Abstract
The effectiveness of psychotherapies, such as interpersonal and social rhythm therapy (IPSRT), is supported by randomized controlled trials. These trials provide minimal direction regarding feasibility of psychotherapy delivery models. The study purpose was to identify factors facilitating implementation and sustainability of an IPRST group for patients with bipolar disorder. Qualitative data were assessed by the normalization process model (NPM). The results demonstrate feasibility of implementation with experienced clinicians, program coordination, and leadership support. Sustainability challenges include aftercare groups, space, and clinician time. The NPM provides a useful framework for evaluation of factors influencing the feasibility of psychotherapy delivery models.
Based upon evidence from randomized controlled trials (Frank et al., 2005; Frank et al., 2008) and supported by clinical guidelines (APA, 2002; Hirschfeld, 2005; Scottish Intercollegiate Guidelines Network [SIGN], 2005), evidence-based psychotherapies, such as interpersonal and social rhythm therapy (IPSRT), are effective in the treatment of bipolar disorders. A systematic review of randomized controlled trials of psychological therapy for bipolar disorder found the bipolar specific therapies effective in preventing or delaying episode recurrence (Lam, Burbeck, Wright, & Pilling, 2009).
IPSRT is a focused psychotherapy for bipolar disorder which addresses both interpersonal problems and the need for daily social routines to obtain mood stability and increase periods of wellness. Management of interpersonal stressors, role transitions, disruptions in daily schedules, and medication adherence are the focus of psychotherapy (Frank et al., 2005; Frank et al., 2008; Miklowitz et al., 2007).
Clinical effectiveness of psychotherapy, however, does not guarantee successful implementation, integration, or sustainability in clinical practice. Identification of the factors promoting and inhibiting integration of psychotherapy delivery models into practice may enhance the acceptance and subsequent utilization of evidenced based psychotherapy in practice. The normalization process model (NPM) provides a multifactorial framework for evaluation of both integration feasibility and sustainability within the context of a specific psychiatric practice.
CLINICAL QUESTION
The Mayo Clinic Depression Center identified the unmet need for an evidenced based psychotherapy program for patients with mood disorders, particularly bipolar disorder. The research evidence for IPSRT contributed to development of the 2-week IPSRT group program (IPSRT-G). Although participants reported improved depressive symptoms at IPSRT-G completion and at 12-week follow up, clinical improvement does not address the question of integration and sustainability in clinical practice (Hoberg, Ponto, Nelson, & Frye, 2013).
The purpose of this paper is to identify the factors influencing integration and sustainability of IPSRT-G delivered as a 2 week program for outpatients with bipolar I or II disorder. The clinical question addressed was: What are the necessary elements of a 2-week outpatient IPSRT-G psychotherapy program for bipolar I and II patients that make it feasible and sustainable in a tertiary care medical setting?
Patient and clinician factors were considered in evaluation of feasibility. Patient feasibility factors included patient evaluation of treatment effectiveness; perception of mood and behavior change; learning of core components of IPSRT; completion of homework; evaluation of format/structure; and program completion. The patient feasibility measures were obtained from treatment evaluation (TE) and fidelity to treatment (Appendix) forms. Clinician feasibility factors included the availability of clinician time; inter rater reliability; necessary psychotherapy skills; IPSRT training; secretarial and scheduling support; group room availability; and number of participant referrals. The clinician feasibility factors were obtained from formal and informal clinical and operational staff discussions and tracking of the factors in the meeting minutes and the project log.
THEORETICAL FRAMEWORK
The normalization process model (NPM) provides a systems approach toward understanding the implementation, integration, and sustainability of healthcare technologies and interventions into daily clinical practice. Although tested in efficacy trials, it is postulated that these new innovations need to be applied and modified to specific clinical settings to be routinely available in health care. The NPM has been applied to process evaluation in decision support technologies, telemedicine, nurse-led heart failure clinics, language interpretation services, and tuberculosis treatment (Atkins, Lewin, Ringsberg, & Thorson, 2011; Elwyn, Legare, van der Weijden, Edwards, & May, 2008; May, 2006; May, Mair, Dowrick, & Finch, 2007). Although not specific to group psychotherapy delivery models, the NPM has been applied to implementation of national mental health standards, such as suicide prevention in primary care settings and trials of a new psychosocial problem solving therapy (Gask, Rogers, Campbell, & Sheaff, 2008; May, Mair, et al., 2007). Normalization process theory was reported to facilitate understanding of the patient perspective of treatment burden (Gallacher, May, Montori, & Mair, 2011). Both clinician and patient perspectives were considered important in determining feasibility of the IPSRT-G delivery model. The NPM framework improved qualitative research by “elucidating detail, complexity, and meaning beyond the initial thematic analysis” and by considering “relationships within and between constructs” (MacFarlane & O’Reilly-de Brun, 2012, p. 615). The interconnections between the detail, complexity, and meaning of a new intervention for a particular clinical practice and how the process of implementation changes these connections affects the extent to which the intervention becomes part of routine practice. Carl May emphasized that “an innovation is almost never a thing-in-itself”, rather innovations “are shaped by the social world(s) in which they are set, and by their associated ensembles of individual and collective beliefs, behaviors, and activities” (May, 2012, p. 26).
Despite research evidence supporting the clinical effectiveness of IPSRT, it was unknown whether IPSRT could be implemented in a psychotherapy group delivery model within the context of the medical center and whether the psychotherapy and 2-week delivery model would be acceptable to clinicians and patients. The NPM provides a framework for evaluating feasibility from the medical center, clinician, and patient perspective and for evaluating the likelihood of the IPSRT-G delivery model becoming part of the available psychotherapy services.
The NPM concepts of interactional workability, skill-set workability, relational integration, and contextual integration identify factors which promote or inhibit implementation and sustainability of evidence-based psychotherapy delivery models, such as IPSRT-G, within a particular psychiatric context. Interactional workability describes how a complex intervention, such as the IPSRT-G program, affects interaction between clinicians, clinical assistants, secretaries, schedulers, and patients within the clinical practice and the collaboration that occurs or needs to occur in accomplishing the work. Skill-set workability describes how the division of labor within the psychiatric department is influenced by the IPSRT-G program, how the work tasks are assigned and accepted by staff or patients. Relational integration describes how the new psychotherapy delivery model interconnects with the psychiatric clinicians’ current psychotherapy expertise, knowledge of IPSRT, confidence, and accountability in application of that knowledge to specific patient care interventions in the group program. Furthermore, relational integration considers the patients’ confidence and accountability in applying the interventions to their circumstances and their trust in the clinician. Contextual integration describes how IPSRT-G utilizes resources and changes infrastructure, policies, and procedures within the psychiatric practice. Contextual integration considers how the allocation of resources for the IPSRT-G may be perceived by other programs, in context of increasingly finite resources (May, 2006; May, Finch, et al., 2007; May, Mair, et al., 2007). The NPM concept descriptions, factors assessed and tools utilized are listed in Table 1.
Table 1.
Normalization Process Model Construct Description, Feasibility Factors and Tracking Tools.
| Construct description | Feasibility factors assessed | Tracking tools |
|---|---|---|
| Interactional workability describes how a complex intervention affects interactions between health care clinicians, staff, and patients within the clinical practice. | Multidisciplinary team relationships. Referral source education. Recruitment of referrals. Determination of available clinician time. Number of clinicians completing assessments. Number of participants entering and completing the program. | Project log |
| Relational integration describes how a complex intervention relates to current knowledge and relationships in health care practice. | Establishment of clinician and leadership meetings and frequency. Clinician participation in review of the literature, evaluating the evidence, and learning the therapy. Evaluation of participants’ perception of benefit. Spontaneous comments by participants and clinicians. | Meeting minutes Project log Fidelity to treatment form Treatment evaluation form |
| Skill-set workability describes how the division of health care labor is influenced by a complex intervention. | Allocation and acceptance of tasks by discipline. Development of competence in particular tasks by discipline. Current skills of clinicians. Establishment of inter-rater reliability. Training attendance. Participant learning of concepts and completion of homework. | Project log Fidelity to treatment form Treatment evaluation form |
| Contextual integration describes how a complex intervention relates to the context of the health care organization. | Departmental funding for training and materials. Secretarial and scheduling support. Time for program coordination. Priority scheduling of group rooms. History of support for group programs. Cost effectiveness of group programs in the department. | Project log Fidelity to treatment form |
Note. Adapted from “Understanding the Implementation of Complex Interventions in Health Care: The Normalization Process Model,” by C. May, T. Finch, F. Mair, L. Ballini, C. Dowrick, M. Eccles, …B. Heaven, 2007, BMC Health Services Research, 7(148), 1–7. doi:10.1186; 1472-6963-7-148. Copyright 2007 by May et al.; licensee BioMed Central Ltd.
METHOD
Sample and Setting
This study was approved by the Mayo Clinic Institutional Review Board (IRB # 09–003781). Thirty-one patients were referred from Mayo Clinic Depression Center clinicians between October 2009 and January 2010. Eighteen of the thirty-one patients provided written informed consent after receiving a complete description of the project.
Participants were outpatients diagnosed with bipolar I or II depression currently on mood stabilizing treatments with or without concurrent antidepressant medication. Inclusion criteria for the IPSRT-G study were: adults aged 18–65 and current episode of major depression associated with bipolar I or II disorder confirmed by the Structured Clinical Interview for DSM-IV-TR Axis I disorders (SCID) (First, Spitzer, Gibbon, & Williams, 2005). Four patients were ineligible secondary to failure to confirm their bipolar depression diagnosis. Exclusion criteria included: current manic or mixed symptoms as defined by a Young Mania Rating Scale (YMRS) (Young, Biggs, Ziegler, & Meyer, 1978) score of ≥ 15; active suicidal ideation defined by the Inventory of Depressive Symptomatology-Clinician Rated (IDS-C) (Trivedi et al., 2004) question # 18 (response > 2); substance abuse as defined by a screening score on the Alcohol Use Disorders Identification Test-4 (AUDIT) (Bohn, Babor, & Kranzler, 1995) (≥ 5) or confirmation of substance use disorder by SCID diagnostic interview; axis II personality disorder as primary focus of treatment upon review of the electronic medical record; unstable or acute medical condition; or limited English speaking proficiency. Details of the sample, setting, and intervention have been described previously (Hoberg et al., 2013). Nine of the fourteen eligible patients began one of two IPSRT-G programs.
Qualitative data were analyzed according to the constructs of the NPM and the descriptive summary of the TE form. Fidelity to IPSRT-G treatment was assessed by adherence to the fidelity to treatment form.
Study Design
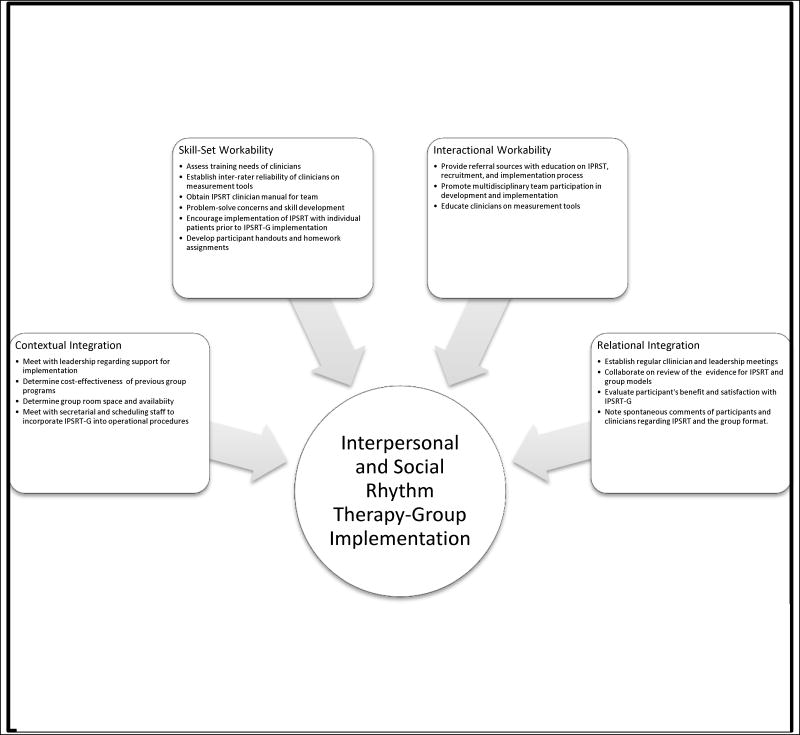
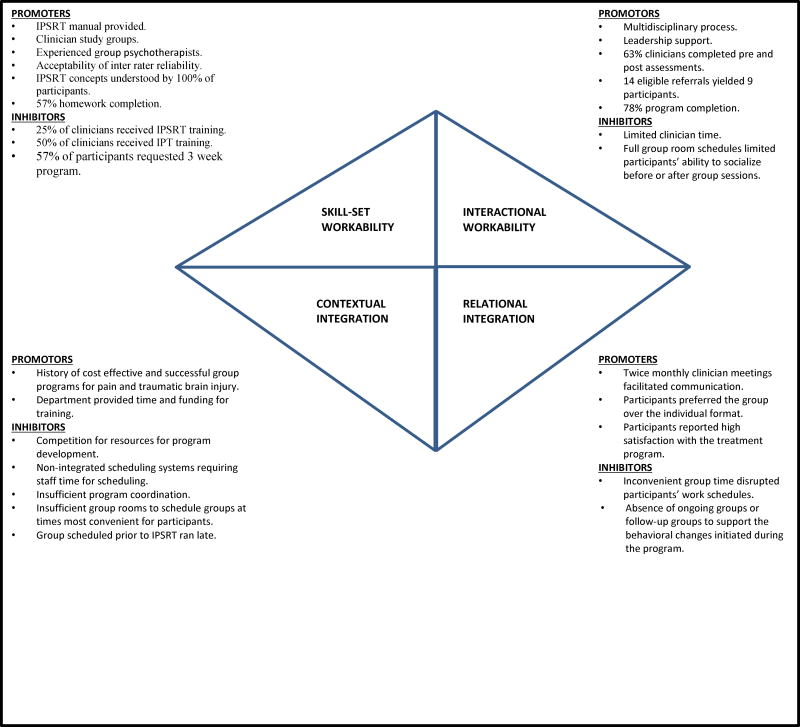
This project used a descriptive approach to qualitative research. The NPM concepts provided the framework to delineate the IPSRT-G implementation process; determine tasks, feasibility factors and tracking tools; and then to categorize the factors which could impact long-term integration and sustainability of IPSRT-G. Figure 1 lists the implementation tasks organized by the NPM constructs. The factors influencing implementation of IPSRT-G were identified utilizing a project log, meeting minutes, fidelity to treatment and TE forms as listed in Table 1. The feasibility factors were categorized by the first author utilizing the NPM concepts as promoting or inhibiting integration within the psychiatric department (Figure 2).
Fig 1.
Interpersonal and social rhythm therapy-group implementation tasks. Adapted from “Understanding the Implementation of Complex Interventions in Health Care: The Normalization Process Model”, by C. May, T. Finch, F. Mair, L. Ballini, C. Dowrick, M. Eccles,…B. Heaven, 2007, BMC Health Services Research, 7(148), 1–7. doi: 10.1186; 1472-6963-7-148. Copyright 2007 by May et al.; licensee BioMed Central Ltd.
Fig 2.
Feasibility of IPSRT-G utilizing the normalization process model. Adapted from “Understanding the Implementation of Complex Interventions in Health Care: The Normalization Process Model”, by C. May, T. Finch, F. Mair, L. Ballini, C. Dowrick, M. Eccles,…B. Heaven, 2007, BMC Health Services Research, 7(148), 1–7. doi: 10.1186; 1472-6963-7-148. Copyright 2007 by May et al.; licensee BioMed Central.
The IPSRT-G intervention consisted of delivering IPSRT as two 60 minute individual psychotherapy sessions followed by six 60 minute group psychotherapy sessions. The group sessions occurred over 2 weeks. The intervention was designed for eight participants in each of two IPSRT-G program series. The design of eight participants per group was intended to comply with the group psychotherapy billing guidelines of the medical center. Although participants were not billed for their study participation, the study was intended to determine the feasibility of the intervention delivery model in the context of existing regulations.
The intervention adapted IPSRT from an individual psychotherapy to a group psychotherapy format. Individual IPSRT generally occurs over 20–24 sessions, with the interpersonal and social rhythm therapy goals formulated within the first five sessions (Frank, 2005). The IPSRT-G format of two individual therapy sessions permitted a comprehensive evaluation of the participant’s illness timeline with identification of the interpersonal and social rhythm factors impacting the participant’s recent illness episode. The group sessions focused on implementation of strategies toward social rhythm stabilization and improvement of interpersonal relationships (Hoberg et al., 2013).
The development and implementation teams consisted of nine multidisciplinary clinicians: two psychiatric licensed clinical social workers (LICSWs), three psychiatrists (MDs), two psychiatric clinical nurse specialists (CNSs), one psychologist (PhD), and one master’s level psychiatric registered nurse (RN) assigned to the integrated mood disorder group of the medical center’s psychiatric department. Including these mood clinicians was intended to facilitate incorporation of the IPSRT-G delivery model into the continuum of care for mood disorders by building relationships and facilitating communication early in the project.
Eight clinicians, excluding the first author, were preferred to minimize time burden for eight potential participants in each program series. Since the participants established therapeutic relationships with the first author, it was determined that objectivity would be improved if the baseline and dismissal assessments were conducted by clinicians who were not conducting the psychotherapy. Having eight clinicians permitted the participant assessments to be completed simultaneously upon conclusion of the final group session. Participants did not need to wait or return at a later time for their assessment.
The development team (two LICSWs, one psychiatrist (MAF), two CNSs, RN, and the PhD) reviewed the literature on bipolar depression, IPSRT, and group psychotherapy. This team developed the IPSRT-G structure, treatment evaluation and fidelity to treatment forms, and determined measurement tools to measure pre and post IPSRT-G change in mood and functioning.
The implementation team included the MD, LICSWs, CNSs, and RN from the development team and added two psychiatrists (SK and MW). The PhD (KSV) was unable to participate in the implementation phase secondary to time constraints. The implementation phase required clinicians to have flexibility to conduct the baseline and dismissal patient assessments. All implementation team members were educated on use of the participant assessments and demonstrated competence by rating of videotaped patient interviews. Weekly IPSRT study groups were scheduled to consolidate self-study of the IPSRT clinician manual, discuss application to current therapy patients, and provide peer supervision in conducting IPSRT for patients with bipolar depression. The study groups were primarily attended by the psychotherapist staff (LICSWs and CNSs). The LICSWs and CNSs had received interpersonal therapy training and had previous group psychotherapy experience. Team members assisted in recruitment, education of referral sources, baseline and dismissal patient assessments, and observation for fidelity to treatment.
The first author conducted all psychotherapy sessions during the project for consistency during the implementation phase. The group therapy sessions were videotaped or observed by one psychiatric licensed clinical social worker (GB) for adherence to the fidelity to treatment form. GB had received interpersonal therapy training and attended IPSRT clinician sessions during a national conference. Although IPSRT training is not essential, peer supervision is desirable when using IPSRT (Frank, 2005). GB was able to provide peer supervision in addition to assessment of adherence to the treatment structure. Supervision and adherence to the IPSRT structure was important since IPSRT was unfamiliar to the majority of clinicians at the medical center prior to implementation of this project.
Assessment Tools
The fidelity to treatment form outlined the IPSRT-G topics adapted from the IPSRT clinician manual (Frank, 2005).
The TE assessed treatment effectiveness and learning from the participant’s perspective and provided an opportunity for the participant to write in remarks. The TE was developed by the author and coauthor (KSV). The coauthor had expertise in qualitative research and patient education materials. Content validity was addressed through feedback from mood clinicians. The TE asked participants (a) to rate the helpfulness of IPSRT-G; mood and behavior change; and learning of core IPSRT components utilizing a 0–10 Likert rating scale; (b) to comment on preferences regarding therapy frequency, session length, group versus individual format and delivery enhancements; and (c) to indicate whether they would recommend the therapy for other patients.
RESULTS
Seven out of nine participants completed all IPSRT-G sessions. The seven participants had a mean age of 46 ± 16.97 years and index depression duration of 4.64 ± 4.21 months. Baseline depression decreased significantly at 2 weeks and 12 weeks (P = .03). Baseline functioning improved significantly at 12 weeks (P = .03). Characteristics of the participants are described in Table 2 (Hoberg et al., 2013).
Table 2.
IPSRT-G Participant Characteristics as a Percentage of the Sample (Number in Parentheses) and Mean (SD).
| Characteristic | Completed (n = 7)
|
Withdrew (n = 2)
|
||
|---|---|---|---|---|
| M (SD) | % (no.) | M (SD) | % (no.) | |
| Age | 46 (16.97) | 24.5 (4.95) | ||
| Female | 86% (6) | 50% (1) | ||
| Caucasian | 100% (7) | 100% (2) | ||
| Education (years) | 15.42 (2.07) | 14.5 (2.12) | ||
| Marital status | ||||
| Married | 43% (3) | 0 | ||
| Single | 43% (3) | 100% (2) | ||
| Widowed | 14% (1) | 0 | ||
| Employment status | ||||
| Full time | 57% (4) | 0 | ||
| Part time | 29% (2) | |||
| Student | 0 | 50% (1) | ||
| Disabled | 14% (1) | 0 | ||
| Unemployed | 0 | 50% (1) | ||
| Bipolar I | 57% (4) | 50% (1) | ||
| Bipolar II | 43% (3) | 50% (1) | ||
| DSM IV-TR co morbidities | ||||
| Anxiety disorder | 43% (3) | 50% (1) | ||
| Personality disorder | 14% (1) | 0 | ||
| Alcohol use disorder | 14% (1) | 50% (1) | ||
| Baseline Measures | ||||
| Inventory of depressive symptomatology- clinician rated | 33 (12.34) | 28 (14.14) | ||
| Beck Depression Inventory-II | 33.14 (7.03) | 26 (15.55) | ||
| Young Mania Rating Scale | 6.71 (3.55) | 8 (8.48) | ||
| Sheehan Disability Scale | 22 (3.74) | 12.5 (4.94) | ||
| Clinical global impressions- bipolar version | 4 (0.58) | 4 (1.41) | ||
| Medication compliance | 1.29 (0.49) | 1.5 (0.70) | ||
The NPM constructs of skill-set workability, interactional workability, contextual integration, and relational integration provided the framework for qualitative analysis. Factors influencing the workability and integration of IPSRT-G are listed in Figure 2 and support the feasibility of implementation of a 2 week IPSRT-G program. Skill-set workability is facilitated by (a) clinicians receiving the IPSRT manual, (b) clinicians’ expertise and years of group psychotherapy experience, (c) acceptability of inter-rater reliability, (d) participants reporting understanding of the concepts, and (e) 57% of participants completing homework assignments. Interactional workability is enhanced by (a) the multidisciplinary team process, (b) leadership support, (c) 63% of the clinicians providing the pre and post participant assessments, (d) 14 eligible referrals yielding 9 participants, and (e) 78% participant completion of the 2 week program. Contextual integration is affirmed by the (a) cost effectiveness of current group programs for pain and traumatic brain injury, and (b) dedication of departmental resources of clinician time and funding to the IPSRT-G program. Relational integration is fostered by (a) scheduling of twice monthly clinician meetings, (b) participant preference for the group rather than individual format, and (c) high level of participant satisfaction with the IPSRT-G program.
Although the majority of identified factors promote feasibility of the IPSRT-G program, 71% (5/7) of the contextual integration factors inhibited feasibility. These inhibiting factors include insufficient staff time for program coordination, non-integrated scheduling systems, and limited late afternoon group rooms. Interactional workability may be negatively impacted by the small number of IPSRT-G participants, despite the majority of eligible referrals (9/14) beginning the IPSRT-G program. The five patients, who did not participate, cited barriers of inclement weather, transportation, severity of depressive symptoms, and time constraints as reasons for not participating in the IPSRT-G program.
Evaluation of the IPSRT-G treatment and structure was obtained from the participant responses to the TE form (Table 3). The group format was preferred by 86% of the seven participants who completed IPSRT-G: “it was helpful to bounce ideas and get suggestions from others that experience the same problems” and “learning from each other was beneficial”. One participant indicated no preference between the group and individual format. The majority (71%) indicated that the 60 minute length of the sessions was “just right”. One participant indicated a preference for 120 minute sessions. The frequency of three group sessions per week for 2 weeks was considered “just right” by 43%, whereas 29% preferred that the sessions occur over 3 or more weeks indicating, “it would be nice to have a group that meets weekly led by a therapist” and “I would prefer the sessions twice a week for three weeks, more time to practice in between”. The remaining 29% were unsure or had no preference. A majority of participants (57 %) cited preference for a 3 week program over the 2 week program for delivery enhancement. The content was considered adequate by 71% of the participants. More content was desired by 29% of the participants to include “more about anxiety and depression and how that influences schedules”.
Table 3.
Participant Evaluation of Treatment (n = 7).
| Just right % (no.) | Too little % (no.) | Too much % (no.) | Not sure/No preference % (no.) | |
|---|---|---|---|---|
| Length | 71% (5) | 29% (2) | 0% | 0% |
| Frequency | 43% (3) | 29% (2) | 0% | 29% (2) |
| Content | 71% (5) | 29% (2) | 0% | 0% |
| Group format | 86% (6) | 0 % | 0% | 14% (1) |
The majority of participants (86%) would recommend IPSRT-G for other patients. Participants described increased self-confidence associated with understanding the connection between moods, interpersonal stressors, and daily scheduling. One participant indicated, “It would be good for someone in a bipolar episode because that is when a routine is not present”. Another participant commented, “This program helped me to look at myself and distinguish a pattern of mood fluctuations based on different situations and disruptions of irregular schedule.” The seven participant comments regarding the most helpful components of the IPSRT-G program are listed in Table 4.
Table 4.
Participant Quotations Regarding the Most Helpful Components of IPSRT-G (n = 7).
| “Being with others who are understanding.” |
| “Recognizing illness can be controlled by me and not the other way around.” |
| “Seeing how changes/disruptions in my schedule play a big part in my mood fluctuations.” |
| “The Social Rhythm Metric sheets were helpful. I gained some insight from the patterns of behavior when my schedule changed too much. Also the group itself, the sharing with others.” |
| “Identifying what I need to work on.” |
| “Identification of relationships between stressors and particular events. Suggestions on how to manage these two extremes.” |
| “Listening to the group members’ ideas and experiences.” |
Fidelity to IPSRT-G treatment was found to be 100% adherent to the outlined structure and discussion topics.
DISCUSSION
The findings of this implementation project suggest that IPSRT-G delivered in a 2 week program is feasible for a large tertiary medical center as measured by treatment evaluation, adherence to IPSRT-G structure, and the NPM constructs. The IPSRT treatment and group delivery model were evaluated positively and well received by the participants. Participants described benefit from being able to discuss IPSRT strategies with others having the same diagnosis. Clinicians were interested in learning about the psychotherapy and participating in the feasibility project. Leadership provided departmental resources including funding and time.
For sustainability of the IPSRT-G program, group room space, program coordination, and dedicated clinician time are necessary. A 3 week program and/or aftercare or maintenance groups may improve learning, provide support, and maintain behavior change for participants. Strategies to increase the number of participants will be essential to maintain program capacity and cost efficiency.
The findings from this feasibility project will be utilized to implement the next steps toward developing a full day IPSRT-G program for patients with bipolar and depressive disorders. The quantitative clinical outcomes and qualitative process outcomes will be shared with leadership and the department clinicians to provide an overview of the therapy and the factors promoting and inhibiting implementation and normalization of an IPSRT-G program into the psychiatric care at the medical center. Utilizing the clinicians from the IPSRT-G project for peer supervision and mentoring of therapists in IPSRT could enhance skill-set workability for the additional staff needed for a full day program. Having a multidisciplinary team facilitated the interactional workability related to communication, understanding of the IPRST framework, and strengthening of the relationships among clinicians interested in treatment of mood disorders. These relationships promoted referrals from the inpatient and outpatient settings and will be essential in generating a sufficient number of referrals to support continuing the IPSRT-G program. Sufficient referrals will be necessary to meet organizational expectations for cost effective group programs and contextual integration. Defined opportunities for mood clinicians to discuss assessment and treatment of patients with mood disorders will promote relational integration of IPSRT-G into the scope of treatment recommendations and maintain a high level of evidenced based practice. In the same way as patients referenced the curative factor of universality and being amid others with mood disorders, so clinicians may feel less alone in treating complex illnesses when working as a team.
Limitations
Study outcomes and interpretation are limited by methodological considerations. The TE was developed to obtain participant evaluation of the IPSRT-G treatment but was not rigorously tested for validity or reliability. No specific tool was developed to obtain the clinician evaluation; rather the clinician evaluation was obtained through formal and informal discussions. The small number of participants limits interpretation of the results. Small group size may have inflated the positive program evaluation, in that participants likely had more opportunity for discussion than if the group size had been larger. The feasibility results, as intended by the NPM, are specific to the Midwestern medical center and may not be generalizable to other mental health practices.
Implications for Practice
Process evaluation models, such as the NPM, may increase the availability of evidence-based mental health care by identifying the factors necessary for implementation and sustainability of psychotherapy delivery models, such as IPSRT-G, within specific organizations. While promoting factors influence implementation of the psychotherapy delivery model, the inhibiting factors challenge the long-term sustainability of the model and need to be addressed for the psychotherapy to become routinely available and integrally imbedded within a specific health care organization.
Although specific to IPSRT-G delivery and the Midwestern medical center, the identified promoting factors of leadership/clinician support and positive participant evaluation are likely necessary for successful implementation of psychotherapy group delivery models in other mental health care organizations. Similarly, overcoming the challenges by (a) designating time and clinician teams to the program, (b) marketing the program to referral sources and potential participants, (c) developing aftercare programs and maintenance groups, and (d) scheduling of late afternoon groups may enhance sustainability for many delivery models.
In conclusion, process evaluation utilizing the NPM constructs of skill-set workability, interactional workability, relational integration and contextual integration can enhance the integration of psychotherapy delivery models into the context of a specific mental health care organization and facilitate availability of evidence based treatments. This project identified feasibility factors influencing integration of a group psychotherapy model into a busy clinical practice. Developing strategic responses for the challenges, such as marketing of programs, scheduling late afternoon groups, prioritizing group room space and utilizing clinician teams may facilitate successful integration of evidence based psychotherapy delivery models. Integration and sustainability of evidence based psychotherapy, such as IPSRT, may increase the availability of effective therapy for people with bipolar disorder, decrease health care costs, and improve the lives of these individuals.
Acknowledgments
The authors wish to acknowledge the contributions of Cindy Stoppel, Department of Psychiatry and Psychology, Mayo Clinic, Rochester, Minnesota in study implementation.
This research was partially supported by the Center for Translational Science Activities (CTSA) at Mayo Clinic. This center is funded in part by a grant from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) (RR024150 PI: Rizza). Its contents are the sole responsibility of the authors and do not necessarily represent the official view of CTSA, NCRR or NIH.
This research was funded in part by Mayo Foundation.
APPENDIX. FIDELITY TO TREATMENT FORM
Directions: Please check areas completed.
Session 1: Individual therapy session.
___Reviewed goals of treatment: (a) reduction of symptoms, (b) prevention of future episodes, (c) improvement in interpersonal functioning, and (d) regularity of social rhythms.
___Reviewed the Social Rhythm Metric-II.
___Completed the illness timeline.
Comments:
Session 2: Individual therapy session.
___ Completed the interpersonal inventory.
___ Defined two primary interpersonal focus areas.
___ Reviewed the Social Rhythm Metric-II and identified their target times.
Comments:
Session 3: First group session.
___Reviewed confidentiality.
___Members introduced themselves by discussing desired changes in their daily schedule.
___ Discussed the connection between mood and daily social rhythms.
___ Discussed strategies to move closer to the target times for activities as time allows.
Comments:
Session 4: Second group session.
___Reviewed Social Rhythm Metric-II and strategies members have implemented to move toward their targets.
___Discussed grief for the lost healthy self and significance of the diagnosis of bipolar disorder.
___Reviewed role of medication adherence and understanding of bipolar disorder.
___Included unresolved grief issues, if applicable.
Comments:
Session 5: Third group session.
___Reviewed Social Rhythm Metric-II noting difficulties related to grief, medication adherence, understanding of bipolar disorder and daily rhythms.
___Discussed role disputes identified by group members.
Comments:
Session 6: Fourth group session.
___Reviewed Social Rhythm Metric-II noting relationship with role disputes.
___Discussed role transitions identified by group members.
Comments:
Session 7: Fifth group session.
___Reviewed Social Rhythm Metric-II noting relationship to role transitions.
___Discussed strategies for unexpected disruptions in routines.
___Participants wrote down relevant strategies.
Comments:
Session 8: Final group session.
___Reviewed plans to maintain progress on social rhythm scheduling and interpersonal problem solving.
___Reviewed illness management strategies including medication adherence, medication follow-up, target symptoms, and interpersonal support.
Comments:
Adapted from “Treating bipolar disorder: A clinician’s guide to interpersonal and social rhythm therapy”, by E. Frank. Copyright by Guilford Press.
Footnotes
Author Roles: AAH conducted the psychotherapy sessions, analyzed the data and wrote the article. KSV developed the treatment evaluation form and edited the article. JE, GB, SK, RS, MW, and MJM collected the data and edited the article. MAF conducted the patient interviews for inter-rater reliability and provided consultation.
Declaration of Conflicting Interests: Astrid A. Hoberg, Kristin S. Vickers, Joanne Ericksen, Grant Bauer, Simon Kung, Randy Stone, Mark Williams, and Mary Jo Moore report no conflict of interest with respect to the authorship and/or publication of this article. Mark A. Frye disclosure: Grant support -Pfizer, National Alliance for Schizophrenia and Depression (NARSAD), National Institute of Mental Health (NIMH), National Institute of Alcohol Abuse and Alcoholism (NIAAA), Mayo Foundation. Consultant - Dainippon Sumittomo Pharma, Merck, Sepracor. CME supported activity -Astra-Zeneca, Bristol-Myers Squibb, Eli Lilly and Co., GlaxoSmithKline, Merck, Otsuka Pharmaceuticals, Pfizer, Sanofi-Aventis.
References
- American Psychiatric Association (APA) Practice guideline for the treatment of patients with bipolar disorder. 2. Arlington, VA: American Psychiatric Association; 2002. Retrieved from. http://www.psychiatryonline.com/pracGuide/pracGuideTopic_8.aspx. [DOI] [PubMed] [Google Scholar]
- Atkins S, Lewin S, Ringsberg KC, Thorson A. Provider experiences of the implementation of a new tuberculosis treatment programme: A qualitative study using the normalisation model. BMC Health Sciences Research. 2011;11(275):1–9. doi: 10.1186/1472-6963-11-275. http://dx.doi.org/10.1186/1472-6963-11-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohn MJ, Babor TF, Kranzler HR. The alcohol use disorders identification test (AUDIT): Validation of a screening instrument for use in medical settings. Journal of Studies on Alcohol. 1995;56(4):423–432. doi: 10.15288/jsa.1995.56.423. [DOI] [PubMed] [Google Scholar]
- Elwyn G, Legare F, van der Weijden T, Edwards A, May C. Arduous implementation: Does the normalisation process model explain why it’s so difficult to embed decision support technologies for patients in routine clinical practice. Implementation Science. 2008;3(57):1–9. doi: 10.1186/1748-5908-3-57. http://dx.doi.org/10.1186/1748-5908-3-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV-TR Axis I Disorders. New York: Biometrics Research, New York State Psychiatric Institute; 2005. [Google Scholar]
- Frank E. Treating bipolar disorder: A clinician’s guide to interpersonal and social rhythm therapy. New York: The Guilford Press; 2005. [Google Scholar]
- Frank E, Kupfer DJ, Thase ME, Mallinger AG, Swartz HA, Fagiolini AM, et al. Two year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Archives of General Psychiatry. 2005;62:996–1004. doi: 10.1001/archpsyc.62.9.996. [DOI] [PubMed] [Google Scholar]
- Frank E, Soreca I, Swartz HA, Fagiolini AM, Mallinger AG, Thase ME, et al. The role of interpersonal and social rhythm therapy in improving occupational functioning in patients with bipolar I disorder. The American Journal of Psychiatry. 2008;165(12):1559–1565. doi: 10.1176/appi.ajp.2008.07121953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallacher K, May CR, Montori VM, Mair FS. Understanding patient’s experiences of treatment burden in chronic heart failure using normalization process theory. Annals of Family Medicine. 2011;9(3):235–243. doi: 10.1370/afm.1249. http://dx.doi.org/10.1370/afm.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gask L, Rogers A, Campbell S, Sheaff R. Beyond the limits of clinical governance: The case of mental health in English primary care. BMC Health Services Research. 2008;8(63):1–10. doi: 10.1186/1472-6963-8-63. http://dx.doi.org/10.1186/1472-6963-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschfeld RM. Guideline watch: Practice guideline for the treatment of patients with bipolar disorder. Arlington, VA: American Psychiatric Association; 2005. Retrieved from. http://www.psychiatryonline.com/pracGuide/pracGuideTopic_8.aspx. [Google Scholar]
- Hoberg AA, Ponto J, Nelson PJ, Frye MA. Group interpersonal and social rhythm therapy for bipolar depression. Perspectives in Psychiatric Care. 2013 doi: 10.1111/ppc.12008. http://dx.doi.org/10.1111/ppc.12008 (Advance online publication) [DOI] [PMC free article] [PubMed]
- Lam DH, Burbeck R, Wright K, Pilling S. Psychological therapies in bipolar disorder: The effect of illness history on relapse prevention-a systematic review. Bipolar Disorders. 2009;11:474–482. doi: 10.1111/j.1399-5618.2009.00724.x. [DOI] [PubMed] [Google Scholar]
- MacFarlane A, O’Reilly-de Brun M. Using a theory-driven conceptual framework in qualitative health research. Qualitative Health Research. 2012;22(5):607–618. doi: 10.1177/1049732311431898. http://dx.doi.org/10.1177/1049732311431898. [DOI] [PubMed] [Google Scholar]
- May C. A rational model for assessing and evaluating complex interventions in health care. BMC Health Services Research. 2006;6(86):1–11. doi: 10.1186/1472-6963-6-86. http://dx.doi.org/10.1186/1472-6963-6-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May C. Agency and implementation: Understanding the embedding of healthcare innovations in practice. Social Science & Medicine. 2012;78(2013):26–33. doi: 10.1016/j.socscimed.2012.11.021. http://dx.doi.org/10.1016/j.socscimed.2012.11.021. [DOI] [PubMed] [Google Scholar]
- May C, Finch T, Mair F, Ballini L, Dowrick C, Eccles M, Heaven B. Understanding the implementation of complex interventions in health care: The normalization process model. BMC Health Services Research. 2007;7(148):1–7. doi: 10.1186/1472-6963-7-148. doi: 10.1186; 1472-6963-7-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May C, Mair F, Dowrick C, Finch T. Process evaluation for complex interventions in primary care: Understanding trials using the normalization process model. BMC Family Practice. 2007;8(42):1–9. doi: 10.1186/1471-2296-8-42. http://dx.doi.org/10.1186/1471-2296-8-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Otto MW, Frank E, Reilly-Harrington NA, Kogan JN, Sach GS, et al. Intensive psychosocial intervention enhances functioning in patients with bipolar depression: Results from a 9-month randomized controlled trial. The American Journal of Psychiatry. 2007;164(9):1340–1347. doi: 10.1176/appi.ajp.2007.07020311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scottish Intercollegiate Guidelines Network (SIGN) Bipolar affective disorder: A national clinical guideline (SIGN clinical guideline 82) 2005 Retrieved from. http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id=7285&nbr=004338&string=Bipolar.
- Trivedi MH, Rush AJ, Ibrahim HM, Carmody TJ, Biggs MM, Suppes T, Kashner TM. The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: A psychometric evaluation. Psychological Medicine. 2004;34(1):73–82. doi: 10.1017/s0033291703001107. [DOI] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity, and sensitivity. The British Journal of Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]