Abstract
Inguinal herniation of the urinary bladder is an extremely rare occurrence involving less than 5% of inguinal hernias reported in literature. These hernias require a high index of suspicion for their diagnosis and pose significant challenges to the operating surgeon. The majority of these hernias have been repaired by an open technique. We report two cases managed laparoscopically.
Keywords: Bladder, hernia, inguinoscrotal hernia, laparoscopic, repair, scrotal cystocele
INTRODUCTION
Inguinal herniation of the urinary bladder is a rare occurrence involving less than 5% of inguinal hernias reported in literature.[1,2] Any portion of the bladder can herniate ranging from a small diverticulum to the entire bladder itself which is also referred to as scrotal cystocele. Most of these hernias present as a groin swelling and can be asymptomatic or have profound symptomology. These hernias can pose significant challenges to the operating surgeon and demonstrate the importance of an adequate history, physical examination, and pre-operative planning in all patients.[3] In the majority of cases reported in literature, these hernias have been managed by an open approach. We present two cases of large inguinoscrotal hernias involving the urinary bladder which were managed by laparoscopic repair.
CASE REPORTS
Case 1 (Patient BL)
A 63-year-old male, heavy goods vehicle driver was referred by his general practitioner with a 5-month history of frequency of micturition and a right groin swelling. He reported that pressure exerted on the groin swelling made him void more urine after he had finished his initial void. On examination, the right groin swelling was indeed noted to decrease in size when compressed after voiding.
An ultrasound scan of the renal tract and right groin demonstrated a right inguinal hernia containing the urinary bladder [Figure 1a and b]. The findings were subsequently confirmed by a magnetic resonance imaging (MRI) scan of the abdomen and pelvis, which suggested a right inguinal hernia, containing a large bladder diverticulum [Figure 2]. At flexible cystoscopy, a large bladder diverticulum with a narrow neck was noted. The patient was offered an elective laparoscopic right inguinal hernia repair and excision of the bladder diverticulum.
Figure 1(a, b).
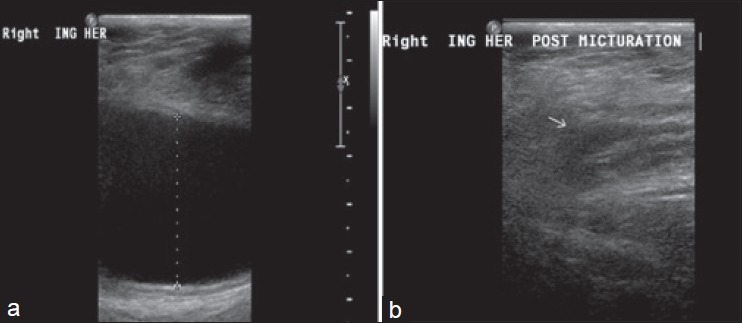
Ultrasound scan of the right groin demonstrating a right inguinal hernia containing the urinary bladder
Figure 2.

Magnetic resonance imaging showing bladder hernia
The procedure was performed under a general anesthetic with antibiotic prophylaxis. Four ports (2 × 12 mm and 2 × 5 mm excel bladeless trochars) were inserted after establishing pneumoperitoneum via Hassan's technique. Laparoscopy revealed a large direct right inguinal hernia containing the bladder diverticulum. Following right inguinal dissection, herniotomy was attempted via traction and external pressure. This was unsuccessful; therefore, a small incision was made laparoscopically in the conjoint tendon which enabled the hernia to be reduced.
The neck of the diverticulum was identified and confirmed by simultaneous flexible cystoscopy. The diverticulum was subsequently transected using a 35-cm harmonic scalpel (Ethicon harmonic ace). The bladder defect was closed with 4.0 vicryl in a continuous running suture. Flexible cystoscopy confirmed no leak of urine from the bladder following which an 18 Charriere silver-coated urethral catheter was inserted. A 10 × 15 cm Dacron mesh (Cousin Biotech) was tacked over the inguinal defect. This type of mesh was chosen due to concerns regarding the infection risk following opening of the bladder. A size 20 Robinsons drain was inserted. The bladder diverticulum was removed via the umbilical port which was subsequently closed with 1.0 PDS suture. Total operative time was 240 min. The patient had an uneventful post-operative stay and was discharged home after 6 days with an indwelling catheter.
Histology of the tissue revealed a portion of bladder mucosa, detrusor muscle, and attached fat measuring 130 × 112 × 30 mm. The specimen was therefore not a bladder diverticulum as had been suspected clinically. A cystogram performed 2 weeks later showed an intact bladder [Figure 3] following which the catheter was removed. He was noted to have a small scrotal hematoma at his 3-week follow-up appointment. This resolved spontaneously and he was discharged 6 months following his surgery.
Figure 3.

Post-operative cystogram
Case 2 (Patient GH)
A 73-year-old man was referred with an enlarging right groin swelling and urinary incontinence. An ultrasound scan of the scrotum 9 months earlier had demonstrated a right hydrocoele which was being managed conservatively. He had worn a truss for a right inguinal hernia in the early 1990s; however, on further investigation at that stage, a hernia could not be demonstrated and therefore no treatment was given.
On examination, a large mass was palpable in the right groin extending into the scrotum. The penis was buried within the scrotum and on retracting the foreskin and applying pressure to the right groin mass, urine was voided.
A urethral catheter was inserted draining a residual of 1000 ml clear urine. After catheterization, the right groin mass had significantly decreased in size. We suspected the right groin swelling represented a herniated bladder and this was confirmed by a cystogram [Figure 4]. Ultrasound scan of the renal tract demonstrated bilateral hydronephrosis; therefore, bilateral nephrostomies were inserted which were eventually converted to ureteric stents. He subsequently underwent laparoscopic bladder hernia repair.
Figure 4.

Pre-operative cystogram
The procedure was performed under general anesthesia with 1.5 g intravenous cefuroxime and 500 mg metronidazole prophylaxis. An 18 Charriere silver-coated urethral catheter was inserted at the start of the procedure. Four ports (1 × 12 mm, 1 × 10 mm, and 2 × 5 mm Excel bladeless trochars) were inserted after establishing pneumoperitoneum via Hassan's technique. Following incision of the peritoneum and right inguinal dissection, herniotomy was achieved via retraction and external pressure. A 12 × 15 cm Dacron mesh (Cousin Biotech) was tacked over the inguinal defect and a drain was not inserted as the bladder had not been opened. Total operative time was 120 min.
The patient had an uneventful post-operative recovery and was discharged after 3 days following a successful trial of void. His stents were removed 6 weeks after surgery and his serum creatinine was stable at 168 umol/L. He remained well and was discharged after 5 months.
DISCUSSION
Bladder hernias are an uncommon clinical finding. The first case was reported by Felix Platter in 1550 and there have subsequently been a number of published case series.[4] Most bladder hernias occur through the inguinal and femoral canals. These locations account for 75% and 23% of bladder containing hernias, respectively. The remainder herniate through the perineum, ischiorectal, obturator, and abdominal wall openings.[5,6]
Bladder hernias may be classified anatomically into extraperitoneal, paraperitoneal, and intraperitoneal depending on their relation to the peritoneum. The majority is extraperitoneal with the other types occurring infrequently.[4,7] A variety of etiologies have been described including ageing, obesity, urinary outlet obstruction, and loss of bladder tone with weakness of the supporting structures.[1,4]
Small bladder hernias are usually asymptomatic and discovered incidentally during surgery or during imaging studies performed for other purposes. Large inguinoscrotal hernias classically present with two-staged micturition in keeping with our first case. The first stage involves spontaneous voiding, whereas the second is due to manual pressure on the hernia. Reduction in size of the hernia after voiding, as was seen in both of our described cases, is also a common finding and raises the suspicion of a bladder hernia. Certain non-specific symptoms such as frequency, urgency, hematuria, and nocturia may also be encountered; however, it is difficult to dissociate similar symptoms arising from coexisting conditions such as bladder outlet obstruction or urinary tract infection.[1]
A number of associated complications have been described including sepsis, renal failure, unilateral or bilateral hydronephrosis, strangulation with ischemia or infarction of the bladder, vesicoureteric reflux, and cystolithiasis.[1,8] The finding of bilateral hydronephrosis as in our second case suggests bilateral ureteric involvement. This is a rare occurrence and requires treatment with bilateral nephrostomy insertion as retrograde stent insertion may be technically challenging.
The diagnosis is usually confirmed radiologically. Some authors suggest ultrasonography should be used to asses all large inguinoscrotal hernias in order to avoid intraoperative injuries.[9,10] Some authors have suggested the presence of a bladder hernia should be considered when fluid is found in the groin on an USS. However, Zajaczkowski et al. report that although USS is important for screening the upper urinary tract, it is poor at evaluating bladder containing scrotal hernias.[1,4]
Alternative radiological investigations such as computed tomography or MRI can add invaluable information during the pre-operative planning of these patients.[11,12,13] Both imaging modalities are particularly useful for evaluating the size, position, and contents of the hernial sac and to identify associated pathologies or complications such as hydronephrosis or strangulation.[14] Some authors have highlighted the ability of MRI to differentiate the different types of bladder hernias due to its superior soft tissue resolution and the ability to perform imaging in any plane as well as dynamic examinations during straining.[13] If these investigations are not readily available, a combination of a cystogram and flexible cystoscopy performed pre-operatively or intraoperatively, which can help further visualize structures and delineate anatomy adequately.[15] Cystoscopy is essential for assessing the lower urinary tract, urethral orifices, and bladder pathologies such as calculi or tumor.[4]
Appropriate pre-operative radiological and endoscopic evaluations are essential in the management of these hernias as inadvertent bladder injury is not uncommon during an unplanned attempted repair. Gomella et al. reported a 38% rate of unrecognized bladder injury in repair of large inguinoscrotal hernias. The post-operative complications of these injuries include sepsis, massive hematuria, and fistula formation.[5]
The most frequently reported surgical management of a herniated bladder is an open repair. Bjurlin et al. suggest that an inguinal incision permits an adequate approach to the bladder and hernial sac.[7,11] Helleman et al., in their approach, adopted the Bassini technique for repair of the hernia and argued against the use of a mesh in the presence of urine contaminated operative field.[8] Other authors recommend using a modified lichtenstein approach to repair the hernia. This approach involves reduction of the hernia followed by hernioplasty without transverse fascial tension, followed by mesh placement.[15,16] Bisharat et al. recommend that a bladder hernia found incidentally during herniorrhaphy should either be reduced back to its anatomic location in the space of Retzius or a selective resection of the herniated bladder component followed by standard inguinal hernia repair. These authors also advise that a bladder diverticulectomy should be undertaken if a large diverticulum or diverticular tumor is present.[1]
Both the patients discussed in our series underwent a laparoscopic repair of bladder hernias. Laparoscopy offers a number of advantages when compared to an open approach. Apart from improved visibility of the bladder and its surrounding structures, it assists in a more rapid recovery, lower analgesia requirements, and improved cosmesis. There are currently very few cases of laparoscopic repair of bladder hernias in the published literature. Our search of the medline and embase databases only identified two other cases utilizing a minimally invasive approach.
Valdivia et al. described a trans-pre-peritoneal laparoscopic approach using three ports to gain access to the hernia. After reintroducing the hernial components into the pelvic cavity, a polypropylene circular mesh was used to close the defect. The total operative time was 1 h and 30 min and the patient was discharged from hospital after 24 h resuming normal daily activities after 4 days.[17]
Similarly, Charuzi et al. also used a pre-peritoneal approach to repair a bladder hernia laparoscopically; however, they did not report any specific operative details such as number of ports used, operative time or post-operative length of stay.[18] Sung et al. describe their experience of a robotic repair of a bladder hernia which was undertaken as part of a robotic prostatectomy. They used a transperitoneal approach utilizing the da Vinci™ robot system. A GORE-TEXR, (W. L. Gore and Associates, Inc. Medical Products Division), soft tissue patch was used to repair the hernia. Total operative time was 200 min which reflects the total time for repair of the hernia and prostatectomy.[19]
CONCLUSION
Herniation of the urinary bladder is a rare clinical finding with a variety of potentially significant complications. A detailed history and physical examination are keys to diagnosis. Radiological and endoscopic assessments are extremely important components of the pre-operative management. Although most authors to date have employed an open approach to surgical repair, we have confirmed that these hernias can be managed safely laparoscopically with excellent post-operative outcomes. In centers where laparoscopic hernia repair is regularly performed, we feel it could eventually become the standard approach. Laparoscopy generally offers a short hospital stay compared to open surgery, lesser analgesia requirement, quicker to mobilize, and return to normal day-to-day activities.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Bisharat M, O’Donnell ME, Thompson T, MacKenzie N, Kirkpatrick D, Spence RA, et al. Complications of inguinoscrotal bladder hernias: A case series. Hernia. 2009;13:81–4. doi: 10.1007/s10029-008-0389-6. [DOI] [PubMed] [Google Scholar]
- 2.Levine B. Scrotal cystocele. J Am Med Assoc. 1951;147:1439–44. doi: 10.1001/jama.1951.73670320003013a. [DOI] [PubMed] [Google Scholar]
- 3.Angus LD, Cardoza S. Scrotal cystocele: A surgical pitfall. Br J Hosp Med (Lond) 2008;69:594. doi: 10.12968/hmed.2008.69.10.31324. [DOI] [PubMed] [Google Scholar]
- 4.Zajaczkowski T. Scrotal bladder hernia: Report of two cases. Int Urol Nephrol. 2007;39:479–84. doi: 10.1007/s11255-006-9028-2. [DOI] [PubMed] [Google Scholar]
- 5.Gomella LG, Spires SM, Burton JM, Ram MD, Flanigan RC. The surgical implications of herniation of the urinary bladder. Arch Surg. 1985;120:964–7. doi: 10.1001/archsurg.1985.01390320084018. [DOI] [PubMed] [Google Scholar]
- 6.Watson LF. Anatomy, etiology, symptoms, diagnosis, differential diagnosis, prognosis and treatment. 3rd ed. St. Louis: Mosby; 1948. Hernia; p. 32. [Google Scholar]
- 7.Bjurlin MA, Delaurentis DA, Jordan MD, Richter HM. Clinical and radiographic findings of a sliding inguinoscrotal hernia containing the urinary bladder. Hernia. 2010;14:635–8. doi: 10.1007/s10029-009-0597-8. [DOI] [PubMed] [Google Scholar]
- 8.Helleman JN, Willemsen P, Vanderveken M, Cortvriend J, Van Erps P. Incarcerated vesico-inguinal hernia: A case report. Acta Chir Belg. 2009;109:815–7. doi: 10.1080/00015458.2009.11680547. [DOI] [PubMed] [Google Scholar]
- 9.Oruç MT, Akbulut Z, Ozozan O, Coşkun F. Urological findings in inguinal hernias: A case report and review of the literature. Hernia. 2004;8:76–9. doi: 10.1007/s10029-003-0157-6. [DOI] [PubMed] [Google Scholar]
- 10.Catalano O. US evaluation of inguinoscrotal bladder hernias: Report of three cases. Clin Imaging. 1997;21:126–8. doi: 10.1016/s0899-7071(96)00018-6. [DOI] [PubMed] [Google Scholar]
- 11.Pasquale MD, Shabahang M, Evans SR. Obstructive uropathy secondary to massive inguinoscrotal bladder herniation. J Urol. 1993;150:1906–8. doi: 10.1016/s0022-5347(17)35931-1. [DOI] [PubMed] [Google Scholar]
- 12.Izes BA, Larsen CR, Izes JK, Malone MJ. Computerized tomographic appearance of hernias of the bladder. J Urol. 1993;149:1002–5. doi: 10.1016/s0022-5347(17)36280-8. [DOI] [PubMed] [Google Scholar]
- 13.Bernaerts A, de Beeck BO, Hoekx L, Parizel PM. Paraperitoneal indirect inguinal bladder hernia: MR demonstration. Abdom Imaging. 2005;30:685–8. doi: 10.1007/s00261-005-0316-6. [DOI] [PubMed] [Google Scholar]
- 14.Kuo WY, Lin TY, Lee WJ. Urinary bladder hernia: An unusual presentation of abdominal pain. Emerg Med J. 2010;27:489. doi: 10.1136/emj.2009.074195. [DOI] [PubMed] [Google Scholar]
- 15.Wagner AA, Arcand P, Bamberger MH. Acute renal failure resulting from huge inguinal bladder hernia. Urology. 2004;64:156–7. doi: 10.1016/j.urology.2004.03.040. [DOI] [PubMed] [Google Scholar]
- 16.Peiró F, Zaragozá C, Castaño S, Olavarrieta L, García-Aguado R, Vivó M. Giant inguino-scrotal bladder hernia. Report of a case. Ambul Surg. 2001;9:23–4. doi: 10.1016/s0966-6532(00)00068-8. [DOI] [PubMed] [Google Scholar]
- 17.Valdivia Uría JG, Valle Gerhold J. Preperitoneal laparoscopic bladder hernia repair. J Urol. 1995;154:1127–8. doi: 10.1016/s0022-5347(01)66996-9. [DOI] [PubMed] [Google Scholar]
- 18.Charuzi I, Mogutin B, Alis M, Kyzer S. Laparoscopic repair of inguinoscrotal hernia with complete herniation of the urinary bladder. Hernia. 2000;4:167–9. [Google Scholar]
- 19.Sung ER, Park SY, Ham WS, Jeong W, Lee WJ, Rha KH. Robotic repair of scrotal bladder hernia during robotic prostatectomy. J Robotic Surg. 2008;2:209–11. doi: 10.1007/s11701-008-0108-4. [DOI] [PubMed] [Google Scholar]


