Abstract
Purpose
Few studies of sport-related traumatic brain injury (TBI) are population-based or rely on directly observed data on cause, demographic characteristics, and severity. This study addresses the epidemiology of sport-related TBI in a large population.
Methods
Data on all South Carolina hospital and emergency department encounters for TBI, 1998–2011, were analyzed. Annual incidence rate of sport-related TBI was calculated, and rates were compared across demographic groups. Sport-related TBI severity was modeled as a function of demographic and TBI characteristics using logistic regression.
Results
A total of 16,642 individuals with sport-related TBI yielded an average annual incidence rate of 31.5/100,000 population with a steady increase from 19.7 in 1998 to 45.6 in 2011. The most common mechanisms of sport-related TBI were kicked in football (38.1%), followed by fall injuries in sports (20.3%). Incidence rate was greatest in adolescents ages 12–18 (120.6/100,000/persons). Severe sport-related TBI was strongly associated with off-road vehicular sport (odds ratio [OR], 4.73; 95% confidence interval [95% CI], 2.92–7.67); repeated head trauma (OR, 4.36; 95% CI, 3.69–5.15); equestrian sport (OR, 2.73; 95% CI, 1.64–4.51); and falls during sport activities (OR, 2.72; 95% CI, 1.67–4.46).
Conclusions
The high incidence of sport-related TBI in youth, potential for repetitive mild TBI, and its long-term consequences on learning warrants coordinated surveillance activities and population-based outcome studies.
Keywords: Sport-related TBI, Severity, Concussion, Mechanism of injury, Repetitive TBI
Introduction
Each year, 1.7 million Americans experience traumatic brain injury (TBI), with 275,000 hospitalizations and 52,000 deaths occurring as a result [1]. TBI, including concussion, can lead to chronic and long-term disability [2]. Population-based studies indicate ~40% of TBI survivors developed persistent functional deficits within a year [3,4]. Population-based studies of sports and recreation-related TBI (sport-TBI) are sparse and yield equivocal results. For example, incidence rates of sport-TBI derived from data sources that are not representative of the base population yield widely discrepant annual estimates ranging from 2.6/100,000 to 124/100,000 population [5,6]. Differing target populations and case ascertainment criteria resulted in wide variation in estimates, and risk factors for severity of sport-TBI are inadequately evaluated [7]. Most published studies are based on self-report from household surveys, various data sources lacking uniform variable definition, or targeted surveys from athletics programs in high schools and colleges [8–11].
Many studies of sport-TBI focused on professional athletes, high school, and college players; specific types of sport; or specific TBI type (mainly concussions) and relied on reports of coaches, athletic trainers, and trained observers with emphasis on evaluating kinematics and time elapsing before returning to play [10–17]. These studies report incidence rates based on exposure time and play seasons as the denominator, which hamper comparability with population-based rate estimates [18]. Nonetheless, the greater incidence of concussion in contact sports such as football and rugby, gender differences as a function of the type of sport, and greater risk of TBI with repetitiveness of head trauma have been reported from these studies [10,15,16,18–21].
Although the estimates of sport-TBI in the literature vary widely, researchers agree on the increasing trend during the past 20 years [19,20,22]. This trend may be attributed to (1) increased case detection because of heightened awareness of the deleterious effects of concussions and mild TBI on memory and behavior; (2) stricter regulation in reporting sport injuries; and (3) increased awareness of the beneficial effects of physical activity in health-seeking behavior, in turn promoting greater participation in sport activities and free plays in communities [20,22–24].
Our study addresses gaps in the literature of sport-TBI by using data from an ongoing surveillance program of central nervous system trauma that receives detailed information on all clinical encounters in a statewide population with uniform coding criteria and data definitions. The study used external cause of injury codes (E-codes) specific to sport injuries, in combination with E-codes that indicate places of occurrence to arrive at a conservative but reasonably accurate population-based incidence rates in a statewide population. Specifically, we examined the mechanisms by which injuries occurred, TBI type, frequency of TBI (repetitiveness), and severity of TBI to identify high-risk population groups. The study hypothesizes that persons with previous TBI and older individuals are more likely to have severe sport-TBI than those without any evidence of previous TBI and youngest age group.
Methods
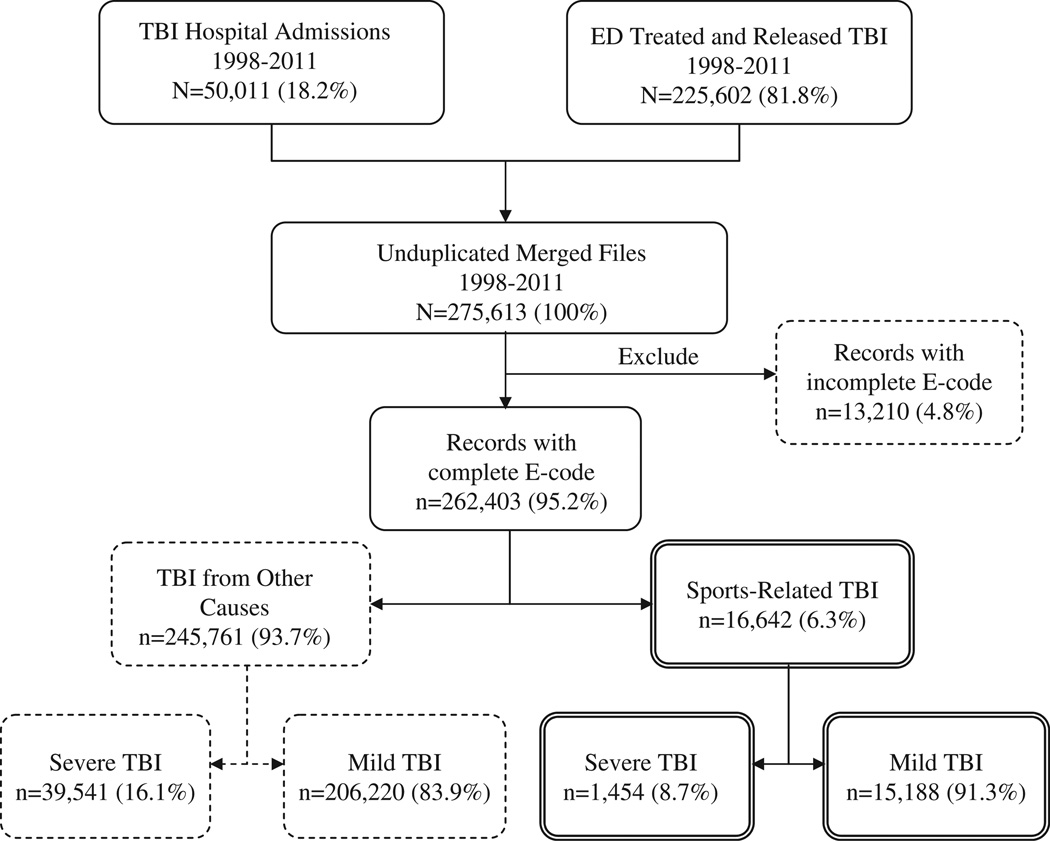
Data sources used for this study are from an ongoing surveillance activity of TBI in South Carolina put in place since 1996. All 65 nonfederal hospitals and 67 emergency departments (ED) that provide health services to the civilian population of the state are included. Self-standing private physician offices and urgent care facilities are not included. Detailed information about the surveillance system and the data inventory are found at http://academicdepartments.musc.edu/sctbifr/survey.htm. E-code completion rates of the TBI surveillance system are 95.2% and 92% for primary and secondary E-codes, respectively. Data, including person identifiers, were obtained on all persons evaluated in the ED or hospitalized for TBI from January 1, 1998, through December 31, 2011. TBI cases were ascertained through use of the International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) [25] diagnosis codes 800–801, 803–804, 850–854, and 959.01 [26]. We excluded patients coded for late effects of TBI (905.0, 907.0), repeat admissions for the same TBI, and observations with missing primary E-codes (Fig. 1). The TBI surveillance system incorporates a data evaluation protocol in which 12% and 30% of ED and hospital records on TBI are abstracted to ascertain the diagnosis and acquire additional information. The Medical University of South Carolina Institutional Review Board approved this study. Sport-relatedness of TBI was ascertained based on E-codes with mention of sport activities (Table 1). For ambiguous causes, such as “falls” or “struck by/struck against,” TBI was considered sports-related if the injury occurred in places of sports (stadium, gymnasium, tennis court, etc.).
Fig. 1.
Flowchart of identification of persons with sports-related TBI, South Carolina ED and hospital discharge, 1998–2011.
Table 1.
ICD-9-CM codes used in sports-related TBI and types of brain injuries, South Carolina ED and hospital discharges
| ICD-9-CM codes | Description | Count (N = 16,642) | Percent |
|---|---|---|---|
| A. Mechanism of injury code (E-code) | |||
| E886.0 | Tackles in sports, collision with another person | 606 | 3.6 |
| E917.0 | Kicked or struck by in sport (football/rugby) | 6335 | 38.1 |
| E917.5, [E917.9 with E849.4]* | Striking against/struck by in sports; struck by (in place of sport) | 1808 | 10.9 |
| E828.2 | Horseback rider injury (Equestrian sport) | 1531 | 9.2 |
| E821.0–821.1, E821.8–821.9 | Off highway motorized vehicles (ATVs and RUVs) | 2684 | 16.1 |
| [E919.8 with E849.4]* | Power-sport and recreational machinery used (in place of sport) | ||
| E885.0–885.4 | Fall from rollerblades, skateboard, scooter, ski, snowboard | ||
| E884.0–884.1 | Fall from playground equipment, fall from a cliff (in hiking) | 3385 | 20.3 |
| [E886.9 with E849.4]* | Fall from collision with another person (in place of sport) | ||
| [E888.0–.1, 888.8–.9 with 849.4]* | Falls all other (in place of sport) | ||
| E830–838 (.4 and .5) | Water sports and recreational activities | 293 | 1.8 |
| E910–910 (.0–.2), E917.2 | Drowning/submersion/running water injury (Detail shaded area) | ||
| E883.0 | Injuries from diving/jumping into water (swimming pool) | ||
| E830.4–830.5 | Injuries from watercraft causing submersion to skier/swimmer | ||
| E831.4–831.5 | Injuries from collision/being hit by watercraft to skier/swimmer | ||
| E832.4–832.5 | Submersion/drowning in water transport injuring skier/swimmer | ||
| E833.4–833.5 | Fall on stairs or ladders in water transport injuring skier/swimmer | ||
| E834.4–834.5 | Fall from one level to another injuring skier/swimmer | ||
| E835.4–835.5 | Other and unspecified fall in water transport skier/swimmer | ||
| E836.4–836.5 | Machinery accident in water transport injuring skier/swimmer | ||
| E837.4–837.5 | Explosion fire or burning in watercraft injuring skier/swimmer | ||
| E838.4–838.5 | Water skiing and Diving with/without equipment | ||
| E910.0–910.2 | Drowning and submersion in skiing and other sport activities | ||
| E917.2 | Striking against in running water (Kayaking, whitewater rafting) | ||
| B. Nature of injury codes (N-code) | |||
| 850.0–850.5, 850.9 | Concussions without intracranial hemorrhage, laceration, or contusion | 8191 | 49.2 |
| 854.0–854.1 | Unspecified intracranial and brain injuries without skull fracture | 160 | 1.0 |
| 851.0–853.3 | Intracranial hemorrhage, laceration, contusion without skull fracture | 616 | 3.7 |
| 800.0–801.9, 803.0–804.9 | Skull fractures with/without intracranial injury | 888 | 5.3 |
| 959.01 | Head injury, unspecified | 6787 | 40.8 |
ATV = all-terrain vehicle; ED = emergency department; ICD-9-CM = International Classification of Diseases, 9th revision, Clinical Modification; RUV = recreational utility vehicle; TBI = traumatic brain injury.
Mechanism codes in brackets do not mention sports. These codes are considered sports-related when the events occurred in place of sports E849.4. Italicized emphasis added.
Definitions
The dependent variable, TBI severity, was determined by translating diagnosis codes into the Abbreviated Injury Scale (AIS) of the head region and dichotomized into mild (AIS = 2) or severe (AIS = 3–6) [27] via the use of ICDMAP software [28]. AIS derived from translation of diagnosis codes exhibited very good interrater reliability and validity [29,30]. Mechanism of injury was categorized on the basis of E-codes as shown in Table 1, section A. Although TBI in bicyclists is common, ICD-9-CM coding does not allow distinguishing between transport-related and sport-related TBI; therefore, bicycling is not included in these analyses. TBI type was classified on the basis of the ICD-9-CM diagnosis codes (Table 1, section B). Demographic variables were categorized as shown in Table 2.
Table 2.
Characteristics of persons with sport-related TBI, South Carolina ED and hospital discharges
| Total | Injury severity | ||
|---|---|---|---|
| Severe | Mild | ||
| N = 16,642 (%) | n = 1454 (%) | n = 15,188 (%) | |
| Mechanism of injury (E-code) | |||
| Tackled during sports | 606 (3.6) | 19 (1.3) | 587 (3.9) |
| Kicked during football | 6335 (38.1) | 422 (29.0) | 5913 (38.9) |
| Struck during sports | 1808 (10.9) | 77 (5.3) | 1731 (11.4) |
| Fell during sports | 3385 (20.3) | 248 (17.1) | 3137 (20.7) |
| Equestrian | 1531 (9.2) | 198 (13.6) | 1333 (8.8) |
| Off-road vehicular sport | 2684 (16.1) | 469 (32.3) | 2215 (14.6) |
| Injury during watersports | 293 (1.7) | 21 (1.4) | 272 (1.8) |
| Type of brain injury | |||
| Concussion | 8191 (49.2) | 60 (4.1) | 8131 (53.5) |
| ICI | 776 (4.7) | 603 (41.5) | 173 (1.1) |
| Skull fracture with ICI | 888 (5.3) | 791 (54.4) | 97 (0.6) |
| Unspecified head Injury | 6787 (40.8) | 0 (0.0) | 6787 (44.7) |
| Age group at injury, y | |||
| 0–11 | 4004 (24.1) | 247 (17.0) | 3757 (24.7) |
| 12–18 | 6187 (37.2) | 379 (26.1) | 5808 (38.2) |
| 19–24 | 3028 (18.2) | 263 (18.1) | 2765 (18.2) |
| 25–34 | 1388 (8.3) | 188 (12.9) | 1200 (7.9) |
| 35–44 | 932 (5.6) | 136 (9.4) | 796 (5.2) |
| 45–64 | 863 (5.2) | 165 (11.3) | 698 (4.6) |
| 65+ | 240 (1.4) | 76 (5.2) | 164 (1.1) |
| Gender | |||
| Female | 5113 (30.7) | 379 (26.1) | 4734 (31.2) |
| Male | 11,529 (69.3) | 1075 (73.9) | 10,454 (68.8) |
| Race | |||
| White | 12,464 (74.9) | 1225 (84.2) | 11,239 (74.0) |
| Black | 3557 (21.4) | 173 (11.9) | 3384 (22.3) |
| Other | 621 (3.7) | 56 (3.9) | 565 (3.7) |
| Socioeconomic status, U.S. dollars | |||
| High (≥$75,000) | 3168 (19.0) | 250 (17.2) | 2918 (19.2) |
| Middle ($36,000–74,000) | 6400 (38.5) | 624 (42.9) | 5776 (38.0) |
| Low (≤$35,000) | 7074 (42.5) | 580 (39.9) | 6494 (42.8) |
| Comorbid conditions | |||
| No | 15,383 (92.4) | 1172 (80.6) | 14,211 (93.6) |
| Yes | 1259 (7.6) | 282 (19.4) | 977 (6.4) |
| Concomitant injuries | |||
| No | 12,047 (72.4) | 828 (56.9) | 11,219 (73.9) |
| Yes | 4595 (27.6) | 626 (43.1) | 3969 (26.1) |
| Repetitive TBI? | |||
| No | 15,632 (93.9) | 1189 (81.8) | 14,443 (95.1) |
| Yes | 1010 (6.1) | 265 (18.2) | 745 (4.9) |
| Season of injury | |||
| Autumn (22 Sep–20 Dec) | 4532 (27.2) | 315 (21.7) | 4217 (27.8) |
| Winter (21 Dec–19 Mar) | 2875 (17.3) | 257 (17.7) | 2618 (17.2) |
| Spring (20 Mar–20 Jun) | 4639 (27.9) | 484 (33.3) | 4155 (27.4) |
| Summer (21 Jun–21 Sep) | 4596 (27.6) | 398 (27.4) | 4198 (27.6) |
| Venue of care | |||
| ED | 15,204 (91.4) | 691 (47.5) | 14,513 (95.6) |
| Inpatient | 1438 (8.6) | 763 (52.5) | 675 (4.4) |
| Trauma facility level | |||
| Undesignated | 4875 (29.3) | 301 (20.7) | 4574 (30.1) |
| Level I | 3498 (21.0) | 594 (40.8) | 2904 (19.1) |
| Level II | 1329 (8.0) | 135 (9.3) | 1194 (7.9) |
| Level III | 6940 (41.7) | 424 (29.2) | 6516 (42.9) |
ED = emergency department; ICI = intracranial injury; TBI = traumatic brain injury.
Socioeconomic status (SES) was approximated by combining the median household income of the individual’s census tract and health insurance coverage. Those covered by Medicaid or the Medically Indigent Assistance Program were considered “low SES” regardless of the median household income of the census tract. We used the Elixhauser comorbidity scale [31] to identify comorbid conditions, such as seizures and hypoglycemic episodes, which might increase the risk of severe TBI. All ICD-9-CM diagnosis fields were searched for these comorbid conditions; individuals were dichotomized into “yes” or “no.” An individual with injuries to body regions other than the head was classified as having concomitant injury. Hospital trauma facility level is assigned by the SC Department of Health and Environmental Control based on national guidelines. Repetitive TBI was classified based on the occurrence of multiple sport-TBIs at least 3 days apart.
Statistical analysis
Data analyses relied on SAS software package, version 9.3.1 [32]. Confidence intervals (CI) for proportions were constructed assuming independence of the proportions under normal approximation. Rates were calculated based on the bridge population estimates obtained from the National Center for Health Statistics [33]. The denominator was adjusted to reflect the civilian population of SC receiving health care from nonfederal hospitals. Associations of the independent variables with TBI severity were assessed with the use of univariate and multivariable logistic regression using the generalized logit model. Variables with bivariate association, P ≤ .10, were included in the multivariable model. Multicollinearity among covariates was evaluated by assessing the deviations of the regression coefficients and their standard errors in the fitted univariate and multivariate models, and none were found [34]. Model fit and discriminatory capacity was assessed using the Hosmer–Lemeshow Goodness-of-fit test and receiving operating characteristic, respectively [35]. The unadjusted and adjusted odds ratios (OR) and 95% CI are reported.
Results
From 1998 through 2011, there were 16,642 individuals identified with sport-TBI yielding an average annual incidence rate of 31.5/100,000 population. The most common mechanism of sport-TBI was being kicked in football/rugby (38.1%), followed by fall injuries in sports and/or play activities (20.3%), and off-road motorized vehicle (OMV) injuries (16.1%). OMV-related sport-TBI occurred in young adults (mean age 22.7 years; 95% CI, 22.2–23.8). TBI resulting from equestrian sport represented 9.2%. Large proportions of equestrian sport-TBI occurred among white (93%) and female (70%) patients (data not shown).The least common mechanism was water sports (1.8%) such as diving and waterskiing. Concussion was the most common type of TBI in sport (49.2%) (Table 1).
Table 2 shows characteristics of persons with sport-TBI. Most sport-TBI (93.2%) was mild. Sport-TBI was more frequent in those ages 12–18 years (37.2%) and in males (69.3%). White patients accounted for 75% and persons in the middle SES group accounted for 38.5% of the persons with sport-TBI versus 65% and 30% of the state population, respectively. Conversely, the high SES group represents 19.0% of sport-TBI but 28.6% of the state population. Nearly 95% of the sport-TBIs were evaluated in the ED.
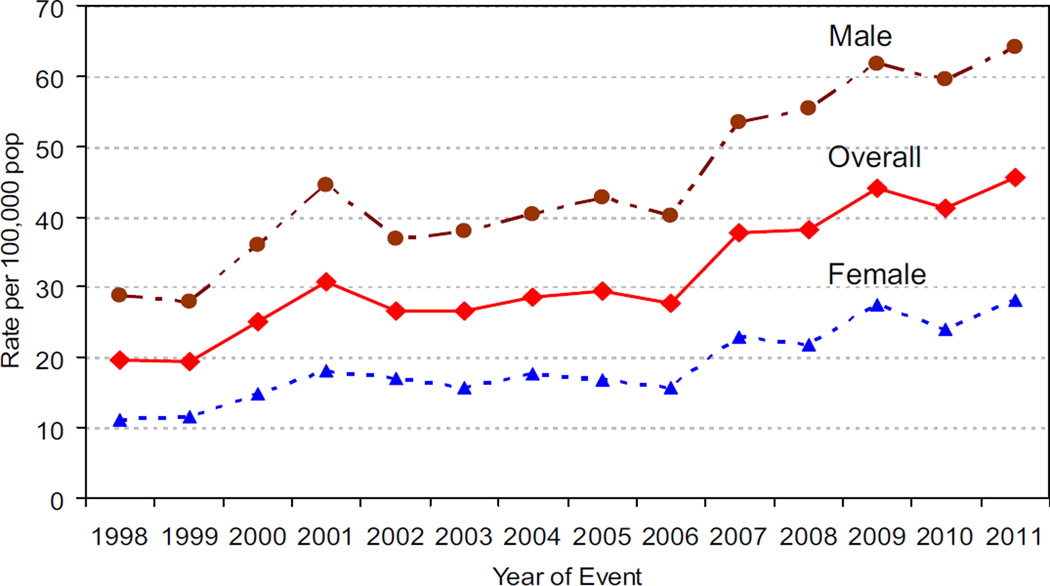
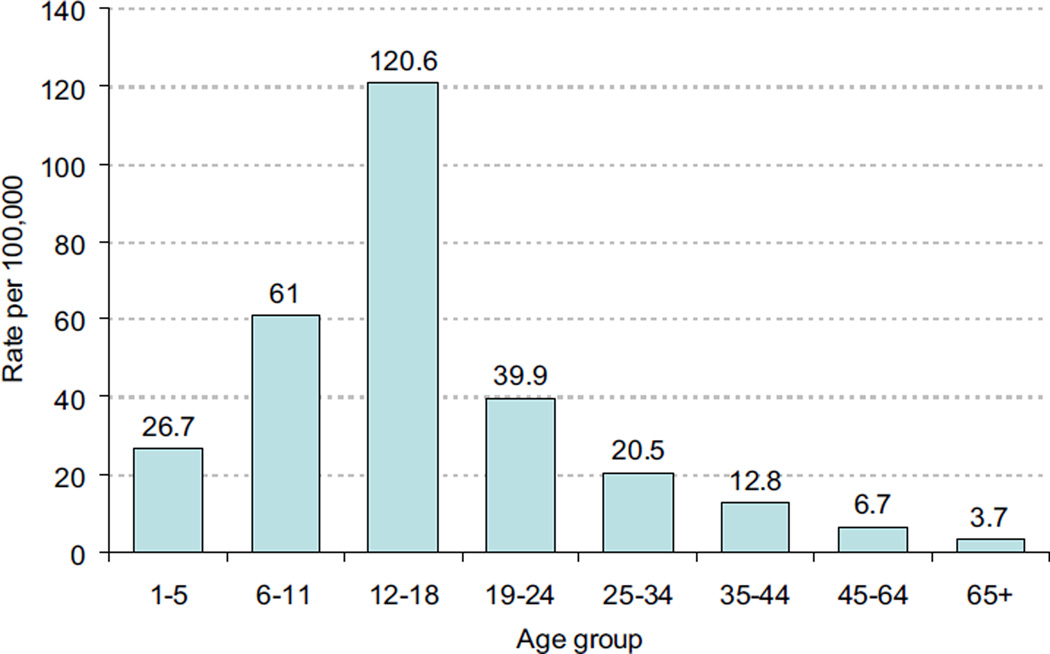
Incidence rates per 100,000 persons increased from 19.7 in 1998 to 45.6 in 2011 (Fig. 2). Although change in incidence rates from baseline was greater in female than in male patients (131% vs. 123%), gender difference in rates widened with advancing calendar years (17.4 in 1998 and 35.9 in 2011). All trends were statistically significant. Incidence rate was greatest in the 12- to 18-year age group (120.6/100,000 population) followed by the 6- to 11-year age group (61.0/100,000 population); after age 18 years, the incidence rate decreased precipitously (Fig. 3).
Fig. 2.
Trend of sports-related TBI by gender, South Carolina ED and hospital discharges.
Fig. 3.
Incidence rate of sports-related TBI by age group, South Carolina ED and hospital discharges, 1998–2011.
In our analysis, there were 1010 individuals (6.1%) with repetitive sport-TBI—5.6% had two and 0.5% sustained ≥3 sport-TBIs. Persons aged ≤24 years accounted for 85% of the repetitive sport-TBI (data not shown). Examination of risk factors after adjusting for covariates in the model shows persons with severe sport-TBI were four times more likely to have had previous sport-TBI than persons without previous sport-TBI (OR, 4.36; 95% CI, 3.69–5.15; Table 3). Persons with severe sport-TBI were 4.70 times more likely (95% CI, 3.35–6.60) to have been age ≥65 years than persons ages 0–11 years although they accounted for only 1.4% of sport-TBI. Risk of severe sport-TBI increased steadily with advancing age and was greater in male (OR, 1.85; 95% CI, 1.57–2.17) than female patients.
Table 3.
Risk characteristics associated with severity of sport-TBI, South Carolina ED and hospital discharges
| Risk characteristics | Unadjusted | Adjusted* |
|---|---|---|
| Odds ratio (95% CI) | Odds ratio (95% CI) | |
| Mechanism of injury | ||
| Tackle during sports | 1.00 (Referent) | 1.00 (Referent) |
| Kicked during football | 2.21 (1.38–3.52) | 2.46 (1.53–3.96) |
| Struck during sports | 1.37 (0.83–2.29) | 1.60 (0.95–2.70) |
| Fall during sports | 2.44 (1.52–3.93) | 2.72 (1.67–4.46) |
| Equestrian | 4.59 (2.84–7.42) | 2.73 (1.64–4.51) |
| Off-road vehicular sport | 6.55 (4.10–10.46) | 4.73 (2.92–7.67) |
| Injury during watersports | 2.39 (1.264.51) | 1.96 (1.02–3.78) |
| Age group at injury, y | ||
| 0–11 | 1.00 (Referent) | 1.00 (Referent) |
| 12–17 | 0.99 (0.84–1.17) | 0.96 (0.80–1.15) |
| 18–24 | 1.45 (1.21–1.73) | 1.36 (1.12–1.66) |
| 25–34 | 2.39 (1.96–2.92) | 1.86 (1.49–2.32) |
| 35–44 | 2.60 (2.08–3.25) | 2.01 (1.57–2.58) |
| 45–64 | 3.59 (2.91–4.45) | 2.40 (1.87–3.08) |
| 65+ | 7.05 (5.22–9.52) | 4.70 (3.35–6.60) |
| Race | ||
| White | 1.00 (Referent) | 1.00 (Referent) |
| Black | 0.47 (0.40–0.55) | 0.56 (0.47–0.66) |
| Other | 0.91 (0.69–1.20) | 1.07 (0.79–1.44) |
| Gender | ||
| Female | 1.00 (Referent) | 1.00 (Referent) |
| Male | 1.28 (1.14–1.45) | 1.85 (1.57–2.17) |
| Socioeconomic status, U.S. dollars | ||
| High (≥$75,000) | 1.00 (Referent) | 1.00 (Referent) |
| Middle ($36,000–74,000) | 1.26 (1.08–1.47) | 1.13 (0.95–1.33) |
| Low (≤$35,000) | 1.04 (0.89–1.22) | 1.14 (0.96–1.34) |
| Comorbid conditions? | ||
| No | 1.00 (Referent) | 1.00 (Referent) |
| Yes | 3.51 (3.03–4.05) | 2.07 (1.75–2.45) |
| Concomitant Injuries? | ||
| No | 1.00 (Referent) | 1.00 (Referent) |
| Yes | 2.14 (1.92–2.39) | 1.47 (1.30–1.66) |
| Repetitive TBI? | ||
| No | 1.00 (Referent) | 1.00 (Referent) |
| Yes | 4.32 (3.71–5.03) | 4.36 (3.69–5.15) |
| Trauma facility level | ||
| Undesignated | 1.00 (Referent) | 1.00 (Referent) |
| Level I | 3.10 (2.68–3.60) | 3.01 (2.58–3.51) |
| Level II | 1.72 (1.39–2.12) | 1.59 (1.27–1.99) |
| Level III | 0.99 (0.85–1.15) | 1.05 (0.90–1.23) |
CI = confidence interval; ED = emergency department; TBI = traumatic brain injury.
Adjusted for all independent variables listed in the table.
The risk of severe sport-TBI varied by the mechanism of injury. Compared with sport-TBI caused by tackle-in-sport, significantly increased associations were noted in OMV (OR, 4.73; 95% CI, 2.92–7.67); fall-in-sport (OR, 2.72; 95% CI, 1.67–4.46); equestrian sport (OR, 2.73; 95% CI, 1.64–4.51), kicked in football (OR, 2.46; 95% CI, 1.53–3.96) and injury in water-sport (OR, 1.96; 95% CI, 1.02–3.78). Persons with at least one comorbid condition (OR, 2.07; 95% CI, 1.75–2.45) and concomitant injuries (OR, 1.47; 95% CI, 1.30–1.66) had greater risk of severe sport-TBI than persons without comorbid condition and without concomitant injury, respectively.
Discussion
We analyzed data from a population-based TBI surveillance system spanning 14 years to provide a comprehensive yet conservative incidence rate of sport-TBI in a statewide population and quantification of risk characteristics of sport-TBI severity. Because of the lack of specificity of E-codes, population-based epidemiological studies are limited and risk factors of severity have not been adequately evaluated. E-codes that mention sport are so limited that only a third of sport-related injuries are identifiable by these codes [36]. To offset this limitation, one study used Bayesian conditional probabilities to approximate sport-related injuries. However, these estimates are controversial because prior and posterior distributions represent subjective states of knowledge [37,38]. We chose the frequentist approach of counting actual events using both mechanism and place of injury E-codes (Table 1) to enhance case detection.
Our findings showed an incidence rate of 31.5/100,000 population. Although our rate is lower than estimates provided from studies based on self-report and the National Electronic Injury Surveillance System [8,9], it was much greater than earlier estimates from state-based surveillance systems [5] and comparable to estimate from the National Hospital Ambulatory Medical Care Survey [6]. The annual incidence rate of sport-TBI increased steadily throughout the observation period as noted in other studies [19,22]. In affirmation of our hypotheses, the odds of severe sport-TBI increased with advancing age and increased fourfold in persons with repetitive sport-TBI.
Kicked in football was the most frequent mechanism accounting for 38.1% of all sport-TBI and 29% of all severe sport-TBI. Although the specific E-code (E917.0) mentions both football and rugby, the latter is a rare sport activity in South Carolina [39]. As seen in other studies, TBI from being kicked in football occurred primarily in the 12- to 24-year age range (72.4%), a segment of the population likely to participate in middle, high school, and college football [14,40].
Falls were the second most common mechanism (20.3%). Falls from rollerblading, skateboarding, and nonmotorized scooters accounted for 43.6% of the fall injuries. The popularity of skateboarding and roller-skating among adolescents and the potential for head trauma deserve more attention. A recent analysis of the National Trauma Data Bank indicated 41.5% of skateboard-related injuries were TBIs and helmet use was a mere 7.2% [41]. Falls from playground equipment accounted for 37%; 88.6% were among children ages 6–11 years. Accidental falls without specific mention of sport activity but occurring in places of sport represented 21.0%.
Sport-TBI attributable to OMV accounted for 16.1% of the injuries and showed the strongest association with severe sport-TBI. The use of OMV for hunting and racing in rugged fields has continued to increase, posing public health concerns as these vehicles have considerable rollover tendencies and causing head trauma among riders who don’t use helmets [42–44]. The mean age of persons with OMV-related sport-TBI in our dataset is 22.7 years (95% CI, 22.2–23.8), compared with 24.1 years from 11,589 persons with OMV-related sport-TBI from U.S. trauma center data [44].
Similar to other studies, most equestrian sport-TBI occurred among white (93%), female patients (70%) with a median age of 31 years [45]. The risk of injury from competitive equestrian sport was estimated to be threefold greater than motorcycle racing, with greater risk in inexperienced riders [46]. Although water sports are among the top five popular sports in South Carolina [39], it was the least common cause of sport-TBI (2.1%). The discordance between the popularity of water sports and the small numbers of sport-TBI from water sport may be attributable to a greater likelihood of mortality from drowning. From 1998 to 2010, mortality from drowning in South Carolina was 3.4 times more frequent than morbidity with 913 deaths versus 293 survivors [47].
A major concern in sport-TBI is the potential for repetitiveness of TBI because having sustained one TBI increased the risk of subsequent TBI [48–50]. Concussion is a major concern either because acute signs and symptoms are subtle and easily ignored or misconceptions of the clinical symptoms of concussion lead to insufficient recovery time [10,51,52]. Repetitive concussions can lead to second impact syndrome, a fatal condition associated with diffuse brain edema and herniation or chronic traumatic encephalopathy, a condition with symptoms ranging from depressive and psychotic symptoms to cognitive dysfunction and dementia [21,51,53]. In our data 1010 persons (6.1%) had repetitive sport-TBI with disproportionate occurrence among those aged 25 years and younger (80.0%; 95% CI, 77.5–82.5), raising concern about long-term deficit in cognitive skills and behavior [10].
Concussions and unspecified head injury were the most frequent TBI type, accounting for 90.0% of sport-TBI. Concussion may be the signature lesion of sport-TBI. On the basis of our historical surveillance data and a study from the Centers for Disease Control and Prevention [54], nearly all cases coded with 959.01 would have been coded as concussion unspecified (850.9) or intracranial injury of unspecified nature (854.0) before the implementation of 959.01 in 1998. It is therefore likely that a large proportion of 959.01 codes pertain to poorly defined concussions [55]. Of all concussion diagnoses in our database, 87.2% occurred in those aged 25 years or younger. Although the overwhelming majority of concussions are mild, the potential effects of even mild TBI on neurocognitive functioning and memory processing is a cause of concern [56,57].
Male patients had thrice as many sport-TBI than female patients and were 1.85 times more likely to have severe sport-TBI. Although our finding is consistent with most studies, other studies found greater concussion scores and ominous brain injury outcomes in females [20,58]. Nonetheless, dissimilarities in case ascertainment criteria and age range of the target population hamper comparability with published studies. One possible explanation for greater risk of severe sport-TBI in males is residual confounding, such as the force exerted during collision/kick in sports. Males tend to have more body mass and faster speed than females. In one study, having a lower body mass index was found to be protective of concussion regardless of gender [18,59]. Another explanation is that males are more likely than females to try risky maneuvers such as tackling during play [40].
The most common comorbid conditions were diabetes, cardiovascular disease, and neurologic disorders. The odds of sustaining a severe sport-TBI in persons with at least one comorbid condition are twice that of persons without comorbid conditions. Chronic illnesses are important intrinsic host factors, contributing to physical frailty and intensify the effect of injury [60,61]. The prevalence of comorbid conditions was age dependent—4.7% in persons aged younger than 25 years and 18.7% in persons aged 25 years and older. Similarly, persons with severe sport-TBI were 1.5 times more likely to have concomitant injuries. This association may be due to the intensity of the external force causing the trauma. Studies of motor vehicle crashes have shown trauma induced by high-energy forces tends to affect multiple body regions and result in more severe TBI [62]. The two most common mechanisms of injury associated with concomitant injury were OMV (30.6%; 95% CI, 29.3–31.9) and kicked during football (26.3%; 95% CI, 25.0–27.5). Finally, persons with severe sport-TBI were more likely to be treated in level I and II trauma centers, confirming the intent of trauma centers in treating trauma appropriately [63].
The study has several limitations. First, case-ascertainment relied on administrative data susceptible to various coding irregularities. E-code accuracy relies on the coders’ ability to identify the correct cause of injury. However, the TBI surveillance system has an ongoing data evaluation protocol that includes medical chart review of randomly selected observations to validate the accuracy of the ICD-9-CM codes and periodic data evaluation shows good reliability and completeness of E-codes. Second, the surveillance system does not capture TBI visits to federal facilities, limiting representativeness of the data to the general population of the state. However, to offset dilution of the rates and to preserve representativeness, we adjusted the denominator by excluding residents of the state that receive health care from military and veteran establishments based on the 2010 census information. Third, only those hospitalized or seen in the ED for TBI are included in these data, which may reflect the seriousness of injury, suggesting milder sport-TBI cases who did not seek medical attention or who were treated in private clinics were not counted, contributing to underestimation of sport-TBI and repetitive TBI rates. Nonetheless, our data reflect cases that warranted medical attention. Such cases may serve as a suitable proxy to understanding the risk factors for mild sport-TBI not captured by the TBI surveillance system. Fourth, duplicate observations may contribute to redundant information and overestimation of rates. However, the data include a unique personal identifier allowing identification of repeat visits for the same sport-TBI. Fifth, the rate of bicycle-related sport-TBI could not be estimated as the existing E-code scheme does not distinguish transportation-related bicycle injuries from sport- and recreation-related injuries.
Our study has several strengths. The data derive from a legally mandated statewide TBI surveillance system, allowing us to capture all ED visits to provide population-based estimates of sport-TBI. The TBI surveillance system adheres to CDC surveillance guidelines and has been extensively validated increasing confidence in the reliability of the data used for analysis [64]. Our methodological approach of identifying sport-TBI based on both external cause of injury and place of injury E-codes maximized case ascertainment. To our knowledge, this is the first population-based analyses of sport-TBI that relied on unweighted hard data covering 14 years. Although our incidence estimate is conservative compared to estimates derived from weighted samples, it is perhaps the best estimate of incidence of sport-TBI in a statewide population because of the representativeness of the numerator to the base civilian population in the state. Further, we quantified the risk of severe sport-TBI compared with mild sport-TBI by controlling for potential confounders.
Conclusion
The incidence of sport-TBI is increasing, corresponding with societal awareness of the benefits of physical activity. The rate is greatest in those aged 12–18 years, and concussion is the predominant TBI type. Severity increased with repetitive TBI and older age. Intrinsic risk characteristics such as gender and pre-existing chronic illnesses contributed to the risk of severe sport-TBI. Further, the high incidence of concussion in youth with repetitiveness may have long-term intellectual and behavioral consequences that warrant coordinated surveillance activities and further population-based outcome studies.
Acknowledgments
This study was partially supported by a grant from the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, grant number U17/CCU421926 (PI: Anbesaw Selassie, DrPH). The study is also supported by the South Carolina Department Disabilities and Special Needs, Head and Spinal Cord Division. The contents do not necessarily represent the opinion of the funding agencies, and should not be assumed as endorsement by the Federal and State Government.
References
- 1.Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002–2006. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010. [Google Scholar]
- 2.Corrigan JD, Hammond FM. Traumatic brain injury as a chronic health condition. Arch Phys Med Rehabil. 2013;94(6):1199–1201. doi: 10.1016/j.apmr.2013.01.023. [DOI] [PubMed] [Google Scholar]
- 3.Whiteneck G, Brooks CA, Mellick D, Harrison-Felix C, Terrill MS, Noble K. Population-based estimates of outcomes after hospitalization for traumatic brain injury in Colorado. Arch Phys Med Rehabil. 2004;85(4) Suppl. 2:S73–S81. doi: 10.1016/j.apmr.2003.08.107. [DOI] [PubMed] [Google Scholar]
- 4.Selassie AW, Zaloshnja E, Langlois JA, Miller T, Jones P, Steiner C. Incidence of long-term disability following traumatic brain injury hospitalization, United States, 2003. J Head Trauma Rehabil. 2008;23(2):123–131. doi: 10.1097/01.HTR.0000314531.30401.39. [DOI] [PubMed] [Google Scholar]
- 5.Thurman DJ, Branche CM, Sniezek JE. The epidemiology of sports-related traumatic brain injuries in the United States: recent developments. J Head Trauma Rehabil. 1998;13(2):1–8. doi: 10.1097/00001199-199804000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Bazarian JJ, McClung J, Shah MN, Cheng YT, Flesher W, Kraus J. Mild traumatic brain injury in the United States, 1998–2000. Brain Inj. 2005;19(2):85–91. doi: 10.1080/02699050410001720158. [DOI] [PubMed] [Google Scholar]
- 7.NIH Consensus Development Panel on Rehabilitation of Persons with Traumatic Brain Injury. Consensus conference. Rehabilitation of persons with traumatic brain injury. JAMA. 1999;282(10):974–983. [PubMed] [Google Scholar]
- 8.Conn JM, Annest JL, Gilchrist J. Sports and recreation related injury episodes in the US population, 1997–99. Inj Prev. 2003;9(2):117–123. doi: 10.1136/ip.9.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control And Prevention. Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged </=19 years–United States, 2001–2009. MMWR Morb Mortal Wkly Rep. 2011;60(39):1337–1342. [PubMed] [Google Scholar]
- 10.Guskiewicz KM, McCrea M, Marshall SW, Cantu RC, Randolph C, Barr W, et al. Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290(19):2549–2555. doi: 10.1001/jama.290.19.2549. [DOI] [PubMed] [Google Scholar]
- 11.Crisco JJ, Wilcox BJ, Beckwith JG, Chu JJ, Duhaime AC, Rowson S, et al. Head impact exposure in collegiate football players. J Biomech. 2011;44(15):2673–2678. doi: 10.1016/j.jbiomech.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kerr ZY, Marshall SW, Guskiewicz KM. Reliability of concussion history in former professional football players. Med Sci Sports Exerc. 2012;44(3):377–382. doi: 10.1249/MSS.0b013e31823240f2. [DOI] [PubMed] [Google Scholar]
- 13.Powell JW, Barber-Foss KD. Traumatic brain injury in high school athletes. JAMA. 1999;282(10):958–963. doi: 10.1001/jama.282.10.958. [DOI] [PubMed] [Google Scholar]
- 14.Guskiewicz KM, Weaver NL, Padua DA, Garrett WE., Jr Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28(5):643–650. doi: 10.1177/03635465000280050401. [DOI] [PubMed] [Google Scholar]
- 15.Marshall SW, Spencer RJ. Concussion in rugby: the hidden epidemic. J Athl Train. 2001;36(3):334–338. [PMC free article] [PubMed] [Google Scholar]
- 16.Colvin AC, Mullen J, Lovell MR, West RV, Collins MW, Groh M. The role of concussion history and gender in recovery from soccer-related concussion. Am J Sports Med. 2009;37(9):1699–1704. doi: 10.1177/0363546509332497. [DOI] [PubMed] [Google Scholar]
- 17.Crisco JJ, Fiore R, Beckwith JG, Chu JJ, Brolinson PG, Duma S, et al. Frequency and location of head impact exposures in individual collegiate football players. J Athl Train. 2010;45(6):549–559. doi: 10.4085/1062-6050-45.6.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schulz MR, Marshall SW, Mueller FO, Yang J, Weaver NL, Kalsbeek WD, et al. Incidence and risk factors for concussion in high school athletes, North Carolina, 1996–1999. Am J Epidemiol. 2004;160(10):937–944. doi: 10.1093/aje/kwh304. [DOI] [PubMed] [Google Scholar]
- 19.Lincoln AE, Caswell SV, Almquist JL, Dunn RE, Norris JB, Hinton RY. Trends in concussion incidence in high school sports: a prospective 11-year study. Am J Sports Med. 2011;39(5):958–963. doi: 10.1177/0363546510392326. [DOI] [PubMed] [Google Scholar]
- 20.Laker SR. Epidemiology of concussion and mild traumatic brain injury. PM R. 2011;3(10) Suppl. 2:S354–S358. doi: 10.1016/j.pmrj.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 21.Rabadi MH, Jordan BD. The cumulative effect of repetitive concussion in sports. Clin J Sport Med. 2001;11(3):194–198. doi: 10.1097/00042752-200107000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Covassin T, Swanik CB, Sachs ML. Epidemiological considerations of concussions among intercollegiate athletes. Appl Neuropsychol. 2003;10(1):12–22. doi: 10.1207/S15324826AN1001_3. [DOI] [PubMed] [Google Scholar]
- 23.Pate RR, Trost SG, Levin S, Dowda M. Sports participation and health-related behaviors among US youth. Arch Pediatr Adolesc Med. 2000;154(9):904–911. doi: 10.1001/archpedi.154.9.904. [DOI] [PubMed] [Google Scholar]
- 24.Kozlowski KF, Leddy JJ, Tomita M, Bergen A, Willer BS. Use of the ICECI and ICD-10 E-Coding structures to evaluate causes of head injury and concussion from sport and recreation participation in a school population. Neuro-Rehabilitation. 2007;22(3):191–198. [PubMed] [Google Scholar]
- 25.American Medical Association. International classification of diseases, 9th revision, clinical modification. Chicago (IL): Saunders; 2009. [Google Scholar]
- 26.Butler JA, Langlois JA. Central nervous system injury surveillance: data submission standards. Atlanta (GA): Department of Health and Human Services, Centers for Disease Control and Prevention, Control NCfIPa; 2000. [Google Scholar]
- 27.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–196. [PubMed] [Google Scholar]
- 28.Center for Injury Research and Policy. ICDMAP-90 Software. Baltimore (MD): The Johns Hopkins University and Tri-Analytics, Inc; 1997. The Johns Hopkins University School of Public Health. [Google Scholar]
- 29.MacKenzie EJ. Injury severity scales: overview and directions for future research. Am J Emerg Med. 1984;2(6):537–549. doi: 10.1016/0735-6757(84)90081-0. [DOI] [PubMed] [Google Scholar]
- 30.MacKenzie EJ, Steinwachs DM, Shankar B. Classifying trauma severity based on hospital discharge diagnoses. Validation of an ICD-9CM to AIS-85 conversion table. Med Care. 1989;27(4):412–422. doi: 10.1097/00005650-198904000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 32.SAS Institute. Statistical analytical software. Version 9.3.1 ed. Cary (NC): SAS Institute Inc; 2011. [Google Scholar]
- 33.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) Bridged-race population estimates, United States [Web page] National Center for Health Statistics; 2012. [cited 20.10.2012]. http://wonder.cdc.gov/bridged-race-v2011.html. [Google Scholar]
- 34.Darlington GA, Armtage P, Colton T. Encyclopedia of biostatistics. Chichester, West Sussex (UK): John Wiley & Sons; 1998. Collinearity; pp. 788–789. [Google Scholar]
- 35.Hosmer DW, Lemeshow S. Applied logistic regression. New York: John Wiley & Sons; 2000. The multinominal logistic regression model. [Google Scholar]
- 36.Micheli LJ, Glassman R, Klein M. The prevention of sports injuries in children. Clin Sports Med. 2000;19(4):821–834. doi: 10.1016/s0278-5919(05)70239-8. [DOI] [PubMed] [Google Scholar]
- 37.Dempsey RL, Layde PM, Laud PW, Guse CE, Hargarten SW. Incidence of sports and recreation related injuries resulting in hospitalization in Wisconsin in 2000. Inj Prev. 2005;11(2):91–96. doi: 10.1136/ip.2004.006205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gelman A, Shalizi CR. Philosophy and the practice of Bayesian statistics. Br J Math Stat Psychol. 2013;66(1):8–38. doi: 10.1111/j.2044-8317.2011.02037.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.South Carolina Athletic Administrators Association. Popular Sports Poll. [accessed 09.08.13];2012 http://www.ihigh.com//atboa/poll_2434.html. [Google Scholar]
- 40.Gessel LM, Fields SK, Collins CL, Dick RW, Comstock RD. Concussions among United States high school and collegiate athletes. J Athl Train. 2007;42(4):495–503. [PMC free article] [PubMed] [Google Scholar]
- 41.Lustenberger T, Talving P, Barmparas G, Schnuriger B, Lam L, Inaba K, et al. Skateboard-related injuries: not to be taken lightly. A National Trauma Databank analysis. J Trauma. 2010;69(4):924–927. doi: 10.1097/TA.0b013e3181b9a05a. [DOI] [PubMed] [Google Scholar]
- 42.Denning GM, Jennissen CA, Harland KK, Ellis DG, Buresh CT. Off-highway vehicle parks: Combining environment, knowledge, and enforcement for all-terrain vehicle injury prevention. Accid Anal Prevent. 2013;52C:64–70. doi: 10.1016/j.aap.2012.12.015. [DOI] [PubMed] [Google Scholar]
- 43.Mattei TA, Bond BJ, Hafner JW, Jr, Morris MJ, Travis J, Hannah G, et al. Definition and measurement of rider-intrinsic physical attributes influencing all-terrain vehicle safety. Neurosurg Focus. 2011;31(5):E6. doi: 10.3171/2011.9.FOCUS11176. [DOI] [PubMed] [Google Scholar]
- 44.Bowman SM, Aitken ME, Helmkamp JC, Maham SA, Graham CJ. Impact of helmets on injuries to riders of all-terrain vehicles. Inj Prev. 2009;15(1):3–7. doi: 10.1136/ip.2008.019372. [DOI] [PubMed] [Google Scholar]
- 45.Fleming PR, Crompton JL, Simpson DA. Neuro-ophthalmological sequelae of horse-related accidents. Clin Exp Ophthalmol. 2001;29(4):208–212. doi: 10.1046/j.1442-9071.2001.00430.x. [DOI] [PubMed] [Google Scholar]
- 46.O’Day J. Horse riding: a dangerous sport. Clin Exp Ophthalmol. 2001;29(4):207. doi: 10.1046/j.1442-9071.2001.00415.x. [DOI] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention (CDC) NCHS. Drowning Deaths in SC Multiple Cause of Death, 1999–2010 on CDC WONDER Online Database. 2010 http://wonder.cdc.gov/mcd-icd10.html.
- 48.Saunders LL, Selassie AW, Hill EG, Nicholas JS, Horner MD, Corrigan JD, et al. A population-based study of repetitive traumatic brain injury among persons with traumatic brain injury. Brain Inj. 2009;23(11):866–872. doi: 10.1080/02699050903283213. [DOI] [PubMed] [Google Scholar]
- 49.Annegers JF, Grabow JD, Kurland LT, Laws ER., Jr The incidence, causes, and secular trends of head trauma in Olmsted County, Minnesota, 1935–1974. Neurology. 1980;30(9):912–919. doi: 10.1212/wnl.30.9.912. [DOI] [PubMed] [Google Scholar]
- 50.Albright JP, McAuley E, Martin RK, Crowley ET, Foster DT. Head and neck injuries in college football: an eight-year analysis. Am J Sports Med. 1985;13(3):147–152. doi: 10.1177/036354658501300301. [DOI] [PubMed] [Google Scholar]
- 51.Kushner DS. Concussion in sports: minimizing the risk for complications. Am Family Phys. 2001;64(6):1007–1014. [PubMed] [Google Scholar]
- 52.Chrisman SP, Rivara FP, Schiff MA, Zhou C, Comstock RD. Risk factors for concussive symptoms 1 week or longer in high school athletes. Brain Inj. 2013;27(1):1–9. doi: 10.3109/02699052.2012.722251. [DOI] [PubMed] [Google Scholar]
- 53.McKee AC, Stein TD, Nowinski CJ, Stern RA, Daneshvar DH, Alvarez VE, et al. The spectrum of disease in chronic traumatic encephalopathy. Brain. 2013;136(Pt 1):43–64. doi: 10.1093/brain/aws307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Coronado VG, McGuire LC, Sarmiento K, Bell J, Lionbarger MR, Jones CD, et al. Trends in Traumatic Brain Injury in the U.S. and the public health response: 1995–2009. J Safety Res. 2012;43(4):299–307. doi: 10.1016/j.jsr.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 55.Leibson CL, Brown AW, Ransom JE, Diehl NN, Perkins PK, Mandrekar J, et al. Incidence of traumatic brain injury across the full disease spectrum: a population-based medical record review study. Epidemiology. 2011;22(6):836–844. doi: 10.1097/EDE.0b013e318231d535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nance ML, Polk-Williams A, Collins MW, Wiebe DJ. Neurocognitive evaluation of mild traumatic brain injury in the hospitalized pediatric population. Ann Surg. 2009;249(5):859–863. doi: 10.1097/SLA.0b013e3181a41ae5. [DOI] [PubMed] [Google Scholar]
- 57.Lovell MR, Collins MW, Iverson GL, Field M, Maroon JC, Cantu R, et al. Recovery from mild concussion in high school athletes. J Neurosurg. 2003;98(2):296–301. doi: 10.3171/jns.2003.98.2.0296. [DOI] [PubMed] [Google Scholar]
- 58.Dick RW. Is there a gender difference in concussion incidence and outcomes? Br J Sports Med. 2009;43(Suppl. 1):i46–i50. doi: 10.1136/bjsm.2009.058172. [DOI] [PubMed] [Google Scholar]
- 59.Darrow CJ, Collins CL, Yard EE, Comstock RD. Epidemiology of severe injuries among United States high school athletes: 2005–2007. Am J Sports Med. 2009;37(9):1798–1805. doi: 10.1177/0363546509333015. [DOI] [PubMed] [Google Scholar]
- 60.Selassie AW, Fakhry SM, Ford DW. Population-based study of the risk of in-hospital death after traumatic brain injury: the role of sepsis. J Trauma. 2011;71(5):1226–1234. doi: 10.1097/TA.0b013e318226ecfc. [DOI] [PubMed] [Google Scholar]
- 61.Shoko T, Shiraishi A, Kaji M, Otomo Y. Effect of pre-existing medical conditions on in-hospital mortality: analysis of 20,257 trauma patients in Japan. J Am Coll Surg. 2010;211(3):338–346. doi: 10.1016/j.jamcollsurg.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 62.Siegel JH, Loo G, Dischinger PC, Burgess AR, Wang SC, Schneider LW, et al. Factors influencing the patterns of injuries and outcomes in car versus car crashes compared to sport utility, van, or pick-up truck versus car crashes: Crash Injury Research Engineering Network Study. J Trauma. 2001;51(5):975–990. doi: 10.1097/00005373-200111000-00024. [DOI] [PubMed] [Google Scholar]
- 63.Mullins RJ, Mann NC. Population-based research assessing the effectiveness of trauma systems. J Trauma. 1999;47(3 Suppl.):S59–S66. doi: 10.1097/00005373-199909001-00013. [DOI] [PubMed] [Google Scholar]
- 64.Selassie AW, Pickelsimer EE, Ferguson PL, Gravelle W, Gu JK. South Carolina Traumatic Brain Injury Follow-up Registry Manual of Operations. Charleston (SC): Medical University of South Carolina; 2004. [Google Scholar]