Abstract
Family-centered preventive interventions have been proposed as relevant to mitigating psychological health risk and promoting resilience in military families facing wartime deployment and reintegration. This study evaluates the impact of a family-centered prevention program, Families OverComing Under Stress Family Resilience Training (FOCUS), on the psychological adjustment of military children. Two primary goals include: 1) Understanding the relationships of distress among family members using a longitudinal path model to assess relations at the child and family level, and 2) Determining pathways of program impact on child adjustment. Multilevel data analysis using structural equation modeling was conducted with de-identified service delivery data from 280 families (505 children ages 3-17) in two follow-up assessments. Standardized measures included Service Member and Civilian parental distress (Brief Symptom Inventory, PTSD Checklist – Military), child adjustment (Strengths and Difficulties Questionnaire), and family functioning (McMaster Family Assessment Device). Distress was significantly related among the service member parent, civilian parent and children. FOCUS improved family functioning, which in turn significantly reduced child distress at follow-up. Salient components of improved family functioning in reducing child distress mirrored resilience processes targeted by FOCUS. These findings underscore the public health potential of family-centered prevention for military families, and suggest areas for future research.
INTRODUCTION
A decade of war has underscored the challenges and sacrifices imposed upon children by a parent's military service. By the fall of 2010 more than 2.1 million service members, almost half of them parents, had deployed to support Operation Enduring Freedom and Operation Iraqi Freedom. Of these, about 48% had deployed at least twice, with many serving multiple times. For many military children in the last decade, an entire childhood has been defined by at least one parent leaving and returning in the context of dangerous duties. A growing research literature has documented heightened risk for psychological health problems among service members, spouses and children associated with these challenges. 1-6 Increasingly, military, veteran and national leadership have recognized the urgent need to support military families both to maintain readiness and mitigate the impact of deployment stress.7 Adapting, implementing and evaluating preventive programs for military families have emerged as an important public health need.8 This study utilizes a multilevel path analysis to evaluate the impact of a family-centered preventive service program designed to promote family resilience on military child emotional and behavioral outcomes, and to provide an initial test of targeted family resilience mechanisms as pathways of psychological health promotion for military children.
Research on the impact of wartime deployments on military families indicates the reverberations of stress across family members and the family system.5,9-10 The critical role of individual and family resilience in managing deployment challenges have been identified within scientific, clinical and policy communities. 8, 11 In particular, strategies that draw upon current models of resilience have underscored the importance of family-level processes and relationships to the reduction of distress in children.12-13 Development and implementation of effective family prevention programs will be enhanced by identifying and testing the specific impact of resilience-enhancing interventions on family processes, and examining the impact of enhanced family functioning on child adjustment.12, 14-15
Decades of child development and prevention science provide strong evidence for the benefits of family-centered interventions in supporting positive parent and child psychological health, and suggest promise for military and veteran families.16-18 Convergent research has consistently identified key factors that contribute to child resilience in the context of adversity, including parent psychological health, parent-child relationships, parenting/co-parenting and environmental support.14-15,19-20 Family-level characteristics and interactions have been identified as potential mediators of children's ability to adapt and thrive following exposure to stress.4-5,9 Initial studies support these factors as relevant for military children negotiating deployment stress.4,9,18-22
These findings suggest the potential benefit of interventions that are consistent with current models of psychological resilience, and designed to enhance family functioning and relationships for reducing distress in children.12-13 In particular, interventions that target family functioning theorized to support family resilience processes such as effective communication, emotional awareness and regulation, collaborative problem solving, and development of shared meaning about stressful experiences hold promise for supporting military families affected by stress.12,23 While multiple studies have documented the salience of these family processes to adaptive responses to stress, trauma and loss,24 most have been cross-sectional or qualitative in design, or have not been conducted with military populations. Evaluation of a family-centered prevention program implemented at scale with military families offers the opportunity to examine whether changes in child psychological health symptoms are significantly mediated by improvements in resilient family processes.
Since 2008, the U.S. Navy Bureau of Medicine and Surgery contracted with a team from UCLA and Harvard to implement the family-centered prevention program Families OverComing Under Stress Family Resiliency Training (FOCUS) and a suite of related services at active duty military installations known as the FOCUS Project.16 Adapted from the team's established evidence-based family-centered preventive interventions shown to improve psychological health and family functioning over longitudinal follow-up in other settings,16,25 FOCUS was customized for military families affected by deployment and reintegration challenges in partnership with military providers and community members.12,16,18 During its first 20 months of operation, this tiered public health implementation provided a “suite” of integrated prevention services based on core evidence-based practices. FOCUS delivered family resiliency training for individual families, as well as parent and child resilience skills building groups, to over 5,000 military children, spouses, and service members. The FOCUS Project also provided family-centered consultations, briefings, and educational workshops to over 100,000 family members, providers and other community members .16 All of these services were designed to enhance specific family processes theorized to support resilience in the context of stress. The FOCUS program evaluated in this report includes individual family assessment, education and skill enhancement, as well as the construction of individual and family narrative timelines, an activity designed to develop increased understanding within the family regarding their experiences.12, 18
Prior evaluation of the FOCUS program delivery from the initial implementation period showed significant reductions in service member, spouse and child distress and concurrent improvements in family functioning.26 While these initial findings indicated positive impact, an important next step was to identify whether reductions in child distress were mediated by theorized improvements in family functioning, and if one or more of the resilient family functioning processes would be more central to distress reduction than others.27 This information would help inform preventive programs for military families, as well as contribute to our understanding of transmission of deployment and reintegration stress among family members.
Previous research has identified the sources of family stress as “direct,” for example, the worry attendant to having a loved one at risk, the reductions in available emotional and financial resources across the family,4,28 or “indirect” when stress burdens are due to interactions with a family member who is highly distressed, symptomatic or engaging in uncharacteristic or stress-inducing behaviors.29-30 Such is the case with the studies of military families from the Vietnam War era forward that have documented the impact of parental PTSD on spouses and children.31 Current research examining the family impact of deployment stressors suggest that most are mediated by parent and family factors and may be considered primarily indirect or “secondary.” 9,30 Signs of distress among children are also significantly linked to levels of distress among parents, both caretaker and service member.1,5,32 A primary shortcoming of current literature, however, is that most studies focus on the individual prevalence of psychological disorders among service members, spouses and children with limited information on the concordance of difficulties among family members.6,33 Even studies that explicitly look at the relationship of distress levels between parents and children generally do not capture the systemic view of distress concordance across the family system.21
The first goal of the current study was to develop a systemic understanding of the relationships of distress among active duty families facing deployment stress that attended the FOCUS program. To do this, we utilized a multilevel path model that describes the relationships between levels of distress measured at program entry among service member parents, civilian parents, and children. We anticipated significant correlations among service member distress (anxiety and depression), service member post traumatic stress symptoms, civilian spouse adjustment, child adjustment and family functioning.
The second goal of the study was to evaluate the pathways of program impact on child psychological health symptoms utilizing longitudinal assessment data following program participation. Consistent with the underlying theoretical model of family resilience, we hypothesized that improvement in family functioning would mediate improvements in child psychological health outcomes. In addition, we anticipated that the specific family functioning processes that are associated with resilience and targeted by FOCUS (e.g., emotional awareness and regulation, problem solving and communication in families) might account for greater variance in child outcomes.
METHODS
Participants
Data are from a secondary analysis of de-identified data originally collected (July 2008 to February 2010) for the purpose of customized delivery and program quality improvement of the family centered preventive intervention for military families. Participating families included families with at least one active duty military parent, and at least one dependent child age 3 and older. Data presented here are from 11 US Marine Corps and US Navy installations located in California (4 sites), North Carolina, Hawaii, Okinawa (Japan), Virginia (2 sites), Mississippi, and Washington State. The final sample for this analysis consists of 280 families with at least one service member parent and one or more children (505 children, 44% female child, average child age, 7.5 years, range 3 to 17 years). Of this sample, 35.4% participated at US Navy installations and 65.6% at US Marine Corps installations. Both the military and civilian/caretaker self report parent provided data for this analysis; primary caretaker (280 civilian parents) child report data was used for child outcomes. This study of program evaluation data was approved by the UCLA Institutional Review Board.
Procedures
The manualized prevention program, FOCUS Family Resilience Training, is delivered to individual families including the service member and civilian/caretaker parent, and children ages 3-18. Delivered in eight modularized sessions, FOCUS includes parent-only, child-only and family sessions. The program provides family level education about (1) Stress reactions, including helping the family to identify reminders that trigger unhelpful responses, and linking specific stress reactions to breakdowns in family cohesion, communication, routines, and parenting activities; (2) Family communication, such as similarities and differences among family members’ understanding of and reactions to deployment and reintegration experiences; (3) Identifying and utilizing family strengths; and (4) Guidance about child development and common stress reactions. FOCUS also trains parents and children in family level cognitive behavioral skills designed to promote resilience, including emotional regulation, goal setting, problem solving, trauma/separation/ loss stress reminder management, and communication.26, 34 FOCUS providers, identified as “resiliency trainers,” are master- or doctoral-level child and family mental health providers that complete in-person and web-based training. UCLA provides weekly model supervision, reviews fidelity measures and delivery notes, conducts site visits, and provides emergency support and technical assistance. Centralized management ensures program standardization and quality improvement processes.
Measures
The program utilizes a web-based family assessment at time of entry, completion, 1 month and 4-6 months post completion. The full assessment protocol includes standardized psychological health, family functioning and coping measures completed by children and parents in order to identify areas of strength and challenge, make timely referrals and conduct quality control.26 Assessment measures utilized in this study are described in detail below. Except for single-item demographics and the number of visits, all variables were constructed as latent variables.
Baseline variables included the demographics of child age (in years), and child gender (coded as 1 = male, 2 = female). Parental distress was reported for each parent (military and civilian/caretaker). Distress was assessed with three scales from the Brief Symptom Inventory (BSI), 35 a self-report inventory with extensively published psychometric data and community norms by gender. The somatic complaints, depression, and anxiety subscales were used as indicators of parental distress. Another indicator of deployment related distress, the PTSD Checklist-Military (PCL-M), a 17-item self-report measure, assessed the severity of PTSD symptoms in the past month for the military parent.36
Child initial distress was assessed using the Strengths and Difficulties Questionnaire parent report (SDQ),37 a widely used instrument with subscales for conduct problems, emotional symptoms, hyperactivity/inattention, peer relationship problems, and pro-social behavior. (Pro-social behavior was reverse-scored in these analyses). Normative data are available for each gender and for ages 3-18. The subscales were used as indicators of a latent variable representing child distress (coefficient alpha = .66).
Longitudinal assessment variables consisted of: 1) the number of session visits attended by the families during the intervention delivery period (adjusted for family size as families with more children require more visits to complete program sessions including boosters when appropriate); 2) a latent variable representing positive change in family adjustment from enrollment to intervention exit on the McMaster Family Assessment Device (FAD) completed by caretakers.38 The FAD was used to assess overall family functioning, and specific family processes (problem solving, communication, affective responsiveness, affective involvement, behavior control, and roles) and was administered at program entry and exit. Scores at entry were subtracted from scores at exit to derive scores reflecting improvement in family adjustment and were used as indicators of a latent variable representing Positive Change in FAD (coefficient alpha = .82). 3) A second latent variable representing reduced emotional distress among participating children in longitudinal follow up after program completion. This variable was the difference between the emotional and behavioral distress (SDQ) assessed at baseline and then again at 4 to 6 month follow up as reported by the caretaker parent. There was substantial interest in determining whether changes in the family functioning processes associated with family resilience and targeted by the program (problem solving, communication, affective responsiveness, affective involvement) would be the most efficacious in predicting reduction in child distress. The individual components of the FAD were tested individually in a secondary analysis as predictors of change in the SDQ to determine their relative contributions.
Data Analyses
The EQS structural equations program39 estimated a two-level model using a maximum likelihood (ML) approach.39-41 We used a multilevel model because observations among members of the same family are not independent and thus violate assumptions about independent samples. We initially determined that a multilevel model was appropriate by assessing the intraclass correlations among the indicator variables. 42 For instance, child distress intraclass correlations ranged from .14 to .23, intraclass correlations among difference scores on child distress ranged from .12 to .22. Thus, children's distress levels were more alike within their families than across families. In this study, the family level portion of the multilevel model was of most interest in assessing the impact of FOCUS because the program was implemented at the family level and because all children within a family had the same scores for items assessed among their parents including the parent distress scores, the military parent PCL, number of visits, and change in family adjustment (caretaker reported FAD). Of course, impact of gender of the child could only be assessed at the child level of the analysis as this was not a family-level variable.
Goodness-of-fit of the models was evaluated with the Bentler-Liang Likelihood Ratio Statistic (BLLRS), the Comparative Fit Index (CFI), and the standardized root mean square residual (SRMR).39,43 The CFI, which ranges from 0 to 1, reports the improvement in fit of the hypothesized model over a model of complete independence among the measured variables. Values equal or greater than .95 are desirable and indicate that 95% of the covariation in the data is reproduced by the hypothesized model. The SRMR is a measure representing the size of residuals. Values less than .08 are desirable and indicate a close fitting model.43
An initial confirmatory factor analysis (CFA) tested the factor structure of the hypothesized model and also provided correlations among all of the factors without regard to the multilevel nature of the data set. Significant correlated error residuals were allowed between similar items (e.g., distress of military parent, distress of civilian parent) to improve model fit and account for significant associations. Once the factor structure was confirmed, a similar multilevel CFA was conducted to determine correlations and factor loadings at the family level. Then, the hypothesized multilevel path model was tested in which the individual level baseline variables of child age and gender, and child initial distress were used to predict reduced child distress. At the family level, child age, military parent distress, civilian/caretaker parent distress, child initial distress, and military parent PCL were used as predictors of positive change in FAD, and the number of visits. Number of visits attended also was anticipated to predict Positive Change in FAD. In turn, Positive Change in FAD was hypothesized to predict Reduced Child Distress. Number of visits was also used initially as a direct predictor of reduced child distress. Baseline predictor variables were allowed to correlate among themselves. Nonsignificant paths and covariances were dropped gradually using the suggested model-evaluation procedure of MacCallum. 44
RESULTS
Confirmatory Factor Analyses
The preliminary CFA before the multilevel analysis indicated a well-fitting model (ML χ2 (N = 505) = 495.75, 253 df; CFI = .95, SRMR = .049). All factor loadings were statistically significant (p ≤ .001). Table 1 presents the factor loadings, means, and standard deviations of the measured variables for the entire group as well as factor loadings in the multilevel CFA (family level). Of note, means of parent distress (BSI) and child distress (SDQ) were generally higher than those in the general population.35, 37 Table 2 reports the correlations among the latent variables and the single-item variables for both the preliminary CFA model and the multilevel CFA model. The 2-stage multilevel CFA had an excellent fit: BLLRS χ2 = 502.75, 309 df; CFI = 1.00, SRMR = .038. Of note in Table 2, distress among the military parent, caretaker parent, and their children was highly inter-correlated. Associations among the distress variables were higher at the family level than in the individual level. This result is particularly notable in the association between caretaker parent distress and child initial distress (.59 at the family level, .35 at the individual level that does not account for dependencies within the family). Positive changes in the FAD were associated with reductions in child distress and with the number of FOCUS program visits, although relationships were stronger at the family level. Baseline distress of the caretaker parent and distress of the child were associated with more positive change in FAD at the family level. This is partly due to lower scores at baseline in the FAD for the more distressed individuals and thus, larger possible changes over time. A similar relationship held for the child's initial distress and greater reduction in stress at follow-up. They were higher at baseline and thus, had more opportunity for improvement at follow-up in their change scores.
Table 1.
Summary statistics and factor loadings in the individual CFA model and in the family level CFA model.
| Variable | Mean (S. D.) | Factor Loading* |
|---|---|---|
| (%) | Individual/ Family Level | |
| Baseline | ||
| Child Age (years) (range = 3 to 17) | 7.44 (3.54) | NA** |
| Child Gender (% female) | (44%) | NA |
| Military Parent Distress | ||
| BSI Somatic (0 to 18) | 1.43 (2.93) | .80/.77 |
| BSI Depression (0 to 20) | 2.99 (3.99) | .77/.80 |
| BSI Anxiety (0 to 20) | 3.17 (3.78) | .85/.84 |
| Civilian Parent Distress | ||
| BSI Somatic (0 to 18) | 1.96 (3.11) | .76/.77 |
| BSI Depression (0 to 19) | 3.82 (4.01) | .71/.69 |
| BSI Anxiety (0 to 17) | 3.71 (3.70) | .89/.87 |
| Child Initial Distress (1 to 10) | ||
| Conduct problems | 2.72 (2.25) | .73/.90 |
| Emotional symptoms | 3.20 (2.49) | .36/.92 |
| Hyperactivity/inattention | 4.52 (2.79) | .64/.89 |
| Peer relationship problems | 2.17 (2.00) | .43/.92 |
| Prosocial behavior (reversed) | 2.24 (2.10) | .51/.46 |
| Military parent PCL (17 to 82) | 25.17 (11.13) | NA |
| Four month follow-up | ||
| Positive Change in FAD (Posttest-pretest difference) | ||
| Problem solving (−0.67 to 1.67) | 0.21 (0.42) | .65/.67 |
| Communication (−.89 to 1.44) | 0.14 (0.39) | .73/.73 |
| Affective responsiveness (−1.17 to 1.5) | 0.16 (0.46) | .64/.76 |
| Affective involvement (−0.86 to 1.57) | 0.11 (0.43) | .54/.55 |
| Behavior control (−1.22 o 1.44) | 0.14 (0.37) | .52/.55 |
| Roles (−0.82 to 1.09) | 0.17 (0.35) | .71/.68 |
| Number of visits (1-33) | 15.45 (4.69) | NA |
| Reduced Child Distress (Pretest-posttest difference) | ||
| Conduct problems (−6 to 7) | 1.07 (2.02) | .67/.88 |
| Emotional symptoms (−6 to 10) | 1.11 (2.34) | .42/.84 |
| Hyperactivity/inattention (−6 to 9) | 0.85 (2.27) | .44/.78 |
| Peer relationship problems (−5 to 8) | 0.73 (1.82) | .42/.80 |
| Prosocial behavior (reversed) (−5 to 7) | 0.80 (1.87) | .46/.49 |
All factor loadings significant, p ≤ .001.
NA = Not applicable
Table 2.
Correlations among single-items and latent variables. Family level correlations below diagonal; individual correlations above diagonal.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Child age | - | .01 | .02 | −.03 | −.08 | .02 | −.01 | .09* | −.05 |
| 2. Child female | NA | - | −.06 | −.07 | −.17** | −.04 | −.01 | .02 | −.08 |
| 3. Military Parent Distress | .06 | NA | - | .28** | .24** | .78** | .14** | .17** | .12* |
| 4. Caretaker Parent Distress | −.05 | NA | .33** | - | .35** | .18** | .23** | .14** | .12* |
| 5. Child Initial Distress | .16 | NA | .31** | .59** | - | .19** | .12* | .08 | 53** |
| 6. Military PCL | .05 | NA | .74** | .22** | .20* | - | .10* | .14** | .15** |
| 7. Positive change in FAD | .06 | NA | .12 | .25** | .27** | .08 | - | .17** | .21** |
| 8. Number of visits | .20* | NA | .19** | .13* | .07 | .14* | .17** | - | .09 |
| 9. Reduced Child Distress | .22 | NA | .15 | .21* | .46** | .20* | .31** | .06 | - |
p < .05
p < .01
p < .001
NA = child gender not applicable in family level analysis.
Path Model
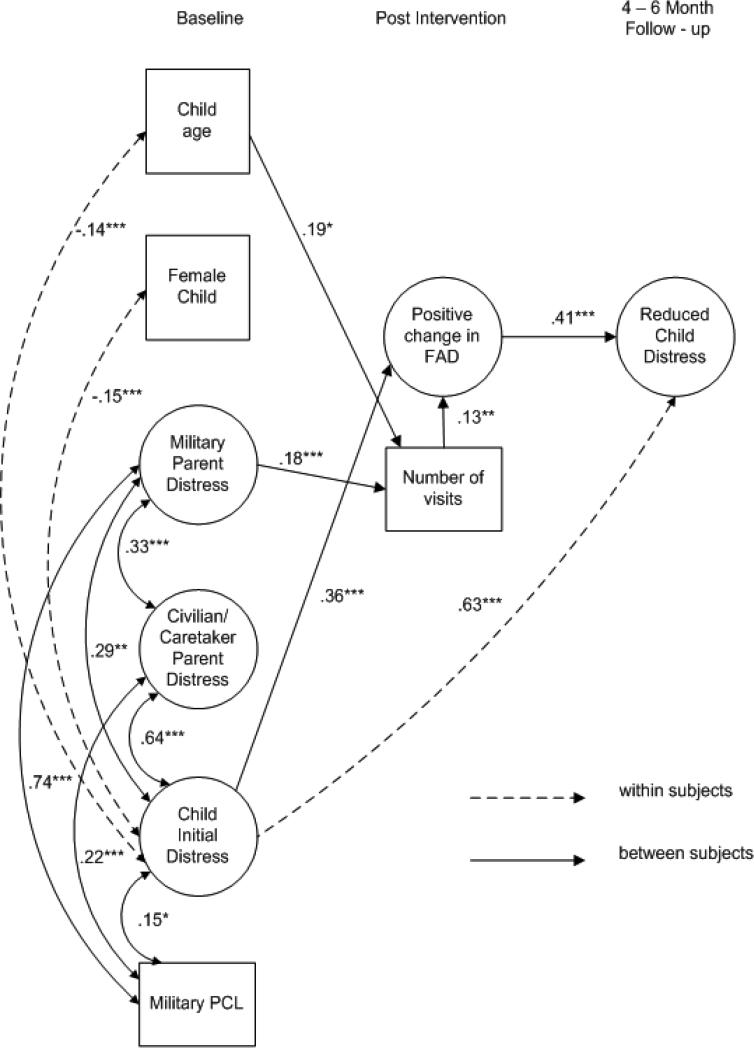
The final trimmed path model is depicted in Figure 1. Fit indexes were excellent: BLLRS χ2 = 522.50, 337 df; CFI = 1.00, SRMR = .041. Significant individual-level correlations and regression paths are depicted with dotted lines such as those associated with gender which can only be an individual variable; family-level correlations and regression paths are depicted with solid lines. At the individual level, younger children and boys were more likely than older children or girls to have distress. At the family level, greater distress in the military parent predicted increased number of visits attended in the intervention. The number of visits attended predicted more positive change in FAD. Children with more initial distress were associated with more positive change in FAD, indicating that parents who reported stress in their children were more likely to also demonstrate improvement over time in their family functioning. Of most importance, a positive change in FAD was associated with reduced child distress, a key goal of the intervention. This portion of the model explained 17% of the variance in Reduced Child Distress. In addition, although number of session visits did not directly predict reduced child distress, it did have a significant indirect effect on reduced child distress, mediated through a positive change in FAD (p ≤ .001).
Figure 1.
Path model for FOCUS families (N = 280 families; 505 children). Latent constructs are in circles, single items are in rectangles; 1-headed arrows depict standardized regression paths, 2-headed arrows represent correlations (standardized covariances). Dotted lines represent significant within subjects associations, solid lines represent family-level associations (* = p ≤ .05, ** = p ≤ .01,*** = p < .001.)
The individual components of the FAD were also assessed separately to find out which aspects were most influential in predicting change in child distress. The most influential subscale was affective involvement, which had a regression coefficient of .34 and explained 11% of the variance in reduced child distress. Problem solving had a regression coefficient of .31 and communication had a regression coefficient of .30. Each explained 9% of the variance in reduced child distress. Roles had a coefficient of .27 and explained 7% of the variance; affective responsiveness had a coefficient of .17 and explained 3% of the variance. Behavior control was minimal in explained reduction in child distress (regression coefficient = .05, 0% explained).
DISCUSSION
Wartime military operations impact entire families, not just individual service members.45 As a military and national public health priority, the overall wellness of military families is critical to promoting psychological resilience and mitigating deployment stress risk for all family members, including the service member. Recognizing these priorities, policy directives and increased resources across the Department of Defense and Veteran's Administration have focused on the development and dissemination of prevention and treatment approaches that support military and veteran families along a continuum of care.13,17,46-48 Increased understanding of the nuanced ways that deployment and reintegration stress is transmitted across family members will assist providers in refining prevention programs designed to promote psychological health in service members and their families.
As anticipated, we found that psychological stress in military families reverberates throughout the family. For families participating in the FOCUS program, distress among the service member parent, civilian/caretaking parent and children were all significantly related at program entry. This was also evidenced by the high intraclass correlations within families, which necessitated a multilevel approach to this study. Relative to community norms, children entering the intervention had elevated levels of emotional and behavioral symptoms, and their parents had greater anxiety and depression symptoms on standardized measures.35,37 As expected, children were more likely to be highly distressed when their caretaker parents were distressed. Notably, there were similar and significant relationships between service members’ distress and that of their family members, whether spouse or child. These data underscore the relevance of addressing psychological distress across family systems. Simply treating one member of military families, often the service member, for psychological distress and related mental health problems is likely not optimal. 8-9
Consistent with earlier findings, this longitudinal evaluation provides further support that the FOCUS program reduces distress in military children26 and provides expanded evidence that allows us to investigate how enhancing family functioning can strengthen military families; in this case through the positive adjustment of children. Both FOCUS and its foundational interventions16 were designed both to strengthen families through theoretically grounded family resilience constructs, as well as to mitigate parental and child distress. This evaluation was undertaken to identify which intervention or family factors are the most salient in reducing military children's distress over time. We found improved family adjustment predicted reduced distress among military children (r = .41, 17% of variance explained), supporting the relevance of family resilience processes as intervention targets. Notably the aspects of family functioning associated with hypothesized family resilience processes seemed to be more salient than others in reducing military children's distress, providing initial confirmatory support for the specific family-level targets of this program.12
Other factors also predicted reductions in military children's distress. Intervention dosage was associated with reductions in distress. Greater program attendance predicted improved family functioning, with the association of intervention dosage with child outcomes mediated through improved family functioning. Interestingly, more distress on the part of the service member parent predicted more attendance for the family as a whole. Perhaps more distressed service member parents or their spouses had greater motivation to develop the resilience skills that this program provides.
We acknowledge the limitations of this study. There is the possibility of response bias in the reporting of military children's distress because the child scores are based upon the caretaker parent's report. In addition, improvements in child adjustment may be attributable in part to maturational change; however, the follow-up period was only six months and the children's distress was not likely to change solely due to maturity within this short time period. Further, this study is an evaluation of a service program, rather than a controlled study design. Future evaluations would benefit from an intervention control group. Although we recognize these limitations, we feel they are balanced by the importance, timeliness, and uniqueness of the sample and the longitudinal design that uses meaningful change scores within a multilevel context.
Study Implications
Our findings indicate that deployment related stress reverberates through the entire family relational system, and is not limited to service members deploying to war. Notably, these evaluation findings are among the first to show that a family-centered prevention program designed to improve resilience processes can lead to improved longitudinal psychological health outcomes for military children affected by parental deployment. Given the urgent need for enhancing the continuum of effective preventive psychological health services for military and veteran families, these evaluation findings provide initial guidance to understanding the public health potential for family-centered prevention strategies, and suggest important areas for future research.
REFERENCES
- 1.Chandra A, Lara-Cinisomo S, Jaycox LH, Tanielian T, Han B, Burns RM, Ruder T. Views from the Homefront: The experience of children from military families. RAND Center for Military Health Policy Research; Santa Monica, CA: 2011. [Google Scholar]
- 2.Gorman LA, Blow AJ, Ames BD, Reed PL. National Guard families after combat: Mental health, use of mental health services, and perceived treatment barriers. Psychiatr Serv. 2011;62(1):28–34. doi: 10.1176/ps.62.1.pss6201_0028. [DOI] [PubMed] [Google Scholar]
- 3.Mansfield AJ, Kaufman JS, Engel CC, Gaynes BN. Deployment and mental health diagnoses among children of US army personnel. Arch Pediatr Adolesc Med. 2011;165(11):999–1005. doi: 10.1001/archpediatrics.2011.123. [DOI] [PubMed] [Google Scholar]
- 4.Chandra A, Lara-Cinisomo S, Jaycox LH, Tanielian T, Burns RM, Ruder T, Han B. Children on the Homefront: The Experience of Children from Military Families. Pediatrics. 2010;125(1):16–25. doi: 10.1542/peds.2009-1180. [DOI] [PubMed] [Google Scholar]
- 5.Lester P, Peterson K, Reeves J, Knauss L, Glover D, Mogil C, Duan N, Saltzman W, Pynoos R, Wilt K, Beardslee W. The long war and parental combat deployment: effects on military children and at-home spouses. J Am Acad Child Adolesc Psychiatry. 2010;49(4):310–320. [PMC free article] [PubMed] [Google Scholar]
- 6.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13 – 22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 7.Weinick RM, Beckjord EB, Farmer CM, Martin LT, Gillen EM, Acosta JD, Helmus TC. Programs addressing psychological health and traumatic brain injury among US military service members and their families. RAND Corp., Center for Military Health Policy Research; Santa Monica, CA.: 2011. [Google Scholar]
- 8.MacDermid-Wadsworth S, Lester P, Marini C, Cozza S, Sornborger J, Strouse T, Beardslee W. Approaching Family-Focused Systems of Care for Military and Veteran Families. Military Behavioral Health. 2013;1:1–10. Doi: 10.1080/21635781.2012.721062. [Google Scholar]
- 9.Gerwirtz AH, Polusny MA, DeGarmo DS, Khaylis A, Erbes CR. Post-traumatic stress symptoms among National Guard soldiers deployed to Iraq: Associations with parenting behaviors and couple adjustment. J Consult Clin Psychol. 2010;78:599 – 610. doi: 10.1037/a0020571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cozza SJ, Chun RS, Polo JA. Military families and children during Operation Iraqi Freedom. Psychiatr Q. 2005;76(4):371 – 378. doi: 10.1007/s11126-005-4973-y. [DOI] [PubMed] [Google Scholar]
- 11.Defense Centers of Excellence (DCoE) for Psychological Health and Traumatic Brain Injury [October 15, 2012];Resilience and Preventive Directorate. 2010 Available at http://www.dcoe.health.mil/WhoWeAre/Directorates/ResilienceandPreventionDirectorate.asp x.
- 12.Saltzman WR, Lester P, Beardslee WR, Layne CM, Woodward K, Nash WP. Mechanisms of risk and resilience in military families: Theoretical and empirical basis of a family-focused resilience enhancement program. Clin Child Fam Psychol Rev. 2011;14(3):213 – 230. doi: 10.1007/s10567-011-0096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MacDermid-Wadsworth SM, Samper R, Schwarz R, Nishida J, Nyaronga D. Understanding and promoting resilience in military families. Military Family Research Institute, Purdue; West Lafayette, IN: 2008. [Google Scholar]
- 14.Luthar SS. Resilience in development: A synthesis of research across five decades. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology. Wiley; Hoboken, NJ: 2006. pp. 740–795. [Google Scholar]
- 15.Rutter P, Freedenthal S. Osman A: Assessing protection from suicidal risk: Psychometric properties of the Suicide Resilience Inventory. Death Stud. 2008;32(2):142 – 153. doi: 10.1080/07481180701801295. [DOI] [PubMed] [Google Scholar]
- 16.Beardslee WR, Lester P, Klosinski L, Saltzman W, Woodward K, Nash W, Mogil C, Koffman R, Leskin G. Family-centered preventive intervention for military families: Implications for implementation science. Prev Sci. 2011;12(4):339–348. doi: 10.1007/s11121-011-0234-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Institute of Medicine (IOM) Returning Home from Iraq and Afghanistan: Preliminary Assessment of Readjustment Needs of Veterans, Service members, and Their Families. The National Academies Press; Washington, D.C.: 2010. [September 25, 2011]. Available at http://www.iom.edu/Reports/2010/Returning-Home-from-Iraq-and-Afghanistan-Preliminary-Assessment.aspx. [PubMed] [Google Scholar]
- 18.Lester P, Leskin G, Woodward K, Saltzman W, Nash W, Mogil C, Paley B, Beardslee W. Wartime deployment and military children: Applying prevention science to enhance family resilience. In: MacDermid Wadsworth S, Riggs D., editors. Risk and Resilience in U.S. Military Families. Springer; New York, NY: 2010. pp. 149–174. [Google Scholar]
- 19.Masten AS. Ordinary magic: Resilience processes in development. Am Psychol. 2001;56(3):227 – 238. doi: 10.1037//0003-066x.56.3.227. [DOI] [PubMed] [Google Scholar]
- 20.Chu A, Lieberman A. Clinical implications of traumatic stress from birth to age five. Annu Rev Clin Psychol. 2010;6:469 – 494. doi: 10.1146/annurev.clinpsy.121208.131204. [DOI] [PubMed] [Google Scholar]
- 21.Gewirtz A, Forgatch M, Wieling E. Parenting practices as potential mechanisms for child adjustment following mass trauma. J Marital Fam Ther. 2008;34(2):177 – 192. doi: 10.1111/j.1752-0606.2008.00063.x. [DOI] [PubMed] [Google Scholar]
- 22.Castaneda LW, Harrell MC, Varda DM, Hall KC, Beckett M K, Stern S. Deployment experiences of Guard and Reserve families. RAND Center for Military Health Policy Research; Santa Monica, CA: 2008. [Google Scholar]
- 23.Walsh F. Strengthening family resilience. Guilford; New York: 2006. [Google Scholar]
- 24.Walsh F. A family resilience framework for clinical practice: Integrating developmental theory and systemic perspectives. In: Borden W, editor. Reshaping theory in contemporary social work: Toward a critical pluralism in clinical practice. Columbia University Press; New York: 2010. pp. 146 – 176. [Google Scholar]
- 25.Lester P, Rotheram-Borus MJ, Elia C, Elkavich A, Rice E. TALK: Teens and adults learning to communicate. In: LeCroy CW, editor. Evidence-based treatment manuals for children and adolescents. Oxford University Press; New York: 2008. pp. 170–285. [Google Scholar]
- 26.Lester P, Saltzman W, Woodward K, Glover D, Leskin G, Bursch B, Pynoos R, Beardslee W. Evaluation of a family centered prevention intervention for military children and families facing wartime deployments. Am J Public Health. 2012;102(S1):S48–S54. doi: 10.2105/AJPH.2010.300088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Compas BE, Champion JE, Forehand R, Cole DA, Reeslund KL, Fear J, Roberts L. Coping and parenting: Mediators of 12-month outcomes of a family group cognitive–behavioral preventive intervention with families of depressed parents. J Consult Clin Psychol. 2010;78(5):623 – 634. doi: 10.1037/a0020459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Waldrep DA, Cozza SJ, Chun RS. The impact of deployment on the military family. In: the National Center for Post Traumatic Stress Disorder, editor. The Iraq War Clinician Guide. 2nd ed. Department of Veterans Affairs; Washington, DC: 2004. [October 15, 2012]. pp. 83 – 86. Available at http://www.phoenixhouse.org/wp-content/uploads/2010/12/iraq_clinician_guide_v2.pdf. [Google Scholar]
- 29.Nash W. Combat operational Stress control: The family dynamic professional development training course. Department of the Navy; Washington, DC: 2009. [November 2, 2012]. Available at http://hosted.mediasite.com/mediasite/Viewer/?peid=15d8a8ddadc145f18b0d688ad302d87b. [Google Scholar]
- 30.Palmer C. A theory of risk and resilience factors in military families. Mil Psychol. 2008;20(3):205 – 217. [Google Scholar]
- 31.Galovski T, Lyons JA. Psychological sequelae of combat violence: A review of the impact of PTSD on the veteran's family and possible interventions. Aggress Violent Behav. 2004;9(5):477–501. [Google Scholar]
- 32.Flake EM, Davis BE, Johnson PL, Middleton LS. The psychosocial effects of deployment on military children. J Dev Behav Pediatr. 2009;30:271 – 278. doi: 10.1097/DBP.0b013e3181aac6e4. [DOI] [PubMed] [Google Scholar]
- 33.Friedman MJ. Posttraumatic stress disorder among military returnees from Afghanistan and Iraq. Am J Psych. 2006;163:586 – 593. doi: 10.1176/ajp.2006.163.4.586. [DOI] [PubMed] [Google Scholar]
- 34.Lester P, Mogil C, Saltzman W, Woodward K, Nash W, Leskin G, Beardslee W. Families overcoming under stress: Implementing family-centered prevention for military families facing wartime deployments and combat operational stress. Military medicine. 2011;176(1):19–25. doi: 10.7205/milmed-d-10-00122. [DOI] [PubMed] [Google Scholar]
- 35.Derogatis LR. BSI, Brief Symptom Inventory: Administration, Scoring & Procedures Manual. National Computer Systems; Minneapolis, MN: 1993. [Google Scholar]
- 36.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility.. Paper presented at the 9th Annual Meeting of ISTSS; San Antonio, TX. 1993; [November 2, 2012]. Available at www.pdhealth.mil/library/downloads/pcl_sychometrics.doc. [Google Scholar]
- 37.Goodman RFT, Simmons H, Gatward R, Meltzer H. Using the strengths and difficulties questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br J Psychiatry. 2000;177:534 – 539. doi: 10.1192/bjp.177.6.534. [DOI] [PubMed] [Google Scholar]
- 38.Ryan CE, Epstein NB, Keitner GI, Miller IW, Bishop DS. Evaluation and treating families: The McMaster Approach. Routledge/Taylor and Francis; New York: 2005. [Google Scholar]
- 39.Bentler PM. EQS 6 structural equations program manual. Multivariate Software; Encino, CA: 2006. [Google Scholar]
- 40.Bentler PM, Liang J. Two-level mean and covariance structures: Maximum likelihood via an EM algorithm. In: Duan N, Reise S, editors. Multilevel modeling: methodological advances, issues, and applications. Lawrence Erlbaum; Mahwah, NJ: 2002. pp. 49–66. [Google Scholar]
- 41.Muthén B, Satorra A. Complex sample data in structural equation modeling. In: Marsden PV, editor. Sociological methodology. American Sociological Association; Washington, DC: 1995. pp. 267–316. [Google Scholar]
- 42.Muthén B. Multilevel covariance structure analysis. Sociol Methods Res. 1994;22:376–398. [Google Scholar]
- 43.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1 – 55. [Google Scholar]
- 44.MacCallum R. Specification searches in covariance structure modeling. Psychol Bull. 1986;100:107–120. [Google Scholar]
- 45.McFarlane AC. Military deployment: The impact on children and family adjustment and the need for care. Curr Opin Psychiatry. 2009;22(4):369–373. doi: 10.1097/YCO.0b013e32832c9064. [DOI] [PubMed] [Google Scholar]
- 46. [October 15, 2012];Joining Forces: Taking Action to Serve America's Military Families. http://www.whitehouse.gov/joiningforces.
- 47.Department of Defense (DOD) Task Force on Mental Health [September 25, 2011];An achievable vision: Report of the Department of Defense Task Force on Mental Health. 2007 Available at http://www.apa.org/releases/Military DeploymentTaskForceReport.pdf.
- 48. [September 25, 2011];White House Committee Report: Strengthening our Military Families: Meeting America's Commitment. 2007 Available at http://www.defense.gov/home/features/2011/0111_initiative/strengthening_our_military_janu ary_2011.pdf.