Abstract
Context
Little is known about how geographic variation of cardiovascular procedures compares between beneficiaries with Medicare Advantage (MA) and Medicare fee-for-service (MFFS).
Objective
To compare regional cardiovascular procedure rates between MFFS and MA beneficiaries.
Design
Cross-sectional study comparing rates of coronary angiography, percutaneous coronary intervention (PCI), and coronary artery bypass grafting (CABG).
Setting
32 Hospital Referral Regions (HRRs) in 12 states.
Patients (or Participants)
Medicare beneficiaries over age 65 between 2003–2007.
Main Outcome Measure(s)
Rates of coronary angiography, PCI and CABG.
Results
We evaluated a total of 878,339 MA patients and 5,013,650 MFFS patients across 32 HRRs. Compared with MFFS patients, MA patients had lower age-, sex-, race, and income-adjusted procedure rates for angiography (16.5/1000 person-years vs. 25.9/1000; p <0.001) and PCI (6.8/1000 vs. 9.8/1000; p<0.0001) but similar rates for CABG (3.1/1000 vs. 3.4/1000; p=0.33). Procedure rates varied widely among both MA and MFFS patients. For angiography, the rates ranged from 9.8/1000 to 40.6/1000 for MA beneficiaries and from 15.7/1000 to 44.3/1000 for MFFS beneficiaries. For PCI, the rates ranged from 3.5/1000 to 16.8/1000 for MA and from 4.7/1000 to 16.1/1000 for MFFS. The rates for CABG ranged from 1.5/1000 to 6.1/1000 for MA and from 2.5/1000 to 6.0/1000 for MFFS. Across regions, we found no statistically significant correlation between MA and MFFS beneficiary utilization for angiography (r = 0.19, p = 0.29) and modest correlations for PCI (r= 0.33, p = 0.06) and CABG (r = 0.35, p =0.05). Among MA beneficiaries, demographic(age, gender, race, and income) adjusted rates were highly correlated with demographic and disease adjusted rates ( r = 0.82 for angiography, 0.87 for PCI, and 0.97 for CABG; p<0.0001).
Conclusions
Rates of angiography and PCI, were significantly lower among MA than MFFS beneficiaries while rates of CABG were not significantly different. Rates varied widely at the HRR level among both MA beneficiaries and MFFS beneficiaries. While capitation through MA is associated with lower angiography and PCI procedure rates, the substantial geographic variation suggests that capitation alone will not lead to reductions in the variations seen in cardiovascular procedure use.
Introduction
Treatment of cardiovascular (CV) disease is one of the largest drivers of health care cost in the U.S., accounting for $273 billion annually.1 CV procedures are major contributors to this high cost. Studies consistently demonstrate several-fold geographic variation in rates of CV procedures across the U.S.2–5 For example, the 2007 rate of coronary angiography varied nearly 6-fold from 6.8 per 1000 Medicare fee-for-service (MFFS) beneficiaries in Honolulu, HI to 39.8 per 1000 in Gulfport, MS.
The vast majority of the studies of geographic variation in clinical practice have been performed among the MFFS population.6 In contrast, relatively little is known about variation in the rates of healthcare utilization among the 23% of Medicare beneficiaries who are covered under capitated plans via the Medicare Advantage (MA) program.7 If the primary reason for geographic variation in healthcare utilization is varying financial incentives for physicians, one would expect that overall CV procedure rates and variation in procedure rates would be lower for MA patients than for MFFS patients.. On the other hand, if factors such as differences in patient clinical characteristics,8;9 patient preferences for treatment, or local practice culture10 are the central drivers of variation then one would expect that overall CV procedure rates and variation in procedure rates would be similar for MA patients than for MFFS patients.
Therefore, the objective of this study was to compare the overall rates and local area rates of coronary angiography, percutaneous coronary intervention (PCI), and coronary artery bypass grafting (CABG) between MFFS and MA beneficiaries living in the same communities. We hypothesized that compared with MFFS, overall rates and the degree of geographic variation of CV procedure use would be lower within the MA program.
Methods
Study Design
We conducted a cross sectional study comparing rates of coronary angiography, PCI, and CABG among MFFS and MA beneficiaries over the 5-year period spanning 2003–2007.
Data Sources
Medicare Fee for Service (MFFS) patients
The study sample of MFFS patients was drawn from the Medicare enrollment database (i.e., “Denominator” files). This database includes monthly indicators of whether beneficiaries are enrolled in an MFFS or MA plan, as well as demographic information including dates of birth and death, sex, race, and residential ZIP codes.
Medicare Advantage (MA) patients
The study sample of beneficiaries with MA plans was drawn from a population of approximately 11 million patients served by integrated delivery systems within the Cardiovascular Research Network (CVRN).11–13 In brief, the CVRN is a National Heart, Lung, and Blood Institute-sponsored consortium of 15 health systems with dedicated research divisions. The research divisions compile their data, consisting of administrative, claims, and clinical electronic health record data, into standardized research repositories called the Virtual Data Warehouse to facilitate collaborative research.12 Twelve CVRN sites participated in this study.
Geographic Area
For this analysis, we used the Hospital Referral Region (HRR) as the geographic unit of analysis. HRRs have been defined by the Dartmouth Atlas project based on referral patterns for tertiary care.6 HRRs are designed to approximate healthcare markets, in which practice patterns may be similar. Patients were assigned to HRRs by their ZIP code of residence.
Procedure Identification
Procedures were identified among MFFS patients via inpatient and outpatient facility claims as well as physician claims. The use of outpatient claims was necessary as angiography and PCI are increasingly performed on an outpatient basis.14 Procedures were identified among MA patients via administrative claims or the electronic health record within participating CVRN health plans.12 MA patients with health plans not participating within the CVRN are not included in this analysis. Physician and facility for the same procedure on approximately the same date were assumed to be redundant.
For both MFFS and MA data, coronary angiography was identified by ICD-9 codes 37.22, 37.23, 88.55, 88.56, 88.57 or CPT codes 93508, 93539, 93540, 93545, 93556. PCI was identified by ICD-9 codes 00.66, 36.01, 36.02, 36.05, 36.06, 36.07, 36.09 or CPT codes 92980–92984, 92995, 92996, G0290, G0291. CABG was identified by ICD 9 codes 36.1X and CPT codes 33510–33536.
Geographic Analysis
The study was restricted to patients living in HRRs (n=32) with a minimum of 6000 CVRN MA beneficiaries to assure precision and stability of the HRR-level procedure rates. In these HRRs, we included only MA or MFFS patients between the ages of 65 and 99 years, as Medicare coverage is nearly universal after age 65 years. Rates per 1000 enrollee-years were determined by dividing the total number of procedures among the population within a given HRR over the timeframe by the population within that region accounting for partial-year enrollees. Crude rates were then adjusted for age, gender, race, and income using the indirect adjustment method with the national MFFS rates as the standard rates.15 We used 2000 U.S. census per capita income data mapped to zip codes to estimate the mean income for MA and MFFS patients.
To compare procedure rates across HRRs and between MA and MFFS beneficiaries, we used generalized linear models with a Poisson distribution and a deviance scale parameter to adjust for over-dispersion. Outcome variables were the age, gender, race and income adjusted procedure counts and person-year denominators were included as a logged offset term. MA versus MFFS insurance status, HRR location, and income variables were added to these models. We calculated the variation reduction due to the addition of a variable using over-dispersion parameters estimated in Poisson models. The over-dispersion of count data is caused by unmeasured variables and an over-dispersion parameter is used in Poisson models to account for the fact that the variance is not equal to the mean. If a variable is associated with outcome and is added in a Poisson model, the over-dispersion of count data is lessened and its parameter decreases. We used the decrease of the over-dispersion parameters as a measure of variation reduction in this analysis
We explored the degree of regional variation between MA and MFFS beneficiaries in two ways; we calculated the degree of variation between the maximum and minimum adjusted HRR-level procedure rates, and we performed a Levene test to compare variances.
We used a Spearman Rank-Order correlation coefficient to assess the correlations between the HRR rates for: 1) MA and MFFS beneficiaries for each procedure; 2) angiography and PCI in both MA and MFFS populations; and 3) PCI and CABG in both the MA and MFFS populations. To estimate how much of the variability was associated with region compared to MA/MFFS status, we used linear regression with the age and gender adjusted regional rate as the outcome and region and MA/MFFS status as predictors.
Within the CVRN only, we additionally adjusted for the presence of coronary heart disease, cardiovascular risk factors (hypertension, hyperlipidemia, and diabetes).16 The following ICD-9 codes were used: 272.0–272.4 for hyperlipidemia; 401.XX-404.XX for hypertension; 250.XX for diabetes; and 410.XX, 412.XX, and 414.0 for prior coronary heart disease. We used a Spearman correlation coefficient to determine the correlation between the demographically adjusted (age, gender, and race only) procedure rates and demographically and disease (coronary heart disease/risk-factor adjusted) procedure rates at the HRR level.
Statistical analyses were conducted using SAS 9.3 (Cary, NC). A p-value of <0.05 was considered to be significant. The IRBs at the University of Pennsylvania and each CVRN site either approved or ceded to the Kaiser Northern California IRB.
Results
This study included 12 CVRN integrated health care delivery systems which represented 32 distinct HRRs. Within these HRRs were 878,339 MA patients and 5,013,650 MFFS patients. The proportion of study patients enrolled in a MA plan varied across HRRs from 3% in the Georgia HRRs to 28% in the Northern California HRRs (Table 1). MA and MFFS patients were demographically similar but the MA patients did have slightly lower rates of diabetes (21% vs. 24%), hyperlipidemia (44% vs. 50%), and prior coronary artery disease (13% vs 19%). Due to the large sample sizes, all differences between the groups were significant (p<0.001).
Table 1.
Populations of Medicare patients within and surrounding each Cardiovascular Research Network delivery system (average for 2003–2007)
| CVRN Delivery System | Hospital Referral Regions | Medicare Advantage population (n=878,339)* | Medicare FFS population (n=5,013,650) | CVRN percent of total |
|---|---|---|---|---|
| KP Colorado | Denver, Boulder | 61,807 | 189,088 | 25 |
| KP Northern California | Santa Rosa, San Francisco, Sacramento, Fresno, Napa, San Jose, Alameda County, Stockton, San Mateo County, Contra Costa County | 325,337 | 823,606 | 28 |
| KP Southern California | Orange County, Los Angeles, San Bernadino, San Diego, Ventura | 164,248 | 1,205,717 | 12 |
| KP Northwest | Portland, Salem | 56,980 | 206,586 | 22 |
| KP Georgia | Atlanta | 16,576 | 510,073 | 3 |
| KP Hawaii | Honolulu | 27,153 | 110,313 | 20 |
| Group Health Cooperative | Seattle, Tacoma, Olympia, Everett | 67,986 | 415,784 | 14 |
| HealthPartners | Minneapolis, St. Paul | 50,794 | 460,492 | 10 |
| Henry Ford | Detroit, Dearborn | 21,196 | 319,143 | 6 |
| Harvard Pilgrim | Boston | 47,612 | 554,760 | 8 |
| Lovelace Sandia | Albuquerque | 30,702 | 156,805 | 16 |
| Marshfield | Marshfield Clinic | 14,665 | 61,283 | 19 |
FFS – Fee-For-Service; KP – Kaiser Permenante; CVRN – Cardiovascular Research Network
The number of Medicare Advantage patients enrolled in a CVRN health care delivery system; this does not include Medicare beneficiaries enrolled in other Medicare Advantage plans located in these regions.
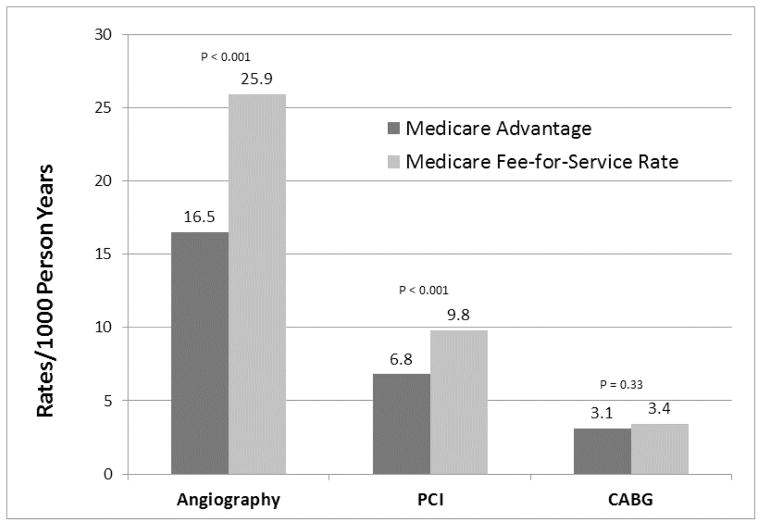
Compared with MFFS patients, MA patients had lower age-, sex-, race, and income-adjusted procedure rates for angiography (6.5/1000 vs. 25.9/1000; p <0.0001, rate ratio (RR) 0.64; 95% CI 0.54 – 0.75) and PCI (6.8/1000 vs. 9.8/1000; p<0.0001; RR 0.70; 95% CI 0.59–0.83) but similar rates for CABG (3.1/1000 vs. 3.4/1000; p=0.33; RR 0.93: 95% CI 0.80–1.08)(Figure 1).
Figure 1.
A Comparison of Cardiovascular Procedure Rates Between Beneficiaries Served by Health Plans Within the Cardiovascular Research Network and Beneficiaries with Fee-For-Service Reimbursement Plans.
PCI – Percutaneous Coronary Intervention; CABG – Coronary Artery Bypass Grafting
MA patients had lower age-, sex-, race, and income-adjusted procedure rates for angiography (16.5/1000 person-years vs. 25.9/1000; p <0.001) and PCI (6.8/1000 vs. 9.8/1000; p<0.0001) but similar rates for CABG (3.1/1000 vs. 3.4/1000
When exploring procedure rates across HRRs, we found wide geographic variation among both MA and MFFS patients. For angiography, the rates among MA beneficiaries ranged from 9.8/1000 person-years to 40.6/1000 person-years, while the rates within MFFS ranged from 15.7/1000 person-years to 44.3/1000 person-years with no statistically significant difference in the variances (37.1 vs. 49.9, p=0.56). For PCI, the rates among MA beneficiaries ranged from 3.5/1000 person-years to 16.8/1000 person-years, while the rates among MFFS beneficiaries ranged from 4.7/1000 person-years to 16.1/1000 person-years with no statistically significant difference in the variances (7.0 vs. 8.0, p=0.77). For CABG, the rates among MA beneficiaries ranged from 1.5/1000 person-years to 6.1/1000 person-years, while the rates among MFFS beneficiaries ranged from 2.5/1000 person-years to 6.0/1000 person-years with no statistically significant difference in the variance (1.2 vs. 0.68, p =0.14).
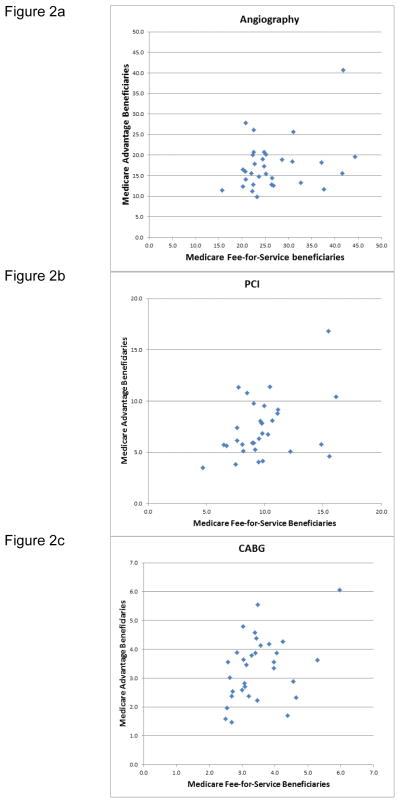
We found no statistically significant correlation between MA and MFFS beneficiary utilization for angiography (r = 0.19, p = 0.29, Figure 2a) and modest correlations for PCI (r= 0.33, p = 0.06, Figure 2b) and CABG (r = 0.35, p =0.05, Figure 2c). In our Poisson analysis, we found that the variation in the rates of angiography was reduced by 19% when payment structure (MA vs. MFFS) was added to the model and was further reduced to a total of 50% when region (HRR) was added to the model. For PCI, the variation was reduced by 11% with payment structure only and by a total of 47% when region was added to the model. For CABG, the variation was reduced by 1% with payment structure only and by a total of 36% when region was added to the model.
Figure 2.
Figure 2a–c. Comparison of the average a) angiography; b) PCI; and c) CABG age, gender, and race adjusted rates per 1000 person-years between Medicare Advantage beneficiaries and Medicare Fee-for-service beneficiaries from 2003–2007 across the hospital referral regions. PCI – Percutaneous Coronary Intervention; CABG – Coronary Artery Bypass Grafting
When exploring the correlation of procedures at the HRR level, we found that rates of coronary angiography were highly correlated with rates of PCI (r = 0.88, p < 0.0001)) and rates of PCI were modestly correlated with rates of CABG (r = 0.54, p<0.0001)
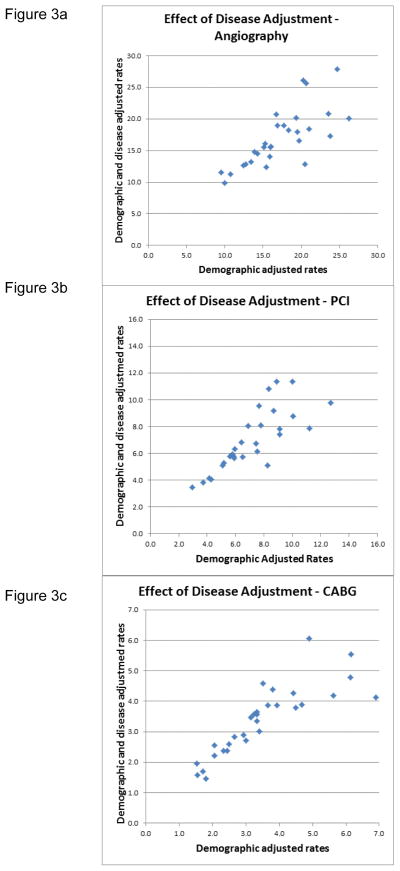
Within the CVRN only, the demographically adjusted (age, gender, race, and income only) rates for angiography were highly correlated with the demographically and disease adjusted (coronary heart disease/risk-factor) procedure rates (r = 0.82, p <0.0001, Figure 3a). For PCI, the demographically adjusted and demographically and disease adjusted rates were also highly correlated (r = 0.85, p < 0.0001, Figure 3b). For CABG, the demographically adjusted and demographically and disease adjusted rates were also highly correlated (r = 0.94, p < 0.0001, Figure 3c).
Figure 3.
Figure 3a–c. The comparison of rates adjusted for age, sex, and race with rates additionally adjusted for presence of diabetes, hypertension, hyperlipidemia, and prior coronary artery disease within the Medicare Advantage population across the hospital referral regions. PCI – Percutaneous Coronary Intervention; CABG – Coronary Artery Bypass Grafting
Discussion
We compared overall rates of and geographic variation in the use of major CV procedures between MA and MFFS beneficiaries across 32 HRRs. We found that rates of angiography and PCI were significantly lower among MA beneficiaries while the rates for CABG were not significantly different. We also found that CV procedure rates varied widely at the HRR level among both MA beneficiaries and MFFS beneficiaries. The HRR-level procedure rates were modestly correlated between MA and MFFS beneficiaries for PCI and CABG but not for angiography. Finally, demographically adjusted procedure rates were highly correlated with demographically and disease adjusted rates.
This project has several strengths. First, we directly compared rates between MA and MFFS beneficiaries. Very few studies have done this because comprehensive administrative claims data for MA patients has not been readily available. Data sources such as the CVRN are among the few ways to capture procedure rates within MA systems. Because evolving payment policy including accountable care organizations17 emphasize capitation, it is critical that we better understand its effects on health care utilization. Second, the CVRN is large and geographically diverse with patients that are comparable to those in the surrounding populations.13 Third, we include both inpatient and outpatient rates. Prior reports documenting geographic variation of procedures generally only include inpatient rates.6 While this is appropriate for procedures like CABG that are always performed in the hospital, counting inpatient rates alone underestimates rates for procedures performed on large numbers of outpatients, including angiography and PCI. Fourth, most geographic variation studies have not adjusted for differences in population clinical characteristics.9;18 In this study we not only adjusted for patient demographics but also adjusted for pre-existing coronary heart disease as well as risk factors for coronary heart disease.
The finding that MA patients have lower angiography and PCI rates underscores the need for additional research to determine the extent to which this is due to differences in population characteristics, more efficient utilization of procedures among MA patients (i.e., overuse in MFFS), or harmfully restrictive utilization management among MA patients (i.e., underuse in MA). One explanation for the differences in rates seen in this report could be that MA beneficiaries are healthier and require fewer CV procedures than MFFS beneficiaries.19 We partially address this by showing that disease and demographically adjusted rates are highly correlated with the demographically adjusted rates. Future research should explore if the differences in procedure rates between MA and MFFS patients are associated with differences in appropriateness and in clinical outcomes.
The degree of regional variation was similar for MA and MFFS beneficiaries, suggesting that factors beyond payment mechanisms influence practice variations. For some medical interventions, regional variation has been strongly associated with supply, for example, length of stay in an ICU is associated with the regional number of ICU beds.20 Similarly, prior research suggests that the rate of cardiac catheterization is associated with the regional supply of cardiac catheterization labs.21 The variation seen in this study may be a function of the availability of the procedures. In other research, patient-level factors including patient preferences and disease variability have had a relatively small influence on variations in utilization.22–27 The fact that the variation did not diminish with disease adjustment in our analysis further supports this point. Prior research exploring appropriateness in angiography at the regional level suggests that regions with higher rates perform a higher number of both appropriate and inappropriate procedures.5 Finally, other research suggests that the central drivers of practice variation are implicit professional norms or the local practice culture.10;28 To understand each of these potential factors better, future research should explore the influences of physician supply, procedure capacity, social norms, practice culture, and appropriateness of procedure use.
The finding that the regional rates for PCI and CABG are correlated between the MA and the MFFS beneficiaries is consistent with prior studies comparing utilization between capitated and FFS reimbursement systems. Data from the California Office of Statewide Health Planning and Development demonstrated that patients enrolled in integrated health care delivery systems had similar patterns of geographic variation compared with FFS patients in the number and length of stay of their hospitalizations.29 In the Kaiser Permanente healthcare system, more than two-fold variations have been seen across regions in the average number of hospital days in the last six months of life. While those numbers were lower than the number of hospital days seen in MFFS patients in these same regions, the patterns of use were correlated at the region level.30 Our report extends those findings by directly exploring patient level utilization in procedure rates between a much larger population of MA and MFFS patients and by demonstrating that the degree of variation and the correlation persists even after adjusting for population clinical characteristics.
Several limitations should be considered when interpreting these findings. First, we were unable to assess the degree to which regional variations were influenced by procedural appropriateness or patient preferences. Second, these results were not linked to clinical outcomes, so we do not know if differential use of CV procedures within an HRR affects patient outcomes. Third, patients choosing a MA plan may be different than patients in MFFS, and this implies that the “correct” rate of CV procedure use may be different in these populations.31 Fourth, we were unable to adjust for smoking, one of the most important risk factors for coronary artery disease. Fifth while all MA plans receive capitated payments from the government, there are different models of delivery such as “staff” models where providers are salaried and work directly for the health management organization and “group” or “network” models where providers are contracted by the health plan. Given that many of the organizations participating in the CVRN are a mixture of these models, we were unable to analyze this effect in this report but this would be an important avenue for future research.
Conclusions and implications
Geographic variation in health services in the MFFS population has fueled the perception of an inefficient, ineffective American healthcare system.22;32 Until the causes of geographic variation are understood, shedding light on the sources of variability remains an important research and quality improvement endeavor. Indeed, comparing “the effectiveness of accountable care systems and usual care on costs, processes of care, and outcomes for geographically defined populations of patients” is one of the Institute of Medicine’s 100 priorities for comparative effectiveness research.33 Capitation in various forms is anticipated to be an effective means of reducing future health care cost growth, particularly cost growth resulting from unnecessary care. While this report demonstrates that capitation is associated with lower procedure rates for angiography and PCI, the substantial geographic variation suggests that capitation alone will not lead to reductions in the wide variations seen in CV procedure use.
Table 2.
Comparison of CVRN Medicare Advantage Patients and Co-located Medicare Fee-for-service Patients
| Medicare Advantage* (n=878,339) | Medicare FFS* (n=5,013,650) | |
|---|---|---|
|
| ||
| Age | ||
| - 65–69 | 30 | 34 |
| - 70–74 | 24 | 20 |
| - 75–79 | 20 | 18 |
| - 80–84 | 15 | 14 |
| - 85–99 | 12 | 13 |
|
| ||
| Female gender | 55 | 57 |
|
| ||
| Non-black race | 94 | 93 |
|
| ||
| Diabetes | 21 | 24 |
|
| ||
| Hypertension | 62 | 61 |
|
| ||
| Hyperlipidemia | 44 | 50 |
|
| ||
| Prior Coronary Artery Disease | 13 | 19 |
|
| ||
| Proportion of angiographies performed as outpatients | 28 | 36 |
|
| ||
| Proportion of PCI performed as outpatients | 9 | 7 |
FFS – Fee for service; PCI – percutaneous coronary intervention; CVRN – Cardiovascular Research Network.
Data are percentages. All differences are statistically significant p<0.001.
Acknowledgments
Dr. Matlock was supported by a career development award from the National Institutes on aging (1K23AG040696). The project was supported by the National Heart Lung and Blood Institute and the Cardiovascular Research Network (U19 HL91179-01, 1RC2HL101666-01, and 1R01HL086919).
Footnotes
Dr. Matlock had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors have no conflicts of interest to declare.
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript
Reference List
- 1.Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the Future of Cardiovascular Disease in the United States. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 2.Matlock DD, Lucas FL, Malenka D, et al. Regional variation in the use of implantable cardioverter-defibrillators for primary prevention: results from the National Cardiovascular Data Registry. Circ Cardiovasc Qual Outcomes. 2011 Jan 1;4(1):114–21. doi: 10.1161/CIRCOUTCOMES.110.958264. [DOI] [PubMed] [Google Scholar]
- 3.Lucas FL, Sirovich BE, Gallagher PM, Siewers AE, Wennberg DE. Variation in Cardiologists’ Propensity to Test and Treat: Is It Associated With Regional Variation in Utilization? Circ Cardiovasc Qual Outcomes. 2010 May;3(3):253–60. doi: 10.1161/CIRCOUTCOMES.108.840009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wennberg DE, Birkmeyer JD, Birkmeyer NJO. The Dartmouth Atlas of Cardiovascular Health Care. Chicago: AHA Press; 1999. [Google Scholar]
- 5.Ko DT, Wang Y, Alter DA, et al. Regional variation in cardiac catheterization appropriateness and baseline risk after acute myocardial infarction. J Am Col Cardiol. 2008;51:716–723. doi: 10.1016/j.jacc.2007.10.039. [DOI] [PubMed] [Google Scholar]
- 6. [Accessed July 1, 2012.];The Dartmouth Atlas of Health Care. http://www.dartmouthatlas.org.
- 7.Zarabozo C, Harrison S. Payment Policy And The Growth Of Medicare Advantage. Health Aff. 2009;28:w55–w67. doi: 10.1377/hlthaff.28.1.w55. [DOI] [PubMed] [Google Scholar]
- 8.Bach PB. A Map to Bad Policy -- Hospital Efficiency Measures in the Dartmouth Atlas. N Engl J Med. 2010;362:569–574. doi: 10.1056/NEJMp0909947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson HV. Regional Variation: Only Moderately Interesting: A Word of Caution. Circ Cardiovasc Qual Outcomes. 2010;3:6–7. doi: 10.1161/CIRCOUTCOMES.109.927103. [DOI] [PubMed] [Google Scholar]
- 10.Barnato AE, Bost JE, Farrell MH, et al. Relationship between staff perceptions of hospital norms and hospital-level end-of-life treatment intensity. J Palliat Med. 2007;10:1093–1100. doi: 10.1089/jpm.2006.0258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.HMO Research Network. [Accessed July 1, 2012.]; http://www.hmoresearchnetwork.org/
- 12.Magid DJ, Gurwitz JH, Rumsfeld JS, Go AS. Creating a research data network for cardiovascular disease: the CVRN. Expert Rev Cardiov Ther. 2008;6:1043–1045. doi: 10.1586/14779072.6.8.1043. [DOI] [PubMed] [Google Scholar]
- 13.Go AS, Magid DJ, Wells B, et al. The Cardiovascular Research Network: a new paradigm for cardiovascular quality and outcomes research. Circ Cardiovasc Qual Outcomes. 2008;1:138–147. doi: 10.1161/CIRCOUTCOMES.108.801654. [DOI] [PubMed] [Google Scholar]
- 14.Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States, 2001–2008. JAMA. 2011;305:1769–1776. doi: 10.1001/jama.2011.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gordis L. Epidemiology. Amsterdam: Elsevier Science; 2004. [Google Scholar]
- 16.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 17.The Patient Protection and Affordable Care Act.
- 18.Bach PB. A Map to Bad Policy -- Hospital Efficiency Measures in the Dartmouth Atlas. N Engl J Med. 2010;362:569–574. doi: 10.1056/NEJMp0909947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cooper AL, Trivedi AN. Fitness memberships and favorable selection in Medicare Advantage plans. N Engl J Med. 2012;366:150–157. doi: 10.1056/NEJMsa1104273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fisher ES, Wennberg JE. Health care quality, geographic variations, and the challenge of supply-sensitive care. [Review] [23 refs] Perspect Biol Med. 2003;46:69–79. doi: 10.1353/pbm.2003.0004. [DOI] [PubMed] [Google Scholar]
- 21.Wennberg DE, Dikens JD, Soule DN, et al. The Relationship between the Supply of Cardiac Catheterization Laboratories, Cardiologists and the Use of Invasive Cardiac Procedures in Northern New England. J Health Serv Res Po. 1997;2:75–80. doi: 10.1177/135581969700200204. [DOI] [PubMed] [Google Scholar]
- 22.Sutherland JM, Fisher ES, Skinner JS. Getting Past Denial -- The High Cost of Health Care in the United States. N Engl J Med. 2009;361:1227–1230. doi: 10.1056/NEJMp0907172. [DOI] [PubMed] [Google Scholar]
- 23.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care.[see comment][summary for patients in Ann Intern Med. 2003 Feb 18;138(4):I36; PMID: 12585853] Ann Intern Med. 2003;138:273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 24.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care.[see comment][summary for patients in Ann Intern Med. 2003 Feb 18;138(4):I49; PMID: 12585852] Ann Intern Med. 2003;138:288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 25.Fowler FJ, Jr, Gallagher PM, Anthony DL, Larsen K, Skinner JS. Relationship between regional per capita Medicare expenditures and patient perceptions of quality of care. [see comment] JAMA. 2008;299:2406–2412. doi: 10.1001/jama.299.20.2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anthony DL, Herndon MB, Gallagher PM, et al. How much do patients’ preferences contribute to resource use? Health Aff. 2009;28:864–873. doi: 10.1377/hlthaff.28.3.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matlock DD, Peterson PN, Wang Y, et al. Variation in use of dual-chamber implantable cardioverter-defibrillators: results from the national cardiovascular data registry. Arch Intern Med. 2012 Apr 23;172(8):634–41. doi: 10.1001/archinternmed.2012.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lin CY, Farrell MH, Lave JR, Angus DC, Barnato AE. Organizational determinants of hospital end-of-life treatment intensity. Med Care. 2009;47:524–530. doi: 10.1097/MLR.0b013e31819261bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baker LC, Fisher ES, Wennberg JE. Variations In Hospital Resource Use For Medicare And Privately Insured Populations In California. Health Aff. 2008;27:w123–w134. doi: 10.1377/hlthaff.27.2.w123. [DOI] [PubMed] [Google Scholar]
- 30.Stiefel M, Feigenbaum P, Fisher ES. The dartmouth atlas applied to kaiser permanente: analysis of variation in care at the end of life. The Permanente Journal. 2008;12:4–9. doi: 10.7812/tpp/07-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGuire TG, Newhouse JP, Sinaiko AD. An economic history of Medicare part C. Milbank Q. 2011;89:289–332. doi: 10.1111/j.1468-0009.2011.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.The Institute of Medicine. Clinical Practice Guidelines: Directions for a New Program. 1990 [Google Scholar]
- 33.The Institute of Medicine. 100 Initial Priority Topics for Comparative Effectiveness Research. 2009 [Google Scholar]