, preparing meals, doing housework, taking medications, managing money), and ambulation. A disability was defined as a need for help with, or an inability to perform, 1 or more of the activities listed. For ambulation, walking independently with a cane was not defined as a disability. These questions were derived from the ADL and instrumental activities of daily living portions of the Older Americans Resources and Services Multidimensional Functional Assessment Questionnaire (OMFAQ).48 Methodology from the OMFAQ was used to categorize subjects by function into the following groups: excellent or good function; mild disability; or moderate or severe disability. Briefly, those with excellent or good functional status could perform all ADLs without assistance, and those with mild disability could perform all but 1 to 3 ADLs and could get through a single day without help. Those with moderate or severe disability needed regular assistance with at least 4 ADLs, and might have had difficulty getting through a single day unassisted.
In addition to these standardized measures, the participants in the MSHA were asked a series of questions about their health. The questions were introduced with the following sentence: “Now, I will read a list of health problems that people often have. For each problem that I read, please tell me if you have had it in the past year. You can just answer yes or no.” The health conditions elicited were high blood pressure, heart and circulation problems, stroke or the effects of stroke, arthritis or rheumatism, Parkinson disease, other neurologic problems, eye trouble, ear trouble, dental problems, chest problems, stomach trouble, kidney trouble, loss of bladder control, loss of bowels control, diabetes, foot or ankle trouble, skin problems, fractures, cancer, and memory loss. Subsequently, participants were asked to report other health problems, and these were simply listed. We totaled the number of positive answers a participant gave, which produced a score from 0 to 36. The maximum score for any individual was 16. For baseline comparisons and for graphic representations, we categorized the score into 0 health problems, 1 to 3 health problems, 4 to 6 health problems, and 7 or more health problems. For all other analyses, we considered the score as a continuous risk. After these questions, participants were asked the following: “How much do your health troubles stand in the way of doing the things you want to do?” Possible answers were “not at all,” “a little,” and “a great deal.”
Time to death was considered the primary outcome for these analyses. Death during the 5-year interval was obtained by proxy reports, death certificates, and administrative records. Mortality was coded as either alive or deceased by the time 2 assessment. The time to death was determined using the methodology of the Canadian Study of Health and Aging.14 Briefly, if death certificate data were available (n = 247), the date of death on the death certificate was used. If death certificate data were not available, then the date of death was obtained from proxy report (n = 73) or administrative data (n = 97). The participants were considered to have been censored after the end of the time 2 follow-up phase, which included deaths up to the clinical assessments at time 2.
Statistical analyses
All participants for whom complete data were available were included in this analysis (N = 1751). Associations between time 1 variables, and between time 1 variables and the risk of mortality were assessed using χ2 tests and ANOVA (analysis of variance). To determine differences in the risk of death over time, Kaplan-Meier plots were constructed and log-rank tests were used. To adjust for the effect of confounding variables, Cox proportional hazards regression models were constructed with the outcome being the time to death. Covariates included age, sex, education, CES-D score, MMSE score, OMFAQ score, marital status, living arrangement, and multimorbidity scale score. Continuous variables were entered directly into the model, while categorical variables were entered as dummy variables. For graphs and bivariate analyses, we categorized the multimorbidity score; for regression models, we considered it as a continuous measure. Interactions were sought by stratifying analyses, and by the inclusion of interaction terms into Cox proportional hazards models. Analyses were conducted in SPSS, version 9, and Stata, version 10.
RESULTS
There were 1751 participants who participated in the screening questionnaire. Of these, 417 had died by the end of the 5-year observation period. There were very few people with no chronic health problems (n = 88), and the mean (SD) number of health complaints was 4.4 (2.9). Those with more multimorbidities were older, more likely to be women, and had less education. They also had lower MMSE scores, and substantially more depressive symptoms. There was also a very strong relationship between multimorbidity and disability, as well as a strong association between multimorbidity and health troubles interfering with daily life (Table 1).
Table 1.
Baseline characteristics of sample by number of comorbid conditions: N = 1751.
| CHARACTERISTICS |
NO. OF COMORBID CONDITIONS
|
TOTAL SAMPLE | |||
|---|---|---|---|---|---|
| NONE (N = 88) | 1–3 (N = 662) | 4–6 (N =605) | ≥ 7 (N =396) | ||
| Mean age, y | 74.2* | 76.2* | 78.2* | 79.4* | 77.5 |
| Female sex, % | 47.7* | 52.1* | 60.5* | 68.7* | 58.5 |
| Mean education, y | 10.7* | 9.7* | 9.4* | 8.3* | 9.3 |
| Living alone, % | 34.1* | 38.4* | 42.6* | 50.8* | 42.4 |
| Marital status, % | |||||
| • Never married | 8.0 | 6.6 | 5.5 | 4.5 | 5.8 |
| • Married | 59.8* | 55.7* | 50.2* | 41.7* | 50.9 |
| • Separated or divorced | 4.6 | 3.3 | 2.5 | 2.8 | 3.0 |
| • Widowed | 27.6* | 34.3* | 41.8* | 51.0* | 40.3 |
| Functional status, % | |||||
| • Excellent or good | 93.2* | 81.4* | 57.4* | 30.1* | 62.1 |
| • Mild impairment | 5.7* | 13.1* | 29.9* | 44.7* | 25.7 |
| • Moderate or severe impairment | 1.1* | 5.4* | 12.7* | 25.3* | 12.2 |
| Troubles interfere with activities, % | |||||
| • A great deal | 0.0* | 7.0* | 34.7* | 52.0* | 22.9 |
| • A little | 14.8* | 28.5* | 42.4* | 35.0* | 34.1 |
| • Not at all | 85.2* | 64.5* | 32.9* | 12.9* | 43.0 |
| Mean MMSE score (range 0–30) | 27.5* | 26.7* | 26.2* | 25.2* | 26.2 |
| Mean CES-D score (range 0–60) | 3.2* | 4.7* | 8.3* | 12.4* | 7.6 |
CES-D—Centre for Epidemiologic Studies Depression Scale, MMSE—Mini-Mental State Examination.
Denotes significant difference between groups (P < .05).
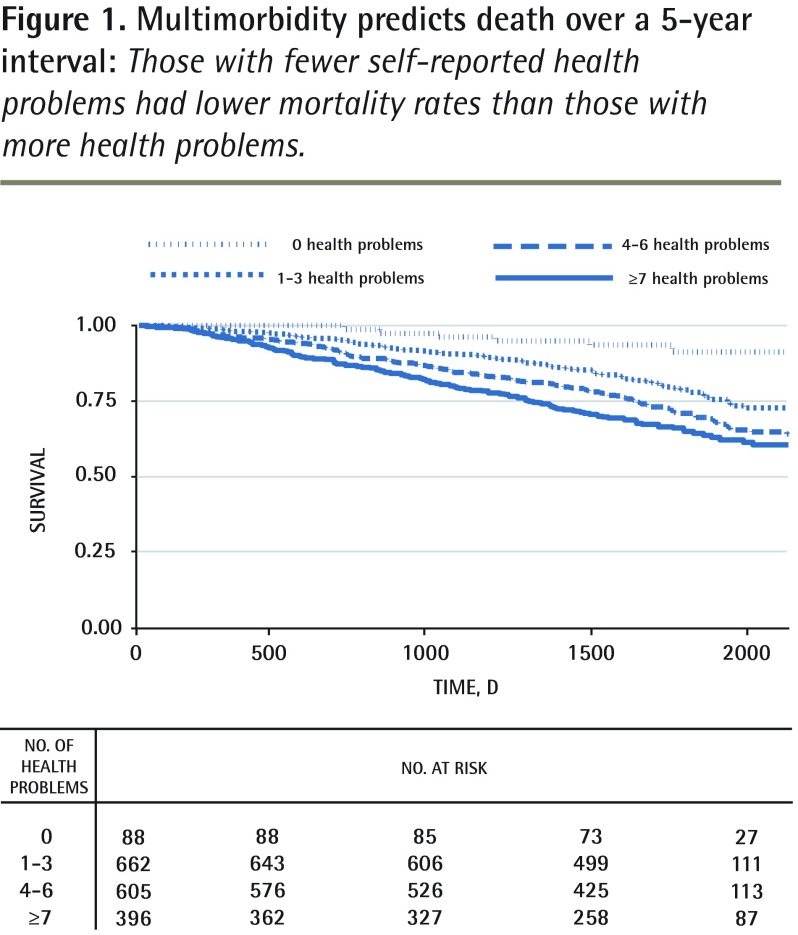
There was also a strong association between multimorbidity and mortality (Figure 1). In Cox regression models, this effect remained strong and statistically significant (P < .05) after adjusting for age, sex, and education, with more multimorbidities predicting a higher mortality risk (Table 2, model 2). Increasing age and male sex were associated with a higher mortality rate. Inclusion of depressive symptoms and cognitive function reduced the strength of the association between multimorbidity and mortality (Table 2, model 3). After further inclusion of functional status in the model, multimorbidity was no longer significantly associated with mortality (Table 2, model 4). Only age, sex, and cognition remained significant predictors (P < .05) after considering the effect of disability, which was strongly associated with mortality.
Figure 1.
Multimorbidity predicts death over a 5-year interval: Those with fewer self-reported health problems had lower mortality rates than those with more health problems.
Table 2.
The association between multimorbidity and 5-year mortality in community-dwelling older adults: N = 1751.
| FACTOR |
HAZARD RATIO FOR 5-YEAR MORTALITY (95% CI)
|
|||
|---|---|---|---|---|
| MODEL 1 | MODEL 2 | MODEL 3 | MODEL 4 | |
| Comorbid conditions | 1.09 (1.05 to 1.12) | 1.06 (1.02 to 1.09) | 1.04 (1.00 to 1.08) | 1.00 (0.96 to 1.04) |
| Older age | 1.08 (1.06 to 1.09) | 1.07 (1.05 to 1.08) | 1.06 (1.04 to 1.07) | |
| Female sex | 0.53 (0.43 to 0.64) | 0.54 (0.44 to 0.66) | 0.50 (0.41 to 0.62) | |
| More education | 0.98 (0.96 to 1.01) | 1.01 (0.98 to 1.04) | 1.00 (0.97 to 1.04) | |
| Marital status | ||||
| • Never married | Reference | Reference | ||
| • Married | 0.82 (0.55 to 1.23) | 0.89 (0.59 to 1.33) | ||
| • Separated or divorced | 1.30 (0.69 to 2.46) | 1.36 (0.72 to 2.58) | ||
| • Widowed | 0.96 (0.64 to 1.45) | 1.03 (0.68 to 1.55) | ||
| MMSE score | 0.94 (0.92 to 0.97) | 0.96 (0.93 to 0.99) | ||
| CES-D score | 1.01 (1.00 to 1.02) | 1.01 (0.99 to 1.02) | ||
| Functional status | ||||
| • Excellent or good | Reference | |||
| • Mild impairment | 1.80 (1.39 to 2.33) | |||
| • Moderate or severe impairment | 2.54 (1.91 to 3.41) | |||
CES-D—Centre for Epidemiologic Studies Depression Scale; MMSE—Mini-Mental State Examination.
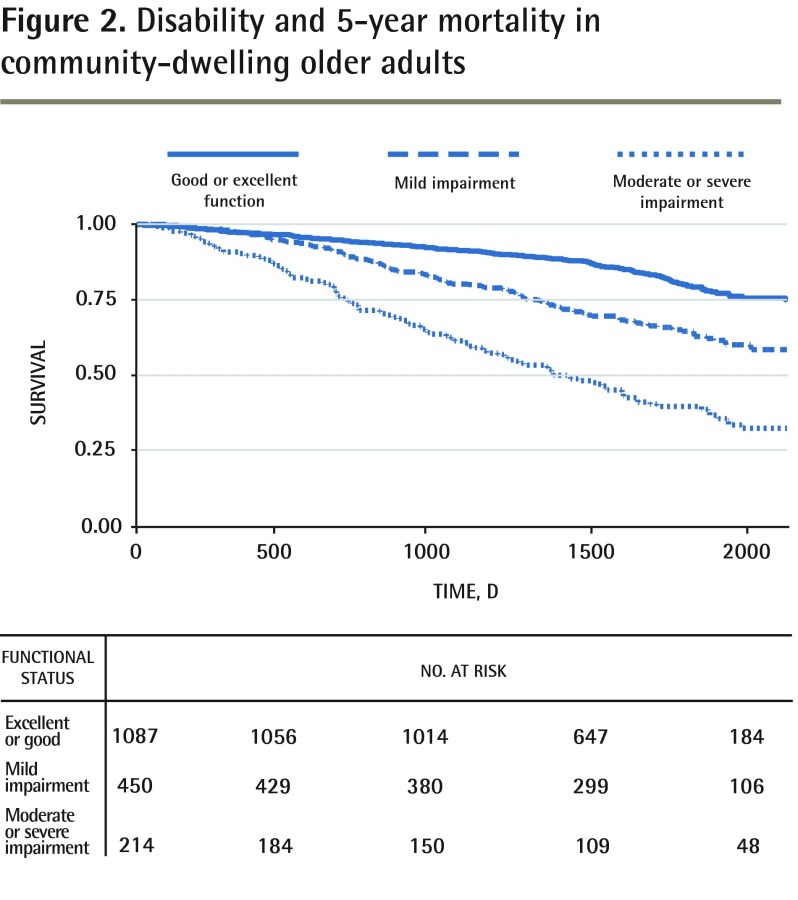
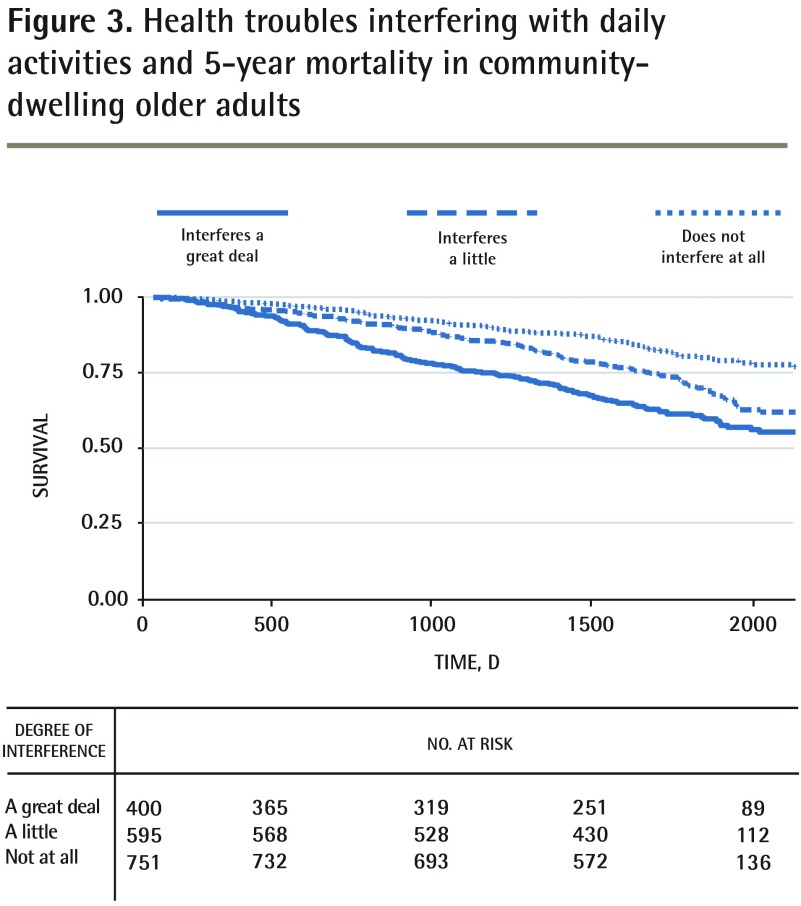
The association between disability and mortality noted in the regression models (Table 2) was also reflected in survival curves (Figure 2). Answers to the simple question, “How much do your health troubles stand in the way of doing the things you want to do?” also strongly predicted mortality (Figure 3): 16% of those who answered “not at all” were deceased by time 2 versus 26% of those who answered “a little” and 35% of those who responded “a great deal” (P < .01, χ2 test).
Figure 2.
Disability and 5-year mortality in community-dwelling older adults
Figure 3.
Health troubles interfering with daily activities and 5-year mortality in community-dwelling older adults
DISCUSSION
We have observed that number of self-reported health problems is associated with education, sex, depressive symptoms, and functional status. Further, this simple sum is a predictor of 5-year mortality in older adults in models adjusting for some important confounding factors. When the effect of functional status was considered, the effect of multimorbidity was no longer significant. Functional status itself predicted mortality in unadjusted and adjusted models, and even a very basic self-report of how much health problems interfered with daily lives was very strongly associated with 5-year survival.
We also found that multimorbidity was more common in those with fewer years of formal education. This finding is similar to that of Barnett et al,11 who found a strong and graded association between social position and multimorbidity in patients in Scotland. Schafer et al also found that social position, but not living arrangement or marital status, predicted multi-morbidity.49 They found that the association was particularly strong in men, and for cardiovascular clusters of disease. Further research is needed into the effects of social position, and lifetime risk factors for multi-morbidity. Even late in life, improvements in the economic and social conditions of older populations might be important in preventing multimorbidity; conversely, deteriorations in economic and social conditions might have adverse effects.
We found that the effect of multimorbidity was attenuated by disability. Indeed, the effects of most of the predictor factors were attenuated. This finding is very similar to that of Marengoni et al,50 who found that chronic disability rather than multimorbidity emerged as the strongest negative prognostic factor for functionality and survival in a population-based cohort of older adults in Sweden. Landi et al also found that disability was a stronger predictor of death than multimorbidity in a cohort of older adults.51 A possible explanation for the attenuation of the effect of multimorbidity is that disability and multimorbidity were highly collinear. This might make the interpretation of the regression models difficult. Alternatively, disability might mediate the effect of multimorbidity on mortality. Multimorbidity might cause disability, which in turn predicts death. Indeed, our findings support the notion of disease progression—as we go through life, we might acquire risk factors, then disease states, which accumulate to produce a period of disability before death. Further long-term longitudinal studies are needed to explore the complex relationship between diseases and disability.
Limitations
There are substantial limitations to our study. First, the measure of multimorbidity was rudimentary: we used a simple tally of diseases and complaints. The items were all self-reported and missed potentially important health conditions. There was also no measurement of disease severity or stage, which might predict mortality. We did not weight any particular problem more highly than others (eg, a stroke counted as much as foot troubles) although some diseases and health complaints might be more important than others.52 We also did not attempt to determine if there were interactions between our items. Interactions between diseases might be greater than the effect of each disease state. Finally, we did not include any biomedical measures. Subclinical or unreported clinical conditions might be important predictors of health outcomes.53 However, including disease severity measures, biomedical data, accurate weighting of conditions and disease interactions would all likely strengthen the associations that we observed. The questions we used were simple and nonintrusive, and yet the answers still strongly predicted death. Further, the effect was cumulative, with even minor problems contributing to the overall effect.
Conclusion
When dealing with unwell people and populations, the sum of problems might be more important than any individual problem. Considering complexity, multiple problems, and the cumulative effect of deficits over time is critical to the care of older adults. For clinicians, it is important to consider the cumulative effect of numerous diseases, rather than simply considering diseases in isolation. Incorporating functional status into clinical decisions, such as screening and deciding on the aggressiveness of care, is also critical. For administrators our findings are important, as health policy decisions need to consider the importance of aggregate disease burden and disability in management decisions.54 Of note, many commonly used case-mix adjustments do not consider disability. This could reduce the accuracy of adjustments for outcomes such as quality of care, hospital mortality, and length of stay. For researchers, it is clear that further inquiry is needed into how risk factors and diseases interact over time, and how to prevent multimorbidity and disability.
Acknowledgments
The Manitoba Study of Health and Aging was funded primarily by Manitoba Health, with additional funding provided through the Canadian Study of Health and Aging by the Seniors Independence Research Program of the National Health Research and Development Program of Health Canada. No endorsement from these agencies is implied. The sponsors had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of the article.
EDITOR’S KEY POINTS
This study found that number of self-reported health problems was associated with education, sex, depressive symptoms, and functional status. Multimorbidity was also more common in those with fewer years of formal education, and the effect of multimorbidity was attenuated by disability.
For clinicians, it is important to consider the cumulative effect of numerous diseases, rather than simply considering diseases in isolation. Incorporating consideration of functional status into clinical decisions, such as whether to perform screening and deciding on the aggressiveness of care, is also critical.
Many commonly used case-mix adjustments do not consider disability. This could reduce the accuracy of adjustments for outcomes such as quality of care, hospital mortality, and length of stay. Further inquiry is needed into how risk factors and diseases interact over time, and how multimorbidity and disability can be prevented.
POINTS DE REPÈRE DU RÉDACTEUR
Cette étude a montré que le nombre de problèmes de santé dont se plaint un patient est en rapport avec la scolarité, son sexe, son état fonctionnel et la présence de symptômes dépressifs. On a aussi observé que la multi-morbidité est plus fréquente chez ceux qui ont moins d’années de scolarité et que l’effet de la multi-morbidité est atténué par la présence d’incapacités.
Le clinicien doit tenir compte de l’effet cumulatif résultant de maladies multiples plutôt que de considérer chacune individuellement. Il est également crucial de prendre en compte l’état fonctionnel lors de décisions cliniques, comme lorsqu’on envisage un dépistage ou qu’on décide du degré d’agressivité d’un traitement.
Plusieurs ajustements couramment utilisés pour des cas semblables ne tiennent pas compte des incapacités. Cela risque de réduire la précision des ajustements pour des issues comme la qualité des soins, la mortalité hospitalière et la durée du séjour. D’autres études seront nécessaires pour comprendre comment les facteurs de risque et les maladies interagissent dans le temps, et comment la multi-morbidité et l’incapacité peuvent être prévenues.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
Dr St John gathered the data. All authors contributed to the concept and design of the study; data analysis and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Marengoni A, Rizzuto D, Wang HX, Winblad B, Fratiglioni L. Patterns of chronic multimorbidity in the elderly population. J Am Geriatr Soc. 2009;57(2):225–30. doi: 10.1111/j.1532-5415.2008.02109.x. [DOI] [PubMed] [Google Scholar]
- 2.Schäfer I, von Leitner EC, Schon G, Koller D, Hansen H, Kolonko T, et al. Multimorbidity patterns in the elderly: a new approach of disease clustering identifies complex interrelations between chronic conditions. PLoS ONE. 2010;5(12):e15941. doi: 10.1371/journal.pone.0015941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van den Bussche H, Koller D, Kolonko T, Hansen H, Wegscheider K, Glaeske G, et al. Which chronic diseases and disease combinations are specific to multimorbidity in the elderly? Results of a claims data based cross-sectional study in Germany. BMC Public Health. 2011;11:101. doi: 10.1186/1471-2458-11-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hughes LD, McMurdo ME, Guthrie B. Guidelines for people not for diseases: the challenges of applying UK clinical guidelines to people with multimorbidity. Age Ageing. 2013;42(1):62–9. doi: 10.1093/ageing/afs100. Epub 2012 Aug 21. [DOI] [PubMed] [Google Scholar]
- 5.Britt HC, Harrison CM, Miller GC, Knox SA. Prevalence and patterns of multi-morbidity in Australia. Med J Aust. 2008;189(2):72–7. doi: 10.5694/j.1326-5377.2008.tb01919.x. [DOI] [PubMed] [Google Scholar]
- 6.Fortin M, Hudon C, Haggerty J, Akker M, Almirall J. Prevalence estimates of multimorbidity: a comparative study of two sources. BMC Health Serv Res. 2010;10:111. doi: 10.1186/1472-6963-10-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glynn LG, Valderas JM, Healy P, Burke E, Newell J, Gillespie P, et al. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pract. 2011;28(5):516–23. doi: 10.1093/fampra/cmr013. [DOI] [PubMed] [Google Scholar]
- 8.Salisbury C, Johnson L, Purdy S, Valderas JM, Montgomery AA. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. BMJ. 2011;61(582):e12–21. doi: 10.3399/bjgp11X548929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Oostrom SH, Picavet HS, van Gelder BM, Lemmens LC, Hoeymans N, van Dijk CE, et al. Multimorbidity and comorbidity in the Dutch population— data from general practices. BMC Public Health. 2012;12:715. doi: 10.1186/1471-2458-12-715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marengoni A, Winblad B, Karp A, Fratiglioni L. Prevalence of chronic diseases and multimorbidity among the elderly population in Sweden. Am J Public Health. 2008;98(7):1198–200. doi: 10.2105/AJPH.2007.121137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 12.Fortin M, Stewart M, Poitras ME, Almirall J, Maddocks H. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. 2012;10(2):142–51. doi: 10.1370/afm.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.France EF, Wyke S, Gunn JM, Mair FS, McLean G, Mercer SW. Multimorbidity in primary care: a systematic review of prospective cohort studies. BMJ. 2012;62(597):e297–307. doi: 10.3399/bjgp12X636146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tate RB, Michaels L, Cuddy TE, Bayomi DJ. Clinical diagnoses before age 75 and men’s survival to their 85th birthday: the Manitoba Follow-up Study. Gerontologist. 2013;53(1):133–41. doi: 10.1093/geront/gns050. Epub 2012 Apr 30. [DOI] [PubMed] [Google Scholar]
- 15.Lascaratos J, Poulacou-Rebelacou E. The roots of geriatric medicine: care of the aged in Byzantine times (324–1453 AD) Gerontology. 2000;46(1):2–6. doi: 10.1159/000022125. [DOI] [PubMed] [Google Scholar]
- 16.Lapin A. Why should Byzantium be considered as a cradle of clinical geriatrics? [article in German] Wien Med Wochenschr. 2008;158(17–18):471–80. doi: 10.1007/s10354-008-0578-z. [DOI] [PubMed] [Google Scholar]
- 17.Sheldon JH. The social medicine of old age. Oxford, UK: Oxford University Press; 1948. [Google Scholar]
- 18.Fortin M, Lapointe L, Hudon C, Vanasse A. Multimorbidity is common to family practice. Is it commonly researched? Can Fam Physician. 2005;51:244–5. Available from: www.cfp.ca/content/51/2/244.long. Accessed 2014 Apr 3. [PMC free article] [PubMed] [Google Scholar]
- 19.Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009;7(4):357–63. doi: 10.1370/afm.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diederichs C, Berger K, Bartels DB. The measurement of multiple chronic diseases—a systematic review on existing multimorbidity indices. J Gerontol A Biol Sci Med Sci. 2011;66(3):301–11. doi: 10.1093/gerona/glq208. [DOI] [PubMed] [Google Scholar]
- 21.Huntley AL, Johnson R, Purdy S, Valderas JM, Salisbury C. Measures of multimorbidity and morbidity burden for use in primary care and community settings: a systematic review and guide. Ann Fam Med. 2012;10(2):134–41. doi: 10.1370/afm.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hudon C, Fortin M, Vanasse A. Cumulative Illness Rating Scale was a reliable and valid index in a family practice context. J Clin Epidemiol. 2005;58(6):603–8. doi: 10.1016/j.jclinepi.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 23.Salvi F, Miller MD, Grilli A, Giorgi R, Towers AL, Morichi V, et al. A manual of guidelines to score the modified cumulative illness rating scale and its validation in acute hospitalized elderly patients. J Am Geriatr Soc. 2008;56(10):1926–31. doi: 10.1111/j.1532-5415.2008.01935.x. [DOI] [PubMed] [Google Scholar]
- 24.Tooth L, Hockey R, Byles J, Dobson A. Weighted multimorbidity indexes predicted mortality, health service use, and health-related quality of life in older women. J Clin Epidemiol. 2008;61(2):151–9. doi: 10.1016/j.jclinepi.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 25.Brilleman SL, Salisbury C. Comparing measures of multimorbidity to predict outcomes in primary care: a cross sectional study. Fam Pract. 2013;30(2):172–8. doi: 10.1093/fampra/cms060. Epub 2012 Oct 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perkins AJ, Kroenke K, Unutzer J, Katon W, Williams JW, Jr, Hope C, et al. Common comorbidity scales were similar in their ability to predict health care costs and mortality. J Clin Epidemiol. 2004;57(10):1040–8. doi: 10.1016/j.jclinepi.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Fortin M, Hudon C, Dubois MF, Almirall J, Lapointe L, Soubhi H. Comparative assessment of three different indices of multimorbidity for studies on health-related quality of life. Health Qual Life Outcomes. 2005;3:74. doi: 10.1186/1477-7525-3-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fortin M, Bravo G, Hudon C, Lapointe L, Almirall J, Dubois MF, et al. Relationship between multimorbidity and health-related quality of life of patients in primary care. Qual Life Res. 2006;15(1):83–91. doi: 10.1007/s11136-005-8661-z. [DOI] [PubMed] [Google Scholar]
- 29.Fortin M, Bravo G, Hudon C, Lapointe L, Dubois MF, Almirall J. Psychological distress and multimorbidity in primary care. Ann Fam Med. 2006;4(5):417–22. doi: 10.1370/afm.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gunn JM, Ayton DR, Densley K, Pallant JF, Chondros P, Herrman HE, et al. The association between chronic illness, multimorbidity and depressive symptoms in an Australian primary care cohort. Soc Psychiatry Psychiatr Epidemiol. 2012;47(2):175–84. doi: 10.1007/s00127-010-0330-z. [DOI] [PubMed] [Google Scholar]
- 31.Kadam UT, Croft PR. Clinical multimorbidity and physical function in older adults: a record and health status linkage study in general practice. Fam Pract. 2007;24(5):412–9. doi: 10.1093/fampra/cmm049. [DOI] [PubMed] [Google Scholar]
- 32.Aarts S, den Akker M, Bosma H, Tan F, Verhey F, Metsemakers J, et al. The effect of multimorbidity on health related functioning: temporary or persistent? Results from a longitudinal cohort study. J Psychosom Res. 2012;73(3):211–7. doi: 10.1016/j.jpsychores.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 33.Gross CP, Guo Z, McAvay GJ, Allore HG, Young M, Tinetti ME. Multimorbidity and survival in older persons with colorectal cancer. J Am Geriatr Soc. 2006;54(12):1898–904. doi: 10.1111/j.1532-5415.2006.00973.x. [DOI] [PubMed] [Google Scholar]
- 34.Glynn LG, Buckley B, Reddan D, Newell J, Hinde J, Dinneen SF, et al. Multimorbidity and risk among patients with established cardiovascular disease: a cohort study. BMJ. 2008;58(552):488–94. doi: 10.3399/bjgp08X319459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stuck AE, Walthert JM, Nikolaus T, Büla CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48(4):445–69. doi: 10.1016/s0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- 36.Fried LP, Guralnik JM. Disability in older adults: evidence regarding significance, etiology, and risk. J Am Geriatr Soc. 1997;45(1):92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- 37.Noyes K, Liu H, Temkin-Greener H. Medicare capitation model, functional status, and multiple comorbidities: model accuracy. Am J Manag Care. 2008;14(10):679–90. [PMC free article] [PubMed] [Google Scholar]
- 38.Boyd CM, Boult C, Shadmi E, Leff B, Brager R, Dunbar L, et al. Guided care for multimorbid older adults. Gerontologist. 2007;47(5):697–704. doi: 10.1093/geront/47.5.697. [DOI] [PubMed] [Google Scholar]
- 39.Noël PH, Parchman ML, Williams JW, Jr, Cornell JE, Shuko L, Zeber JE, et al. The challenges of multimorbidity from the patient perspective. J Gen Intern Med. 2007;22(Suppl 3):419–24. doi: 10.1007/s11606-007-0308-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salisbury C, Sampson F, Ridd M, Montgomery AA. How should continuity of care in primary health care be assessed? BMJ. 2009;59(561):e134–41. doi: 10.3399/bjgp09X420257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity Guiding principles for the care of older adults with multimorbidity: an approach for clinicians. J Am Geriatr Soc. 2012;60(10):E1–25. doi: 10.1111/j.1532-5415.2012.04188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity Patient-centered care for older adults with multiple chronic conditions: a stepwise approach from the American Geriatrics Society. J Am Geriatr Soc. 2012;60(10):1957–68. doi: 10.1111/j.1532-5415.2012.04187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition—multimorbidity. JAMA. 2012;307(23):2493–4. doi: 10.1001/jama.2012.5265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith SM, Soubhi H, Fortin M, Hudon C, O’Dowd T. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2012;(4):CD006560. doi: 10.1002/14651858.CD006560.pub2. [DOI] [PubMed] [Google Scholar]
- 45.Smith SM, Soubhi H, Fortin M, Hudon C, O’Dowd T. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ. 2012;345:e5205. doi: 10.1136/bmj.e5205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.St John PD, Montgomery PR. Do depressive symptoms predict mortality in older people? Aging Ment Health. 2009;13(5):674–81. doi: 10.1080/13607860902774493. [DOI] [PubMed] [Google Scholar]
- 47.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48(8):314–8. [PubMed] [Google Scholar]
- 48.Fillenbaum GG. Multidimensional functional assessment of older adults: the Duke Older Americans Resources And Services Procedures. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- 49.Schäfer I, Hansen H, Schon G, Hofels S, Altiner A, Dahlhaus A, et al. The influence of age, gender and socio-economic status on multimorbidity patterns in primary care. First results from the Multicare Cohort Study. BMC Health Serv Res. 2012;12:89. doi: 10.1186/1472-6963-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marengoni A, von Strauss E, Rizzuto D, Winblad B, Fratiglioni L. The impact of chronic multimorbidity and disability on functional decline and survival in elderly persons. A community-based, longitudinal study. J Intern Med. 2009;265(2):288–95. doi: 10.1111/j.1365-2796.2008.02017.x. [DOI] [PubMed] [Google Scholar]
- 51.Landi F, Liperoti R, Russo A, Capoluongo E, Barillaro C, Pahor M, et al. Disability, more than multimorbidity, was predictive of mortality among older persons aged 80 years and older. J Clin Epidemiol. 2010;63(7):752–9. doi: 10.1016/j.jclinepi.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 52.Diederichs CP, Wellmann J, Bartels DB, Ellert U, Hoffmann W, Berger K. How to weight chronic diseases in multimorbidity indices? Development of a new method on the basis of individual data from five population-based studies. J Clin Epidemiol. 2012;65(6):679–85. doi: 10.1016/j.jclinepi.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 53.Fried LP, Kronmal RA, Newman AB, Bild DE, Mittelmark MB, Polak JF, et al. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA. 1998;279(8):585–92. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 54.Lee SJ, Go AS, Lindquist K, Bertenthal D, Covinsky KE. Chronic conditions and mortality among the oldest old. Am J Public Health. 2008;98(7):1209–14. doi: 10.2105/AJPH.2007.130955. [DOI] [PMC free article] [PubMed] [Google Scholar]