Abstract
Purpose
The higher prevalence of respiratory allergic disease may be due to increased exposure to inhalation allergens. We conducted a survey of allergic diseases in autumn and winter with detection of major indoor allergens in major cities in Korea.
Methods
We enrolled 110 subjects from the fourth Korea National Health and Nutrition Examination Survey with stratified, cluster, and systematic sampling procedures. All participants answered a health questionnaire as well as underwent a skin prick test (SPT) and ImmunoCAP for 11 indoor major allergens. We also measured the levels of 5 major allergens (Der f 1, Der p 1, Can f 1, Bla g 1, and Asp f 1) in fine indoor dust from the houses of 60 subjects with a 2-site ELISA.
Results
The prevalence of allergic rhinitis and asthma were 25.5% and 7.3%, respectively. The most common sensitized allergens identified by SPT and ImmunoCAP were Dermatophagoides farinae (40.9%, 36.8%), followed by cockroach (23.6%, 19.5%), mugwort (13.6%, 22.9%), oak (9.1%, 22.9%), Japanese hop (9.1%, 8.6%), and dog dander (8.2%, 6.9%). There was a modest discrepancy between SPT and ImmunoCAP. Der f 1 and Der p 1 were detected in 91.7% and 45.0% of the enrolled houses, respectively. Der f 1 indicated high concentrations in all specific provinces in Korea; however, Der p 1 measured high only in the south. Dog dander allergens were present in 71.7% of houses; however, Bla g 1 was present in only 11.7% of houses and Asp f 1 was not detected in any houses.
Conclusions
The most important inhalant allergens in Korea are house dust mites followed by cockroach, mugwort, oak, Japanese hop, and dog dander in indoor environment, in which The dominant species of house dust mites were different according to region.
Keywords: Allergen, skin test, dust, indoor, Korea
INTRODUCTION
The global prevalence and economic burden of allergic diseases has increased.1,2,3,4,5 The prevalence of allergic rhinitis, allergic conjunctivitis and asthma are 38.7%, 18.3%, and 10.3%, respectively, in Korean school-aged children.1 For Korean adults, allergic rhinitis and asthma are 20.9% and 11.7%, respectively.6 Environmental factors are considered more crucial than genetic factors for the recent increase in the prevalence of allergic diseases.7 Environmental factors such as smoking, lifestyle, obesity, pets, diet, and air pollution are considered causative or augmenting factors of allergic diseases.8,9,10 House dust is an important indoor pollutant due to its inclusion of various indoor allergens such as house dust mites (HDM), animal dander, cockroach allergen, and adjuvant materials from microbiologic organisms such as chitin, endotoxins, and β-glucan.11 HDMs are the primary inhalant allergen,12,13,14 and about 60% of the Korean population is sensitized to HDM.6,15
The Korean National Health and Nutrition Examination Survey (KNHANES) has been conducted by the Korean Centers for Disease Control and Prevention since 1998 to compile basic resources for national health information; in addition, a Phase IV survey was conducted from 2007 to 2009. We conducted a nationwide survey in the autumn and winter in specific Korean localities to determine the distribution of allergic diseases and important indoor aeroallergens.
MATERIALS AND METHODS
Participants
This study applied stratified, cluster, and systematic sampling procedures to select enumeration districts based on population, housing data and enumeration district information from the 2005 Population and Housing Census. Stratification variables were region, dong (neighborhood), eup (town), myeon (township), and housing type. The sample composition was adjusted to be representative of the population; subsequently, sampling was conducted by dividing the population into 4 spheres split into 2 to 4 regions that formed 2 to 3 layers. Following the principle of a percentage quota for each layer, 200 samples were allocated to each. The allocated sample dong, eup, and myeon were extracted through probability sampling proportional to size based on the number of enumeration districts. We applied systematic sampling procedures to extract and investigate apartment and conventional dwelling enumeration districts based on the characteristics of the selected sample dong, eup, and myeon according to housing type. All 4,600 household members were included as research subjects. Among them, 219 general subjects were selected for the preliminary investigation after consultation with the Chronic Disease Investigation Division (the department initiating the research). Four spheres nationwide (Seoul, Busan, Gwangju, Daejeon, Daegu, Incheon, Jeonju, and Gyeonggi-do) were evenly included in the preliminary investigation; subsequently, the proportion of housing type was 3:2 for apartments and conventional dwellings (row houses) (Fig. 1).
Fig. 1.
A map of Korea presenting 4 spheres and specific 8 localities.
Among the 219 candidates, we invited 171 candidates who were 10 years of age or older to participate in this study. Among these, 110 candidates (in 60 families comprised of 36 apartment families and 24 detached house families) who understood the survey and volunteered to participate were enrolled in the allergic disease survey and SPT from November 3, 2009 to February 26, 2010. Among the 110 candidates, 12 candidates were under 18 years old (mean age 14.3 years). Candidates completed a health questionnaire that included information on the presence of allergic disease (such as asthma, allergic rhinitis, atopic dermatitis, and allergic conjunctivitis) and pet inhabitance. Atopy was defined by the presence of specific IgE to any 11 aeroallergens determined by SPT or ImmunoCAP.
Questionnaire survey for the presence of allergic diseases and indoor air condition
The KNHANES Phase IV questionnaire included questions on asthma and allergic rhinoconjunctivitis. We used an ISAAC survey questionnaire that included a KNHANES Phase IV questionnaire with questions on atopic dermatitis, drug allergy and pet inhabitance.9
Skin prick test
The allergy skin prick test (SPT) utilized 11 common aeroallergens (Allergopharma, Hamburg, Germany): D. farinae, D. pteronyssinus, cockroach, Alternaria, cat dander, dog dander, oak, birch, grass, mugwort, ragweed, and Japanese hop. We also included a positive control (1% histamine in saline with 0.3% phenol and 50% glycerol) and negative control (saline with 0.3% phenol and 50% glycerol). Candidates who had received antihistamines 7 days prior to the test were excluded from the SPT. The results were read 15 minutes after the SPT and a wheal larger than 3 mm (compared to the negative control) for each allergen was defined as positive.
Serum IgE measurement
We used the ImmunoCAP® system to measure the levels of specific IgE to 6 aeroallergens (D. farinae, Blattella germanica, dog dander, oak, mugwort and Japanese hop) in 110 participants. Results greater than 0.35 kU/L for specific IgE were defined as positive.
Protein extraction from house dust and major allergen measurements
House dust was collected from the bedclothes of candidates using the same vacuum cleaner (LG Electronics, Changwon, Korea) for 2 minutes per 1 m2 of bedding. The power of the vacuum was 500 W. Collected house dust (100 mg) was placed into 2 mL of borated buffered saline (pH 8.0) and extracted for 24 hours at 4℃ and then centrifuged. The supernatants were stored at -20℃ until measured. The levels of 5 major allergens in the supernatants were measured by a 2-site ELISA (INDOOR Biotechnologies Inc. [IBI], Charlottesville, Virginia, USA).
Statistical analysis
Statistical analyses were performed using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA). Variables were compared using a chi-square test. The concordance between the 2 methods was established using Kappa statistics and an A P value less than 0.05 was considered statistically significant.
RESULTS
Prevalence of respiratory allergic diseases and inhalant allergen sensitization determined by skin prick test or ImmunoCAP
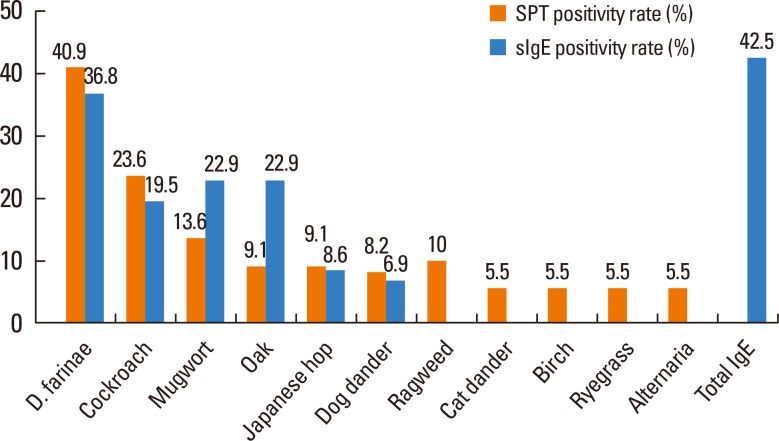
The prevalence of asthma and allergic rhinitis was 7.3% and 25.5%, respectively, which corresponded to the results of the previous study.6 Fig. 2 shows the sensitization rate to each allergen by SPT and ImmunoCAP IgE measurements. According to the SPT, the prevalence of atopy was 56%. The highest rates were observed in D. farinae (40.9%), followed by cockroach (23.6%), mugwort (13.6%), ragweed (10%), oak (9.1%), Japanese hop (9.1%), and dog dander (8.2%) by SPT. A total of 83.9% of total atopy patients were positive to D. farinae and/or cockroach and 94.6% of atopy patients were positive to either D. farinae, cockroach, oak, or Japanese hop. We measured 6 important inhalant allergens sIgE by ImmunoCAP. The most common sensitizers were D. farinae (36.8%), mugwort (22.9%), oak (22.9%), cockroach (19.5%), Japanese hop (8.6%), and dog dander (6.9%).
Fig. 2.
Positive rate to skin prick test and specific IgE determined by ImmunoCAP.
SPT, skin prick test; sIgE, specific immunoglobulin E; D. farina, Dermatophagoides farinae.
Concordance rate of SPT and ImmunoCAP
Table 1 shows the kappa statistics with concordance rates between SPT and ImmunoCAP tests. Only the kappa statistics of mugwort and D. farinae were higher than 0.6, and cockroach was 0.507. The value of other allergens such as dog dander (0.389) and oak (0.353) are not satisfactory for concordance and Japanese hop even indicated a negative value.
Table 1.
Kappa statistics showing the concordance rate of specific IgE and SPT for each allergen
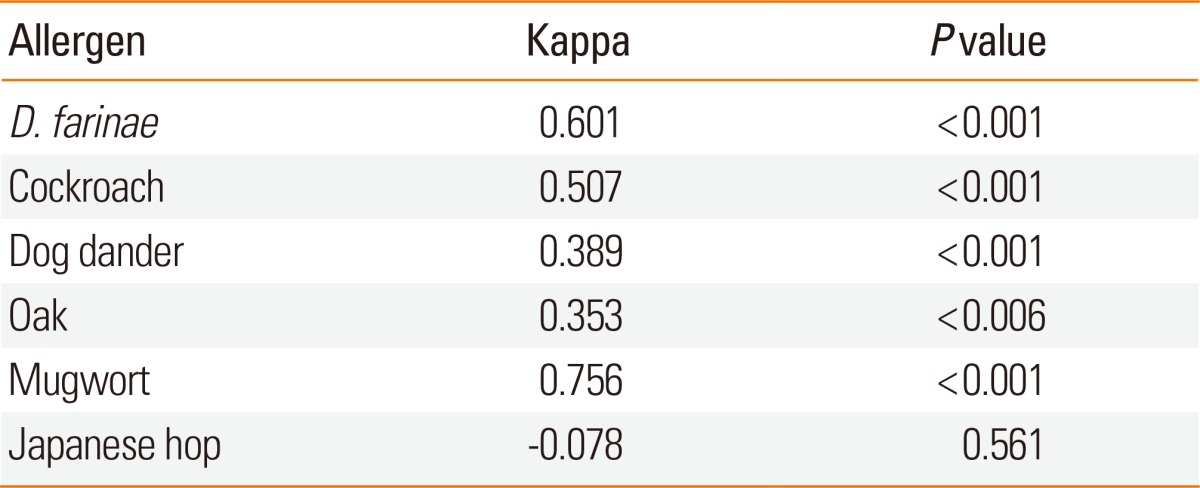
SPT, skin prick test; D. farina, Dermatophagoides farinae.
Inter-group analysis by atopy
We divided participants into 2 groups according to presence of atopy. There were no differences in age, sex, life style, presence of asthma, allergic rhinitis, allergic conjunctivitis, and atopic dermatitis as determined by the Korean version of ISAAC questionnaire (Table 2).
Table 2.
Clinical characteristics of the study subjects according to atopy status
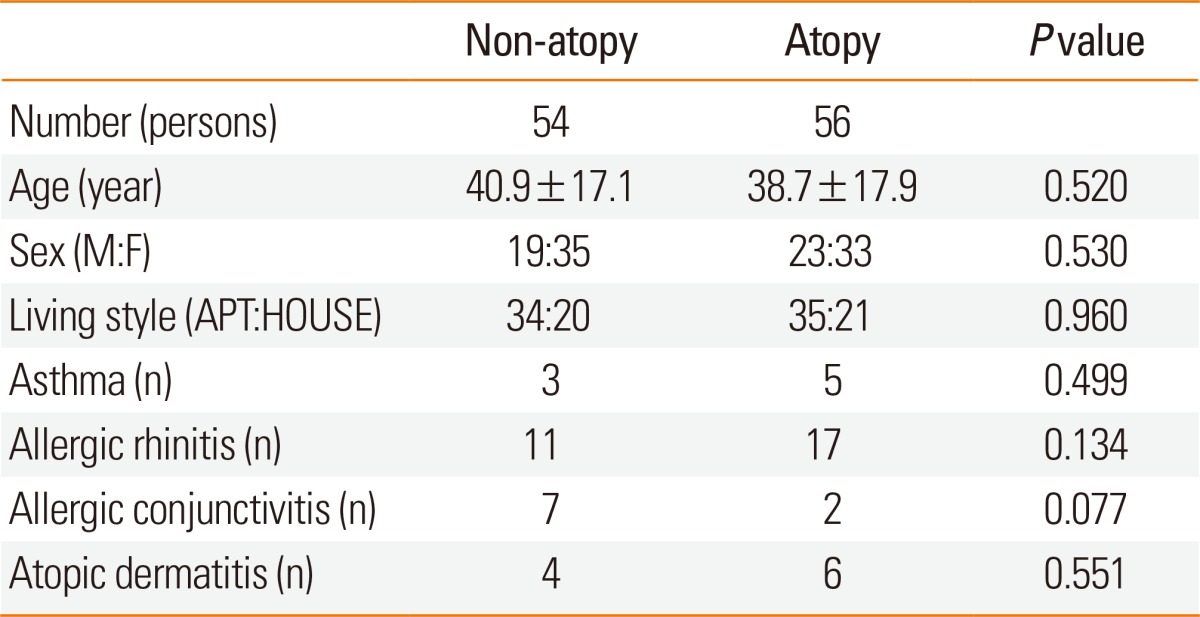
APT, apartment.
Detection of indoor major allergens in fine bedding dust
Table 3 shows the detection rates for 5 major allergens measured by a 2-site ELISA. Der f 1 in house dust was detected in 91.7% of enrolled houses and Der p 1 was detected in 45.0% of houses. Geographically, D. farinae was detected evenly nationwide; however, D. pteronyssinus was detected only in cities located in southern provinces such as Busan and Gwangju (Fig. 3).
Table 3.
Detection of major allergens in fine house dust (bedding)
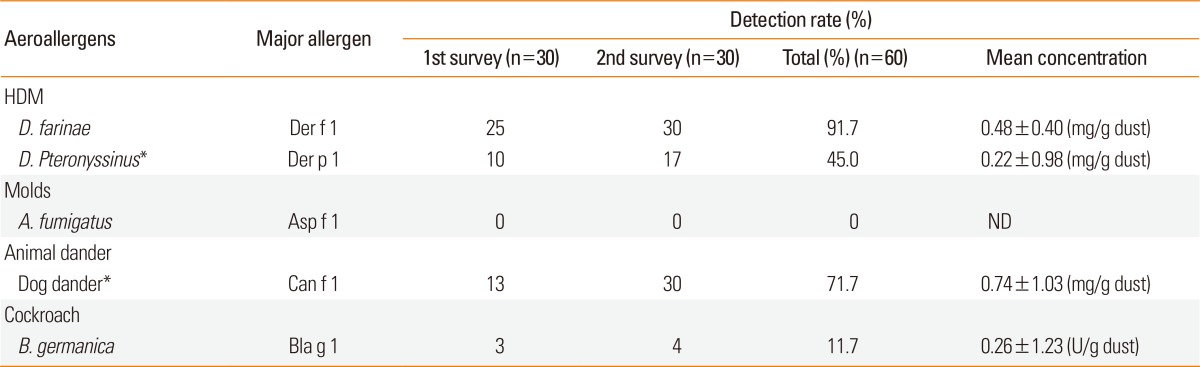
*P<0.05, significantly increased level in 2nd survey (winter) compared with 1st survey (late autumn).
HDM, house dust mite; D. farina, Dermatophagoides farinae; D. pteronyssinus, Dermatophagoides pteronyssinus; A. fumigates, Aspergillus fumigatus; B. germanica, Blattella germanica, ND, not detected.
Fig. 3.
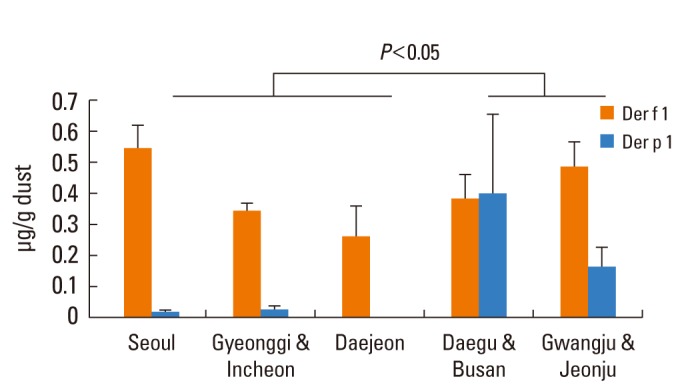
Nationwide geographical distribution of group 1 major allergens of house dust mites.
Can f 1 had higher rates in the 5 houses with dogs compared with houses without dogs (Fig. 4). Group 1 major allergen of Aspergillus fumigatus was not detected in any house.
Fig. 4.
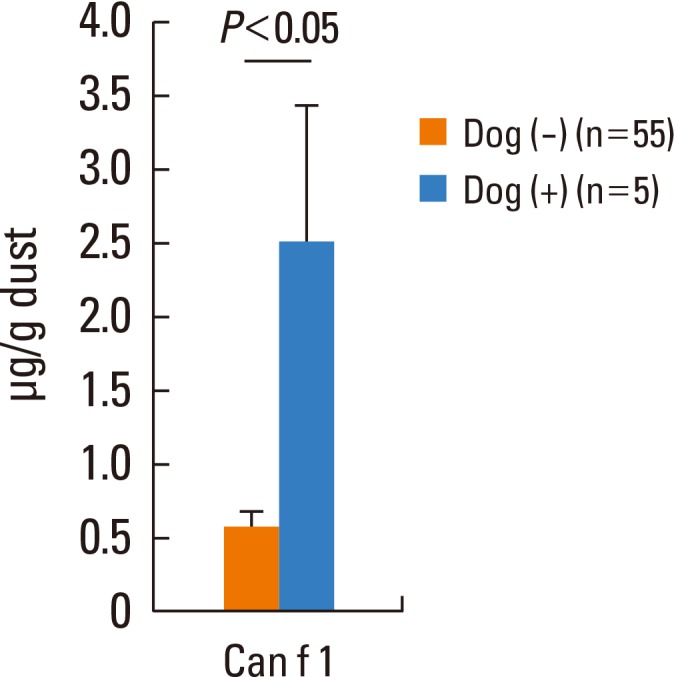
Group 1 major allergen of dog dander levels determined by a 2-site ELISA according to dog inhabitance.
DOG (+), Houses with dogs; DOG (-), Houses without dogs.
DISCUSSION
It is important to accurately investigate the prevalence of allergic diseases and the level of exposure to indoor allergens from indoor environments. However, the previous Phase 1-3 KNHNES was insufficient to determine the prevalence of allergic diseases or to determine the exposure from Korean domestic indoor environments. Therefore, we conducted a nationwide survey on allergic diseases in autumn and winter and the levels of indoor allergens using various diagnostic tools. The data showed that HDM, cockroach, mugwort, oak, Japanese hop, ragweed, and dog dander are important inhalant allergens in Korea. The number of households with pets has increased and pet inhabitancy has became one of the major risk factors for the development of allergic diseases.16 Grass is the most important global pollen; however, this study did not include grass pollen for the SPT and ImmunoCAP specific IgE measurement due to the low rate of exposure to grass pollen in Korea.17,18
The data indicated a significant discrepancy between the results of SPT and ImmunoCAP IgE measurement. The value of the agreement can be defined by the kappa value. Usually, a kappa value higher than 0.6 is considered a substantial or almost perfect concordance.19 Only the kappa value of mugwort and D. farinae was acceptable. Other allergens such as cockroach, oak, dog dander were not sufficient to assume concordance and an even a negative kappa value was found for (Table 1).
A SPT is time-consuming (taking about 30 minutes) and the results of the SPT depend on the investigator, drug history, and skin status. Investigators may inject the allergens in different ways and to various depths; consequently, the SPT may be inappropriate for large epidemiologic studies. The measurement of specific IgE in serum can be more appropriate as it is faster and does not depend on the investigator, drug history, or skin status. However, cost is a drawback of ImmunoCAP measurement in epidemiologic studies. There are various tools available to measure specific IgE. Multiplex measurement methods such as the multiple allergen simultaneous test, AdvanSure (LG Life Science, Daejeon), and RIDA (R-Biopharm, Germany) can measure 36-40 specific IgEs in serum simultaneously. However, the correlation and concordance rates between multiplex measurement and ImmunoCAP in some inhalant allergens are unsatisfactory because each test can vary in sensitivity and specificity.20,21 The measurement of specific IgEs by the ImmunoCAP system is highly sensitive, specific, and convenient; consequently, we recommend that laboratory tests include the ImmunoCAP system to measure specific IgE levels in serum.
This survey has some limitations. We diagnosed allergic diseases by a Korean version of the ISSAC questionnaire that is dependent on the memory of respondents. An accurate diagnosis of allergic diseases must be supplemented by in vivo or in vitro diagnostic procedures. In the present study, allergic conjunctivitis was more prevalent in the non-atopy group, which suggests that supplementary diagnostic tools or allergy specialist interview and physical examination are essential for accurate evaluation.
We conducted a 2-site ELISA to measure the levels of indoor aeroallergens using monoclonal antibodies. Monoclonal antibodies are epitope specific and may not detect all isoallergens of major allergens;22 consequently, this method has not yet been validated for the standardization of allergen extract.23,24 Measurement results are dependent of the type of 2-site ELISA kit; consequently, the Committee for Biologics Equivalent Research (CBER) of FDA use polyclonal antibodies for allergen standardization. Aspergillus fungus is ubiquitous and a well-known indoor fungus; however, we were unable to detect Asp f 1. This suggests that the exposure of Aspergillus fumigatus is not serious in Korea and may explain the low incidence of allergic bronchopulmonary aspergillosis in Korea.25
The level of aeroallergens can vary by geography. Fig. 2 shows that Der p 1 was only detected in a small number of houses in the middle province of Korea; however, the level of Der p 1 is similar to Der f 1in the southern part of the Korean peninsula and suggests that D. pteronyssinus is the co-predominant HDM with D. farinae in these areas. These results corresponded to a previous study that indicated that the presence of D. farinae was nationwide (Seoul 63.6%; Gwangju 63.6%, Busan 79.6%; Incheon 96.5%; Daejon 83.9%; Jeonju 87.2%, Chongju 95.2%); however, D. pteronyssinus was detected predominantly in Busan (Yongkwan-ub 72.5%, Yongdo 64.9%).26
Another limitation of the present survey is that it was conducted only in the autumn and winter; consequently, the levels of HDM, cockroach, and Aspergillus fumigatus allergens may be higher in the summer.27
Levels of allergens can vary by pet inhabitancy.28,29 There was no difference in Fel d 1 level between houses with cats and houses without; however, the results may be due to the small sample size of only 2 houses with cats. We may have obtained better results if more houses with cats had been included in the samples. Despite this limitation, Can f 1 and Fel d 1 were detected in 71.7% and 66.7% of total houses, respectively, which suggests that pet allergen plays a major role for the development of allergic diseases in Korea. The high detection rate of Can f 1 and Fel d 1 in houses without cats and dogs is caused by the physical characteristics of animal dander.30 Dog and cat dander easily spreads to other areas due to its easy adherence to clothes, carpet and furniture; consequently, Can f 1 and Fel d 1 can be detected in many houses without pets.31,32 So, pet ownership is not always correlated with the development of sensitization to pets.33
The present study represents a nationwide survey on allergic disease in autumn and winter in major cities in Korea. We propose an indoor aeroallergen and allergic disease survey model in accordance with the KNHANES and recommend an ImmunoCAP system to diagnose atopy and a 2-site ELISA test to measure aeroallergens in indoor environments.
Footnotes
There are no financial or other issues that might lead to conflict of interest.
References
- 1.Suh M, Kim HH, Sohn MH, Kim KE, Kim C, Shin DC. Prevalence of allergic diseases among Korean school-age children: a nationwide cross-sectional questionnaire study. J Korean Med Sci. 2011;26:332–338. doi: 10.3346/jkms.2011.26.3.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee SI, Shin MH, Lee HB, Lee JS, Son BK, Koh YY, Kim KE, Ahn YO. Prevalences of symptoms of asthma and other allergic diseases in korean children: a nationwide questionnaire survey. J Korean Med Sci. 2001;16:155–164. doi: 10.3346/jkms.2001.16.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beasley R, Ellwood P, Asher I. International patterns of the prevalence of pediatric asthma the ISAAC program. Pediatr Clin North Am. 2003;50:539–553. doi: 10.1016/s0031-3955(03)00050-6. [DOI] [PubMed] [Google Scholar]
- 4.Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, Gibson P, Ohta K, O'Byrne P, Pedersen SE, Pizzichini E, Sullivan SD, Wenzel SE, Zar HJ. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008;31:143–178. doi: 10.1183/09031936.00138707. [DOI] [PubMed] [Google Scholar]
- 5.Downs SH, Marks GB, Sporik R, Belosouva EG, Car NG, Peat JK. Continued increase in the prevalence of asthma and atopy. Arch Dis Child. 2001;84:20–23. doi: 10.1136/adc.84.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park HS, Choi GS, Cho JS, Kim YY. Epidemiology and current status of allergic rhinitis, asthma, and associated allergic diseases in Korea: ARIA Asia-Pacific workshop report. Asian Pac J Allergy Immunol. 2009;27:167–171. [PubMed] [Google Scholar]
- 7.Strachan DP. The role of environmental factors in asthma. Br Med Bull. 2000;56:865–882. doi: 10.1258/0007142001903562. [DOI] [PubMed] [Google Scholar]
- 8.The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet. 1998;351:1225–1232. [PubMed] [Google Scholar]
- 9.Ellwood P, Asher MI, Beasley R, Clayton TO, Stewart AW ISAAC Steering Committee. The international study of asthma and allergies in childhood (ISAAC): phase three rationale and methods. Int J Tuberc Lung Dis. 2005;9:10–16. [PubMed] [Google Scholar]
- 10.Hong SJ, Lee MS, Sohn MH, Shim JY, Han YS, Park KS, Ahn YM, Son BK, Lee HB Korean ISAAC Study Group. Self-reported prevalence and risk factors of asthma among Korean adolescents: 5-year follow-up study, 1995-2000. Clin Exp Allergy. 2004;34:1556–1562. doi: 10.1111/j.1365-2222.2004.02084.x. [DOI] [PubMed] [Google Scholar]
- 11.Jeong KY, Hong CS, Lee JS, Park JW. Optimization of allergen standardization. Yonsei Med J. 2011;52:393–400. doi: 10.3349/ymj.2011.52.3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Voorhorst R, Spieksma FT, Varekamp H, Leupen MJ, Lyklema AW. The house-dust mite (Dermatophagoides pteronyssinus) and the allergens it produces. Identity with the house-dust allergen. J Allergy. 1967;39:325–339. [Google Scholar]
- 13.Miyamoto T, Oshima S, Ishizaki T, Sato SH. Allergenic identity between the common floor mite (Dermatophagoides farinae Hughes, 1961) and house dust as a causative antigen in bronchial asthma. J Allergy. 1968;42:14–28. doi: 10.1016/0021-8707(68)90128-7. [DOI] [PubMed] [Google Scholar]
- 14.Jeong KY, Park JW, Hong CS. House dust mite allergy in Korea: the most important inhalant allergen in current and future. Allergy Asthma Immunol Res. 2012;4:313–325. doi: 10.4168/aair.2012.4.6.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee SY, Kwon JW, Seo JH, Song YH, Kim BJ, Yu J, Park KS, Kim H, Kim EJ, Lee JS, Hong SJ. Prevalence of atopy and allergic diseases in Korean children: associations with a farming environment and rural lifestyle. Int Arch Allergy Immunol. 2012;158:168–174. doi: 10.1159/000330820. [DOI] [PubMed] [Google Scholar]
- 16.Morris DO. Human allergy to environmental pet danders: a public health perspective. Vet Dermatol. 2010;21:441–449. doi: 10.1111/j.1365-3164.2010.00882.x. [DOI] [PubMed] [Google Scholar]
- 17.Oh JW, Kang IJ, Kim SW, Kook MH, Kim BS, Cheong JT, Lee HB. The association between the concentration of pollen and outbreak of pollinosis in childhood. Pediatr Allergy Respir Dis. 2009;19:4–11. [Google Scholar]
- 18.Oh JW, Lee HR, Kim JS, Lee KI, Kang YJ, Kim SW, Kook MH, Kang HY, Kim JS, Lee MH, Lee HB, Kim KE, Pyun BY, Lee SI, Han MJ. Aerobiological study of pollen and mold in the 10 states of Korea. Pediatr Allergy Respir Dis. 2000;10:22–33. [Google Scholar]
- 19.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 20.Lee YW, Sohn JH, Lee JH, Hong CS, Park JW. Allergen-specific IgE measurement with the IMMULITE 2000 system: intermethod comparison of detection performance for allergen-specific IgE antibodies from Korean allergic patients. Clin Chim Acta. 2009;401:25–32. doi: 10.1016/j.cca.2008.10.034. [DOI] [PubMed] [Google Scholar]
- 21.Lee JH, Park KH, Kim HS, Kim KW, Sohn MH, Kim CH, Lee JS, Hong CS, Park JW. Specific IgE measurement using AdvanSure® system: Comparison of detection performance with ImmunoCAP® system in Korean allergy patients. Clin Chim Acta. 2012;413:914–919. doi: 10.1016/j.cca.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 22.Park JW, Kim KS, Jin HS, Kim CW, Kang DB, Choi SY, Yong TS, Oh SH, Hong CS. Der p 2 isoallergens have different allergenicity, and quantification with 2-site ELISA using monoclonal antibodies is influenced by the isoallergens. Clin Exp Allergy. 2002;32:1042–1047. doi: 10.1046/j.1365-2222.2002.01421.x. [DOI] [PubMed] [Google Scholar]
- 23.van Ree R, Chapman MD, Ferreira F, Vieths S, Bryan D, Cromwell O, Villalba M, Durham SR, Becker WM, Aalbers M, André C, Barber D, Cistero Bahima A, Custovic A, Didierlaurent A, Dolman C, Dorpema JW, Di Felice G, Eberhardt F, Fernandez Caldas E, Fernandez Rivas M, Fiebig H, Focke M, Fötisch K, Gadermaier G, Das RG, Gonzalez Mancebo E, Himly M, Kinaciyan T, Knulst AC, Kroon AM, Lepp U, Marco FM, Mari A, Moingeon P, Monsalve R, Neubauer A, Notten S, Ooievaar-de Heer P, Pauli G, Pini C, Purohit A, Quiralte J, Rak S, Raulf-Heimsoth M, San Miguel Moncin MM, Simpson B, Tsay A, Vailes L, Wallner M, Weber B. The CREATE project: development of certified reference materials for allergenic products and validation of methods for their quantification. Allergy. 2008;63:310–326. doi: 10.1111/j.1398-9995.2007.01612.x. [DOI] [PubMed] [Google Scholar]
- 24.van Ree R. Indoor allergens: relevance of major allergen measurements and standardization. J Allergy Clin Immunol. 2007;119:270–277. doi: 10.1016/j.jaci.2006.10.033. [DOI] [PubMed] [Google Scholar]
- 25.Park JW, Kim HS, Byen JW, Koe SH, Hong YK, Kim CW, Choe K, Hong CS. The prevalence of allergic bronchopulmonary aspergillosis in asthmatics with positive skin reactivity to Aspergillus fumigatus antigens. Korean J Allergy. 1997;17:510–521. [Google Scholar]
- 26.Ree HI, Jeon SH, Lee IY, Hong CS, Lee DK. Fauna and geographical distribution of house dust mites in Korea. Korean J Parasitol. 1997;35:9–17. doi: 10.3347/kjp.1997.35.1.9. [DOI] [PubMed] [Google Scholar]
- 27.Kosik-Bogacka DI, Kalisinska E, Henszel L, Kuzna-Grygiel W. Seasonal dynamics of house dust mites in dust samples collected from sleeping places in north-western Poland. Zoonoses Public Health. 2012;59:8–15. doi: 10.1111/j.1863-2378.2011.01409.x. [DOI] [PubMed] [Google Scholar]
- 28.Medjo B, Atanaskovic-Markovic M, Nikolic D, Spasojevic-Dimitrijeva B, Ivanovski P, Djukic S. Association between pet-keeping and asthma in school children. Pediatr Int. 2013;55:133–137. doi: 10.1111/ped.12071. [DOI] [PubMed] [Google Scholar]
- 29.Smallwood J, Ownby D. Exposure to dog allergens and subsequent allergic sensitization: an updated review. Curr Allergy Asthma Rep. 2012;12:424–428. doi: 10.1007/s11882-012-0277-0. [DOI] [PubMed] [Google Scholar]
- 30.Ling M, Long AA. Pet dander and difficult-to-control asthma: therapeutic options. Allergy Asthma Proc. 2010;31:385–391. doi: 10.2500/aap.2010.31.3390. [DOI] [PubMed] [Google Scholar]
- 31.Berge M, Munir AK, Dreborg S. Concentrations of cat (Fel d1), dog (Can f1) and mite (Der f1 and Der p1) allergens in the clothing and school environment of Swedish schoolchildren with and without pets at home. Pediatr Allergy Immunol. 1998;9:25–30. doi: 10.1111/j.1399-3038.1998.tb00296.x. [DOI] [PubMed] [Google Scholar]
- 32.Patchett K, Lewis S, Crane J, Fitzharris P. Cat allergen (Fel d 1) levels on school children's clothing and in primary school classrooms in Wellington, New Zealand. J Allergy Clin Immunol. 1997;100:755–759. doi: 10.1016/s0091-6749(97)70269-0. [DOI] [PubMed] [Google Scholar]
- 33.Park YB, Mo EK, Lee JY, Kim JH, Kim CH, Hyun IG, Choi JH. Association Between Pet Ownership and the Sensitization to Pet Allergens in Adults With Various Allergic Diseases. Allergy Asthma Immunol Res. 2013;5:295–300. doi: 10.4168/aair.2013.5.5.295. [DOI] [PMC free article] [PubMed] [Google Scholar]