Abstract
Prenatal health care counseling is associated with positive health outcomes for mothers and infants. Moreover, pregnant women are considered a vulnerable population at risk of being victims of intimate partner violence. Pregnancy provides a unique opportunity to identify and refer women experiencing intimate partner violence to community resources; however, in prior research, most women reported that their prenatal care providers did not talk to them about intimate partner violence. Given the importance for providers to offer prenatal health care counseling on intimate partner violence, it is concerning that there is scant knowledge on Asian, Native Hawaiian, and other Pacific Islander mothers' experiences in this area. The study's objectives were (a) to determine the proportion of mothers who received prenatal health care counseling on intimate partner violence; and, (b) to examine racial differences of those who received prenatal health care counseling on intimate partner violence. Hawai‘i's Pregnancy Risk Assessment Monitoring System (PRAMS) data from 2004–08 were analyzed for 8,120 mothers with information on receipt of intimate partner violence prenatal health care counseling. Overall, 47.7% of mothers were counseled on intimate partner violence. Compared to Whites, Native Hawaiians, Japanese, Chinese, and Koreans were significantly less likely to report receiving prenatal health care counseling in intimate partner violence, but the opposite association was observed for Samoans. Intimate partner violence continues to be a significant problem for women, thus, this study's findings may be used as important baseline data to measure the progress made given the implementation of the new Guidelines for Women's Preventive Services in intimate partner violence screening and counseling.
Keywords: Asian, Native Hawaiian, Pacific Islander, intimate partner violence, prenatal health care counseling
Pregnant women are considered a vulnerable population at risk of intimate partner violence (IPV). In one study of pregnant women, the rates of physical IPV by their male partners 12 months prior to and during their pregnancy were 7% and 5%, respectively.1 Another review reported the prevalence of violence to be as high as 20% during pregnancy.2 Additionally, studies have demonstrated that women who experience IPV both prior to and during pregnancy are at risk for numerous poor health outcomes;3–8 furthermore, the adverse mental health consequences of IPV can be long-term and debilitating.9,10 A 2001 systematic review and meta-analysis paper reported that pregnant women experiencing IPV were 1.4 times more likely to have a low birth weight baby, compared to pregnant women who did not experience IPV.11
Given these statistics, it is imperative that screening for IPV occur during prenatal health care (PNC) visits in order to promote positive health outcomes for the mothers and infants. Pregnancy provides a unique opportunity to identify and refer women experiencing IPV to community resources; however, a population-based study found that 61–78% of the women reported that their prenatal care providers did not talk about physical IPV with them.12 The American Congress of Obstetricians and Gynecologists (ACOG) guidelines recommend that physicians screen all patients for IPV. Pregnant women in particular should be screened throughout the course of the pregnancy because it may take more than one screening before a woman discloses her experience with IPV.13 The ACOG guidelines have recently been supported by a new mandate. On August 1, 2011, the US Department of Health and Human Services (DHHS) adopted additional Guidelines for Women's Preventive Services. Included in these guidelines are free screening and counseling for interpersonal and domestic violence for all women beginning August 2012 for all new health plans.14
An examination of the literature yielded inconsistent rates of screening and counseling for IPV during prenatal visits. For example, Horan and colleagues surveyed 189 obstetrician-gynecologists and found that while approximately 68% reported screening for patients for IPV when they suspected IPV, only 39% routinely screened for IPV at the first prenatal visit.15 However, in a recent report, only prenatal care providers who received prompts and cues for assessing IPV risk were found to actually have a provider-patient IPV discussion with pregnant women with a known history of IPV.16 A study using the 1996 and 1997 Pregnancy Risk Assessment Monitoring System (PRAMS) data from 14 states (Alabama, Alaska, Arkansas, Colorado, Florida, Georgia, Maine, Michigan, New York, North Carolina, Oklahoma, South Carolina, Washington, and West Virginia) reported that 22.4% to 38.5% of women discussed physical IPV with their physicians during their prenatal care visits. Women who were more likely to be counseled were Black, Hispanic, young (<20 and 20 to 29 years old), had a high school education or less, or paid for prenatal care with Medicaid.12
There is a particular knowledge gap, however, regarding the receipt of PNC counseling on physical IPV among Asian American, Native Hawaiian, and other Pacific Islander (NHOPI) mothers. Small sample sizes of Asian Americans and NHOPIs in some studies resulted in Asian Americans and NHOPIs being combined into one group or being excluded from data analyses.17 However, it is important that efforts be made to address these understudied groups, especially knowing that these populations are rapidly expanding in the United States. For instance, the Asian American population grew by 46% from 2000 to 2010, making it the fastest-growing racial group in the United States.18,19 The NHOPI population has also experienced a growth of 40%. In total, there are approximately 18.5 million Asian Americans and NHOPIs in the United States.16,17
The state of Hawai'i has a large population of Asian Americans and NHOPIs. In fact, Honolulu County is the only county in the United States with an Asian American majority (57%).19 According to the 2010 US Census, there were more than 1.36 million persons residing in Hawai‘i.20 To complicate matters, nearly 24% of persons in Hawai‘i report more than one federal race group.21 There is quite a difference in the population estimates between those who only report a single race (NHOPIs - 10%, Asians - 38.6%, and Whites - 24.7%) from those who report their race in combination with one or more races (NHOPIs - 26.2%, Asians - 57.4%, and Whites - 41.5%). Even this categorization of federal race groups into distinct Asian and NHOPI race groups does not recognize the known heterogeneity of Asian Americans and NHOPIs within each race group in regards to language, culture, and nativity.22,23
Given the racial diversity and the population growth of Asian Americans and NHOPIs, it is important to examine differences in screening rates by race-ethnicity to determine if there are specific populations that are being underserved in screening, and thus, target resources to such populations. To the authors' knowledge, no studies have directly examined the prevalence of and racial differences in receiving PNC counseling on IPV among Asian American and NHOPI mothers. Thus, the specific aims of this study were to; (a) determine the proportion of mothers who received PNC counseling on IPV; and (b) examine racial differences of those who received PNC counseling on IPV. The study results may be utilized as baseline data to measure the impact of the DHHS Guidelines for Women's Preventive Services among a diverse Asian American and NHOPI population. Moreover, this study addresses a specific goal of Healthy People 2020 to “improve the health and well-being of women, infants, children, and families.”24
Methods
Data Source
This study analyzed existing de-identified data from Hawai‘i's PRAMS for the years 2004-08 (N = 8,120 respondents). PRAMS is a project of the Centers for Disease Control and Prevention and state health departments. PRAMS is an ongoing state-and population-based surveillance system that monitors selected maternal behaviors and experiences among women before, during, and after a pregnancy that resulted in a live birth. The PRAMS data is weighted to reflect the resident population of births in the State of Hawai‘i through adjustment for sampling design, noncoverage, and nonresponse.
Response Rates
The original sample size was 8,490 mothers, but 370 (4.2%) mothers reported that they did not receive prenatal health care, thus, were excluded from the analyses. The total sample size for this study was 8,120. The overall response rate was 76.1%, of which 79.7% completed the survey by mail in the first phase and the remaining 20.3% completed the survey by phone. For persons who responded in the mail phase, 73.4% did so in the first mailing. At the time the mothers completed the survey, the infant's mean age was 17.4 weeks (range 10-39 weeks). Out of the 8,120 mothers in this study, the proportions of respondents in the overall sample for each year were 20.6% (2004), 20.1% (2005), 21.3% (2006), 21.6% (2007), and 16.5% (2008).
Dependent Variable
Receipt of PNC counseling on IPV was categorized as yes or no based on response to a question in which mothers were asked if a doctor, nurse, or other health care worker talked with them during any of their PNC visits about IPV by their husbands/partners.
Independent Variables
Race
Mothers are able to self-report as many racial groups as they want on the birth certificate. The Hawai‘i birth certificate collects information on all racial/ethnic groups entered, but these are converted to one of 22 single racial groups by an algorithm implemented by the Office of Health Status Monitoring (OHSM) in the Hawai‘i Department of Health.25 This conversion to a single race group places all women into a single race and thus precludes the ability to analyze as a separate group the approximately one third of the mothers who have a live birth in Hawai‘i reporting more than one race.26 Single race groups, provided by OHSM, were categorized into Native Hawaiian, Samoan, and other Pacific Islander (Guamanian; other Pacific Islander), Filipino, Japanese, Chinese, Korean, and other Asian (Vietnamese; Asian Indian; other Asian), White, and the remainder were put into an all others category (Puerto Rican; Portuguese; American Indian; Black; Cuban; Mexican; all others).
Having Experienced IPV
Having experienced IPV was defined as reporting physical violence from a current or former husband or partner before and/or during pregnancy. There were four individual questions with two referring to the “12 months before you got pregnant” and the other two referring to during their “most recent pregnancy.” The questions were equivalent with each being asked in the two time periods:
Did an ex-husband or ex-partner push, hit, slap, kick, choke, or physically hurt you in any other way? (yes/no); and,
Were you physically hurt in any way by your husband or partner? (yes/no).
For the purpose of this analysis, these questions were combined into a composite variable and having experienced IPV was determined by a yes response to either question in the two time periods.
Other Socio-demographics Variables
Maternal age was a continuous variable. The household income categories included: < $10,000, $10,000–24,999, $25,000–49,999, and $50,000+ with income missing in about 7.4% of records. Maternal education was based on total number of years of education as reported on the birth certificate and categorized as “<High School” for mothers with <12 years, “High School or Equivalent” for mothers with 12 years, “Some College” for mothers with 13–15 years, and “College Graduate” for mothers with 16 or more years. Marital status was parsed into “married” and “not married.” For geography, comparisons were made by County and further grouped into urban and rural classification with all counties in Hawai‘i considered rural except for Honolulu County which was classified as urban, as the majority of the population in Honolulu County live in a federally designated urban area, and there is no finer delineation of geography in PRAMS than at the county level.
Respondents were asked, “Are you currently in school or working outside the home?” Therefore, employment/school was a binary variable (yes/no). Health insurance status was categorized as having private insurance, Medicaid, or being uninsured.
Data Analysis
The analysis included descriptive statistics and Chi-squared tests. Bivariate and multivariate logistic regressions of any experience with PNC counseling in IPV (yes; no) were conducted. There were two variables, maternal residence and region, that were found not to be significantly related to any experience with PNC counseling in IPV (at the 0.05 threshold) in the bivariate logistic regressions, and were therefore excluded from the multivariate logistic regression models. However, some variables remained in the analyses if they were deemed theoretically important based on prior research including socioeconomic status, health insurance, and experience with physical IPV. Models were adjusted for age, marital status, health insurance, education, employment/in school, household income, and experience with physical IPV. In the adjusted analyses, an interaction between mothers' race and experience with IPV was explored. Stata version11.1(College Station, TX: StataCorp LP) was used to conduct the data analyses, and the “svy” commands were used to account for the complex sampling design in order to provide accurate variance estimates.27
Human Subjects Protection
This study was approved by the Committee on Human Research at the University of Hawai‘i at Manoa. A data sharing agreement was completed with the Hawai‘i PRAMS program within the Hawai‘i State Department of Health.
Results
Descriptive Analyses
The weighted distribution of mothers by race was 20.2% White, 27.9% Native Hawaiian, 3.0% Samoan, 18.6% Filipino, 12.3% Japanese, 3.5% Chinese, 1.6% Korean, 1.8% other Asian, 5.0% other Pacific Islander, and 6.3% all others (Table 1). The mean age of the mothers was 28.0 years, approximately 65% were married, less than half were employed or in school (45.2%), and most had public or private health insurance (86.7%). Nearly 18% had an annual household income of less than $10,000, 23.2% of $10,000–24,999, 25.1% of $25,000–49,999, and 34.1% of $50,000 or more. More than one in four mothers had at least completed a college education (26.6%), 25.1% some college, and 48.3% high school or less. Less than three out of ten mothers resided in rural areas (28.5%) with the remaining in urban areas. Most mothers resided in Honolulu County (71.5%) while the remaining mothers resided in Hawai‘i County (12.7%), Maui County (10.9%), and Kaua‘i County (4.9%).
Table 1.
Sample Characteristics of Study Population: Hawai‘i Pregnancy Risk Assessment Monitoring System, 2004–2008
| Unweighted Number | Weighted percentage (95% CI) | |||
| Received prenatal health care counseling in intimate partner violence, % | 8,120 | 47.7 (46.6, 48.8) | ||
| Race | ||||
| White | 1,541 | 20.2 (19.9, 20.5) | ||
| Native Hawaiian | 1,771 | 27.9 (27.6, 27.9) | ||
| Samoan | 196 | 3.0 (2.6, 3.4) | ||
| Filipino | 1,559 | 18.6 (18.4, 18.7) | ||
| Japanese | 960 | 12.3 (11.7, 12.8) | ||
| Chinese | 835 | 3.5 (3.4, 3.7) | ||
| Korean | 371 | 1.6 (1.5, 1.7) | ||
| Other Asian | 130 | 1.8 (1.5, 2.1) | ||
| Other Pacific Islander | 307 | 5.0 (4.5, 5.5) | ||
| All Other | 432 | 6.3 (5.8, 6.9) | ||
| Age (years), mean (SE) | 8,120 | 28.0 (0.1), (27.9, 28.2) | ||
| Marital status, % | ||||
| Married | 5,602 | 64.6 (63.2, 65.3) | ||
| Not married | 2,518 | 35.4 (34.7, 36.8) | ||
| Health insurance (%) | ||||
| Private insurance | 5,757 | 67.5 (66.4, 68.5) | ||
| Medicaid | 1,346 | 19.2 (18.3, 20.1) | ||
| Uninsured | 1,033 | 13.3 (12.5, 14.1) | ||
| Education, % | ||||
| College Graduate | 2,515 | 26.6 (25.3, 27.2) | ||
| Some college | 2,099 | 25.1 (24.0, 26.1) | ||
| High school or equivalent or less than a high school education | 3,384 | 48.3 (47.5, 49.7) | ||
| Employed/In school % | 3,668 | 45.2 (44.0, 46.2) | ||
| Household income (%) | ||||
| <$10,000 | 1,170 | 17.6 (17.0, 18.8) | ||
| $10,000–24,999 | 1,666 | 23.2 (22.1, 24.1) | ||
| $25,000–49,999 | 1,878 | 25.1 (24.1, 26.1) | ||
| $50,000+ | 2,889 | 34.1 (32.9, 35.0) | ||
| Region, % | ||||
| Urban | 6,001 | 71.5 (70.6, 72.6) | ||
| Rural | 2,118 | 28.5 (27.4, 29.4) | ||
| Maternal residence, % | ||||
| Hawai‘i County | 930 | 12.7 (12.0, 13.5) | ||
| Honolulu County | 6,002 | 71.5 (71.0, 72.6) | ||
| Kaua‘i County | 371 | 4.9 (4.3, 5.3) | ||
| Mau‘i County | 817 | 10.9 (10.1, 11.5) | ||
| Experienced intimate partner violence from current/former husband/partner before/during pregnancy, % | 464 | 6.4 (5.9, 7.0) | ||
| Number of prenatal health care visits, mean (SE) | 7,921 | 11.1 (0.1) | ||
| Total sample, no. | 8,120 | 100.0 | ||
Note: Percentages might not equal 100% due to rounding.
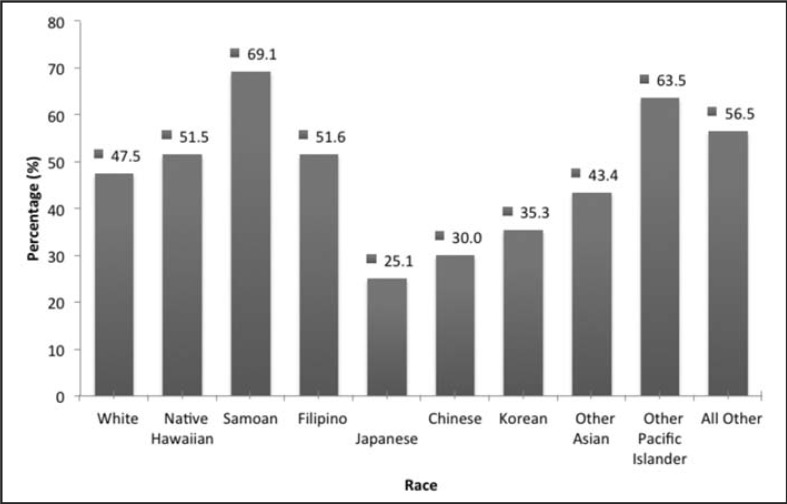
Overall, less than half of the mothers were counseled on IPV during prenatal care (47.7%), and almost 1 in 16 women who had a live birth reported having experienced IPV in the prior year from a current/former husband or partner (6.4%). The weighted proportions for receipt of PNC counseling on IPV, by race were: 47.5% White, 51.5% Native Hawaiian, 69.1% Samoan, 51.6% Filipino, 25.1% Japanese, 30.0% Chinese, 35.3% Korean, 43.4% other Asian, 63.5% other Pacific Islander, and 56.5% all others (Figure 1).
Figure 1.
Weighted Percentages of Receipt of Prenatal Health Care Counseling in Intimate Partner Violence, by Race.
Logistic Regression Analyses
In the crude models, Samoan, Native Hawaiian, Filipino, other Pacific Islander, and all other mothers were significantly more likely to report receiving PNC counseling on IPV compared to White mothers (Table 2). Japanese, Chinese, and Korean mothers were less likely to report receiving PNC counseling in IPV. In the final models adjusted for age, marital status, health insurance, education, employment/school, household income, and having experienced IPV, Samoan mothers were still more likely to have received PNC counseling in IPV, whereas Japanese, Chinese, and Korean mothers were less likely to have received PNC counseling in IPV compared to White mothers. However, in the adjusted analysis, Native Hawaiian mothers became less likely to report receiving PNC counseling in IPV compared to White mothers. This reversal from the unadjusted analysis was present when education, income and marital status were each individually added to the model with just race. The initial differences seen in Filipino, other Pacific Islanders, other Asian, and all others were no longer significant in the fully adjusted models.
Table 2.
Multivariate Analyses of Receipt of Prenatal Health Care Counseling in Intimate Partner Violence Among Mothers in Hawai‘i, Pregnancy Risk Assessment Monitoring System, 2004–2008.
| Crude OR [95% CI] | Multivariate AOR [95% CI] | |||
| Race (White†) | ||||
| Native Hawaiian | 1.18 (1.02, 1.35) | 0.82 (0.70, 0.96) | ||
| Filipino | 1.18 (1.02, 1.36) | 1.06 (0.90, 1.24) | ||
| Japanese | 0.37 (0.21, 0.44) | 0.44 (0.36, 0.53) | ||
| Chinese | 0.47 (0.39, 0.57) | 0.56 (0.46, 0.69) | ||
| Korean | 0.60 (0.47, 0.77) | 0.69 (0.53, 0.90) | ||
| Samoan | 2.48 (1.80, 3.42) | 1.51 (1.08, 2.12) | ||
| Other Asian American | 0.85 (0.59, 1.22) | 0.78 (0.51, 1.18) | ||
| Other Pacific Islander | 1.92 (1.49, 2.49) | 1.20 (0.89, 1.61) | ||
| All Other | 1.44 (1.16, 1.78) | 1.21 (0.95, 1.54) | ||
| Age | 0.94 (0.93, 0.95) | 0.97 (0.96, 0.98) | ||
| Marital status (Married†) | ||||
| Not married | 1.70 (1.54, 1.87) | 1.00 (0.88, 1.14) | ||
| Health insurance (Private†) | ||||
| Medicaid | 2.40 (2.11, 2.72) | 1.46 (1.23, 1.73) | ||
| Uninsured | 1.58 (1.37, 1.82) | 1.07 (0.91, 1.27) | ||
| Education (College Graduate†) | ||||
| Some college | 2.05 (1.81, 2.33) | 1.43 (1.24, 1.65) | ||
| High school or equivalent or less than a high school education | 3.30 (2.94, 3.71) | 1.96 (1.69, 2.27) | ||
| Employed/In school (Yes†) | 0.80 (0.73, 0.88) | 0.91 (0.81, 1.01) | ||
| Household income ($50,000+†) | ||||
| <$10,000 | 2.80 (1.67, 2.15) | 1.49 (1.23, 1.80) | ||
| $10,000–24,999 | 2.54 (2.23, 2.90) | 1.52 (1.29, 1.78) | ||
| $25,000–49,999 | 1.90 (1.67, 2.15) | 1.34 (1.17, 1.54) | ||
| Experienced intimate partner violence before/during pregnancy (Yes†) | 1.24 (1.02, 1.50) | 0.95 (0.77, 1.18) | ||
Notes: AOR = adjusted odds ratio; results significant at the P<.05 level are italicized. Models were adjusted for age, marital status, health insurance, education, employment/in school, household income, and experience with physical IPV.
Reference group.
In the adjusted models, age, marital status, employment and experience with IPV were found to be non-significant in mothers reporting receiving PNC counseling in IPV. The adjusted analyses also revealed that compared to mothers with private health insurance, mothers who had Medicaid were significantly more likely to report receiving PNC counseling in IPV; however, there was no significant difference compared with the uninsured mothers. Furthermore, the adjusted analyses showed that compared to mothers who were college graduates, mothers who received less than a high school education or some college were significantly more likely to report receiving PNC counseling in IPV. Additionally, compared to mothers with a household income of $50,000 or more, mothers with a household income of less than $50,000 were significantly more likely to report receiving PNC counseling in IPV.
Discussion
Fewer than half of the mothers (47.7%) discussed IPV with their provider during at least one of their PNC visits. Unadjusted analyses revealed that Samoan, Native Hawaiian, Filipino, other Pacific Islander, and all other mothers are more likely to report receipt of prenatal counseling on IPV than White mothers, but after controlling for a number of factors, the direction of association among Native Hawaiians changed. Thus, adjusted analyses revealed that compared to White mothers, Native Hawaiian, Japanese, Chinese and Korean mothers were significantly less likely to report receiving PNC counseling on IPV. Adjusted analyses revealed that Samoans were significantly more likely to report receipt of PNC counseling on IPV, while other associations became statistically insignificant. The reasons for these observations warrant further explorations, as universal counseling on IPV should be conducted similarly across all racial populations.
While overall, 6.4% of recent mothers reported experience with IPV, and the crude OR (1.24, 95% CI (1.02–1.50) indicated those who experienced IPV were more likely to be counseled, the adjusted analysis indicated that there was no relationship between a mothers' experience with IPV and mothers' reporting having received PNC counseling on IPV. This study demonstrated that Native Hawaiian, Korean, Chinese, and Japanese mothers were all less likely than Whites to report receiving prenatal counseling for IPV during pregnancy. Many of these groups have higher prevalence estimates for experiencing IPV compared to Whites with Native Hawaiians (10.0%), Samoan (8.0%), and Filipino (6.2%) having higher estimates, while Chinese mothers (2.3%) having lower estimates compared to White mothers (3.9%) in Hawai‘i (PRAMS, 2004–2008).28 This highlights the need to provide appropriate counseling for those most at risk for IPV. Furthermore, Native Hawaiians are more likely to experience IPV, yet less likely to be screened for IPV in PNC visits. Though Chinese mothers reported lower rates of having experienced IPV, they are also less likely to receiving PNC counseling on IPV compared to White mothers. The reasons for these observations warrant further explorations, as universal counseling in IPV should be conducted similarly across all racial populations.
Strengths
PRAMS is a population based surveillance system that collects important data on many maternal and child health issues. Hawai‘i PRAMS collects detailed sub-population data, which is unique given that data on Asian Americans and NHOPI are often reported as an aggregate in many national analyses due to sample size constraints. Hawai‘i PRAMS includes large sample sizes of some of these subgroups. Therefore, this dataset offers researchers the distinct opportunity to investigate racial differences for some of these subgroups which, in turn, allows a more in-depth understanding of these subgroups' health status and experiences with health care.
Since the DHHS guidelines regarding free screening and counseling for interpersonal and domestic violence for all women takes effect August 2012 (for all new health plans), this study's findings may be utilized as baseline data to assist in the evaluation of the effectiveness of the adoption of the new guidelines in Hawai‘i.
Limitations
As with many surveys, PRAMS data are self-reported. PRAMS are administered after the delivery of a live infant; thus, mothers are asked to recall their experiences including whether they have received advice at any point during pregnancy related to IPV. Moreover, PRAMS asks women about their experience with physical IPV but not emotional abuse, which is an important IPV type that deserves equal merit, particularly because prior research has demonstrated that emotional abuse results in similarly poor health outcomes as physical abuse.29 Tiwari and colleagues, for instance, reported that psychological IPV was more common among Chinese women.30 Furthermore, the experience of physical IPV is likely under-reported even in this primarily mail-based survey.
Another limitation of this study described in the methods section is that race categorization is limited to the single race reported in the Hawai‘i birth certificate data. Due to the large proportion of mothers who are of multiple race groups in Hawai‘i, the ability to generalize these results is limited when considering those reporting more than one race. Other race groups including specific Asian American (eg, Vietnamese) and NHOPI subpopulations (eg, Guamanian) occur in small proportions in the State and thus are not sufficiently represented in the Hawai‘i PRAMS sample. The Hawai‘i PRAMS is also provided only as an English survey so women who do not feel comfortable with English may not complete the survey and thus, may be under-represented.
A final limitation is that PRAMS only surveys women with pregnancies that result in a live birth. Rates for PNC counseling in IPV may be different among women who experienced spontaneous or induced abortion and this may vary by race/ethnicity.
Study Implications/Next Steps
While this study analyzed racial differences in receiving PNC counseling in IPV among mothers, it is also important to be aware of issues related to barriers in accessing prenatal health care. For example, a previous study utilized the 2004–07 Hawai‘i PRAMS data to determine the association between IPV and PNC access by race. This study reported that the experience with IPV was significantly associated with NHOPI and Asian Americans reporting one or more barriers to accessing prenatal health care.31 This finding suggests that these populations encounter more barriers (ie, logistical; financial/health insurance; personal) and, thus, may have fewer opportunities to receive PNC counseling.
Future health services intervention research should include a focus on both women who experience high rates of IPV as well as those women that are less likely to receive appropriate counseling in IPV during prenatal care. Additional research related to particular Asian American and NHOPI subpopulations is needed to gain a better understanding of the PNC experience in regards to IPV screening and counseling.
In addition to research, findings from this study will have important programmatic implications. For example, because more than half of the mothers in this study reported that their providers did not talk to them about IPV during any of their PNC visits, it may be appropriate to provide training for providers regarding the importance of screening for risk as well as providing appropriate treatment and/or referral. While it is highly likely that many health care institutions would inform their providers of the new DHHS guidelines to screen and counsel for IPV, some providers may require training if they have not conducted such screenings on a regular basis prior to the implementation of the new guidelines. Changes in health practices that facilitate provider-patient IPV discussion (ie, prompts and cues to assess for IPV risk) may be required if routine assessments are to actually occur. Finally, it is important to state that asking women about IPV does not increase the risk of harm to the woman's health or safety;32 rather, asking women about IPV is a first and necessary step to ensure the safety of the women, a healthy pregnancy and quality of life.
Acknowledgements
We would like to thank the Hawai‘i PRAMS Program and the Centers for Disease Control and Prevention for providing us data access.
Conflict of Interest
None of the authors identify a conflict of interest.
References
- 1.Saltzman LE, Johnson CH, Gilbert BC, Goodwin MM. Physical abuse around the time of pregnancy: an examination of prevalence and risk factors in 16 states. Matern Child Health J. 2003 Mar;7(1):31–43. doi: 10.1023/a:1022589501039. [DOI] [PubMed] [Google Scholar]
- 2.Gazmararian JA, Lazorick S, Spitz AM, Ballard TJ, Saltzman LE, Marks JS. Prevalence of violence against pregnant women. JAMA. 1996 Jun 26;275(24):1915–1920. [PubMed] [Google Scholar]
- 3.Silverman JG, Decker MR, Reed E, Raj A. Intimate partner violence victimization prior to and during pregnancy among women residing in 26 U.S. states: associations with maternal and neonatal health. Am J Obstet Gynecol. 2006 Jul;195(1):140–148. doi: 10.1016/j.ajog.2005.12.052. [DOI] [PubMed] [Google Scholar]
- 4.Danielson KK, Moffitt TE, Caspi A, Silva PA. Comorbidity between abuse of an adult and DSM-III-R mental disorders: evidence from an epidemiological study. Am J Psychiatry. 1998 Jan;155(1):131–133. doi: 10.1176/ajp.155.1.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Golding JM. Intimate Partner Violence as a Risk Factor for Mental Disorders: A Meta-Analysis. Journal of Family Violence. 1999;14(2):99–132. [Google Scholar]
- 6.Plichta S. The effects of woman abuse on health care utilization and health status: a literature review. Womens Health Issues. 1992 Fall;2(3):154–163. doi: 10.1016/s1049-3867(05)80264-6. [DOI] [PubMed] [Google Scholar]
- 7.Stark E, Flitcraft A. Killing the beast within: woman battering and female suicidality. Int J Health Serv. 1995;25(1):43–64. doi: 10.2190/H6V6-YP3K-QWK1-MK5D. [DOI] [PubMed] [Google Scholar]
- 8.Norton IM, Manson SM. An association between domestic violence and depression among Southeast Asian refugee women. J Nerv Ment Dis. 1992 Nov;180(11):729–730. doi: 10.1097/00005053-199211000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Basile K. Sexual Violence in the Lives of Girls and Women. In: Kendall-Tackett KA, editor. Handbook of Women, Stress, and Trauma. New York: Brunner-Routledge Taylor Francis Group; 2005. pp. 101–122. [Google Scholar]
- 10.World Health Organization, author. World report on violence and health: Summary. [July 21, 2011]. http://www.who.int/violence_injury_prevention/violence/world_report/en/summary_en.pdf.
- 11.Murphy CC, Schei B, Myhr TL, Du Mont J. Abuse: a risk factor for low birth weight? A systematic review and meta-analysis. CMAJ. 2001 May 29;164(11):1567–1572. [PMC free article] [PubMed] [Google Scholar]
- 12.Durant T, Colley Gilbert B, Saltzman LE, Johnson CH. Opportunities for intervention: discussing physical abuse during prenatal care visits. Am J Prev Med. 2000 Nov;19(4):238–244. doi: 10.1016/s0749-3797(00)00232-4. [DOI] [PubMed] [Google Scholar]
- 13.American Congress of Obstetricians and Gynecologists, author. Screening Tools—Domestic Violence. [September 10, 2011]. http://www.acog.org/departments/dept_notice.cfm?recno=17&bulletin=585.
- 14.U.S. Department of Health & Human Services, author. Affordable Care Act Rules on Expanding Access to Preventive Services for Women. 2011. [September 9, 2011]. http://www.healthcare.gov/news/factsheets/womensprevention08012011a.html.
- 15.Horan DL, Chapin J, Klein L, Schmidt LA, Schulkin J. Domestic violence screening practices of obstetrician-gynecologists. Obstet Gynecol. 1998 Nov;92(5):785–789. doi: 10.1016/s0029-7844(98)00247-6. [DOI] [PubMed] [Google Scholar]
- 16.Humphreys J, Tsoh JY, Kohn MA, Gerbert B. Increasing discussions of intimate partner violence in prenatal care using Video Doctor plus Provider Cueing: a randomized, controlled trial. Womens Health Issues. 2011 Mar-Apr;21(2):136–144. doi: 10.1016/j.whi.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ta VM, Juon HS, Gielen AC, Steinwachs D, Duggan A. Disparities in use of mental health and substance abuse services by Asian and Native Hawaiian/other Pacific Islander women. Journal of Behavorial Health Services and Research. 2008 Jan;35(1):20–36. doi: 10.1007/s11414-007-9078-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Humes KR, Jones NA, Ramirez RR, U.S. Census Bureau Overview of Race and Hispanic: 2010. [September 9, 2011]. http://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf.
- 19.U.S. Census Bureau, author. Facts for Features: Asian/Pacific American Heritage Month: May 2011. 2011. [September 9, 2011]. http://www.census.gov/newsroom/releases/archives/facts_for_features_special_editions/cb11-ff06.html.
- 20.U.S. Census Bureau, author. Profile of General Population and Housing Characteristics: 2010 Demographic Profile Data (Hawaii) [September 12, 2011]. http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=DEC_10_DP_DPDP1&prodType=table.
- 21.U.S. Census Bureau, author. Profile of General Population and Housing Characteristics: 2010: Hawaii. 2010 American Community Survey 1-Year Estimates. 2010. [October 12, 2011]. http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=DEC_10_DP_DPDP1&prodType=table.
- 22.Reeves T, Bennett C. The Asian and Pacific Islander Population in the United States: March 2002. Vol. 2005. Washington, DC.: Current Population Reports, P20-540, U.S. Census Bureau; 2003. [Google Scholar]
- 23.Foo LJ. Introduction. Asian American Women: Issues, Concerns, and Responsive Human and Civil Rights Advocacy. 2002. [January 29, 2008]. pp. 11–20. Available at: http://www.aapip.org/pdfs/aaw_02_preface.pdf.
- 24.U.S. Department of Health and Human Services, author. Healthy People 2020 Objectives. 2011. [April 26, 2011]. http://www.healthypeople.gov/2020/topicsobjectives2020/pdfs/HP2020objectives.pdf.
- 25.Sorenson CA, Wood B, Prince EW. Race & ethnicity data: Developing a common language for public health surveillance in Hawaii. Californian Journal of Health Promotion. 2003;1(Special Issue Hawaii):91–104. [Google Scholar]
- 26.Hamilton BE, Ventura SJ. Characteristics of births to single- and multiple-race women: California, Hawaii, Pennsylvania, Utah, and Washington, 2003. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2007 May 3;55(15):1–20. [PubMed] [Google Scholar]
- 27.Stata Statistical Software: Release 11.0 [computer program] College Station: Stata Corporation; 2009. [Google Scholar]
- 28.Hawaii PRAMS, Hawaii Department of Health, Family Health Services Divison, author. Hawaii PRAMS Trend Report 2000–2008. Honolulu, HI: 2010. [Google Scholar]
- 29.Coker AL, Smith PH, Bethea L, King MR, McKeown RE. Physical health consequences of physical and psychological intimate partner violence. Arch Fam Med. 2000 May;9(5):451–457. doi: 10.1001/archfami.9.5.451. [DOI] [PubMed] [Google Scholar]
- 30.Tiwari A, Fong DY, Yuen KH, et al. Effect of an advocacy intervention on mental health in Chinese women survivors of intimate partner violence: a randomized controlled trial. JAMA. 2010 Aug 4;304(5):536–543. doi: 10.1001/jama.2010.1052. [DOI] [PubMed] [Google Scholar]
- 31.Ta VM, Hayes D. Racial differences in the association between partner abuse and barriers to prenatal health care among Asian and native Hawaiian/other Pacific Islander women. Matern Child Health J. 2010 May;14(3):350–359. doi: 10.1007/s10995-009-0463-4. [DOI] [PubMed] [Google Scholar]
- 32.Koziol-McLain J, Giddings L, Rameka M, Fyfe E. Intimate partner violence screening and brief intervention: experiences of women in two New Zealand Health Care Settings. J Midwifery Womens Health. 2008 Nov-Dec;53(6):504–510. doi: 10.1016/j.jmwh.2008.06.002. [DOI] [PubMed] [Google Scholar]