Abstract
A 49-year-old man following a road traffic accident (RTA) had an unstable pelvic fracture with urethral injury. Internal pelvic fixation with Supra-pubic catheter (SPC) drainage of his bladder was done. This failed to stop the bleeding and a pelvic angiography with bilateral internal iliac embolization using steel coils was performed successfully controlling the bleeding. After 4 weeks, the patient developed wound infection (Clavien Grade III) and on exploration, bladder necrosis was found. A urinary diversion using ileal conduit with excision of bladder was performed. A biopsy of the excised bladder confirmed bladder necrosis with a foreign material (coil) in one arterial lumen.
Keywords: Bladder necrosis, embolization, internal iliac artery, pelvic fracture
INTRODUCTION
Transcatheter arterial embolization (TAE) is an established, well-recognized, and life-saving method of controlling intractable hemorrhage in pelvic fractures.[1,2,3] Despite a clearly defined role, complications profile of this procedure remains unpredictable and often undesirable. Necrosis of the target organ such as gluteal muscle necrosis,[4] avascular necrosis of femur,[5] sciatic palsy, deep sepsis, bowel infarction,[2] and bladder necrosis[6,7,8] have been reported in the literature.
Urinary bladder necrosis has been an extremely uncommon and devastating complication of arterial embolization. Only three previous cases have been reported [Table 1]. We report a case of bladder necrosis following embolization of internal iliac artery for uncontrolled bleeding in a patient with pelvic fracture. It usually presents after 4 weeks of internal iliac artery embolization, and a high index of suspicion is required in detecting the early and non-specific signs of bladder necrosis and urgent surgical intervention is needed.
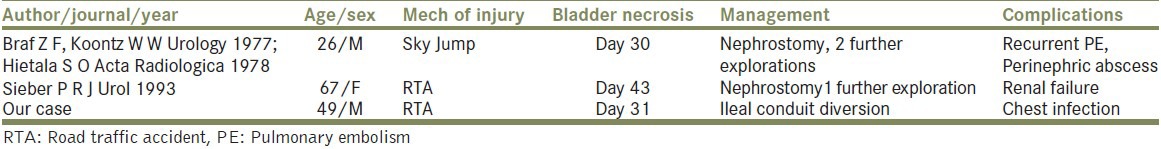
Table 1.
Cases of bladder necrosis following pelvic fracture embolization in literature
CASE REPORT
A 49-year-old man was brought in the accident and emergency department following a road traffic accident (RTA). During the initial resuscitation the patient was noted to have an unstable pelvic fracture along with urethral injury, but there was no intra-abdominal injury. Internal pelvic fixation was performed in theatre along with supra-pubic catheter (SPC) drainage of his bladder for his urethral disruption. Pelvic fixation failed to stop the bleeding and the patient was then taken to the interventional radiology suite. A pelvic angiography and bilateral internal iliac embolization using steel coils were performed which successfully controlled the bleeding.
After 4 weeks of embolization the patient developed wound infection at the site of SPC drainage. On exploration of wound bladder necrosis was noted [Figure 1] and a urinary diversion using ileal conduit with excision of bladder was performed. A biopsy of the excised bladder confirmed bladder necrosis along with a foreign material (coil) in one arterial lumen consistent with embolization [Figure 2]. Two weeks later, the patient developed chest infection and subsequently died from acute respiratory distress syndrome.
Figure 1.

Operative photograph of the necrotic bladder
Figure 2.
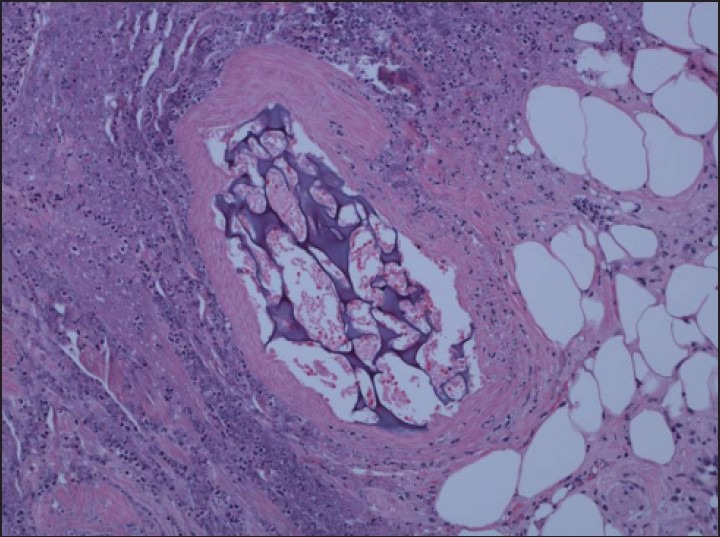
Foreign body (coil) in the arteriole lumen with adjacent necrotic bladder, (H and E) magnification power x400
DISCUSSION
Bladder necrosis following embolization for pelvic fracture is rare and so far only three cases (2 of them for the same patient). All previous cases, including our case, were secondary to embolization following trauma. Necrosis can occur with unilateral internal iliac embolization as mentioned in previous case reports[6,7,8] or bilateral embolizations as was seen in our case. Two to three percent of all pelvic fractures require embolization to control hemorrhage.[1,3] Pelvic angiography and embolization are an effective method to control bleeding in emergency situations with a reported success of 90-100%.[9] Bladder necrosis has also been reported following hydrodistention, radiation exposure, infection, carcinoma, or iatrogenic damage to the bladder vascular supply.[10,11,12,13]
The blood supply of bladder is mainly from the anterior division of internal iliac artery via the superior and inferior vesical artery, obturator and inferior gluteal artery and in females additionally via the uterine and vaginal arteries. Although bladder has a good collateral circulation and can withstand vascular insult well, rarely embolization of the main feeding artery results in ischemia and gangrene. To reduce the risk of ischemic necrosis identification of the bleeding vessel and selective embolization is recommended.
The main stay of management of bladder necrosis involves urinary diversion either via bilateral nephrostomies or an ileal conduit urostomy. Following nephrostomy and urethral catheter drainage for 7-9 weeks the bladder had healed in both cases.[6,8] Sieber et al. mention debridement of necrotic tissue and bladder repair due to extra-peritoneal bladder rupture, which did not work, and their patient subsequently required urinary diversion via bilateral nephrostomies.
The mortality from pelvic fractures is up to 15%, but in patients requiring embolization it is between 20 and 47%.[1,3,8] This rise in mortality is due to associated multiple injuries with a hemodynamically compromised unstable patient. Agolini and co-workers recommend embolization within 3 h of arrival and establishing the presence of collaterals during angiography for a mortality of <15%.
CONCLUSION
Bladder necrosis is an extremely rare complication of pelvic embolization, but should be kept in mind especially in cases of pelvic trauma. It presents after a few weeks and is best managed by initial urinary diversion for 8-10 weeks after which a cystogram should be done to rule out extravasation from bladder, which usually heals during this time.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Cook RE, Keating JF, Gillespie I. The role of angiography in the management of haemorrhage from major fractures of the pelvis. J Bone Joint Surg Br. 2002;84:178–82. doi: 10.1302/0301-620x.84b2.12324. [DOI] [PubMed] [Google Scholar]
- 2.Perez JV, Hughes TM, Bowers K. Angiographic embolisation in pelvic fracture. Injury. 1998;29:187–91. doi: 10.1016/s0020-1383(97)00175-7. [DOI] [PubMed] [Google Scholar]
- 3.Agolini SF, Shah K, Jaffe J, Newcomb J, Rhodes M, Reed JF., 3rd Arterial embolization is a rapid and effective technique for controlling pelvic fracture hemorrhage. J Trauma. 1997;43:395–9. doi: 10.1097/00005373-199709000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Takahira N, Shindo M, Tanaka K, Nishimaki H, Ohwada T, Itoman M. Gluteal muscle necrosis following transcatheter angiographic embolisation for retroperitoneal haemorrhage associated with pelvic fracture. Injury. 2001;32:27–32. doi: 10.1016/s0020-1383(00)00098-x. [DOI] [PubMed] [Google Scholar]
- 5.Obaro RO, Sniderman KW. Case report: Avascular necrosis of the femoral head as a complication of complex embolization for severe pelvic haemorrhage. Br J Radiol. 1995;68:920–2. doi: 10.1259/0007-1285-68-812-920. [DOI] [PubMed] [Google Scholar]
- 6.Sieber PR. Bladder necrosis secondary to pelvic artery embolization: Case report and literature review. J Urol. 1994;151:422. doi: 10.1016/s0022-5347(17)34969-8. Review. [DOI] [PubMed] [Google Scholar]
- 7.Braf ZF, Koontz WW., Jr Gangrene of bladder. Complication of hypogastric artery embolization. Urology. 1977;9:670–1. doi: 10.1016/0090-4295(77)90319-3. [DOI] [PubMed] [Google Scholar]
- 8.Hietala SO. Urinary bladder necrosis following selective embolization of the internal iliac artery. Acta Radiol Diagn (Stockh) 1978;19:316–20. doi: 10.1177/028418517801900204. [DOI] [PubMed] [Google Scholar]
- 9.Wong YC, Wang LJ, Ng CJ, Tseng IC, See LC. Mortality after successful transcatheter arterial embolization in patients with unstable pelvic fractures: Rate of blood transfusion as a predictive factor. J Trauma. 2000;49:71–5. doi: 10.1097/00005373-200007000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Grossklaus DJ, Franke JJ. Vesical necrosis after hydrodistension of the urinary bladder in a patient with interstitial cystitis. BJU Int. 2000;86:140–1. doi: 10.1046/j.1464-410x.2000.01739.x. [DOI] [PubMed] [Google Scholar]
- 11.Pandey A, Beier J, Dobkowicz L, Wolf S, Keller H. Extensive necrosis of the bladder with hypostatic abscess: A late complication after radiotherapy. Onkologie. 2010;33:116–8. doi: 10.1159/000277763. [DOI] [PubMed] [Google Scholar]
- 12.Porcu G, Roger V, Jacquier A, Mazouni C, Rojat-Habib MC, Girard G, et al. Uterus and bladder necrosis after uterine artery embolisation for postpartum haemorrhage. BJOG. 2005;112:122–3. doi: 10.1111/j.1471-0528.2005.00306.x. [DOI] [PubMed] [Google Scholar]
- 13.Nabi G, Sheikh N, Greene D, Marsh R. Therapeutic transcatheter arterial embolization in the management of intractable haemorrhage from pelvic urological malignancies: Preliminary experience and long-term follow-up. BJU Int. 2003;92:245–7. doi: 10.1046/j.1464-410x.2003.04328.x. [DOI] [PubMed] [Google Scholar]


